Professional Documents
Culture Documents
Degenerative Diseases of The MS System
Uploaded by
Nikko DioOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Degenerative Diseases of The MS System
Uploaded by
Nikko DioCopyright:
Available Formats
Degenerative Diseases of the MS System Arthritis (joint inflammation) is a common, often crippling condition.
Assessment findings include joint pain, swelling, tenderness, heat, and difficult movement. Arthritis affects people regardless of age, race, socioeconomic group, or sex (although some kinds of arthritis are more common in women) Joint diseases have occurred for millions of years. Evidence of osteoarthritis has been identified in skeletal remains of dinosaurs living 100 years ago and in the skeletons of prehistoric people and Egyptian mummies. The cause of arthritis is unknown and has no cure it is often possible, however, to prevent or correct its crippling effects. Medication may be used and surgical techniques can sometimes restore function and relieve pain. Physical therapy is valuable in relieving pain and preventing deformity. There are acute and chronic forms of arthritis. There are two basic arthritic pathologic processes: 1. Inflammation -exudative, proliferative, combination 2. Degenerative Changes INFECTIOUS Rheumatoid Arthritis is the most virulent form of arthritis, it is a chronic, systemic disease with inflammatory connective tissue changes. Most often, small, peripheral joints (fingers and wrist joints) Bilateral affectation Women are affected two or three times more often than are men. While it occurs at any age, it is most common in people between ages 20 and 40 Etiology is unknown. Some speculate that the disease is caused by: a. An undefined virus or some other microorganism (Mycoplasma)
b. Metabolic aberrations c. Immunologic mechanisms (B-lymphocytes) Pathology of RA. If, unarrested, pathologic joint changes in RA pass through four stages 1. 2. 3. 4. Synovitis Pannus formation Fibrous ankylosis Bony ankylosis
Assessment Findings Early in the disease each exacerbation tends to be more stubborn than the preceding one. Occasionally, permanent remission occurs, but this is not usual. RA is generally progressive and deformity-producing. Onset of Rheumatoid Arthritis: Usually insidious Associated with physical and/or emotional stress
Synovial Joints: (Mainly hands and feet) Warm, tender, red, painful Guarded movement Limited ROM Limited strength Stiffness and pain worst in the morning
X-ray may show: Feet: Stiff, painful Broadened forefoot Depressed metatarsal heads Cockup toe deformity Soft tissue swelling Osteoporosis Cartilage erosion Narrowed joint space Bony cysts
Eyes: (In advanced disease) Episcleritis Keratoconjunctivitis
Hands: Red palms Enlarged dorsal veins Ulnar drift Joint pain and stiffness Weak grip Inability to make tight fist
Severe Wrist subluxation Finger swan neck Finger Boutonniere Z-shaped thumb
Systemic Effects Slight fever Malaise, weakness Weight loss Numb, tingling hands and feet Enlarged lymph nodes Enlarged spleen Depression Anorexia Fatigue by early afternoon
Laboratory Findings Serum protein factors (rheumathoid factors) ESR C-reactive protein WBC (slight) Leukopenia Abnormal synovial fluids
Subcutaneous nodules characteristic lesions of RA Pain is variable in intensity and tends to be most persistent upon use of involved joints.
Stiffness is often the most constant problem. Osteoarthritis (Degenerative Joint Disease/ Hyperthropic Arthritis) A non-inflammatory degenerative disease Unilateral affectation Most common form of arthritis Unknown cause but is associated with congenital abnormalities, genetic predisposition, aging, trauma, and obesity Weight bearing joints are mostly affected (Hip, Knee, Cervical and Lumbosacral joints) More prevalent in men before age 45. After 55, it is more common in women. Primary OA unknown cause Secondary OA caused by other conditions Pathology of OA Cartilage matrix is worn away and the bones rub together, causing painful, swollen joints Cartilage erosion follows. A proliferative response at joint margins then produces outgrowths of cartilage and bone called osteophytes or spurs Characteristic hypertrophic spurs swellings called Heberdens nodes and Bouchards node in terminal interphalangeal finger joints. Unlike RA, OA is not a systematic disease OA is often a wear-and-tear process. Mostly overweight. Assessment Findings It often produces no symptoms and intervention is not required. Symptoms usually develop gradually and progress slowly. Aching pain is the common symptom of OA. Other assessment findings include limited motion or contractures, and muscle spasm. Unlike RA, the pain with OA is more pronounced after exercise.
Night pain and morning stiffness may also occur. Flexion contraction of the hip and loss of ability to extend the knee may be disabling. Pain at rest may be caused by muscle spasm. Symptom severity and the degree of degenerative joint changes are often not correlated. Therefore, a person with minor degenerative changes may be quite uncomfortable, while a person with advanced changes may have few or no symptoms. Crepitus are often detectable X-ray abnormalities are often apparent, but laboratory findings indicative of inflammation are absent Intervention The main goals are: Preventing joint deformity Preserving joint function Reducing inflammation and pain
Rest Physical and emotional rest are important. Complete bed rest is indicated for a limited time for its anti-inflammatory effect. Positioned to prevent deformities The patient should lie flat on the back with affected joints in position of extension up to 10 hours a day while on bed rest. A small pillow may be placed under the ankles to straighten the knees. Position arms with palms upward by placing small pillows under elbows or wrists to maintain extension. Use sandbags and trochanter rolls as necessary to maintain proper body alignment. Splints may be used to rest inflamed joints. Splints are removed periodically and the joints exercised to prevent fibrous ankylosis
Physical therapy To strengthen weakened muscles and improve function. Isometric exercises are important in maintaining muscle function even when splints are applied. Exercise must be done within the persons pain tolerance Never massage acutely inflamed joints, because it my aggregate the inflammation
Teaching proper posture Heat and cold application to relieve aches, swelling and stiffness. Serves as an anesthetic effect
Medication Aspirin Analgesic and anti-inflammatory Nursing considerations: 1. Take with food 2. Watch signs of bleeding Other NSAIDs Adrenocorticosteroids
Surgical treatment Tendon transfers A functioning tendon is shifted from its original attachment to a new one to restore the action that has been lost. Osteotomy Excising or cutting through bone Synovectomy Removal of synovial Arthodesis Surgical immobilization or fusion of joint Arthroplasty
Surgical formation or reformation of a joint with or without replacement of joint parts with prostheses Joint replacement Silicone implants are used to replace joints as small as those of fingers Total Hip Replacement Total Knee Replacement
Gouty Arthritis Is a familial disorder of purine metabolism resulting in abnormal amounts of urates in the body. Purines are products from the digestion of certain proteins. Inability to properly metabolize purines produces an excessive accumulation of uric acid in the blood plasma. As a result, urate crystals may be deposited throughout the body. These deposits initiate local irritation and an inflammatory response. Acute attacks of gouty arthritis may accompany other disorders (hematopoietic disorders such as polycythemia or leukemia). These attacks are called secondary gout Arthritis is the main clinical problem with gout. Early in the course of illness, a recurring, acute arthritis occurs that is usually monoarticular. Later a chronic, deforming arthritis develops. About 95% of people with gout are men over 30. If gout develops in women, it is usually after the menopause. Gout is characterized by acute periodic episodes of joint pain, swelling, and inflammation. Foot joints and knee are most often affected On histologic examination it is characterized by the formation of tophi in soft tissues or monosodium urate crystals in synovium or synovial fluids The attack is usually sudden, occurring at night. Crushing and often pulsating pain increases until there is no relief from any body position. It is most often involves the metatarsophalangeal joint of the great toe. The involved joint is usually intensely painful, swollen, and extremely tender Xray shows punched out areas in the bone
3 stages 1. Asymptomatic Hyperuricemia 2. Acute gouty arthritis 3. Tophaceous gout Intervention Colchicine To reduce frequency of acute attacks Probenecid Block the tubular reabsorption of filtered urate in the kidneys Allopurinol Inhibits uric acid formation Dietary management Surgical removal of large tophi
Osteoporosis Is a metabolic bone disorder in which bone mass is decreased. Bone become borous and brittle Bone resorption occurs faster than bone formation Most often affects women between ages 50 and 70 Osteoporosis may occur: Primary lost of estrogen Secondary Cushing Long term large doses of corticosteroids Prolonged immobilization Calcium deficiency
It can be detected by x-ray and nuclear medicine scans Symptoms begin with pain in weight bearing vertebrae. Bodys supporting structure is weak, therefore risk for spontaneous fractures Intervention Symptomatic Goals are to control pain and prevent fractures.
Gentle exercise is important. Estrogen may decrease bone resorption and Flouride may promote bone formation. Calcium and Vit. D may be taken either in the diet or as a supplement
Osteomalacia Is a disorder in which adult bone becomes spongy because of disturbed calcium and phosphate metabolism resulting from: Lack of dietary intake of vitamin D The bodys failure to absorb or use vitamin D Lack of exposure to ultraviolet rays Osteomalacia may be identified by reduced calcium and phosphorus levels, rachitic bone deformities, bone pain and tenderness, x-ray changes. Biopsy may help establish diagnosis. A smaller disorder occurs in children like rickets Intervention Vitamin D Adequate intakes of calcium Calcium salts and phosphate supplements may be prescribed
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Personal Data SheetDocument4 pagesPersonal Data SheetLeonil Estaño100% (7)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- DR Sinatra HEART, HEALTH & NUTRITIONDocument8 pagesDR Sinatra HEART, HEALTH & NUTRITIONalekad65100% (2)
- Nutrilite Diet Supplementsin FinalDocument2 pagesNutrilite Diet Supplementsin FinalAnisur RehmanNo ratings yet
- The Cambridge World History of Human DiseaseDocument1,203 pagesThe Cambridge World History of Human DiseasePaulo Henrique Neto Pais100% (1)
- Purines and Nitrogenous BasesDocument4 pagesPurines and Nitrogenous BasesIan FranciaNo ratings yet
- Moringa Oleifera - Cancer, Lupus, Arthritis, Gout, Diabetes PDFDocument5 pagesMoringa Oleifera - Cancer, Lupus, Arthritis, Gout, Diabetes PDFzultrsb689100% (1)
- Rheumatology Best of Five DONEDocument28 pagesRheumatology Best of Five DONEAlo'a NajjarNo ratings yet
- Therapeutic DietsDocument8 pagesTherapeutic DietsmArLoN91% (11)
- Gout and Its Permanent Cure With Homeopathic Medicine - Bashir Mahmud ElliasDocument6 pagesGout and Its Permanent Cure With Homeopathic Medicine - Bashir Mahmud ElliasBashir Mahmud Ellias100% (2)
- Dr. Rabia 1700 Plab Material McqsDocument1,092 pagesDr. Rabia 1700 Plab Material McqsMuhammad Amin100% (9)
- Presentation - Uric AcidDocument31 pagesPresentation - Uric AcidTc Khoon100% (1)
- Case StudyDocument17 pagesCase StudyNikko DioNo ratings yet
- Medicine Alaa Notes (All Files Merged) - Best Pro Choice-.Pdf-1Document120 pagesMedicine Alaa Notes (All Files Merged) - Best Pro Choice-.Pdf-1maimoona suleman100% (6)
- Medsurg ReviseDocument1 pageMedsurg ReviseNikko DioNo ratings yet
- Suturing TechniquesDocument1 pageSuturing TechniquesNikko DioNo ratings yet
- DioDocument4 pagesDioNikko DioNo ratings yet
- Drug ReviseDocument6 pagesDrug ReviseNikko DioNo ratings yet
- Figures of SpeechDocument4 pagesFigures of SpeechNikko DioNo ratings yet
- C Teaching1Document3 pagesC Teaching1Nikko DioNo ratings yet
- Drug ReviseDocument6 pagesDrug ReviseNikko DioNo ratings yet
- Racial Disparity in Emergency Department Triage: BackgroundDocument1 pageRacial Disparity in Emergency Department Triage: BackgroundNikko DioNo ratings yet
- Instruments El MataryDocument173 pagesInstruments El MataryNikko DioNo ratings yet
- Try Lang PoDocument1 pageTry Lang PoNikko DioNo ratings yet
- TriadsDocument1 pageTriadsNikko DioNo ratings yet
- Management of Acute Gouty Arthritis With A Polyherbal Unani FormulationDocument148 pagesManagement of Acute Gouty Arthritis With A Polyherbal Unani Formulationadilnnj100% (1)
- Chapter 1Document57 pagesChapter 1Angni, AsnoraNo ratings yet
- Gouty Arthritis Health TeachingDocument14 pagesGouty Arthritis Health TeachingnesjynNo ratings yet
- Gensco Pharma's Transdermal Colchicine, ColciGel®, For Treatment of Acute Gout Flares With Negligible Systemic Absorption Improving Tolerability With Less Side EffectsDocument3 pagesGensco Pharma's Transdermal Colchicine, ColciGel®, For Treatment of Acute Gout Flares With Negligible Systemic Absorption Improving Tolerability With Less Side EffectsPR.comNo ratings yet
- Gout and Diet CokeDocument4 pagesGout and Diet CokeJohnNo ratings yet
- Asam UratDocument38 pagesAsam UratRai Fit TimikaNo ratings yet
- Human Anatomy and Physiology 9Th Edition Marieb Test Bank Full Chapter PDFDocument37 pagesHuman Anatomy and Physiology 9Th Edition Marieb Test Bank Full Chapter PDFAlexandraPerrymzyd100% (9)
- A Thesis On Homoeopathic Management of GoutDocument3 pagesA Thesis On Homoeopathic Management of GouthirenNo ratings yet
- RematikDocument66 pagesRematikYolla LitaNo ratings yet
- L-16 Purine Biochemistry and Uric Acid Metabolism - XMLDocument18 pagesL-16 Purine Biochemistry and Uric Acid Metabolism - XMLJulia HangaNo ratings yet
- Blood Fluid Examination StrasingerDocument4 pagesBlood Fluid Examination StrasingerChristin SchlittNo ratings yet
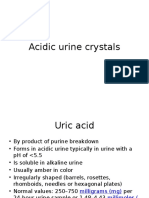
- Acidic Urine CrystalsDocument11 pagesAcidic Urine CrystalsAdriana GarciaNo ratings yet
- Pharmacology: Drug Therapy of GoutDocument81 pagesPharmacology: Drug Therapy of GoutYousef JafarNo ratings yet
- Nutrients: Uric Acid and Plant-Based NutritionDocument15 pagesNutrients: Uric Acid and Plant-Based Nutrition劉靖騰No ratings yet
- CC Junsay Nicole Xyza T. Learning Interaction FormDocument10 pagesCC Junsay Nicole Xyza T. Learning Interaction FormNicole Xyza JunsayNo ratings yet
- Chapter IDocument11 pagesChapter IJay Ar100% (1)
- Human Anatomy and Physiology 9th Edition Marieb Test BankDocument16 pagesHuman Anatomy and Physiology 9th Edition Marieb Test Bankjillhenrysetcjnzrfp100% (28)
- ArthritisDocument69 pagesArthritisKavya sriNo ratings yet
- 99 High Yield Internal Medicine Facts Part 2Document9 pages99 High Yield Internal Medicine Facts Part 2DaanishNo ratings yet
- Mnemonics On Pathology and MicrobiologyDocument105 pagesMnemonics On Pathology and MicrobiologyAyerhs Hahs67% (3)