Professional Documents
Culture Documents
Teaching Plan Fo Cord Car1
Uploaded by
jaden1233Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Teaching Plan Fo Cord Car1
Uploaded by
jaden1233Copyright:
Available Formats
TEACHING PLAN FOR MOTHER AND NEWBORN DESCRIPTION OF THE LEARNER: The learners are pregnant mothers with
37-38 weeks AOG, mothers who had no previous experience and mothers who had experience in caring for a child and cord care. They are from La Union. There are no cultural or spiritual concerns in terms of cord care and maternal concerns. LEARNING NEED: To define maternal care and newborn care and Additional guideline on breastfeeding and self care activities. LEARNING DIAGNOSIS: Knowledge deficit: Maternal and newborn care related to lack of experience of maternal and newborn care GOAL: To increase knowledge on maternal and newborn care and to apply this new knowledge in care of the newborn. BEHAVIORAL LEARNING OBJECTIVES LEARNING CONTENT TEACHING STRATEGY, METHODS AND ACTIVITIES TIME ALLOTMENT METHOD OF EVALUATION
After 15 to 20 minutes of health teaching, the client will be able to: 1. Define and state importance of Perineal, Breast, and self care activities. Definition and importance Perineal, breast and self care activities. One-on-one discussion; use of visual aids/ handouts 1 minute Instant oral feedback: The patient was able to share her realization, understanding, and their appreciation regarding the importance of perineal, breast and self care activities. Instant oral feedback The patient was able to share her realization, understanding, and their appreciation regarding the cord care and was able to define emotional adjustment. Instants oral feedback The patient was able to enumerate 4 out 7 danger signs to report.
2. Define Emotional Adjustment
Definition of emotional adjustment
Lecture handout
discussion,
3 minutes
3. Enumerate 4 out 7 Danger signs to report?
Danger signs to report by the One-on-one mother discussion; use of visual aids/ handouts
1 minute
4. Demonstrate skin care and cord care
Techniques in skin and cord care
Discussion, visual aids, demo-return demo
2 minutes
Demo/ Return Demo The patient was able to demonstrate the proper techniques in skin and cord care. Instant oral feedback The patient was able to define what breastfeeding is. Instant oral feedback The patient was able to define what is lactation process.
5. Give the importance of breastfeeding
Define breastfeeding
Handout
1 minutes
6. Define breastfeeding: Define the lactation process Breast-feeding: Lactation Process
Handout
1 minute
7. Demonstrate positioning and latching on
Techniques in latching on and positioning.
Discussion, visual aids, demo-return demo
5 minutes
Demo/ Return-Demo The patient was able to demonstrate the proper drying techniques in newborn cord care. Demo/ Return-Demo The patient was able to demonstrate the proper drying techniques in newborn cord care. Demo/ Return-Demo The patient was able to demonstrate the proper drying techniques in newborn cord care.
8. Demonstrate the use of pumping
Techniques on how to do manual expression
Discussion, visual aids, demo-return demo
2 minutes
9. Demonstrate proper ways in burping the child.
Techniques for burping the breastfed baby
Discussion, visual aids, demo-return demo
3 minutes
10. Know how to store breast milk
Things to consider in storing breast milk.
Discussion, visual aids, demo-return demo
1 minute
11. Enumerate 3 Signs of engorgement
Signs of engorgement
Handout
1 minute
Newborn: 1. Enumerate facts about Bowel Patterns Bowel patterns of newborn Discussion, handout 2 minutes Instant oral feedback: The patient was able to share her realization, understanding, and their appreciation regarding the Bowel patterns of newborn Instant oral feedback: The patient was able to share her realization, understanding, and their appreciation regarding the infant behaviour Instant oral feedback: The patient was able to share her realization, understanding, and their appreciation regarding the sleeping patterns of newborn Instant oral feedback: The patient was able to share her realization, understanding, and their appreciation regarding the coping mechanisms in terms of crying and emotional needs Instant oral feedback: The patient was able to share her realization, understanding, and their appreciation regarding the dangers signs to report in newborn care Instant oral feedback: The patient was able to share her realization,
2. Understand Infant Behavior
Infant behaviour
Discussion, visual aids
5 minutes
3. States understanding Sleeping Patterns
Sleeping patterns of newborn
Discussion, visual aids
2 minutes
4. Enumerate ways on how to Cope with a. Crying b. Emotional needs
Coping mechanisms in terms Discussion, visual aids of crying and emotional needs
2 minutes
5. Enumerate Danger Signs to Report
Dangers signs to report in newborn care
Discussion, visual aids
2 minutes
6. Enumerate importance of newborn screening.
Importance of newborn screening
Discussion, visual aids
3 minutes
understanding, and their appreciation regarding Importance of newborn screening.
LEARNING CONTENT: Perineal Care Perineal care is usually called peri care. It means washing the genitals and anal area. Peri care can be done during a bath or as a separate procedure. Peri care prevents skin breakdown of perineal area, itching, burning, odor, and infections. Perineal care is very important in maintaining the clients' comfort. More frequent care is required for clients who are incontinent or for those who have an indwelling catheter. Make every effort to respect the modesty of clients and be gentle when cleansing this sensitive area. Self-care Activities Ambulate when possible, with assist Sleep and rest as much as possible Wash hands Eat well balanced diet WHY???? This will reduce the risk of thrombus formation Constipation is a common problem Caring for an infant is physically and psychologically demanding, rest and sleep will benefit mother and baby
Ensures enough nutrition for breast feeding Hand washing will help prevent bacterial transmission of mother and baby Breast Care Wear supportive bra or apply cabbage leaves or ice packs Wash hands, but not breasts If nipples are sore, apply some expressed colostrums or breast milk Emotional Adjustment: Inform her that she may feel some mild depression, anxiety, pre-occupation and forgetfulness. Emphasize that this is normal for the first few days after birth. If symptoms are severe and persist beyond the first few days after birth, have her contact her physician. Drastic hormonal changes in body can cause some short-term emotional disturbances Danger signs to report Persistent significant bleeding Skin feels cool and clammy Heart feels like its racing Dizziness Refuses to interact with baby markedly depressed Loss of appetite
WHY???? These may be signs of shock from excessive bleeding these may be signs of post partum depression Both of these put mother and baby at risk Cord Care: How Do I Care For My Babys Umbilical Cord?
Keep the area clean. Pediatricians used to recommend cleaning the base of the cord with rubbing alcohol but now most of them prefer that the stump is left completely alone, because alcohol is believed to irritate the skin and sometimes delays healing. Other alternative methods in caring for your babys cord include the use of Goldenseal Root and Echinacea. It is best to consult your childs pediatrician for his/her recommendation. Keep the area dry. Allow the cord to be exposed to air as often as possible. This allows the base of the cord to dry and will decrease the amount of time that is required for healing to occur. Using newborn diapers that have a special cut out or folding your babys diaper down will help keep the c ord from being irritated. If weather permits, dress your baby in a t-shirt and diaper only to allow more time for the cord to dry out. Only give sponge baths. Do not bathe your baby in a sink or special tub until after the umbilical cord has fallen off. If your baby does take a bath, make sure to fan the area to dry it completely. You do not want to rub it dry as this could cause irritation. Allow the cord to heal naturally. It may be tempting to help the cord dry out and fall off especially if it appears to be hanging on by a thread, but it is best to allow this to happen naturally. Refrain from picking and pulling the cord off.
BREASTFEEDING Best for baby /Reduces incidence of allergies /Economical Antibodies /Stool ineffective /Temperature is always ideal/ Fresh/ Emotionally Bonding/ Easy once established/ Digested easily (2-3 hours)/ Immediately available /Nutritionally optional /Gastroenteritis reduced LACTATION - Breast milk looks like nonfat milk. It is thin and almost blue-tinged in appearance. - Before breastfeeding, mothers must wash their hands to be sure they are free of pathogens picked up from handling perineal pads or other sources. Washing her breasts is not necessary unless she notices caked colostrums (first breast fluid characterized as a thin yellowish fluid secreted by the breasts during the second trimester onwards but most evident in the first 2 to 3 days after birth and before the onset of true lactation) on the nipples. POSITIONING TECHNIQUES IN BREASTFEEDING - Lying on her side with a pillow under her head is a good position to assume when she is first attempting to breastfeed. This relieves fatigue because it allows the infant to rest on the bed. - Another position that the mother can utilize is sitting position with a pillow under the baby. Using a football hold with the baby supported on a pillow also may be helpful, especially if the mother had a cesarean birth. - Brushing the infants cheek with a breast nipple stimulates a newborns rooting reflex. The baby then turns toward the breast. Do not try to initiate a rooting reflex by pressing a babys face against the mothers breast; this will cause the child to turn away from the mother and toward your hand. - If a woman has large breasts, the infant may have trouble breathing while nursing because tissue presses against the nose. The mother can prevent this happening by grasping the areolar margin of her breast between her thumb and forefinger, holding the bulk of the breast supported while her infant feeds. This also makes the nipple more protruberant.
- Frequent feeding is advantageous to sustain a milk supply, because the more often the breasts are emptied, the more efficiently they will fill and continue to maintain a good supply of milk. - Help the infant break away from the breast when they are finished feeding. Insert a finger in the corner of the infants mouth or pull down the infants chin to release suction. Otherwise, the baby may pull too hard on the nipple, causing crack or soreness. TECHNIQUES FOR BURPING THE BREAST-FED BABY Some infants seem to swallow little air when they are breast-fed, whereas others swallow a great deal. As a rule, it is helpful to bubble (burp) newborns after they have emptied the first breast and again after the total feeding. Placing the baby over one shoulder and gently patting or stroking the back is an acceptable position. However, this position is not always satisfactory for a small infant, who has poor head control. Holding the baby in a sitting position on the lap, then leaning the child forward against one hand, with the index finger and thumb supporting the head, is often the best position to use. This position provides head support but leaves the other hand free to pat the babys back. Laying the baby prone across the lap is another alternative position. PREVENTING OR RELIEVING ENGORGEMENT The primary method for relieving engorgement is emptying the breasts of milk by having the infant suck as much as before. If an infant cannot grasp a nipple strongly because of engorgement, warm packs applied to both breasts for a few minutes before feeding, combined with massage to begin milk flow, often facilitates drainage and promotes breast softness so the infant can suck. Manual expression or the use of a breast pump to complete emptying of the breasts after the baby has nursed can help maintain or promote a good milk supply during the period of engorgement. Assure the mother that symptoms of engorgement are healthy; it is an indication that her breasts are producing milk. Engorgement is only temporary and should begin to subside 24 hours after it first becomes apparent.
Signs of engorgement Breasts feel firm, tender and hot, may be shiny and taut Areola may be firm and nipple flattened Usually resolves within 24 hours May use ice packs, cabbage leaves or ibuprofen to relieve discomfort Storage of breast milk Long term storage should be in hard plastic or glass Special plastic bags for human milk may be used short-term Store in serving sizes of 2-4 oz to prevent wast Breast milk can remain at room temperature for up to 8 hours Can refrigerate for up to 5 days May freeze for up to 6 months Make sure to date the containers Thaw milk gradually, do not microwave Bowel Patterns Meconium is passed within first 12-24 hours after birth After initiation of feeding, will have greenish brown transition stool Stools change with nutrition Bowel patterns may be indicative on nutritional status
Milk stool will appear by fourth day, which is yellow and pasty Breastfed infants will have at least 3 stools every 24 hours Lack of stool may indicate bowel obstruction Urinary Patterns 2-6 voiding per day for first 2 days 6-8 voiding per day of straw colour urine after 3-4 days consult physician if urine is pink or orange Indicates adequate fluid intake May indicate insufficient fluid intake
Weight Patterns Baby will lose some weight in first 3-5 days Infant should gain approximately 20-28g /day or 200g/week for first 3 months Notify physician if baby continues to lose weigh after 5 days Weight loss from fluid loss and increased metabolic rate Slow weight gain may be related to inadequate feeding
Infant Behavior Responds to touch, tracks parents eyes, responds to moms voice Cries to signify hunger, pain, desire for attention Likes to cuddle Readily upset by usual noises, wetness, or new experiences A healthy infant accomplishes behavioural and physiologic tasks Behaviour characteristics form basis of social capabilities Sleeping Patterns Newborns sleep approximately 17 hours a day May need to arouse baby for feeding By the fourth week, infant may stay awake from one feeding to the next Coping with Crying If baby is crying try: o Getting the baby warmer-swaddle or get skin to skin with baby to sooth o Feed baby Do not shake baby
If you are agitated, put the baby down and walk away for a few minutes. Emotional Needs Interact and play often with newborn If infant is crying try comfort and quieting techniques Use eye to eye contact Danger Signs to Report Fever: Temperature >100.4 Hypothermia: temperature below 97.7 Less than two diapers after 48 hours or less than three soiled diapers after fifth day Poor feeding or little interest in food Bleeding or purulent drainage from umbilical cord or circumcision Labored breathing with flared nostrils or apnea of more than 15 second Importance of Newborn Screening:
This is done by doing a heel stick on baby and running a blood analysis This is done by collecting a urine same and doing a urinalysis This will help to determine adequate physiologic adaptation and identify disorders that can adversely affect the childs life The Purpose of Newborn Screening
There are a number of potentially devastating diseases that can be present in a newborn but hidden at the time of birth. These diseases, if undetected by newborn screening, have the potential to cause medical problems as the baby grows, and severely alter a life that could have otherwise been normal.
Reference: Lowdermilk, D. L., Perry, S. E. & Cashion, K. (2010). Maternity nursing, (8th ed.). St. Louis: Mosby Elsevier. American Academy of Pediatrics/American College of Obstetricians and Gynecologists. (2007). Guidelines for Perinatal Care
Maternal and Child Health Nursing: Care of the Childbearing and Childrearing Family, 5th edition, by Pillitteri, Adele, et al. Tabers Cyclopedic Medical Dictionary, 18th edition, by Thomas, Clayton L., et al Principles of Anatomy and Physiology, 9th edition, by Tortora, Gerard J., et al Fairbank et al. Health Technology Assessment 2000; 4:1-57
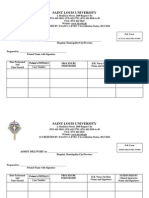
Saint Louis University School of Nursing Bonifacio Street, Baguio City
Teaching Plan for Proper Breastfeeding
Presented to the Faculty of the College of Nursing
In partial fulfilment for the Requirements for the Related Learning Experience for Summer 2014
Submitted to Prof. Blas Purganan Clincial Instructor
Tupac, Rushnol Jade P. BSN III-f4
March 31, 2014 Monday
You might also like
- Eu 4.18.18Document16 pagesEu 4.18.18Kimberly SmithNo ratings yet
- Case ScenarioDocument2 pagesCase ScenarioMARIA ANGELIKA DEL ROSARIONo ratings yet
- Pathophysiology of StrokeDocument2 pagesPathophysiology of StrokeACe JAy100% (2)
- PostpartumDocument7 pagesPostpartummaryNo ratings yet
- PRS Ear Instillation - GlovaDocument3 pagesPRS Ear Instillation - GlovaAndrea Colleen GlovaNo ratings yet
- Nursing Care of A Family With A Preschool Child: Chapter OverviewDocument95 pagesNursing Care of A Family With A Preschool Child: Chapter OverviewIra Delos SantosNo ratings yet
- Saint Louis UniversityDocument1 pageSaint Louis Universityjaden1233No ratings yet
- Baby Food ChartsDocument10 pagesBaby Food ChartsAnji EmmadiNo ratings yet
- Common Board Questions LOCALDocument12 pagesCommon Board Questions LOCALJhannNo ratings yet
- Which Statement On Physical Development of Infants and Toddlers Is TRUEDocument9 pagesWhich Statement On Physical Development of Infants and Toddlers Is TRUEKristylle Renz100% (1)
- Daughter Detox - Peg StreepDocument269 pagesDaughter Detox - Peg StreepWai YanNo ratings yet
- Teaching Plan For Proper Breast Feeding Begh ErDocument7 pagesTeaching Plan For Proper Breast Feeding Begh ErAmira Fatmah QuilapioNo ratings yet
- Health Teaching Nursery BGHDocument7 pagesHealth Teaching Nursery BGHAmira Fatmah QuilapioNo ratings yet
- NSO - Adam's Forward Bend TestDocument2 pagesNSO - Adam's Forward Bend TestMaha AmilNo ratings yet
- Breastfeeding TPDocument8 pagesBreastfeeding TPShaira Tan100% (1)
- Breastfeeding FinalDocument25 pagesBreastfeeding FinalWengel RedkissNo ratings yet
- Viernes, Jemalyn BSN 2-3 Assessment Diagnosis Planning Implementation Rationale EvaluationDocument8 pagesViernes, Jemalyn BSN 2-3 Assessment Diagnosis Planning Implementation Rationale EvaluationJeMalyn VieRnesNo ratings yet
- Nursing Care Plan Assessment Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Intervention and Rationale EvaluationDocument23 pagesNursing Care Plan Assessment Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Intervention and Rationale EvaluationyusivileidyNo ratings yet
- Activity 2 - Bigleap - Immediate Care of The Newborn (Updated)Document5 pagesActivity 2 - Bigleap - Immediate Care of The Newborn (Updated)Cameron De GuzmanNo ratings yet
- Care PlansDocument7 pagesCare PlansFirenze Fil100% (6)
- Health Education Plan - Case StudyDocument7 pagesHealth Education Plan - Case StudyRenzy Mayven Pedriña LobatonNo ratings yet
- Asynchronous Activity#2Document10 pagesAsynchronous Activity#2Nur Sanaani100% (1)
- Corrected NCP Case 3 Intrapartum NCPDocument2 pagesCorrected NCP Case 3 Intrapartum NCPReyzel PahunaoNo ratings yet
- Ko Mapigilang Humilik Kapag Ako'yDocument6 pagesKo Mapigilang Humilik Kapag Ako'yDivine Dela CruzNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care PlanRhitzle Ann100% (1)
- MCN SF Chapter 17 QuizDocument3 pagesMCN SF Chapter 17 QuizKathleen AngNo ratings yet
- Nutrition and Malnutrition Resource UnitDocument22 pagesNutrition and Malnutrition Resource UnitMitch GatdulaNo ratings yet
- Module 8 Problem Analysis Using Ethical TheoriesDocument4 pagesModule 8 Problem Analysis Using Ethical TheoriesJewell Nivera CarpioNo ratings yet
- Health Teaching Plan Group 1 CDocument2 pagesHealth Teaching Plan Group 1 CKirstie CapitanNo ratings yet
- Care of Mother, Child, and Adolescents (Well Clients) NCM - 107 Nursing Care Plan Assessment Diagnosis Plan Intervention EvaluationDocument4 pagesCare of Mother, Child, and Adolescents (Well Clients) NCM - 107 Nursing Care Plan Assessment Diagnosis Plan Intervention EvaluationSophia Caisip100% (1)
- Normal Spontaneous DeliveryDocument4 pagesNormal Spontaneous Deliveryvivian magnoNo ratings yet
- H. Nursing Care Plan: Altered Parenting RoleDocument2 pagesH. Nursing Care Plan: Altered Parenting RoleClovie ArsenalNo ratings yet
- Labor Induced AugmentedDocument9 pagesLabor Induced Augmentednursereview83% (6)
- A Typology of Nursing Problems in Family Nursing PracticeDocument3 pagesA Typology of Nursing Problems in Family Nursing PracticeDizerine Mirafuentes RolidaNo ratings yet
- Family Nursing Care Plan ChapterDocument1 pageFamily Nursing Care Plan ChapterJhe PangsNo ratings yet
- Environmental SanitationDocument5 pagesEnvironmental SanitationNessa Layos MorilloNo ratings yet
- Health Teaching Plan FormDocument2 pagesHealth Teaching Plan FormChadd Vyllmorr VillarinNo ratings yet
- Nursing Care Plan in OBDocument2 pagesNursing Care Plan in OBKaren ValdezNo ratings yet
- NCP Case 1Document6 pagesNCP Case 1boomer SeargeNo ratings yet
- Nursing Care PlansDocument14 pagesNursing Care PlansTels Dela PeñaNo ratings yet
- Case Study NCPDocument4 pagesCase Study NCPKelly OstolNo ratings yet
- Sample FNCPDocument5 pagesSample FNCPBeng Bheng100% (1)
- Management of The Sick Child Aged 2 Months Up To 5 YearsDocument3 pagesManagement of The Sick Child Aged 2 Months Up To 5 Yearstiban_07No ratings yet
- Soapie DocumentationDocument2 pagesSoapie DocumentationJubilee AngNo ratings yet
- NURSING CARE PLAN Interrupted Breastfeeding: Student Nurses' CommunityDocument3 pagesNURSING CARE PLAN Interrupted Breastfeeding: Student Nurses' CommunitySaira SucgangNo ratings yet
- Nursing Care Plan D-CDocument2 pagesNursing Care Plan D-CGian MonillaNo ratings yet
- Ncma Course Task 13 PDFDocument1 pageNcma Course Task 13 PDFJaja ManezNo ratings yet
- Teaching Plan Deviced For Teenage Mother and NewbornDocument34 pagesTeaching Plan Deviced For Teenage Mother and NewbornYzel Vasquez AdavanNo ratings yet
- Meal Planning For A College Student: Saint Louis University School of NursingDocument7 pagesMeal Planning For A College Student: Saint Louis University School of NursingMaranatha BuenaventuraNo ratings yet
- Far Eastern University: Evidence Based NursingDocument5 pagesFar Eastern University: Evidence Based NursingandreaNo ratings yet
- Self Breast ExaminationDocument2 pagesSelf Breast ExaminationMaye Marquino Lofranco NeriNo ratings yet
- Bag Technique 2 UCDocument2 pagesBag Technique 2 UCSoleil Maxwell0% (1)
- CASE STUDY: Pre Labor Infant With Respiratory Distress SyndromeDocument4 pagesCASE STUDY: Pre Labor Infant With Respiratory Distress SyndromeE.R.ONo ratings yet
- Post-Partum CareDocument4 pagesPost-Partum CarejoethemangoNo ratings yet
- Assessment Nursing Diagnosis Rationale Desired Outcome Interventions Justification EvaluationDocument7 pagesAssessment Nursing Diagnosis Rationale Desired Outcome Interventions Justification EvaluationPJNo ratings yet
- Changing A Bowel Diversion Ostomy WITH ANSWERDocument9 pagesChanging A Bowel Diversion Ostomy WITH ANSWERJohn Pearl FernandezNo ratings yet
- Neonatal JaundiceDocument12 pagesNeonatal JaundiceJustine NyangaresiNo ratings yet
- Drug StudyDocument2 pagesDrug StudyJayran Bay-anNo ratings yet
- Imbalanced Nutrition Less Than Body RequirementsDocument2 pagesImbalanced Nutrition Less Than Body RequirementsSundaraBharathiNo ratings yet
- Assessment Nursing Diagnosis Goal/ Objective Intervention EvaluationDocument1 pageAssessment Nursing Diagnosis Goal/ Objective Intervention Evaluationjezreel ibarraNo ratings yet
- CHN - IdbDocument11 pagesCHN - IdbCharm RoweNo ratings yet
- Prenatal Care NCPDocument10 pagesPrenatal Care NCPAlex AntipordaNo ratings yet
- Jose Rizal University: College of NursingDocument11 pagesJose Rizal University: College of NursingDhan Mark Trinidad100% (3)
- NDT Reviewer PDFDocument9 pagesNDT Reviewer PDFAnonymousTargetNo ratings yet
- Teaching Plan For Proper Breast Feeding Begh ErDocument7 pagesTeaching Plan For Proper Breast Feeding Begh ErSandy DuranNo ratings yet
- Breastfeeding: Newborn Bathing PracticesDocument2 pagesBreastfeeding: Newborn Bathing PracticesA.I. RiponNo ratings yet
- JournalDocument9 pagesJournaljaden1233No ratings yet
- Templates For CasesDocument6 pagesTemplates For Casesjaden1233No ratings yet
- Causes of Kidney FailureDocument4 pagesCauses of Kidney Failurejaden1233No ratings yet
- Handout Birth Control-SignedDocument2 pagesHandout Birth Control-Signedjaden1233No ratings yet
- Predisposing Factors: Mother and Child Relationship Not Good No Father GuidanceDocument28 pagesPredisposing Factors: Mother and Child Relationship Not Good No Father Guidancejaden1233No ratings yet
- Support 1Document8 pagesSupport 1jaden1233No ratings yet
- What We Learn Before We Are Born-TedDocument4 pagesWhat We Learn Before We Are Born-TedalbinkhanNo ratings yet
- Study Note Ga Eng 26 02 18 PDFDocument15 pagesStudy Note Ga Eng 26 02 18 PDFvikramNo ratings yet
- What Is A Normal TemperatureDocument2 pagesWhat Is A Normal Temperature菁菁No ratings yet
- Lesson 4 Infancy by HurlockDocument44 pagesLesson 4 Infancy by HurlockJessica Recaido100% (1)
- Table ContentDocument12 pagesTable ContenthiwotNo ratings yet
- Child Development 0-3 MonthsDocument12 pagesChild Development 0-3 MonthsNita FarlisaNo ratings yet
- Conf PrenatalsensorydevelopmentDocument2 pagesConf Prenatalsensorydevelopmentapi-259661638No ratings yet
- MARKETING REPORT ON NestléDocument15 pagesMARKETING REPORT ON NestléManisha SinhaNo ratings yet
- Copil SanatosDocument123 pagesCopil SanatosZâna CicăNo ratings yet
- Lesson Plan On Neonatal ConvulsionDocument19 pagesLesson Plan On Neonatal ConvulsionASHISH KUMAR YADAV100% (1)
- Examination of The Newborn InfantDocument15 pagesExamination of The Newborn InfantWilda AwliaNo ratings yet
- Cross-Covering The Well Baby Nursery and Pedi-Med Service: Intensive Care Nursery House Staff ManualDocument5 pagesCross-Covering The Well Baby Nursery and Pedi-Med Service: Intensive Care Nursery House Staff ManualSedaka DonaldsonNo ratings yet
- Postnatal Care Postnatal Care OverviewDocument11 pagesPostnatal Care Postnatal Care OverviewviannikkkyNo ratings yet
- Extra Reading Unit 7. Robot BabyDocument1 pageExtra Reading Unit 7. Robot BabyIba LaçiNo ratings yet
- Paediatrics Notes-2017 BatchDocument102 pagesPaediatrics Notes-2017 BatchMohan EthirajanNo ratings yet
- Policy On PacifiersDocument4 pagesPolicy On PacifiersمعتزباللهNo ratings yet
- Colic Essay OutlineDocument2 pagesColic Essay OutlineSyaie SyaiedaNo ratings yet
- Group 12 The Family With An InfantDocument126 pagesGroup 12 The Family With An InfantGrace JPNo ratings yet
- Ayurvedic Postpartum Rejuvenation Guide Samadhi Ayurveda & MassageDocument3 pagesAyurvedic Postpartum Rejuvenation Guide Samadhi Ayurveda & Massageforu_raghuNo ratings yet
- Development of Food Preferences PDFDocument22 pagesDevelopment of Food Preferences PDFThalesJNo ratings yet
- UK Stokke Collection Catalogue 2Document31 pagesUK Stokke Collection Catalogue 2Zamzila KassimNo ratings yet
- Mira CradleDocument3 pagesMira CradlemyjasbirNo ratings yet
- Obstetrics and Gynecology Osce: Bimanual Vaginal (PV) ExaminationDocument9 pagesObstetrics and Gynecology Osce: Bimanual Vaginal (PV) Examinationvichram100% (1)
- Clinical ExemplarDocument5 pagesClinical Exemplarapi-300362033No ratings yet
- Neonatal JaundiceDocument5 pagesNeonatal JaundiceIzwan KyNo ratings yet