Professional Documents
Culture Documents
Vakcinacija U Nemackoj Germany Ip Vakcina
Uploaded by
Nikola Ivankovic0 ratings0% found this document useful (0 votes)
168 views3 pagesu vezi obavezne vakcine u Nemackoj
Original Title
Vakcinacija u Nemackoj Germany Ip Vakcina
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentu vezi obavezne vakcine u Nemackoj
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
168 views3 pagesVakcinacija U Nemackoj Germany Ip Vakcina
Uploaded by
Nikola Ivankovicu vezi obavezne vakcine u Nemackoj
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
GERMANY
!n Germany approximately 90 of vaccines are given in the offices of private
physicians. The remaining 10 are given in public health clinics, schools, or day
care centers through special programs of the Lander or by occupational health
physicians. Physicians can choose among all avialable licensed vaccines. Combined
vaccines, as the hexavalent product, are widely used. vaccines are not produced
locally.
!mmunisation in Germany is voluntary. There are no school or day care requirements
regarding immunization, either nationally or in any state. !mmunisation status is
checked at school entry mandatory. These data have to be delivered to the Robert
Koch !nstitute (RK!). The RK! is responsibele for measuring the vaccine coverage at
the national leve. There are great differences between the vaccine coverage between
the Laender and the counties within the Laender. A plan for Eliminating Neasles has
been launched in 1998 and NNR coverage is increasing in the recent years.
Nationwide data are available at the RK! Homepage (www.rki.de,
!nfektionsschutzf!mpfenf!mpfstatus).
The Standing vaccination Committee (ST!KO) is the major federal commission
concerned with vaccination issues. The immunization schedule recommended by
ST!KO is published by the Robert Koch !nstitute (RK!). RK! provides all
administrative support to ST!KO. Although ST!KO may only recommend vaccines
which are licensed in Germany, it is important to note that these recommendations
have no legal authority. Further, ST!KO recommendations do not have to be
approved or endorsed by the Ninistry of Health. Thus, there are no official
government recommendations at the national level and no mandatory vaccines. The
federal states make the official recommendations for the populations within their
geographic jurisdiction and usually follow ST!KO recommendations closely. To date,
the Laender, at a minimum, have always followed ST!KO recommendation and may
be more expansive. For example, some states may recommend viral influenza
vaccine for a greater proportion of their population than ST!KO. Besides the
immunisation schedule for babies, children, adolescents and adults in Germany the
ST!KO makes also recommendations for special occupational groups (e.g. medical
staff (HepA;B, !nfluenza), police (HepB), travellers, patients with chronic dieseases,
special risk groups (drug users (HepB), homosexuals (HepA,B), prisoners, pregnant
women, close contacts to newborns (pertussis) etc.
Although the vaccination plan is nationally recommended, regions can decide
independently to include in the schedule also vaccinations for other diseases, on the
basis of the local epidemiological situation.
The national vaccination plan approved in 2005 includes recommendations on
PCv, NEN-C and chicken pox vaccinations for selected groups of individuals (i.e.
individual with high risk of acquiring the infection andfor developing severe clinical
picture), but Regions can also decide for additional vaccination policies at local level.
There is no central government financing for childhood immunizations. The
vast majority (90) of vaccines are purchased in the private sector and 90 of
these are paid for by statutory insurance policies. Statutory insurance is paid for by
payroll taxes on employees and employers. Children are covered by their parents'
policies. The remaining 10 of vaccines purchased in the private sector are paid by
supplemental private insurance policies or travellers (travel-related vaccines are not
free of charge). The remaining 10 of administered vaccines not purchased in the
private sector are provided by the states as part of special immunization programs in
the schools or as part of day care catch-up programs.
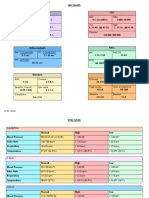
Recommended immunisation schedule for babies, children, adolescents and adults in
Germany (source: German Standing Committee on vaccination (ST!KO): 7f2006
http:ffwww.rki.defcln_011fnn_9759+0fDEfContentf!nfektfEpidBullfArchivf2006f30__
06,template!d=raw,property=publicationFile.pdff30_06
DTaP
1
Hib
1
HepB
1
IPV
1
Pneumo-
coccal
Men C MMR
2
Vari-
cella
dTap
Birth Yes
3
2 months Yes Yes Yes Yes Yes (PCv)
3months Yes Yes
+
Yes
+
Yes
+
Yes (PCv)
4 months Yes Yes Yes Yes Yes (PCv)
11-14
months
Yes Yes Yes Yes Yes (PCv)
Yes Yes
15-23
months
Yes
5
Yes Yes
6
5- 6 years Yes
9-17 years
Yes
7
Yes
Yes
> 1S years
> 60 years Yes (PPv)
every 6
years
Legend:
D: diphtheria vaccine (normal dose); d: low dose diphtheria vaccine
(booster dose)
aP: acellular pertussis vaccine, ap: low dose acellular pertussis
vaccine (booster dose)
Hib: haemophilus !nfluenzaeTyp B vaccine !Pv: inactivated polio vaccine
HepB: hepatitis B vaccine Nen C: meningococcal type C
conjugate vaccine
PCv: pneumococcal heptavalent coniugate vaccine; PPv: pneumococcal 23valent
polysaccharide vaccine
NNR: measles, mumps, rubella vaccine; NNRv: combined measles,
mumps, rubella, varicella vaccine
1
Given at least + weeks apart with a required minimum of six months between
final (11-1+ months dose) and penultimate dose
2
Ninimum interval of + weeks required between doses
3
Recommended for newborns of HbsAg positive mothers or to mothers with
unknown HbsAg status
+
Given only if administered as a combination vaccine containing a pertussis
component (aP), otherwise the second dose is recommended at + months
5
0ne dose in the 2nd year of life; should not be administered simultaneously
with NNR+monovalent varicella vaccine or NNRv vaccine
6
Second dose if administered as combined NNRv-vaccine
7
Primary HepB vaccination for previously unvaccinated persons and completion
of the course in those incompletely vaccinate
You might also like
- Cdi 2106 CDocument2 pagesCdi 2106 CVerdi LeonardoNo ratings yet
- Community Health Nursing (Learning Feedback Diary (LFD #25)Document3 pagesCommunity Health Nursing (Learning Feedback Diary (LFD #25)Angelica Malacay RevilNo ratings yet
- EPI Vaccines Revised Oct 2010Document18 pagesEPI Vaccines Revised Oct 2010Jei JayNo ratings yet
- Immunization Review GPDocument46 pagesImmunization Review GPKishore ChandkiNo ratings yet
- Expanded Program ImmunizationDocument4 pagesExpanded Program ImmunizationLheiDanielMariellMonteroNo ratings yet
- CHN 1 LEC WEEK 9 Records in Family Health Nursing PracticeDocument14 pagesCHN 1 LEC WEEK 9 Records in Family Health Nursing PracticeSenyorita ArdiNo ratings yet
- Vaccine Indication and ContraindicationDocument34 pagesVaccine Indication and ContraindicationMusa yohanaNo ratings yet
- National Immunization Program: Ray Anthony A. Camaliga, M.D Level 1 Resident DFCMDocument39 pagesNational Immunization Program: Ray Anthony A. Camaliga, M.D Level 1 Resident DFCMAnthony AbulNo ratings yet
- Expanded Program On ImmunizationDocument7 pagesExpanded Program On ImmunizationEllaine B. PatalinghugNo ratings yet
- Hilary Butler Hep B VaxDocument14 pagesHilary Butler Hep B VaxMeryl DoreyNo ratings yet
- NIP Schedule2016Document2 pagesNIP Schedule2016JS57No ratings yet
- Immunization Routine Table1Document9 pagesImmunization Routine Table1MeeKo VideñaNo ratings yet
- Universalimmunisationprogram 171120044520Document22 pagesUniversalimmunisationprogram 171120044520Gagan GargNo ratings yet
- Expanded Immunization ProgramDocument8 pagesExpanded Immunization ProgramKim Harold SalasNo ratings yet
- Diagnosis/vaccination/: Hepatitis B VaccineDocument6 pagesDiagnosis/vaccination/: Hepatitis B Vaccinereza satriaNo ratings yet
- The Value of Rotavirus Vaccination in Europe A Call For ActionDocument21 pagesThe Value of Rotavirus Vaccination in Europe A Call For ActionYELYMARNo ratings yet
- Expanded Program On ImmunizationDocument7 pagesExpanded Program On ImmunizationGLadys Gegare100% (1)
- Expanded Program On ImmunizationDocument4 pagesExpanded Program On ImmunizationKrizle AdazaNo ratings yet
- National Immunisation Program Schedule: (AS AT MAY 2012)Document2 pagesNational Immunisation Program Schedule: (AS AT MAY 2012)docivirusNo ratings yet
- Current Presumptive Immunization SchedulesDocument4 pagesCurrent Presumptive Immunization SchedulesPedro Julian Tenorio ApesteguiNo ratings yet
- Immunizations: Policies and Procedures: Intensive Care Nursery House Staff ManualDocument2 pagesImmunizations: Policies and Procedures: Intensive Care Nursery House Staff ManualSedaka DonaldsonNo ratings yet
- Table 2: Summary of WHO Position Papers - Recommended Routine Immunizations For ChildrenDocument8 pagesTable 2: Summary of WHO Position Papers - Recommended Routine Immunizations For Childrenfadityo1No ratings yet
- Adult ImmunizationDocument6 pagesAdult ImmunizationAmit GoelNo ratings yet
- Other Congenital and Perinatal InfectionsDocument3 pagesOther Congenital and Perinatal InfectionsRabi SyedNo ratings yet
- Table 2: Summary of WHO Position Papers - Recommended Routine Immunizations For ChildrenDocument7 pagesTable 2: Summary of WHO Position Papers - Recommended Routine Immunizations For ChildrenKrishnendu PramanikNo ratings yet
- Local Media3061431616755544477Document42 pagesLocal Media3061431616755544477Kim Harold SalasNo ratings yet
- Antigen Vaccination of Health Care Workers RecommendedDocument2 pagesAntigen Vaccination of Health Care Workers RecommendedNico Angelo CopoNo ratings yet
- Expanded Program For Immunization CHD ReportDocument12 pagesExpanded Program For Immunization CHD ReportCristalPagcaliwangan0% (1)
- Immunization EPI Huda 201212Document5 pagesImmunization EPI Huda 201212Aerish TupazNo ratings yet
- Expanded Program On ImmunizationDocument6 pagesExpanded Program On ImmunizationAiza Oronce100% (1)
- Hepatitis Vaccines: Keywords: Hepatitis A, B, C, D, and E VaccinesDocument18 pagesHepatitis Vaccines: Keywords: Hepatitis A, B, C, D, and E VaccinesPutri Anita AchmadNo ratings yet
- HHVVHHDocument2 pagesHHVVHHYessaminNo ratings yet
- Table 4 Feb 2023 EnglishDocument2 pagesTable 4 Feb 2023 Englishgocelij948No ratings yet
- Epi PowerpointDocument29 pagesEpi PowerpointFelisa Lacsamana Gregorio100% (3)
- Immunistion Schedule CardDocument2 pagesImmunistion Schedule CardRohini SelvarajahNo ratings yet
- 1 s2.0 S0264410X19301252 MainDocument6 pages1 s2.0 S0264410X19301252 MainJuliana Menara de Souza MarquesNo ratings yet
- Immunization UipDocument20 pagesImmunization Uipdevesh gargNo ratings yet
- Childhood ImmunizationDocument16 pagesChildhood ImmunizationApple Grace TalamonNo ratings yet
- Expanded Program On ImmunizationDocument7 pagesExpanded Program On ImmunizationVanessa Abboud100% (1)
- Measle Vac Gap in GermanyDocument8 pagesMeasle Vac Gap in GermanyNancy KawilarangNo ratings yet
- DPBH Technical Bulletin 06-06-16 - Use of Tdap and TD VaccineDocument1 pageDPBH Technical Bulletin 06-06-16 - Use of Tdap and TD VaccineBlayne OsbornNo ratings yet
- Macdona Masali AssignmentDocument5 pagesMacdona Masali AssignmentMasali MacdonaNo ratings yet
- Pentavalent Vaccine Guide For HWs With Answers To FAQsDocument8 pagesPentavalent Vaccine Guide For HWs With Answers To FAQsVamsidhar KavikondalaNo ratings yet
- Expanded Program On Immunization CHNDocument4 pagesExpanded Program On Immunization CHNgeralynroseNo ratings yet
- MGA VACCINE NA SAKOP NG NIP: BCG Birth Dose, Hepatitis B Birth Dose, OralDocument3 pagesMGA VACCINE NA SAKOP NG NIP: BCG Birth Dose, Hepatitis B Birth Dose, OralVanessa AbboudNo ratings yet
- EPIDocument7 pagesEPIheng_gutierrezNo ratings yet
- National Perinatal Hepatitis B Prevention Program: 2009 - 2017Document10 pagesNational Perinatal Hepatitis B Prevention Program: 2009 - 2017Suwandi ChangNo ratings yet
- SdsadsdadsDocument143 pagesSdsadsdadsKayeNo ratings yet
- SummaryDocument6 pagesSummaryChristine AlmoraNo ratings yet
- Epi NotesDocument5 pagesEpi NoteshoneykrizelNo ratings yet
- Department of Health - Expanded Program On Immunization - 2012-05-16Document7 pagesDepartment of Health - Expanded Program On Immunization - 2012-05-16MasterclassNo ratings yet
- Extended Program of ImmunizationDocument39 pagesExtended Program of ImmunizationJohn Go LiNo ratings yet
- Epi 2020 For SharingDocument69 pagesEpi 2020 For SharingEmmy Krisha Marie PatrimonioNo ratings yet
- IMMUNIZATIONDocument17 pagesIMMUNIZATIONZenasB.PalomaNo ratings yet
- Health Advice and Immunizations for TravelersFrom EverandHealth Advice and Immunizations for TravelersNo ratings yet
- The Routine Immunisation ScheduleDocument10 pagesThe Routine Immunisation ScheduleJamesWaitonNo ratings yet
- Summary of The WHO Position On Rubella Vaccine-July 2020Document3 pagesSummary of The WHO Position On Rubella Vaccine-July 2020Enchantia R. NightshadeNo ratings yet
- Good Health in the Tropics: Advice to Travellers and SettlersFrom EverandGood Health in the Tropics: Advice to Travellers and SettlersNo ratings yet
- Influenza vaccination: What does the scientific proof say?: Could it be more harmful than useful to vaccinate indiscriminately elderly people, pregnant women, children and health workers?From EverandInfluenza vaccination: What does the scientific proof say?: Could it be more harmful than useful to vaccinate indiscriminately elderly people, pregnant women, children and health workers?No ratings yet
- Medical Terminology and PhrasesDocument60 pagesMedical Terminology and Phrasesapi-3743320No ratings yet
- Disease and IllnessDocument3 pagesDisease and IllnessAntonius Robby100% (1)
- Varicella Immunization CertDocument2 pagesVaricella Immunization CertShaikahamedNo ratings yet
- Notifiable Conditions FormDocument3 pagesNotifiable Conditions FormDarius DeeNo ratings yet
- Copy of Integumentary Student Resources 1Document12 pagesCopy of Integumentary Student Resources 1Alondra Hernandez ReyesNo ratings yet
- Virology TableDocument10 pagesVirology TablekevinNo ratings yet
- Nclex Cram SheetDocument24 pagesNclex Cram Sheettoni100% (5)
- VirologyLearnTable 2017-Sketchy PDFDocument4 pagesVirologyLearnTable 2017-Sketchy PDFdfgbdfgNo ratings yet
- Amarina Study Guide 20Document94 pagesAmarina Study Guide 20Jamila Ziyaeva100% (14)
- Chick ListDocument1 pageChick ListMohammed ElhashimiNo ratings yet
- Congenital Infections - Dr. R. Adhi Teguh SpA (K)Document65 pagesCongenital Infections - Dr. R. Adhi Teguh SpA (K)syak turNo ratings yet
- Nephrotic SyndromeDocument14 pagesNephrotic SyndromeAnna Michael AbdullahNo ratings yet
- New Frontiers 2 SB TranscriptsDocument47 pagesNew Frontiers 2 SB TranscriptsNguyễn Ngọc Mai KhanhNo ratings yet
- What Are The Symptoms of Chicken PoxDocument6 pagesWhat Are The Symptoms of Chicken PoxManoj CharayaNo ratings yet
- Communicable Disease AnswersDocument11 pagesCommunicable Disease AnswersRika MaeNo ratings yet
- Flaccid BladderDocument29 pagesFlaccid BladderphotosaurusrapNo ratings yet
- NLE PreBoard QuestionsDocument73 pagesNLE PreBoard QuestionsAaron Johnson Fantastico JarrellNo ratings yet
- ChickenpoxDocument2 pagesChickenpoxwq984c2kkfNo ratings yet
- Dr. Deshinta - Adult Vaccination Pontianak PDFDocument38 pagesDr. Deshinta - Adult Vaccination Pontianak PDFIzka P RahmaniaNo ratings yet
- DNA VirusDocument4 pagesDNA VirusShirlene Anne LeongsonNo ratings yet
- Opportunistic Infections: Dr. Baldev S. PrajapatiDocument69 pagesOpportunistic Infections: Dr. Baldev S. PrajapatiZazzZaffaNo ratings yet
- Intern Program - Health Evaluation Form: If Yes, Please List BelowDocument2 pagesIntern Program - Health Evaluation Form: If Yes, Please List BelowJHON FREDY VELÁSQUEZNo ratings yet
- SWT Microbiology DamsDocument80 pagesSWT Microbiology DamsvamshidhNo ratings yet
- Chicken Pox - NCPDocument2 pagesChicken Pox - NCPMaria Kyla VicenteNo ratings yet
- OTC TableDocument60 pagesOTC TableShamel Eshak75% (4)
- Trish BrochureDocument2 pagesTrish Brochureapi-266206554No ratings yet
- Chapter 43: Nursing Care of A Family When A Child Has An Infectious Disorder The Infectious Process #1 Infectious Disease in ChildrenDocument20 pagesChapter 43: Nursing Care of A Family When A Child Has An Infectious Disorder The Infectious Process #1 Infectious Disease in ChildrenMark oliver Gonzales100% (1)
- 9 Opportunistic InfectionsDocument14 pages9 Opportunistic InfectionsArini B. MulyaniNo ratings yet
- Chapter I VaricellaDocument5 pagesChapter I VaricellaKismet SummonsNo ratings yet
- Final Exam MCQsDocument23 pagesFinal Exam MCQsTrang Nguyen50% (2)