Professional Documents
Culture Documents
Anatomic Relationship Between Impacted Third Mandibular Molar
Uploaded by
Bulfendri DoniCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anatomic Relationship Between Impacted Third Mandibular Molar
Uploaded by
Bulfendri DoniCopyright:
Available Formats
Available online at www.sciencedirect.
com
British Journal of Oral and Maxillofacial Surgery 51 (2013) e215e219
Anatomic relationship between impacted third mandibular molar and the mandibular canal as the risk factor of inferior alveolar nerve injury
Guang-zhou Xu, Chi Yang , Xin-Dong Fan , Chuang-Qi Yu, Xie-Yi Cai, Yong Wang, DongMei He
Department of Oral and Maxillofacial Surgery, Peoples Republic of China Accepted 21 January 2013 Available online 11 February 2013
Abstract Our aim was to explore the relation between the site of the mandibular canal and neurosensory impairment after extraction of impacted mandibular third molars. We organised a retrospective study of 537 extractions in 318 patients in which the affected tooth was intersected by the mandibular canal. This was veried by cone-beam computed tomography (CBCT), and we analysed the relation between the site of the canal and the likelihood of injury to the inferior alveolar nerve (IAN) after extraction of the third molar. The relation between the position of the root of the tooth and the mandibular canal was categorised into 4 groups: I = root above the canal; II = on the buccal side; III = on the lingual side; and IV = between the roots. The overall rate of neurosensory impairment after extraction was 6% (33/537). It occurred in 9/272 patients (3%) in group 1, 16/86 (19%) in group II, and in 8/172 (5%) in group III. There was no neurosensory impairment in group IV where the canal was between the roots. There were signicant differences between group II and groups I and III (p < 0.01), but not between groups I and III (p = 0.32). The risk of damage to the inferior alveolar nerve is increased if third molars intersect with the mandibular canal, particularly on its buccal side. 2013 The British Association of Oral and Maxillofacial Surgeons. Published by Elsevier Ltd. All rights reserved.
Keywords: Cone beam computed tomography; Mandibular canal; Impacted mandibular third molar; Inferior alveolar nerve
Introduction Neurosensory impairment is a common complication of extraction of impacted mandibular third molars, and the incidence ranges from 0.5% to 8%.1,2 However, the incidence
This work was supported by Science and Technology Commission of Shanghai (08DZ2271100) and Shanghai PuDong new District Health Bureau (PW2011D-4). Corresponding authors at: Department of Oral and Maxillofacial Surgery, Ninth Peoples Hospital, Shanghai Jiao Tong University School of Medicine, No. 639, Zhi-Zao-Ju Rd., 200011 Shanghai, Peoples Republic of China. Tel.: +86 23271699 5218. E-mail addresses: yangchi63@hotmail.com (C. Yang), fanxindong@yahoo.com.cn, xgzmy1@163.com (X.-D. Fan).
of permanent injury to the mandibular nerve is reported to be less than 1%.3 As a result of the close proximity of the third molars and the mandibular canal, the inferior alveolar nerve (IAN) may be damaged during extraction. This could lead to temporary or permanent numbness or reduced sensation in the lower lip. The incidence of injury to the IAN differs according to the selection criteria used, such as surgeons experience, the age and sex of the patients, the type of anaesthesia, the anatomical relation between the mandibular canal and the third molars, and the degree of tissue damage caused by the operation.46 The purpose of this study was to evaluate the incidence of damage to the IAN after extraction of third molars in patients in whom the anatomical relation between the third molar and the mandibular canal differed.
0266-4356/$ see front matter 2013 The British Association of Oral and Maxillofacial Surgeons. Published by Elsevier Ltd. All rights reserved.
http://dx.doi.org/10.1016/j.bjoms.2013.01.011
e216
G.-z. Xu et al. / British Journal of Oral and Maxillofacial Surgery 51 (2013) e215e219
Materials and methods This retrospective study was approved by our local institutional review board. Patients All patients attended the Department of Oral and Maxillofacial Surgery, Ninth Peoples Hospital, Shanghai Jiao Tong University School of Medicine. Inclusion criteria were: all those whose third molars were intersected by the mandibular canal as diagnosed by panoramic radiography and conrmed by cone-beam computed tomography (CBCT); those in whom there was no bony tissue between the third molar and the canal on imaging (the molar being extremely close to the IAN); those who had third molars extracted; and those for whom the clinical records and CBCT obtained preoperatively and after at least 6 months postoperatively were available. All third molars were extracted by the same surgeon using similar surgical instruments under local anaesthesia (2% articaine and epinephrine 1:1000.000). All patients were informed of possible complications including the risk of damage to the nerve after removal of the tooth, and gave consent before extraction. During the operation a full-thickness triangular mucoperiosteal ap was reected, and the buccal bone was removed with a diamond burr under continuous irrigation with sterile saline at room temperature.
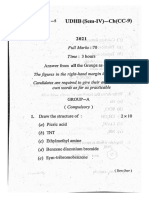
After adequate ostectomy, the tooth was removed and the socket cleaned. The tooth was sectioned whenever necessary. Postoperatively the patients were followed up regularly (the next day, and after 1 week, 1 month, 3 months, and 6 months). Relation between third molars and the mandibular canal on CBCT The relation between the impacted third molars and the manidbular canal was evaluated independently in the coronal plane on CBCT by 2 experienced oral and maxillofacial surgeons and a radiologist. Three doctors reached the same conclusion after reviewing the radiographs. The relations were divided into 4 types: I = root above the mandibular canal; II = root on the buccal side; III = root on the lingual side; and IV = canal between the roots (Fig. 1). Neurosensory assessment Sensation was evaluated by subjective monitoring of the feeling in the lower lip and the skin of the chin preoperatively and at different times postoperatively. Criteria for numbness were: symptom-free = no numbness; curable = numbness can be cured within 6 months; and incurable = numbness cannot be cured within 6 months.
Fig. 1. The relation between the position of the impacted teeth and the mandibular canal were divided into 4 categories by coronal cone-beam computed tomography with the mandibular canal as reference (outlined in yellow). (a) Category I = root above the canal; (b) II = on the buccal side; (c) III = on the lingual side; and (d) IV = canal between the roots, where there is no bone between the tooth root and the inferior alveolar canal.
G.-z. Xu et al. / British Journal of Oral and Maxillofacial Surgery 51 (2013) e215e219
e217
Table 1 Relation of positions between the impacted teeth and the mandibular canal in 537 patients on cone beam computed tomography in the coronal plane, and damage to the inferior alveolar nerve (IAN) in these groups after extraction of teeth. Type and position I: above mandibular canal II: on the buccal side III: on the lingual side IV: between the roots Total No symptoms 263 70 164 7 504 Damage to the IAN 9 16 8 0 33 Total 272 86 172 7 537 RR 0.34 4.94 0.66 p-Value 0.006 <0.0001 0.32
RR, relative risk. Type II differed signicantly from types I and III, but types I and III did not differ signicantly.
Statistical analysis We compared the incidence of damage to the IAN in the 4 groups after the teeth had been extracted. Data were analysed with the help of the Statistical Package for the Social Sciences version 13.0 (SPSS Inc., IBM, NY, USA). We used the chi square test to assess the signicance of differences among the types.
Results We studied 537 impacted third molars in 318 consecutive patients (138 men and 180 women, mean age at extraction 26 (range 2036) years who fullled the selection criteria between November 2008 and September 2011. Most of them were mesioangular and vertical impactions based on Winters classication; horizontal impacted teeth were in the minority. A total of 272 were above the mandibular canal (51%), 86 on the buccal side (16%), 172 on the lingual side (32%), and the canal was between the roots in 7 teeth (1%). The results are shown in Table 1. Of the 33 patients with numbness of the lower lip, 23 healed within a week, and the other 10 healed within 6 months. In no case was it permanent.
Discussion Damage to the IAN is a serious complication of the extraction of mandibular third molars. The risk factors include the surgeons experience, the age and sex of the patient, the degree of operative tissue damage, surgical instruments, and postoperative oedema. The most important factor, however, is the anatomical relation between the impacted third molar and the mandibular canal.79 Accurate preoperative imaging to conrm the relation is therefore important for predicting the degree of difculty, and the risk of damage. Panoramic radiography has become a routine preoperative examination for impacted mandibular third molars, as it can display panoramic views of both the dentition and the mandible simultaneously. It also has other benets such as low cost, low dose of radiation, and convenience. However, it does not support imaging in the coronal, sagittal, and axial planes, and it cannot be used to display the relation between the impacted
teeth and the mandibular canal in 3 dimensions. Rood and Shehab10 found a signicant relation between diversion of the canal, narrowing of the root, interruption of the white line by the nerve, and injury to the nerve. Some workers thought that the bone line of the mandibular canal is more likely to be interrupted by the impacted tooth if panoramic radiography shows the impacted tooth intersecting the mandibular canal, and it is also more likely to come into contact with the canal if the root of the impacted tooth is narrowing.9,11 Other workers have reported that the impacted tooth is more likely to come into contact with the canal if the bone line cannot be identied on panoramic radiography. We consider that panoramic lm does not reect the relations between the impacted teeth and the mandibular canal as accurately as CT, which should be used as the gold standard for judging these relations. It has been proved that CBCT is the best way of displaying the mandibular canal from different directions, including buccolingual, coronal, and axial directions.12,13 CBCT has the advantages over multislice spiral CT in dental research in that it provides better images of teeth and their surrounding structures.14 It also means less exposure to radiation for the patients, and it can improve spatial resolution of the images.15 It can be used to observe the relation between the impacted teeth and the mandibular canal in 3-dimensions when necessary, and it can be used to reconstruct upper and lower alveolar bones so that their height, thickness, and density can be measured to an accuracy of 0.1 mm. Finally, it is cheaper than traditional CT.16 Because the coronal plane of CBCT is the only one that shows the whole range of positional relations between the third molar and the mandibular canal in the same plane, we divided the relation between the impacted teeth and the canal into 4 categories. The results showed that patients whose molar roots intersected with the mandibular canal had a higher risk of having an injury to the IAN, particularly on the buccal side. We think that trauma during surgical extractions is responsible for this. During the operation the elevator is inserted between the impacted tooth and the buccal alveolar bone, which may cause the root to compress the IAN. Similar results have been found in other studies.17,18 However, the reported samples are relatively small. Ueda et al. categorised the shape of the IAC in 3 groups: round oroval, teardrop, and dumbbell.19 They found that the shape of the inferior alveolar canal (IAC) was closely related to injury to
e218
G.-z. Xu et al. / British Journal of Oral and Maxillofacial Surgery 51 (2013) e215e219 5. Jerjes W, Swinson B, Moles DR, et al. Permanent sensory nerve impairment following third molar surgery: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:e17. 6. Palma-Carri C, Garca-Mira B, Larrazabal-Morn C, Pe narrocha-Diago M. Radiographic signs associated with inferior alveolar nerve damage following lower third molar extraction. Med Oral Patol Oral Circ Bucal 2010;15:e88690. 7. Nakayama K, Nonoyama M, Takaki Y, et al. Assessment of the relationship between impacted mandibular third molars and inferior alveolar nerve with dental 3-dimensional computed tomography. J Oral Maxillofac Surg 2009;67:258791. 8. Rood JP. Degrees of injury to the inferior alveolar nerve sustained during the removal of impacted mandibular third molars by the lingual split technique. Br J Oral Surg 1983;21:10316. 9. Sedaghatfar M, August MA, Dodson TB. Panoramic radiographic ndings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg 2005;63:37. 10. Rood JP, Shehab BA. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg 1990;28:205. 11. Szalma J, Lempel E, Jeges S. The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:294302. 12. Ylikontiola L, Moberg K, Huumonen S, Soikkonen K, Oikarinen K. Comparison of three radiographic methods used to locate the mandibular canal in the buccolingual direction before bilateral sagittal split osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:73642. 13. Ohman A, Kivijrvi K, Blombck U, Flygare L. Pre-operative radiographic evaluation of lower third molars with computed tomography. Dento-Maxillo-Facial Radiol 2006;35:305. 14. Friedland B, Donoff B, Dodson TB. The use of 3-dimensional reconstructions to evaluate the anatomic relationship of the mandibular canal and impacted mandibular third molars. J Oral Maxillofac Surg 2008;66:167885. 15. Araki K, Maki K, Seki K, et al. Characteristics of a newly developed dentomaxillofacial X-ray cone beam CT scanner (CB MercuRay): system conguration and physical properties. Dento-Maxillo-Facial Radiol 2004;33:519. 16. Hashimoto K, Kawashima S, Kameoka S, et al. Comparison of image validity between cone beam computed tomography for dental use and multidetector row helical computed tomography. Dento-Maxillo-Facial Radiol 2007;36:46571. 17. Maegawa H, Sano K, Kitagawa Y, et al. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;96:63946. 18. Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Berg SJ. Position of the impacted third molar in relation to the mandibular canal, diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int J Oral Maxillofac Surg 2009;38:96471. 19. Ueda M, Nakamori K, Shiratori K, et al. Clinical signicance of computed tomographic assessment and anatomic features of the inferior alveolar canal as risk factors for injury of the inferior alveolar nerve at third molar surgery. J Oral Maxillofac Surg 2012;70:51420. 20. Eyrich G, Seifert B, Matthews F, et al. 3-Dimensional imaging for lower third molars: is there an implication for surgical removal? J Oral Maxillofac Surg 2011;69:186772. 21. Sanmart-Garcia G, Valmaseda-Castelln E, Gay-Escoda C. Does computed tomography prevent inferior alveolar nerve injuries caused by lower third molar removal? J Oral Maxillofac Surg 2012;70:511. 22. Alessandri Bonetti G, Bendandi M, Laino L, Checchi V, Checchi L. Orthodontic extraction: riskless extraction of impacted lower third molars close to the mandibular canal. J Oral Maxillofac Surg 2007;65:25806. 23. Dolanmaz D, Yildirim G, Isik K, Kucuk K, Ozturk A. A preferable technique for protecting the inferior alveolar nerve: coronectomy. J Oral Maxillofac Surg 2009;67:12348.
the IAN. These results suggest that assessment of the shape of the IAC and its cortication state at the time of extraction of third molars may be clinically useful.19 We found no neurosensory impairment in cases in which the mandibular canal was between the roots. Perhaps the numbers in group IV are too small (n = 6) to show the incidence of damage to the IAN. Whether CT is useful for predicting the risk of postoperative impairment of the IAN before removal of impacted lower third molars is controversial. Some scholars think that 3-dimensional CT information reduces the risk of impairment after removal of lower third molars.20 Others, however, think that CT is useful only for diagnostic purposes, but does not seem to reduce the risk of injuring the IAN.21 We think that impacted third molars that are intersected by the mandibular canal (diagnosed on panoramic radiograph) should be conrmed by CT or CBCT. Those patients in whom the roots of the third molar are close to the canal, particularly on the buccal side, should be told of the possibility of complications after removal of the third molar and provide written informed consent if operation is necessary. Of course the surgeons should make exact operation plans, and operations should be gentle and avoid scraping the alveolar fossa or operating on the buccal mucosa if the affected tooth is on the buccal side. If paraesthesia of the lower lip develops postoperatively, appropriate treatment should be prompt. Surgeons should use other relatively safer procedures to extract those teeth, such as orthodontic traction or coronectomy.2225 In conclusion, CBCT in the coronal plane can accurately show the relation between the impacted third molar and the mandibular canal, which can help the surgeons make precise surgical plans and reduce the incidence of complications, particularly damage to the IAN. Patients with roots intersected by the mandibular canal have a higher risk of IAN damage during extraction, particularly on the buccal side of the canal.
Conict of interest The authors declare that they have no conict of interest.
References
1. Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Can Dental Assoc 2007;73:3257. 2. Rood JP. Permanent damage to inferior alveolar and lingual nerves during the removal of impacted mandibular third molars: comparison of two methods of bone removal. Br Dent J 1992;172:10810. 3. Blaeser BF, August MA, Donoff RB, Kaban LB, Dodson TB. Panoramic radiographic risk factors for inferior alveolar nerve injury after third molar extraction. J Oral Maxillofac Surg 2003;61:41721. 4. Valmaseda-Castelln E, Berini-Ayts L, Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001;92:37783.
G.-z. Xu et al. / British Journal of Oral and Maxillofacial Surgery 51 (2013) e215e219 24. Cilasun U, Yildirim T, Guzeldemir E, Pektas ZO. Coronectomy in patients with high risk of inferior alveolar nerve injury diagnosed by computed tomography. Oral Maxillofac Surg 2011;69: 155761.
e219
25. Tolstunov L, Javid B, Keyes L, Nattestad A. Pericoronal ostectomy: an alternative surgical technique for management of mandibular third molars in close proximity to the inferior alveolar nerve. J Oral Maxillofac Surg 2011;69:185866.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Lip Nose DeformityDocument3 pagesLip Nose DeformityBulfendri DoniNo ratings yet
- Cleft Lip and PalateDocument56 pagesCleft Lip and PalateBulfendri DoniNo ratings yet
- Extraction of FourDocument3 pagesExtraction of FourBulfendri DoniNo ratings yet
- A Single Dose of Amoxicillin and Dexamethasone ForDocument8 pagesA Single Dose of Amoxicillin and Dexamethasone ForBulfendri DoniNo ratings yet
- 2021 SEM 4 CC 9 OrganicDocument3 pages2021 SEM 4 CC 9 OrganicGaurav KumarNo ratings yet
- IEEE and IEC StandardsDocument11 pagesIEEE and IEC StandardschupzptNo ratings yet
- AlternatorDocument14 pagesAlternatorTaraknath MukherjeeNo ratings yet
- Shape of Water in Rotating Bucket - Physics Stack ExchangeDocument3 pagesShape of Water in Rotating Bucket - Physics Stack ExchangeHector TrianaNo ratings yet
- Xii Chemistry MCQ (Haloalanes & Haloarenrs)Document7 pagesXii Chemistry MCQ (Haloalanes & Haloarenrs)SanjanasanjuNo ratings yet
- Cswip Appendix 01Document23 pagesCswip Appendix 01Nsidibe Michael EtimNo ratings yet
- Gaggenau DF 291-760Document1 pageGaggenau DF 291-760PurcellMurrayNo ratings yet
- BioFluid Mechanics 1Document29 pagesBioFluid Mechanics 1roxannedemaeyerNo ratings yet
- Ap T240 13Document92 pagesAp T240 13mehdiNo ratings yet
- Chapter 1 AssignmentDocument4 pagesChapter 1 Assignmenthamster808100% (3)
- PHYSICS Lab Manual - 2023-24Document30 pagesPHYSICS Lab Manual - 2023-24Vinushree Santhoshkumar100% (4)
- Abacus PlusDocument4 pagesAbacus PlusPhương Chính NghĩaNo ratings yet
- Thermal Engineering PDFDocument5 pagesThermal Engineering PDFabhinavgiri17No ratings yet
- A Deep Dive Into The Latest HPC SoftwareDocument38 pagesA Deep Dive Into The Latest HPC SoftwareSundar NilNo ratings yet
- Thumb Rules For Civil Engineers PDFDocument4 pagesThumb Rules For Civil Engineers PDFA KNo ratings yet
- Transformation To An Agile and Virtualized World: Operations Center of The FutureDocument1 pageTransformation To An Agile and Virtualized World: Operations Center of The FuturepinardoNo ratings yet
- Chameleon ChipDocument2 pagesChameleon ChipChetan KumarNo ratings yet
- Cj2m-Cpu, - md21 Cpu Units, Pulse I o Modules Datasheet en PDFDocument29 pagesCj2m-Cpu, - md21 Cpu Units, Pulse I o Modules Datasheet en PDFKhairy YaakobNo ratings yet
- Confidence IntervalDocument22 pagesConfidence Intervallloyd balinsuaNo ratings yet
- Bogiflex KGD20 - For PlantDocument13 pagesBogiflex KGD20 - For PlantAnonymous PVXBGg9TNo ratings yet
- The ParagraphDocument4 pagesThe Paragraphapi-238710927No ratings yet
- Degree of Kinematic IndeterminacyDocument8 pagesDegree of Kinematic IndeterminacyshahrukhNo ratings yet
- DSI - MPS® Transfer System Compact Trainer I4.0 - EN - DID1089 (Screen)Document2 pagesDSI - MPS® Transfer System Compact Trainer I4.0 - EN - DID1089 (Screen)mhafizanNo ratings yet
- Week 4.damping ElementsDocument5 pagesWeek 4.damping ElementsTrophie NilemoaNo ratings yet
- Certificate of Analysis: Sulfate IC CRM - 1000 MG/LDocument2 pagesCertificate of Analysis: Sulfate IC CRM - 1000 MG/LasanalyticalNo ratings yet
- Remote Sensing of Environment: SciencedirectDocument28 pagesRemote Sensing of Environment: SciencedirectAmmara HabibNo ratings yet
- Fmaths 3RD Term YR11 PlanDocument28 pagesFmaths 3RD Term YR11 Planadegunloye temitopeNo ratings yet
- Chapter 4 Structure EditedDocument9 pagesChapter 4 Structure Editedyeshi janexoNo ratings yet
- TUC5+ Modbus ID Details PDFDocument10 pagesTUC5+ Modbus ID Details PDFvijikeshNo ratings yet