Professional Documents
Culture Documents
Antimicrobial Stewardship at Transition of Care From Hospital To Community
Uploaded by
Zamrotul IzzahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antimicrobial Stewardship at Transition of Care From Hospital To Community
Uploaded by
Zamrotul IzzahCopyright:
Available Formats
Antimicrobial Stewardship at Transition of Care from Hospital to Community Author(s): Nabin K.
Shrestha, MD, MPH; Archana Bhaskaran, MD; Nikole M. Scalera, MD, MS; Steven K. Schmitt, MD; Susan J. Rehm, MD; Steven M. Gordon, MD Reviewed work(s): Source: Infection Control and Hospital Epidemiology, Vol. 33, No. 4, Special Topic Issue: Antimicrobial Stewardship (April 2012), pp. 401-404 Published by: The University of Chicago Press on behalf of The Society for Healthcare Epidemiology of America Stable URL: http://www.jstor.org/stable/10.1086/664758 . Accessed: 26/12/2012 05:37
Your use of the JSTOR archive indicates your acceptance of the Terms & Conditions of Use, available at . http://www.jstor.org/page/info/about/policies/terms.jsp
.
JSTOR is a not-for-profit service that helps scholars, researchers, and students discover, use, and build upon a wide range of content in a trusted digital archive. We use information technology and tools to increase productivity and facilitate new forms of scholarship. For more information about JSTOR, please contact support@jstor.org.
The University of Chicago Press and The Society for Healthcare Epidemiology of America are collaborating with JSTOR to digitize, preserve and extend access to Infection Control and Hospital Epidemiology.
http://www.jstor.org
This content downloaded on Wed, 26 Dec 2012 05:37:29 AM All use subject to JSTOR Terms and Conditions
infection control and hospital epidemiology
april 2012, vol. 33, no. 4
concise communication
Antimicrobial Stewardship at Transition of Care from Hospital to Community
Nabin K. Shrestha, MD, MPH;1 Archana Bhaskaran, MD;1 Nikole M. Scalera, MD, MS;1 Steven K. Schmitt, MD;1 Susan J. Rehm, MD;1 Steven M. Gordon, MD1
Mandatory infectious disease consultation for parenteral antimicrobials at hospital discharge resulted in avoiding postdischarge parenteral antimicrobials in 28% of patients. No emergency department visit or rehospitalization within 30 days for these patients was a consequence of parenteral antimicrobial avoidance. Antimicrobial stewardship at transition of care is effective in reducing unnecessary antimicrobial use. Infect Control Hosp Epidemiol 2012;33(4):401-404
The purpose of this study was to examine whether parenteral antimicrobial avoidance through antimicrobial stewardship at the terminal end of hospitalization led to harm from inadequately treated infection, by comparing emergency department (ED) visits and rehospitalizations for patients in whom CoPAT was approved and those in whom it was avoided.
methods
This was a retrospective cohort study. The study protocol was reviewed and approved by the institutional review board. The Cleveland Clinic CoPAT Registry identies all patients discharged from hospital on parenteral antimicrobial therapy. The relevant elds in this registry are obtained from data entered in a structured data entry form (the CoPAT form) in the electronic health record (EHR), populated by ID attending physicians as part of routine work ow in the hospital. No patient can leave the hospital on parenteral antimicrobials without having a CoPAT form lled out. In February 2010 an electronic form for requesting ID consultation was introduced in the computerized provider order entry system of the Cleveland Clinic EHR. One of the required elds in the ID consultation request form is whether the consultation includes a CoPAT request. This infrastructure allows for easy identication of all ID consultations and also for all CoPAT consultation requests. All electronic ID consultation requests were examined to identify CoPAT consultations. All such consultations for patients 18 years or older between February 14, 2010, and May 14, 2010, were included. There were no exclusions. CoPAT avoidance was dened as cessation of all antimicrobials prior to hospital discharge or switching from a parenteral to an all-oral antimicrobial regimen. Patient demographic and clinical characteristics were collected by review of the EHR. All ID consultations were reviewed for nal CoPAT disposition and divided into 2 groups (approved or avoided). The clinical course was followed for all patients for the 30 days following discharge from hospital to determine whether they had any ED visit or hospital readmission within that time. The proportions of consultations with at least 1 subsequent ED visit or rehospitalization within 30 days of hospital discharge were compared across the 2 groups. Reasons for ED visits and hospital readmissions were also noted for those patients in whom CoPAT was avoided.
Antimicrobial stewardship programs have been strongly supported by the Infectious Diseases Society of America, the Society for Healthcare Epidemiology of America, and the American Society of Hospital Pharmacists.1,2 Major goals of such programs are to slow the development of antimicrobial resistance and to use antimicrobials in a cost-effective manner. A substantial proportion of antimicrobial use in hospitals is inappropriate.3 A multidisciplinary antimicrobial utilization team has been shown in a randomized controlled trial to improve the appropriateness of antimicrobial use.4 Most antimicrobial stewardship efforts are based on the 2 core strategies of prior authorization and/or prospective audit and feedback.1 Such programs thus focus on the front end of antimicrobial therapy in hospital settings. Many patients who receive antimicrobials in hospital are also discharged on antimicrobial therapy, to complete the treatment course at home or in long-term acute care centers, skilled nursing facilities, outpatient infusion centers, or dialysis centers.5 In the absence of antimicrobial stewardship, there is little to prevent patients from being discharged from hospital on inappropriate antimicrobial therapy. All patients who are to be discharged from the Cleveland Clinic hospital on parenteral antimicrobial therapy must be evaluated by an infectious disease (ID) staff physician, who shapes and approves the treatment plan and assumes responsibility for oversight of the antimicrobial treatment course.6 This process ensures that some patients who would have otherwise been discharged on community-based parenteral anti-infective therapy (CoPAT) will not leave the hospital on the same therapy, or, indeed, on any parenteral antimicrobial therapy, as a consequence of the ID consultation. However, overzealous antimicrobial avoidance in the name of stewardship could harm patients through inadequate treatment and could undermine the benets of hospitalization.
results
During the above 3-month period, 244 CoPAT consultation requests were received by the ID department. CoPAT was approved in 175 (72%) and avoided in 69 (28%) of the consultations. Of the 69 where CoPAT was avoided, oral anti-
This content downloaded on Wed, 26 Dec 2012 05:37:29 AM All use subject to JSTOR Terms and Conditions
402
infection control and hospital epidemiology
april 2012, vol. 33, no. 4
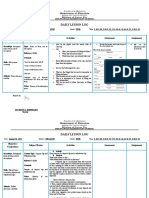
microbials were prescribed instead in 42 (17% of all consultations), and antimicrobials were avoided altogether in 27 (11% of all consultations). Characteristics of consultations in which CoPAT was approved and avoided are outlined in Table 1. Outpatient infectious disease follow-up with an ID physician familiar with the patient was scheduled in 167 (75%) of consultations: 150 of 175 approved (86%) and 17 of 69 avoided (25%). In the CoPAT-avoided group, there was an ED visit or rehospitalization in 27 of 69 (39%), compared to 46 of 129 (26%) in the CoPAT-approved group (odds ratio, 1.80; 95% condence interval, 0.993.29; P p .05), a difference that did not reach statistical signicance. There was also no signicant difference when ED visits and readmissions were compared separately for the 2 groups. Figure 1 depicts the reason for ED visit or rehospitalization for consultations where CoPAT was avoided, with the most common cause being the occurrence of new clinical problems. No ED visit or rehospitalization was for relapsed or untreated infection and thus was not a direct result of avoidance of parenteral antimicrobials.
discussion
This study demonstrates that an antimicrobial stewardship strategy of antimicrobial oversight at care transition via an institutional policy of mandatory ID consultation requirement for every patient being discharged from hospital on parenteral antimicrobials results in avoidance of CoPAT in more than one-fourth of all patients, without increasing the risk of ED visit or readmission for an untreated or inadequately treated infection. Although not statistically signicant, the CoPAT-avoided group appeared to have more ED visits and rehospitalizations, but the relatively small sample size limited the studys ability to detect signicant differences. The study was nevertheless reassuring in showing that none of
table 1. Consultation Characteristics Characteristic
the ED visits or rehospitalizations for the CoPAT-avoided patients was because of an infection that was missed or inadequately treated. CoPAT avoidance was associated with lower ID follow-up appointments made, but it would not be fair to state that this may have contributed to the increased ED visits and rehospitalizations. Most of the CoPAT-avoided patients did not have a reason to warrant ID follow-up. One could argue that the ID follow-up prevented ED visits and rehospitalizations for non-ID reasons in the CoPAT-approved group, but that would be difcult to prove. A limitation of the study is that the retrospective review may not have identied all ED visits and rehospitalizations outside the Cleveland Clinic. About 75%80% of patients for whom an ID appointment is made actually show up for the appointment, increasing the likelihood that any outside ED visit or rehospitalization would be noted in the EHR. Because one of the ID physicians at Cleveland Clinic is listed as the physician overseeing the home care episode, we are usually notied whenever a patient receiving antimicrobial therapy at home is rehospitalized elsewhere. For the CoPAT-avoided patients, our ability to identify outside ED visits and rehospitalizations would have been a little more limited. However, we should still have identied the majority of such events. Although the hospital is a large referral hospital, more than 60% of our hospitalized patients are from Cuyahoga County. The integrated nature of our EHR allowed us to identify all ED visits and rehospitalizations at the Cleveland Clinic and in all 8 regional hospitals of the Cleveland Clinic Health System. Most of the ED visits and rehospitalizations would have occurred within this network of hospitals. Antimicrobial stewardship efforts provide value to hospitals. Controlling antimicrobial prescribing has been shown to result in demonstrable reductions in antimicrobial resistance and Clostridium difcile infections.7 Antimicrobial steward-
CoPAT avoided (n p 69) 59 (16) 38 (55) 47 17 5 8 4 8 0 2 (68) (25) (7) (516) (6) (12) (00) (13)
CoPAT approved (n p 175) 59 (14) 101 (58) 138 33 5 10 15 13 0 2 (79) (19) (3) (521) (9) (7) (01) (14)
Patient age, mean (SD), years Male patient Patient race Caucasian African American Other Duration of hospitalization, median (IQR), days Type of consultation Urgent consultation Weekend consultation Days to respond to consultation request, median (IQR) Duration followed by the ID service, median (IQR), days Outpatient ID follow-up scheduled with ID physician familiar with the patient
17 (25)
150 (86)
note. Data are no. (%) unless otherwise indicated. CoPAT, community-based parenteral antiinfective therapy; ID, infectious disease; IQR, interquartile range; SD, standard deviation.
This content downloaded on Wed, 26 Dec 2012 05:37:29 AM All use subject to JSTOR Terms and Conditions
antimicrobial stewardship at care transition
403
gure 1. Emergency department visit and rehospitalization reasons for patients in whom community-based parenteral anti-infective therapy was avoided.
ship programs have also been shown to produce cost savings.8 Expanding antimicrobial stewardship efforts to encompass antimicrobial evaluation at discharge from hospital would be expected to have still greater impact on overall appropriate antimicrobial use in society. It would be a huge and impractical undertaking for any facility to monitor each and every antimicrobial prescribed at the time of discharge from hospital. However, targeting higher-risk antimicrobial treatment plans is a reasonable goal. Parenteral antimicrobial therapy places patients at risk for both drug adverse effects and vascular access complications. Antimicrobial adverse effects have been reported to occur frequently in patients receiving parenteral antimicrobials at home, with the frequency of different adverse effects varying from 2% to 16% and vascular access complications varying from 9% to 11%.9 Antimicrobial stewardship programs do not have a direct reach in the community; thus, efforts to control parenteral antimicrobial therapy when patients are transitioning from hospital to community would target higher-risk antimicrobial treatment plans before patients leave the hospital. There are many factors that contribute to the success of the Cleveland Clinic CoPAT program. Expectation of ID review for every patient leaving the hospital on parenteral antimicrobial therapy is part of the organizational culture of the Cleveland Clinic. Postdischarge arrangements are made by case managers, whose standard work ow dictates the arrangement of postdischarge parenteral antibiotic therapy based on instructions in the CoPAT form (which can be signed electronically only by an ID attending physician). These conditions make it extremely unlikely that any patient can leave the hospital on parenteral antimicrobial therapy
without having been seen by an ID physician. There are no standard criteria for antimicrobial selection or duration. The ID physicians have the freedom to prescribe antimicrobials as they see t, and there is certainly practice variation among them. The philosophy of the program is that ID physicians are generally more likely to use antimicrobials appropriately than are non-ID physicians. The Cleveland Clinic culture of having all postdischarge parenteral antimicrobial therapy managed by ID physicians was built up and has been maintained by positioning the ID consultation as a service rather than a requirement. An ID consultation ensures that the patient will have continuity of care of his or her infectious illness across the transition from hospital to community, with a specied ID physician accepting responsibility. When a patient is discharged from the hospital, it is still possible for a physician to prescribe an oral antimicrobial other than what is recommended by an ID physician. In reality it rarely happens, because there is the appreciation that the ID recommendations are based on a full evaluation of the patient and the ID consultation ensures that there is an identied ID physician who can be held accountable if there are consequences of denial of antimicrobial therapy. There is no question that it requires commitment to deliver on this expectation, but our model of care demonstrates that it can be done. We believe that a mandatory ID consultation requirement at discharge for all patients leaving hospital on parenteral antimicrobials is a critical component of an effective antimicrobial stewardship strategy at this important care transition point. Not having a mandatory requirement is likely to be less effective. It has previously been shown that antimicrobial stewardship efforts were circumvented when cli-
This content downloaded on Wed, 26 Dec 2012 05:37:29 AM All use subject to JSTOR Terms and Conditions
404
infection control and hospital epidemiology
april 2012, vol. 33, no. 4
nicians had an option that allowed them to bypass the process.10 In summary, a policy of mandatory predischarge ID consultation for every patient anticipated to be discharged from hospital on parenteral antimicrobials serves as a safe and effective antimicrobial stewardship strategy by avoiding unnecessary antimicrobial use in a substantial number of patients at a critical transition of care in healthcare delivery.
acknowledgments
Potential conicts of interest. All authors report no conicts of interest relevant to this article. All authors submitted the ICMJE Form for Disclosure of Potential Conicts of Interest, and the conicts that the editors consider relevant to this article are disclosed here. Afliations: 1. Department of Infectious Disease, Cleveland Clinic, Cleveland, Ohio. Address correspondence to Nabin K. Shrestha, MD, MPH, 9500 Euclid Avenue/G-21, Cleveland, OH 44195 (shrestn@ccf.org). Presented in part: 21st Annual Meeting of the Society for Healthcare Epidemiology of America; Dallas, Texas; April 14, 2011 (Poster 86). Received September 28, 2011; accepted December 13, 2011; electronically published March 15, 2012. 2012 by The Society for Healthcare Epidemiology of America. All rights reserved. 0899-823X/2012/3304-0014$15.00. DOI: 10.1086/664758
references
1. Dellit TH, Owens RC, McGowan JE Jr, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 2007;44: 159177.
2. ASHP statement on the pharmacists role in antimicrobial stewardship and infection prevention and control. Am J Health-Syst Pharm 2010;67:575577. 3. Cusini A, Rampini SK, Bansal V, et al. Different patterns of inappropriate antimicrobial use in surgical and medical units at a tertiary care hospital in Switzerland: a prevalence survey. PLoS ONE 2010;5:e14011. 4. Camins BC, King MD, Wells JB, et al. Impact of an antimicrobial utilization program on antimicrobial use at a large teaching hospital: a randomized controlled trial. Infect Control Hosp Epidemiol 2009;30:931938. 5. Tice AD, Rehm SJ, Dalovisio JR, et al. Practice guidelines for outpatient parenteral antimicrobial therapy: IDSA guidelines. Clin Infect Dis 2004;38:16511672. 6. Gordon SM, Shrestha NK, Rehm SJ. Transitioning antimicrobial stewardship beyond the hospital: the Cleveland Clinics community-based parenteral anti-infective therapy (CoPAT) program. J Hosp Med 2011;6(suppl 1):S24S30. 7. Ohl CA, Dodds Ashley ES. Antimicrobial stewardship programs in community hospitals: the evidence base and case studies. Clin Infect Dis 2011;53(suppl 1):S23S28; quiz, S29S30. 8. Ruttimann S, Keck B, Hartmeier C, Maetzel A, Bucher HC. Long-term antibiotic cost savings from a comprehensive intervention program in a medical department of a university-afliated teaching hospital. Clin Infect Dis 2004;38:348356. 9. Hoffman-Terry ML, Fraimow HS, Fox TR, Swift BG, Wolf JE. Adverse effects of outpatient parenteral antibiotic therapy. Am J Med 1999;106:4449. 10. LaRosa LA, Fishman NO, Lautenbach E, Koppel RJ, Morales KH, Linkin DR. Evaluation of antimicrobial therapy orders circumventing an antimicrobial stewardship program: investigating the strategy of stealth dosing. Infect Control Hosp Epidemiol 2007;28:551556.
This content downloaded on Wed, 26 Dec 2012 05:37:29 AM All use subject to JSTOR Terms and Conditions
You might also like
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- TKT Module 1 Task Type 4 Introduction To Odd One Out Tasks PDFDocument9 pagesTKT Module 1 Task Type 4 Introduction To Odd One Out Tasks PDFRachel Maria RibeiroNo ratings yet
- The Learning Principle PRINTDocument5 pagesThe Learning Principle PRINTnurulNo ratings yet
- Sediment Gravity FlowDocument38 pagesSediment Gravity FlowkorewaNo ratings yet
- David Burlock LamoreauxDocument21 pagesDavid Burlock LamoreauxLeena RogersNo ratings yet
- Ma de 601Document4 pagesMa de 601hang tranNo ratings yet
- R.K. Anand Contempt Delhi HC JudgementDocument112 pagesR.K. Anand Contempt Delhi HC JudgementSampath BulusuNo ratings yet
- Russian Military Intervention in The Syrian Civil War PDFDocument62 pagesRussian Military Intervention in The Syrian Civil War PDFMendiburuFranciscoNo ratings yet
- Marciniak Barbara The PleiadiansDocument89 pagesMarciniak Barbara The Pleiadiansaman100% (3)
- Hot Mix Asphalt Overlay Splice: (Pavement Termination Detail)Document1 pageHot Mix Asphalt Overlay Splice: (Pavement Termination Detail)JUAN RULFONo ratings yet
- Workshop On Previewing - CECARDocument12 pagesWorkshop On Previewing - CECARestefaany tejada100% (2)
- Affiliate Marketing Step by StepDocument27 pagesAffiliate Marketing Step by StepJulia FawcettNo ratings yet
- Approach SlabDocument2 pagesApproach SlabMahmood Mufti100% (1)
- VMGODocument3 pagesVMGOklirt carayoNo ratings yet
- Lesson Plan Template 2017 7 3Document4 pagesLesson Plan Template 2017 7 3api-424474395No ratings yet
- Holy QURAN - Unicode Font EditionDocument462 pagesHoly QURAN - Unicode Font Editionalqudsulana8971% (7)
- Restful ApiDocument27 pagesRestful ApiBlank UserNo ratings yet
- IN Basket Exercise PDFDocument4 pagesIN Basket Exercise PDFSyed Salman ShahNo ratings yet
- Morocco Expat GuideDocument10 pagesMorocco Expat GuidefredNo ratings yet
- In The Star Schema DesignDocument11 pagesIn The Star Schema DesignppavandsNo ratings yet
- Vendor Document Cover SheetDocument11 pagesVendor Document Cover SheetSagar SawantNo ratings yet
- C C C !" # # $C% & #'C%Document12 pagesC C C !" # # $C% & #'C%Sneha ShahNo ratings yet
- 2021 Test3 Part5Document9 pages2021 Test3 Part5Sicut DilexiNo ratings yet
- Chapter 9 - Worksheet1finalDocument27 pagesChapter 9 - Worksheet1finalTansu Erin ŞarlakNo ratings yet
- Tong Hop Bai Tap Trac Nghiem Ve Cac Thi Trong Tieng AnhDocument7 pagesTong Hop Bai Tap Trac Nghiem Ve Cac Thi Trong Tieng Anhthanh truc bùiNo ratings yet
- August 30-Filling Out FormsDocument3 pagesAugust 30-Filling Out FormsJocelyn G. EmpinadoNo ratings yet
- Ritter Insurance Broker PresentationDocument10 pagesRitter Insurance Broker Presentationritter.roNo ratings yet
- God Only Knows Chords UkuleleDocument3 pagesGod Only Knows Chords UkuleleMark0% (1)
- Aspiration PneumoniaDocument3 pagesAspiration PneumoniaEllen Hennings100% (1)
- Paediatrica Indonesiana: Ari Kurniasih, Guslihan Dasa Tjipta, Muhammad Ali, Emil Azlin, Pertin SianturiDocument6 pagesPaediatrica Indonesiana: Ari Kurniasih, Guslihan Dasa Tjipta, Muhammad Ali, Emil Azlin, Pertin SianturiHarry FebryantoNo ratings yet
- Tutorial Week 10 (Group 2)Document4 pagesTutorial Week 10 (Group 2)Nuranis QhaleedaNo ratings yet