Professional Documents
Culture Documents
Malaria Epidemic in Sub-Saharan Africa
Uploaded by
AnastasiafynnOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Malaria Epidemic in Sub-Saharan Africa
Uploaded by
AnastasiafynnCopyright:
Available Formats
05/11/53
Epidemiology
Malaria kills over one million children
Malaria
Presented by Daniel Ansong
Dept of Paediatrics
90 90% of malaria death occurs in sub 3000 death per day Prevalence in Ghana?
Saharan Africa
every year
Cerebral malaria BCS <=2
Site %CM Gabon Ghana Kenya Malawi Gambia % Mortality CM C M NON-CM CM P-value
Severe anaemia: Hb<5g/dl or PCV < 15 15%
% Mortality Site % SA SA SA NON-SA SA P-VALUE
Total
8.7 14.1 14 5.4 5.1 6.2 8.4
20 2 0.5 18.8 18 16.7 16 21.7 21 31.0 31 19.6 19
1.9 3.2 3.0 1.5 7.2 2.7
<0.001 <0.001 <0.001 <0.001 <0.001 <0.001
Gabon Ghana Kenya Malawi Gambia Total
25.5 25.8 15.8 8.9 27.0 19.1
5.1 6.1 3.7 7.1 12.4 5.9
2.9 5.1 3.8 2.1 7.2 3.7
0.03 0.29 0.9 <0.001 0.07 <0.001
Hyperlactemia lactate > 5mmol/l
Site % HL % Mortality HL HL Non-HL HL P-value
Hypoglycaemia: Blood glucose < 2.2 mmol/l
Si t e Gabon Ghana Kenya Malawi Gambia Total % HG 6.6 5.0 3.8 2.1 6.3 6.9 % Mortality HG H G Non-HG HG 11.6 2.9 27.5 4.2 21.3 3.1 15.8 2.3 10.3 5.8 15.9 3.2 P-value <0.001 <0.001 <0.001 <0.001 0.09 <0.001
Gabon Ghana Kenya Malawi Gambia Total
43.3 23.6 13.3 32.4 38.6 27.6
6.2 13.2 11.1 5.4 15.8 8.8
1.5 2.9 2.7 1.2 4.1 2.3
<0.001 <0.001 <0.001 <0.001 <0.001 <0.001
05/11/53
Diagnosis
Laboratory Clinical
Laboratory Diagnosis
Malaria Diagnostic Procedure
Thin and Thick film using Giemsa Staining Buffy coat preparation of concentrate mps Use of Rapid Immunodiagnostic strip test
Malaria positivity 1-10 parasites per 100 high power fields (HPF) + 11-100 Parasites per 100 HPF 11 ++ ++ 1-10 parasites in every HPF +++ More than 10 parasites per HPF ++++
Presentation
Mild Severe
Pathophysiology of Severe Malaraia
Role of RBC (Sequestration of RBC in deep
vascular beds of vital organs. Role of Cytokines-TNF, Interleukin, Nitrous oxide Role of Lactic Acid Role of Platelets and other cells Role of the Spleen, Liver and other organs
05/11/53
Anaemia
Striking contrast between the palm of of a Kenyan child with anaemia, and that of his mother. Severe anaemia is of is the leading cause of of death in in children with m a l a ri a .
Hypothesis for severe anaemia
The sludging hypothesis (High proportion The permeability hypothesis Mechanical hypothesis Immunological hypothesis
of parasitized RBC in organs)
Severe malaria
Clinical signs suggestive of severe malaria
Haematological indices Hb <5.0g/dl PCV <15 15 Biochemical indices Blood Lactate level >5 mmol/l Blood Glucose of < 2.2 mmol/l Abnormal liver function Abnormal Renal function
05/11/53
Severe malaria
Clinical indices Prostration Inability to sit without support Inability to suck Inability to stand and walk without support Respiratory distress Haemoglobinuria Convulsion Blantyre coma score of <2
Outline classification of severe malaria in children Group 1:
Children at immediately increase risk of dying who require parenteral antimalarial drugs and support therapy
Prostrated children Respiratory distress (acidotic breathing)
Group 2: Group 3:
Children with a haemoglobin level <5g/dl or a PCV <15 15% Children with 2 or more convulsions within a 24 hours period Children who require parentral treatment because of persistent vomiting
but who lack any specific clinical or laboratory features or group 1 or 2.
Blantyre coma scale A coma scale for Children
Best motor response
Localized painful stimulus With-drawl limb from pain Non-specific or absent response Appropriate cry Moan or inappropriate cry None Direction (eg follows mothers face) Not directed 2 1 0 2 1 0 1 0
Severe malaria
Clinical indices
Prostration Impaired consciousness Multiple convulsions Circulation collapse Pulmonary oedema Abnormal bleeding Jaundice Haemoglobinuria Severe anaemia
Verbal response
Eye movements
Complication with malaria
Cerebral malaria Malaria with Renal failure Malaria associated impaired vision Malaria associated with ataxic gait Malaria associated with hearing loss Malaria with gram negative sepsis Hyper-reactive malaria syndrome HMS (Tropical splenomegaly syndrome) TSS Burkitts lymphoma
05/11/53
05/11/53
Complications of malaria
Cerebral malaria Definition: Patients unable to localized a painful stimulus (Blantyre coma scale of <=2 with malaria parasite and no other <= cause of neuropathy.
Cerebral malaria Malaria with Renal failure Malaria associated impaired vision Malaria associated with ataxic gait Malaria associated with hearing loss Malaria with gram-negative sepsis Hyper-reactive malaria syndrome HMS (Tropical splenomegaly syndrome) TSS Burkitts lymphoma
Cerebral malaria
A child with cerebral malaria, exhibiting severe opisthotonic (extensor) posturing. Between 10% to 10 to 20 20% of of children with cerebral malaria die, while approximately 7% are left with n e u ro l o g i c a l s e q u e l a e .
05/11/53
Acute renal failure
Common complication of severe falciparum malaria Almost exclusively in adults an older children Serum creatinine concentration >265 mol/l (3mg/dl)
with 24 hour urine output <400ml, in spite of rehydration, in patients who have asexual forms of p.falciparum in their peripheral blood film Typical presentation of patient with delayed referral and/or delayed treatment. Common in males Definition of Malaria Acute Renal failure (MARF)
Acute Renal Failure
Two Categories of MARF 1. Acute renal failure with multiple organ failure 1.
(Associated with poor prognosis)
2. Acute infection with renal failure (Good prognosis 2.
provided there is dialyisis available.
Hyper-reactive malaria syndrome (HMS) Hyper-reactive malaria syndrome (HMS)
Diagnostic Criteria for HMS
HMS is a specific disorder characterized by massive
splenomegaly and anaemia.
Common disorder in many malarious areas and affects
up to two perecent of the population in West Africa.
HMS occurs twice as frequently in female as in males
and any person over 10 years can be affected
Spleen of a least 10 cm Long-term residence in malarious area Raised serum IgM Response to anti-malaria drugs Minor Criteria Liver biopsy showing hepatitic sinusoidal lymphocytosis Normal immune response to antigen challenge Normal phytohaemagglutination response Hypersplenism Lymphocyte proliferation Familial occurrence
Major Criteria
Management of Malaria
Objective behind the management of malaria To provide prompt treatment To reduce burden of parasitaemia To identify complications and respond appropriately and
promptly To minimizes the extent of complications To prevent infections
Clinical Malaria
Mild and moderate
Severe and complicated Malaria
Oral medication and monitoring
Parenteral medication
05/11/53
Treatment of malaria Management of malaria
Chemotherapy for severe malaria
Choice of treatment will depend of the clinical condition
of the patient and some genetic consideration
Treatment of Malaria
Patient with severe falciparum malaria and those who
Chemotherapy Chloroquine Amodiaquine Quinine Sulfadoxine and pyrimethamine (SP) Artesimine derivative Supportive treatment Fluids Anticonvulsants Analgesic Antipyretics Packed Red Cells others
are vomiting will require parentral treatment at least during the initial phase of management.
Prior medication will guide the choice of antimalaria
Treatment of malaria
Quinine
Treatment of Malaria
Side effect of Quinine
Currently the most widely used drug in the management of severe Dose regime 20 20mg/kg body weight as a start dose (Deep
falciparum malaria. intramuscular injection. Followed by maintenance dose of 10 10mg/kg body weight after 12 12hours and subsequently 12 12hours interval till patient can tolerate oral medication Oral quinine is given at 10 10mg/kg body weight (3X daily ) for the additional days. Maximum of 7days is allowed. IV-quinine is recommended but requires strict monitoring IV
Severe life threatening toxicity are rare Cinchonism-When plasma concentration is more than 5mg/L. Characterized by Tinnitus, high tone deafness, nausea, uneasiness, malaise and blurring of vision. Vomiting is likely if core temperatures are high.- Not and indication for stopping treatment
2. 2. 3. 3 . 4. 4.
Hypotension, Myocardial conduction disturbances blindness, deafness, and coma is associated with plasma concentration below 20 20mg/L Hypoglycaemia-Due to hyper-Insulinaemia Thrombocytopenia, coombs-positive haemolytic anaemia, haemolytic uraemic Syndrome
Treatment of malaria C hl o r o q ui ne
Drug Resistance
multiply or to survive in the presence of concentrations of a drug that normally destroy parasites of the same species or prevent their multiplication. Levels of Resistance: RI RI-Following treatment, parasitaemia clears but a recrudescence occurs. RII Following treatment, there is a reduction but not a clearance of parasitaemia RIII-Following treatment there is no reduction of parasitaemia
Definition: Defined by WHO as the ability of parasite to
Remains an effective treatment for severe malaria in those few
areas where p. falciparum retains full sensitivity
Amodiaquine Amodiaquine may be a useful substitute for chloroquine when oral Amodiaquine is rapidly and extensively converted to a
treatment is required. Parentral formulation is not available pharmacologically active metabolite, des-ethylamodiaquine, following oral administration, ant it seems that this metabolite is responsible for most of the antimalaria activity.
05/11/53
Prevention Vector control
Residual Indoor Spraying Outdoor spraying Use of ITBNs Indoor spraying
Chemo-prophylaxis
Chloroquine Progaunil Mefloquine
Vaccine
Thank you
Assignment
Write briefly on malaria preventive
initiatives in sub-Saharan Africa (Maximum of 2 pages)
You might also like
- Malaria: Dr. Shree Narayan Yadav Internal Medicine Resident NamsDocument44 pagesMalaria: Dr. Shree Narayan Yadav Internal Medicine Resident Namsasyanadhikary18No ratings yet
- Managing Malaria: Treatment and Prevention StrategiesDocument47 pagesManaging Malaria: Treatment and Prevention Strategiesadamu mohammadNo ratings yet
- Management of Complicated MalariaDocument36 pagesManagement of Complicated MalariaAnu SinhaNo ratings yet
- Management of Severe Malaria: Kitwe Teaching Hospital Department of PaediatricsDocument24 pagesManagement of Severe Malaria: Kitwe Teaching Hospital Department of PaediatricsDorcas KafulaNo ratings yet
- Malaria: Dr. Shree Narayan Yadav Internal Medicine Resident NamsDocument40 pagesMalaria: Dr. Shree Narayan Yadav Internal Medicine Resident Namsasyanadhikary18No ratings yet
- Malaria Transmission, Species, Clinical Features & TreatmentDocument33 pagesMalaria Transmission, Species, Clinical Features & TreatmentAndarge ImperialNo ratings yet
- MalariaDocument41 pagesMalariaMohiuddin AhmedNo ratings yet
- Acute Febrile IllnessesDocument96 pagesAcute Febrile IllnessesHAlid mohammed100% (1)
- Malaria LectureDocument32 pagesMalaria LectureNwosu Ogbonna GabrielNo ratings yet
- Malaria: Etiology, Pathogenesis, Clinical Presentation and ManagementDocument30 pagesMalaria: Etiology, Pathogenesis, Clinical Presentation and ManagementHUSNAH SULAIMANNo ratings yet
- Malaria: Definition: Infection Due To PlasmodiumDocument17 pagesMalaria: Definition: Infection Due To PlasmodiumCLEMENTNo ratings yet
- Malaria MB CHB January 2018-FinalDocument36 pagesMalaria MB CHB January 2018-Finalokwadha simionNo ratings yet
- Malaria: Pathophysiology, Clinical Manifesta6ons and TreatmentDocument14 pagesMalaria: Pathophysiology, Clinical Manifesta6ons and TreatmentGuilhermeNo ratings yet
- Protozoal InfectionDocument66 pagesProtozoal InfectionGEM SCANNo ratings yet
- MalariaDocument27 pagesMalariaHadi El-MaskuryNo ratings yet
- Malaria UnderstandingDocument29 pagesMalaria UnderstandingAmit yadavNo ratings yet
- SEI - INEP - 0137469 - Projeto BásicoDocument29 pagesSEI - INEP - 0137469 - Projeto BásicoMARLOMbran HERRNo ratings yet
- Nephrotic SyndromeDocument49 pagesNephrotic SyndromeAMA237No ratings yet
- Pathology of Common Glomerular Syndromes: DR Purushotham KrishnappaDocument34 pagesPathology of Common Glomerular Syndromes: DR Purushotham KrishnappaTarin IslamNo ratings yet
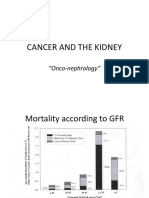
- Cancer and The KidneyDocument29 pagesCancer and The Kidney[ qιlα ]No ratings yet
- MalariaDocument44 pagesMalariasantosh goitNo ratings yet
- Treating Complicated Malaria in ChildrenDocument36 pagesTreating Complicated Malaria in ChildrenMwanja MosesNo ratings yet
- Nephrotic Syndrome Definition and CausesDocument23 pagesNephrotic Syndrome Definition and CausesamlymarsNo ratings yet
- Malaria Es PregcyDocument61 pagesMalaria Es PregcyNinaNo ratings yet
- Case Study - Nephrotic SyndromeDocument42 pagesCase Study - Nephrotic Syndromefarmasi rsud cilincingNo ratings yet
- Common Renal DiseasesDocument59 pagesCommon Renal DiseasesBegashawNo ratings yet
- Glomerular Diseases Part II: Georgette E. Lee, MD, FPCP, DPSNDocument75 pagesGlomerular Diseases Part II: Georgette E. Lee, MD, FPCP, DPSNToyoNo ratings yet
- Nephrotic Syndrome: DR Naing Naing Oo SenioturerDocument16 pagesNephrotic Syndrome: DR Naing Naing Oo SenioturerAbdulrahman NajiNo ratings yet
- Approach Nefroritic SXDocument58 pagesApproach Nefroritic SX[ qιlα ]No ratings yet
- G6PD Deficiency RBC Hemolysis from TMP-SMXDocument63 pagesG6PD Deficiency RBC Hemolysis from TMP-SMXAppu ayyala100% (2)
- Understanding Glomerular Disease: C.M. Yuan Nephrology SVC Walter Reed Army Medical Center Washington, DC 20307Document40 pagesUnderstanding Glomerular Disease: C.M. Yuan Nephrology SVC Walter Reed Army Medical Center Washington, DC 20307mondy199646No ratings yet
- Nephrotic Syndrome in Adult (Bahan Kuliah)Document49 pagesNephrotic Syndrome in Adult (Bahan Kuliah)Jkp PhieNo ratings yet
- MBBS-4 No014090Document43 pagesMBBS-4 No014090diphylleia90grayiNo ratings yet
- Malaria by professor Motea Al-AwlaqiDocument23 pagesMalaria by professor Motea Al-AwlaqiMotea AlawlaqiNo ratings yet
- HELLP SyndromeDocument11 pagesHELLP Syndromeumar akhsaniNo ratings yet
- Red Cell DisordersDocument46 pagesRed Cell DisordersSofi Nur FitriaNo ratings yet
- Malaria NewDocument29 pagesMalaria Newham sotheaNo ratings yet
- Nephrotic SyndromeDocument15 pagesNephrotic SyndromeMaryam MohamedaliNo ratings yet
- The Hellp Syndrome: DR Dohbit Sama Obs-Gyn H.G.O.P.Y - YaoundeDocument19 pagesThe Hellp Syndrome: DR Dohbit Sama Obs-Gyn H.G.O.P.Y - Yaoundemusinguzi albertNo ratings yet
- Yenny - Pemicu 4Document8 pagesYenny - Pemicu 4Yenny DarmawanNo ratings yet
- Plasma University: Guriel-GalgadudDocument26 pagesPlasma University: Guriel-GalgadudDr AbdulkadirNo ratings yet
- Nephrotic Syndrome in ChildrenDocument36 pagesNephrotic Syndrome in ChildrenMalueth AnguiNo ratings yet
- Pituitary Lecture1Document37 pagesPituitary Lecture1أديبNo ratings yet
- Malaria Other ComplicationsDocument36 pagesMalaria Other ComplicationsmaircusNo ratings yet
- Nephrotic and NephriticDocument27 pagesNephrotic and Nephritictam meiNo ratings yet
- Renal Disease in PregnancyDocument19 pagesRenal Disease in PregnancyDani DanyNo ratings yet
- HematuriaDocument42 pagesHematuriaAhmad SobihNo ratings yet
- Managing Eclampsia: A Guide to Treatment and PreventionDocument34 pagesManaging Eclampsia: A Guide to Treatment and Preventionاحمد وائل عبد الشافى ابو المعاطى UnknownNo ratings yet
- FARMAKOTERAPI pada PASIEN MALARIADocument47 pagesFARMAKOTERAPI pada PASIEN MALARIAEnvhy WinaNo ratings yet
- Interstitial NephritisDocument21 pagesInterstitial NephritisAhmed RaadNo ratings yet
- Presentation 2Document43 pagesPresentation 2tadeleNo ratings yet
- 07.bone Marrow Failures in ChildrenDocument36 pages07.bone Marrow Failures in ChildrenPascalNo ratings yet
- MANAGEMENT OF MALARIA: CLINICAL GUIDE AND CASE STUDYDocument55 pagesMANAGEMENT OF MALARIA: CLINICAL GUIDE AND CASE STUDYAnu SinhaNo ratings yet
- Severe Plasmodium Falciparum Malaria: Utility of Exchange TransfusionDocument11 pagesSevere Plasmodium Falciparum Malaria: Utility of Exchange TransfusionArja' WaasNo ratings yet
- Pediatric Malaria Treatment & Management: Approach Considerations, Intensive Care, Deterrence and PreventionDocument4 pagesPediatric Malaria Treatment & Management: Approach Considerations, Intensive Care, Deterrence and PreventionVivi DeviyanaNo ratings yet
- Acute Lymphoblastic LeukemiaDocument7 pagesAcute Lymphoblastic LeukemiaSahara EffendyNo ratings yet
- Hemolytic Uremic Syndrome: Prof. Pediatric Nephrology Sindh Institute of Urology & Transplanatation PakistanDocument111 pagesHemolytic Uremic Syndrome: Prof. Pediatric Nephrology Sindh Institute of Urology & Transplanatation PakistanDr. Mir Uzair HashmiNo ratings yet
- Nephrotic Syndrome 5th Year Lecture 2011Document7 pagesNephrotic Syndrome 5th Year Lecture 2011Gutierrez MarinellNo ratings yet
- HELLP Syndrome: Guide to the Rare Pregnancy ComplicationDocument2 pagesHELLP Syndrome: Guide to the Rare Pregnancy ComplicationAnonymous EA9uILwJ08No ratings yet
- My CVDocument4 pagesMy CVAnastasiafynnNo ratings yet
- CarbohydratesDocument16 pagesCarbohydratesAnastasiafynnNo ratings yet
- VisualDocument17 pagesVisualAnastasiafynnNo ratings yet
- Anaesthesia Resident's HandbookDocument445 pagesAnaesthesia Resident's HandbookAnastasiafynn50% (2)
- Blood Glucose MonitoringDocument2 pagesBlood Glucose MonitoringAnastasiafynnNo ratings yet
- YawsDocument15 pagesYawsAnastasiafynnNo ratings yet
- Turnitin Originality ReportDocument9 pagesTurnitin Originality ReportfynneroNo ratings yet
- It SpecialistDocument3 pagesIt SpecialistAnastasiafynnNo ratings yet
- Schools JobsDocument3 pagesSchools JobsAnastasiafynnNo ratings yet
- Sym DromeDocument4 pagesSym DromeAnastasiafynnNo ratings yet
- HirsutismDocument22 pagesHirsutismAnastasiafynnNo ratings yet
- Biochemistry of The Liver and Kidney. Urine Formation.Document22 pagesBiochemistry of The Liver and Kidney. Urine Formation.AnastasiafynnNo ratings yet
- Us 134Document2 pagesUs 134452bobNo ratings yet
- CCS - Handbook of Anesthesiology (2005)Document180 pagesCCS - Handbook of Anesthesiology (2005)Rojelle LezamaNo ratings yet
- Type 1 Diabetes: Endocrine Glands Insulin Pump Glucose Test Insulin Pump Type I DiabetesDocument9 pagesType 1 Diabetes: Endocrine Glands Insulin Pump Glucose Test Insulin Pump Type I DiabetesAnastasiafynnNo ratings yet
- CirculationDocument4 pagesCirculationAnastasiafynnNo ratings yet
- Biochemistry of Liver and KidneyDocument24 pagesBiochemistry of Liver and KidneyAnastasiafynnNo ratings yet
- Membrane Structure and Function ReviewDocument5 pagesMembrane Structure and Function ReviewAnastasiafynnNo ratings yet
- Biochemistry of Blood, Muscle and Connective Tissue.Document21 pagesBiochemistry of Blood, Muscle and Connective Tissue.Anastasiafynn100% (1)
- Biochemistry of Bone Tissueдокумент Microsoft WordDocument19 pagesBiochemistry of Bone Tissueдокумент Microsoft WordAnastasiafynnNo ratings yet
- Biochemistry of Liver and KidneyDocument24 pagesBiochemistry of Liver and KidneyAnastasiafynnNo ratings yet
- Blood Circulation System and It Regulation. Blood Circulation in Facial RegionDocument23 pagesBlood Circulation System and It Regulation. Blood Circulation in Facial RegionAnastasiafynnNo ratings yet
- Water and Sodium BalanceDocument4 pagesWater and Sodium Balanceapi-3712326No ratings yet
- Biochemistry - As Science - Biomolecules. Structure and Properties of Enzymes - Isoenzymes.Document41 pagesBiochemistry - As Science - Biomolecules. Structure and Properties of Enzymes - Isoenzymes.AnastasiafynnNo ratings yet
- CCS - Handbook of Anesthesiology (2005)Document180 pagesCCS - Handbook of Anesthesiology (2005)Rojelle LezamaNo ratings yet
- Behaviourial ScienceDocument4 pagesBehaviourial ScienceAnastasiafynnNo ratings yet
- Anaesthesia Resident's HandbookDocument445 pagesAnaesthesia Resident's HandbookAnastasiafynn50% (2)
- AcidosisDocument2 pagesAcidosisAnastasiafynnNo ratings yet
- Amino Acids Metabol Synth of UreaDocument32 pagesAmino Acids Metabol Synth of UreaAnastasiafynn100% (1)
- Water and Sodium BalanceDocument4 pagesWater and Sodium Balanceapi-3712326No ratings yet
- Thesis PromptsDocument7 pagesThesis Promptsauroratuckernewyork100% (2)
- Cytogenectics Reading ListDocument2 pagesCytogenectics Reading ListHassan GillNo ratings yet
- Mafia Bride by CD Reiss (Reiss, CD)Document200 pagesMafia Bride by CD Reiss (Reiss, CD)Aurniaa InaraaNo ratings yet
- Endodontic Emergencies GuideDocument27 pagesEndodontic Emergencies GuideJitender Reddy100% (1)
- System Bus in Computer Architecture: Goran Wnis Hama AliDocument34 pagesSystem Bus in Computer Architecture: Goran Wnis Hama AliGoran WnisNo ratings yet
- (Salim Ross) PUA 524 - Introduction To Law and The Legal System (Mid Term)Document4 pages(Salim Ross) PUA 524 - Introduction To Law and The Legal System (Mid Term)Salim RossNo ratings yet
- Thick Seam Mining Methods and Problems Associated With It: Submitted By: SAURABH SINGHDocument13 pagesThick Seam Mining Methods and Problems Associated With It: Submitted By: SAURABH SINGHPrabhu PrasadNo ratings yet
- Gizmotchy 3 Element Complete Assembly InstructionsDocument5 pagesGizmotchy 3 Element Complete Assembly InstructionsEuropaNo ratings yet
- DX DiagDocument42 pagesDX DiagVinvin PatrimonioNo ratings yet
- Estimating PSCC for Electrical InstallationsDocument2 pagesEstimating PSCC for Electrical InstallationsgmuitaNo ratings yet
- Vee 2003Document14 pagesVee 2003Syed faizan Ali zaidiNo ratings yet
- The Seven Seals of Revelation and The SevenDocument14 pagesThe Seven Seals of Revelation and The Sevenyulamula100% (2)
- Bioav 3Document264 pagesBioav 3Sabiruddin Mirza DipuNo ratings yet
- ZO 503 Physiological Chemistry by Dr.S.S.KunjwalDocument22 pagesZO 503 Physiological Chemistry by Dr.S.S.KunjwalAbhishek Singh ChandelNo ratings yet
- IRC-114-2013 Use of Silica Fume in Rigid PavementDocument14 pagesIRC-114-2013 Use of Silica Fume in Rigid PavementZakee MohamedNo ratings yet
- Nec TutorialDocument5 pagesNec TutorialbheemasenaNo ratings yet
- Benokraitis, Benokraitis Nijole Vaicaitis - Marriages & Families - Changes, Choices, and Constraints-Pearson (2015)Document617 pagesBenokraitis, Benokraitis Nijole Vaicaitis - Marriages & Families - Changes, Choices, and Constraints-Pearson (2015)colleen100% (1)
- Stress-Busting Plan for Life's ChallengesDocument3 pagesStress-Busting Plan for Life's Challengesliera sicadNo ratings yet
- Pyrolysis ProjectDocument122 pagesPyrolysis ProjectSohel Bangi100% (1)
- No-Till For Micro Farms: The Deep-Mulch Method (Lean Micro Farm)Document20 pagesNo-Till For Micro Farms: The Deep-Mulch Method (Lean Micro Farm)Chelsea Green PublishingNo ratings yet
- Latihan Soal Recount Text HotsDocument3 pagesLatihan Soal Recount Text HotsDevinta ArdyNo ratings yet
- MIL (Second Quarter)Document13 pagesMIL (Second Quarter)Menma ChanNo ratings yet
- Hci01 HumanComputerInteraction OverviewDocument140 pagesHci01 HumanComputerInteraction OverviewAlexSpiridonNo ratings yet
- BCMEDocument9 pagesBCMEVenkateshwaran VenkyNo ratings yet
- Black BeautyDocument70 pagesBlack BeautyMeryem DevirgenNo ratings yet
- X TensoqaDocument2 pagesX TensoqaLeo CabelosNo ratings yet
- Chair Locker Provides Storage and Space SavingsDocument32 pagesChair Locker Provides Storage and Space SavingsElza S. GapuzNo ratings yet
- 11.trouble Shooting For TMDocument9 pages11.trouble Shooting For TMfrezgi birhanuNo ratings yet
- Linked ListDocument83 pagesLinked Listshahida18No ratings yet
- Cave Rescue ActivityDocument6 pagesCave Rescue Activityshweta bambuwalaNo ratings yet