Professional Documents
Culture Documents
Annex11 ImportantRemindersForThePhilHealthClaimForms (November2013)
Uploaded by
Chrysanthus HerreraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Annex11 ImportantRemindersForThePhilHealthClaimForms (November2013)
Uploaded by
Chrysanthus HerreraCopyright:
Available Formats
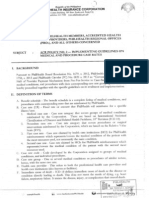
Republic of the Philippines
PHILIPPINE HEALTH INSURANCE CORPORATION
Citystate Centre Building, 709 Shaw Boulevard, Pasig City Healthline 441-7444 www.philhealth.gov.ph
Important Reminders for the Implementation of PhilHealth Claim Forms 1, 2 and 3
(November 2013)
I. General Reminders A. In conjunction with the implementation of the All Case Rates Policy, all claims for PhilHealth reimbursements shall utilize the PhilHealth Claim Form 1 (CF1), Claim Form 2 (CF2), and Claim Form 3 (CF3) revised November 2013. B. All claim forms submitted to PhilHealth shall be properly and completely filled out following the guidelines contained in Annex 11. Otherwise, it shall be returned to sender (RTS). C. As mentioned in the Implementing Guidelines on Medical and Procedure Case Rates (ACR POLICY No. 2), Health Care Providers shall comply with the following rules: 1. The Corporation shall only allow return of claims to the sender (RTS) for correction/revision/completion for claims with admission dates on or before March 31, 2014. RTS shall no longer be allowed for all claims with date of admission starting April 1, 2014. Instead, these claims shall be denied. 2. All claims that were returned to the sender for correction or completion shall be refiled within 60 days from receipt of notice; otherwise, it shall be denied. The basis for the receipt of notice shall be the date received by the HCI representative. D. Claim forms shall be returned to sender (RTS) if the said documents were submitted by fax or sent via email including any or all attachments thereto. E. Health Care Institutions shall ensure that the attached document is consistent with the name of the patient reflected in the claim forms. Any discrepancies shall result to return of the claim. F. Printed forms must be filled out completely using BLACK/BLUE BALLPOINT PEN. Computerized or typewritten mode of filling out the claims form is acceptable. G. Use additional claim forms if necessary. Fill out applicable fields only. H. Claim forms shall be reproduced by all providers in Long-size paper (8 inches x 13 inches) by any electronic or manual means for the purpose of filing claims. However, all rights to these forms shall reside solely with PhilHealth. II. Specific Reminders for Claim Form 1 (CF1) A. For local availment, Claim Form 1, together with other PhilHealth Claim Forms and other supporting documents, should be filed within sixty (60) calendar days from the date of discharge. B. For reimbursement of claims for benefits availed abroad, Claim Form 1, together with other supporting documents, should be filed within one hundred eighty (180) calendar days from the date of discharge. All pertinent documents should be translated into English when confinement is in non-English speaking countries. C. In CF1 Part III (Member Certification), the thumbmark of the member/representative must be affixed and duly witnessed/assisted by a HCI representative in case either the member or representative is unable to sign the said document. D. For employed members, CF1 shall be returned to sender (RTS) if the date of signature in employers certification (Part IV, item 4) is more than 30 days before the start of confinement.
Page 1 of 2
III. Specific Reminders for Claim Form 2 (CF2) A. The health care provider shall indicate the complete admitting and discharge diagnoses in Part II item 6 and 7 of Claim Form 2. Additional copies of CF2 may be used if the space provided for the diagnoses is not sufficient. The health care provider shall only fill out the appropriate parts and shall leave the rest of CF 2 blank. Additional codes for specific requirements for each case rate shall be reflected in the discharge diagnosis (e.g., dehydration code for acute enteritis). B. The health care provider shall write legibly the correct and complete ICD-10 and RVS codes corresponding to the discharge diagnosis/es and shall be held primarily responsible for any errors that may be found therein on post audit. C. For procedures with laterality (see ACR Policy No 2, Annex 7), the health care provider shall tick the appropriate box (left, right, or both) in item 7; otherwise, the claim shall be returned to sender. Tick boxes for laterality shall be left blank for other procedures (i.e., procedures without laterality). D. The health care provider shall ensure that the amount indicated in Part III item A of Claim Form 2 is based on what is written in the Statement of Account (SOA). E. For repetitive procedures (see ACR Policy No 2, Table 2 Procedure List A): 1. The health care provider shall indicate the discharge diagnosis with corresponding ICD 10 code, and related procedures with corresponding RVS code/s in Item 7 of CF2. The date of procedure shall be left blank. Instead, the health care provider shall tick the appropriate box in item 8 of CF2 and indicate the dates of session/procedure in the blank space opposite the procedure. 2. A maximum of two repetitive procedures shall be ticked in Item 8a of CF 2. All procedures checked under Item 8a of CF2 shall be reflected in Item 9 as first and second case rates respectively. 3. Multiple sessions/cycles of the repetitive procedures can be indicated per claim. However, a maximum of one month of procedures shall be included per claim. 4. All procedures ticked in Item 8a shall be written in Item 9 under ICD 10/RVS Code. Only one case rate (indicated by the ICD 10 or RVS code) shall be written per line. F. Under Part II, Item 9 of CF2, only one code shall be indicated for the first case rate and one code for the second case rate (if applicable). G. In CF2 Part III item B, the thumbmark of the patient/representative must be affixed and duly witnessed/assisted by a HCI representative in case either the patient or representative is unable to sign the said document. IV. Specific Reminder for Claim Form 3 (CF3) A properly and completely filled out Claim Form 3 shall be required for Maternity Care Package claims and for all cases managed in Primary Care Facilities.
Page 2 of 2
You might also like
- Ra 10354Document13 pagesRa 10354CBCP for LifeNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex 10 List of Alternative Documents For Record of Operative or Surgical TechniqueDocument14 pagesPhilHealth Circular No. 0035, s.2013 Annex 10 List of Alternative Documents For Record of Operative or Surgical TechniqueChrysanthus HerreraNo ratings yet
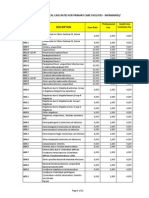
- PhilHealth Circular No. 0035, s.2013 Annex 6 List of Procedure CaseRates For Primary Care FacilitiesDocument22 pagesPhilHealth Circular No. 0035, s.2013 Annex 6 List of Procedure CaseRates For Primary Care FacilitiesChrysanthus Herrera100% (2)
- PhilHealth Circular No. 0035, s.2013 Annex 4 Examples and Scenarios For The All Case Rates Implementing GuidelinesDocument7 pagesPhilHealth Circular No. 0035, s.2013 Annex 4 Examples and Scenarios For The All Case Rates Implementing GuidelinesChrysanthus HerreraNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex 5 List of Medical Case Rates For Primary Care FacilitiesDocument22 pagesPhilHealth Circular No. 0035, s.2013 Annex 5 List of Medical Case Rates For Primary Care FacilitiesChrysanthus HerreraNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex 2 List of Procedure Case RatesDocument98 pagesPhilHealth Circular No. 0035, s.2013 Annex 2 List of Procedure Case RatesChrysanthus Herrera50% (2)
- PhilHealth Circular No. 0035, s.2013 Annex 1 List of Medical Case RatesDocument111 pagesPhilHealth Circular No. 0035, s.2013 Annex 1 List of Medical Case RatesChrysanthus Herrera80% (5)
- PhilHealth Circular No. 0035, s.2013 Annex 3 List of Medical Conditions and Procedures Allowed As Second Case RateDocument31 pagesPhilHealth Circular No. 0035, s.2013 Annex 3 List of Medical Conditions and Procedures Allowed As Second Case RateChrysanthus Herrera0% (1)
- CF1Document1 pageCF1Kim ViñasNo ratings yet
- Medical conditions allowed for referral packageDocument7 pagesMedical conditions allowed for referral packageChrysanthus HerreraNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex 9 Referral FormDocument1 pagePhilHealth Circular No. 0035, s.2013 Annex 9 Referral FormChrysanthus HerreraNo ratings yet
- Annex 7 procedures with lateralityDocument11 pagesAnnex 7 procedures with lateralityChrysanthus HerreraNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex11 PhilHealthClaimForm3 Frontpage (RevisedNovember2013)Document2 pagesPhilHealth Circular No. 0035, s.2013 Annex11 PhilHealthClaimForm3 Frontpage (RevisedNovember2013)Chrysanthus HerreraNo ratings yet
- GUIDELINES ON PROPER ACCOMPLISHMENT OF PHILHEALTH CLAIM FORM 1Document4 pagesGUIDELINES ON PROPER ACCOMPLISHMENT OF PHILHEALTH CLAIM FORM 1Ash CampiaoNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex 11 PhilHealth Claim Form 3 Back Page (Revised November 2013)Document1 pagePhilHealth Circular No. 0035, s.2013 Annex 11 PhilHealth Claim Form 3 Back Page (Revised November 2013)Chrysanthus HerreraNo ratings yet
- Tabata WorkoutDocument1 pageTabata WorkoutEmily HeadingsNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex11 - GuidelinesOnTheProperAccomplishmentOfClaimForm2 (November2013)Document8 pagesPhilHealth Circular No. 0035, s.2013 Annex11 - GuidelinesOnTheProperAccomplishmentOfClaimForm2 (November2013)Chrysanthus HerreraNo ratings yet
- PhilHealth Circular No. 0035, s.2013 Annex11 - PhilHealthClaimForm2 (Revisednovember2013)Document2 pagesPhilHealth Circular No. 0035, s.2013 Annex11 - PhilHealthClaimForm2 (Revisednovember2013)Chrysanthus HerreraNo ratings yet
- Philippine Health Insurance Corporation Circular No. 0035, S. 2013 - Implementing Guidelines On The Medical and Procedure Case RatesDocument17 pagesPhilippine Health Insurance Corporation Circular No. 0035, S. 2013 - Implementing Guidelines On The Medical and Procedure Case RatesChrysanthus HerreraNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Project Management in Practice 6th Edition Meredith Solutions ManualDocument25 pagesProject Management in Practice 6th Edition Meredith Solutions ManualMatthewFosteroeqyp98% (48)
- Rhetorical AnalysisDocument4 pagesRhetorical Analysisapi-495296714No ratings yet
- Carnival Panorama Deck Plan PDFDocument2 pagesCarnival Panorama Deck Plan PDFJuan Esteban Ordoñez LopezNo ratings yet
- Y-Chromosome Analysis in A Northwest Iberian Population: Unraveling The Impact of Northern African LineagesDocument7 pagesY-Chromosome Analysis in A Northwest Iberian Population: Unraveling The Impact of Northern African LineagesHashem EL-MaRimeyNo ratings yet
- New Earth Mining Iron Ore Project AnalysisDocument2 pagesNew Earth Mining Iron Ore Project AnalysisRandhir Shah100% (1)
- Yiseth Tatiana Sanchez Claros: Sistema Integrado de Gestión Procedimiento Ejecución de La Formación Profesional IntegralDocument3 pagesYiseth Tatiana Sanchez Claros: Sistema Integrado de Gestión Procedimiento Ejecución de La Formación Profesional IntegralTATIANANo ratings yet
- The Brief History of HumanismDocument17 pagesThe Brief History of HumanismVihaan VadnereNo ratings yet
- Kotak ProposalDocument5 pagesKotak ProposalAmit SinghNo ratings yet
- OathDocument5 pagesOathRichard LazaroNo ratings yet
- Prospero'sDocument228 pagesProspero'sIrina DraganescuNo ratings yet
- 11th English ExamDocument4 pages11th English ExamsandchhonkarNo ratings yet
- Sources and Historiography of Kerala CoinageDocument68 pagesSources and Historiography of Kerala CoinageRenuNo ratings yet
- KYC FAQsDocument5 pagesKYC FAQsmicorreNo ratings yet
- Meaning and Purpose of LawsDocument12 pagesMeaning and Purpose of LawsChuphyl MatreNo ratings yet
- Comprehensive Disaster Management Programme (CDMP II) 2013 Year-End ReviewDocument18 pagesComprehensive Disaster Management Programme (CDMP II) 2013 Year-End ReviewCDMP BangladeshNo ratings yet
- Qualities of Officiating OfficialsDocument3 pagesQualities of Officiating OfficialsMark Anthony Estoque Dusal75% (4)
- The Human Person As An Embodied SpiritDocument8 pagesThe Human Person As An Embodied SpiritDrew TamposNo ratings yet
- Essential Rabbi Nachman meditation and personal prayerDocument9 pagesEssential Rabbi Nachman meditation and personal prayerrm_pi5282No ratings yet
- This Content Downloaded From 181.65.56.6 On Mon, 12 Oct 2020 21:09:21 UTCDocument23 pagesThis Content Downloaded From 181.65.56.6 On Mon, 12 Oct 2020 21:09:21 UTCDennys VirhuezNo ratings yet
- Psu Form 111Document2 pagesPsu Form 111Ronnie Valladores Jr.No ratings yet
- Cross Culture Management & Negotiation IBC201 Essay TestDocument2 pagesCross Culture Management & Negotiation IBC201 Essay TestVu Thi Thanh Tam (K16HL)No ratings yet
- Dedication: ZasmDocument15 pagesDedication: ZasmZesa S. BulabosNo ratings yet
- Guide to Sentence Inversion in EnglishDocument2 pagesGuide to Sentence Inversion in EnglishMarina MilosevicNo ratings yet
- Daimler Co Ltd v Continental Tyre and Rubber Co control and enemy characterDocument1 pageDaimler Co Ltd v Continental Tyre and Rubber Co control and enemy characterMahatama Sharan PandeyNo ratings yet
- Simple Present: Positive SentencesDocument16 pagesSimple Present: Positive SentencesPablo Chávez LópezNo ratings yet
- MBA Capstone Module GuideDocument25 pagesMBA Capstone Module GuideGennelyn Grace PenaredondoNo ratings yet
- CHAPTER-1 FeasibilityDocument6 pagesCHAPTER-1 FeasibilityGlads De ChavezNo ratings yet
- R164Document9 pagesR164bashirdarakNo ratings yet
- Ignorantia Juris Non ExcusatDocument3 pagesIgnorantia Juris Non ExcusatXymon Bassig0% (1)
- 1 Herzfeld, Michael - 2001 Sufferings and Disciplines - Parte A 1-7Document7 pages1 Herzfeld, Michael - 2001 Sufferings and Disciplines - Parte A 1-7Jhoan Almonte MateoNo ratings yet