Professional Documents
Culture Documents
Assessment Dignosis Planning Implementation Evaluation: Nursing Process: What To Do Assessment
Uploaded by
Rgn McklOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessment Dignosis Planning Implementation Evaluation: Nursing Process: What To Do Assessment
Uploaded by
Rgn McklCopyright:
Available Formats
NURSING PROCESS: framework for providing professional, quality nursing care.
It directs nursing activities for health promotion, health protection, and disease prevention and is used by nurses in every practice setting and specialty. The nursing process provides the basis for critical thinking in nursing (Alfaro-LeFavre, 1998, p. 64). ASSESSMENT Gather pertinent data Interpret data Keep an open mind by questioning assumptions about data Thinking about what information to collect Determining significance data Making conclusions about the data DIGNOSIS Develop conclisions Seek reasons and principles that justify nursing nursing judgements Test conclusions againt criteria Suspends judgement when data is insufficient Differentiate essential and trivial data PLANNING Explore alternative actions Collaborate with others Examine assumtions Reframe problems in order to generate solutions Generate ideas and possible solutions Action is based on rationales IMPLEMENTATION Communicate with others to solve complex problems Accurately report data and clues EVALUATION Establish standards logically Analyze course of action Critique outcomes Evaluate the conclusions
NURSING PROCESS: WHAT TO DO Assessment When a patients history is assessed, it should include those people who share living and sleeping spaces and can provide important information about the patients sleep behavior. Four areas of assessment are to be addressed concerning sleep disorders. These areas are: Sleep History Medical History Diet and drug History, and Psychosocial History
The SLEEP HISTORY should include the impact of the sleep complaint on the individuals daily life. Obtaining a 24-hour sleep diary over the course of a week or two can help identify the daily sleep pattern. The observations of bed-partners or caregivers are important contributions to the sleep history. It is necessary to obtain a thorough MEDICAL HISTORY in the assessment of a sleep complaint. Ask about existing health problems and medication use, particularly in situations when older adults self-medicate with over-the-counter (OTC) products. Various medical conditions may contribute to sleep disturbances.
A DRUG HISTORY that includes prescription and nonprescription medications, as well as alcohol, caffeine, and nicotine, is essential to sleep assessment. A PSYCHOSOCIAL HISTORY should first begin with PSYCHIATRIC ILLNESSES, such as anxiety, depression and dementia. This should be followed by a SOCIAL HISTORY that includes experiences, such as grieving the illness, or loss of friends and family, and translocation.
Nursing Diagnosis Sleep Pattern Disturbances Risk for Injury Altered Thought Processes Ineffective Coping
A. The American Sleep Disorders Association classifies sleep disturbances into four categories: 1. Dyssomnias disorders of initiating and maintaining sleep and of excessive sleepiness; 2. Parasomnias disorders or arousal, partial arousal, and sleep stage transition. Arousal disorders are presumed to be due to an abnormal arousal mechanism. Forced arousal from sleep can induce episodes. The "classical" arousal disorders are sleepwalking (somnambulism), sleep terrors and confusional arousals. Experts believe the various types of arousal disorders are related and share some characteristics. These arousals occur when a person is in a mixed state of being both asleep and awake, generally coming from the deepest stage of nondreaming sleep. This means a person is awake enough to act out complex behaviors but still asleep and not aware or able to remember these actions. 3. Disorders associated with medical or psychiatric disorders; 4. Proposed sleep disorders disorders that continue to be studied, in an effort to make them better defined. B. Periodic limb movements in sleep (PLMS) and sleep-related breathing disorders, including apnea and hypopnea, may cause sleep arousals. However, older adults with these conditions often do not recognize that the conditions are disturbing sleep. 1. Periodic limb movements in sleep (PLMS) is a condition in which the legs kick or jerk at 20- to 40-second intervals throughout the night, resulting in fragmented sleep (brief arousals that occur throughout the night and reduce the total amount of time spent in deep levels of sleep), complaints of insomnia, and at times, complaints of excessive daytime sleepiness. A related disorder, restless legs syndrome (RLS), produces disagreeable leg sensations that are relieved only by moving the legs. RLS can occur prior to sleep onset and in the daytime, when the individual is in a relaxed state. C. The onset of acute illness or the progression of chronic illness may cause sleep disorders.
Pain caused by arthritis, fractures, cancer, or other conditions may manifest in sleep delay or disruption. D. Commonly occurring problems of older adults including nocturia, dementia, alcoholism, and depression are known causes of sleep disturbance. Planning Goal will be made to promote normal, restful sleep for clients having sleep disturbances and/ or difficulties Interventions to promote sleep and rest A. Treatment for sleep-related disorders in the older adult includes both nonpharmacologic and pharmacologic options. B. Individuals who are identified as having PLMS or sleep-related breathing disorder should be referred for further assessment and treatment. It is important to manage the medical conditions, psychological disorders, and other symptoms that interfere with sleep. C. NONPHARMACOLOGIC OPTION: C.1. Remove contributing factors. The first line of treatment in all sleep-related disorders is to remove the suspected contributing factors. If symptoms are related to a medical illness, that illness should be treated. C.1.1. Drugs identified as likely to be interfering with sleep should be reassessed and, if possible, changed after consultation with the individuals physician. C.1.2. If sleep assessment identifies alcohol, caffeine, or nicotine use as possible causes of sleep disorder, counseling about smoking cessation and alcohol intake must be offered to these individuals. Decreasing caffeine and fluid intake late in the day may help promote sleep. Reducing fluid intake in the evening can help reduce the need to void during the night. C.1.3. If obesity is a complicating health factor, treatment should include regular exercise, and other strategies to effect a lifestyle change. C.2. Patient Education. It is important to help the older adult client to understand the nature of a sleep disturbance and how to recognize age-related changes in sleep. Provide him/her with information about factors that affect sleep and encourage the older adult to maintain a sleep diary. Teach the patient about and implement Sleep Hygiene Measures C.3.1. Develop and support consistent and rest-promoting bedtime routines: Maintain a consistent retiring and waking time. The routine could include changing into night clothes, washing face and teeth, and going to the bathroom immediately before bedtime. Assist in the bedtime routine. Offer a bedtime snack or beverage, but do not offer those that negatively influence sleep such as coffee, teas, or sodas. The bedroom should be used for sleep only. Other daily
C.3.
activities should be carried out in another room, if possible. Developing a sleep story that the older adult can think about once he or she enters the bed may promote a restful state of mind. Frequent daytime napping should be discouraged. A daily exercise routine, depending on physical ability, should be developed. C.3.2. Use relaxation techniques to promote sleep. Arthritis, pain, joint discomfort and illness-associated stresses cause sleep disturbances. Teach the patient progressive relaxation and to listen to music or use guided imagery. Create an environment conducive to sleep. One critical factor contributing to sleep disorders in hospitalized older adults is the noise level created by activity and talking by nurses and other hospital caregivers. Close the patient door, turn the light down or use a night light, lower your voice, set the room temperature to the patients preference, and provide at least 6 hours of uninterrupted sleep. C.3.3. When awakening during the night, avoid looking at the clock; frequent time checks will heighten anxiety and make sleep onset more difficult. Turn the clock away from the patients view. C.3.4. Expose the person to bright sunlight upon awakening, but should be avoided just before bedtime. In fact, television watching should be discouraged because of the light intensity that triggers wakefulness. C.4. C.5. Use of Positive Airway Pressure Cognitive-behavior therapy is designed to change poor sleep habits, change the patients beliefs and attitudes that may exacerbate insomnia.
D. PHARMACOLOGIC OPTION D.1. Pharmacologic intervention is recommended for the older adult for short-term use only. Sedative / hypnotic drugs are used to treat sleep disorders in older adults. When necessary, a benzodiazepine with a short or intermediate action is suggested. Temazepam (Restoril) and Triazolam, (Halcion), two drugs of this class of Benzodiazepines, have good effects at low doses and fewer potential side effects than longer acting drugs. A two-week maximum time period should be observed to avoid dependence on these sleep aids. Behavioral and pharmacological approaches are effective for the short term management of sleep disturbances in older adults. Sleep improvements are better sustained through behavioral treatment and close monitoring and reassessment of adherence to the treatment plan. Evaluation Determines whether the interventions have promoted a normal sleep pattern, minimized sleep deprivation symptoms, and improved client understanding of how to promote sleep.
Umlauf, M.G., Chasens, E. R., & Weaver, T. E. (2003). Excessive sleepiness. In M. Mezey, T. Fulmer, I. Abraham, & D. A. Zwicker (Eds.). Geriatric nursing protocols for best practice. (2nd ed., pp. 47-65). Redeker, N. S. (2000). Sleep in acute care settings: An integrative review. Journal of Nursing Scholarship
You might also like
- Fundamentals Note TakingDocument3 pagesFundamentals Note TakingJero BallesterosNo ratings yet
- Acid Base Balance: Carol Johns, MSN, RNDocument36 pagesAcid Base Balance: Carol Johns, MSN, RNkatrinasdNo ratings yet
- Cardiovascular FunctionDocument157 pagesCardiovascular FunctionJonnabelle PadillaNo ratings yet
- Simple Guide For Basic Nursing InterventionsDocument13 pagesSimple Guide For Basic Nursing InterventionsMelvin NizelNo ratings yet
- Rhythm P Wave PR Interval QRS Rate Regularity Life Threatening CausesDocument3 pagesRhythm P Wave PR Interval QRS Rate Regularity Life Threatening CausesLedio XhezairiNo ratings yet
- Or Illness Were Often Related To Superstitious: Beliefs and The Treatment Also Often Involved Magical CuresDocument29 pagesOr Illness Were Often Related To Superstitious: Beliefs and The Treatment Also Often Involved Magical CuresMitchee ZialcitaNo ratings yet
- Cardiovascular ADocument3 pagesCardiovascular AAutumn AllisonNo ratings yet
- Nurses Note DONEDocument1 pageNurses Note DONEjhenssineNo ratings yet
- Med Surg Test 4 Study GuideDocument29 pagesMed Surg Test 4 Study GuideJessNo ratings yet
- Emergency Approaches To Neurosurgical ConditionsDocument217 pagesEmergency Approaches To Neurosurgical Conditionsashwini sharmaNo ratings yet
- Concept Map SepsisDocument4 pagesConcept Map SepsisSavanna ChambersNo ratings yet
- Nursing Concept MapDocument2 pagesNursing Concept MapMary Mann100% (1)
- NURS 4369 Preceptor Packet Core 2013Document11 pagesNURS 4369 Preceptor Packet Core 2013Aruna Chezhian100% (1)
- CC Concept MapDocument9 pagesCC Concept Mapapi-606252228No ratings yet
- X-Ray Interpretation Skills: Dr. Hisham AlsanawiDocument68 pagesX-Ray Interpretation Skills: Dr. Hisham AlsanawiVika DamayNo ratings yet
- Concept Map 1Document5 pagesConcept Map 1api-396919069No ratings yet
- NLN Pharmacology Study Guide Final 6-3-2013Document65 pagesNLN Pharmacology Study Guide Final 6-3-2013الأغا محمد زكارنة100% (2)
- Universally Accepted AbbreviationsDocument4 pagesUniversally Accepted AbbreviationsPamela Dela Cerna BrionesNo ratings yet
- HemaDocument15 pagesHemauzbekistan143No ratings yet
- Quotes NursingDocument14 pagesQuotes NursingFreddy ÁlvaroNo ratings yet
- Case StudyDocument6 pagesCase StudyMarie-Suzanne Tanyi100% (1)
- Nitroglycerin: Deficient Fluid VolumeDocument13 pagesNitroglycerin: Deficient Fluid VolumeSheana TmplNo ratings yet
- Pathophysiology of DMDocument5 pagesPathophysiology of DMRgn Mckl100% (3)
- Basic Nursing Fundamentals EliminationDocument35 pagesBasic Nursing Fundamentals Eliminationlisa100% (1)
- Usos de Bite Blocks PDFDocument25 pagesUsos de Bite Blocks PDFNatasha RiveraNo ratings yet
- NandaDocument28 pagesNandaAmit MartinNo ratings yet
- Handout NSNA Student PresentationDocument14 pagesHandout NSNA Student PresentationlisaNo ratings yet
- Infective EndocarditisDocument68 pagesInfective EndocarditisDr. Rajesh PadhiNo ratings yet
- Nutrition Study Guide - NursingDocument3 pagesNutrition Study Guide - NursingKaren HutchinsonNo ratings yet
- Heart Failure Case StudyDocument2 pagesHeart Failure Case StudyRC0% (1)
- Barangay Health PlanDocument1 pageBarangay Health PlanRgn McklNo ratings yet
- Nidana Panchaka 1-7Document73 pagesNidana Panchaka 1-7Sreeja Mohandas100% (1)
- Completed Concept MapDocument4 pagesCompleted Concept Mapapi-607361848No ratings yet
- This Study Resource Was: Maternity Case 5: Fatime SanogoDocument2 pagesThis Study Resource Was: Maternity Case 5: Fatime SanogoNicole AngelNo ratings yet
- Vitamin B12 Patient Teaching My FirstDocument5 pagesVitamin B12 Patient Teaching My FirstLaura HernandezNo ratings yet
- Part I: Emergency Department (ED) : SKINNY ReasoningDocument6 pagesPart I: Emergency Department (ED) : SKINNY ReasoningUzumaki KNo ratings yet
- Lemone 6e Chapter 31Document47 pagesLemone 6e Chapter 31Husein Fatih ArafatNo ratings yet
- Concept Map COPDDocument2 pagesConcept Map COPDnursing concept mapsNo ratings yet
- n360 Concept Map Care Plan Week 3 Sheryl SatoDocument15 pagesn360 Concept Map Care Plan Week 3 Sheryl Satoapi-283363983No ratings yet
- ISBAR Worksheet Olivia Jones Jasgou1752Document1 pageISBAR Worksheet Olivia Jones Jasgou1752Jasmyn Rose100% (1)
- BloodDocument27 pagesBloodRagda AhmedNo ratings yet
- Acetylsalicylic Acid AspirinDocument1 pageAcetylsalicylic Acid AspirinE100% (5)
- STUDENT Sepsis Rapid ReasoningDocument6 pagesSTUDENT Sepsis Rapid Reasoningghodghod123No ratings yet
- Brain Dump NUR 213 FINALDocument37 pagesBrain Dump NUR 213 FINALkelsey jackson100% (1)
- CNO. Ethical Framework - StudentDocument42 pagesCNO. Ethical Framework - StudentdanushaNo ratings yet
- ATI Nursing ModulesDocument9 pagesATI Nursing ModulestgushikaNo ratings yet
- MedSurgATI1Document97 pagesMedSurgATI1LeelanRamphal100% (1)
- Care PlanDocument2 pagesCare PlanLorina Lynne ApelacioNo ratings yet
- Medsurg ReviewDocument34 pagesMedsurg ReviewestberryNo ratings yet
- Nursing Concept Map 1Document3 pagesNursing Concept Map 1Norah Okafor Ezike67% (3)
- Acute Renal Failure-Student-Rapid ReasoningDocument4 pagesAcute Renal Failure-Student-Rapid Reasoningapi-268403950No ratings yet
- Ati RN 2016 NutritionDocument6 pagesAti RN 2016 NutritionStan Tan0% (1)
- Medsurg 2007Document15 pagesMedsurg 2007WisdomIsMisery100% (1)
- Nursing NotesDocument6 pagesNursing NotesLinguumNo ratings yet
- Fetal Alcohol Syndrome Brochure For Nursing SchoolDocument2 pagesFetal Alcohol Syndrome Brochure For Nursing SchoolKrystal Cowley Miller100% (1)
- NUR100 Sherpath CH 3 Community Based Nursing Public Health NursingDocument12 pagesNUR100 Sherpath CH 3 Community Based Nursing Public Health Nursingcaloy2345caloyNo ratings yet
- Community Health Nursing Notes (Second Year)Document6 pagesCommunity Health Nursing Notes (Second Year)anette katrinNo ratings yet
- Community Health Study GuideDocument9 pagesCommunity Health Study GuideShae Thomas100% (3)
- Portfolio NFDN 2004 1Document4 pagesPortfolio NFDN 2004 1api-306095474100% (1)
- Nursing Care PlanDocument6 pagesNursing Care PlanChesca MejiaNo ratings yet
- Shock SIRS & MODS - Lewis Flashcards - QuizletDocument17 pagesShock SIRS & MODS - Lewis Flashcards - QuizletNursyNurseNo ratings yet
- Care of Adults 26 Endocrine ManagementDocument26 pagesCare of Adults 26 Endocrine ManagementGaras AnnaBerniceNo ratings yet
- GI Notes For Exam 3Document4 pagesGI Notes For Exam 3cathyNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- Being An Ideal Filpino Holds A Lot of Responsibility and AccountabilityDocument1 pageBeing An Ideal Filpino Holds A Lot of Responsibility and AccountabilityRgn McklNo ratings yet
- Monthly Accomplishment Report Front PageDocument2 pagesMonthly Accomplishment Report Front PageRgn Mckl100% (1)
- Science and Technology in AsiaDocument6 pagesScience and Technology in AsiaRgn McklNo ratings yet
- FAQ On SALN Final March2016Document8 pagesFAQ On SALN Final March2016Julius AlemanNo ratings yet
- SWEETSHOTS PHOTOBOOTH Contract New Barrio ContractDocument4 pagesSWEETSHOTS PHOTOBOOTH Contract New Barrio ContractRgn McklNo ratings yet
- Pathophysiology: Next PageDocument3 pagesPathophysiology: Next PageRgn McklNo ratings yet
- Global Malnutrition and MetabolismDocument49 pagesGlobal Malnutrition and MetabolismRgn McklNo ratings yet
- Dalenat Bhs Dispensing 2021: Date Name AGE Date of Birth Illness Medicine (S) RemarksDocument1 pageDalenat Bhs Dispensing 2021: Date Name AGE Date of Birth Illness Medicine (S) RemarksRgn McklNo ratings yet
- Teaching PlanDocument6 pagesTeaching PlanRgn McklNo ratings yet
- Resignation LetterDocument1 pageResignation LetterRgn McklNo ratings yet
- Pathophysiology :DDocument6 pagesPathophysiology :DRgn Mckl100% (1)
- Post Stroke PamphletDocument2 pagesPost Stroke PamphletRgn McklNo ratings yet
- Amniotic FluidDocument68 pagesAmniotic FluidRgn McklNo ratings yet
- Hemispheric Stroke Scale by G1Document23 pagesHemispheric Stroke Scale by G1Rgn McklNo ratings yet
- Cervical MucusDocument24 pagesCervical MucusRgn McklNo ratings yet
- SweatDocument22 pagesSweatRgn McklNo ratings yet
- Dr. Dr. Juliandi Harahap, MADocument28 pagesDr. Dr. Juliandi Harahap, MAAnna GozaliNo ratings yet
- Nasal Polyp DR Eva 2018Document37 pagesNasal Polyp DR Eva 2018hudaNo ratings yet
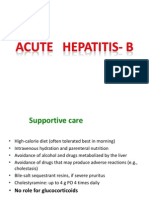
- Hepatitis BDocument48 pagesHepatitis BHari Suthan TNo ratings yet
- Actinomyces Israelii in The Review: Female GenitalDocument6 pagesActinomyces Israelii in The Review: Female GenitalfranciscaNo ratings yet
- Inserting IV Cannula LessonsDocument3 pagesInserting IV Cannula LessonsAlkenedy KahalNo ratings yet
- Drug Description: 5% Dextrose in 0.9% Sodium ChlorideDocument2 pagesDrug Description: 5% Dextrose in 0.9% Sodium ChlorideJesse ViolaNo ratings yet
- Lumbar Myofascial Pain SyndromeDocument8 pagesLumbar Myofascial Pain SyndromeYani Desi YantiNo ratings yet
- AsdasdDocument15 pagesAsdasdJohn Paulo RamosNo ratings yet
- Alice in Wonderland Syndrome - EditedDocument9 pagesAlice in Wonderland Syndrome - Editedcharles wambuiNo ratings yet
- Pancreatic Pathology For The SurgeonDocument10 pagesPancreatic Pathology For The SurgeonSanjaya SenevirathneNo ratings yet
- Review Jurnal 2Document10 pagesReview Jurnal 2UlfahNo ratings yet
- NRSG 780 - Health Promotion and Population Health: Module 2: Determinants of HealthDocument44 pagesNRSG 780 - Health Promotion and Population Health: Module 2: Determinants of HealthjustdoyourNo ratings yet
- Cefuroxime Drug StudyDocument4 pagesCefuroxime Drug StudyDona Jane BritosNo ratings yet
- Nursing Management of Gastro Intestinal Problem 2Document20 pagesNursing Management of Gastro Intestinal Problem 2wyneNo ratings yet
- Running Head: CASE MANAGEMENT 1Document12 pagesRunning Head: CASE MANAGEMENT 1Quality workNo ratings yet
- UntitledDocument4 pagesUntitledsharenNo ratings yet
- NCP and DrugsDocument13 pagesNCP and DrugsApRil ANn ChUa BingcangNo ratings yet
- Set 1 Checked: E. Pathological ConditionDocument60 pagesSet 1 Checked: E. Pathological ConditionKunal BhamareNo ratings yet
- L2 Triage PrinciplesDocument38 pagesL2 Triage PrinciplesCrystal CHAN (FABULOUS)No ratings yet
- J.B. Family Case Presentation Group 1Document67 pagesJ.B. Family Case Presentation Group 1Jeno Luis AcubNo ratings yet
- Rumana Shaikh 333 Pharmacology - Individual Task Topic 23-24 (VI Semester)Document10 pagesRumana Shaikh 333 Pharmacology - Individual Task Topic 23-24 (VI Semester)Rumana ShaikhNo ratings yet
- Narrative ReportDocument1 pageNarrative ReportMelvin Aurelio100% (1)
- Vaginal Cleansing Before Unscheduled Cesarean DeliveryDocument14 pagesVaginal Cleansing Before Unscheduled Cesarean Deliveryida husenNo ratings yet
- Non Invasive Imaging in NASHDocument3 pagesNon Invasive Imaging in NASHParul SoodNo ratings yet
- Drug Eruptions 2 Medical Students-1Document24 pagesDrug Eruptions 2 Medical Students-1Abdelmouez AnwerNo ratings yet