Professional Documents
Culture Documents
Cardiovascular System: Blood
Uploaded by
Koh Yen SinOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiovascular System: Blood
Uploaded by
Koh Yen SinCopyright:
Available Formats
Cardiovascular system: Blood 1) Blood: consists of plasma and formed elements eg RBC, WBC, platelets Function: (a) Transport
of dissolved gases, which are oxygen and carbon dioxide (b) Distribution of nutrients eg absorption from digestive tract and the release from liver or adipose tissue (c) Transport of metabolic wastes to the site of excretion such as the kidneys (d) Transport of enzymes and hormones to specific target tissues (e) Act as a buffer to stabilize pH and electrolyte composition of intestinal fluids eg lactic acids in muscles (f) Prevent loss of fluid though damaged vessels or injured sites (g) Defense against toxins and pathogens eg immune system (h) Stabilization of body temperature eg through blood flow Hypovolemic: low blood volume Normovolemic: normal blood volume Hypervolemic: excessive blood volume 2) Plasma - 55% of volume of whole blood - Water: 92% of the plasma volume - Differences between interstitial fluid and plasma Concentration of dissolved - Oxygen concentration: higher in oxygen and carbon dioxide plasma oxygen diffuses out of blood vessels into the peripheral tissues - Carbon dioxide concentration: lower in plasma carbon dioxide diffuse from the tissues into the blood vessels Concentration of dissolved - Plasma has significant quantities of proteins protein: large size and globular shape prevent protein from crossing capillary walls 3 major classes of plasma proteins Albumins - Major contribution to osmotic pressure of plasma - Transport of fatty acids, steroid hormones and other substances by attaching to lipids Globulins - Immunoglobulin ( antibodies): attack foreign proteins and pathogens - Transport globulin: bind to small ions, hormones that are insoluble or may be filtered out of the blood by the kidneys Fibrinogen - Essential for blood clotting - Fibrinogen interact to form large and insoluble strands
of fibrin; provides basic scaffold for blood clot 3) Red Blood cells (erythrocytes) - Hematocrit: % of whole blood contributed by formed elements ; closely approximately the volume of erythrocytes; often refer as packed cell volume - Structure of red blood cells Biconcave region with a think central region and thick outer margin Biconcave shape: provide strength and flexibility and disproportionately large surface area Large surface are: permit rapid diffusion of oxygen biconcave shape: form stacks called rouleaux can bend and flex: able to squeeze through small-diameter capillaries - RBC life span and circulation Lack mitochondria, ER, ribosomes and nuclei Obtain energy through anaerobic respiration and rely on glucose from surrounding plasma Protein synthesis cannot occur: proteins cannot be replaced Wear and tear and no replaced mechanism: 120 days life span - Haemoglobin Responsible for the transport of oxygen and carbon dioxide Red pigment: oxygenated blood has bright red colour, deoxygenated blood has deep red colour; account for the colour in artery and veins Structure: 2 alpha- and 2 beta- chains; each subunits contains one heme group; each heme group has an iron ion which can interact with oxygen The iron-oxygen interaction is weak; oxygen is able to dissociate with iron ion without destroying the integrity of RBC Carbon dioxide bind to the amino acids of the globin subunit - Blood types Surface antigens ( agglutinogens): glycolipids or glycoproteins whose characteristics are genetically determined A,B, D (Rh) Antibodies ( immunoglobulin- agglutinins) attack foreign surface antigens; RBC clump together: known as agglutination or hemolyze, plug small vessels in organs such as kidneys, depriving them of circulation and damaging them 4) Leucocytes ( White blood cells) - Function: defend the body from invasion by pathogens and remove toxins, wastes and abnormal or damaged cells - Two main classes of leukocytes: granular leukocytes- have granular inclusion and agranular leukocytes- no cytoplasmic granules - Leukopenia- inadequate number of leucocytes. Leukocytosis- excessive number of leucocytes
Diapedesis- the migration of white blood cells through the intact walls of blood vessels and into the surrounding tissue Granular leucocytes- Neutrophils, eosinophils and basophils Agranular leuocytes- monocytes and lymphocytes Neutrophils Cytoplasm- with pale, neutral staining granules containing lysosomal enzymes and bactericidal compounds Polymorphonuclear leukocytes nucleus with many lobes 1st to arrive at an injury site Function: attack and digest bacteria Short life span: 12 hours. Its breakdown release chemical that attract other neutrophils and others that has a broad antibiotic activity against the pathogens Eosinophils ( Acidophils) Granules stained with eosin: an acidic red dye deep red granules Bilobed nucles ( two lobed nucleus) Are phagocytic cells attracted to foreign compounds that have reacted with the circulating antibodies Increase drastically during an allergic reaction Are attached to injury sites, where they release enzymes to reduce the degree of inflammation and to control its spread to adjacent cells Basophils Numerous granules that stain with basic dyes- deep purple or blue Migrate to sites of injury and cross the capillary endothelium to accumulate within the damaged tissues discharge their granules into the interstitial fluids Granules- contains histamine (dilates blood vessels) and heparin (prevent blood clotting) increase inflammatory response at injury sites by increasing capillary and venule permeability. Release chemicals that stimulate mast cells and attract basophils to the area Monocytes Largest White blood cells Kidney bean-shaped nucleus Called free macrophages outside the bloodstream. Highly mobile as compared to the fixed immobile macrophages Usually arrive at the injury site shortly after the first neutrophils Release chemicals that attract and stimulate other monocytes and phagocytic cells Release substances that lure fibroblasts into the region Lymphocytes: Primary cells of the lymphoid system For specific immunity: an ability to mount a counterattack on invading pathogens or foreign proteins on an individual basis T cells: enter peripheral tissues and attack pathogens directly
B cells: differentiate into plasmocytes and produce antibodies that attack pathogens at distant portions of the body NK cells: for immune surveillance- destruction of abnormal tissue cells 5) Blood conditions - Sickle cell anemia Mutation affecting the amino acid sequence of the beta-chain of haemoglobin molecules After releasing the oxygen molecules, the Hb molecules clustered into rods, and the cells become stiff and curved- trapped in capillaries and lack of oxygen in peripheral tissues - Anemia: the oxygen-carrying capacity of blood is reduced due to low hematocrit value or reduced amount of haemoglobin - Polycythemia: elevated hematocrit value with normal blood volume Erythrocytosis: polycythemia of RBC Polycythemia vera: an increase in all blood cells - Hemophilia: inherited blood disorder that is characterized by inadequate production of clotting factors 6) Platelets ( Thrombocytes) - Normal red bone marrow megakaryocytes: enormous cells with large nuclei. Nucleus: lobed or ring-shaped. Contains many GA, ribosomes and mitochondria. - Megakaryocytes manufacture membrane, enzymes and structural proteins shedding cytoplasm in membrane-enclosed packets: platelets - Circulates for 10-12 days before being removed by phagocytes - 1/3 of platelets are stored in spleen and other vascular organs as reserves for circulatory crisis such as severe bleeding - Thrombocytopenia and thrombocytosis: low platelet count and high platelet count - Functions: Transport of chemical important for clotting process Formation of temporary patch at the walls of damaged vessels via clumping of platelets Active contraction after formation of clot has occurred: reduces size of clot 7) Hematopoiesis: process of blood formation - Pluripotential stem cells myeloid stem cells and lymphoid stem cells - Myeloid stem cells: two form red blood cells and megakaryocytes. Three form various form of leucocytes - Lymphoid stem cells: form T-cells and plasmocytes
Erythropoiesis: process of red blood cells formation Produced in red bone marrow: vertebrae, sternum, ribs, skull, scapulae, pelvis, proximal limb bones Fatty yellow bone marrow can be converted into red bone marrow Regulated by Erythropoiesis- stimulating hormone or erythropoietin Erythropoietin is secreted and produced under hypoxic condition, in the kidneys Two major effects: increased rate of cell division in erythroblasts and stem cells that produced erythroblasts, speeds up the rate of maturation in RBC, primarily by accelerating the rate of hemoglobin synthesis Stages of erythropoiesis: erythroblasts ( immature cells that actively produce hemoglobin) reticulocytes( nuclei shredded) mature erythrocytes Leukopoiesis: process of forming white blood cells Originate in bone marrow Lymphopoiesis: also originate in bone marrow, but many migrate to thymus Immature B-cells and NK cells: Bone marrow. Immature T-cells: thymus glands
You might also like
- Composition and Functions: BloodDocument86 pagesComposition and Functions: BloodYeyeh SantosNo ratings yet
- The Cardiovascular SystemDocument79 pagesThe Cardiovascular Systemhed-ikaquinoNo ratings yet
- Chapter 19 - BloodDocument5 pagesChapter 19 - Bloodtomorrow.today.yesterday .yesterdayNo ratings yet
- Blood Components and FunctionsDocument10 pagesBlood Components and FunctionsShiela Mae SagayoNo ratings yet
- Blood CirculatoryDocument5 pagesBlood CirculatoryRekesh SaeedNo ratings yet
- Unit 2-Blood Guided NotesDocument5 pagesUnit 2-Blood Guided NotesJeanette IrambonaNo ratings yet
- Blood and Lymphatic PhysiologyDocument63 pagesBlood and Lymphatic PhysiologyhardianNo ratings yet
- Blood ReviewDocument13 pagesBlood ReviewDeleted AccountNo ratings yet
- LEC1 - Definition & Scope of Hematology To Red Blood Cell StudiesDocument11 pagesLEC1 - Definition & Scope of Hematology To Red Blood Cell StudiessuperbbloomNo ratings yet
- BLG111Document7 pagesBLG111Manasseh LawrenceNo ratings yet
- Blood HBDocument31 pagesBlood HBBHUWAN BASKOTANo ratings yet
- Blood Lectie Generala Eng-2454Document56 pagesBlood Lectie Generala Eng-2454IngaŞaragovNo ratings yet
- Components of Blood - Red Blood Cells, White Blood Cells, and PlateletsDocument20 pagesComponents of Blood - Red Blood Cells, White Blood Cells, and PlateletsVishal SharmaNo ratings yet
- Blood Composition and Functions: Indian Institute of Technology PatnaDocument41 pagesBlood Composition and Functions: Indian Institute of Technology PatnaHritik KumarNo ratings yet
- L32: Blood Cells: Learning ObjectivesDocument10 pagesL32: Blood Cells: Learning Objectives李超然No ratings yet
- Components of BloodDocument9 pagesComponents of BloodEricBuguinaNo ratings yet
- Nurs 107 Blood Physiology Lecture 4Document46 pagesNurs 107 Blood Physiology Lecture 4Ann AgyeiwaaNo ratings yet
- Chapter 10 Blood AnatomyDocument5 pagesChapter 10 Blood AnatomyChiara Mae NiñalNo ratings yet
- PSG 712 Blood-1Document54 pagesPSG 712 Blood-1preciousNo ratings yet
- BLOOD Update-1Document56 pagesBLOOD Update-1ahmadfadi343No ratings yet
- Blood Summary NotesDocument4 pagesBlood Summary NotesLaura FernandezNo ratings yet
- Blood: Figure 1: Shows Separated Blood Layers by CentrifugeDocument7 pagesBlood: Figure 1: Shows Separated Blood Layers by Centrifugeحسين مهديNo ratings yet
- Composition of Blood and Cellular Elements: Learning ObjectivesDocument11 pagesComposition of Blood and Cellular Elements: Learning Objectivesmarinak_6No ratings yet
- Blood and Its Components-NotesDocument10 pagesBlood and Its Components-NotesKelvin RequenaNo ratings yet
- Lecture 1 - Introduction To HematologyDocument30 pagesLecture 1 - Introduction To Hematologyimam100% (1)
- Blood Anatomy Physiology HandoutsDocument6 pagesBlood Anatomy Physiology HandoutsKids JangNo ratings yet
- Blood and Immunity PowerpointDocument94 pagesBlood and Immunity Powerpointapi-263357086100% (1)
- Haemopoiesis: Composition of Whole Blood & Its ComponentsDocument8 pagesHaemopoiesis: Composition of Whole Blood & Its ComponentsSafiya JamesNo ratings yet
- Circulatory SystemDocument74 pagesCirculatory SystemMICHAEL AFIADENYONo ratings yet
- Blood Part 1Document35 pagesBlood Part 1Keziah TampusNo ratings yet
- BLOODDocument9 pagesBLOODArianne Jen GenotivaNo ratings yet
- The Cardiovascular System BloodDocument102 pagesThe Cardiovascular System BloodJerilee SoCute WattsNo ratings yet
- BLOOD PresentationDocument33 pagesBLOOD PresentationLezlie Jane SahaliNo ratings yet
- 1.anaemia Intro, Retic, IndicesDocument69 pages1.anaemia Intro, Retic, IndicesInaGargNo ratings yet
- Chapter 17 Anatomy and Physiology NotesDocument10 pagesChapter 17 Anatomy and Physiology NotesZachary WatsonNo ratings yet
- Anaphy Midterm Notes (The Blood Summary)Document4 pagesAnaphy Midterm Notes (The Blood Summary)Zosia Sage100% (1)
- CH 15 BloodDocument6 pagesCH 15 Bloodsann1992No ratings yet
- Histology of Blood Cells and FunctionsDocument6 pagesHistology of Blood Cells and FunctionsgerginNo ratings yet
- BloodDocument56 pagesBloodGail Justine Chongco GonzalesNo ratings yet
- Darah Dan LimfatikDocument55 pagesDarah Dan Limfatikadisty sncNo ratings yet
- Anatomi Fisiologi Manusia: HematologiDocument54 pagesAnatomi Fisiologi Manusia: HematologiARUMNo ratings yet
- Hematology Lecture: Introduction to Blood Cells & FunctionsDocument3 pagesHematology Lecture: Introduction to Blood Cells & FunctionspuhtaytoeNo ratings yet
- Blood Cells and The Hematopoetic SystemDocument53 pagesBlood Cells and The Hematopoetic SystemMeet RandhawaNo ratings yet
- 4 BloodDocument43 pages4 BloodAn ThịnhNo ratings yet
- Haemolytic Anaemia: HyperspleenismDocument21 pagesHaemolytic Anaemia: HyperspleenismZabihullahNo ratings yet
- Histology of Blood CellsDocument80 pagesHistology of Blood CellsKamal AhmedNo ratings yet
- BLOODDocument12 pagesBLOODRinalyn BalderramaNo ratings yet
- Biology ReviewerDocument5 pagesBiology Reviewer13l4nk17No ratings yet
- Blood Notes PDFDocument13 pagesBlood Notes PDFsyedurrahman855No ratings yet
- CVS BloodDocument39 pagesCVS BloodMohan GuptaNo ratings yet
- Blood cells, coagulation overviewDocument7 pagesBlood cells, coagulation overviewsenjicsNo ratings yet
- Chapter 17 Blood and 18 Review AnswersDocument4 pagesChapter 17 Blood and 18 Review Answersmamun0zNo ratings yet
- The Hematologic SystemDocument7 pagesThe Hematologic SystemanyaNo ratings yet
- Heamatology Chapter 1Document38 pagesHeamatology Chapter 1Taima'a AlamaratNo ratings yet
- Kelainan DarahDocument136 pagesKelainan DarahMerina P. DwiNo ratings yet
- Blood and Bone Marrow Cells and FunctionsDocument52 pagesBlood and Bone Marrow Cells and FunctionsJophter BandaNo ratings yet
- Blood Cells and Anemia GuideDocument5 pagesBlood Cells and Anemia GuideAmarissa A. TsabitaNo ratings yet
- Kuliah 5 Blood-SsDocument31 pagesKuliah 5 Blood-SsputracahyaNo ratings yet
- Chapter 30 Nursing Assessment Hematologic SystemDocument14 pagesChapter 30 Nursing Assessment Hematologic Systemmedic-24100% (1)
- Time Series Notes From TextbookDocument15 pagesTime Series Notes From TextbookKoh Yen SinNo ratings yet
- LSM3221 RevisionDocument20 pagesLSM3221 RevisionKoh Yen SinNo ratings yet
- Lecture 3 and 4 LSM2241Document6 pagesLecture 3 and 4 LSM2241Koh Yen SinNo ratings yet
- The Ecstacy of Communication - BaudrillardDocument5 pagesThe Ecstacy of Communication - BaudrillardMardawud JamiNo ratings yet
- Medieval BodiesDocument2 pagesMedieval BodiesKoh Yen SinNo ratings yet
- BrailleDocument1 pageBrailleKoh Yen SinNo ratings yet
- Essay Writing 101Document7 pagesEssay Writing 101Koh Yen SinNo ratings yet
- Yen Sin LSM 1103 Cheat SheetDocument2 pagesYen Sin LSM 1103 Cheat SheetKoh Yen SinNo ratings yet
- Vturn-NP16 NP20Document12 pagesVturn-NP16 NP20José Adalberto Caraballo Lorenzo0% (1)
- WSO 2022 IB Working Conditions SurveyDocument42 pagesWSO 2022 IB Working Conditions SurveyPhạm Hồng HuếNo ratings yet
- WSAWLD002Document29 pagesWSAWLD002Nc BeanNo ratings yet
- SM RSJ 420 800Document77 pagesSM RSJ 420 800elshan_asgarovNo ratings yet
- Rockwool 159: 2.2 Insulation ProductsDocument1 pageRockwool 159: 2.2 Insulation ProductsZouhair AIT-OMARNo ratings yet
- Treatment of Fruit Juice Concentrate Wastewater by Electrocoagulation - Optimization of COD Removal (#400881) - 455944Document5 pagesTreatment of Fruit Juice Concentrate Wastewater by Electrocoagulation - Optimization of COD Removal (#400881) - 455944Victoria LeahNo ratings yet
- NLOG GS PUB 1580 VGEXP-INT3-GG-RPT-0001.00 P11-06 Geological FWRDocument296 pagesNLOG GS PUB 1580 VGEXP-INT3-GG-RPT-0001.00 P11-06 Geological FWRAhmed GharbiNo ratings yet
- Ethamem-G1: Turn-Key Distillery Plant Enhancement With High Efficiency and Low Opex Ethamem TechonologyDocument25 pagesEthamem-G1: Turn-Key Distillery Plant Enhancement With High Efficiency and Low Opex Ethamem TechonologyNikhilNo ratings yet
- Insurance Principles, Types and Industry in IndiaDocument10 pagesInsurance Principles, Types and Industry in IndiaAroop PalNo ratings yet
- Week 6 Blood and Tissue FlagellatesDocument7 pagesWeek 6 Blood and Tissue FlagellatesaemancarpioNo ratings yet
- MR23002 D Part Submission Warrant PSWDocument1 pageMR23002 D Part Submission Warrant PSWRafik FafikNo ratings yet
- Aço X6NiCrTiMoVB25!15!2 - 1.4980 Austenitic SteelDocument2 pagesAço X6NiCrTiMoVB25!15!2 - 1.4980 Austenitic SteelMoacir MachadoNo ratings yet
- M-LVDT: Microminiature Displacement SensorDocument2 pagesM-LVDT: Microminiature Displacement Sensormahdi mohammadiNo ratings yet
- TSS-TS-TATA 2.95 D: For Field Service OnlyDocument2 pagesTSS-TS-TATA 2.95 D: For Field Service OnlyBest Auto TechNo ratings yet
- Test Report OD63mm PN12.5 PE100Document6 pagesTest Report OD63mm PN12.5 PE100Im ChinithNo ratings yet
- Business Startup Practical Plan PDFDocument70 pagesBusiness Startup Practical Plan PDFShaji Viswanathan. Mcom, MBA (U.K)No ratings yet
- The Danger of Microwave TechnologyDocument16 pagesThe Danger of Microwave Technologyrey_hadesNo ratings yet
- g21 Gluta MsdsDocument3 pagesg21 Gluta Msdsiza100% (1)
- 07 Chapter2Document16 pages07 Chapter2Jigar JaniNo ratings yet
- ItilDocument11 pagesItilNarendar P100% (2)
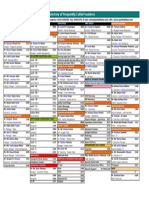
- Directory of Frequently Called Numbers: Maj. Sheikh RahmanDocument1 pageDirectory of Frequently Called Numbers: Maj. Sheikh RahmanEdward Ebb BonnoNo ratings yet
- 2020-11 HBG Digital EditionDocument116 pages2020-11 HBG Digital EditionHawaii Beverage GuideNo ratings yet
- Pictorial History of AOTADocument5 pagesPictorial History of AOTAThe American Occupational Therapy Association0% (4)
- Bio-Tank Guidelines for Indian RailwayDocument51 pagesBio-Tank Guidelines for Indian Railwayravi100% (2)
- Grade 3 science syllabus 1st and 2nd semesterDocument2 pagesGrade 3 science syllabus 1st and 2nd semesterelyzabeth SibaraniNo ratings yet
- Female Reproductive System Histology IDocument5 pagesFemale Reproductive System Histology ISolomon Seth SallforsNo ratings yet
- RA8485 Animal Welfare Act (Carabao Slaughter)Document2 pagesRA8485 Animal Welfare Act (Carabao Slaughter)Jazreth Gaile100% (1)
- of Types of Nuclear ReactorDocument33 pagesof Types of Nuclear Reactormandhir67% (3)
- CHAPTER3 Foundations of Individual BehaviorDocument32 pagesCHAPTER3 Foundations of Individual BehaviorLynoj AbangNo ratings yet
- Cement ReportDocument86 pagesCement ReportSohaibNo ratings yet