Professional Documents
Culture Documents
Drug Study
Uploaded by
donelynpintach0 ratings0% found this document useful (0 votes)
718 views3 pagesits for pedia,actually
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentits for pedia,actually
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
718 views3 pagesDrug Study
Uploaded by
donelynpintachits for pedia,actually
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 3
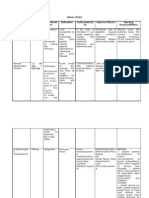
CEFTAZIDIME
Trade Name: Ceptaz, Tazidime, Fortaz, Tazicef
Classification: Cephalosporin 3rd generation
Doctor’s Order: 50mg/kg IV q 8hr
Drug Action: It inhibits the synthesis of bacterial cell wall which then causes cell death
Indication: Ceftazidime is indicated to the patient to treat respiratory tract infection, to
manage its manifesting symptoms and especially to eliminate its causative
agent.
Contraindication: It is contraindicated to patients with:
> allergy to cephalosporins
> allergy to penicillins
> renal failure
Side Effects:
CNS: headache, dizziness, lethargy
GI: nausea, vomiting, diarrhea, anorexia, abdominal pain,flatulence
Hypersensitivity: rash to fever
Local: pain, phlebitis
Other: Superinfections, disulfram like action with alcohol
Adverse Effects:
GI: pseudomembranous colitis
Hematologic: bone marrow depression
Hypersensitivity: anaphylaxis
Nursing Considerations:
1. Assess liver and kidney dysfunction, skin status, culture of affected area
2. Arrange for sensitivity tests before and during the therapy
3. For direct IV administration, reconstitute 1g in 10ml sterile water for injection.
Give over 3-5 mins.
4. For intermittent administration, further dilute in 500-100mL solution and
administer over 30-60mins.
5. Do not add Ceftazidime to solutions containing aminoglycosides.
6. Have Vitamin K available in case of hypothrombinemia occurs
7. Discontinue if hypersensitivity occurs.
Health Teachings:
1. Inform the patient and significant others that certain side effects may occur:
stomach upset or diarrhea
2. Instruct the patient to avoid alcohol intake while on the drug therapy and for 3
days after because severe reactions may occur
3. Remind the patient and the significant others to report severe diarrhea,
difficulty of breathing, unusual tiredness or fatigue, pain at injection site.
4. Remind the patient and significant others to complete the entire prescription
and instruct the patient not to stop medication despite the feeling better.
5. Inform the patient to return for follow up check up (ear, throat culture and x-
ray)
HYOSCINE BUTYLBROMIDE
Trade Name: Scopolaine Hbr, Scopace
Classification: Anticholinergic
Doctor’s Order: 0.006mg/kg IV
Drug Action: It is anticholinergic with CNS depressant effects. It inhibits excessive
motility and hypertonus of the GI tract. It blocks the effects of
acetylcholine at muscarinic cholinergic receptors that mediate the effects
of parasympathetic postganglionic impulses, depressing salivary and
bronchial secretions, inhibiting vagal influences on the heart relaxing the
GI and GU tracts, inhibiting gastric acid secretion.
Indication: This drug is indicated to the patient to inhibit excessive motility and
hypertonus of the GI tract
Contraindication: It is contraindicated to patients with:
> hypersensitivity to > bladder neck obstruction
anticholinergic drugs > bronchial asthma
> stenosing peptic ulcer > COPD
> severe ulcerative colitis > cardiac arrythmias
> liver and kidney dysfunction > use cautiously with Down
syndrome, brain damage,
hyperthyroidism
Side Effects:
CNS: pupil dilation, photophobia, blurred vision, headache, drowsiness
GI: dry mouth, constipation,
GU: Urinary hesitancy and retention
Other: nasal congestion, decreased sweating
Adverse Effect: anaphylaxis
Nursing Considerations:
1. Assess hypersensitivity to anticholinergic drugs, presence of stenosing peptic
ulcer, severe ulcerative colitis, liver and kidney dysfunction, bladder neck
obstruction,bronchial asthma, COPD, cardiac arrhythmias, Down syndrome, brain
damage, hyperthyroidism. Assess vital signs, adventitious and bowel sounds,
reflexes
2. Ensure adequate hydration
3. Provide environmental control (temperature) to prevent hyperpyrexia
4. Protect solution from light
Health Teachings:
1. Instruct the patient to avoid hot environments because they will be heat intolerant
and dangerous reactions may occur.
2. Inform the patient/family that these side effects may occur: dizziness, drowsiness
(avoid tasks requiring alertness), constipation (proper diet and increase oral fluid
intake), dry mouth (frequent mouth care), blurred vision (avoid tasks requiring
acute vision), difficulty in urinating (empty bladder before drug administration)
3. Instruct the patient to alcohol because serious sedation could occur.
4. Instruct patient/family to report rash, flushing, difficulty in breathing, tremors,
irregular heartbeat, abdominal distention, severe persistent dry mouth.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Psur Template PDFDocument17 pagesPsur Template PDFVidhya GGNo ratings yet
- Medicinal Chemistry (MCQs Exam)Document10 pagesMedicinal Chemistry (MCQs Exam)AbCc100% (6)
- Neomycin Is An Aminoglycoside AntibioticDocument5 pagesNeomycin Is An Aminoglycoside AntibioticDeby Nareswari HuslanNo ratings yet
- Pediatric Practice Math ProblemsDocument3 pagesPediatric Practice Math ProblemsKaren HutchinsonNo ratings yet
- WHO Pharm 2-2023Document19 pagesWHO Pharm 2-2023Paola Cristini Gama SilvaNo ratings yet
- Jovelyne J Remigio Rcrim, Mscrim Units: Prepared byDocument13 pagesJovelyne J Remigio Rcrim, Mscrim Units: Prepared byDean Mark AnacioNo ratings yet
- Special Resource: Drugs To Be Used With A Filter For Preparation And/or AdministrationDocument5 pagesSpecial Resource: Drugs To Be Used With A Filter For Preparation And/or Administrationemiliow_1No ratings yet
- Pregnancy Heart Disease v28 WebDocument1 pagePregnancy Heart Disease v28 WebMishka LaldaparsadNo ratings yet
- Dosage CalculationsDocument8 pagesDosage CalculationsReinna Angel CampoNo ratings yet
- Colchicine TabletsDocument16 pagesColchicine TabletsSaket SharmaNo ratings yet
- S 002 LBLDocument35 pagesS 002 LBLRDZENNo ratings yet
- TDM of LidocaineDocument19 pagesTDM of LidocaineNikkiiNo ratings yet
- Pharma Notes 1Document9 pagesPharma Notes 1Mayya FirdousNo ratings yet
- CNS Drugs: Drugs Acting On Central Nervous SystemDocument17 pagesCNS Drugs: Drugs Acting On Central Nervous Systemreza_juNo ratings yet
- Drug Study ArraDocument5 pagesDrug Study ArraPaul ManaloNo ratings yet
- Guidance For Industry Botanical Drug ProductsDocument52 pagesGuidance For Industry Botanical Drug ProductsJY MarNo ratings yet
- Drug PhenerganDocument1 pageDrug PhenerganSrkocherNo ratings yet
- Chapter 10Document45 pagesChapter 10Hannah BuquironNo ratings yet
- A Fatal Case of Benzodiazepine WithdrawalDocument3 pagesA Fatal Case of Benzodiazepine WithdrawalSusanNo ratings yet
- Laxatives & Antidiarrheals UseDocument19 pagesLaxatives & Antidiarrheals UseDhurjati MajumdarNo ratings yet
- Drugs That Lower The Seizure Threshold: Andrew W HitchingsDocument10 pagesDrugs That Lower The Seizure Threshold: Andrew W HitchingsesraaNo ratings yet
- Injection guidelines summaryDocument1 pageInjection guidelines summaryAnn A.No ratings yet
- Tiaft Drug Concentration Reference TableDocument20 pagesTiaft Drug Concentration Reference TablerodrigoNo ratings yet
- Dose Response StudiesDocument2 pagesDose Response StudiesSooraj Rajasekharan KarthaNo ratings yet
- FINAL Drug StudyDocument2 pagesFINAL Drug StudycasedraftNo ratings yet
- Rekap Resep - 2021-03-01T160848.881Document2,906 pagesRekap Resep - 2021-03-01T160848.881Dhita AnaleptaNo ratings yet
- Ranbaxy Case StudyDocument12 pagesRanbaxy Case StudyNitin KashyapNo ratings yet
- Dose Response RelationshipDocument24 pagesDose Response RelationshipPoonam RaiNo ratings yet
- Dr. Anggraini Alam's Curriculum Vitae and COVID-19 Treatment OptionsDocument18 pagesDr. Anggraini Alam's Curriculum Vitae and COVID-19 Treatment Optionsgina aghnnia hudaNo ratings yet
- Jurnal Tension HeadacheDocument15 pagesJurnal Tension HeadacheRisya Malida SinulinggaNo ratings yet