Professional Documents
Culture Documents
Text
Uploaded by
Putra ImanullahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Text
Uploaded by
Putra ImanullahCopyright:
Available Formats
Otorhinolaryngology Clinics: An International Journal, May-August 2012;4(2):71-76
71
Central Vertigo
AIJOC
REVIEW ARTICLE
Central Vertigo
Michael Strupp, Thomas Brandt
10.5005/jp-journals-10003-1089
ABSTRACT
Central vertigo can clinically manifest in three ways: Acute onset
of vertigo and dizziness, recurrent attacks and chronic central
vertigo. In patients with acute onset of symptoms it is essential
to differentiate between central and peripheral vertigo because
this has major diagnostic and therapeutic implications. A
differentiation can most often be achieved by a careful neuro-
ophthalmological and neuro-otological bedside examination.
One should look in particular for the following five signs of central
lesions: skew deviation/vertical divergence (as a component of
the ocular tilt reaction), gaze-evoked nystagmus contralateral
to a spontaneous nystagmus, saccadic smooth pursuit, acute
nystagmus in combination with a nonpathological head-impulse
test and central fixation nystagmus. The most frequent forms of
central vertigo with recurrent attacks are vestibular migraine
and episodic ataxia type 2. Clinically relevant types of chronic
or chronic progressive central vertigo are neurodegenerative
disorders affecting the cerebellum which are often associated
with cerebellar ocular motor dysfunction, in particular downbeat
nystagmus. Treatments of choice for a prophylactic therapy of
vestibular migraine are betablocker, topiramate or valproic acid.
A new treatment option for episodic ataxia type 2 and downbeat
nystagmus are aminopyridines (potassium channel blockers).
Keywords: Stroke, Multiple sclerosis, Ocular tilt reaction, Skew
deviation, Downbeat nystagmus, Unbeat nystagmus.
How to cite this article: Strupp M, Brandt T. Central Vertigo.
Otorhinolaryngol Clin Int J 2012;4(2):71-76.
Source of support: Nil
Conflict of interest: None declared
INTRODUCTION
From an anatomical point of view central vestibular forms
of vertigo can be caused by lesions along the central
vestibular pathways, which extend from the vestibular nuclei
in the medulla oblongata to the integration centers in the
rostral midbrain and to the ocular motor nuclei (via the
vestibulo-ocular reflex, VOR), and to the vestibulo-
cerebellum (flocculus, paraflocculus, vermis and nodulus),
the thalamus, and multisensory vestibular cortex areas in
the temporoparietal cortex.
6
From a clinical point of view
the most relevant anatomical structures for central vertigo
and dizziness are infratentorial areas, i.e. the brain stem,
the cerebellum and connecting pathways (Fig. 1). These
forms of vertigo are often clearly defined clinical syndromes,
such as Wallenbergs syndrome with typical ocular motor,
perceptual and postural manifestations that permit a precise
topographic diagnosis of brain stem lesions or cerebellar
lesions. The clinical examination of eye movements and of
nystagmus can also be helpful for localizing the lesion site.
7
The most relevant etiologies are ischemic lesions, multiple
sclerosis (MS) plaque or hemorrhage, for instance, due to
cavernomas.
Differential Diagnosis: Peripheral vs
Central Vestibular Vertigo
In the acute phase after the sudden occurrence of rotatory
vertigo the first question concerns the differential diagnosis:
Is it a peripheral or a central vestibular vertigo caused by
an acute stroke? In the latter case, specific diagnostics and
therapy must be performed without delay. A five-step
procedure to look for central vestibular or ocular motor
dysfunction is recommended:
8,20
Fig. 1: From a clinical point of view, central vertigo is most often caused by infratentorial lesions affecting the brainstem, the cerebellum
or connecting pathways (left). Most often central vestibular lesions are associated with central ocular motor dysfunction because the
vestibular and the ocular motor system use similar or adjacent nuclei and pathways
72
JAYPEE
Michael Strupp, Thomas Brandt
Skew deviation/vertical divergence (as part of the ocular
tilt reaction)
Gaze-evoked nystagmus contralateral to a spontaneous
nystagmus
Saccadic smooth pursuit
Nonpathological head-impulse test in patients with an
acute nystagmus,
Central fixation nystagmus (which contrary to peripheral
vestibular spontaneous nystagmus is not suppressed by
visual fixation).
The presence of a skew deviation/vertical divergence, a
gaze-evoked nystagmus in the opposite direction to that of
a spontaneous nystagmus, saccadic smooth pursuit, a normal
head-impulse test in a patient with acute vertigo and
nystagmus,
24
and a fixation nystagmus indicate a lesion of
the brain stem (in particular a vestibular pseudoneuritis,
Fig. 2), or more seldom a lesion of the cerebellum. However,
one has to point out that a central lesion is possible if the
head-impulse test is pathological. This 5-step procedure
yields a sensitivity of more than 95% for evidence of a
central lesion; this sensitivity is higher than that possible
with an early magnetic resonance imaging (MRI) with
diffusion-weighted sequences (88%).
20
Central Vestibular Anatomical Structures
The most important structures in central vestibular forms
of vertigo are the neuronal pathways mediating the VOR.
They travel from the peripheral labyrinth over the vestibular
nuclei in the medullary brain stem to the ocular motor nuclei
(III, IV, VI) and the supranuclear integration centers in the
pons and midbrain (interstitial nucleus of Cajal, INC; and
rostral interstitial nucleus of the medial longitudinal fascicle,
riMLF).
4,7
Ascending pathways travel contralaterally and
ipsilaterally
32
over the posterolateral thalamus up to a
network of vestibular areas in the parietotemporal cortex
and the insula, e.g. the parietoinsular vestibular cortex
(PIVC), areas in the superior temporal gyrus, and inferior
parietal lobes, which are, e.g. responsible for perception.
4
Descending pathways lead from the vestibular nuclei along
the medial and lateral vestibulospinal tract into the spinal
cord to mediate postural control. In addition, there are
numerous pathways to the vestibulocerebellum.
Etiology
Central vestibular syndromes are most often the result of
lesions of these pathways or of core areas caused by
infarction, hemorrhage (in particular due to canvernomas)
multiple sclerosis (MS) plaques, for instance in the root entry
zone of the 8th cranial nerve (Fig. 2) or rarely tumors. More
seldom are pathological stimuli as occur in paroxysmal brain
stem attacks (with ataxia and dysarthria) in MS or lacunar
infarctions. Vestibular epilepsy is even rarer.
Central Vestibular Syndromes
To differentiate central vestibular forms of vertigo from
other forms, it is helpful to refer to how long the symptoms
last:
Short rotatory or postural vertigo attacks lasting seconds
to minutes or for a few hours are caused by transient
ischemic attacks within the vertebrobasilar territory,
vestibular migraine, paroxysmal brain stem attacks with
ataxia/dysarthria in MS, and the rare vestibular epilepsy.
Attacks of rotatory or postural vertigo lasting hours to
several days, generally with additional brain stem
deficits, can be caused by an infarction, hemorrhage or
MS plaques in the brain stem and/or vestibule-
cerebellum, seldom by a long-lasting attack of vestibular
migraine.
Persisting postural imbalance and dizziness, combined
with a tendency to fall, is usually caused by permanent
damage to the brain stem or the cerebellum bilaterally,
e.g. downbeat nystagmus syndrome due to impaired
function of the flocculus/paraflocculus or most often
transient in upbeat nystagmus syndrome due to
paramedian pontomedullary or pontomesencephalic
damage (infarction, hemorrhage, tumor, intoxication).
Central Vestibular Syndromes in the
three Planes of Action of the VOR
Based on the functional anatomy central vestibular
syndromes can be classified into three different forms
depending on the plane: Sagittal (pitch) plane, vertical (roll)
plane and horizontal (yaw) plane. The clinical findings
correlate with this classification. For instance, impaired
Fig. 2: Magnetic resonance image of a patient with vestibular
pseudoneuritis, a disorder of the vestibulo-ocular reflex in the yaw
plane. The T2-weighted shows an MS plaque in the root entry zone
of the eighth cranial nerve on the right side
Otorhinolaryngology Clinics: An International Journal, May-August 2012;4(2):71-76
73
Central Vertigo
AIJOC
function in the pitch plane is characterized by a vertical
down- or upbeat nystagmus, in the roll plane by an ocular
tilt reaction and yaw plane by pure horizontal nystagmus.
Vestibular Syndromes in the
Sagittal (Pitch) Plane
Vestibular syndromes in the sagittal (pitch) plane are
characterized by a vertical nystagmus, i.e. a downbeat or
an upbeat nystagmus. They have so far been attributed to
lesions in the following places: paramedian bilaterally in
the medullary and pontomedullary brain stem, the ponto-
mesencephalic brain stem with the adjacent cerebellar
peduncle, in the paramedian pons, or the cerebellar
flocculus/paraflocculus bilaterally.
23
Despite the numerous
clinical studies performed on upbeat and downbeat
nystagmus as well as the many hypotheses proposed to
explain their pathomechanism, so far the pathophysiology
of the disorders has not been clarified.
25
Downbeat Nystagmus
The downbeat nystagmus (DBN) syndrome is a fixation
nystagmus that beats downward in primary gaze position,
is exacerbated on lateral gaze and in head-hanging position,
and can have a rotatory component. It is the most frequently
acquired fixation nystagmus and is accompanied by a
combination of visual and vestibulocerebellar ataxia with a
tendency to fall backward, past-pointing upward and a
disturbance of vertical gaze pursuit.
23
DBN is often
associated with other oculomotor, cerebellar, and vestibular
disorders, e.g. gaze pursuit, OKN or the visual suppression
of the VOR. The intensity of idiopathic DBN is dependent
on head positionit is less in upright than in supine or prone
positionsand on the time of dayit is stronger in the
morning than at noon or in the afternoon.
26
The syndrome
is frequently persistent.
There seem to be various forms of DBN with different
degrees of disturbance. Various mechanisms are currently
under discussion, in particular, an impairment of the vertical
gaze-pursuit system with spontaneous upward drift. Here
the flocculus/paraflocculus seems to play a special role,
since its damage leads to a disinhibition of the vestibular
pathways of the superior vestibular nucleus to the
oculomotor nucleus. This fits with findings from functional
imaging studies that have proven that patients with
idiopathic downbeat nystagmus have a hypometabolism or
a reduced activity in the flocculus/paraflocculus as well as
in the pontomedullary brain stem (Figs 3A to D).
15,16
In
contrast, structural MRI found atrophies of the gray matter
not in the flocculus/paraflocculus but in the lateral portions
of the cerebellar hemispheres (lobule VI) and in the
oculomotor vermis.
15
As mentioned above DBN is often caused by a bilaterally
impaired function of the flocculus/paraflocculus
16
often
associated with an atrophy of the cerebellum, rarely due to
drugs, in particular anticonvulsant. It is even more rarely
induced by a lesion on the floor of the fourth ventricle.
Accordingly idiopathic cases occur most often (38%),
degenerative disorders of the cerebellum in 20% of cases,
vascular lesions in 9%, malformations in 7%; the more
seldom causes like toxic drug damage, lesions in MS and
paraneoplastic syndromes, vestibular migraine, vitamin B
12
deficiency or traumatic and hypoxic injuries occur in
decreasing frequency.
31
It can, however, also be caused,
but more seldom, by a paramedian lesion of the medulla
oblongata, for example, in MS, hemorrhage, infarction or
tumor.
There are two subgroups of the idiopathic form of DBN:
one with clear cerebellar signs without cerebellar pathology
in MRI and the other a combination with bilateral vestibulo-
pathy, peripheral polyneuropathy, or a cerebellar syndrome,
suggesting a multisystem degeneration. In 89% of patients
with CANVAS syndrome (cerebellar ataxia with neuropathy
and bilateral vestibular areflexia syndrome) a circumscribed
atrophy of the cerebellum of the anterior and dorsal vermis
and crus I was seen in MRI.
22,29
Upbeat Nystagmus
Upbeat nystagmus (UBN) is rarer than DBN. It is also a
fixation-induced jerk nystagmus that beats upward in
Figs 3A to D: Functional MRI in patients with downbeat nystagmus.
A reduction of the activations in the flocculus on both sides was
also observed in patients with downbeat nystagmus during vertical
gaze pursuit movements (Kalla et al, 2006)
74
JAYPEE
Michael Strupp, Thomas Brandt
primary gaze position, is partially dependent on position, and
is combined with a disorder of the vertical smooth-pursuit
eye movements, a visual and vestibulospinal ataxia with a
tendency to fall backward, and past-pointing downward. On
the one hand, the pathoanatomical location of most acute
lesions is paramedian in the medulla oblongata, in neurons
of the paramedian tract, close to the caudal part of the
perihypoglossal nucleus, which is responsible for vertical
gaze-holding.
25
On the other, lesions have been reported to
be paramedian in the tegmentum of the pontomesencephalic
junction, the brachium conjunctivum and probably in the
anterior vermis. The symptoms persist as a rule for several
weeks but are not permanent. Because the eye movements
generally have larger amplitudes, oscillopsia in upbeat
nystagmus is very distressing and impairs vision. UBN due
to damage of the pontomesencephalic brain stem is frequently
combinedespecially in MS patientswith a unilateral or
bilateral internuclear ophthalmoplegia (INO), indicating that
the MLF is affected. The main etiologies are bilateral lesions
in MS, brain stem ischemia or tumor, Wernickes
encephalopathy, cerebellar degeneration and dysfunction of
the cerebellum due to intoxication.
Therapy for DBN and UBN
It is therapeutically expedient to try to treat the symptoms
of persisting downbeat nystagmus with various drugs.
28
In the last years the potassium channel blockers 3,4-
diaminopyridine and 4-aminopyridine have been proven
to have a positive effect, above all in DBN (Figs 4A to E)
and also in single cases of UBN.
14,17,18,27,30
Since
4-aminopyridine is more effection than 3, 4-diaminopyri-
dine, 4-aminopyridine is nowadays preferred.
19
4-aminopyridine can intensify the Purkinje cell activity
13
and thus improve the reduced inhibiting influence of the
cerebellum on vertical eye movements. Since epileptic
attacks or heart rhythm disordersespecially at higher
dosages-can occur, an electrocardiogram (EKG) should
be performed before and ca. 30 minutes after the first
ingestion of 5 mg 4-aminopyridine in order to detect early
any lengthening of the QT interval.
27
The standard dosage
is 5 mg tid. The sustained-release form of 4-aminopyridine
(Fampyra TM) is also effective.
Since generally UBN slowly resolves after an acute
occurrence, therapy for its symptoms is often not
Figs 4A to E: Effect of 3,4-diaminopyridine (3,4-DAP) on downbeat nystagmus (DBN). Influence of 3,4-DAP on the average velocity of
the slow phase of DBN (measured by 2D-videography). The figures (A to D) show the average velocity of the slow phase of DBN for each
patient. (A) Controls vs 3,4-DAP; (C) controls vs placebo. Both groups (B) and (D) show a so-called box plot with average, median and
50% percentile values as well as the standard deviation for the controls vs 3,4-DAP (B) and controls vs placebo (D). 3,4-DAP reduced the
maximal velocity of the slow phase of DBN from 7.2/s to 3.1/s 30 mins after ingestion of 20 mg 3,4-DAP (p < 0.001). In (E) is an original
recording of the vertical eye positions before and 30 mins after ingestion of the medication [from (Strupp et al, 2003)]. Since
4-aminopyridine is more effective than 3,4-diaminopyridine nowadays 4-aminopyridine is preferred
Otorhinolaryngology Clinics: An International Journal, May-August 2012;4(2):71-76
75
Central Vertigo
AIJOC
necessary. In cases of very disturbing oscillopsias due to
large amplitudes of the nystagmus or longer duration one
can try 4-aminopyridine (3 5 mg/d orally)
14
or memantine
(2 10 mg/d orally). If both are ineffective, one can try
baclofen (2 5 mg/d orally).
1
Vestibular Syndromes in the
Vertical (Roll) Plane
These syndromes indicate an acute unilateral deficit of the
graviceptive vestibular pathways, which run from the
vertical canals and otoliths in the brain stem over the
ipsilateral (medial and superior) vestibular nuclei and the
contralateral MLF to the ocular motor nuclei and integration
centers for vertical and torsional eye movements (INC and
riMLF) in the rostral midbrain.
4
Unilateral lesions of the
vestibulocerebellar structures (e.g. the uvula, nodulus,
dentate nucleus) can also induce signs in the roll plane.
2
More rostral to the midbrain, only the vestibular projection
of the VOR for perception in the roll plane (determination
of the subjective visual vertical, SVV) runs over the
vestibular nuclei, the posterolateral thalamus
12
to the
parietoinsular vestibular cortex in the posterior insula.
5
The
crossing of these pathways at pontine level is especially
important for topographic diagnosis of the brain stem. All
signs of lesions in the roll planesingle components or a
complete ocular tilt reaction (i.e. head tilt, vertical
divergence of the eyes, ocular torsion, SVV deviation)
exhibit an ipsiversive tilt (ipsilateral eye lowermost) in cases
of a pontomedullary lesion (medial and superior vestibular
nuclei) below the decussation in the brain stem. All signs
in the roll plane perceptual and posturalexhibit
contraversive deviations (contralateral eye lowermost) in
cases of unilateral pontomesencephalic lesions of the brain
stem above the decussation and indicate a deficit of the MLF
or of the supranuclear center of the INC. Perceptual deficits
in the sense of pathological deviations of the SVV occur
during unilateral deficits along the entire VOR projection
and of the vestibulocerebellum. They are one of the most
sensitive signs of acute brain stem lesions (in ca. 90% of
cases of acute unilateral infarctions).
11
Deviation of the SVV
in the acute phase is more pronounced in patients with
lesions of the vestibular nuclei (Wallenbergs syndrome)
than in patients with vestibular neuritis; this means an
average of 9.8 as opposed to 7.
9
The remission of the
perceptual deficits over a period of ca. 2 to 4 weeks is very
similar in both diseases.
The etiology of these unilateral lesions is frequently an
infarction of the brain stem, or the paramedian thalamus as
well as hemorrhages, which extend into the rostral
midbrain.
11
The course and prognosis depend also here on
the etiology of the underlying illness. In the frequent
ischemias a significant and generally complete recovery
from the symptoms in the roll plane can be expected within
days to weeks due to central compensation over the opposite
side.
9,10
Vestibular Syndromes in the
Horizontal (Yaw) Plane
Vestibular syndromes in the horizontal (yaw) plane with a
pure horizontal nystagmus are rare. They can be caused by
horizontal canal benign paroxysmal positioning vertigo.
3
Central syndromes in yaw are most often due to lesions in
the area of the root entry zone of the vestibular nerve into
the medulla oblongata, the medial and/or superior vestibular
nuclei, and the integration centers for horizontal eye
movements (nucleus praepositus hypoglossi). Other clinical
signs are ipsilateral caloric hyporesponsiveness, horizontal
gaze deviation, a tendency to fall to the affected side, and a
past-pointing corresponding to a deviation of the subjective
straight-ahead. The clinical symptoms are similar to those
of an acute peripheral vestibular lesion as occurs in
vestibular neuritis and thus is also called vestibular
pseudoneuritis. In most cases, however, there is a horizontal
rotatory nystagmus. A purely central yaw plane syndrome
is rare, because the area of a lesion that can theoretically
cause a pure tonus imbalance in the yaw plane adjoins and
in part overlaps with structures in the vestibular nuclei,
which are also responsible for vestibular function in the
roll plane. For this reason mixed patterns are found more
frequently. Thus, skew deviation is the only sensitive, but
not specific sign that indicates a vestibular pseudoneuritis
as opposed to vestibular neuritis.
8
Further, the horizontal
head-impulse test also does not allow a clear differentiation
between neuritis and pseudoneuritis: 9% of patients with a
pontocerebellar infarction have a positive test as well.
24
The most common causes include ischemic infarctions
or MS plaques (Fig. 2) within the vestibular nuclei or
fascicles.
21
If the lesion extends beyond the vestibular nuclei,
other accompanying brain stem symptoms can be detected.
Since, a unilateral medullary ischemic or inflammatory brain
stem lesion is mostly present, the prognosis is favorable
because central compensation takes place over the opposite
side. The symptoms can be expected to resolve slowly within
days to weeks. Thus, central compensation can be promoted
by early balance training together with the simultaneous
treatment of the underlying illness.
REFERENCES
1. Averbuch-Heller L, Tusa RJ, Fuhry L, Rottach KG, Ganser GL,
Heide W, et al. A double-blind controlled study of gabapentin
and baclofen as treatment for acquired nystagmus. Ann Neurol
1997;41:818-25.
76
JAYPEE
Michael Strupp, Thomas Brandt
2. Baier B, Bense S, Dieterich M. Are signs of ocular tilt reaction
in patients with cerebellar lesions mediated by the dentate
nucleus? Brain 2008;131:1445-54.
3. Baloh RW, Jacobsen K, Honrubia V. Horizontal semicircular
canal variant of benign positional vertigo. Neurology
1993;43:2542-49.
4. Brandt T, Dieterich M. Vestibular syndromes in the roll plane:
Topographic diagnosis from brain stem to cortex. Ann Neurol
1994;36:337-47.
5. Brandt T, Dieterich M, Danek A. Vestibular cortex lesions affect
the perception of verticality [see comments]. Ann Neurol
1994;35:403-12.
6. Brandt T, Dieterich M, Strupp M. Vertigo and dizziness -
common complaints. London: Springer 2012.
7. Buttner-Ennever JA. Mapping the oculomotor system. Prog
Brain Res 2008;171:3-11.
8. Cnyrim CD, Newman-Toker D, Karch C, Brandt T, Strupp M.
Bedside differentiation of vestibular neuritis from central
vestibular pseudoneuritis. J Neurol Neurosurg Psychiatry
2008;79:458-60.
9. Cnyrim CD, Rettinger N, Mansmann U, Brandt T, Strupp M.
Central compensation of deviated subjective visual vertical in
Wallenbergs syndrome. J Neurol Neurosurg Psychiatry
2007;78:527-28.
10. Dieterich M, Brandt T. Wallenbergs syndrome: Lateropulsion,
cyclorotation and subjective visual vertical in thirty-six patients.
Ann Neurol 1992;31:399-408.
11. Dieterich M, Brandt T. Ocular torsion and tilt of subjective visual
vertical are sensitive brainstem signs. Ann Neurol 1993a;33:
292-99.
12. Dieterich M, Brandt T. Thalamic infarctions: Differential effects
on vestibular function in the roll plane (35 patients). Neurology
1993b;43:1732-40.
13. Etzion Y, Grossman Y. Highly 4-aminopyridine sensitive
delayed rectifier current modulates the excitability of guinea
pig cerebellar Purkinje cells. Exp Brain Res 2001;139:419-25.
14. Glasauer S, Kalla R, Buttner U, Strupp M, Brandt T. 4-
aminopyridine restores visual ocular motor function in upbeat
nystagmus. J Neurol Neurosurg Psychiatry 2005;76:451-53.
15. Hufner K, Stephan T, Kalla R, Deutschlander A, Wagner J,
Holtmannspotter M et al. Structural and functional MRIs disclose
cerebellar pathologies in idiopathic downbeat nystagmus.
Neurology 2007;69:1128-1135.
16. Kalla R, Deutschlander A, Hufner K, Stephan T, Jahn K,
Glasauer S, et al. Detection of floccular hypometabolism in
downbeat nystagmus by fMRI. Neurology 2006;66:281-83.
17. Kalla R, Glasauer S, Buttner U, Brandt T, Strupp M. 4-
aminopyridine restores vertical and horizontal neural integrator
function in downbeat nystagmus. Brain 2007;130:2441-51.
18. Kalla R, Glasauer S, Schautzer F, Lehnen N, Buttner U, Strupp
M, Brandt T. 4-aminopyridine improves downbeat nystagmus,
smooth pursuit and VOR gain. Neurology 2004;62:1228-29.
19. Kalla R, Spiegel R, Claassen J, Bardins S, Hahn A, Schneider E,
et al. Comparison of 10-mg doses of 4-aminopyridine and 3,4-
diaminopyridine for the treatment of downbeat nystagmus. J
Neuroophthalmol 2011;31:320-25.
20. Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker
DE. HINTS to diagnose stroke in the acute vestibular syndrome:
Three-step bedside oculomotor examination more sensitive than
early MRI diffusion-weighted imaging. Stroke 2009;40:
3504-10.
21. Kim HA, Lee H. Isolated vestibular nucleus infarction
mimicking acute peripheral vestibulopathy. Stroke 2010;41:
1558-60.
22. Kirchner H, Kremmyda O, Hufner K, Stephan T, Zingler V,
Brandt T, et al. Clinical, electrophysiological, and MRI findings
in patients with cerebellar ataxia and a bilaterally pathological
head-impulse test. Ann NY Acad Sci 2011;1233:127-38.
23. Leigh RJ, Zee D. The neurology of eye movements. Oxford,
New York: Oxford University Press 2006.
24. Newman-Toker DE, Kattah JC, Alvernia JE, Wang DZ. Normal
head impulse test differentiates acute cerebellar strokes from
vestibular neuritis. Neurology 2008;70:2378-85.
25. Pierrot-Deseilligny C, Milea D. Vertical nystagmus: clinical
facts and hypotheses. Brain 2005;128:1237-46.
26. Spiegel R, Rettinger N, Kalla R, Lehnen N, Straumann D,
Brandt T, et al. The intensity of downbeat nystagmus during
daytime. Ann NY Acad Sci 2009;1164:293-99.
27. Strupp M, Schuler O, Krafczyk S, Jahn K, Schautzer F, Buttner
U, Brandt T. Treatment of downbeat nystagmus with 3,4-
diaminopyridine: A placebocontrolled study. Neurology
2003;61:165-70.
28. Strupp M, Thurtell MJ, Shaikh AG, Brandt T, Zee DS, Leigh
RJ. Pharmacotherapy of vestibular and ocular motor disorders,
including nystagmus. J Neurol 2011;258:1207-22.
29. Szmulewicz DJ, Waterston JA, Halmagyi GM, Mossman S,
Chancellor AM, Mclean CA, Storey E. Sensory neuropathy as
part of the cerebellar ataxia neuropathy vestibular areflexia
syndrome. Neurology 2011;76:1903-10.
30. Tsunemi T, Ishikawa K, Tsukui K, Sumi T, Kitamura K,
Mizusawa H. The effect of 3,4-diaminopyridine on the patients
with hereditary pure cerebellar ataxia. J Neurol Sci 2010;292:
81-84.
31. Wagner JN, Glaser M, Brandt T, Strupp M. Downbeat
nystagmus: Aetiology and comorbidity in 117 patients. J Neurol
Neurosurg Psychiatry 2008;79:672-77.
32. Zwergal A, Buttner-Ennever J, Brandt T, Strupp M. An
ipsilateral vestibulothalamic tract adjacent to the medial
lemniscus in humans. Brain 2008;131:2928-35.
ABOUT THE AUTHORS
Michael Strupp (Corresponding Author)
Professor, Depart ment of Neurology and Clinical Neuro-
physiology, German Dizziness Center, University Hospital
Munich, Campus Grosshadern, Marchioninistrasse 15, 81377
Munich, Germany, e-mail: michael.strupp@med.uni-muenchen.de
Thomas Brandt
Professor, Department of Neurology, Institute of Clinical Neuroscience
German Dizziness Center, University Hospital Munich, Campus
Grosshadern, Marchioninistrasse 15, 81377 Munich, Germany
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- ApptermDocument5 pagesApptermPutra ImanullahNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Palmoplantar PustulosisDocument6 pagesPalmoplantar PustulosisputraimanullahNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- WHOenlguideDocument2 pagesWHOenlguideOctoNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- A Comparative Study of Total Quality Management of Health Care System in India and Iran - 2011Document5 pagesA Comparative Study of Total Quality Management of Health Care System in India and Iran - 2011Putra ImanullahNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Pustular Diseases: Laboratory Findings, DiagnosisDocument4 pagesPustular Diseases: Laboratory Findings, DiagnosisPutra ImanullahNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Journal Public HealthDocument30 pagesJournal Public HealthPutra ImanullahNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
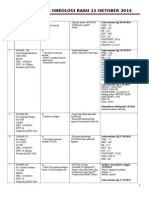
- Koran Bedah Onkologi 15 OktoberDocument2 pagesKoran Bedah Onkologi 15 OktoberPutra ImanullahNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- (Kop Surat AMSA Universitas) : Letter of Recommendation Candidates For Executive Board of AMSA Indonesia 2012-2013Document1 page(Kop Surat AMSA Universitas) : Letter of Recommendation Candidates For Executive Board of AMSA Indonesia 2012-2013Putra ImanullahNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Vertigo: A Review of Common Peripheral and Central Vestibular DisordersDocument7 pagesVertigo: A Review of Common Peripheral and Central Vestibular DisordersPutra ImanullahNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- WHOenlguideDocument2 pagesWHOenlguideOctoNo ratings yet
- Sepsis 1Document18 pagesSepsis 1Putra ImanullahNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Document6 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 15000)Putra ImanullahNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Case 5 Concept MappingDocument1 pageCase 5 Concept MappingPutra ImanullahNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Community Outreach TeamDocument3 pagesCommunity Outreach TeamRio Indra PrajaNo ratings yet
- EAMSC2013 Updates 1130 PDFDocument2 pagesEAMSC2013 Updates 1130 PDFPutra ImanullahNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- EAMSC2013 Updates 1130 PDFDocument2 pagesEAMSC2013 Updates 1130 PDFPutra ImanullahNo ratings yet
- Medel SonataDocument54 pagesMedel Sonatamaclab macNo ratings yet
- Secondary SurveyDocument2 pagesSecondary SurveySakta SuryagunaNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Pharyngeal ReflexDocument3 pagesPharyngeal ReflexAyra Nakrish AlvarezNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- HBSE 3303 Dysarthria & ApraxiaDocument4 pagesHBSE 3303 Dysarthria & ApraxiasohaimimohdyusoffNo ratings yet
- 47 Case ReportDocument4 pages47 Case Reportsusanti bulanNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Cerebrovascular Accident CVADocument8 pagesCerebrovascular Accident CVAFlora Angeli PastoresNo ratings yet
- Ulcerative Colitis 1. Chief ComplaintDocument5 pagesUlcerative Colitis 1. Chief Complaintdrnareshkumar3281No ratings yet
- Anticoagulants 2019Document11 pagesAnticoagulants 2019Srijan VermaNo ratings yet
- Pediatric Case StudyDocument29 pagesPediatric Case Studyapi-296281683No ratings yet
- 02 Full Crown PreparationDocument35 pages02 Full Crown PreparationSurgaBetariJelita100% (1)
- Nurs FPX 4010 Assessment 2 Interview and Interdisciplinary Issue IdentificationDocument4 pagesNurs FPX 4010 Assessment 2 Interview and Interdisciplinary Issue Identificationfarwaamjad771No ratings yet
- Management During Labor of Multiple Pregnancy: Manish Gupta Roll No-47Document10 pagesManagement During Labor of Multiple Pregnancy: Manish Gupta Roll No-47manishNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Fundamentals of Nursing Exam 2Document23 pagesFundamentals of Nursing Exam 2eka100% (2)
- The Nursing Assessment Cheat Sheet (ADPIE)Document3 pagesThe Nursing Assessment Cheat Sheet (ADPIE)ajaz100% (1)
- Anatomy of The Human Airways. Lymph Node Stations and InterventionalDocument6 pagesAnatomy of The Human Airways. Lymph Node Stations and Interventionalandika pradanaNo ratings yet
- Death CertificateDocument16 pagesDeath CertificateWisnu Agung WiyanggaNo ratings yet
- Monitoring & Care of Ventilated ChildrenDocument12 pagesMonitoring & Care of Ventilated ChildrenRajakumar Padur Sivaraman100% (2)
- Padma (2021) A Comparative Study To Assess The Level of Patient Satisfaction On Quality of Nursing Care Among Parturients Admitted in Government and Private Hospitals at Lucknow.Document12 pagesPadma (2021) A Comparative Study To Assess The Level of Patient Satisfaction On Quality of Nursing Care Among Parturients Admitted in Government and Private Hospitals at Lucknow.Diego RiveraNo ratings yet
- Koo Quay Keong V Ooi Peng Jin London Lucien (2016) 5 SLR 0130Document16 pagesKoo Quay Keong V Ooi Peng Jin London Lucien (2016) 5 SLR 0130a b cNo ratings yet
- Celecoxib & Ketoprofen For Pain ManagementDocument8 pagesCelecoxib & Ketoprofen For Pain ManagementUbaidillah AfiffNo ratings yet
- Guidance On Recording of Interventions: The SocietyDocument2 pagesGuidance On Recording of Interventions: The SocietyRaju NiraulaNo ratings yet
- Performance of PRISM III and PELOD-2 Score in A PICUDocument6 pagesPerformance of PRISM III and PELOD-2 Score in A PICUAnantaBenvenutoNo ratings yet
- Treatment Aspects in Perioperative NursingDocument51 pagesTreatment Aspects in Perioperative NursingShibin Jacob100% (2)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- NCP Acute PainDocument2 pagesNCP Acute PainNecheal BaayNo ratings yet
- Insulin Adjustment Workbook CompleteDocument53 pagesInsulin Adjustment Workbook CompleteDiabestes-stuff100% (1)
- The Finnish Open Dialogue Approach To PDFDocument8 pagesThe Finnish Open Dialogue Approach To PDFJoão Vitor Moreira MaiaNo ratings yet
- NCP Proper TahbsoDocument3 pagesNCP Proper TahbsoMiriam EstradaNo ratings yet
- Operations Manual: Gynnie® OB/GYN StretcherDocument234 pagesOperations Manual: Gynnie® OB/GYN StretcheroyanedelmacarenaNo ratings yet
- Lista e Librave MjekesoreDocument4 pagesLista e Librave MjekesoreEmily OwenNo ratings yet
- Nur 129 Exam 2Document4 pagesNur 129 Exam 2Stephanie DuvergeNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (28)