Professional Documents
Culture Documents
Renal Regulation of Potassium Balance
Uploaded by
Sam TagardaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Renal Regulation of Potassium Balance
Uploaded by
Sam TagardaCopyright:
Available Formats
Renal Regulation of Potassium Balance Potassium found mostly in intracellular fluid, only 2% in extracellular fluid (closely monitored) 2/3
/3 of body fluid intracellular- collective cytosolic volume of all cells -140-150 mEq/L cytosolic K concentration 1/3 extracellular fluid -Normal: 4 mEq/L K concentration
Resting membrane potentials of nerve and muscle tissues are strongly influenced by the ratio of intracellular to extracellular potassium concentration. Increase extracellular potassium concentration depolarizes the resting membrane potential Decrease extracellular potassium concentration hyperpolarizes cell membranes REGULATION OF POTASSIUM BETWEEN THE INTRACELLULAR AND EXTRACELLULAR COMPARTMENTS Factors that affect extracellular potassium concentration: the total amount of potassium in the body excretion of an amount of urinary potassium equal to the amount of potassium ingested minus the small amounts eliminated in the feces and sweat the distribution of this potassium between the extracellular and intracellular fluid compartments.
RENAL POTASSIUM HANDLING The control of renal function is the major mechanism by which total-body potassium is maintained in balance. Potassium is freely filtered into Bowmans space. 90% is reabsorbed by the proximal tubule and thick ascending limb of the loop of Henle Conserve K - reabsorbed in the distal nephron and medullary collecting duct Body gets rid of K - large amount is secreted in the distal nephron The chief means of regulation lies in control over secretion in parts of the nephron beyond the loop of Henle Proximal Tubule 65% of K reabsorbed unregulated Via: concentration gradient set up when water is reabsorbed & by entrainment with the rapidly reabsorbed water (solvent drag). Thick ascending limb K enter in both membranes actively
1. K pumped into the epithelial cells from the tubular lumen with sodium via Na-K- 2Cl antiporters 2. K from the interstitium via the Na-K-ATPase K exit passively less K than sodium in the lumen, K recycled for multiporter to work
Secretion in the Distal Nephron and its Regulation Principal Cells secrete K - uptake of potassium from the interstitium via the Na-K-ATPase
ROMK (Renal outer medulla) BK (big) Low dietary loads of potassium, there is virtually no secretion on both channels Normal K load - ROMK channels are moved to the luminal membrane and secrete potassium. BK channels-close High excretion rate: both types of channel are present in the luminal membrane secreting potassium
Intercalated Cells (type A)- reabsorb K- reabsorb potassium via the H-K-ATPase in the luminal membrane, which actively takes up potassiumfrom the lumen and then allows potassium to enter the interstitium across the basolateral membrane via potassium channels
Effects of Diuretics Diuretics are agents that increase urine volume and reduce ECF volume. Effects: Increase Na and H20 excretion Side Effect: Increase K excretion Osmotic Diuresis - high filtration of solute that is not reabsorbed) or treatment with diuretics that block sodium reabsorption in the proximal tubule, loop of Henle, or distal convoluted tubule Potassium reabsorption in the proximal tubule and Henles loop is linked to sodium reabsorption diuretics that act on these sites inhibit sodium and potassium reabsorption Decreased Reabsorption of Na & K volume of fluid flowing to the distal nephron per unit Time increased potassium secretion and, hence, excretion Weak Diuretics K sparing Effects of Acid-Base Changes on Potassium Excretion Alkalosis: hypokalemia (low plasma potassium concentration) Acidosis: hyperkalemia Reason of effects: Elevations and depressions in the extracellular concentration of hydrogen ions lead to a de facto exchange of these ions with cellular cations (K)
Low intracellular pH inhibits pumps including Na-K-ATPase and potassium channel activity; high intracellular pH reverses these effects and relieves this inhibition (effectively stimulating the pump and the potassium channels)
You might also like
- Module 2 - Connective Tissue CellsDocument12 pagesModule 2 - Connective Tissue CellsSam TagardaNo ratings yet
- Module 2 - MPS Cells Location and FunctionsDocument35 pagesModule 2 - MPS Cells Location and FunctionsSam TagardaNo ratings yet
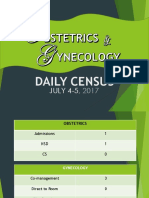
- DAILY CENSUS REPORT FOR OBSTETRICS AND GYNECOLOGY DEPARTMENTS JULY 4-5, 2017Document22 pagesDAILY CENSUS REPORT FOR OBSTETRICS AND GYNECOLOGY DEPARTMENTS JULY 4-5, 2017Sam TagardaNo ratings yet
- Module 36 Concept MapDocument1 pageModule 36 Concept MapSam TagardaNo ratings yet
- MODULE 30 - (Development of The Nervous Sytem)Document7 pagesMODULE 30 - (Development of The Nervous Sytem)Sam TagardaNo ratings yet
- Module 1 - TonicityDocument1 pageModule 1 - TonicitySam TagardaNo ratings yet
- Module 2 - Basal Lamina, Cell Polarity, Cell RenewalDocument21 pagesModule 2 - Basal Lamina, Cell Polarity, Cell RenewalSam TagardaNo ratings yet
- Module 35Document21 pagesModule 35Sam TagardaNo ratings yet
- Bien PhysicsDocument5 pagesBien PhysicsSam TagardaNo ratings yet
- Anti-Streptolysin ODocument48 pagesAnti-Streptolysin OSam TagardaNo ratings yet
- Electrolytes (4 Email)Document51 pagesElectrolytes (4 Email)Sam TagardaNo ratings yet
- Trace ElementsDocument18 pagesTrace ElementsSam TagardaNo ratings yet
- BacteriologyDocument3 pagesBacteriologySam TagardaNo ratings yet
- Module 36Document6 pagesModule 36Sam TagardaNo ratings yet
- 04 Lecture PPTDocument46 pages04 Lecture PPTSam TagardaNo ratings yet
- Blood GasesDocument41 pagesBlood GasesSam TagardaNo ratings yet
- Muscular triangles of the neckDocument3 pagesMuscular triangles of the neckSam TagardaNo ratings yet
- 7.20 Reflex MechanismDocument2 pages7.20 Reflex MechanismSam TagardaNo ratings yet
- HPIDocument1 pageHPISam TagardaNo ratings yet
- Spinal CordDocument5 pagesSpinal CordSam TagardaNo ratings yet
- Summation & Termination of NeurotDocument17 pagesSummation & Termination of NeurotSam TagardaNo ratings yet
- PancreasDocument2 pagesPancreasSam TagardaNo ratings yet
- Motor TestDocument1 pageMotor TestSam TagardaNo ratings yet
- Laboratory Tests For HemostasisDocument4 pagesLaboratory Tests For HemostasisSam TagardaNo ratings yet
- Viral Meningitis Causes, Symptoms and TreatmentDocument4 pagesViral Meningitis Causes, Symptoms and TreatmentSam TagardaNo ratings yet
- 104 Skull, Mandible & The Facial BonesDocument68 pages104 Skull, Mandible & The Facial BonesSam Tagarda100% (1)
- Acid Base PhysiologyDocument58 pagesAcid Base PhysiologySam TagardaNo ratings yet
- 93 Miles Practice QuestionsDocument9 pages93 Miles Practice QuestionsSam TagardaNo ratings yet
- Gross AnatomyDocument32 pagesGross AnatomySam TagardaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 9700 s13 QP 42Document24 pages9700 s13 QP 42Peter KachouhNo ratings yet
- 7,8-Handling of Na+ & Glucose by The Renal TubulesDocument11 pages7,8-Handling of Na+ & Glucose by The Renal TubulesOsama MohamedNo ratings yet
- Basic Medial Science of The Kidney: The Scientific Basis of Clinical Disease, Marc Imhotep Cray, M.D.Document193 pagesBasic Medial Science of The Kidney: The Scientific Basis of Clinical Disease, Marc Imhotep Cray, M.D.Marc Imhotep Cray, M.D.100% (3)
- Animal Physiology AssignmentDocument26 pagesAnimal Physiology AssignmentAnjali MunjalNo ratings yet
- Acute Renal Failure Due to Acute Tubular NecrosisDocument13 pagesAcute Renal Failure Due to Acute Tubular Necrosisshaznay delacruzNo ratings yet
- DEFINE Homeostasis, Osmoregulation, Thermoregulation and Excretion. 1. HomeostasisDocument14 pagesDEFINE Homeostasis, Osmoregulation, Thermoregulation and Excretion. 1. HomeostasisStrange NazarNo ratings yet
- Acid Base BalanceDocument38 pagesAcid Base BalanceAvlya Zelyka0% (1)
- Dokumen - Pub - Target Jipmer Dec 2018 9811156083 9788184452662 PDFDocument216 pagesDokumen - Pub - Target Jipmer Dec 2018 9811156083 9788184452662 PDFAnil SharmaNo ratings yet
- Reabsorption of SodiumDocument19 pagesReabsorption of Sodiumpriya shettyNo ratings yet
- HomeostasisDocument18 pagesHomeostasisEmelia DeeNo ratings yet
- Soal Tes ImpsqDocument3 pagesSoal Tes ImpsqNandaNo ratings yet
- Acute Tubular Renal AcidosisDocument10 pagesAcute Tubular Renal AcidosisBarda GulanNo ratings yet
- UrinaryDocument87 pagesUrinaryJohn Paolo Dalida SalazarNo ratings yet
- 2 UrinarySystemDocument83 pages2 UrinarySystemLemuel Lagasca Razalan IVNo ratings yet
- Renal Physiology Acid Base BalanceDocument136 pagesRenal Physiology Acid Base BalanceTaimoor Ul HassanNo ratings yet
- NBME Form 26 Questions Only PDFDocument54 pagesNBME Form 26 Questions Only PDFFaizan KhawajaNo ratings yet
- Kidney, Excretion & OsmoregulationDocument65 pagesKidney, Excretion & OsmoregulationZaura100% (1)
- Kidney Introduction PDF 508Document10 pagesKidney Introduction PDF 508Shailesh DixitNo ratings yet
- Principles of Renal Physiology: Fifth EditionDocument15 pagesPrinciples of Renal Physiology: Fifth EditionAISHANo ratings yet
- Chloride The Queen of Electrolytes 2012Document9 pagesChloride The Queen of Electrolytes 2012Carlos PalominoNo ratings yet
- Uranium in Drinking-Water: Background Document For Development of WHO Guidelines For Drinking-Water QualityDocument23 pagesUranium in Drinking-Water: Background Document For Development of WHO Guidelines For Drinking-Water QualityAdel SukerNo ratings yet
- Histology Study Guide Kidney Histology: Kidney (Corpuscles and Tubules)Document17 pagesHistology Study Guide Kidney Histology: Kidney (Corpuscles and Tubules)Vlad TomaNo ratings yet
- Chloride The Queen of ElectrolytesDocument9 pagesChloride The Queen of ElectrolytesYancy Erazo DoradoNo ratings yet
- @@@ Regenerating Tubular Epithelial Cells of The KidneyDocument8 pages@@@ Regenerating Tubular Epithelial Cells of The KidneyeullobaNo ratings yet
- Chapter 27 GuytonDocument6 pagesChapter 27 GuytonGabriella ChafrinaNo ratings yet
- Regulation of Acid-Base BalanceDocument4 pagesRegulation of Acid-Base BalanceMich Therese Abejero100% (1)
- Kidney Pathophysiology, Toxicology, andDocument13 pagesKidney Pathophysiology, Toxicology, andS.CruzNo ratings yet
- Urinary Tract PhysiologykulDocument72 pagesUrinary Tract PhysiologykulAya KamajayaNo ratings yet
- P1710 Robbins & Kumar Basic Pathology 11th EditionDocument936 pagesP1710 Robbins & Kumar Basic Pathology 11th EditionpoopziNo ratings yet
- Case 8 GUS - AKIDocument210 pagesCase 8 GUS - AKIGroup 12 Sofia HanaNo ratings yet