Professional Documents
Culture Documents
Abolishing Mammography Screening Programs?
Uploaded by
mjwalshCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Abolishing Mammography Screening Programs?
Uploaded by
mjwalshCopyright:
Available Formats
The
NEW ENGLA ND JOURNAL
of
MEDICINE
Perspective
Abolishing Mammography Screening Programs? A View from the Swiss Medical Board
Nikola Biller-Andorno, M.D., Ph.D., and Peter Jni, M.D.
n January 2013, the Swiss Medical Board, an independent health technology assessment initiative under the auspices of the Conference of Health Ministers of the Swiss Cantons, the Swiss Medical
Association, and the Swiss Academy of Medical Sciences, was mandated to prepare a review of mammography screening. The two of us, a medical ethicist and a clinical epidemiologist, were members of the expert panel that appraised the evidence and its implications. The other members were a clinical pharmacologist, an oncologic surgeon, a nurse scientist, a lawyer, and a health economist. As we embarked on the project, we were aware of the controversies that have surrounded mammography screening for the past 10 to 15 years. When we reviewed the available evidence and contemplated its implications in detail, however, we became increasingly concerned. First, we noticed that the ongoing debate was based on a series of reanalyses of the same, predominantly outdated trials. The first trial started more than 50 years ago in New York City and the last trial in 1991 in the United Kingdom.1 None of these trials were initiated in the era of modern breast-cancer treatment, which has dramatically improved the prognosis of women with breast cancer. Could the modest benefit of mammography screening in terms of breast-cancer mortality that was shown in trials initiated between 1963 and 1991 still be detected in a trial conducted today? Second, we were struck by how nonobvious it was that the benefits of mammography screening
n engl j med nejm.org
outweighed the harms. The relative risk reduction of approximately 20% in breast-cancer mortality associated with mammography that is currently described by most expert panels2 came at the price of a considerable diagnostic cascade, with repeat mammography, subsequent biopsies, and overdiagnosis of breast cancers cancers that would never have become clinically apparent. The recently published extended follow-up of the Canadian National Breast Screening Study is likely to provide reliable estimates of the extent ofoverdiagnosis. After 25 years of follow-up, it found that 106 of 484 screen-detected cancers (21.9%) were overdiagnosed.3 This means that 106 of the 44,925 healthy women in the screening group were diagnosed with and treated for breast cancer unnecessarily, which resulted in needless sur1
The New England Journal of Medicine Downloaded from nejm.org by MICHAEL J WALSH on April 17, 2014. For personal use only. No other uses without permission. Copyright 2014 Massachusetts Medical Society. All rights reserved.
PERS PE C T IV E
Abolishing Mammography Screening Programs?
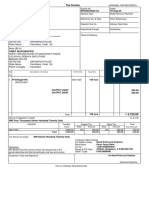
A Womens Perception of the Effect of Mammography
With screening
876 Women alive 80 Women die from breast cancer 44 Women die from other causes
Without screening
160 Women die from breast cancer 44 Women die from other causes
796 Women alive
B Real Effect of Mammography
With screening
951 or 952 Women alive 4 Women die from breast cancer
Without screening
951 Women alive 5 Women die from breast cancer 44 Women die from other causes
44 or 45 Women die from other causes
U.S. Womens Perceptions of the Effects of Mammography Screening on Breast-Cancer Mortality as Compared with the Actual Effects. Panel A shows the views of 50-year-old women in the United States regarding the effect of mammography every 2 years on the 10-year risk of death from breast cancer (at left), as compared with no screening (at right). The areas of the squares are proportional to the numbers of women per 1000 who would be alive (blue), die from breast cancer (orange), or die from other causes (yellow). The numbers were calculated from womens perceived relative and absolute risk reductions for breast-cancer deaths (Domenighetti et al.4) and U.S. mortality statistics for 2008 from the Centers for Disease Control and Prevention. Panel B shows the actual effect of mammography screening on breast-cancer deaths, with numbers calculated from breast-cancer mortality data for 2008 from the National Cancer Institute and U.S. mortality statistics for 2008, assuming a relative risk reduction of 20% for breast-cancer mortality in women invited to undergo screening (Independent U.K. Panel2).
gical interventions, radiotherapy, chemotherapy, or some combination of these therapies. In addition, a Cochrane review of 10 trials involving more than 600,000 women showed there was no evidence suggesting an effect of mammography screening on overall mortality.1 In the best case, the small reduction in breast-cancer deaths was attenuated by deaths from other causes. In the worst case, the reduction was canceled out by deaths caused by coexisting conditions or by the harms of screening and associated over2
treatment. Did the available evidence, taken together, indicate that mammography screening indeed benefits women? Third, we were disconcerted by the pronounced discrepancy between womens perceptions of the benefits of mammography screening and the benefits to be expected in reality. The figure shows the numbers of 50-yearold women in the United States expected to be alive, to die from breast cancer, or to die from other causes if they are invited to undergo regular mammography every
n engl j med nejm.org
2 years over a 10-year period, as compared with women who do not undergo mammography. The numbers in Panel A are derived from a survey about U.S. womens perceptions,4 in which 717 of 1003 women (71.5%) said they believed that mammography reduced the risk of breast-cancer deaths by at least half, and 723 women (72.1%) thought that at least 80 deaths would be prevented per 1000 women who were invited for screening. The numbers in Panel B reflect the most likely scenarios according to available trials1-3: a relative risk reduction of 20% and prevention of 1 breastcancer death. The data for Switzerland, reported in the same study, show similarly overly optimistic expectations. How can women make an informed decision if they overestimate the benefit of mammography so grossly? The Swiss Medical Boards report was made public on February 2, 2014 (www.medical-board.ch). It acknowledged that systematic mammography screening might prevent about one death attributed to breast cancer for every 1000 women screened, even though there was no evidence to suggest that overall mortality was affected. At the same time, it emphasized the harm in particular, false positive test results and the risk of overdiagnosis. For every breast-cancer death prevented in U.S. women over a 10-year course of annual screening beginning at 50 years of age, 490 to 670 women are likely to have a false positive mammogram with repeat examination; 70 to 100, an unnecessary biopsy; and 3 to 14, an overdiagnosed breast cancer that would never have become clinically apparent.5 The board therefore recommended that no new systematic mam-
The New England Journal of Medicine Downloaded from nejm.org by MICHAEL J WALSH on April 17, 2014. For personal use only. No other uses without permission. Copyright 2014 Massachusetts Medical Society. All rights reserved.
PE R S PE C T IV E
Abolishing Mammography Screening Programs?
mography screening programs be introduced and that a time limit be placed on existing programs. In addition, it stipulated that the quality of all forms of mammography screening should be evaluated and that clear and balanced information should be provided to women regarding the benefits and harms of screening. The report caused an uproar and was emphatically rejected by a number of Swiss cancer experts and organizations, some of which called the conclusions unethical. One of the main arguments used against it was that it contradicted the global consensus of leading experts in the field a criticism that made us appreciate our unprejudiced perspective resulting from our lack of exposure to past consensus-building efforts by specialists in breastcancer screening. Another argument was that the report unsettled women, but we wonder how to avoid unsettling women, given the available evidence. The Swiss Medical Board is nongovernmental, and its recommendations are not legally binding. Therefore, it is unclear whether the report will have any effect on the policies in our country. Although Switzerland is a small country, there are notable differences among regions, with the French- and Italianspeaking cantons being much more in favor of screening programs than the German-speaking
cantons a finding suggesting that cultural factors need to be taken into account. Eleven of the 26 Swiss cantons have systematic mammography screening programs for women 50 years of age or older; two of these programs were introduced only last year. One German-speaking canton, Uri, is reconsidering its decision to start a mammography screening program in light of the boards recommendations. Participation in existing programs ranges from 30 to 60% variation that can be partially explained by the coexistence of opportunistic screening offered by physicians in private practice. At least three quarters of all Swiss women 50 years of age or older have had a mammogram at least once in their life. Health insurers are required to cover mammography as part of systematic screening programs or within the framework of diagnostic workups of potential breast disease. It is easy to promote mammography screening if the majority of women believe that it prevents or reduces the risk of getting breast cancer and saves many lives through early detection of aggressive tumors.4 We would be in favor of mammography screening if these beliefs were valid. Unfortunately, they are not, and we believe that women need to be told so. From an ethical perspective, a public health program that does not clearly
produce more benefits than harms is hard to justify. Providing clear, unbiased information, promoting appropriate care, and preventing overdiagnosis and overtreatment would be a better choice.
The views expressed in this article are those of the authors and do not necessarily reflect those of all members of the expert panel of the Swiss Medical Board. Disclosure forms provided by the authors are available with the full text of this article at NEJM.org. From the Institute of Biomedical Ethics, University of Zurich, Zurich (N.B.-A.), and the Institute of Social and Preventive Medicine and Clinical Trials Unit Bern, Department of Clinical Research, University of Bern, Bern (P.J.) both in Switzerland; and the Division of Medical Ethics, Department of Global Health and Social Medicine, Harvard Medical School, Boston (N.B.-A.). Dr. BillerAndorno is a member of the expert panel of the Swiss Medical Board; Dr. Jni was a member of the panel until August 30, 2013. This article was published on April 16, 2014, at NEJM.org. 1. Gtzsche PC, Jrgensen KJ. Screening for breast cancer with mammography. Coch rane Database Syst Rev 2013;6:CD001877. 2. Independent UK Panel on Breast Cancer Screening. The benefits and harms of breast cancer screening: an independent review. Lancet 2012;380:1778-86. 3. Miller AB, Wall C, Baines CJ, Sun P, To T, Narod SA. Twenty five year follow-up for breast cancer incidence and mortality of the Canadian National Breast Screening Study: randomised screening trial. BMJ 2014; 348:g366. 4. Domenighetti G, DAvanzo B, Egger M, et al. Womens perception of the benefits of mammography screening: populationbased survey in four countries. Int J Epidemiol 2003;32:816-21. 5. Welch HG, Passow HJ. Quantifying the benefits and harms of screening mammography. JAMA Intern Med 2014;174:448-54.
DOI: 10.1056/NEJMp1401875
Copyright 2014 Massachusetts Medical Society.
n engl j med nejm.org
The New England Journal of Medicine Downloaded from nejm.org by MICHAEL J WALSH on April 17, 2014. For personal use only. No other uses without permission. Copyright 2014 Massachusetts Medical Society. All rights reserved.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Motivate! 2 End-Of-Term Test Standard: Units 1-3Document6 pagesMotivate! 2 End-Of-Term Test Standard: Units 1-3Oum Vibol SatyaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- GRADE 8 English Lesson on Indian LiteratureDocument3 pagesGRADE 8 English Lesson on Indian LiteratureErold TarvinaNo ratings yet
- GVP College of Engineering (A) 2015Document3 pagesGVP College of Engineering (A) 2015Abhishek SunilNo ratings yet
- IAS 8 Tutorial Question (SS)Document2 pagesIAS 8 Tutorial Question (SS)Given RefilweNo ratings yet
- CFA三级百题 答案Document163 pagesCFA三级百题 答案vxm9pctmrrNo ratings yet
- Aromatic Saturation Catalysts: CRI's Nickel Catalysts KL6564, KL6565, KL6515, KL6516Document2 pagesAromatic Saturation Catalysts: CRI's Nickel Catalysts KL6564, KL6565, KL6515, KL6516Ahmed SaidNo ratings yet
- What Would Orwell Think?Document4 pagesWhat Would Orwell Think?teapottingsNo ratings yet
- Unit 3 Test A Test (Z Widoczną Punktacją)Document4 pagesUnit 3 Test A Test (Z Widoczną Punktacją)Kinga WojtasNo ratings yet
- The Power of Compounding: Why It's the 8th Wonder of the WorldDocument5 pagesThe Power of Compounding: Why It's the 8th Wonder of the WorldWaleed TariqNo ratings yet
- 6 Holly Fashion Case StudyDocument3 pages6 Holly Fashion Case StudyCaramalau Mirela-Georgiana0% (1)
- Plusnet Cancellation FormDocument2 pagesPlusnet Cancellation FormJoJo GunnellNo ratings yet
- Alberta AwdNomineeDocs Case Circle BestMagazine NewTrailSpring2016Document35 pagesAlberta AwdNomineeDocs Case Circle BestMagazine NewTrailSpring2016LucasNo ratings yet
- Importance of Time Management To Senior High School Honor StudentsDocument7 pagesImportance of Time Management To Senior High School Honor StudentsBien LausaNo ratings yet
- The Mckenzie MethodDocument24 pagesThe Mckenzie MethodMohamed ElMeligieNo ratings yet
- Soal Ulangan Harian Smester 1 Kelas 8 SMP BAHASA INGGRISDocument59 pagesSoal Ulangan Harian Smester 1 Kelas 8 SMP BAHASA INGGRISsdn6waykhilauNo ratings yet
- Corporate Process Management (CPM) & Control-EsDocument458 pagesCorporate Process Management (CPM) & Control-EsKent LysellNo ratings yet
- The Conflict With Slavery and Others, Complete, Volume VII, The Works of Whittier: The Conflict With Slavery, Politicsand Reform, The Inner Life and Criticism by Whittier, John Greenleaf, 1807-1892Document180 pagesThe Conflict With Slavery and Others, Complete, Volume VII, The Works of Whittier: The Conflict With Slavery, Politicsand Reform, The Inner Life and Criticism by Whittier, John Greenleaf, 1807-1892Gutenberg.org100% (1)
- A Story Behind..: Dimas Budi Satria Wibisana Mario Alexander Industrial Engineering 5Document24 pagesA Story Behind..: Dimas Budi Satria Wibisana Mario Alexander Industrial Engineering 5Owais AwanNo ratings yet
- Fact-Sheet Pupils With Asperger SyndromeDocument4 pagesFact-Sheet Pupils With Asperger SyndromeAnonymous Pj6OdjNo ratings yet
- 5.1 Physical Farming Constraints in Southern CaliforniaDocument1 page5.1 Physical Farming Constraints in Southern CaliforniaTom ChiuNo ratings yet
- CL Commands IVDocument626 pagesCL Commands IVapi-3800226100% (2)
- Masters of Death: The Assassin ClassDocument5 pagesMasters of Death: The Assassin Classjbt_1234No ratings yet
- The Rescue FindingsDocument8 pagesThe Rescue FindingsBini Tugma Bini Tugma100% (1)
- TIA Portal v11 - HMI ConnectionDocument4 pagesTIA Portal v11 - HMI ConnectionasdasdasdasdasdasdasadaNo ratings yet
- Trends Interiors Architecture Fashion Lifestyle: 6 Spring 2013 Collector's EditionDocument116 pagesTrends Interiors Architecture Fashion Lifestyle: 6 Spring 2013 Collector's EditionFernanda RaquelNo ratings yet
- Kasapreko PLC Prospectus November 2023Document189 pagesKasapreko PLC Prospectus November 2023kofiatisu0000No ratings yet
- Endoplasmic ReticulumDocument4 pagesEndoplasmic Reticulumnikki_fuentes_1100% (1)
- Orbit BioscientificDocument2 pagesOrbit BioscientificSales Nandi PrintsNo ratings yet
- Kerala Dinesh Beedi - WikipediaDocument12 pagesKerala Dinesh Beedi - Wikipediaaymanamna2016No ratings yet
- Concepts of Cavity Prep PDFDocument92 pagesConcepts of Cavity Prep PDFChaithra Shree0% (1)