Professional Documents
Culture Documents
Br. J. Anaesth.-1999-Stoneham-910-9
Uploaded by
Justy GuavaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Br. J. Anaesth.-1999-Stoneham-910-9
Uploaded by
Justy GuavaCopyright:
Available Formats
British Journal of Anaesthesia 82 (6): 91019 (1999)
REVIEW ARTICLE
Regional anaesthesia for carotid endarterectomy
M. D. Stoneham
1
* and J. D. Knighton
2
1
Nufeld Department of Anaesthetics, Level 1, Oxford Radcliffe NHS Hospital, Headington,
Oxford OX3 9DU, UK.
2
Department of Anaesthetics, Southampton General Hospital, Tremona Road,
Southampton SO9 4XY, UK
*Corresponding author
Br J Anaesth1999; 82: 91019
Keywords: anaesthetic techniques, regional, cervical plexus; surgery, vascular
Every year in the UK, carotid artery occlusive disease kills
approximately 1 in 100 of the population aged more than
75 yr.
38
The underlying pathophysiology is development of
a plaque at the carotid bifurcation with ulceration and
embolization of thrombus or plaque debris causing transient
ischaemic attacks (TIA) or a stroke. The risk of stroke is
approximately 5% per annum if asymptomatic and 10% per
annum in a patient with TIA. One-third of strokes are
fatal, one-third leave signicant morbidity and one-third
recover.
101
Carotid endarterectomy is a preventative opera-
tion to reduce the incidence of embolic and thrombotic
stroke.
The rst carotid endarterectomy was performed at St
Marys Hospital, London, in 1954.
29
In the UK, by 1992
approximately 3000 were being performed every year.
66
This number had been increasing steadily over the previous
10 yr.
67 68
This increase was probably a result of publication
of the results of large prospective studies from North
America
71
and Europe
33 64
showing the benet of surgical
over medical strategies for the treatment of high grade
(70%) carotid stenosis. In the USA, approximately
100 000 carotid endarterectomies are performed every
year,
101
much higher proportionately than in the UK, perhaps
because of the greater tendency of American surgeons to
operate on patients with asymptomatic carotid stenosis.
However, the surgical indications for carotid endarterectomy
in the UK are also changing, with more asymptomatic
patients
73
and more patients with recovered strokes
52
being
operated on. This trend is likely to continue in the future,
with greater emphasis on preventative medicine and screen-
ing for cardiovascular diseases. Indeed, the European
Carotid Surgery Trial data suggest that there will be a three-
to ve-fold increase per annum in the number of carotid
endarterectomies performed.
33
Unfortunately, carotid endarterectomy carries a signicant
perioperative mortality rate from stroke and myocardial
British Journal of Anaesthesia
infarction which may even approach 5%.
2 52 71 103
Thus
anaesthetic and surgical techniques are constantly under
scrutiny to try to reduce this relatively high incidence of
morbidity and mortality for an operation which in itself is
only preventative. Regional anaesthesia is an alternative
to general anaesthesia which has attracted considerable
attention amid claims of a reduction in operative morbidity
and mortality.
105
This review describes the problems and
some solutions for providing regional anaesthesia for carotid
endarterectomy.
Regional or general anaesthesia?
There can be few operations in which there is such a
discrepancy between the opinions of anaesthetists and
surgeons, in terms of the best anaesthetic technique to use,
as there is for carotid endarterectomy surgery.
In the UK, carotid endarterectomy has traditionally been
performed under general anaesthesia because of surgeons
and patients preferences,
66
but perhaps additionally because
many British anaesthetists are not comfortable or trained
to perform cervical plexus blocks or cervical epidural
anaesthesia.
38
However, in the USA, regional anaesthesia
for carotid endarterectomy is used more commonly. A
recent survey of 216 American neuro-anaesthesiologists
found that 17% of carotid endarterectomies were performed
under regional anaesthesia,
17
although overall in the USA
this value is probably much higher as American neuro-
surgeons appear less inclined to use regional anaesthesia
than vascular surgeons. There has been more interest
recently on both sides of the Atlantic Ocean with the
increasing body of evidence that morbidity, and even
mortality, may be reduced if carotid surgery is carried out
using a regional anaesthetic technique.
97
This has now
reached the point where a multicentre, prospective, random-
ized, controlled comparison of regional vs general anaesthe-
Regional anaesthesia for CEA
sia for carotid endarterectomy is about to start in the UK (Mr
M. Gough, Professor C. Warlowe, personal communication).
Of prime concern during carotid endarterectomy is protec-
tion of the brain during carotid cross-clamping.
1
For a
patient under general anaesthesia, this is a considerable
problem and various techniques have been used to detect
inadequate cerebral perfusion, including the use of: carotid
artery stump pressure measurement
58
; electroencephalo-
graph (EEG) processing
63
; somatosensory evoked poten-
tials
49
; transcranial Doppler of the middle cerebral artery
89
;
near infrared spectroscopy
26
; and combinations of some of
these techniques.
1
Transcranial Doppler may also facilitate
reliable detection of particulate embolization during opera-
tion
88
and thus give the surgeon acoustic feedback during
dissection, clamping and unclamping of the internal carotid
artery.
1
Near infrared spectroscopy is a relatively new
technique with high sensitivity but relatively low specicity,
but which certainly merits further attention.
26
Surgeons and anaesthetists use one or more of these
techniques to determine which patients require bypass of
the carotid cross-clamp by insertion of an internal carotid
artery shunt.
34 81
Unfortunately, all of these methods have
relatively poor sensitivity and specicity in detecting inad-
equate cerebral perfusion. Thus, for example, some surgeons
insert a shunt on all patients or, alternatively, the anaesthetist
may augment arterial pressure pharmacologically in an
attempt to maintain cerebral blood ow during general
anaesthesia.
In contrast, during a regional anaesthetic technique, a
conscious patient provides a very sensitive and specic,
albeit indirect, monitor of cerebral perfusion. Changes in
speech, cerebration or motor power after carotid cross-
clamping indicate inadequate cerebral perfusion and the
immediate need to insert a shunt. Carotid endarterectomy
is one of the few operations with such an appropriate
monitor of the patients well-being. The requirement for
carotid shunting is reduced to only 1015% using a regional
anaesthetic technique if strict criteria for shunting are
applied.
13 35 36
This may itself be benecial as the use of a
shunt has a nite risk of stroke,
94
although the use of
routine or selective shunting in carotid surgery has not been
shown to affect outcome signicantly in either direction.
21
Advocates of general anaesthesia for carotid endarter-
ectomy cite several advantages of the technique,
38 99
includ-
ing: airway control throughout the procedure; tight control
of arterial carbon dioxide concentration; cerebral protective
effects of barbiturates; and the possibility of inducing
hypothermia if required.
29
However, there are known dis-
advantages, apart from the requirement for cerebral perfu-
sion monitoring during carotid cross-clamping, including:
potential steal phenomenon of isourane
30
; the fact that
high concentrations of isourane are required to achieve
cerebral protection
60
; and postoperative nausea and vomit-
ing which may occur with general anaesthesia. Additionally,
cardiovascular instability is common and difcult to prevent
under general anaesthesia, because of the sympathoadrenal
911
responses to induction of anaesthesia, tracheal intubation,
surgical incision and tracheal extubation in this group of
patients who may have severely compromised coronary and
cerebral circulation.
Proponents of regional anaesthesia claimother advantages
apart from ease of monitoring cerebral perfusion,
105
including: lower requirement for shunting
13 36
; lower cardio-
vascular morbidity
2
; shorter ICU and hospital stay
2
; less
expense overall than general anaesthesia
39
; and avoidance
of intubation in patients with COPD. There are more subtle
advantages, such as avoidance of blind arterial pressure
augmentation and its potentially detrimental effects on the
heart
101
and better cerebral autoregulation compared with
general anaesthesia.
57
However, there are clearly disadvant-
ages with this method, such as: complications of the various
regional techniques; problems of emergency intraoperative
airway control; the fact that it does not prevent myocardial
ischaemia
50
; and the high degree of patient co-operation
and contact required throughout the procedure.
Against this highly polarized background, is there any
rm evidence that either of the techniques is associated
with an improvement in outcome? Unfortunately no large,
prospective, randomized studies are available to draw rm
conclusions. A recent meta-analysis by Tangkanakul,
Counsell and Warlow
97
of all studies published comparing
regional and general anaesthesia for carotid endarterectomy
noted that there were only three randomized studies examin-
ing 143 patients, but that there were 17 non-randomized
studies investigating almost 6000 patients, which were
subject to the potential aws and biases of non-randomized,
retrospective studies. Denite conclusions are thus not
possible. However, the authors concluded that there are
potentially important benets from performing carotid
endarterectomy under local anaesthesia and recommended
that a prospective randomized study of 2000 patients be
conducted to answer the question. Such a study would have
90% power to detect a 50% difference in perioperative
stroke or death at the 5% signicance level.
97
Of the three published, randomized, controlled studies,
only one has shown signicant differences in outcome in a
group of 100 patientsa small reduction in the incidence
of local haematoma in patients receiving local anaesthesia
and a signicant decrease in carotid shunting.
36
Two other
randomized studies examined a smaller number of patients
and concentrated on haemodynamic differences, showing
that hypertension was more common in the peroperative
period
75
and hypotension was more common after operation
in the local anaesthetic groups.
75 77
However, in the non-
randomized studies, there were apparently large differences
in outcome between general and regional anaesthesia. Thus
there are studies showing a signicant reduction in the
incidence of perioperative stroke,
35
cardiovascular post-
operative complications (including myocardial ischaemia,
arrhythmia, myocardial infarction and heart failure)
2
and
hospital and ICU stay.
39
Combining the data from these non-
randomized studies, Tangkanakul, Counsell and Warlow
97
Stoneham and Knighton
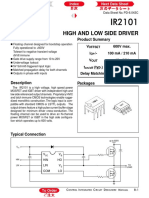
Fig 1 Anatomy of the cervical dermatomes.
suggest that overall, within 30 days of operation, the use
of regional anaesthesia is associated with a 50% reduction
in the relative odds of death, stroke, myocardial infarction
and pulmonary complications such as pneumonia, pulmon-
ary embolus and prolonged intubation. However, the authors
point out many aws in the non-randomized studies, includ-
ing the retrospective nature, use of non-sequential analysis
and the fact that in many, statistical analysis of the number
of arteries operated on was performed, not the number of
patients (i.e. some patients underwent bilateral procedures).
Clearly, in order to undergo the second carotid endarter-
ectomy, a patient must survive the rst operation.
A denitive answer to the question as to which technique
is best is eagerly awaited. Meanwhile, regional anaesthesia
for carotid surgery is becoming increasingly popular in the
UK, with several vascular surgeons and anaesthetists having
recently adopted or considering adopting the technique. In
the UK, we are ideally placed to conduct a randomized,
controlled study of general vs regional anaesthesia for
carotid endarterectomy which might nally settle this
important question.
Which regional anaesthetic technique should
be used?
Carotid endarterectomy under regional anaesthesia requires
block of the second (C2), third (C3) and perhaps the
fourth (C4) cervical dermatomes (Fig. 1) which may be
accomplished in several different ways. No differences in
morbidity or mortality have been shown between these
different regional techniques. Regional anaesthesia is suit-
able for any of the surgical approaches to the carotid artery,
including transverse and vertical incisions, although local
anaesthetic supplementation will be required if a transverse
incision crosses the midline.
Local inltration
The use of local inltration alone has been described
18 27
and is currently used by some surgeons, although this
technique may be slow, uncomfortable, and would certainly
not be tolerated well by all patients. Many surgeons do not
912
Fig 2 Surface markings for deep cervical plexus block.
have the patience to use this technique effectively although
it is certainly feasible. Thus it may be more appropriate to
use a regional technique.
Cervical epidural anaesthesia
This is not used much in the UK, although there are large
case series reporting its successful use in patients undergoing
carotid surgery, particularly in France.
6 7 10 45 76
For place-
ment of the epidural catheter, patients are positioned sitting
with the neck exed, chin on chest, to open the lower
cervical interspaces. A 16- or 18-gauge Tuohy needle is
introduced in the midline with a drop of saline in the hub,
which is aspirated inwards by negative pressure when the
needle enters the cervical epidural space (hanging drop
technique). An epidural catheter is then threaded through
the Tuohy needle to leave 34 cm in the epidural space.
After negative aspiration, a suitable test dose is administered
followed by 1015 ml of a local anaesthetic solution, such
as 0.5% bupivacaine.
Proponents of cervical epidural anaesthesia cite the sim-
plicity and success of the technique.
6
However, all cervical
and upper thoracic nerve roots are potentially affected
bilaterally. There is signicant associated morbidity, includ-
ing a high incidence of cardiovascular side effects such as
hypotension and bradycardia, respiratory failure requiring
intubation in 1%, dural puncture in 0.5% and bloody tap
in 2%.
6
Alterations in pulmonary function are detectable in
100% of recipients and its use for routine clinical purposes
has therefore been condemned.
11
Additionally, in our experi-
ence, placement of a cervical epidural in an elderly patient
with calcied spinous ligaments in the sitting position using
the hanging drop technique is not to be undertaken lightly.
Cervical plexus block, which is easier to perform, affects
unilateral nerve roots only and has less cardiovascular side
effects, is a safer alternative.
Deep cervical plexus block
100
The cutaneous distribution of the cervical plexus is shown
in Figure 1. It may be blocked either deep, as the spinal
nerves lie on the cervical transverse processes (Fig. 2, 3),
Regional anaesthesia for CEA
Fig 3 Deep cervical plexus block.
Fig 4 Supercial cervical plexus block.
or supercially, as the cutaneous branches emerge from the
posterior border of the sternocleidomastoid (Fig. 4). For
carotid surgery, commonly a deep cervical plexus block is
used alone
36 96 102
or a combination of deep and supercial
cervical plexus block.
2 3 15 23 24 39 59 69
Deep cervical plexus
block is technically more difcult to perform and may be
associated with more serious complications than supercial
cervical plexus block,
55
although it may be more reliable
and provide better postoperative analgesia.
92 93
The deep
block may be performed by single injection at C3 or C4,
as rst described by Winnie and colleagues,
102
or by a
three-injection technique at C2, C3 and C4, as described
by Moore.
61
The modied single-injection technique of
Winnie and colleagues
102
at C3 is favoured by the authors
and is described in detail below (Fig. 2, 3).
The patient lies supine, slightly sitting up, with the head
turned to the opposite side. The skin is disinfected with
chlorhexidine in alcohol. The cervical transverse processes
are palpated manually, approximately 1 cm posterior to
the posterior border of the sternocleidomastoid. The C3
transverse process may be located by counting up from the
C6 transverse process (Chassaignacs tubercle) which is at
913
the level of the cricoid cartilage. After intradermal inltra-
tion of 1% lidocaine 0.25 ml at the level of the C3 transverse
process, a 1-inch, 25-gauge needle is introduced at right
angles to the skin but aiming in a slightly caudal direction
to avoid intrathecal injection. After location of the transverse
process 12 cm from the skin, or after the patient reports
paraesthesia in the distribution of the cervical plexus (Fig. 1),
0.375% plain bupivacaine 20 ml is injected by a second
operator. An immobile needle technique is used in which a
short length of tubing is placed between the needle and
syringe to minimize needle movement resulting from
manipulation of the syringe. In our experience, it is more
common to attempt injection too posteriorly rather than too
anteriorly.
Controversy persists as to whether paraesthesia should
be actively sought during placement of a regional block,
62
with some evidence that this leads to a higher incidence of
postoperative dysaesthesia.
85
This view has been challenged
as techniques eliciting paraesthesia have been shown to
make axillary brachial plexus block more effective.
84
Deep
cervical plexus block also appears to be more successful in
terms of less additional local anaesthetic requirements when
paraesthesia is elicited during placement
92 93
or when a
nerve stimulator is used to make the block more effective.
59
Our unpublished observations suggest that paraesthesia is
reported by 3050% of patients undergoing deep cervical
block placement. Further study is underway to determine
if the dermatome where paraesthesia is elicited is important
in determining the efcacy of cervical block.
Whichever technique is chosen for deep block there are
serious potential complications, including: vertebral artery
injection producing immediate loss of consciousness or
convulsions
47
; subarachnoid
5 70
or epidural
82
injection; and
phrenic nerve palsy. The latter occurs in the majority of
recipients of deep cervical block
15
but appears to be tolerated
reasonably well by those with normal pulmonary function.
16
However, in patients with underlying pulmonary dysfunc-
tion, this may cause severe respiratory embarrassment.
91
In
selected patients with underlying respiratory impairment it
may be more appropriate to perform supercial block alone
which is effective for surgery.
92 93
Other potential side effects of deep cervical plexus block
include: local haematoma (which is rarely a signicant
problem); hoarseness (caused by recurrent laryngeal nerve
involvement); dysphagia; stellate ganglion block, which
may be bilateral
91
; and Horners syndrome.
14 55
Aspiration
of blood during placement of cervical plexus blocks is
common, occurring in as many as 30% of cases.
25
Therefore,
it is vital to aspirate frequently during injection of local
anaesthetic to avoid intravascular injection, which may have
profound consequences, including immediate grand mal
seizure.
25
Complications may also be caused by surgery
itself, particularly cranial nerve damage, which may occur
in up to 25% of patients undergoing carotid endarter-
ectomy.
22 83 95 106
Stoneham and Knighton
Supercial cervical plexus block
Supercial block is rarely used alone for carotid surgery.
The deep branches of the cervical plexus supplying the
neck muscles are not blocked and therefore there is the
theoretical drawback of lack of neuromuscular block making
surgery on deep structures more difcult.
46 55
Despite this,
supercial block is certainly an effective technique for
carotid artery surgery.
92 93
It has been used to ll in
inadequately blocked dermatomes from the deep block.
55
Supercial cervical plexus block is simpler to perform than
deep block (Fig. 4). With the patient positioned as for the
deep block, the skin is disinfected and an intradermal bleb
of 1% lidocaine is raised at the midpoint of the posterior
border of the sternocleidomastoid. Bupivacaine 0.375%
(20 ml) is injected in the subcutaneous plane along the
posterior body of the sternocleidomastoid in cranial and
caudal directions fromthis point. We have found it benecial
to inltrate with local anaesthetic solution along the inferior
border of the mandible, to block afferent branches from the
facial nerve. This appears to reduce the pain associated
with prolonged use of a retractor under the mandible at the
cephalad end of the incision.
Attention should be paid to the total dose of local
anaesthetic administered when using combined deep and
supercial cervical plexus blocks. Large doses of local
anaesthetic approaching toxic limits have been used
40
and
plasma concentrations have been reported as approaching
toxic levels after combined deep and supercial cervical
plexus blocks.
98
The question of which local anaesthetic
agent to use is also relevant. Bupivacaine or lidocaine or a
mixture of the two are commonly used, although the use
of lidocaine alone may not provide adequate analgesia for
the duration of the procedure. It may on occasions last up
to 3 h. The use of ropivacaine has also recently been
described
53
which may have advantages over bupivacaine
in terms of its safety prole.
Preoperative patient assessment
Patients requiring carotid artery surgery commonly have
co-existing medical problems: indeed, widespread arterial
disease is not uncommon. The most common complications
after carotid artery surgery are cardiac. Therefore, the
preoperative visit should be directed at identifying active
cardiovascular disease, particularly evidence of heart failure,
uncontrolled angina, recent myocardial infarction or aortic
valvular disease. A resting electrocardiograph (ECG) should
be available for all patients but a detailed cardiac work-up
is required only if there are active symptoms or signs of
cardiac disease.
74
Patients requiring coronary artery surgery
and carotid surgery are usually operated on sequentially with
the more critical surgery performed rst.
56
Hypertension is
the single major risk factor in stroke
28
and adequate control
of arterial pressure before operation signicantly reduces the
risk of postoperative hypertension or neurological events.
4
Control of arterial pressure should have been achieved
914
before presentation for carotid artery surgery and normal
antihypertensive medications should be given on the morn-
ing of surgery, together with anti-anginal medications.
It is often the case that patients have been receiving
antiplatelet medications, such as low-dose aspirin or dipyrid-
amole, and these are usually continued until the day of
surgery, although individual surgeons preferences may vary.
Many of these patients are diabetic, and the perioperative
management of diabetes mellitus should be the same regard-
less of whether they receive regional or general anaesthesia.
Complications such as renal impairment should be identi-
ed, and occasionally retinopathy (proliferative, with a high
risk of haemorrhage) should be treated before carotid
artery surgery. Hyperglycaemia may worsen the damage to
ischaemic brain tissue
78
and must be avoided. The use of
insulin/dextrose/potassium infusions may be required to
control insulin-treated diabetics.
Respiratory disease is also common in this population in
whom there is a high prevalence of tobacco smoking.
Asthma and chronic obstructive pulmonary disease are
probably easier to manage in the awake, non-intubated
patient than in the patient under general anaesthesia. Occa-
sionally, such patients are unable to tolerate the procedure
without repeated coughing or respiratory difculties when
lying still under surgical drapes for 23 h. Additionally,
some techniques of regional anaesthesia may cause further
respiratory compromise associated with phrenic nerve para-
lysis. Thus a detailed history and examination should predict
high-risk patients in whom pulmonary function testing will
give a more detailed assessment, and in a few cases such
information will identify patients for whom an alternate
regional technique is appropriate, or even that general
anaesthesia is required. Anxiolytic premedication with a
benzodiazepine or opioid is required for most patients, but
over-sedation during the period of carotid artery cross-
clamping must be avoided.
Patients will also be encountered who have had previous
carotid surgery and require re-operation for stenosis.
Regional anaesthesia may be used successfully in these
patients despite the difculty of the operative dissection
and the fact that the disease may extend unusually high
into the internal carotid artery.
80
When the disease is very
high, local anaesthetic supplementation by the surgeon is
invariably required.
At the preoperative visit, considerable efforts should be
made explaining to a patient the benets of undergoing
carotid surgery under regional anaesthesia. It is our experi-
ence that persuading a patient to undergo carotid endarter-
ectomy under regional anaesthesia is not a problem when
the concept of monitoring cerebral perfusion during carotid
clamping is explained in greater detail. When combined
with the knowledge that they will receive adequate sedation,
that the anaesthetist will be talking to them throughout the
procedure and that general anaesthesia may still be induced
if required, the number of patients that refuse regional
anaesthesia outright is very low.
Regional anaesthesia for CEA
Perioperative monitoring
Monitoring, instituted before placement of the regional
block, consists of ve-lead electrocardiography (leads II
and V5),
32
invasive arterial pressure measured from the
contralateral radial artery and started before placement of
the block, a non-invasive arterial pressure cuff, oxygen
saturation (Sp
O
2
) and end-tidal carbon dioxide partial pres-
sure (PE
CO
2
), which may be approximated using a 2-m
length of ne manometer tubing placed within the oxygen
face mask.
8
Patients are given oxygen 4 litre min
1
via a
face mask throughout the procedure. I.v. access via a
peripheral cannula of at least 16-gauge is required and
an infusion of crystalloid commenced. Additional venous
access may be required for infusion of vasoactive drugs.
Small amounts of a benzodiazepine (diazepam 510 mg or
midazolam 12 mg) may be administered i.v. for anxiolysis
during insertion of the regional block, but when surgery
commences, further sedative medication should be avoided
if possible to allow meaningful assessment of the patients
neurological condition during cross-clamping. When in the
operating theatre, the operating table can be positioned so
that the patient is in a deck chair conguration which
may be more comfortable than a standard supine position.
Patients should be encouraged to empty their bladder
immediately before arrival in the anaesthetic room.
Diagnosis, management and treatment of
perioperative problems
Neurological dysfunction
It is of paramount importance during regional anaesthesia
for carotid endarterectomy that verbal contact with the
patient is maintained throughout the operation as this is the
principal reason for performing the surgery with the patient
awake. Patients who develop symptoms of cerebral
ischaemia such as slurring of speech, altered grip strength
or decreased conscious level after a 2-min trial cross-clamp
of the internal carotid artery should have a carotid shunt
inserted immediately to maintain ipsilateral carotid ow.
9
Even so, these patients are more likely to develop postopera-
tive neurological complications.
23
Patients who develop
changes in neurological function often do so at the time of
cross-clamping, but there may be a signicant delay in
presentation, which may be related to episodes of peri-
operative hypotension.
51
The patients head should be easily accessible to the
anaesthetist throughout the procedure, which may be
accomplished by elevating the surgical drapes away from
the patients head using a Mayo table or an L bar (Fig. 5).
The contralateral arm should also be accessible to facilitate
testing of grip strength.
Alternative methods of assessing motor power in the
limbs include the use of a childs squeezy toy, held in the
patients contralateral hand and squeezed intermittently by
the patient to demonstrate motor power qualitatively
90
or
915
Fig 5 Patient undergoing carotid endarterectomy under deep cervical
plexus block. Note accessibility of the patients head and use of the Bair
Hugger (see text for details).
the use of an air-lled bag attached to a pressure transducer
held by the patient and which, when squeezed intermittently,
generates a visible pressure waveform on an attached
monitor.
42
Patient discomfort
No regional technique for carotid endarterectomy is perfect
on every occasion. The largest published series describing
1000 cervical blocks for carotid surgery reported a
supplementation rate with local anaesthetic of 53%, with
66% of patients requiring sedation in the peroperative period
and 2.5% requiring conversion to general anaesthesia.
25
There are several reasons for this. First, patients are some-
times encountered in whom the carotid bifurcation or the
internal carotid artery disease extends so high that the
incision has to be extended into tissues not supplied by the
cervical plexus, but rather by cranial nerves. Second, no
matter how effective the block, as tested by analgesia to
pinprick before incision, patients sometimes complain of
pain from dissection around and within the carotid sheath.
This may be a reection of additional afferent bres
accompanying the sympathetic innervation of the carotid
vessel. Finally, the use of surgical retractors, particularly
under the mandible, may also stimulate tissues not covered
by the block. Supplementation of the block should not
therefore be regarded as a failure of the anaesthetic tech-
nique, but as a necessity to allow surgery to proceed
successfully.
Judicial supplementation of the block by the surgeon
with 0.5% lidocaine should therefore be encouraged if
required, but the anaesthetist should be constantly vigilant
to the possibility of intra-arterial injection of local anaes-
thetic. One of the authors has witnessed a grand mal t,
albeit very short-lived, after accidental injection of only
0.5% lidocaine 1 ml into the internal carotid artery under
exactly these circumstances.
Conversion to general anaesthesia
This may ultimately be necessary for a variety of reasons,
including loss of consciousness, airway obstruction, claus-
Stoneham and Knighton
trophobia, restlessness or grand mal seizure.
25
The conver-
sion rate to general anaesthesia is very low, generally
ranging between 1% and 3%.
20 25 35 48 72 86
However, tracheal
intubation of a patient under surgical drapes with an exposed,
or even clamped, internal carotid artery is technically
challenging, associated with haemodynamic instability and
certainly risky for the patient. A minimalist approach is
desirable. Minimal disturbance to the surgical eld and the
patients haemodynamic status may result if a laryngeal
mask airway is used to secure the airway after preoxygena-
tion and induction with propofol. This has been reported
previously for carotid endarterectomy under elective general
anaesthesia
87
and shown to be associated with less hyper-
tensive and tachycardic episodes than general anaesthesia
using a tracheal tube.
54
It is our preferred method if
conversion to general anaesthesia is required in the peroper-
ative period. The use of the L bar over the patients head
enables rapid access for airway control if it is required in
an emergency by swinging the bar away in a caudal direction
without de-sterilizing the open carotid wound.
Haemodynamic instability
Haemodynamic instability tends to be less common during
regional anaesthesia compared with general anaesthesia.
19 20
Arterial pressure is measured in both arms non-invasively
before operation. Arterial pressure during operation is
maintained within 20% of calculated limits either way of
the higher of these recordings. For persistent hypertension,
an i.v. infusion of a vasodilator such as glyceryl trinitrate
15 mg h
1
or beta adrenoceptor block with metoprolol
1 mg or labetalol 5 mg may be used. Persistent hypotension,
although much less common under regional than general
anaesthesia, should also be treated, for example with a
phenylephrine infusion (prepared by diluting phenyl-
ephrine 10 mg in 50 ml saline (200 g ml
1
), infusion rate
130 ml h
1
(3.3100 g min
1
)). Inltration with local
anaesthetic or section of the carotid sinus nerve by the
surgeon is sometimes performed to reduce intraoperative
haemodynamic instability, although it has been shown to
increase the incidence of postoperative hypertension and is
no longer recommended.
31 41
Fluid balance
Major blood losses are rarely a problem during carotid
endarterectomy, so perioperative uid administration should
only replace uid losses. In practice, this is no more than
5001000 ml of crystalloid uid. I.v. infusion of large
volumes of uid can lead to a full bladder which may
require emptying during operation, a challenging problem,
although not insurmountable. Glucose-containing solutions
should not be administered to patients undergoing carotid
cross-clamping because of the deleterious effects of hyper-
glycaemia on potentially ischaemic areas of brain.
78
Patient restlessness
This may be a symptom of inadequate cerebral perfusion.
It may also be the result of a patient lying immobile for
916
Table 1 Postoperative problems after carotid endarterectomy
d Cardiovascular
Hypotension
Hypertension (particularly after carotid sinus nerve section or local
anaesthetic block)
Arrhythmia
Myocardial ischaemia
d Airway obstruction caused by oedema or haematoma
d Neurological decitrequires immediate surgical opinion
d Hyperperfusion syndromeheadache, seizures, haemorrhage
3 h under surgical drapes on a hard operating table with
their head turned to one side. Some patients nd the surgical
drapes claustrophobic and become subjectively hot and
bothered under them. We have found a Bair Hugger forced
air warmer (Augustine Medical, Eden Prairie, MN, USA)
with temperature set on ambient, blowing cool air onto the
patients face, to be a very successful means of overcoming
this problem (Fig. 5).
It is our experience that limiting i.v. sedation to small
doses of benzodiazepines at the beginning of the procedure
enhances patient co-operation with surgery. This is further
ensured by constant reassurance and appropriate augmenta-
tion of the block with local anaesthetic by the surgeon if
required. As a last resort, a low-dose propofol infusion
(e.g. 2050 mg h
1
) may be used. Rarely, patients cannot
tolerate this surgery awake even with adequate regional
block and in these patients there is no substitute for general
anaesthesia.
Postoperative problems
Postoperative problems after carotid endarterectomy are
relatively common (Table 1), which is why careful observa-
tion in a well-staffed recovery area is necessary. Haemo-
dynamic complications are particularly common
104
and
therefore invasive arterial pressure and ECG monitoring
should be continued on recovery. Routine admission to
intensive care is probably not necessary.
79
However, a
period of close observation is worthwhile. Postoperative
haemodynamic monitoring in recovery for 3 h reduced ICU
admission to 2.3% and saved 30% of hospital costs.
43
Twenty-four hour total hospital stay has even been
reported,
37
although most surgeons and anaesthetists would
like to observe their patients after operation for a longer
period. Analgesia may be given but is rarely required
in recovery after a regional technique. If patients are
haemodynamically stable after 4 h, they may be discharged
to the ward. If there is evidence of myocardial ischaemia,
haemodynamic instability or neurological impairment, they
should be transferred to the intensive care unit for further
close monitoring.
Wounds must be observed carefully for signs of swelling
and, if required, re-explored immediately by the surgeons
in the operating theatre. Swelling of wounds may be caused
by frank haematoma
65
but also by generalized oedema of
the cervical tissues which occurs in all patients undergoing
this procedure.
12 44
Regional anaesthesia for CEA
Conclusions
Carotid endarterectomy is likely to become an increasingly
common operation as the population ages, preventative
medicine assumes a higher priority and life expectations
change. Regional anaesthesia is attractive and gaining in
popularity because of easy and reliable monitoring of
cerebral perfusion, lower overall costs and possibly a lower
incidence of morbidity and mortality. Pending the results
of large-scale, randomized, controlled comparisons of gen-
eral vs regional anaesthesia, the experience of the surgical
(and anaesthetic) teams is probably the most important
factor in deciding which anaesthetic technique to use for
carotid endarterectomy. Cervical plexus blocks are suitable
in most patients but a few will always require general
anaesthesia.
Acknowledgements
We thank Sarah Ward who provided the line drawings of the cervical
dermatomes and cervical plexus blocks.
References
1 Ackerstaff RG, vandeVlasakker CJ. Monitoringof brainfunction
during carotid endarterectomy: an analysis of contemporary
methods. J Cardiothorac Vasc Anesth1998; 12: 3417
2 Allen BT, Anderson CB, Rubin BG, et al. The inuence of
anesthetictechniqueonperioperativecomplicationsafter carotid
endarterectomy. J Vasc Surg1994; 19: 83442
3 Andersen CA, Rich NM, Collins GJ jr, McDonald PT. Carotid
endarterectomy: regional versus general anesthesia. AmJ Surg
1980; 46: 3237
4 Asiddao CB, DoneganJH, Whitesell RC, KalbeischJH. Factors
associated with perioperative complications during carotid
endarterectomy. AnesthAnalg1982; 61: 6317
5 Baraka A, Hanna M, Hammoud R. Unconsciousness and apnea
complicating parascalene brachial plexus block: possible
subarachnoid block. Anesthesiology1992; 77: 10467
6 Bonnet F, Derosier JP, PluskwaF, AbhayK, GaillardA. Cervical
epidural anaesthesia for carotid artery surgery. Can J Anaesth
1990; 37: 3538
7 Bonnet F, Szekely B, Abhay K, Touboul C, Boico O, Saada M.
Baroreceptor control after cervical epidural anesthesiainpatients
undergoingcarotidarterysurgery. J CardiothoracAnesth1989; 3:
41824
8 BromagePR. Theeffect of catheter positionontheaccuracyof
end-tidal carbondioxidemeasurement. Anaesthesia1996;51:198
9 Browse NL, Ross Russell R. Carotid endarterectomy and the
Javid shunt: the early results of 215 consecutive operations for
transient ischaemic attacks. Br J Surg1984; 71: 537
10 Campkin TV. Cervical epidural analgesia during carotid artery
surgery. Anaesthesia 1987; 42: 4379
11 Capdevila X, Biboulet P, Rubenovitch J, et al. The effects of
cervical epidural anesthesia with bupivacaine on pulmonary
function in conscious patients. AnesthAnalg1998; 86: 10338
12 Carmichael FJ, McGuire GP, Wong DT, Crofts S, Sharma
S, Montanera W. Computed tomographic analysis of airway
dimensionsafter carotidendarterectomy. AnesthAnalg1996; 83:
1217
13 Castresana EJ, Shaker IJ, Castresana MR. Incidence of shunting
during carotid endarterectomy: Regional versus general
anesthesia. RegAnesth1997; 22: 23S
917
14 CastresanaMR, Brooks AG, Masters RD, CastresanaEJ, Myers
GJ, NewmanWH. Incidenceof dysphagiainpatientsundergoing
carotidendarterectomyusingdeepandsupercial cervical plexus
block anesthesia. AnesthAnalg1994; 79: S52
15 CastresanaMR, MastersRD, CastresanaEJ, StefanssonS, Shaker
IJ, Newman WH. Incidence and clinical signicance of
hemidiaphragmatic paresis in patients undergoing carotid
endarterectomy during cervical plexus block anesthesia.
J NeurosurgAnesthesiol 1994; 6: 213
16 CastresanaMR, MastersRD, Shaker IJ, NewmanWH, Castresana
EJ. Bedsidepeakexpiratoryowratepredictshemidiaphragmatic
paralysis inpatients undergoingcarotidendarterectomies under
cervical plexus block anesthesia. Anesthesiology1994; 81: A1447
17 Cheng MA, Theard MA, Tempelhoff R. Anesthesia for carotid
endarterectomy:asurvey. J NeurosurgAnesthesiol 1997;9:21116
18 Connolly JE. Carotid endarterectomy in the awake patient. Am
J Surg1985; 150: 15965
19 Corson JD, Chang BB, Leopold PW, et al. Perioperative
hypertension in patients undergoing carotid endarterectomy:
shorter duration under regional block anesthesia. Circulation
1986; 74: 1114
20 Corson JD, Chang BB, Shah DM, Leather RP, DeLeo BM,
Karmody AM. The inuence of anesthetic choice on carotid
endarterectomy outcome. ArchSurg1987; 122: 80712
21 Counsell CE, Salinas R, Naylor R, Warlow CP. Routine or
selectivecarotidarteryshuntingduringcarotidendarterectomy
and the different methods of monitoring in selective shunting.
In: WarlowCP, VanGijnJ, SandercockP, CandeliseL, Langhorne
P, eds. Stroke Module of the Cochrane Database of Systematic
Reviews [updated 01 December 1997]. Available in the Cochrane
Library[databaseondiskandCDROM]; TheCochraneCollaboration.
Issue1. Oxford: Update Software, 1998 (updated quarterly)
22 Curran AJ, Smyth D, Sheehan SJ, Joyce W, Hayes DB, Walsh
MA. Recurrent laryngeal nerve dysfunction following carotid
endarterectomy. J RColl SurgEdinb1997; 42: 16870
23 Davies MJ, Mooney PH, Scott DA, Silbert BS, Cook RJ.
Neurologic changes during carotid endarterectomy under
cervical block predict a high risk of postoperative stroke.
Anesthesiology1993; 78: 82933
24 Davies MJ, Murrell GC, Cronin KD, Meads AC, Dawson A.
Carotid endarterectomy under cervical plexus blocka
prospectiveclinical audit. AnaesthIntensiveCare1990; 18: 21923
25 DaviesMJ, Silbert BS, Scott DA, CookRJ, MooneyPH. Supercial
and deep cervical plexus block for carotid artery surgery: A
prospective study of 1000 blocks. RegAnesth1997; 22: 4426
26 de-Letter JA, SieHT, Thomas BM, et al. Near-infraredreected
spectroscopy and electroencephalography during carotid
endarterectomyinsearchof anewshunt criterion. Neurol Res
1998; 20(Suppl. 1): S237
27 Donato AT, Hill SL. Carotid arterial surgery using local
anesthesia: a private practice retrospective study. Am J Surg
1992; 58: 44650
28 Dyker ML, Wolf PA, Barnett HJM, et al. Risk factors in stroke.
Stroke1984; 15: 110511
29 Eastcott HHG, Pickering GW, Robb CG. Reconstruction of
internal carotid artery in a patient with intermittent attacks of
hemiplegia. Lancet 1954; 2: 9946
30 Eger EI II. Thepharmacologyof isourane. Br J Anaesth1984; 56
(Suppl. 1): 7199S
31 Elliott BM, Collins GJ jr, Youkey JR, Donohue HJ jr, Salander
JM, Rich NM. Intraoperative local anesthetic injection of the
carotidsinus nerve. A prospective, randomizedstudy. AmJ Surg
1986; 152: 6959
Stoneham and Knighton
32 Ellis JE, Shah MN, Briller JE, Roizen MF, Aronson S, Feinstein
SB. A comparison of methods for the detection of myocardial
ischemia during noncardiac surgery: automated ST-segment
analysis systems, electrocardiography, and transesophageal
echocardiography. AnesthAnalg1992; 75: 76472
33 European Carotid Surgery Trialists Collaborative Group. MRC
EuropeanCarotidSurgeryTrial: interimresultsfor symptomatic
patients with severe (7099%) or with mild (029%) carotid
stenosis. Lancet 1991; 337: 123543
34 Finocchi C, Gandolfo C, Carissimi T, Del Sette M, Bertoglio C.
Roleof transcranial Doppler andstumppressureduringcarotid
endarterectomy. Stroke1997; 28: 244852
35 Fiorani P, SbarigiaE, SpezialeF, et al. General anaesthesiaversus
cervical block and perioperative complications in carotid artery
surgery. Eur J Vasc Endovasc Surg1997; 13: 3742
36 Forssell C, Takolander R, Bergqvist D, Johansson A, Persson
NH. Local versus general anaesthesia in carotid surgery. A
prospective, randomised study. Eur J Vasc Surg1989; 3: 5039
37 Friedman SG, Tortolani AJ. Reduced length of stay following
carotid endarterectomy under general anesthesia. Am J Surg
1995; 170: 2356
38 Garrioch MA, Fitch W. Anaesthesiafor carotid artery surgery.
Br J Anaesth1993; 71: 56979
39 Godin MS, Bell WH III, Schwedler M, Kerstein MD. Cost
effectiveness of regional anesthesia in carotid endarterectomy.
AmJ Surg1989; 55: 6569
40 Goldberg MJ. Complication of cervical plexus block or fugue
state?AnesthAnalg1995; 81: 11089
41 Gottlieb A, Satariano Hayden P, Schoenwald P, Ryckman J,
Piedmonte M. The effects of carotid sinus nerve blockade on
hemodynamic stability after carotid endarterectomy. J
Cardiothorac Vasc Anesth1997; 11: 6771
42 Halimi P, Guedj P. A simple method of assessing neurologic
motor power of patients duringcarotid endarterectomy. J Clin
Anesth1997; 9: 431
43 HoyleRM, Jenkins JM, Edwards WH sr, Edwards WH jr, Martin
RS, Mulherin JL jr. Case management in cerebral
revascularization. J Vasc Surg1994; 20: 396401
44 Hughes R, McGuire G, MontaneraW, WongD, Carmichael FJ.
Upper airway edema after carotid endarterectomy: the effect
of steroid administration. AnesthAnalg1997; 84: 4758
45 KainumaM,ShimadaY,MatsuuraM.Cervical epidural anaesthesia
in carotid artery surgery. Anaesthesia 1986; 41: 10203
46 Katz J. Atlas of Regional Anesthesia, 2nd Edn. Norwalk,
Connecticut: Appleton &Lange, 1994
47 KozodyR, ReadyLB, BarsaJE, MurphyTM. Doserequirements
of local anaesthesiato producegrandmal seizureduringstellate
ganglion block. CanAnaesthSoc J 1982; 29: 48991
48 Kraiss LW, KilbergL, Critch S, Johansen KJ. Short-stay carotid
endarterectomy is safe and cost-effective. AmJ Surg1995; 169:
51215
49 LamAM, Manninen PH, Ferguson GG, Nantau W. Monitoring
electrophysiologic function during carotid endarterectomy: a
comparison of somatosensory evoked potentials and
conventional electroencephalogram. Anesthesiology 1991; 75:
1521
50 LandesbergG, Erel J, Anner H, et al. Perioperative myocardial
ischemiain carotid endarterectomyunder cervical plexus block
andprophylacticnitroglycerininfusion. J CardiothoracVascAnesth
1993; 7: 25965
51 LawrencePF, AlvesJC, JichaD, Bhirangi K, DobrinPB. Incidence,
timing, and causes of cerebral ischemia during carotid
endarterectomy with regional anesthesia. J Vasc Surg1998; 27:
32934
918
52 LewisDR, IrvineCD, ColeSE, McGrathC, BairdRN, Lamont PM.
Computerisedaudit of carotidendarterectomy: audit loopholes
closed?AnnRColl SurgEngl 1997; 79: 4559
53 Loreggian B, RuffaD, Greco P, et al. Cervical plexus block with
ropivacaine for carotid endarterectomy. Br J Anaesth 1998; 80
(Suppl. 1): A374
54 MariettaDR, Lunn JK, RubyEI, Hill GE. Cardiovascular stability
duringcarotid endarterectomy: endotracheal intubation versus
laryngeal mask airway. J ClinAnesth1998; 10: 547
55 MastersRD, CastresanaEJ, CastresanaMR. Supercial anddeep
cervical plexus block: technical considerations. AmAssoc Nurse
AnesthJ 1995; 63: 23543
56 Mazer CD. Con: Combined coronary and vascular surgery is
not better than separate procedures. J Cardiothorac Vasc Anesth
1998; 12: 22830
57 McClearyAJ, DeardenNM, DicksonDH, WatsonA, GoughMJ.
The differing effects of regional and general anaesthesia on
cerebral metabolismduringcarotid endarterectomy. Eur J Vasc
Endovasc Surg1996; 12: 17381
58 McKay RD, Sundt TM, Michenfelder JD, et al. Internal carotid
artery stump pressure and cerebral blood ow during carotid
endarterectomy: modication by halothane, enurane, and
innovar. Anesthesiology1976; 45: 3909
59 Mehta Y, Juneja R. Regional analgesia for carotid artery
endarterectomy by Winnies single-injection technique using a
nerve detector. J Cardiothorac Vasc Anesth1992; 6: 7723
60 Michenfelder JD, Sundt TM, FodeN, SharbroughFW. Isourane
when compared to enurane and halothane decreases the
frequency of cerebral ischemia duringcarotid endarterectomy.
Anesthesiology1987; 67: 33640
61 Moore DC. Regional Block: a Handbook for Use in the Clinical
Practice of Medicine and Surgery, 4th Edn. Springeld, Illinois:
Charles C Thomas, 1978
62 MooreDC, MulroyMF, ThompsonGE. Peripheral nervedamage
and regional anaesthesia. Br J Anaesth1994; 73: 4356
63 Morawetz RB, Zeiger HE, McDowell HA jr, et al. Correlation
of cerebral blood ow and EEG during carotid occlusion for
endarterectomy (without shunting) and neurologic outcome.
Surgery1984; 96: 1849
64 MRC European Carotid Surgery Trial participants. Randomised
trial of endarterectomy for recently symptomatic carotid
stenosis: nal results of the MRC European Carotid Surgery
Trial (ECST). Lancet 1998; 351: 137987
65 Munro FJ, Makin AP, Reid J. Airway problems after carotid
endarterectomy. Br J Anaesth1996; 76: 1569
66 MurieJA, JohnTG, Morris PJ. CarotidendarterectomyinGreat
Britain and Ireland: practice between 1984 and 1992. Br J Surg
1994; 81: 82731
67 Murie JA, Morris PJ. Carotid endarterectomy in Great Britain
and Ireland. Br J Surg1986; 73: 86770
68 Murie JA, Morris PJ. Carotid endarterectomy in Great Britain
and Ireland: trends and current practice. Br J Surg 1991; 78:
397400
69 Muskett A, McGreevy J, Miller M. Detailed comparison of
regional and general anesthesiafor carotid endarterectomy. Am
J Surg1986; 152: 6914
70 NorrisD, KlahsenA, MilneB. Delayedbilateral spinal anaesthesia
followinginterscalenebrachial plexus block. CanJ Anaesth1996;
43: 3035
71 North American Symptomatic Carotid Endarterectomy Trial
Collaborators. Benecial effect of carotid endarterectomy in
symptomatic patients with high-grade carotid stenosis. N Engl J
Med1991; 325: 44553
Regional anaesthesia for CEA
72 Palmer MA. Comparison of regional and general anesthesiafor
carotid endarterectomy. AmJ Surg1989; 157: 32930
73 Panayiotopoulos YP, Padayachee S, Colchester AC, Taylor PR.
Thechangingindications for carotidendarterectomyintheUK.
Int J ClinPract 1997; 51: 3757
74 Paul SD, Eagle KA. A stepwise strategy for coronary risk
assessment for noncardiac surgery. Med Clin N Am1995; 79:
124161
75 Pluskwa F, Bonnet F, Abhay K, et al. Blood pressure proles
during carotid endarterectomy. Comparing unitrazepam/
fentanyl/nitrous oxide with epidural anaesthesia. Ann Fr Anesth
Reanim1989; 8: 2632
76 PluskwaF, Bonnet F, Touboul C, SzekelyB, RoujasF, Becquemin
JP. [Carotid endarterectomyunder cervical epidural anesthesia.
Analysis of neurologic manifestations]. Ann Fr Anesth Reanim
1988; 7: 3641
77 ProughDS, Scuderi PE, McWhorter JM, Balestrieri FJ, DavisCH,
StullkenEH. Hemodynamicstatusfollowingregional andgeneral
anesthesia for carotid endarterectomy. J Neurosurg Anesthesiol
1989; 1: 3540
78 Pulsinelli WA, LevyDE, Sigsbee B, et al. Increased damage after
ischemic stroke in patients with hyperglycemiawith or without
established diabetes mellitus. Factors associated with
perioperative complications during carotid endarterectomy.
AnesthAnalg1982; 61: 6317
79 Rigdon EE, Monajjem N, Rhodes RS. Criteria for selective
utilization of the intensive care unit following carotid
endarterectomy. AnnVasc Surg1997; 11: 207
80 RockmanCB, Riles TS, Lamparello PJ, et al. Anesthetic methods
in reoperative carotid surgery. AnnVasc Surg1998; 12: 1637
81 Salvian AJ, Taylor DC, HsiangYN, et al. Selective shuntingwith
EEG monitoring is safer than routine shunting for carotid
endarterectomy. Cardiovasc Surg1997; 5: 4815
82 Scammell SJ. Case report: inadvertent epidural anaesthesiaas a
complication of interscalene brachial plexus block. Anaesth
IntensiveCare1979; 7: 567
83 Schauber MD, Fontenelle LJ, Solomon JW, Hanson TL. Cranial/
cervical nerve dysfunction after carotid endarterectomy. J Vasc
Surg1997; 25: 4817
84 Schroeder LE, Horlocker TT, Schroeder DR. The efcacy of
axillary block for surgical procedures about the elbow. Anesth
Analg1996; 83: 74751
85 Selander D, EdshageS, Wolff T. Paresthesiaeor noparesthesiae?
Nervelesions after axillaryblocks. ActaAnaesthesiol Scand1979;
23: 2733
86 ShahDM, DarlingRC, ChangBB, Bock DE, PatyPS, Leather RP.
Carotid endarterectomy in awake patients: its safety,
acceptability, and outcome. J Vasc Surg1994; 19: 101519
87 SilvaL, CostaE, BrimacombeJR. Thelaryngeal mask for carotid
endarterectomy. J Cardiothorac Vasc Anesth1996; 10: 9723
88 SmithJL, Evans DH, Gaunt ME, LondonNJ, Bell PR, Naylor AR.
Experience with transcranial Doppler monitoring reduces the
incidence of particulate embolization during carotid
endarterectomy. Br J Surg1998; 85: 569
89 Spencer MP, ThomasGI, MochringMA. Relationbetweenmiddle
919
cerebral artery blood ow velocity and stump pressure during
carotid endarterectomy. Stroke1992; 23: 143945
90 Spielberger L, Turndorf H, Culliford A, Imparato A. Hand-held
toy squeaker during carotid endarterectomy in the awake
patient. ArchSurg1979; 114: 1034
91 Stoneham MD, Wakeeld TW. Acute respiratory distress
followingdeep cervical plexus block. J Cardiothorac Vasc Anesth
1998; 12: 1978
92 Stoneham MD, Doyle AR, Knighton JD, Dorje P, Stanley JC.
Prospective, randomised comparison of deep or supercial
cervical plexus block for carotid endarterectomy surgery.
Anesthesiology1998; 89: 90712
93 StonehamMD, DoyleAR, KnightonJD, DorjeP, StanleyJC. Deep
or supercial cervical plexus block for carotid endarterectomy.
AnesthAnalg1998; 86: S106
94 Sundt TM, Houser OW, Sharbrough FW. Carotid
endarterectomy: Results, complications and monitoring
techniques. AdvNeurol 1977; 16: 97119
95 Szocik JF, Kellogg W, Wakeeld TW. Temporary facial nerve
palsy during carotid endarterectomy under local anesthesia.
AnesthAnalg1995; 81: 11067
96 Takolander R, Bergqvist D, Hulthen UL, Johansson A, Katzman
PL. Carotid artery surgery. Local versus general anaesthesiaas
related to sympathetic activity and cardiovascular effects. Eur J
Vasc Surg1990; 4: 26570
97 Tangkanakul C, Counsell CE, WarlowCP. Local versus general
anaesthesia in carotid endarterectomy: a systematic review of
the evidence. Eur J Vasc Endovasc Surg1997; 13: 4919
98 Tissot S, Frering B, Gagnieu M, Vallon J, Motin J. Plasma
concentrationsof lidocaineandbupivacaineafter cervical plexus
block for carotid surgery. AnesthAnalg1997; 84: 13779
99 Trop D. Con: carotid endarterectomy: general is safer than
regional anesthesia. J Cardiothorac Anesth1987; 1: 4838
100 Wedel D. Nerve Blocks. In: Miller RD, ed. Anesthesia, 4th Edn.
NewYork: Churchill-Livingstone, 1994; 153564
101 Wilke HJ, Ellis JE, McKinsey JF. Carotid endarterectomy:
Perioperative and anesthetic considerations. J Cardiothorac Vasc
Anesth1996; 10: 92849
102 Winnie AP, RamamurthyS, Durrani Z, Radonjic R. Interscalene
cervical plexus block: a single-injection technic. Anesth Analg
1975; 54: 3705
103 WongJH, FindlayJM, SuarezAlmazor ME. Regional performance
of carotidendarterectomy. Appropriateness, outcomes, andrisk
factors for complications. Stroke1997; 28: 8918
104 Wong JH, Findlay JM, Suarez Almazor ME. Hemodynamic
instability after carotid endarterectomy: risk factors and
associations with operative complications. Neurosurgery 1997;
41: 3541
105 YoungbergJA. Pro: regional anesthesia is preferable to general
anesthesiafor carotidarterysurgery. J CardiothoracAnesth1987;
1: 47982
106 Zannetti S, Parente B, De Rango P, et al. Role of surgical
techniques and operative ndings in cranial and cervical nerve
injuries duringcarotidendarterectomy. Eur J VascEndovascSurg
1998; 15: 52831
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Alat Kesehatan BaruDocument6 pagesAlat Kesehatan BaruJusty GuavaNo ratings yet
- Lapsus: (Report Subtitle)Document3 pagesLapsus: (Report Subtitle)Justy GuavaNo ratings yet
- J Appl Physiol 2007 Supinski 1649 57Document10 pagesJ Appl Physiol 2007 Supinski 1649 57Justy GuavaNo ratings yet
- 1824 7288 39 18Document8 pages1824 7288 39 18Justy GuavaNo ratings yet
- Vidhyaa Kumari Et Al 2012Document12 pagesVidhyaa Kumari Et Al 2012Justy GuavaNo ratings yet
- FEES1Document6 pagesFEES1Justy GuavaNo ratings yet
- 941057Document6 pages941057Justy GuavaNo ratings yet
- Absen IshipDocument2 pagesAbsen IshipJusty GuavaNo ratings yet
- Leaflet KatarakDocument5 pagesLeaflet KatarakJusty GuavaNo ratings yet
- 1824 7288 39 18Document8 pages1824 7288 39 18Justy GuavaNo ratings yet
- Spontaneous Closure of Macular Holes Secondary To Posterior Uveitis: Case Series and A Literature ReviewDocument7 pagesSpontaneous Closure of Macular Holes Secondary To Posterior Uveitis: Case Series and A Literature ReviewJusty GuavaNo ratings yet
- A Review On The Management of Acute Gastroenteritis in ChildrenDocument9 pagesA Review On The Management of Acute Gastroenteritis in ChildrenAnonymous 1EQutBNo ratings yet
- Daftar PustakaDocument1 pageDaftar PustakaJusty GuavaNo ratings yet
- Airway Management PerioperativeDocument9 pagesAirway Management PerioperativeSyarifuddin Abdul JabbarNo ratings yet
- FEES4Document115 pagesFEES4Justy Guava100% (1)
- FEES6Document36 pagesFEES6Justy GuavaNo ratings yet
- Rome III Diagnostic Criteria FGIDsDocument14 pagesRome III Diagnostic Criteria FGIDsPutu Reza Sandhya PratamaNo ratings yet
- StrokeDocument19 pagesStrokesridhar100% (4)
- FEES2Document6 pagesFEES2Justy GuavaNo ratings yet
- FEES1Document6 pagesFEES1Justy GuavaNo ratings yet
- JAnaesthClinPharmacol3013-2229275 061132Document4 pagesJAnaesthClinPharmacol3013-2229275 061132Justy GuavaNo ratings yet
- IndianJAnaesth5815-3581899 095658Document2 pagesIndianJAnaesth5815-3581899 095658Justy GuavaNo ratings yet
- 166 172Document7 pages166 172Justy GuavaNo ratings yet
- Stoneham - Prospective Randomized ComparisonDocument8 pagesStoneham - Prospective Randomized ComparisonJusty GuavaNo ratings yet
- Br. J. Anaesth. 2000 Marhofer 341 5Document5 pagesBr. J. Anaesth. 2000 Marhofer 341 5Justy GuavaNo ratings yet
- Bab IiDocument1 pageBab IiJusty GuavaNo ratings yet
- JAnaesthClinPharmacol30110-2230963 061149Document9 pagesJAnaesthClinPharmacol30110-2230963 061149Justy GuavaNo ratings yet
- 25 29Document5 pages25 29Justy GuavaNo ratings yet
- 04 Caudal BlockDocument3 pages04 Caudal BlockJusty GuavaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- (Razavi) Design of Analog Cmos Integrated CircuitsDocument21 pages(Razavi) Design of Analog Cmos Integrated CircuitsNiveditha Nivi100% (1)
- Lyceum of The Philippines University Cavite Potential of Peanut Hulls As An Alternative Material On Making Biodegradable PlasticDocument13 pagesLyceum of The Philippines University Cavite Potential of Peanut Hulls As An Alternative Material On Making Biodegradable PlasticJayr Mercado0% (1)
- Nickel-Metal Hydride Battery Safety Data SheetDocument8 pagesNickel-Metal Hydride Battery Safety Data SheetYeong WheeNo ratings yet
- Sibuyan Island ResiliencyDocument12 pagesSibuyan Island ResiliencyEndangeredSpeciesNo ratings yet
- GIS AccidentsDocument5 pagesGIS Accidentsali110011No ratings yet
- Math 202: Di Fferential Equations: Course DescriptionDocument2 pagesMath 202: Di Fferential Equations: Course DescriptionNyannue FlomoNo ratings yet
- 7890 Parts-Guide APDocument4 pages7890 Parts-Guide APZia HaqNo ratings yet
- Usjr Temfacil Balance of Work Schedule Aug 25, 2022Document5 pagesUsjr Temfacil Balance of Work Schedule Aug 25, 2022Maribeth PalumarNo ratings yet
- Pitch Manual SpecializedDocument20 pagesPitch Manual SpecializedRoberto Gomez100% (1)
- Apollo TyresDocument78 pagesApollo TyresADITYA33% (3)
- Coleman Product PageDocument10 pagesColeman Product Pagecarlozz_96No ratings yet
- Virchow TriadDocument6 pagesVirchow Triadarif 2006No ratings yet
- O2 Orthodontic Lab Catalog PDFDocument20 pagesO2 Orthodontic Lab Catalog PDFplayer osamaNo ratings yet
- STS Chapter 1 ReviewerDocument4 pagesSTS Chapter 1 ReviewerEunice AdagioNo ratings yet
- Smart Note Taker Saves Time With Air WritingDocument17 pagesSmart Note Taker Saves Time With Air WritingNagarjuna LokkuNo ratings yet
- 中美两国药典药品分析方法和方法验证Document72 pages中美两国药典药品分析方法和方法验证JasonNo ratings yet
- 1.2 - Sewing Machine and Special AttachmentsDocument3 pages1.2 - Sewing Machine and Special Attachmentsmaya_muth0% (1)
- Diia Specification: Dali Part 252 - Energy ReportingDocument15 pagesDiia Specification: Dali Part 252 - Energy Reportingtufta tuftaNo ratings yet
- ADDRESSABLE 51.HI 60854 G Contoller GuideDocument76 pagesADDRESSABLE 51.HI 60854 G Contoller Guidemohinfo88No ratings yet
- Certificate Testing ResultsDocument1 pageCertificate Testing ResultsNisarg PandyaNo ratings yet
- Fake News Poems by Martin Ott Book PreviewDocument21 pagesFake News Poems by Martin Ott Book PreviewBlazeVOX [books]No ratings yet
- Progibb LV Plus PGR - Low Voc FormulationDocument2 pagesProgibb LV Plus PGR - Low Voc FormulationDodik Novie PurwantoNo ratings yet
- Chapter 16 - Energy Transfers: I) Answer The FollowingDocument3 pagesChapter 16 - Energy Transfers: I) Answer The FollowingPauline Kezia P Gr 6 B1No ratings yet
- Letter of MotivationDocument4 pagesLetter of Motivationjawad khalidNo ratings yet
- Front Wheel Steering System With Movable Hedlights Ijariie5360Document6 pagesFront Wheel Steering System With Movable Hedlights Ijariie5360Ifra KhanNo ratings yet
- 9600 DocumentDocument174 pages9600 Documentthom38% (13)
- ROMUS 2012 Flooring CatalogueDocument20 pagesROMUS 2012 Flooring CatalogueDan George IIINo ratings yet
- Fundermax Exterior Technic 2011gb WebDocument88 pagesFundermax Exterior Technic 2011gb WebarchpavlovicNo ratings yet
- Datasheet PDFDocument6 pagesDatasheet PDFAhmed ElShoraNo ratings yet
- Detection and Attribution Methodologies Overview: Appendix CDocument9 pagesDetection and Attribution Methodologies Overview: Appendix CDinesh GaikwadNo ratings yet