Professional Documents
Culture Documents
Does TLR2 Regulate Intestinal Inflammation
Uploaded by
Lavina D'costaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Does TLR2 Regulate Intestinal Inflammation
Uploaded by
Lavina D'costaCopyright:
Available Formats
318
Allan McI Mowat
DOI 10.1002/eji.200940232
Eur. J. Immunol. 2010. 40: 318320
Commentary
Does TLR2 regulate intestinal inammation?
Allan McI Mowat
Division of Immunology, Infection and Inammation, Glasgow Biomedical Research Centre, University of Glasgow, Scotland, UK
There is almost no aspect of the immune response that is not regulated by TLR. Initially described as drivers of the innate immune response to pathogens, it is now clear that the TLR family can also inuence most aspects of adaptive immunity, as well as determine how tissue cells interact with microbes in their environment. In particular, the intestine and its immune system must co-exist with an enormous community of commensal bacteria and are also on constant alert against invading pathogens. Unsurprisingly, there is therefore great interest in how TLR might regulate physiological and pathological reactions in the gut. An article in this issue of the European Journal of Immunology addresses this question with some elegant experiments that indicate that TLR2 is not essential for the pathogenesis or T-cell-mediated regulation of different models of inammatory bowel disease in mice.
Key words: Inammation . Intestinal immunity . TLR2 . Treg
See accompanying article by Boulard et al.
TLR and intestinal immune responses inammatory or protective?
TLR are expressed by many different cell types in the intestine, including macrophages, DC, T lymphocytes and intestinal epithelial cells [1]. Although it is controversial exactly which TLR are expressed by each cell type, TLR function is likely to be central to protective immunity against intestinal pathogens by activating innate effector cells, stimulating the uptake of pathogens by M cells in Peyers patches and inducing the production of cytokines and anti-bacterial peptides [2, 3]. Surprisingly, intestinal TLR also seem to be crucial for limiting inammatory responses and maintaining tissue integrity, indicating a complex interplay between the pro-inammatory and the homeostatic functions of these receptors [4, 5]. As a result, it has become accepted that the balance between these processes is likely to be important for understanding the pathogenesis of
inammatory bowel diseases such as Crohns disease and ulcerative colitis [6]. In support of this, virtually all rodent models of inammatory bowel disease (IBD) are entirely dependent on the presence of commensal bacteria and deletion of TLR signalling in e.g. MyD88 KO mice abolishes spontaneous IBD in IL-2 or IL-10 KO mice [7]. Administration of some TLR ligands has also been reported to exacerbate experimental IBD [8] and both TLR agonists and antagonists are under consideration as therapeutic agents in several human conditions. Given the genetic associations between IBD and polymorphisms in pattern recognition receptors such as NOD-2, TLR2 and TLR4 [9], it would clearly be important to dene the exact contributions of individual TLR to these processes.
TLR2 may not be pathogenic or protective in models of chronic colitis
In this issue of the European Journal of Immunology, Boulard et al. [10] focus their attention on TLR2 and use an elegant combination of experimental systems to show that this receptor
Correspondence: Professor Allan McI Mowat e-mail: a.m.mowat@clinmed.gla.ac.uk
& 2010 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim
www.eji-journal.eu
Eur. J. Immunol. 2010. 40: 318320
HIGHLIGHTS
319
is not required for gut inammation or its regulation. To achieve this, the authors employ three separate models of murine chronic IBD. The rst is the well characterised form of disease that occurs in immunodecient Rag KO mice given puried naive CD41 T cells, and which involves activation of Th17 and/or Th1 cells by commensal organisms. Using various combinations of TL2R KO donors and recipients, it was found that gut pathology did not require TLR2 expression on either the host cells or the pathogenic T cells. In addition, the Foxp31 Treg, which can prevent this disease when co-transferred with naive CD41 T cells, did not need to express TLR2 themselves, nor did the Treg need to interact with TLR21 cells in the hosts. In the second model, the authors used a model of innate colitis developed by the authors themselves [11], in which Rag KO mice on the 129 background develop colitis when infected with Helicobacter hepaticus. This IL-23-mediated disease is entirely driven by the innate immune system and again, it occurred normally in TLR2-decient recipients. In the nal experiments, colitis was induced in immunocompetent mice by infection with H. hepaticus, while at the same time neutralising IL-10R signalling in vivo. As before, colitis was not affected if the host mice did not express TLR2.
studies have suggested might be a particular function of this receptor. Colitis initiated by DSS, ischaemia or by toxic disruption of tight junctions is exacerbated in mice lacking TLR2 and administration of TLR2 ligands can ameliorate DSS colitis. These TLR2-dependent properties appear to be due to cytoprotective effects on epithelial cells, including stimulation of stem cell growth, ZO-1-mediated tight junction formation, NF-kB-mediated prevention of apoptosis and gap junction stabilisation [12]. Although these ndings are clearly at odds with those of Boulard et al. [10], tellingly the earlier results came from models of colitis that are extremely acute in nature and in which the primary event is damage to the epithelium. In contrast, epithelial damage occurring in the models used by Boulard et al. [10] is secondary to the chronic inammation established as a result of immune dysregulation. Thus the protective role of TLR2 signalling in the gut may be limited to sustaining epithelial barrier repair after mechanical insult, rather than modulating chronic inammatory processes. Such a conclusion would have many important implications for our understanding of mucosal homeostasis and TLR biology and further studies correlating barrier function with inammation and TLR2 signalling are warranted.
TLR2 involvement discriminates between acute and chronic colitis?
These complementary approaches provide novel insights into the role of TLR2 in regulating intestinal inammation and raise several intriguing questions. In particular, the ndings challenge previous suggestions that TLR2 ligation plays a critical role in protective and pathogenic processes in intestinal inammation [12]. TLR2 expression is upregulated in human IBD [13] and TLR2 has been reported to mediate activation of host cells by various Helicobacter spp. [14], the organism required for the models of colitis employed by Maloys group [10]. Therefore, it might have been predicted that TLR2 signalling would be particularly relevant in these systems; however, Boulard et al.s studies [10] show this is clearly not the case. Nor is TLR2 required for the intestinal inammation associated with Toxoplasma gondii or Citrobacter rodentium infection [15], whereas a recent report indicates that the spontaneous colitis found in IL-10 KO mice also develops normally on the TLR2 KO background [16]. One explanation for these discrepancies may come from the fact that TLR2-dependent intestinal inammation has only been described in two forms of acute colitis, one being dextran sodium sulphate (DSS) colitis [17] and the other, an unusual form of acute inammation induced by antigen-specic challenge of mice adoptively transferred with TCR-transgenic CD41 T cells [6]. In contrast, the colitis models studied by Boulard et al. [10] are chronic forms of disease and it may therefore be that TLR2 is only important in acute intestinal injury. Clearly, this needs further exploration in additional models of IBD and using other precipitating organisms. Perhaps, an even more surprising nding of this study was that TLR2 had no role in limiting colitis, which several other
TLR2 and Treg in intestinal inammation
A further important nding from the studies of Boulard et al. [10] was that control of T-cell-dependent colitis did not require TLR2 signalling on either the Treg or the host tissues. Again this contrasts with previous ndings of decreased numbers of Foxp31 Treg in TLR2 KO mice and that TLR2 may enhance Treg function [18]. Notably, TLR2 ligation has also been shown to induce retinoic acid production by DC, a property associated with gutderived DC, which drive differentiation of Foxp31 Treg [3]. In addition, probiotic organisms can prevent acute colitis in vivo by inducing TLR2-dependent differentiation of IL-10-producing Treg [19]. However, the work of Boulard et al. [10] indicates clearly that TLR2 is unlikely to have a universal role in determining Tregmediated protection against IBD. Whether these apparent discrepancies again reect differences between acute and chronic forms of gut inammation remains to be determined. In most cases, it may be that TLR2 simply plays an adjunct role in expanding or enhancing Treg activity, rather than being essential for their generation or function.
Concluding remarks
These elegant experiments argue strongly that TLR2 signalling does not have a central role in chronic colitis caused by overactivity of the innate and adaptive immune systems. Signicantly, the chronic models used to make this conclusion are perhaps more similar to human diseases such as Crohns disease than the acute models induced by epithelial damage in which pathogenic or protective roles of TLR2 have been identied. Thus modulation of TLR2 function may not be a useful strategy in this condition;
& 2010 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim
www.eji-journal.eu
320
Allan McI Mowat
Eur. J. Immunol. 2010. 40: 318320
however, this does not exclude the possibility that other TLR may play more important roles, as is suggested by the clear need for MyD88 signalling in a variety of colitis models [4] and by the mounting evidence that different TLR can drive very distinct types of response in the intestine and elsewhere [20]. Indeed, even TLR2 can have different functions depending on whether it dimerises with TLR1 or TLR6, with TLR2-TLR1 being proinammatory and TLR2-TLR6 thought to be anti-inammatory [21]. The studies by Boulard et al. [10] provide clear pathways for how some or all of these ideas can be tested out for individual TLR.
12 Cario, E., Barrier-protective function of intestinal epithelial Toll-like receptor 2. Mucosal. Immunol. 2008. 1: S62S66. 13 Szebeni, B., Veres, G., Dezso, A., Rusai, K., Vannay, A., Mraz, M., Majorova, E. and Arato, A., Increased expression of Toll-like receptor (TLR) 2 and TLR4 in the colonic mucosa of children with inammatory bowel disease. Clin. Exp. Immunol. 2008. 151: 3441. 14 Mandell, L., Moran, A. P., Cocchiarella, A., Houghton, J., Taylor, N., Fox, J. G., Wang, T. C. and Kurt-Jones, E. A., Intact gram-negative Helicobacter pylori, Helicobacter felis, and Helicobacter hepaticus bacteria activate innate immunity via toll-like receptor 2 but not toll-like receptor 4. Infect. Immun. 2004. 72: 64466454. 15 Furuta, T., Kikuchi, T., Akira, S., Watanabe, N. and Yoshikawa, Y., Roles of the small intestine for induction of toll-like receptor 4-mediated innate resistance in naturally acquired murine toxoplasmosis. Int. Immunol. 2006. 18: 16551662. 16 Messlik, A., Schmechel, S., Kisling, S., Bereswill, S., Heimesaat, M. M.,
Conict of interest: The author declares no nancial or commercial conicts of interest.
Fischer, A., Gobel, U. and Haller, D., Loss of Toll-like receptor 2 and 4 leads to differential induction of endoplasmic reticulum stress and proapoptotic responses in the intestinal epithelium under conditions of chronic inammation. J. Proteome Res. 2009. 8: 44064417. 17 Heimesaat, M. M., Fischer, A., Siegmund, B., Kupz, A., Niebergall, J.,
References
1 Cario, E., Innate immune signalling at intestinal mucosal surfaces: a ne line between host protection and destruction. Curr. Opin. Gastroenterol. 2008. 24: 725732. 2 Chabot, S., Wagner, J. S., Farrant, S. and Neutra, M. R., TLRs regulate the gatekeeping functions of the intestinal follicle-associated epithelium. J. Immunol. 2006. 176: 42754283. 3 Manicassamy, S. and Pulendran, B., Modulation of adaptive immunity with Toll-like receptors. Semin. Immunol. 2009. 21: 185193. 4 Rakoff-Nahoum, S., Hao, L. and Medzhitov, R., Role of toll-like receptors in spontaneous commensal-dependent colitis. Immunity 2006. 25: 319329. 5 Rakoff-Nahoum, S., Paglino, J., Eslami-Varzaneh, F., Edberg, S. and Medzhitov, R., Recognition of commensal microora by toll-like receptors is required for intestinal homeostasis. Cell 2004. 118: 229241. 6 Strober, W., Kitani, A., Fuss, I., Asano, N. and Watanabe, T., The molecular basis of NOD2 susceptibility mutations in Crohns disease. Mucosal. Immunol. 2008. 1: S5S9. 7 Strober, W., Fuss, I. and Mannon, P., The fundamental basis of inammatory bowel disease. J. Clin. Invest. 2007. 117: 514521. 8 Rhee, S. H., Im, E., Riegler, M., Kokkotou, E., OBrien, M. and Pothoulakis, C., Pathophysiological role of Toll-like receptor 5 engagement by bacterial agellin in colonic inammation. Proc. Natl. Acad. Sci. USA 2005. 102: 1361013615. 9 De Jager, P. L., Franchimont, D., Waliszewska, A., Bitton, A., Cohen, A., Langelier, D., Belaiche, J. et al., The role of the Toll receptor pathway in susceptibility to inammatory bowel diseases. Genes Immun. 2007. 8: 387397. 10 Boulard, O., Asquith, M. J., Powrie, F. and Maloy, K. J., TLR2-independent induction and regulation of chronic intestinal inammation. Eur. J. Immunol. 2010. 40: 516524. 11 Maloy, K. J., Salaun, L., Cahill, R., Dougan, G., Saunders, N. J. and Powrie, F., CD41CD251T(R) cells suppress innate immune pathology through cytokine-dependent mechanisms. J. Exp. Med. 2003. 197: 111119.
Fuchs, D., Jahn, H. K. et al., Shift towards pro-inammatory intestinal bacteria aggravates acute murine colitis via Toll-like receptors 2 and 4. PLoS One 2007. 2: e662. 18 Gibson, D. L., Ma, C., Rosenberger, C. M., Bergstrom, K. S., Valdez, Y., Huang, J. T., Khan, M. A. and Vallance, B. A., Toll-like receptor 2 plays a critical role in maintaining mucosal integrity during Citrobacter rodentiuminduced colitis. Cell Microbiol. 2008. 10: 388403. 19 Foligne, B., Dessein, R., Marceau, M., Poiret, S., Chamaillard, M., Pot, B., Simonet, M. and Daniel, C., Prevention and treatment of colitis with Lactococcus lactis secreting the immunomodulatory Yersinia LcrV protein. Gastroenterology 2007. 133: 862874. 20 Strober, W., The multifaceted inuence of the mucosal microora on mucosal dendritic cell responses. Immunity 2009. 31: 377388. 21 Depaolo, R. W., Tang, F., Kim, I., Han, M., Levin, N., Ciletti, N., Lin, A. et al., Toll-like receptor 6 drives differentiation of tolerogenic dendritic cells and contributes to LcrV-mediated plague pathogenesis. Cell Host Microbe 2008. 4: 350361.
Abbreviations: DSS: dextran sodium sulphate IBD: inammatory bowel disease Full correspondence: Professor Allan McI Mowat, Division of Immunology, Infection and Inammation, Glasgow Biomedical Research Centre, University of Glasgow, 120 University Place, Glasgow G12 8TA, Scotland, UK Fax: 144-141-330-4297 e-mail: a.m.mowat@clinmed.gla.ac.uk
See accompanying article: http://dx.doi.org/10.1002/eji.200939669 Received: 9/12/2009 Accepted: 11/12/2009
& 2010 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim
www.eji-journal.eu
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- ODY Efenses: Ap Biology Name Animals Form & Function Activity #4 Date HourDocument5 pagesODY Efenses: Ap Biology Name Animals Form & Function Activity #4 Date Hourancientblackdragon0% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Human Anatomy and Physiology AnswersDocument80 pagesHuman Anatomy and Physiology Answersdocabol100% (1)
- Ws1-Membrane Transport WorksheetDocument3 pagesWs1-Membrane Transport WorksheetTy BakrNo ratings yet
- Theories of Drug - Receptor InteractionDocument37 pagesTheories of Drug - Receptor InteractionSunil97% (32)
- Cells Questions and VocabDocument12 pagesCells Questions and VocabFanna Sharma100% (1)
- Gen Bio Periodic TestDocument7 pagesGen Bio Periodic TestRestyness Farochilin Tambo-ong33% (3)
- RibosomeDocument24 pagesRibosomeMaliha JahanNo ratings yet
- Self-Instructional ModuleDocument19 pagesSelf-Instructional ModuleMarlon S. BarangganNo ratings yet
- Microbiology Lab BookDocument83 pagesMicrobiology Lab BookLavina D'costa100% (6)
- Harv Life SC Data SCDocument5 pagesHarv Life SC Data SCLavina D'costaNo ratings yet
- B Hler Et Al 1998 Yeast 2Document9 pagesB Hler Et Al 1998 Yeast 2Lavina D'costaNo ratings yet
- NCERT Solutions Class 12th Biology: Chapter 9 - Strategies For Enhancement in Food ProductionDocument7 pagesNCERT Solutions Class 12th Biology: Chapter 9 - Strategies For Enhancement in Food ProductionLavina D'costaNo ratings yet
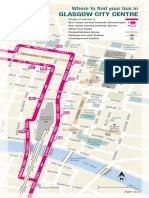
- Glasgow City Centre: Where To Find Your Bus inDocument3 pagesGlasgow City Centre: Where To Find Your Bus inLavina D'costaNo ratings yet
- Lactobacillus Probiotic Protects Intestinal EpitheliumDocument12 pagesLactobacillus Probiotic Protects Intestinal EpitheliumLavina D'costaNo ratings yet
- Agglutinin From Arachis Hypogaea: Site-Specific Monoclonal Antibodies Against PeanutDocument10 pagesAgglutinin From Arachis Hypogaea: Site-Specific Monoclonal Antibodies Against PeanutLavina D'costaNo ratings yet
- Predictions of Cancer Incidence in Wielkopolska in 2018: Dariusz Godlewski, Piotr Wojtyś, Andrzej AntczakDocument6 pagesPredictions of Cancer Incidence in Wielkopolska in 2018: Dariusz Godlewski, Piotr Wojtyś, Andrzej AntczakLavina D'costaNo ratings yet
- PhotosynthesisDocument9 pagesPhotosynthesisbok24No ratings yet
- CHNOPS-simulating Protein SynthesisDocument4 pagesCHNOPS-simulating Protein SynthesisDean GolliferNo ratings yet
- 4 I Morpho - Reversible Cell InjuryDocument21 pages4 I Morpho - Reversible Cell InjuryKartikey MishraNo ratings yet
- Q1. The Diagrams Show Four Types of Linkage, A To D, Which Occur in Biological MoleculesDocument19 pagesQ1. The Diagrams Show Four Types of Linkage, A To D, Which Occur in Biological MoleculesiNo ratings yet
- Gene ExpressionDocument7 pagesGene ExpressionTom Anthony TonguiaNo ratings yet
- LIGAND - Receptors Concept FKG 2012 Univ YarsiDocument29 pagesLIGAND - Receptors Concept FKG 2012 Univ Yarsidayanara_245104654No ratings yet
- ASO Article - GCDocument5 pagesASO Article - GCHaseena SaitNo ratings yet
- 6 Cell CycleDocument31 pages6 Cell CycleaprilNo ratings yet
- Lecture 5Document22 pagesLecture 5SudhanshuNo ratings yet
- Pared Celular M. TuberculosisDocument13 pagesPared Celular M. TuberculosisJose Maria RojasNo ratings yet
- Cellular RespirationDocument18 pagesCellular RespirationegeniasaljonnielpNo ratings yet
- List of Clotting FactorsDocument1 pageList of Clotting FactorsGNiqMNo ratings yet
- 2 ItemDocument9 pages2 ItemDaniberg RimenisNo ratings yet
- Prokaryote Vs EukaryoteDocument19 pagesProkaryote Vs EukaryotehamnaNo ratings yet
- Autoimmune Hepatitis - A Guide For Practicing Clinicians - G. Hirschfield, Et. Al., (Humana, 2012) WWDocument246 pagesAutoimmune Hepatitis - A Guide For Practicing Clinicians - G. Hirschfield, Et. Al., (Humana, 2012) WWIulian MunteanuNo ratings yet
- 135 - Possible MecanismsDocument19 pages135 - Possible MecanismsEduardo BacelarNo ratings yet
- How DNA Controls The Workings of The CellDocument2 pagesHow DNA Controls The Workings of The CelllmaureyNo ratings yet
- A Hydrophila PathogenesityDocument66 pagesA Hydrophila PathogenesityDeepak Ranjan SahooNo ratings yet
- Glycogen Metabolism - Index CardDocument3 pagesGlycogen Metabolism - Index CardKate Alyssa CatonNo ratings yet
- Cell Growth and DivisionDocument23 pagesCell Growth and DivisionWolfwood ManilagNo ratings yet
- Lipolysis and Aerobic ExerciseDocument11 pagesLipolysis and Aerobic ExerciseAna Flávia SordiNo ratings yet
- BIO 201 Macromolecules:: ( Did Not Have To Think, Had To Think, Did Not Know)Document2 pagesBIO 201 Macromolecules:: ( Did Not Have To Think, Had To Think, Did Not Know)silas StatenNo ratings yet