Professional Documents
Culture Documents
WHO Country Cooperation Strategy 2008-2011: Thailand Thailand
Uploaded by
Ikhsan AmadeaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
WHO Country Cooperation Strategy 2008-2011: Thailand Thailand
Uploaded by
Ikhsan AmadeaCopyright:
Available Formats
WHO Country Coopcration Stratcgy
2008-2011
Permanent 8ecretary u||d|ng No.3
4th f|oor, H|n|stry of Pub||c hea|th
T|wanon Road, Huang
Nonthabur| 11000
Tha||and
www.whotha|.org
Thailand
WHO Country Cooperation Strategy
2008-2011
, July
WHO Country Cooperation Strategy 2008-2011 ii
World Health Organization 2007
Publications of the World Health Organization enjoy copyright protection in accordance
with the provisions of Protocol 2 of the Universal Copyright Convention. For rights of
reproduction or translation, in part or in toto, of publications issued by the WHO Regional
Office for South-East Asia, application should be made to the Regional Office for South-
East Asia, World Health House, Indraprastha Estate, New Delhi 110002, India.
The designations employed and the presentation of material in this publication do not
imply the expression of any opinion whatsoever on the part of the Secretariat of the
World Health Organization concerning the legal status of any country, territory, city or
area or of its authorities, or concerning the delimitation of its frontiers or boundaries.
Thailand iii
Contents
Preface .............................................................................................................. v
Foreword ........................................................................................................ vii
Executive Summary .......................................................................................... ix
1. Introduction ............................................................................................... 1
2. Country health and development challenges in Thailand ............................ 3
1. Economic and social development ................................................................. 3
2. Health policies ............................................................................................... 4
3. Burden of disease and the health development situation ................................ 5
3. Development assistance and partnerships:
Aid flow, instruments and coordination..................................................... 17
1. Partnership with UN and other international development agencies ............. 17
2. Partnership with developing countries .......................................................... 19
3. Technical cooperation with other countries .................................................. 19
4. WHO Collaborating Network....................................................................... 20
4. Current WHO cooperation....................................................................... 21
1. Work of the WHO Country Office encompasses .......................................... 21
2. Focus of WHOs collaboration with Thailand ............................................... 21
3. Funding of WHO collaborative programmes. ............................................... 22
4. Fellowships .................................................................................................. 22
5. Regional Sub-units ....................................................................................... 23
6. Staffing ........................................................................................................ 23
7. Office premises ............................................................................................ 24
8. Information and communication technology ................................................ 24
9. Use of CCS .................................................................................................. 24
WHO Country Cooperation Strategy 2008-2011 iv
5. WHO policy framework Global and regional directions ......................... 25
1. Global challenges in health .......................................................................... 25
2. Global health agenda ................................................................................... 26
3. Regional policy framework ........................................................................... 27
6. Strategic agenda: Priorities jointly agreed for WHO cooperation
in and with countries ................................................................................ 28
1. Principles ..................................................................................................... 28
2. Strategic agenda .......................................................................................... 28
3. Modalities of implementation: ..................................................................... 32
7. Implementing the strategic agenda: Implication for
WHO Secretariat, follow-up and next step at each level ........................... 34
1. Introduction................................................................................................. 34
2. Staffing: Current and future.......................................................................... 34
3. Financial allocation ...................................................................................... 35
4. Information and communication support ..................................................... 35
5. Implementation of the strategic agenda ........................................................ 35
Annexes
1. National health development data ............................................................... 37
2. Strategic objectives and their scope under MTSP 2008-2013 ....................... 38
3. MoPH budget in present value and real terms .............................................. 43
4. Health budget allocation for major types of programmes during
the first half of the Ninth National Health Development Plan ....................... 44
5. Thailands scorecard on MDG Targets (Goal 1-7) .......................................... 45
6. Organogram Ministry of Public Health....................................................... 46
7. Morbidity rates of hospitalized cases (per 100 000 population)
due to selected NCDs, injuries and mental illness Thailand
(excluding Bangkok), 20012004 ................................................................. 47
8. Organogram WHO Country Office Thailand ................................................ 48
9. References ................................................................................................... 49
Thailand v
Collaborative activities of the World Health Organization (WHO) in the South-East
Asia (SEA) Region are geared to improve the health status of the population of Member
States. Although WHO has been contributing as a key catalyst to Thailands health
policies and programmes, there is a need to thoroughly analyze and discuss how the
Organization can further improve its contribution to the development of health in
Thailand.
The South-East Asia Region was the first among WHOs Regions to promote the
Country Cooperation Strategy (CCS) as a process to identify how the Organization can
best support health development in our Member States. All 11 Member States of the
Region have prepared their CCSs over the past six years. In the case of Thailand, two
CCSs have already been prepared and have been used continuously as guidelines for
the WHO Country Office (WCO) to plan and coordinate work effectively with their
national as well as international counterparts for health development in the country.
Analyses of the current health situation and the likely scenario over the next four
years have together formed the basis of the priorities outlined in this CCS. The inputs
and suggestions from the Ministry of Public Health, whose officials have been the
major collaborators in developing this document, are appreciated. In addition, the
advice and recommendations of the health development partners in Thailand and the
United Nations Partnership Framework (UNPAF) 2007-2011, of which the WHO
Country Office is also a signatory, were invaluable in guiding the development of this
CCS. The consultative process here will help ensure that WHO inputs provide the
maximum support to health development efforts in the country.
To help achieve the objectives of this CCS and to promote technical assistance
from Thailand to other Member countries, we recognize the importance of a strong
WHO Country Office working closely with key counterparts, keeping in mind local
conditions. Nonetheless, the entire organization is committed to the work of the CCS.
The staff of the WHO Regional Office will use this CCS to determine regional priorities
and support collaborative activities in Thailand. Furthermore, we will also seek assistance,
as necessary, from WHO Headquarters towards bolstering these efforts.
I would like to thank the Ministry of Public Health and Faculty of Tropical Medicine,
Mahidol University, Bangkok for providing office space for the regional-level units,
Communicable Disease Surveillance and Response Sub-unit and the Malaria Mekong
Sub-unit.
Preface
WHO Country Cooperation Strategy 2008-2011 vi
I would like also to specially thank all those who have contributed to development
of this Country Cooperation Strategy, which has the full commitment of the Regional
Office. We will provide our maximum support towards achieving its objectives over
the next four years. Our joint efforts, I am confident, will help in achieving the maximum
health benefits for the people of Thailand.
Samlee Plianbangchang, M.D., Dr.P.H.
Regional Director
Thailand vii
Thailand is one of the countries in the South-East Asia Region that have an advanced
health infrastructure, a robust surveillance system and public health professionals with
a high degree of expertise. The country has demonstrated excellence and expertise in
many areas of public health, medical specialities and nursing. Thailand has also achieved
many of the Millennium Development Goals (MDGs).
The WHO Country Office (WCO) is in a unique position to have national experts
in both long-term and short-term positions who can contribute to the work of the
Organization in Thailand. The Country Office also facilitates training programmes for
Fellows from neighbouring countries and other Member countries of the Region, for
capacity building.
Even with such remarkable progress, communicable diseases such as HIV/AIDS,
tuberculosis (TB) and avian influenza (AI) continue to have a negative impact on the
country, with certain situations exacerbated by the prevalent circumstances along
Thailands borders. Health promotion efforts and control measures for NCDs are well
advanced in terms of both legislation and intervention. The WCO provides the necessary
support to enhance these efforts.
The purpose of this Country Cooperation Strategy (CCS) is to reflect the medium-
term vision of WHO for its cooperation with Thailand and to elucidate the strategic
framework for such cooperation. The CCS represents a balance between evidence-
based country priorities and organization-wide strategic priorities in order to contribute
optimally to national health development.
It is very timely for WCO Thailand to prepare the new CCS covering the period
2008-2011, since the current Strategy will end in 2007. The WHO Medium-Term
Strategic Plan (MTSP) 2008-2013 is being prepared and a new planning approach has
been introduced. The priorities and strategic framework are based on: (1) National
and international partners recommendations; (2) The national health development
situation, and (3) Strategic objectives of WHO and the Regional Office for South-East
Asia under the MTSP. Overall, the priorities and strategic framework presented in this
CCS are consistent with WHOs strategic objectives in meeting Thailands needs.
We hope that this CCS shall be disseminated and used by national and international
partners in health for better cooperation and collaboration in planning and implementing
relevant activities to enhance the health and well-being of the people of Thailand.
P.T. Jayawickramarajah, M.D., M.Ed., Ph.D
WHO Representative to Thailand
Foreword
WHO Country Cooperation Strategy 2008-2011 viii
Thailand ix
Executive Summary
Since the current Country Cooperation Strategy (CCS) will end in 2007, the preparation
of a new CCS is timely to cover the period of 2008-2011. In the context of a new CCS,
it is relevant to list the following important related documents that are being or have
been prepared for the corresponding period: (a) The 10
th
National Health Development
Plan, 2007-2011; (b) The WHO six-year Medium Term Strategic Plan (MTSP), 2008-
2013, which serves as an outline of WHOs strategic objectives and (c) The United
Nations Partnership Framework, Thailand (UNPAF 2007-2011), of which the WHO
Country Office is also a signatory.
Thailand is a developing country that has registered impressive successes in both
economic and social development, though all regions of the country have not registered
the same degree of advancement. The country also has a long and successful history of
health development. The Ninth Five-Year National Health Development Plan, 2001-
2006, has just been completed, and the Tenth Plan is in the final stages of completion.
The basic principles of these plans are based on a people-centered approach and
philosophy of sufficiency economy. The Thailand Human Development Index has
improved, inexorably aided by major contributions from the robust health indicators.
Almost all MDGs relating to maternal and child mortality have been achieved.
Although considerable progress and achievement has been registered, Thailand
still faces several challenges with the health situation and health development. Some
of the major challenges to advancement of health development are as follows:
(1) Important communicable diseases remain key public health concerns in
Thailand. These include malaria, dengue haemorrhagic fever, HIV/AIDS, TB
and emerging diseases, particularly avian influenza. The coordination of the
disease surveillance and epidemic response, and the efficiency of DOTS at
the peripheral level still leave room for improvement.
(2) Morbidity and mortality of major non-communicable diseases such as injuries
and mental illnesses show a rising trend. The country requires clear and
well-defined national multi-sectoral coordination policies and strategies for
the effective prevention and control of these diseases.
(3) Environmental pollution and contamination of food by hazardous substances
are still important public health issues. Occupational safety standards and
the permissible levels of hazardous substances are yet to be enumerated.
(4) Thailand has increasingly become prone to natural disasters. Although the
government is relatively self-reliant in disaster relief, WHO and the UN Disaster
Management Team have important roles to play to support the country in
WHO Country Cooperation Strategy 2008-2011 x
assessing the health situation and needs as well as coordinating joint action
for health.
(5) Cross-border health risks have become important health and political issues
over the past few years. These risks include the spread of communicable
diseases and drug-resistant pathogens, and also national security. There are
many players involved in the improvement of the living conditions and health
of migrants and refugees along the border of Thailand. Better coordination
among all involved is needed.
(6) Thailand has accorded high priority to health promotion, as is clearly reflected
in the Ninth and Tenth National Health Development Plans. The Ministry of
Public Health (MoPH) has initiated many programme and project approaches.
The Thailand Health Promotion Foundation plays an important role in
financing and advocating health promotion. However, the countrys main
challenge lies in establishing firm levels of collaboration with sectors outside
of the Ministry of Public Health.
(7) The most recent phase of health systems reform began in 2000. Several offices
and institutes were established to strengthen health systems development
and enable the reform process. For example, the National Health Systems
Research Institute (HSRI) established the Health Systems Reform Office to
function as the secretariat for the National Health Systems Reform Committee
to guide health systems development. The International Health Policy
Programme (IHPP) was established to develop and strengthen national
capacity in health policy research and international health. The National
Health Security Office (NHSO) was established in 2003 to expand coverage
of health insurance/security for those citizens who have not as yet been
covered by any government insurance scheme.
The national health budget has gradually increased from 5.8% of the total
government outlay in 1993 to 7.6% in 2004. About 60% of all health expenditure
comes from government sources compared with 40% from private sources. In 2001
the government introduced the Universal Health Care (UC) policy (the 30-Baht
scheme). In April the next year, the government announced universal health care
coverage and in 2007 universal coverage without pay was introduced. In 2004, the
UC scheme represented 75.2% of the total health insurance schemes that covered a
population of about 47 million. There are still issues concerning the quality of services,
sustainability of the schemes, and the resignation of physicians from public service that
need to be addressed.
Thailand is gradually becoming a development partner, like other middle-income
countries, by assisting other developing countries. Therefore, in terms of developmental
assistance, Thailand has received mostly technical support, but only limited financial
support, from donor agencies and countries. In relation to partnerships with developing
Thailand xi
countries, Thailand is active in a number of regional and sub-regional cooperative
initiatives in many sectors including health.
The work of WHO with Thailand is based on the WHO-Country Collaborative
Programme, which is developed on a biennial basis. The WCO focuses overall on
supporting policy development, advocacy, technical advice, and the development of
norms, standards and guidelines. In addition to the WCO, there are two WHO sub-
regional units in Thailand: a) Mekong Malaria Control Project (MMP) that was established
for coordinating malaria control activities in the countries of the Mekong Basin that
involves two WHO Regions and for coordinating border health activities, and b)
Communicable Disease Surveillance and Response (CSR) regional sub-unit that was
established to support countries to strengthen capacities in areas of epidemiology,
disease surveillance and epidemic response. The WCO has National Professional
Officers (NPO) who work in programme planning, monitoring and evaluation, HIV/
AIDS-Tuberculosis, communicable disease control and tobacco control. All other
international technical staff are assigned to work for the above two sub-units.
WHO has established a clear Global and Regional Framework, under the Tenth
General Programme of Work (GPW) and the Medium Term Strategic Plan (MTSP), and
all the offices will work to perform six core functions of WHO.
Based on the above situation analysis and extensive consultations, the following
seven strategic agendas have been identified as priorities for the next four years:
(1) To enhance primary prevention, surveillance and control of communicable
diseases and epidemics;
(2) To integrate measures to reduce the risks of non-communicable diseases
(NCDs), injuries and mental illnesses;
(3) To build capacity and partnerships for health promotion and healthy public
policy;
(4) To strengthen capacity for monitoring and evaluating health systems
development;
(5) To initiate a multi-sectoral approach to address health services for the poor
and at-risk population, including those in border and conflict areas;
(6) To promote environmental health and surveillance of environmental hazards;
(7) To strengthen the development of human resources for health through existing
networks within and outside the country.
WHO Country Cooperation Strategy 2008-2011 viii
Thailand 1
Thailand is one of the countries that has already formulated two Country Cooperation
Strategy (CCS)* reports. The first covered the period of 20022005, and it was later
updated in 2004 for 20042007. As one of the fundamental principles of the CCS, the
strategic agendas identified in these documents have been used as a basis for the
WHO country collaborative programmes and for the Organizations operations in the
country.
The CCSs were developed in close consultation with the national authorities from
within and outside the Ministry of Public Health (MoPH). Consultations were held
with most UN Agencies and other partners who are active in the health sector. As the
current CCS will end in 2007, it is timely to formulate a new CCS for the following
reasons:
(1) The Royal Thai Government (RTG) has drafted its Tenth National Health
Development Plan (20072011) which outlines its strategies and priorities
based on the vision of sufficiency economy. This will allow WHO to align
its medium-term strategies, including the planning cycle, with the strategies
and priorities of the RTG.
(2) The six-year WHO Medium-Term Strategic Plan (MTSP) based on WHOs
Eleventh General Programme of Work (GPW) 20062015 outlines the
Organizations global strategies covering the period 20082013. This exercise
can take into account the latest WHO long- and medium-term strategies
and priorities while identifying the Organizations strategic agenda for its
technical cooperation with the RTG for the period 20082011. This will also
help RTG respond, in a flexible and dynamic manner, to a changing
international health environment.
(3) The United Nations Development Assistance Framework (UNDAF), which is
referred to in Thailand as the United Nations Partnership Framework (UNPAF),
covering the period 20072011, has just been developed and fully aligned
Introduction
1
*The CCS reflects a medium-term vision of WHO for its work with a given country and defines a strategic agenda
for working with that country. The timeframe is four to six years but may be less for countries in crisis. The CCS
is the WHO instrument used to aligning with the national agenda while harmonizing with the functions of other
organizations in the UN system and other agencies in the country.
WHO Country Cooperation Strategy 2008-2011 2
with the national priorities. WHO, as agreed in the Paris Declaration, follows
the principles for alignment and harmonization of its strategies and
programmes with that of the United Nations system and other development
partners working in the area of health. Although the WHO Country Office,
Thailand did not have a distinctive role to play in the poverty reduction
strategy of UNDAF, the strategy was considered a core value and an
overlapping element that has to be integrated into WHOs strategic objectives.
Taking advantage of the opportunities stated above and in accordance with the
agreements with the national authorities, it was decided to formulate the CCS in Thailand
for WHOs cooperation with RTG over the period of 2008-2011.
Thailand 3
1. Economic and social development
In terms of social and economic development, Thailand has achieved outstanding
progress over the last few decades to emerge a middle-income country. Per capita
income in terms of Purchasing Power Parity (PPP) in 2005 was (Intl. $) 8440. Thailand
has a Human Development Index (HDI) of 0.784, which increased from 0.615 in
1975. The number of people living below the poverty line was reduced by almost two-
thirds between 1990 and 2002. The reach of education has also increased, with almost
all children attending primary school and enrolment in secondary schools rising every
year. Aided by high levels of attendance in schools, the literary rate is currently 92.6%
1
.
Despite this impressive progress, the fruits of development have not reached all
regions of the country in equal measure. While the Bangkok Metropolitan Area in
2002 had less than 2% of its population living in poverty, the incidence of poverty was
as high as 16% in the north, 17% in the north-east, and 8% in the south of the country.
Poverty rates in Narathiwat and Pattani, two of the southern-most provinces, were
18% and 23%, respectively
2
. Furthermore, drawn by Thailands economic wealth and
stability in comparison with some of its neighbours, many migrants arrived in search of
employment and a living. These migrants do not always have full access to social
services such as health care and those not registered are often vulnerable to exploitation.
The Tenth National Health Development Plan, currently in draft form, covering
the period 20072011 will follow the vision and philosophy of the Ninth Plan. This
new plan focuses on three areas for strengthening and developing the national capital
formation: (a) economic capital, (b) social capital, and (c) natural resources and the
environment. Health falls under social capital, and the health sector is considered to
be a new wave in Thailands competitive surge in the context of global trade
liberalization. While the Ninth Plan has emphasized a life-cycle health approach,
promoting healthy lifestyles, improving the quality of health care, disease prevention
and control, and preparing for the need of an ageing population, the Tenth Plan
emphasizes public and national self-reliance in health.
In the past, government administration and services had been largely centralized.
However, decentralization is now an accepted political objective and is gradually being
implemented. Efforts are already on to decentralize public services, including health,
to the 76 provinces and 876 districts, including Bangkok. This will require substantial
efforts to build capacity at the local level.
Country health and development
challenges
2
WHO Country Cooperation Strategy 2008-2011 4
2. Health policies
Thailand has had a long history of health development going back to the 13
th
Century.
More recently, the First (five-year) National Health Development Plan was initiated in
1961, and subsequent plans continued through the Ninth Plan, which covered the
period 20012006. There has been continuous change in and evolution of health
policies in response to the countrys social and health problems and in line with
international developments in health. At the end of the Seventh Plan and throughout
the Eighth Plan, WHO introduced a Health Future Studies approach to the Ministry of
Public Health. Consequently, since 1999 public sector reform, including health, has
been part of the governments agenda.
The Ninth Plan provided a clear vision of a people-centered approach and the
philosophy of a sufficiency economy. Its objectives were to: (a) promote health and
prevent and control diseases; (b) establish health security; (c) build capacity in health
promotion and health system management; and (d) establish measures in generating
knowledge through research. In 2003 Healthy Thailand was adopted as a national
agenda to be used as guidance to reducing behavioural risks and to solve major health
problems in pursuing the target Millennium Development Goals (MDGs) by 2015.
While continuing with the philosophy of sufficiency economy, the Tenth National
Health Development Plan places more emphasis on national self-reliance, quality of
services, peoples values and dignity. Its objectives are as follows:
Develop uniformity and good governance in the management of health
systems.
Accelerate the pro-active health promotion approach to develop basic
elements for good health.
Develop a health culture and ways of life with sufficiency and happiness.
Develop community health systems and a strong primary care service network.
Develop a health service system that will lead to both health care receivers
and health care providers satisfaction.
Develop health security systems with equitability, good quality, and better
distribution.
Develop individuals immune systems and readiness to minimize the impact
from diseases and risks to health.
Develop several alternative healthcare services, integrating the respective
strengths of Thai and international approaches.
Develop a foundation of health knowledge through knowledge management.
Develop societies that do not neglect sufferers and that care for the poor and
disadvantaged people with due respect for their values and human dignity.
Thailand 5
In September 2006, political developments led to the establishment of an interim
government in Thailand. The health minister subsequently announced health policies
that are in line with the Tenth National Health Development Plan. On account of the
problems that were encountered in implementing the 30-Baht health-care scheme,
universal coverage without fees was initiated. In general, health systems reform and
health security, especially social health insurance, will continue to be an important
part of the health development agenda in Thailand for the next four to five years.
3. Burden of disease and the health development situation
Along with Thailands impressive economic development, the government has
developed an effective public health system to improve the health of its population.
Since 1989, Thailands Infant Mortality Ratio (IMR) has improved from 38 per 1000
live births in 1990 to 19.8 in 2005
3
. According to the Millennium Development Goals
Report 2004, the maternal mortality rate, a good indicator of the effectiveness of a
public health system, has decreased from 36.2 per 100,000 live births in 1990 to 14 in
2002, with about 98% of births having been attended by skilled health personnel.
Thailands progress with the MDGs (Annex 5) has been so impressive that the country
has adopted targets beyond those in the MDGs, which are known as the MDG-Plus
targets. However, despite the progress made with the MDGs, challenges still remain in
those regions with a high number living in poverty and among migrant populations,
particularly in the border areas.
Thailand is witnessing a series of both demographic and epidemiologic transitions.
The total fertility rate (TFR) has dropped from 2.41 in 1990 to 1.6 in 2006 with an
average population growth rate of 0.7% in 2004-15
2
. With the reduction in
communicable diseases, improved nutritional status, and the provision for skilled birth
care, the pattern of morbidity and mortality has gradually veered towards non-
communicable Diseases (NCDs), injuries and mental illness.
3.1 Communicable diseases
While progress has been made in the reduction of communicable diseases, some
significant problems remain. These will be the focus of efforts during the next four
years, as enumerated below:
(a) HIV/AIDS: In 1991, the number of new HIV infections reached 143,000,
indicating that Thailand was on the brink of a major health crisis. The
Government, working with NGOs, mobilized effective interventions to
increase general awareness on HIV and thereby reduced the transmission of
HIV appreciably. With the number of new infections at 19,000 per annum
in 2004, Thailand is one of the few countries to make substantial progress in
fighting AIDS. Currently, of the estimated 500,000 people who are living
with AIDS, anti-retroviral drugs (ARVs) are being provided to about 100,000
of them who urgently need such treatment. With the government committal
since October 2003 to the policy of universal access to anti-retroviral drugs
WHO Country Cooperation Strategy 2008-2011 6
for AIDS patients. But with the possibility of limited funds for the same, the
authorities, in March 2007 applied compulsory licensing measures to produce
two low-price, generic HIV/AIDS drugs. Over the past three years there has
been growing concern regarding the increasing incidence of HIV/AIDS among
adolescents, almost consistent with an increasing incidence of sexually
transmitted infections (STIs).
(b) Tuberculosis: Thailand ranks 17
th
of the 22 global high-burden countries for
tuberculosis
4
. The DOTS (Directly Observed Treatment, Strategy) still requires
strengthening to ensure higher case detection and treatment success rates.
In 2004, the country achieved the 70% case detection target. However, the
treatment success rate achieved was 74% which is significantly lower than
the target of 85%. There is a need to strengthen TB programme management
and capacity to guide and oversee the implementation of TB services under
the decentralized health system. The lack of coordination between various
stakeholders including provincial administrations poses constraints to the
programme. Inadequate treatment supervision and sub-optimal drug
procurement and supply management need to be addressed. The emergence
of multi-drug resistance and a high HIV prevalence among TB patients, the issue of
TB among migrants both internal and in the border areas, are other major concerns.
The WHO estimates for tuberculosis incidence and mortality rates in Thailand
in 2005 were 142 and 19 per 100,000 population
4
respectively. These rates
are about three and 80-fold higher respectively than those reported under
the routine surveillance system, Bureau of Epidemiology
5
. However, the
surveillance report has been used for monitoring the disease trends rather
than the actual disease burden (Figure 1).
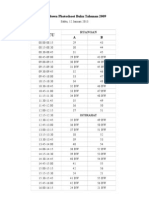
Figure 1: Morbidity and mortality of pulmonary turberculosis, Thailand, 1996-2005
Source: Bureau of Epidemiology (Surveillance Data)
Thailand 7
(c) Vector-borne diseases: The countrywide incidence of malaria has been
decreasing but problems remain in border areas, both in terms of number of
cases and drug resistance. To ensure that the disease will be controlled
completely, malaria is likely to remain a vertical programme before full
integration into the routine health services. While the country has been
successful in case management of dengue haemorrhagic fever (DHF) and in
reducing its case fatality rate to less than 1%, disease morbidity is still high
with an increasing incidence among adults. The main strategies of disease
control have been focused on eliminating vector breeding places by
schoolchildren and on improving the environment using a healthy setting
approach. Long-term results are yet to happen. It should be noted that malaria,
DHF and outbreaks of some other communicable diseases often increase
after natural disasters.
(d) Epidemic preparedness and response: In 2003 there were nine reported cases
of Severe Acute Respiratory Syndrome (SARS) and two deaths due to it in
Thailand. Following reports of human avian influenza (AI) in China and
Vietnam in 2003, Thailand reported confirmed AI outbreaks and deaths in
poultry in July 2004. The first confirmed human case of AI in Thailand occurred
in August 2004 and by the end of November 2006 25 AI cases and 17
deaths in humans were reported. In response to this, the Government
established a multi-sectoral National Committee for Avian Influenza Control,
comprising representatives from the ministries of Public Health, Agriculture,
Natural Resources and Environment, the Institute of Animal Health, the
Bangkok Metropolitan Administration and WHO. However, it is still a
challenge to extend this coordination to the sub-national level because there
is no standard policy and decentralization is still in a transitional phase.
(e) Surveillance: Outbreaks of communicable diseases can be prevented if cases
are detected early as well as the related risk factors and effective action
immediately taken. The performance and quality of disease surveillance in
the provincial health offices and public health laboratory services in provincial
hospitals are not adequate yet. This may adversely affect the timeliness and
effectiveness of responses to epidemics. Health personnel also have to be
trained in risk communication so that families and communities will know
how to avoid high-risk behaviour related to the outbreaks or epidemics.
Efforts to strengthen surveillance systems are also needed to support the
implementation of the new and revised International Health Regulations (IHR)
2005 being implemented since June 2007. The disease surveillance system
and capacity building for epidemiology are the responsibility of the Bureau
of Epidemiology, which has since long been recognized globally as one of a
few successful centres for FETP (Field Epidemiology Training Programme).
The short-course FETP may be considered in tandem with the existing two-
year course to address the increased requirements.
WHO Country Cooperation Strategy 2008-2011 8
3.2 Maternal, child and adolescent health
While Thailand has already achieved MDG targets for child and maternal mortality on
U5MR and MMR (Annex 5), Maternal and Child Health (MCH) and reproductive
health services still need strengthening for poor households and in underserved regions.
Micronutrient deficiencies, especially of iron and iodine, remain and are often associated
with increased morbidity and retarded mental growth. Special attention is required for
adolescent health since this group is susceptible to sexually transmitted diseases such
as HIV. There are separate programmes for MCH, reproductive health and adolescent
health, while target populations are the same or overlap. School health programmes
also need strengthening to support better health practices and health services need to
be adjusted to provide effective services to adolescents.
3.3 Noncommunicable diseases, injuries, and mental health
The burden of disease in Thailand is gradually shifting to noncommunicable diseases,
injuries and mental health. The greatest public health benefits are gained through
prevention of NCD (cardiovascular diseases, cancers and diabetes mellitus in particular),
injuries and mental health disorders. This can be achieved if the risk factors are identified
and appropriate interventions implemented to reduce or avoid these risk factors. In
addition, if NCDs and mental illnesses are detected at an early stage and appropriate
controls initiated, the severity of these can be reduced. It should be noted here that
the burden of noncommunicable diseases usually falls disproportionately on the poor
who often have excess exposure to risk factors and limited access to health services.
Diseases such as diabetes, cancers and of the heart are often not detected till at an
advanced level.
Aware of the increasing trends of NCDs and injuries, the RTG has placed high
priority on prevention and control initiatives. The Bureau of Noncommunicable Diseases
is responsible for NCDs, injury prevention, and tobacco and alcohol control
programmes. The Bureau has made appreciable progress in monitoring the burden of
NCDs and injuries and identifying major behavioural risk factors classified by their
provinces. The Bureau also plans to improve the collection and analysis of NCD and
injury mortality and morbidity data in order to monitor trends and evaluate the success
of interventions for risk factors. Due to the unreliability of incidence data for selected
NCDs, injuries and mental illnesses among the population, cases of hospitalization
with more accurate diagnosis are presented to ascertain the trends in the burden of
disease depicted in Figure 2 and in Annex 7.
Since the NCD and injury prevention and control programmes emphasize the
public health and primary care approaches (rather than secondary and tertiary
treatment), effective multi-sectoral collaboration is required. Clearly, traffic injury
prevention and tobacco and alcohol control programmes cannot be implemented by
the health sector alone. The RTG has demonstrated a strong commitment to the control
Thailand 9
of tobacco use and alcohol consumption by drafting legislations, particularly in the
area of advertisement. However, the major challenge ahead remains how to effectively
reduce risk behaviour (smoking and alcohol consumption) and increase regular exercise
and healthy diet.
The Department of Mental Health, Ministry of Public Health (MoPH), is in the
process of developing National Strategies on Mental Health, based on the Tenth National
Health Development Plan. To ensure the success of implementation, advocacy and
multi-sectoral collaboration are required to address the root of social problems that
are considered to be the major causes of mental illness.
3.4 Environmental health and food safety
After several reorganizations in the government, the main responsibilities for water
supply and sanitation and pollution control services have been transferred from the
Ministry of Public Health to the Ministry of Natural Resources and Environment. The
Bureau of Environmental Health limits its responsibilities to providing technical support
and capacity building, especially to local organizations. The healthy settings approach
is used to promote healthy cities with clean public toilets and healthy markets, schools
and hospitals. The Bureau is currently developing a National Environmental Health
Action Plan (NEHAP). The Health Impact Assessment (HIA) is an important tool to
minimize the adverse environmental influences on health. More support is needed to
improve national capacity for conducting HIAs. Future environmental challenges include
climate change, increasing urbanization, and the danger posed by hazardous waste
Figure 2: Morbidity rates of selected diseases/conditions in Thailand
(excluding Bangkok) 2001-2004
Source: Bureau of Policy and Strategy
WHO Country Cooperation Strategy 2008-2011 10
and chemicals, including exposure to heavy metals in the environment. These
contaminants, from industrial or natural sources, include asbestos, cadmium, arsenic
and lead. Standards have yet to be set for permissible levels of hazardous chemicals in
food, water and the environment, and surveillance of violations should be strictly
enforced.
Although occupational health has been a prime concern for Thailand for more
than 30 years, accidents and diseases caused by the workplace environment are on
the rise. Besides accidents, the most common reports of occupational health incidents
are pesticide poisoning, skin disease due to exposure to chemicals, back pain, lead
poisoning and silicosis. The government response to these problems is rather passive,
and largely confined to providing medical care or financial compensation to the victims.
Effective prevention of occupational hazards is still limited. Systems to report all
occupational health events need to be established and strengthened. Occupational
safety standards should be established and inspections undertaken to ensure compliance.
The promotion of food safety is one of the governments priorities under the
Healthy Thailand campaign. Food should be safe for domestic consumption as well as
for export. The government currently assigns responsibility to several agencies. In the
Ministry of Public Health these include the Food and Drug Agency, the Bureau of
Health Promotion, and the Bureau of Environmental Health. In the Ministry of
Agriculture, the agencies concerned are the National Bureau of Agriculture Commodities
and Food Standards, the Department of Livestock Development, and the Department
of Fisheries. Good coordination and collaboration among these concerned agencies
needs to be strengthened.
3.5 Emergencies
Thailand is prone to natural disasters, a fact demonstrated most tragically by the devastating
tsunami in December 2004 that struck the southern provinces of the country. The country
was affected again by heavy floods during August and September 2006, which hit 47
central and southern provinces and forest fire in the Northern Region in 2007. The Royal
Government of Thailand is self-reliant in disaster relief operations. WHO and the UN
Disaster Management Team have however, supported the country in assessing the health
situation and needs as well as in coordinating joint action for health.
3.6 Cross-border health risks
Thailand shares borders with the Union of Myanmar, the Lao Peoples Democratic
Republic, the Kingdom of Cambodia and Malaysia. However, border health concerns
are mainly located along the Thailand-Myanmar border and within the Mekong Basin
which spans the frontiers with Lao PDR and Cambodia. In the ten provinces of Thailand
that border Myanmar there are 401 000 registered migrants, about 117,000 registered
Thailand 11
in the camps, and an estimated 300 000 to 500 000 people who are not registered
citizens. Malaria is a particular concern in the provinces bordering Myanmar because
they account for nearly 70% of the disease burden in Thailand. On account of the
frequent and unregulated movement of migrants and their varying access to health
services, drug resistance to malaria and tuberculosis are a major concern. This is more
so since these migrants can potentially spread resistant strains to people in other parts
of the country.
Apart from six UN agencies, including WHO, about 25 international NGOs are
working along the Thailand-Myanmar border. Department for International
Development had provided funds to WHO Thailand for its Border Health Programme
during 20012005. While substantial progress had been made, the same cannot be
sustained without inter-agency collaboration and intersectoral support from the
Ministries of Public Health, Foreign Affairs, Interior and Labour.
3.7 Health promotion
Under the umbrella of Healthy Thailand, the Ministry of Public Health initiated nine
programme/project approaches. These are: Child Development, School Children in
Health Promoting Schools, Healthy Families for a Healthy Thailand, Healthy Cities,
Physical Activity and Diet for Health, Reproductive Health, Food Safety, Healthy Public
Toilet and Healthy elderly. Several health promotion programmes, campaigns and
initiatives have been launched in different parts of the country with either targeted
messages or target groups.
While there is adequate infrastructure within the MoPH to implement health
promotion practices and policies through 12 Regional Health Promotion Centres and
75 Provincial Health Offices, the biggest challenge is to establish effective collaboration
and partnerships with other sectors outside the MoPH. These include the Ministries of
Education, Interior, Social Development and Security, and Agriculture and Cooperation,
and NGOs and civil society.
Although the MoPH has a limited budget for developing health promotion, substantial
support is being provided by the Thailand Health Promotion Foundation, established by
the 2001 Health Promotion Foundation Act. Two per cent of the excise taxes on tobacco
and alcohol, or about US$ 55 million annually, has been allocated as revenue for the
Foundation, which serves as a catalyst for health promotion activities. The Foundation is
supervised by a governing board chaired by the Deputy Prime Minister.
In August 2005, the Sixth Global Conference on Health Promotion which yielded
the Bangkok Charter for Health Promotion was organized in Bangkok, Thailand.
Thailand is in the process of implementing the Bangkok Charter actions and
commitments with WHO support.
WHO Country Cooperation Strategy 2008-2011 12
3.8 Health systems
Health systems development and stewardship
Thailand has a developed health infrastructure, and good financial and health resources.
Access to basic health care has steadily increased over the past 30 years. The government
has accorded high priority to social health security to meet the goal of universal
healthcare coverage. However, efforts are needed to improve the quality of services
and to ensure the sustainability of the health system.
There is also the issue of inequitable access to quality health care in different parts
of the country. There are large gaps, for example, between Bangkok and the northeastern
region in the magnitude of health resource distribution. The Bangkok Metropolitan
Area has about one-fourth and one-tenth of the population per bed and per physician
respectively as compared to the corresponding figures for the Northeastern Region
(Table 1). While private hospital beds account for about 25% of the total, these mostly
serve a limited number of patients who can afford them.
The most recent Health Systems Reform began in 2000. The National Health
Systems Research Institute (HSRI) established the Health Systems Reform Office (HSRO)
to serve as the secretariat to the National Health Systems Reform Committee (NHSRC),
which plays a guiding role. With the involvement of society and community
organizations, the Committee drafted the National Health Bill policies to address the
health needs of the people, and to propose an essential health infrastructure that would
sustain the new health systems. After seven years of concerted efforts, the Bill was
finally approved by the Cabinet in March 2007.
The International Health Policy Programme (IHPP), a semi-autonomous
organization, was established in 2001, with joint collaboration by the Ministry of Public
Health and the HSRI. It aims to develop and strengthen national capacity in health
systems, policy research and international health. In 2003, the National Health Security
Office (NHSO) was established with the main responsibility of expanding the coverage
of health insurance or security to the people who have not been covered by any other
government health insurance scheme. It is also responsible for developing standardized
Table 1: Distribution of health resources classfied by region, 2004
Source: Report of Health Resources, Bureau of Policy and Strategy, MoPH
6
.
Thailand 13
benefit packages and financing and ensuring health security rights to target population
groups.
Considerable progress in health systems development particularly in expanding
health services notwithstanding, many national challenges remain. These include
improvement in the equity and efficiency of services among the poor and disadvantaged
groups of the population. At the same time, capacity building in the areas of financial
management, health policy development, healthcare system research, medical
anthropology, and health-related public laws is being enhanced.
With these initiatives Thailand has demonstrated its commitment to health systems
development. The National Health Act should generate healthy public policy that would
then be implemented by all sectors concerned. The National Health Act blends and
balances the philosophy of sufficiency economy and the principles of the Tenth
National Development Plan. Having learned from the experience of the World Health
Assembly, the National Assembly will aim to function effectively, in response to local
and national health needs. In conclusion, the health system in Thailand is geered
towards raising the level of happiness of the people and the quality of their life as
opposed to merely confining itself to the prevention and control of disease.
Health financing
(a) Health expenditure
The national health budget has increased from 5.8% of the total government expenditure
in 1993 to 7.6% in 2004 (Annex 3). As depicted in Table 2, about 60% of total health
expenditure comes from government sources, against 40% from private sources (out-
of-pocket and private prepaid plans). External aid in health is as low as 0.1%0.3% of
annual government health expenditure.
Table 2: Sources of health expenditure (%)
Sources: World Health Report,2006
7
.
WHO Country Cooperation Strategy 2008-2011 14
(b) Health insurance schemes
During 20022004 the budget allocation of the Ministry of Public Health for health
security accounted for 77.8% of total health budget (Annex 4). These funds supported
capitation for nationwide health services under the scheme for universal health care
coverage (UC), at that time called the 30-baht Scheme, including a special fund for
preventive and promotive health services. In 2004, the UC Scheme was estimated to
account for 75.2% of the total health insurance schemes in Thailand, and it covered a
population of about 47 million. Although the study showed the appropriate capitation
rate for the UC is Baht 1,510, the actual per capita payment in 2004 was Baht 1,309
(Table 3).
The UC scheme combined and amalgamated many healthcare coverage schemes
and only three public health insurance schemes remained. These were the Social Security
Scheme (SSS), Civil Servants Medical Benefit Scheme (CSMBS) and the UC Scheme (UCS).
Other important achievements of UC include the continuously increasing utilization
rates of health care at district hospitals (from 14% to 22%) and at primary healthcare
facilities (from 22% to 26%) in 2001 and 2003 respectively, while utilization rates at
provincial hospitals were reduced by 50%
9
. Moreover, the catastrophic health
expenditure, among the group of 10-25% of non-food expenditure on health, was
reduced from 11.9% in 1996 to 7.6 in 2002, and, among > 50% non-food expenditure
group, from 1.4% to 0.5% during the same period
10
.
Table 3: Coverage of health insurance schemes in Thailand in 2004
*Due to overlap in coverage the totals may not add up.
Sources: Jongudomsuk, NHSO Report 2004
8
.
Thailand 15
Health systems and infrastructure
Health care in Thailand is organized and provided by both the private and public
sectors. The Ministry of Public Health (MoPH) is the principal agency responsible for
promoting, supporting, controlling and coordinating all health services for the people.
In addition, there are several agencies playing significant roles in providing health
services as well as health development. These include the Ministries of Defence, Interior,
and Education, the Bangkok Metropolitan Administration, state enterprises, and the
private sector. There are also a number of non-profit agencies that provide health
services to the people. The main sources of their funding are from the MoPH subsidized
budget or from international donors.
Health services in Thailand are generally classified into five categories according
to the level of care:
Self-care level (in the household).
Primary healthcare Level (village level: midwifery centre).
Primary care level (Tambon level: health centre).
Secondary care level (District level: community hospital).
Tertiary care (provincial level: provincial/regional hospital).
According to the Decentralization Act 1999, decision-making and management
authority has been decentralized to the community in response to a demand for local
government accountability and a role in national development. Hence, at the primary
health care and primary care levels, the Tambon Administrative Organizations (TAOs)
are the responsible units for disease prevention and provision of basic health services.
During the past 10 years, the number of private clinics and hospitals in Bangkok
and other provincial cities has rapidly increased. The total number of beds in these
health facilities accounts for about 20% of the total hospital beds. The proportion of
health service utilization by private and public services is 24% and 76% respectively
6
.
3.9 Human resource for health
In 2006 there were 25,932 physicians in Thailand, which is about 12,000 less than the
optimal requirement stipulated by WHO. The inequitable distribution of physicians
and other health personnel between urban and rural, and central and other regions
particularly the north-eastern region is taken into account. According to a Ministry of
Public Health report in 2005, about 76% of the people utilize the services at primary
healthcare facilities and district hospitals, which have no specialists. However, currently
about 77.7% of available physicians are specialists, in either area, who provide services
mostly in major hospitals.
WHO Country Cooperation Strategy 2008-2011 16
The problem of an acute shortage of physicians was exacerbated by a considerable
number of physicians and nurses having resigned from the public health system. Many
of them shifted to private hospitals. There was a net loss of physicians, between 194
(22.0%) to 756 (74.6%), during 20012003
11
. The principal reasons for their resignation
were improved educational opportunities, unsatisfactory hospital management of
government, higher pays, and better work conditions
12
. The biggest exodus was seen
in the three southernmost provinces, due to continous unrest situation in the areas. If
all requests for transfer from these provinces were granted, government hospitals and
clinics would lose 70% of their staff strength
13
.
Thailand, however, has the advantage of two important international HRH
networks, namely, the South-East Asia Public Health Institution Network (SEAPHEIN),
the Asia-Pacific Action Alliance on Human Resources for Health (AAAH) and South-
East Asian Regional Association for Medical Education (SEARME) being located in the
country, whose expertise it can be fully utilized.
Thailand 17
1. Partnership with UN and other international
development agencies
Partnership in health is a key component in the strategy for the progress of health
development in Thailand. The country has established viable mechanisms for
effective coordination and collaboration on two fronts:
Thailand receives support from development partners in terms of technical
and financial resources to strengthen national capacity in specific areas in
the health sector.
Thailand is also gradually becoming a development partner, like other middle
income countries such as Peoples Republic of China, Republic of Korea,
and others, by assisting developing countries, both within and outside the
region, through its foreign policy of forward engagement. It has established
the Thai International Technical Cooperation Agency (TICA) for technical
cooperation with other countries.
With regard to the first issue above, key partners of Thailand in health include UN
agencies (ILO, IOM, UNAIDS, UNDP, UNESCO, UNFPA, UNICEF and WHO),
development banks (The World Bank and Asian Development Bank), bilateral donors
(DFID, USAID, EU, etc.) and a few international NGOs. The Ministry of Public Health
has also established the Thailand MoPHUS CDC Collaboration Center (TUC) to
strengthen national capacity in the prevention and control of epidemics and emerging
communicable diseases.
Thailand has ratified a range of UN conventions and treaties, those on human
rights, child rights (CRC), discrimination against women (CEDAW), labour, environment
and tobacco being among them. In addition to UN country offices, the country hosts
a number of UN regional offices (23 UN agencies and two development banks) which
are based in Bangkok and provide services to neighbouring countries.
The United Nations Development Assistance Framework (UNDAF), referred to as
the United Nations Partnership Framework (20072011) in Thailand, has been
developed jointly with the Royal Thai Government (RTG). In keeping with the UNs
reform, alignment and harmonization agenda, it provides a framework to jointly plan
and support, in a complementary and coordinated manner, the national plans and
Development assistance and partnerships:
Aid flow, instruments and coordination
3
WHO Country Cooperation Strategy 2008-2011 18
strategies in areas where the UN has mandated expertise and comparative advantage.
As a specialized agency, WHO is one of the signatories to this framework, which outlines
the following five areas of cooperation:
(a) Access to quality social services and protection;
(b) Decentralization and provincial/local governance;
(c) Access to comprehensive HIV prevention, treatment, care and support;
(d) Environmental and natural resources management, and
(e) Global partnership for development Thailands contribution.
With regard to the second item above, with large-scale financial contributions
from other development partners being reduced, these do not have permanent
programmes in Thailand any more. Assistance is provided to the country through
targeted areas of action and cooperation. Health-related areas that received financial
and technical cooperation from the development partners in 20042005 including
support for women and gender issues; HIV/AIDS treatment, prevention, and advocacy;
and support for improvement of land and water resources to reduce vulnerability to
natural disasters and enhance productivity.
The UNDAF 20022006 for Thailand was developed with the overarching goal
of promoting the reduction of disparity and ensuring sustainable human
development. An indicative programme resource framework, according to individual
agency mandates, was also made
14
. This is indicated in Table 4 below.
Table 4: UNDA Indicative Programme Resources Framework, 20022004
Thailand 19
2. Partnership with developing countries
Thailand has been active in a number of regional and sub-regional cooperation initiatives
with developing countries in many areas, including health. These initiatives have been
carried out through agencies, mechanism and other initiatives such as the Association
of South-East Asian Nations (ASEAN), Asia-Pacific Economic Cooperation (APEC),
Greater Mekong Sub-region (GMS), Mekong-Ganga Cooperation (MGC), Ayeyawady-
Chao Phraya-Mekong Economic Cooperation Strategy (ACMECS) and the Bay of Bengal
Initiative for Multi-Sectoral Technical and Economic Cooperation (BIMST-EC).
The Greater Mekong Sub-region, which comprises six countries along the Mekong
basin (Cambodia, PR China, Lao PDR, Myanmar, Thailand and Viet Nam), builds strong
partnerships in social and economic cooperation. In the area of health, programmes
such as the Mekong Basin Disease Surveillance (MBDS), Mekong Malaria Programme
and Human Resource Development Projects are included. The Asia-Pacific Action
Alliance on Human Resources for Health (AAAH), its main office being located in
Thailand, is a response to the international recognition of the need for global and
regional action to strengthen country planning for HRH.
Thailand is the only non-member of the Organization for Economic Co-operation
and Development (OECD) that produced a report on Millennium Development Goals
(MDG) -8: The Global Partnership for Development. This goal sets targets for increased
Official Development Assistance (ODA), ensuring access for developing countries to
technology and essential drugs.
By engaging in the South-South development cooperation and taking a leading
role in regional and sub-regional cooperation initiatives, Thailand is actively sharing
with other countries its own knowledge of what it takes to reduce poverty rapidly,
improve health and education, and confront the challenges of environmentally
sustainable development. This cooperation policy has also led to an engagement in
programme development assistance to African countries, notably in the field of HIV/
AIDS prevention, in collaboration with UNDP.
3. Technical cooperation with other countries
During 20042006, a total of 602 Fellows from all Member countries of the South-East
Asia, Western Pacific and Eastern Mediterranean Regions visited Thailand to gain
experience in different medical and health fields. Their fields of study were health
systems, primary health care, health promotion, nursing care, laboratory investigation
and epidemiology. During 20052006 about 50 Thai experts were recruited as
consultants by WHO and other international health-related agencies to work within
and outside the Region. They contributed in varied sectors including health insurance,
quality assurance of laboratory services, disaster preparedness and response, registration
of medicines, HIV/STD, dengue prevention and control, and epidemiology training.
WHO Country Cooperation Strategy 2008-2011 20
4. WHO collaborating network
Currently Thailand has 33 designated and functioning WHO Collaborating Centres
and 35 Centres of Expertise. These centres provided training to national and international
fellows, conducted studies in areas identified or stipulated by WHO, and offered
reference laboratory services. A Network for WHO Collaborating Centres and Centres
of Expertise in Thailand (NEW-CCET) was established to share experiences and
strengthen institutional capacity. The National and Regional Experts System for South-
East Asia Region (NRES) was developed under the NEW-CCET. This system includes
Thai experts and institutional databases. This is a good initiative, but to be fully functional,
it requires improvement and sustainable funding. The role of the NEW-CCET is being
reviewed.
Thailand 21
1. Work of the WHO Country Office encompasses:
Advocacy, technical advice, and technical services/support to the government,
UN agencies and other development partners on health and health-related
matters;
Partnerships and coordination with other stakeholders for effective response,
especially in tackling health issues;
Identifying Thai technical expertise and facilitating the sharing of that expertise
with neighbouring countries, other Regions, and also globally;
Providing administrative support to the Regional Office, HQ and other
Country Offices in arranging fellowships, consultations, conferences and
technical meetings and facilitating laboratory services to Bhutan, Myanmar
and Nepal under the polio eradication programme;
Disseminating WHOs policies and positions through the media and other
communication channels, and
Providing administrative support and common services to WHO sub-regional
health units that are based in Bangkok.
2. Focus of WHOs collaboration with Thailand
WHOs collaboration with Thailand is based on the WHO Country Collaborative
Programme which is developed on a biennial basis. The current CCS 20042007 was
used as a framework and guideline for the development of the biennial programme
budget and workplans in the 2004-2005 and 2006-2007 bienniums. The Country
Office focused on supporting policy development, providing technical advice, and
developing norms and guidelines. In accordance with the CCS 2004-2007 and in
continuation of some priorities from the 2004-2005 biennium, the WHO Country
Office has in the current biennium focused on the following areas of work:
Communicable disease prevention and control, including epidemic alert and
response;
Prevention and management of chronic and non-communicable diseases,
and health promotion;
Current WHO cooperation
4
WHO Country Cooperation Strategy 2008-2011 22
Health research, evidence, and health systems development;
Emergency preparedness and cross-border health;
Immunization and vaccine development;
Technical cooperation among countries, and
Health and environment.
Previous CCSs have helped to focus WHO collaboration with the RTG on a few
priority areas where the Organization has an advantage and for which it receives requests
from the government. Nevertheless, additional efforts are required to streamline the
number of activities carried out within the ambit of these broad priority programmes.
The WHO Country Office still issues a large number of contracts to implement these
activities. The administration of these contracts require considerable time and effort
on the part of the Country Office staff.
In order to ensure that the research and studies undertaken with WHO support
are applied to developing and monitoring health programmes, principal investigators
were requested, at the end of 2006, to present their work at the WHO Country Office.
Many of these were found to be valuable, and feasible to implement. Some have been
replicated within the MoPH and other related institutions. However, it will be useful to
review the studies undertaken and models developed to ensure that there is no
duplication, and that they are practical and feasible.
3. Funding of WHO collaborative programmes.
Budgetary support to carry out these programmes comes from WHOs assessed and
voluntary contributions, and from other international agencies outside WHO. The assessed
contribution for the WHO Country Programme in 20042005 was US$ 5.18 million. In
addition, about US$ 1.69 million in voluntary contribution was mobilized for Thailand
from across WHO, including US$ 281,000 for the tsunami relief operation. There has
been an increase by 11% in assessed contributions for 20062007 to US$ 5.78 million,
following the decision of the 2005 World Health Assembly to increase the assessed
contributions by Member States. In addition to this assessed contribution, the Country
Office has till date received about US$ 23 million through voluntary contributions.
4. Fellowships
From the 19981999 bienniums till the current biennium, the WHO Country Office
has provided 36 long-term fellowships to staff of the Ministry of Public Health and
university. Fellows have completed courses leading to five certificates, 17 Masters degrees
and 14 PhDs in the field of public health, HRH, health economics, health services
management, international health, health policy, health planning and financing,
epidemiology, policy analysis, health promotion, medical anthropology, health service
research, public health nutrition and Genetic Epidemiology.
Thailand 23
5. Regional Sub-units
In addition to the Country Office, WHO has two Regional Sub-units in Thailand:
Mekong Malaria Programme: This is a bi-regional project based in Thailand
to coordinate WHO activities in countries of Mekong Basin.
WHO Regional Sub-unit for Communicable Disease Control (CSR Sub-
unit): The Regional Director decided in 2005 that a CSR Regional Sub-unit
was to be established in Bangkok. The rationale behind this unit being located
outside the Regional Office was its locational advantage, its infrastructure in
terms of transport and communications, and the technical expertise that
Thailand possessed. The decision to establish a sub-unit was in keeping with
the decentralization policy initiated by the Regional Office and the felt need
to establish a regional presence in Bangkok to better interact with agencies
in that part of the Region.
The Sub-unit will operate within the broader context of supporting
countries to develop the required core capacities for: a) implementing the
International Health Regulations (IHR); b) strengthening the Field
Epidemiological Training Programme (FETP); c) the Asia-Pacific Strategy for
Emerging Diseases (APSED); d) developing early warning systems and risk
assessment of potential public health emergencies of international concern
(PHEICs) and response, and e) promoting research, particularly evaluative
research.
At the same time, Thailand will desire maximum benefit of technical
support from the CSR, and the Sub-unit will engage with the MoPH to support
other Member States as well. Although this sub-unit is established under the
Regional Offices technical and administration settings, its operations may
go beyond the Region to assist countries in the Greater Mekong Sub-region,
whenever there is a cross-border outbreak of an important disease.
6. Staffing
Thailand has a relatively small office in terms of number of technical staff. Moreover, it
is able to provide and share technical expertise, particularly with its neighbouring
countries. WHO has played an important role in identifying and facilitating this sharing.
Currently there are only two international professional staff (WR and the
Administrative Officer), six national professional officers and 13 national support staff
in the Thailand Country Office. Additionally, the Regional Sub-units have three
international Professional staff and one General Service staff. The support for the Sub-
unit is covered by funds from outside the country budget. The organogram is provided
in Annex 8.
WHO Country Cooperation Strategy 2008-2011 24
7. Office premises
The Ministry of Public Health has provided office space gratis for the WHO Country
Office as well as for the CSR Regional Sub-unit. The Mekong Regional Sub-unit is
located in the Faculty of Tropical Medicine, Mahidol University, Bangkok.
8. Information and communication technology
Although Thailand has very good communication facilities, the Country Office as well
as the CSR Sub-unit have been connected with the Global Private Network (GPN)
enabling faster connections with the Regional Office and Headquarters. It is equipped
with tele and video conference facilities. In view of Thailands strength in IT expertise,
the Regional Office may consider decentralizing the maintenance and updating of the
ITC system to the Country Office for reasons of expediency.
9. Use of CCS
Overall, the current CCS has been well utilized by the WHO Country Office to develop
workplans that align with the National Health Plan and other national health and
development frameworks. Whether the priorities identified in the previous CCSs have
informed the regional or global strategies and priorities still remains an issue.
The extent to which the priorities identified in the CCS were implemented in line
with the six core functions of WHO is presented in Table 5. The relative weight assigned,
in terms of the number of pluses (+) in the table, is based on the scope of work
undertaken in the biennium 200405 and calendar 2006.
Table 5: Performance in priority areas, in relation to
WHO core functions (20042007)
Thailand 25
1. Global challenges in health
The General Programme of Work (GPW) is the highest-level policy document of WHO.
The Eleventh GPW (2006-2015) sets out the direction for international public health
for the period of 2006 through 2015. The document notes that though there have
been substantial improvements in health over the last 50 years, significant challenges
remain, as elucidated in the following four gaps:
(a) Gaps in social justice: Clearly, poverty is a key factor that impedes access to
quality health services. In some countries, life expectancy of the poor is 20
years lower than other, more privileged members of society. Poor health and
poverty form a vicious cycle. Other factors that reduce access to services are
discrimination by ethnicity or gender and womens health, which are often
not adequately addressed.
(b) Gaps in responsibility: Health problems are no longer merely the
responsibility of those working in health, but also require positive action by
those outside the health sector. International conflicts and national crises
often lead to the disruption of social services, including healthcare.
Globalization and decisions on international trade have a direct impact on
health, especially in pharmaceuticals and the movement of health
professionals. In many countries, ministries of health often do not have the
capacity to influence adequately important causes of ill health that are outside
the purview of the health sector.
(c) Gaps in implementation: Very often the technology to implement cost-
effective interventions to improve health may be available, but is not
implemented because of paucity of funds and human resources, or the
absence of an effective health system. Available resources may often be
allocated to high-cost curative services that tend to favour urban areas, leaving
inexpensive and effective interventions in rural and remote areas neglected.
(d) Gaps in knowledge: Global advances in science and technology have
improved the effectiveness and efficiency of medical services and the
prevention and treatment of diseases. However, information about these
advances is often not available in many countries. In addition, the lack of
information about health conditions and existing rigidities in many countries
WHO policy framework Global
and regional directions
5
WHO Country Cooperation Strategy 2008-2011 26
have in turn made it difficult to formulate and manage effective health policies
and interventions. Even operational research for those most in need of health
services is generally not conducted, thereby reducing the efficiency of key
programmes.
2. Global health agenda
In order to reduce these gaps over the coming ten years, the Eleventh GPW outlines a
global health agenda consisting of seven priority areas:
Investing in health to reduce poverty;
Building individual and global health security;
Promoting universal coverage, gender equality, and health-related human
rights;
Tackling the determinants of health;
Strengthening health systems and equitable access;
Harnessing knowledge, science, and technology, and
Strengthening governance, leadership, and accountability.
The global health agenda is intended for everyone engaged in the field of health
development. WHO will contribute to this agenda by concentrating on its core functions,
which have been built on the comparative advantages of the Organization. In
accordance with the global health agenda and WHOs core functions, the Organization
has set the following priorities:
(1) Providing support to countries in moving to universal coverage with effective
public health interventions;
(2) Strengthening global health security;
(3) Generating and sustaining action across sectors to modify the behavioural,
social, economic, and environmental determinants of health;
(4) Increasing institutional capacities to deliver core public health functions under
the strengthened governance of the ministries of health, and
(5) Strengthening WHOs leadership at global and regional levels and supporting
the work of governments at the country level.
WHO will pursue these priorities through its Medium Term Strategic Plan (MTSP)
(2008-2013) and the biennium budget of the Organization. The Director-General has
clearly placed emphasis on the work of the Organization at the country level. The
Regional Offices and Headquarters have been directed to emphasize support for country
work and implement these priorities in Member States, especially where the health
needs are greatest.
Thailand 27
3. Regional policy framework
The South-East Asia (SEA) Region has the second highest population among the six
WHO Regions and has the greatest burden of disease. While there has been considerable
economic development in this Region in recent years, poverty and poor health remain
significant issues of concern. Many Member countries have faced health emergencies
of varied magnitude in the past decade and the threat of disease outbreaks always
exists. Noncommunicable diseases have also become an increasingly important cause
of morbidity and mortality in the SEA Region. Therefore, the global policy framework
of WHO is appropriate for countries of the Region with special attention towards
strengthening the capacity of Member States to support cost-effective public health
interventions.
The Regional Office has always placed strong emphasis on its work in Member
States. Of the total budget provided to the Region, 75% is allocated for countries
which is the highest ratio among the six Regions. The Regional Director for South-East
Asia has recently enhanced the delegation of authority to country offices to enable
them to plan and implement programmes with a higher degree of independence and
to be more accountable for their work. At the same time, he has emphasized that the
Regional Office staff should give the highest priority to support the work in these
countries.
WHOs core functions
Providing leadership on matters critical to health and engaging in
partnerships where joint action is needed;
Shaping the research agenda and stimulating the generation, translation,
and dissemination of valuable knowledge;
Setting norms and standards, and promoting and monitoring their
implementation;
Articulating ethical and evidence-based policy options;
Providing technical support, catalyzing change, and building sustainable
institutional capacity;
Monitoring the health situation and assessing health trends.
WHO Country Cooperation Strategy 2008-2011 28
1. Principles
The key principles for the WHO Strategic Agenda are to:
Enhance advocacy in supporting government matters critical to health, based
on WHO mandates and governing body resolutions;
Be more selective and focused in determining which health sector
programmes are to be supported;
Maintain flexibility to respond to requests as they arrive, while defining the
boundaries within which WHO will respond and focus on what the
organization can do best;
Emphasize the role of WHO as a policy adviser and broker, and differentiate
WHOs work and performance from that of the government, while continuing
to work as governments key partner in health, and
Seek out opportunities to enhance and strengthen partnerships with UN
agencies and actors, and explicitly take into account the harmonization of
programmes among development partners.
This approach will increase the effectiveness of WHO country programmes. Well-
defined priorities will help to ensure a better match between the needs of the country
and the globally agreed strategic objectives, in which WHO has a clear advantage
compared to other partners.
2. Strategic agenda
Based on the health issues and challenges identified in the situation analysis, WHOs
GPW and Medium Term Strategic Plan, and recognizing WHOs comparative advantage
identified through the consultations with national and international partners, seven
components of the strategic agenda have been jointly agreed for WHOs cooperation
with the Government of Thailand.
Strategic Agenda 1: Enhancing primary prevention, surveillance and
control of communicable diseases and epidemics
Important communicable diseases that are still major public health concerns in Thailand
include malaria and dengue haemorrhagic fever, HIV/AIDS, STI, TB and emerging
Strategic agenda: Priorities jointly agreed for WHO
cooperation in and with countries
6
Thailand 29
diseases, avian influenza in particular. In addition to disease prevention and control
interventions by the government and stakeholders, it is very important to empower
people to know how to avoid risks of contracting diseases. For national self-reliance,
the government has also announced an ambitious plan to strengthen its capacity in
vaccine production. Important strategies include:
Strengthen risk communication skills for health personnel.
Improve managerial skills and coordination in epidemic surveillance and
response, particularly at the peripheral level.
Facilitate quality assurance of laboratory investigations.
Support for monitoring directly observed treatment, short-course (DOTS),
antiretroviral therapy (ART) and malaria treatment at all levels.
Support for timely implementation of IHR.
Support for vaccine production.
Strategic Agenda 2: Integrating measures to reduce risks of non-
communicable diseases (NCDs), injuries and mental illness
NCDs are groups of chronic diseases that have common risk factors. Prevention and
control require multi-sectoral collaboration to address them collectively. The same
principles can be applied for injury prevention. National personnel require managerial
skills, especially in collaboration with multi-stakeholders and for effective
implementation of the programme. Prevention of mental illness will focus on community
mental health by promoting mental health through young children and adolescents.
Important strategies include:
Develop a policy of integrated control measures for non-communicable
diseases, injuries and mental health.
Strengthen capacity on programme management at the central and regional
levels.
Support scaling up of primary prevention and care for NCDs, injuries and
mental illness.
Standardize and systematize NCD risk factor surveillance, as well as morbidity
and mortality surveillance.
Strengthen implementation and monitoring of Global Strategy on Diet, Physical
Activity and Health and Framework Convention for Tobacco Control (FCTC).
Enhance advocacy in implementing the National Mental Health Policy.
Strategic Agenda 3: Building capacity and partnerships for health
promotion and healthy public policy
Thailand has accorded very high priority to health promotion as a most important approach
for public health implementation, as reflected in the Tenth National Health Development
WHO Country Cooperation Strategy 2008-2011 30
Plans and the National Health Act. The Ministry of Public Health is one among many key
players, and it is important that health promotion be sold to the non-health sector to
ensure the success of public health interventions. Attracting investment to health promotion
requires strong evidence of health promotion effectiveness, in terms of raising peoples
health status as well as economical gain. Important strategies include:
Advocate for healthy public policy in different sectors.
Strengthen the National Health Commission and facilitate the roadmap for
the Public Health Initiative under the National Health Act.
Strengthen implementation, evaluation and dissemination of outcomes of
Healthy Setting Approach to all sectors.
Support implementation of the recommendations of the Sixth Global
Conference on Health Promotion.
Integrate concepts and principles of health promotion into the undergraduate
medical and health training school curriculum.
Supporting demonstration and dissemination of evidence-based health
promotion effectiveness for advocacy and policy development.
Strategic Agenda 4: Strengthening capacity for monitoring and
evaluating, and for health systems development
Thailand is undergoing a transition in its health systems development. Many measures
have been initiated, especially in areas of health care financing and decentralization.
To ensure effective implementation, systematic monitoring and evaluation is required.
The Tenth National Health Development Plan and the National Health Act are now
effective. Indicators for monitoring and evaluation of the programme have to be
developed, and the programme has to be assessed as a baseline from the beginning.
Important strategies include:
Build capacity in the area of health policy development, financial
management, health care systems research, medical anthropology, and health-
related laws.
Support monitoring and evaluation of health systems performance, including
decentralization.
Support development of appropriate mechanism for national healthcare
financing.
Advocate for the national policy on trade and health, and for networking
with other countries.
Facilitate technical cooperation among countries (TCC) for global and regional
public health action.
Support the development of appropriate health infrastructure to respond to
health emergencies.
Thailand 31
Streamline essential medicines and prevent the manufacture and circulation
of counterfeit and sub-standard medicines.
Strategic Agenda 5: Multi-sectoral approach to address health services
for the poor and at-risk population, including those in border and
conflict areas
Although Thailand shares borders with Myanmar, Lao PDR, Cambodia, and Malaysia,
the health of the people on the border with Myanmar and in the conflict zones of the
three southern provinces pose the greatest concern. There are many national and
international NGOs that deal with issues concerning migrants, labour and health in
provinces along the border of Thailand and Myanmar. Understanding and collaboration
among the key players is of primary importance. This requires training and orientation
on health-related issues, particularly for all field staff. Important strategies include:
Ensure incorporation of border health issues into the National Security Policy.
Enhance coordination and collaboration among different partners, particularly
those related to border health.
Facilitate collection and dissemination of health-related information.
Build capacity in border health for all related staff
Network for improvement of health services delivery.
Strengthen disease surveillance in key areas.
Strategic Agenda 6: Promoting environmental health and surveillance
of environmental hazards
Thailand has increasingly shifted from an agricultural economy to an industrialized
one, keeping pace with the trends and competitiveness in industry among the nations
of the world. Such a surge towards industrialization brings with it problems of migration,
urbanization and environmental degradation, which sometimes assume colossal
proportions. The environment can be protected most effectively through action by
communities and local organizations. Their participation can be ensured, through
building awareness and capacity. Important strategies include:
Multi-sectoral collaboration for a healthy public policy on environmental
health.
Empower local organizations/communities for environmental protection and
detection of environmental hazards.
Support the development and implementation of environmental health
legislation.
Support the development, implementation and evaluation of the National
Environment Health Action Plan (NEHAP).
WHO Country Cooperation Strategy 2008-2011 32
Build national capacity on health impact assessment (HIA) and promote the
use of the findings for policy development.
Improve collaboration and coordination in the implementation of food safety
programmes among all sectors concerned across the board.
Strategic Agenda 7: Strengthening the development of human resources
for health through existing networks within and outside the country
During the past five years, the country has been coping with the problem of health
personnel migrating from rural to urban areas and from the public to the private sector.
This leads to inequitable access to quality health services. Although there is less migration
of public health personnel compared to those in the medical services, the public health
workforce is not in any better situation. There are inadequate numbers of qualified
public health personnel in the health systems, largely due to economic and career
reasons. It is important that the country should identify appropriate mechanisms to
address issues of human resources for health.
There is a clear strategy for health manpower development that serves the new
health reform under the Ninth National Health Development Plan. This strategy should
be continued under the Tenth Plan. Important strategies include:
Support networks for the development of the National Public Health
Workforce Profile and training institutions.
Promote studies addressing HRH development issues and generate evidence-
based information for policy development.
Support capacity building of the public health workforce in specific areas
according to the countrys needs, within and outside the country.
Advocate for the establishment of a producer-user forum to generate practical
recommendations for development of national HRH.
3. Modalities of implementation:
For technical and administrative effectiveness and efficiency in programme
implementation during the coming biennium, the modality of support will
be shifted from total project support to more direct programme
implementation support, for example, for training, workshops, consultancy
and fellowships.
The WHO Country Office will play a coordinating role in identifying and
recruiting experts required by the country, as well as a facilitating role in
recruiting Thai experts as WHO consultants to work within or outside the
country. Rosters of Thai experts will be made available on the WHO Country
Office website as well as the websites of the WHO Collaborating Centres
and the Regional Directory of Training Institutions (RDTI) in SEARO. The
Country Office will act as a coordinating centre for coordination to recruit
consultants after being initiated by the Regional Office and Headquarters.
Thailand 33
WHO has a policy of long-term (of at least six months) Fellowship support,
with degree, certificate, or diploma programmes, rather than short-term
Fellowship support. Fellowship support should be completed within the same
biennium. Considering sustainability, support will not be provided to the
same programme for more than one biennium. Exchange visits of experts
among Member countries are also encouraged.
WHO Collaborating Centres shall be more fully utilized for the placement of
Fellowships to conduct training and research. .
Since Thailand has been considered to be an ideal centre for hosting meetings,
seminars and conferences, the WHO Country Office will continue to provide
support to the Regional Office and Headquarters in coordinating the
arrangements for the same.
WHO will continue to be actively engaged with organizations of the United
Nations, and will participate in the implementation of United Nations
Partnership Framework (UNPAF) and the health cluster of Inter-Agency
Standing Committee (IASC) on UN humanitarian response and monitoring
of the progress towards the MDGs.
Emphasis will be placed on each priority area of the CCS in relation to WHOs
Core Functions as shown in Table 6 below:
Table 6: Emphasis on priority areas of the CCS 2008-2011 in relation to
WHOs core functions
WHO Country Cooperation Strategy 2008-2011 34
1. Introduction
Compared to the period of the current CCS (2004-2007), there are three major issues
that may have implications for the WHO Secretariat, namely (a) Establishment of the
Regional Sub-unit for Communicable Disease Control and Surveillance (CSR) attached
to the WHO Country Office, (b) Change of staff composition, (c) Change of the
programme planning and implementation process, from setting general objectives to
outlining strategic objectives. These implications include staffing, allocation of financial
resources, information support and follow-up of programme implementation.
2. Staffing: Current and future
Unlike the other countries of the SEA Regions, Thailand is nearly self-sufficient in the
availability of experts in several health fields. The roles of the WHO Country Office in
supporting health development include both technical coordination and direct technical
support. Most of the WHO technical staff in the Country Office are National Professional
Officers (NPOs) instead of internationally-recruited staff. There are six NPOs who are
responsible for (a) programme planning and management, (b) programme monitoring
and evaluation, (c) endemic communicable diseases, (d) HIV/AIDS and tuberculosis
(e) surveillance of tobacco control and, (f) tobacco control. One international staff has
been assigned for the Border Health Programme and for coordinating the Malaria
Mekong Project.
While CSR regional sub-unit and Mekong Malaria Programme (MMP) are
administered and use common services with the Country Office, all Professional staff
are under the technical supervision of the Director, CDS, SEARO. The Coordinator
MMP is also responsible, as team leader, for the Border Health Programme.
To build the technical and managerial capacities of WHO county staff, the Regional
Office encourages horizontal collaboration among Member countries, with technical
supervision or support from the Regional Office, when required. Periodic training and
development of country staff, particularly on programme planning, monitoring and
evaluation, is needed.
Implementing the strategic agenda: Implication
for WHO Secretariat, follow-up and next step at
each level
7
Thailand 35
While staff of the Thailand Country Office have to provide support to their national
counterparts in implementing WHO Country Collaborative Programmes, they also
have to provide administrative support to HQ, the Regional Office as well as other
Country Offices during various consultations, meetings and conferences. Whenever a
programme requires an authority in a particular health area, a suitable national expert
would be the preference of the WHO Country Office and a few government staff may
be recruited for brief periods to collaborate on programme implementation.
3. Financial allocation
It is anticipated that there will be zero growth in the regular budget for the 2008-2009
and 2010-2011 bienniums compared to the current biennium, and additional voluntary
contribution (VC) resources are therefore required. In addition to VC received from
HQ, it is important that the Country Office should build staff capacity to be able to
support the country to mobilize resources to implement important programmes and
activities. With the advantage of the CSR Sub-unit being physically located in the
Ministry of Public Health, it is expected that Thailand may obtain a substantial amount
of VC to support the prevention and control of epidemic communicable diseases,
particularly avian influenza.
Thailand has an open policy for multi-country activities and is ready to provide
country budget support to some countries according to their needs. This, however,
requires better advanced planning to avoid uncertainty and delayed implementation.
4. Information and communication support
Being the hub of coordination and collaboration activities for many WHO collaborative
programmes, the Thailand Country Office requires support to improve the information
and communication systems. The Country Office must regularly update and improve
the WHO Thailand website, including its technical contents.
It is expected that development of the Global Management System (GSM) will be
completed and shall be used as a central tool for all WHO information systems during
this CCS period. Past experiences with AMS and problems in reconciling routine
technical and financial implementation should be considered as lessons learned. To
avoid interruption of routine work, timely support for updating hardware and software
and adequate training of country staff during the transitional period is crucial.
5. Implementation of the strategic agenda
(a) Role of the Country Office:
The WHO Thailand Country Office will provide advocacy support to government
policy within the organizations mandate, offer technical support, and coordinate
WHO Country Cooperation Strategy 2008-2011 36
programme implementation, primarily to inform about capacity building; encourage
an evidence-based approach; promote research, monitoring, and evaluation; and
facilitate inter-country collaboration. Another important role of the WHO Country
Office would be to support the country in mobilizing resources.
(b) Role of the Regional Office:
In spite of the decentralization of authority from the Regional Office to the Country
Office, technical support from the Regional Office, particularly in areas where national
and Country Office expertise is not available, will still be required. This includes
tuberculosis programme management, NCD programme management, preparation
for the implementation of GSM, and the development of a National Environmental
Health Action Plan (NEHAP) and National Health Impact Assessment (HIA) and vaccine
production endeavours. The Regional Office should also provide support and
coordination for some MCAs and some activities that involve countries outside the
South-East Asian Region.
(c) Role of Headquarters:
In consultation with the Regional Office, Headquarters may be requested to provide
support to the Country Office in the following areas:
Demonstration and documentation of effectiveness of health promotion;
Evaluation of health systems reform;
Studies on the implications of trade on health and health systems, and
Acquisition of new technology, production of medicines and vaccines.
Headquarters should also play a key role in mobilizing resources for important
strategic areas where the regular budget is limited, for example, health promotion,
injury, environmental health, and health systems development.
Thailand 37
Annex 1
National health development data
Indicator Unit Source
Finance
General government expenditure on health as a percentage
of total expenditure on health
61.6
General government expenditure on health as a percentage
of total government expenditure
13.6
Per capita total expenditure on health at average exchange
rate (US$)
76
Per capita total expenditure on health in dollars 260
WHR 2006
7
Per capita GDP at average exchange rate (US$) 2,490
Per capita GDP in international dollars 7,930
World Development
Indicators Database,
World Bank, 18 April
2006
15
Per capita government expenditure on health at average
exchange rate (US$)
47
Per capita government expenditure on health in
international dollars
160
Prepaid plans as a percentage of private expenditure on
health
14.6
Private expenditure on health as a percentage of total
expenditure on health
38.4
Out-of-pocket expenditure as a percentage of private
expenditure on health
74.8
Social security on health as a percentage of general
government expenditure on health
32
Total expenditure on health as a percentage of GDP 3.3
WHR 2006
7
Total expenditure on health as a percentage of GDP 6.12
Thailand Health Profile
(2001-2004)
16
Human resources
Health workers (rate per 1000 population)
Physicians 22,435 (0.37)
Nurses 171,605 (2.82)
Midwives 872 (0.01)
Public & environmental health workers 2,151 (0.04)
WHR 2006
7
Service delivery
In-patient beds per 1000 population 2.13
Physician: Hospital beds 1 : 7
Report on Health
Resource and Survey
Data 2004
6
WHO Country Cooperation Strategy 2008-2011 38
Annex 2
Strategic objectives and their scope under MTSP
2008-2013
Strategic objective Scope of strategic objective
1. To reduce the health,
social and economic
burden of communicable
diseases
The work under this Strategic Objective focuses on prevention,
early detection, diagnosis, treatment, control, elimination and
eradication measures to combat communicable diseases that
disproportionately affect poor and marginalized populations.
The diseases to be addressed include, but are not limited to
vaccine-preventable, tropical, zoonotic and epidemic-prone
diseases, excludingHIV/AIDS, tuberculosis and malaria.
2. To combat HIV/AIDS,
malaria and tuberculosis
The work under this Strategic Objective will focus on scaling-up
and improving HIV/AIDS, TB and malaria prevention, treatment,
care and support interventions so as to achieve universal access,
including among high-burden populations, women, infants,
children, adolescents, poor and vulnerable groups; advancing
related research; addressing key bottlenecks that are currently
impeding intervention access, use and quality; and contributing
to the broader strengthening of health systems.
3. Prevent and reduce
disease, disability and
premature death from
chronic noncommunicable
conditions, mental
disorders, violence and
injuries
The work under this Strategic Objective focuses on policy
development, programme implementation, monitoring and
evaluation, strengthening of health and rehabilitation systems
and services, implementation of prevention programmes and
capacity building in the area of chronic noncommunicable
conditions, including cardiovascular diseases, cancer, chronic
respiratory diseases, diabetes, hearing and visual impairment
and genetic disorders, as well as mental, behavioural,
neurological and psychoactive substance use disorders, and
injuries due to road traffic accidents, drowning, burns,
poisoning, falls, violence in the family, community or between
organized groups, and disabilities from all causes.
4. To reduce morbidity and
mortality and improve
health during the key stages
of life, including pregnancy,
childbirth, neonatal period,
childhood and adolescence,
while improving sexual and
reproductive health and
promoting active and
healthy ageing for all
individuals using a life-
course approach and
addressing equity gaps
The work undertaken under this Strategic Objective will focus
on action towards ensuring universal access to and coverage of
effective public health interventions for maternal, newborn,
child, adolescent, and sexual and reproductive health, with
emphasis on addressing gender inequality and health equity
gaps; development of evidence-based, gender-sensitive,
coordinated and coherent approaches to addressing the needs
at key stages of life and improving sexual and reproductive
health, using a life-course approach; fostering synergies between
maternal, newborn, child, adolescent, sexual and reproductive
health along with other public health programmes, and
supporting action to strengthen health systems; and formulation
and implementation of policies and programmes that promote
healthy and active ageing for all individuals.
Thailand 39
Strategic objective Scope of strategic objective
5. To reduce the health
consequences of
emergencies, disasters,
crises and conflicts, and
minimize their social and
economic impact
Joint efforts of the Member States and the Secretariat regarding
this Strategic Objective encompass the following aspects: Health
sector emergency preparedness, intersectoral action for risk and
vulnerability reduction within the framework of the International
Strategy on Disaster Reduction, response to the health needs
(including nutrition as well as water and sanitation) of
emergencies and crises, needs assessment of affected
populations, transition and recovery health actions in post-
conflict and post-disaster situations, fulfilling the mandate of
WHO within the framework of Humanitarian Reform, global
alert and response system for environmental and food safety-
related public health emergencies, threat-specific risk reduction
along with preparedness and response programmes for such
emergencies.
6. To promote health and
development, prevent and
reduce risk factors for
health conditions associated
with tobacco, alcohol, drugs
and psychoactive substance
use, unhealthy diets,
physical inactivity and
unsafe sex
The work under this Strategic Objective focuses on integrated,
comprehensive, multi-sectoral and multidisciplinary health
promotion processes and approaches across all relevant WHO
and country programmes, and the prevention and reduction of
six major risk factors: Use of tobacco, alcohol, drugs and other
psychoactive substances, unhealthy diet and physical inactivity
and unsafe sex.
The main activities involve capacity building for health
promotion across all relevant programmes, risk factor
surveillance, the development of ethical and evidence-based
policies, strategies, interventions, recommendations, standards
and guidelines for health promotion, and the prevention and
reduction of the major risk factors.
7. To address the
underlying social and
economic determinants of
health through policies and
programmes that enhance
health equity and integrate
pro-poor, gender-
responsive and human
rights-based approaches
The work under this Strategic Objectivefocuses on leadership in
intersectoral action on the broad social and economic
determinants of health; improvement of population health and
health equity by better meeting the health needs of the poor,
vulnerable and excluded social groups; connections between
health and various social and economic factors (labour, housing
and educational circumstances; trade and macroeconomic
factors; and the social status of various groups such as women,
children, the elderly, and ethnic minorities); development of
policies and programmes that are ethically sound, responsive to
gender inequalities, effective in meeting the needs of the poor
and other vulnerable groups, and consistent with human rights
norms.
8. To promote a healthier
environment, intensify
primary prevention and
influence public policies in
all sectors so as to address
the root causes of
environmental threats to
health
This Strategic Objective is aimed at addressing and reducing a
broad range of traditional, modern and emerging health and
environmental risks. Its purpose is to encourage strong health
sector leadership for primary prevention of disease through
environmental management as well as support strategic direction
and guidance to mobilize non-health sector actors about how
their policies and investments can lead to win-win development
strategies that also benefit health.
WHO Country Cooperation Strategy 2008-2011 40
Strategic objective Scope of strategic objective
The work undertaken in this Strategic Objective will focus on the
assessment and management of environmental and occupational
health risks, including such risks as unsafe water and inadequate
sanitation; indoor air pollution and solid fuel use; and disease
vector transmission. The scope of this Strategic Objective also
includes: health risks related to change in the global
environment (e.g. climate change and biodiversity loss);
development of new products and technologies (e.g.
nanotechnology); consumption and production of new energy
sources and the increasing number and use of chemicals; and
also health risks related to changes in lifestyles, urbanization and
working conditions (e.g. deregulation of labour, an expanding
informal sector and the export of hazardous working practices to
poor countries).
9. To improve nutrition,
food safety and food
security throughout the life-
course and in support of
public health and
sustainable development
The work under this Strategic Objective focuses on nutritional
quality and safety of foods; promotion of healthy dietary
practices throughout the life-course, starting with pregnant
women and including breastfeeding and adequate
complementary feeding, and considering diet-related chronic
diseases; prevention and control of nutritional disorders,
including micronutrient deficiencies, especially among the
biologically and socially vulnerable, with emphasis on
emergencies, and in the context of HIV/AIDS epidemics;
prevention and control of zoonotic and non-zoonotic foodborne
diseases; stimulation of intersectoral actions promoting the
production and consumption of, and access to, food of
adequate quality and safety; and promotion of higher levels of
investment in nutrition, food safety and food security at the
global, regional and national levels.
10. To improve health
services through better
governance, financing,
staffing and a management
informed by reliable and
accessible evidence and
research
The work to be undertaken as part of this Strategic Objective
will enhance the way health systems perform in response to the
needs and demands of the population. It is underpinned by the
principles of Primary Health Care and Health for All, and a
concern to reduce inequity in access to, and eliminate exclusion
from the benefits of, health care.
It seeks to equitably expand access across the range of services
needed to improve health outcomes and respond to legitimate
demand for care, by matching service response to needs and
demand, by increasing organizational and managerial capacities
of institutions and provider networks, and by strengthening
informed demand; and covers the organization and
management of all population-based and personal health
services individual providers, facilities and provider networks;
public, private and voluntary; at all levels, from those within the
community to tertiary hospitals and specialized services.
Thailand 41
Strategic objective Scope of strategic objective
It is concerned with the promotion of all aspects of quality in
relation to service delivery: patient- and community-
centeredness, responsiveness, continuity of care, as well as
safety, effectiveness and efficiency; with overcoming the
fragmentation that results from the multiplication of disease
specific programmes and initiatives, in ways that are tailored to
local and national circumstances and priorities; and anticipating
how technological innovation, changing needs and evolving
demand will influence service delivery.
11. To ensure improved
access, quality and use of
medical products and
technologies
Medical products include medicines, vaccines, blood and blood
products, cells and tissues of mostly human origin,
biotechnology products, traditional medicines and medical
devices. Technologies include diagnostic tests, imaging and
laboratory tests. The work undertaken under this Strategic
Objective will focus on improving equitable access (as measured
by availability, price and affordability) to essential medical
products and technologies of assured quality (including safety,
efficacy and cost-effectiveness), as well as their sound and cost-
effective use. The sound use of products and technologies
focuses on evidence-based selection; prescriber and patient
information; appropriate diagnostic, clinical and surgical
procedures; vaccination policies; supply systems, dispensing and
injection safety and blood transfusions. Information includes
clinical guidelines, independent product information and ethical
promotion.
12. To provide leadership,
strengthen governance and
foster partnership and
collaboration in
engagement with countries,
to fulfil the mandate of
WHO in advancing the
Global Health Agenda as
set out in the Eleventh
General Programme of
Work
This Strategic Objective facilitates the work of WHO vis-a-vis all
other Strategic Objectives. Responding to priorities in the
Eleventh General Programme of Work, it recognizes that the
context for international health has changed significantly. The
scope of this objective covers three broad, complementary
areas: leadership and governance of the Organization; WHO's
support for, presence in, and engagement with individual
Member States; and the Organization's role in bringing the
collective energy and experience of Member States and other
actors to bear on health issues of global and regional
importance.
The main innovation implicit in this objective is that it seeks to
harness the depth and breadth of WHO's country experience in
order to influence global and regional debates thereby to
influence positively the environment in which national policy-
makers work, and contribute to the attainment of the health-
related Millennium Development Goals and other
internationally agreed upon health-related goals.
WHO Country Cooperation Strategy 2008-2011 42
Strategic objective Scope of strategic objective
13. To develop and sustain
WHO as a flexible and
learning Organization,
enabling it to carry out its
mandate more efficiently
and effectively
The scope of this Strategic Objective covers the functions that
support and enable the work of the Secretariat in countries,
regional offices and Headquarters. The work under this
objective is organized according to the following: entire results-
based management framework and processes, from strategic and
operational planning and budgeting to performance monitoring
and evaluation; management of financial resources through
monitoring, mobilization and coordination at an Organization-
wide level, ensuring an efficient flow of available resources
throughout the Organization; management of human resources,
including human resource planning; recruitment; staff
development and learning; performance management; and
conditions of service and entitlements; provision of operational
support, ranging from the management of infrastructure and
logistics; language services; staff and premises security; staff
medical services; to the management of information technology;
ensuring that there is proper accountability and governance
mechanisms in place across all areas.
In addition, the Strategic Objective covers a broad institutional
reform agenda that will ensure that the above functions are
continuously strengthened and able to provide better, more
efficient and cost-effective support to the rest of the
Organization. This agenda is closely linked to broader reforms
within the United Nations system at both the country and global
level.
Thailand 43
Source: Bureau of Policy and Strategy, Ministry of Public Health, Thailand.
Notes:
(1) MoPH budget figures have include the budget of other agencies under MoPH supervision, i.e. Health
Systems Research Institute and National Health Security Office.
(2) The number in ( ) includes foreign loans for health programmes in 1997-2001.
(3) Since FYs 1995-2001, MoPH has received a supplementary budget for health insurance cards, called
health insurance revolving fund subsidies which were previously included in the MoPHs budget.
(4) Since the FY 2002, the MoPH has received a budget as Health Insurance Revolving Fund instead of
Health Card Revolving Fund. The MoPH continues to administer the revolving fund of the National
Health Security Office for the first three years, after the National Health Security Act came into force.
(5)
a
Consumer price index as of January 2004.
(6) The Health Insurance Revolving Fund does not include personnel and operating costs.
Annex 3
MoPH budget in present value and real terms
(in million baht)
(Extracted from Thailand Health Profile 20012004)
Year
MoPH
budget
Health
insurance
revolving
funds
Total
MoPH
budget
(present
value)
Consumer
price
index
(1994 =
100)
Budget
of 2004
value
Increase/
decrease
from
previous
year
Percentage
of National
Budget
1992 24 640 24 640 92.1 36 572
1993 32 898 32 898 95.1 47 289 +29.3 5.8
1994 39 319 39 319 100 53 749 +13.7 6.3
1995 45 103 730 45 833 105.8 59 219 +10.2 6.4
1996 55 236 625 55 861 112.0 68 180 +15.1 6.7
1997 66 544 1 030
67 574
(68 934)
118.2
78 150
(79 723)
+14.6
(+16.9)
7.3
(7.4)
1998 62 625 1 080
63 705
(65 065)
127.8
68 141
(69 596)
-12.8
(-12.7)
7.7
(7.8)
1999 57 171 2 056
59 277
(62 787)
128.2
63 154
(66 950)
-7.3
(-3.8)
7.2
(7.6)
2000 58 426 2 215
60 641
(63 001)
130.2
63 668
(66 146)
+0.8
(-1.2)
7.1
(7.3)
2001 58 697 2 400
61 097
(61 563)
132.3
63 129
(63 610)
+0.8
(-3.8)
6.7
(6.8)
2002 43 311 27 612 70 923 133.2 72 787 +15.3 6.9
2003 41 996 32 138 74 134 135.7 74 680 +2.6 7.4
2004 45 147 32 578 77 720 136.7
a
77 720 +4.1 7.6
WHO Country Cooperation Strategy 2008-2011 44
Source: Bureau of Policy and Strategy, Ministry of Public Health, Thailand.
Note:
a
For FY 2003, the budget for the disease prevention/ control and health promotion decreased as the Department
of Health had transferred its programme on environmental surveillance and analysis, and water supply provision
to the Ministry of Natural Resource and Environment, according to bureaucratic policy.
b
For FY 2004, budget for the disease prevention/ control and health promotion also decreased as the Department
of Health has revised its role and thus the budget for disease prevention/ control and health promotion under the
health service programme has been shifted to the health systems component of the Health System Development
Support Programme.
Annex 4
Health budget allocation for major types of
programmes during the first half of the Ninth
National Health Development Plan (in million baht)
(Extracted from Thailand Health Profile 20012004)
2002 2003 2004
Type of programmes
Amount Amount
Increase/
decrease
from
2002
Amount
Increase/
decrease
from
2003
Proportion
(%)
1) Universal health
security
53 022.9 57 697.2 +8.8 60 431.2 +4.7 77.8
2) Disease
prevention/control
and health
promotion
7 619.9 6 292.0
a
NA 4 951.2
b
NA 6.4
3) Health systems
development
1 519.6 1 674.0 +10.2 2 474.5 NA 3.2
4) Support for training
and development of
personnel
1 501.5 1 464.6 -2.4 1 459.9 +2.1 1.9
5) Standard and quality
of health services
and products
812.9 819.6 +0.8 1 085.0 +32.4 1.4
6) AIDS prevention and
control
698.7 885.1 +26.7 1 355.1 +53.1 1.7
7) Drug abuse
prevention and
resolution
524.7 538.2 +2.6 1 100.1 +104.4 1.4
8) Thai traditional and
alternative
medicines
39.1 73.7 +88.5 120.1 +63.0 0.2
9) Medical
rehabilitation
services for patients
and the disabled
65.7 79.5 +21.0 82.1 +3.3 0.1
Thailand 45
Annex 5
Thailands scorecard on MDG Targets (Goal 1-7)
Source: Thailand Millennium Developemtn Goals Report 2004
17
.
Target Scorecard Remarks
1. Halve, between 1990 and
2015, the proportion of people
living in extreme poverty
Already achieved Poverty incidence reduced from
27.2% in 1990 to 9.8% 2002.
2. Halve, between 1990 and
2015, the proportion of people
who suffer from hunger
Already achieved Proportion of population under food
poverty line dropped from 6.9%to
2.2%between 1990-2002, and the
prevalence of underweight children
under five dropped from 18.6%to
8.5%between 1990-2000.
3. Ensure that by 2015, boys and
girls alike will be able to
complete a full course of
primary schooling
Highly likely Gross enrolment ratio and the
retention rate indicate that it is
likely that Thailand will achieve
universal primary education well
ahead of 2015.
4. Eliminate gender disparity in
primary and secondary
education, preferably by 2005,
and in all levels of education no
later than 2015
Already achieved Thai girls and boys have had equal
education opportunity. There is a
small gender gap at the primary
level. Girls are outnumbering boys
in higher education.
5. Reduce by two thirds, between
1990 and 2015, the under-five
mortality ratio
Not applicable Given the low starting point 1990,
this target is considered not feasible
and therefore not applicable. The
new feasible target is adopted under
the MDG Plus.
6. Reduce by three-quarters,
between 1990 and 2015, the
maternal mortality ratio
Not applicable Given the low starting point 1990,
this target is considered not feasible
and therefore not applicable. The
new feasible target is adopted under
the MDG Plus.
7. Have halted by 2015 and
begun to reverse the spread of
HIV/AIDS
Already achieved Yearly new infectionshave dropped by
over 80%since 1991. HIV, however
continuesto spread amongsome groups.
Youngpeople continue to be vulnerable.
8. Have haltedby 2015 and
begun to reverse the incidence
of malaria and other major
diseases
Already achieved for malaria Achieved for malaria. The disease is
an area-specific problem, and has
been effectively managed.
9. Integrate the principles of
sustainable development into
country policies and
programmes and reverse the
loss of environmental resources
Potentially Principles of sustainable
development, partnership and
public participation have been
integrated into country policies and
programmes. But reversing the loss
of environmental resources is still
Thailands greatest challenge.
10. Halve by 2015 the proportion
of people without sustainable
access to safe drinking water
and basic sanitation
Already achieved Very close to universal access.
11. By 2020 to have achieved a
significant improvement in the
lives of at least 100 million
slum-dwellers (globally)
Likely Most Thai people, includingslum-
dwellers, have secure tenure. Various
measureshave been implemented and
more are underway to improve the slum
livelihood.
WHO Country Cooperation Strategy 2008-2011 46
Annex 6
Organogram Ministry of Public Health
M
i
n
i
s
t
r
y
o
f
P
u
b
l
i
c
H
e
a
l
t
h
P
r
o
f
e
s
s
i
o
n
a
l
C
o
u
n
c
i
l
s
N
a
t
i
o
n
a
l
H
e
a
l
t
h
B
o
a
r
d
O
f
f
i
c
e
o
f
t
h
e
M
i
n
i
s
t
e
r
P
e
r
m
a
n
e
n
t
S
e
c
r
e
t
a
r
y
C
l
u
s
t
e
r
o
f
M
e
d
i
c
a
l
S
e
r
v
i
c
e
s
D
e
v
e
l
o
p
m
e
n
t
D
e
p
u
t
y
P
e
r
m
a
n
e
n
t
S
e
c
r
e
t
a
r
y
C
l
u
s
t
e
r
o
f
P
u
b
l
i
c
H
e
a
l
t
h
D
e
v
e
l
o
p
m
e
n
t
D
e
p
u
t
y
P
e
r
m
a
n
e
n
t
S
e
c
r
e
t
a
r
y
C
l
u
s
t
e
r
o
f
P
u
b
l
i
c
H
e
a
l
t
h
S
e
r
v
i
c
e
s
S
u
p
p
o
r
t
D
e
p
u
t
y
P
e
r
m
a
n
e
n
t
S
e
c
r
e
t
a
r
y
O
f
f
i
c
e
o
f
t
h
e
P
e
r
m
a
n
e
n
t
S
e
c
r
e
t
a
r
y
B
u
r
e
a
u
o
f
C
e
n
t
r
a
l
A
d
m
i
n
i
s
t
r
a
t
i
o
n
I
n
f
o
r
m
a
t
i
o
n
a
n
d
C
o
m
m
u
n
i
c
a
t
i
o
n
T
e
c
h
n
o
l
o
g
y
C
e
n
t
r
e
P
r
a
b
o
r
o
m
a
r
j
c
h
a
n
o
k
I
n
s
t
i
t
u
t
e
o
f
H
e
a
l
t
h
M
a
n
p
o
w
e
r
D
e
v
e
l
o
p
m
e
n
t
B
u
r
e
a
o
f
I
n
s
p
e
c
t
i
o
n
a
n
d
E
v
a
l
u
a
t
i
o
n
B
u
r
e
a
o
f
P
o
l
i
c
y
a
n
d
S
t
r
a
t
e
g
y
P
r
o
v
i
n
c
i
a
l
A
d
m
i
n
i
s
t
r
a
t
i
o
n
P
r
o
v
i
n
c
i
a
l
P
u
b
l
i
c
H
e
a
l
t
h
O
f
f
i
c
e
s
D
i
s
t
r
i
c
t
H
e
a
l
t
h
O
f
f
i
c
e
s
D
e
p
a
r
t
m
e
n
t
o
f
M
e
d
i
c
a
l
S
e
r
v
i
c
e
s
O
f
f
i
c
e
o
f
t
h
e
S
e
c
r
e
t
a
r
y
P
e
r
s
o
n
n
e
l
D
i
v
i
s
i
o
n
F
i
n
a
n
c
e
D
i
v
i
s
i
o
n
P
l
a
n
n
i
n
g
D
i
v
i
s
i
o
n
N
o
p
p
a
r
a
t
R
a
j
a
t
h
a
n
e
e
H
o
s
p
i
t
a
l
M
e
t
t
a
p
r
a
c
h
a
r
a
k
H
o
s
p
i
t
a
l
(
W
a
t
R
a
i
K
h
i
n
g
)
R
a
j
a
v
i
t
h
i
H
o
s
p
i
t
a
l
L
e
r
d
s
i
n
H
o
s
p
i
t
a
l
P
r
i
e
s
t
H
o
s
p
i
t
a
l
S
i
r
i
n
d
h
o
r
n
N
a
t
i
o
n
a
l
M
e
d
i
c
a
l
R
e
h
a
b
i
l
i
t
a
t
i
o
n
C
e
n
t
r
e
I
n
s
t
i
t
u
t
e
o
f
D
e
n
t
i
s
t
r
y
I
n
s
t
i
t
u
t
e
o
f
P
a
t
h
o
l
o
g
y
P
r
a
s
a
t
N
e
u
r
o
l
o
g
i
c
a
l
I
n
s
t
i
t
u
t
e
N
a
t
i
o
n
a
l
C
a
n
c
e
r
I
n
s
t
i
t
u
t
e
T
h
a
n
y
a
r
a
k
I
n
s
t
i
t
u
t
e
C
h
e
s
t
D
i
s
e
a
s
e
I
n
s
t
i
t
u
t
e
I
n
s
t
i
t
u
t
e
o
f
D
e
r
m
o
t
o
l
o
g
y
I
n
s
t
i
t
u
t
e
o
f
G
e
r
i
a
t
r
i
c
M
e
d
i
c
i
n
e
Q
u
e
e
n
S
i
r
i
k
i
t
N
a
t
i
o
n
a
l
I
n
s
t
i
t
u
t
e
o
f
C
h
i
l
d
H
e
a
l
t
h
B
u
r
e
a
u
o
f
N
u
r
s
i
n
g
B
u
r
e
a
u
o
f
M
e
d
i
c
a
l
T
e
c
h
n
i
c
a
l
D
e
v
e
l
o
p
m
e
n
t
D
e
p
a
r
t
m
e
n
t
f
o
r
D
e
v
e
l
o
p
m
e
n
t
o
f
T
h
a
i
T
r
a
d
i
t
i
o
n
a
l
a
n
d
A
l
t
e
r
n
a
t
i
v
e
M
e
d
i
c
i
n
e
O
f
f
i
c
e
o
f
t
h
e
S
e
c
r
e
t
a
r
y
D
i
v
i
s
i
o
n
o
f
A
l
t
e
r
n
a
t
i
v
e
M
e
d
i
c
i
n
e
I
n
s
t
i
t
u
t
e
o
f
T
h
a
i
T
r
a
d
i
t
i
o
n
a
l
M
e
d
i
c
i
n
e
D
e
p
a
r
t
m
e
n
t
o
f
M
e
n
t
a
l
H
e
a
l
t
h
O
f
f
i
c
e
o
f
t
h
e
S
e
c
r
e
t
a
r
y
P
e
r
s
o
n
n
e
l
D
i
v
i
s
i
o
n
F
i
n
a
n
c
e
D
i
v
i
s
i
o
n
P
l
a
n
n
i
n
g
D
i
v
i
s
i
o
n
S
o
c
i
a
l
M
e
n
t
a
l
H
e
a
l
t
h
D
i
v
i
s
i
o
n
S
r
i
t
h
u
n
y
a
P
s
y
c
h
i
a
t
r
i
c
H
o
s
p
i
t
a
l
M
e
n
t
a
l
H
e
a
l
t
h
R
e
g
i
o
n
a
l
C
e
n
t
r
e
s
1
-
1
2
G
a
l
y
a
r
a
j
a
n
a
g
a
r
i
n
d
r
a
I
n
s
t
i
t
u
t
e
S
o
m
d
e
t
C
h
a
o
p
r
y
a
I
n
s
t
i
t
u
t
e
o
f
P
s
y
c
h
i
a
t
r
y
R
a
j
a
n
u
k
u
l
M
e
n
t
a
l
H
e
a
l
t
h
R
e
t
a
r
d
a
t
i
o
n
I
n
s
t
i
t
u
t
e
M
e
n
t
a
l
H
e
a
l
t
h
T
e
c
h
n
i
c
a
l
D
e
v
e
l
o
p
m
e
n
t
B
u
r
e
a
u
D
e
p
a
r
t
m
e
n
t
o
f
D
i
s
e
a
s
e
C
o
n
t
r
o
l
O
f
f
i
c
e
o
f
t
h
e
S
e
c
r
e
t
a
r
y
P
e
r
s
o
n
n
e
l
D
i
v
i
s
i
o
n
F
i
n
a
n
c
e
D
i
v
i
s
i
o
n
P
l
a
n
n
i
n
g
D
i
v
i
s
i
o
n
B
a
m
r
a
s
n
a
r
a
d
u
r
a
I
n
s
t
i
t
u
t
e
R
a
j
p
r
a
c
h
a
s
a
m
a
s
a
i
I
n
s
t
i
t
u
t
e
O
f
f
i
c
e
o
f
D
i
s
e
a
s
e
P
r
e
v
e
n
t
i
o
n
a
n
d
C
o
n
t
r
o
l
1
-
1
2
B
u
r
e
a
u
o
f
E
p
i
d
e
m
i
o
l
o
g
y
B
u
r
e
a
u
o
f
O
c
c
u
p
a
t
i
o
n
a
l
a
n
d
E
n
v
i
r
o
n
m
e
n
t
D
i
s
e
a
s
e
s
B
u
r
e
a
u
o
f
G
e
n
e
r
a
l
C
o
m
m
u
n
i
c
a
b
l
e
D
i
s
e
a
s
e
s
B
u
r
e
a
u
o
f
V
e
c
t
o
r
-
B
o
r
n
e
D
i
s
e
a
s
e
s
B
u
r
e
a
u
o
f
N
o
n
-
c
o
m
m
u
n
i
c
a
b
l
e
D
i
s
e
a
s
e
s
B
u
r
e
a
u
o
f
A
I
D
S
,
T
B
a
n
d
S
T
I
s
D
e
p
a
r
t
m
e
n
t
o
f
H
e
a
l
t
h
P
e
r
s
o
n
n
e
l
D
i
v
i
s
i
o
n
F
i
n
a
n
c
e
D
i
v
i
s
i
o
n
D
e
n
t
a
l
H
e
a
l
t
h
D
i
v
i
s
i
o
n
P
l
a
n
n
i
n
g
D
i
v
i
s
i
o
n
N
u
t
r
i
t
i
o
n
D
i
v
i
s
i
o
n
S
a
n
i
t
a
t
i
o
n
a
n
d
H
e
a
l
t
h
I
m
p
a
c
t
A
s
s
e
s
s
m
e
n
t
D
i
v
i
s
i
o
n
F
o
o
d
a
n
d
W
a
t
e
r
S
a
n
i
t
a
t
i
o
n
D
i
v
i
s
i
o
n
R
e
p
r
o
d
u
c
t
i
v
e
H
e
a
l
t
h
D
i
v
i
s
i
o
n
D
i
v
i
s
i
o
n
o
f
P
h
y
s
i
c
a
l
A
c
t
i
v
i
t
i
e
s
a
n
d
H
e
a
l
t
h
R
e
g
i
o
n
a
l
H
e
a
l
t
h
P
r
o
m
o
t
i
o
n
C
e
n
t
r
e
s
1
-
1
2
B
u
r
e
a
u
o
f
H
e
a
l
t
h
P
r
o
m
o
t
i
o
n
B
u
r
e
a
u
o
f
E
n
v
i
r
o
n
m
e
n
t
a
l
H
e
a
l
t
h
D
e
p
a
r
t
m
e
n
t
o
f
H
e
a
l
t
h
S
e
r
v
i
c
e
S
u
p
p
o
r
t
B
u
r
e
a
u
o
f
A
d
m
i
n
i
s
t
r
a
t
i
o
n
M
e
d
i
c
a
l
R
e
g
i
s
t
r
a
t
i
o
n
D
i
v
i
s
i
o
n
D
i
v
i
s
i
o
n
o
f
D
e
s
i
g
n
a
n
d
C
o
n
s
t
r
u
c
t
i
o
n
M
e
d
i
c
a
l
E
n
g
i
n
e
e
r
i
n
g
D
i
v
i
s
i
o
n
P
r
i
m
a
r
y
H
e
a
l
t
h
C
a
r
e
D
i
v
i
s
i
o
n
H
e
a
l
t
h
E
d
u
c
a
t
i
o
n
D
i
v
i
s
i
o
n
B
u
r
e
a
u
o
f
H
e
a
l
t
h
S
e
r
v
i
c
e
s
S
y
s
t
e
m
D
e
v
e
l
o
p
m
e
n
t
D
e
p
a
r
t
m
e
n
t
o
f
M
e
d
i
c
a
l
S
e
r
v
i
c
e
s
O
f
f
i
c
e
o
f
t
h
e
S
e
c
r
e
t
a
r
y
D
i
v
i
s
i
o
n
o
f
C
o
s
m
e
t
i
c
s
a
n
d
H
a
z
a
r
d
o
u
s
S
u
b
s
t
a
n
c
e
s
D
i
v
i
s
i
o
n
o
f
B
i
o
l
o
g
i
c
a
l
P
r
o
d
u
c
t
s
D
i
v
i
s
i
o
n
o
f
P
l
a
n
n
i
n
g
a
n
d
T
e
c
h
n
i
c
a
l
C
o
o
r
d
i
n
a
t
i
o
n
D
i
v
i
s
i
o
n
o
f
R
a
d
i
a
t
i
o
n
a
n
d
M
e
d
i
c
a
l
D
e
v
i
c
e
s
R
e
g
i
o
n
a
l
M
e
d
i
c
a
l
S
c
i
e
n
c
e
s
C
e
n
t
r
e
s
1
-
1
2
N
a
t
i
o
n
a
l
I
n
s
t
i
t
u
t
e
o
f
H
e
a
l
t
h
M
e
d
i
c
i
n
a
l
P
l
a
n
t
R
e
s
e
a
r
c
h
I
n
s
t
i
t
u
t
e
B
u
r
e
a
u
o
f
Q
u
a
l
i
t
y
a
n
d
F
o
o
d
S
a
f
e
t
y
B
u
r
e
a
u
o
f
L
a
b
o
r
a
t
o
r
y
Q
u
a
l
i
t
y
S
t
a
n
d
a
r
d
s
B
u
r
e
a
u
o
f
D
r
u
g
s
a
n
d
N
a
r
c
o
t
i
c
s
F
o
o
d
a
n
d
D
r
u
g
A
d
m
i
n
i
s
t
r
a
t
i
o
n
O
f
f
i
c
e
o
f
t
h
e
S
e
c
r
e
t
a
r
y
M
e
d
i
c
a
l
D
e
v
i
c
e
C
o
n
t
r
o
l
D
i
v
i
s
i
o
n
D
r
u
g
C
o
n
t
r
o
l
D
i
v
i
s
i
o
n
N
a
r
c
o
t
i
c
s
C
o
n
t
r
o
l
D
i
v
i
s
i
o
n
F
o
o
d
C
o
n
t
r
o
l
D
i
v
i
s
i
o
n
I
m
p
o
r
t
a
n
d
E
x
p
o
r
t
I
n
s
p
e
c
t
i
o
n
D
i
v
i
s
i
o
n
T
e
c
h
n
i
c
a
l
a
n
d
P
l
a
n
n
i
n
g
D
i
v
i
s
i
o
n
P
u
b
l
i
c
a
n
d
C
o
n
s
u
m
e
r
A
f
f
a
i
r
s
D
i
v
i
s
i
o
n
R
u
r
a
l
a
n
d
L
o
c
a
l
C
o
n
s
u
m
e
r
H
e
a
l
t
h
P
r
o
d
u
c
t
s
P
r
o
t
e
c
t
i
o
n
P
r
o
m
o
t
i
o
n
D
i
v
i
s
i
o
n
B
u
r
e
a
u
o
f
C
o
s
m
e
t
i
c
a
n
d
H
a
z
a
r
d
o
u
s
S
u
b
s
t
a
n
c
e
C
o
n
t
r
o
l
A
g
e
n
c
i
e
s
u
n
d
e
r
t
h
e
S
u
p
e
r
v
i
s
i
o
n
o
f
M
O
P
H
:
H
e
a
l
t
h
S
y
s
t
e
m
s
R
e
s
e
a
r
c
h
I
n
s
t
i
t
u
t
e
N
a
t
i
o
n
a
l
H
e
a
l
t
h
S
e
c
u
r
i
t
y
O
f
f
i
c
e
P
r
a
b
o
r
o
m
a
r
a
j
c
h
a
n
o
k
I
n
s
t
i
t
u
t
e
o
f
H
e
a
l
t
h
W
o
r
k
f
o
r
c
e
D
e
v
e
l
o
p
m
e
n
t
(
A
c
t
r
e
q
u
i
r
e
d
)
N
a
t
i
o
n
a
l
I
n
s
t
i
t
u
t
e
o
f
H
e
a
l
t
h
(
A
c
t
r
e
q
u
i
r
e
d
)
S
t
a
t
e
E
n
t
e
r
p
r
i
s
e
:
G
o
v
e
r
n
m
e
n
t
P
h
a
r
m
a
c
e
u
t
i
c
a
l
O
r
g
a
n
i
z
a
t
i
o
n
P
u
b
l
i
c
O
r
g
a
n
i
z
a
t
i
o
n
s
(
R
o
y
a
l
D
e
c
r
e
e
s
r
e
u
i
r
e
d
)
H
e
a
l
t
h
f
a
c
i
l
i
t
i
e
s
(
R
o
y
a
l
d
e
c
r
e
e
e
n
a
c
t
e
d
f
o
r
B
a
n
P
h
a
e
o
H
o
s
p
i
t
a
l
)
I
n
s
t
i
t
u
t
e
o
f
S
p
e
c
i
a
l
i
t
y
M
e
d
i
c
i
n
e
B
u
r
e
a
u
o
f
E
m
e
r
g
e
n
c
y
M
e
d
i
c
a
l
S
e
r
v
i
c
e
s
S
y
s
t
e
m
I
n
s
t
i
t
u
t
e
o
f
H
o
s
p
i
t
a
l
Q
u
a
l
i
t
y
I
m
p
r
o
v
e
m
e
n
t
a
n
d
A
c
c
r
e
d
i
t
a
t
i
o
n
(
H
A
-
T
h
a
i
l
a
n
d
)
S
o
u
r
c
e
:
M
i
n
i
s
t
e
r
i
a
l
R
e
g
u
l
a
t
i
o
n
s
o
f
t
h
e
M
i
n
i
s
t
r
y
o
f
P
u
b
l
i
c
H
e
a
l
t
h
,
2
0
0
2
N
o
t
e
:
P
u
b
l
i
c
o
r
g
a
n
i
z
a
t
i
o
n
s
a
n
d
a
g
e
n
c
i
e
s
u
n
d
e
r
t
h
e
s
u
p
e
r
v
i
s
i
o
n
o
f
t
h
e
M
O
P
H
a
r
e
n
o
t
u
n
d
e
r
a
n
y
o
f
t
h
e
c
l
u
s
t
e
r
s
.
Thailand 47
Annex 7
Morbidity rates of hospitalized cases (per 100 000
population) due to selected NCDs, injuries and mental
illness Thailand (excluding Bangkok), 20012004
S
o
u
r
c
e
:
B
u
r
e
a
u
o
f
P
o
l
i
c
y
a
n
d
S
t
r
a
t
e
g
y
WHO Country Cooperation Strategy 2008-2011 48
Annex 8
Organogram WHO Country Office Thailand
a
C
S
R
=
C
o
m
m
u
n
i
c
a
b
l
e
D
i
s
e
a
s
e
S
u
r
v
e
i
l
l
a
n
c
e
a
n
d
R
e
s
p
o
n
s
e
S
u
b
-
u
n
i
t
i
s
u
n
d
e
r
t
e
c
h
n
i
c
a
l
s
u
p
e
r
v
i
s
i
o
n
o
f
S
E
A
R
O
,
u
s
i
n
g
W
C
O
c
o
m
m
o
n
s
e
r
v
i
c
e
s
b
M
M
P
=
M
a
l
a
r
i
a
M
e
k
o
n
g
P
r
o
j
e
c
t
i
s
u
n
d
e
r
j
o
i
n
t
t
e
c
h
n
i
c
a
l
s
u
p
e
r
v
i
s
i
o
n
o
f
S
E
A
R
O
a
n
d
W
P
R
O
,
u
s
i
n
g
W
C
O
c
o
m
m
o
n
s
e
r
v
i
c
e
s
c
U
n
d
e
r
p
r
o
c
e
s
s
o
f
r
e
c
r
u
i
t
m
e
n
t
;
d
S
u
p
p
o
r
t
e
d
b
y
C
S
R
a
n
d
o
t
h
e
r
V
C
b
u
d
g
e
t
a
n
d
p
o
o
l
e
d
f
o
r
c
o
m
m
o
n
s
e
r
v
i
c
e
s
i
n
W
C
O
;
c
o
m
m
o
n
s
e
v
i
c
e
s
*
S
S
A
o
r
s
h
o
r
t
-
t
e
r
m
c
o
n
t
r
a
c
t
.
Thailand 49
Annex 9
References
(1) United Nations Development Programme. Human development report 2006: beyond scarcity:
power, poverty and the global water crisis. New York, 2006. (http://hdr.undp.org/hdr2006/
pdfs/report/HDR06-complete.pdf accessed 23 July 2007).
(2) United Nations Development Programme. Thailand human development report 2007: sufficiency
economy and human development. Bangkok, 2007. (http://www.undp.or.th/NHDR2007/
index.html accessed 23 July 2007).
(3) United Nations Population Fund. Country profiles for population and reproductive health: policy
and development indicators 2005., New York: UNFPA and Population Reference Bureau, 2005.
(http://www.unfpa.org/publications/detail.cfm?ID=260&filterListType= accessed 23 July
2007).
(4) World Health Organization. Global tuberculosis control: surveillance, planning, financing: WHO
report 2007. Geveva, 2007. (http://whqlibdoc.who.int/publications/2007/9789241563141_
eng.pdf (File size : 3.4Mb) accessed 23 July 2007)
(5) Ministry of Public Health, Department of Disease Control, Bureau of Epidemiology. Morbidity
and mortality rate of pulmonary TB cases from report 506 (1979-2005). (http://epid.moph.go.th/
dssur/respir/pulmtb.htm accessed 26 July 2007).
(6) Ministry of Public Health, Bureau of Policy and Strategy. Report on health resources 2004,
Bangkok, 2004. (http://203.157.19.191 accessed 26 July 2007).
(7) World Health Organization. The world health report: 2006: working together for health. Geneva,
2006. (http://whqlibdoc.who.int/publications/2006/9241563176_eng.pdf (File size : 6.6 Mb)
accessed 23 July 2007).
(8) Ministry of Public Health. National Health Security Office Annual Report 2004. Nonthaburi,
2004.
(9) Thai National Statistical Office. The 2003 health and welfare survey. Bangkok, 2003. (http://
service.nso.go.th/agrc/health46/eng.htm accessed 26 July 2007).
(10) Tangcharoensathien V, Teokul W, ChanwongpaisarnL. Social Welfare System in Thailand:
Challenges of implementing universal coverage. Bangkok: UNRISD, 2004.
(11) Ministry of Public Health, Bureau of Policy and Strategy. Thailand health profile 2001-2004.
In: Unpublished paper, (extracted from Thailand National Health Profile 2004, page 253,
Table 6.7).
(12) Vasavid, Chitpranee. IHPP Research on Health Care Financing 2003. Presentation at the IHPP
Annual Conference on 14 May 2004. (http://www.ihpp.thaigov.net/research_annual04/
Agenda%203%20Chitpranee.pdf accessed 23 July 2007)
(13) Ministry of Public Health. Minister fears for hospitals. Clipping from the Nation newspaper,
Friday 27 April 2007. (http://eng.moph.go.th/ContentDetails.php?intContentID=16042
&strOrgID=001002002 accessed 26 July 2007).
WHO Country Cooperation Strategy 2008-2011 50
(14) United Nation Country Team in Thailand, UN Resident Coordinators Office. Thailand Common
Country Assessment 2005. Bangkok, 2005. (http://www.undp.org/rbap/Country_Office/CCA/
Cca-Thailand2005.pdf accessed 24 July 2007).
(15) World Bank. World development indicators database. 18 April 2006. (http://
devdata.worldbank.org/data-query/ accessed 23 July 2007).
(16) Wibulpolprasert, S. Thailand health profile 2001-2004. Bangkok: Ministry of Public Health,
2004. (http://www.moph.go.th/ops/health_48/index_eng.htm accessed 23 July 2007).
(17) National Economic and Social Development Board. Thailand millennium development goals
report 2004. Bangkok, 2004.
WHO Country Coopcration Stratcgy
2008-2011
Permanent 8ecretary u||d|ng No.3
4th f|oor, H|n|stry of Pub||c hea|th
T|wanon Road, Huang
Nonthabur| 11000
Tha||and
www.whotha|.org
You might also like
- WHO IndonesiaDocument49 pagesWHO IndonesiaSiAgam DevinfoNo ratings yet
- WHO Country Cooperation Strategy 2007-2011: IndonesiaDocument49 pagesWHO Country Cooperation Strategy 2007-2011: IndonesiatiaaraNo ratings yet
- Review of 40 Years of Primary Health Care Implementation at Country LevelDocument69 pagesReview of 40 Years of Primary Health Care Implementation at Country LevelSyafrida HanumNo ratings yet
- RH Strategy 2016 PDFDocument57 pagesRH Strategy 2016 PDFBethel100% (1)
- Mental Health WHODocument31 pagesMental Health WHORahmat Hidayat100% (1)
- UNFPA-ICPD@15 Full ReportDocument64 pagesUNFPA-ICPD@15 Full ReportPennapa KaweewongprassertNo ratings yet
- WHOCB For AUutismDocument44 pagesWHOCB For AUutismpatriciafernandes.to0% (1)
- Ayrh StrategyDocument68 pagesAyrh StrategyLeel BurtukanNo ratings yet
- Nigeria Hsa Final June2009Document135 pagesNigeria Hsa Final June2009Sabrina Al-Jabry0% (1)
- HIS MasterPlan 2016 2020Document129 pagesHIS MasterPlan 2016 2020nady tepNo ratings yet
- Report of The Meeting of Second South-East Asia Regional Technical Advisory Group On Immunization (Sear Itag)Document30 pagesReport of The Meeting of Second South-East Asia Regional Technical Advisory Group On Immunization (Sear Itag)Vinita VasanthNo ratings yet
- South Sudan National Health Policy 2016 To 2025 2Document40 pagesSouth Sudan National Health Policy 2016 To 2025 2Winny DianaNo ratings yet
- The President S Emergency Plan For AIDS Relief Technical Considerations Provided by PEPFAR Technical Working Groups For FY 2012 COPS and ROPSDocument247 pagesThe President S Emergency Plan For AIDS Relief Technical Considerations Provided by PEPFAR Technical Working Groups For FY 2012 COPS and ROPSAccessible Journal Media: Peace Corps Documents100% (1)
- Idl 57094Document63 pagesIdl 57094Urmi ChakmaNo ratings yet
- Regional Strategy For TM in Western Pacific 2011-2020Document71 pagesRegional Strategy For TM in Western Pacific 2011-2020Nancy KawilarangNo ratings yet
- CPE Report 30 MayDocument122 pagesCPE Report 30 MayadkittipongNo ratings yet
- WG 1NRHMDocument120 pagesWG 1NRHMVivek SinghNo ratings yet
- B3223Document45 pagesB3223Irwan Meidi LubisNo ratings yet
- National Guideline For Patient Safety Incident Reporting and Learning in South Africa Version 2 - Web LayoutDocument82 pagesNational Guideline For Patient Safety Incident Reporting and Learning in South Africa Version 2 - Web LayoutSheena Mabaquiao-PadernalNo ratings yet
- National Health Sector Strategic Plan 2010 - 2015 - Ministry of Health and Sanitation (GoSL)Document64 pagesNational Health Sector Strategic Plan 2010 - 2015 - Ministry of Health and Sanitation (GoSL)MaxxNo ratings yet
- Maternal Health DesignDocument106 pagesMaternal Health DesignKuran AtikaNo ratings yet
- CCS Pakistan 2013 EN 14946Document57 pagesCCS Pakistan 2013 EN 14946Shams LadakNo ratings yet
- THailand UCS Achievement and ChallengesDocument124 pagesTHailand UCS Achievement and ChallengeshsrimediaNo ratings yet
- International Institute For Primary Health Care inDocument29 pagesInternational Institute For Primary Health Care inhabtamu hasenNo ratings yet
- Integrating Gender into the Design of Cash Transfer and Public Works Programmes: Fao Technical Guide 2: A Toolkit on Gender-Sensitive Social Protection Programmes to Combat Rural Poverty and HungerFrom EverandIntegrating Gender into the Design of Cash Transfer and Public Works Programmes: Fao Technical Guide 2: A Toolkit on Gender-Sensitive Social Protection Programmes to Combat Rural Poverty and HungerNo ratings yet
- (Swamedikasi WHO 2009) PDFDocument80 pages(Swamedikasi WHO 2009) PDFTommy Winahyu PuriNo ratings yet
- Estrategias Nacionales de E - SaludDocument223 pagesEstrategias Nacionales de E - SaludRolando PinchettiNo ratings yet
- Urban HEART: Urban Health Equity Assessment and Response ToolDocument48 pagesUrban HEART: Urban Health Equity Assessment and Response ToolSiva Nayak100% (1)
- Guideline For ERMP 2020Document22 pagesGuideline For ERMP 2020Gedefaw Tigabu67% (3)
- Catalysing Young Agri-Entrepreneurs' Investments and Ensuring Their Sustainability: Strategic Planning ToolFrom EverandCatalysing Young Agri-Entrepreneurs' Investments and Ensuring Their Sustainability: Strategic Planning ToolNo ratings yet
- United Nations Inter-Agency Task Force On The Prevention and Control of Non-Communicable DiseasesDocument16 pagesUnited Nations Inter-Agency Task Force On The Prevention and Control of Non-Communicable DiseasesdilaNo ratings yet
- SEA-HSD-366 RevDocument51 pagesSEA-HSD-366 RevWidya HumairaNo ratings yet
- Primary Health Care at Forty: Reflections From South-East AsiaDocument24 pagesPrimary Health Care at Forty: Reflections From South-East AsiaDjaloeGWiwahaNo ratings yet
- Best ApprochesDocument57 pagesBest ApprocheszelalemNo ratings yet
- Summary Mobile HealthDocument31 pagesSummary Mobile HealthmhemaraNo ratings yet
- TaskDocument3 pagesTaskGis ThaNo ratings yet
- Sea Ment 151Document39 pagesSea Ment 151Irene FranzNo ratings yet
- 2020 Grants Call For Proposal Draft v4 23 July 2020Document13 pages2020 Grants Call For Proposal Draft v4 23 July 2020monsalbert13No ratings yet
- Thailand Health Systems ReviewDocument299 pagesThailand Health Systems Reviewpikthaiza tonbootNo ratings yet
- Uganda 10Document181 pagesUganda 10chioma stellaNo ratings yet
- Comprehensive Assessment of National Extension and Advisory Service Systems: An Operational GuideFrom EverandComprehensive Assessment of National Extension and Advisory Service Systems: An Operational GuideNo ratings yet
- AFR-RC67-10 Framework For Health Systems Development-Rev 23.09.17Document19 pagesAFR-RC67-10 Framework For Health Systems Development-Rev 23.09.17digitechconsultsNo ratings yet
- 2010 WHO-Osteopathy BenchmarksDocument36 pages2010 WHO-Osteopathy BenchmarksTây SơnNo ratings yet
- Icd 11Document12 pagesIcd 11iyanh100% (2)
- Strengthening Coherence between Agriculture and Social Protection to Combat Poverty and Hunger in Africa Diagnostic ToolFrom EverandStrengthening Coherence between Agriculture and Social Protection to Combat Poverty and Hunger in Africa Diagnostic ToolNo ratings yet
- VN WHO EURO13FT146 20130518 enDocument5 pagesVN WHO EURO13FT146 20130518 enyi1989No ratings yet
- A Case Study of World Health OrganisationDocument26 pagesA Case Study of World Health OrganisationFarNo ratings yet
- A Manual For Comprehensive Supportive Supervision and Mentoring On Hiv and Aids Health ServicesDocument57 pagesA Manual For Comprehensive Supportive Supervision and Mentoring On Hiv and Aids Health ServicesfikeNo ratings yet
- Person Centered Care Certification ManualDocument94 pagesPerson Centered Care Certification ManualPaula NahasNo ratings yet
- Kenya Health Policy 2014 2030Document87 pagesKenya Health Policy 2014 2030Migori ArtNo ratings yet
- The Health and Population Policy of Uttarakhand: A ReviewDocument56 pagesThe Health and Population Policy of Uttarakhand: A Reviewtarungupta2001No ratings yet
- Draft 2010 Document On The Re-Engineering of Primary Health Care in South AfricaDocument121 pagesDraft 2010 Document On The Re-Engineering of Primary Health Care in South AfricaLaura Lopez Gonzalez100% (1)
- WHO TraditionalDocument78 pagesWHO TraditionalGhina Rizqiani Nh AfifahNo ratings yet
- Strategic Plan For HIV AIDs and STI Care 2008-2010 enDocument40 pagesStrategic Plan For HIV AIDs and STI Care 2008-2010 enChou ChantraNo ratings yet
- The World Health Organization: An Institutional ReviewDocument53 pagesThe World Health Organization: An Institutional ReviewvijayaveeNo ratings yet
- Sea Aids 200Document50 pagesSea Aids 200Rasid Ridha AdamNo ratings yet
- GPP Policy Asia TenggaraDocument83 pagesGPP Policy Asia TenggaraMaria Wisnu DonowatiNo ratings yet
- Essential Health Care Package For SwazilandDocument75 pagesEssential Health Care Package For SwazilandRae Manar100% (1)
- Integrating Gender into Implementation and Monitoring and Evaluation of Cash Transfer and Public Works Programmes: Fao Technical Guide 3From EverandIntegrating Gender into Implementation and Monitoring and Evaluation of Cash Transfer and Public Works Programmes: Fao Technical Guide 3No ratings yet
- Khyber Pakhtunkhwa Health Sector Review: Hospital CareFrom EverandKhyber Pakhtunkhwa Health Sector Review: Hospital CareNo ratings yet
- Tifoid Hepatitis PMJDocument3 pagesTifoid Hepatitis PMJWawan BwNo ratings yet
- Ventricular ArrhytmiaDocument30 pagesVentricular ArrhytmiaIkhsan AmadeaNo ratings yet
- CPCRDocument35 pagesCPCRIkhsan AmadeaNo ratings yet
- Deep NeckSpaces 2002 04 SlidesDocument61 pagesDeep NeckSpaces 2002 04 SlidesIkhsan AmadeaNo ratings yet
- Renew Spss LicenseDocument1 pageRenew Spss LicenseIkhsan AmadeaNo ratings yet
- Ta Mimi 2002Document15 pagesTa Mimi 2002Ikhsan AmadeaNo ratings yet
- The Sign of FourDocument75 pagesThe Sign of FourIkhsan AmadeaNo ratings yet
- Intermediate - PilgrimsDocument3 pagesIntermediate - PilgrimsIkhsan AmadeaNo ratings yet
- Cardiac Prevention and RehabilitationDocument20 pagesCardiac Prevention and RehabilitationIkhsan Amadea100% (1)
- Scle Final AssignmentDocument6 pagesScle Final AssignmentIkhsan AmadeaNo ratings yet
- Referat Entropion On ProgressDocument26 pagesReferat Entropion On ProgressIkhsan AmadeaNo ratings yet
- Waktu: Rundown Photoshoot Buku Tahunan 2009Document1 pageWaktu: Rundown Photoshoot Buku Tahunan 2009Ikhsan AmadeaNo ratings yet
- BartlebyDocument21 pagesBartlebyIkhsan AmadeaNo ratings yet
- Jurnal Reading IKHSAN On ProgressDocument14 pagesJurnal Reading IKHSAN On ProgressIkhsan AmadeaNo ratings yet
- Calon FasilDocument2 pagesCalon FasilIkhsan AmadeaNo ratings yet
- Tetra, Makrolid, AminoglikosidDocument30 pagesTetra, Makrolid, AminoglikosidIkhsan AmadeaNo ratings yet
- Almayer's FollyDocument1 pageAlmayer's FollyIkhsan AmadeaNo ratings yet
- Nej Me 1302063Document3 pagesNej Me 1302063Ikhsan AmadeaNo ratings yet
- Nej Mo A 1114588Document8 pagesNej Mo A 1114588Ikhsan AmadeaNo ratings yet
- Nej Mo A 1307337Document10 pagesNej Mo A 1307337Ikhsan AmadeaNo ratings yet
- Waktu: Rundown Photoshoot Buku Tahunan 2009Document1 pageWaktu: Rundown Photoshoot Buku Tahunan 2009Ikhsan AmadeaNo ratings yet
- 158 428 1 PBDocument1 page158 428 1 PBIkhsan AmadeaNo ratings yet
- Ringkasan Kitab Hadist Bukhari MuslimDocument517 pagesRingkasan Kitab Hadist Bukhari MuslimIkhsan AmadeaNo ratings yet
- Proclamation 916-2008, Definition of Powers and Duties of The Executive Organs of The FDREDocument74 pagesProclamation 916-2008, Definition of Powers and Duties of The Executive Organs of The FDREይህየይስ ተአምኖ100% (3)
- Personnel PoliciesDocument12 pagesPersonnel PoliciesJimcy100% (4)
- BCPC Work Financial Plan 2017Document2 pagesBCPC Work Financial Plan 2017Barangay Zone INo ratings yet
- Tunnelling Machines - Air Locks - Safety Requirements: British Standard Bs en 12110:2002 +A1:2008Document24 pagesTunnelling Machines - Air Locks - Safety Requirements: British Standard Bs en 12110:2002 +A1:2008Jasmine Tso100% (2)
- Revised AIS Rule Vol I Rule 06 2Document50 pagesRevised AIS Rule Vol I Rule 06 2Ramanathan SrinivasanNo ratings yet
- Who en enDocument307 pagesWho en enAafreen ShaikhNo ratings yet
- 18 UW ALICE Report NJ Update 10.19.18 LowresDocument86 pages18 UW ALICE Report NJ Update 10.19.18 LowresWHYY NewsNo ratings yet
- PDF Document 3Document54 pagesPDF Document 3Rodessa ValenciaNo ratings yet
- Ambulance Job DescriptionDocument5 pagesAmbulance Job DescriptionJonette Castro HermidaNo ratings yet
- Classification of DPSPDocument3 pagesClassification of DPSPHarsh DixitNo ratings yet
- 9th Five Year Plan-Sneha GauryDocument9 pages9th Five Year Plan-Sneha GauryVarsha bijuNo ratings yet
- DoshDocument16 pagesDoshイセ ジュ100% (1)
- 7 Dr. Dineros - PhilHealth CHO MHODocument15 pages7 Dr. Dineros - PhilHealth CHO MHOKristel Joy Verzon-BunaganNo ratings yet
- Baseline Assessment Program Portal User ManualDocument33 pagesBaseline Assessment Program Portal User ManualJeff NixonNo ratings yet
- World BankDocument121 pagesWorld Bankbivek kumarNo ratings yet
- History of Valenzuela PDFDocument505 pagesHistory of Valenzuela PDFKylaNo ratings yet
- Health Care Payment PDFDocument174 pagesHealth Care Payment PDFAshri Nur IstiqomahNo ratings yet
- Planned Parenthood Research PaperDocument5 pagesPlanned Parenthood Research Paperapi-355452581100% (1)
- (13,14) Slum Development ProgrammesDocument25 pages(13,14) Slum Development Programmesamatul waseyNo ratings yet
- Ra 11332Document8 pagesRa 11332Dianne MonzonNo ratings yet
- Evacuation ReportDocument2 pagesEvacuation ReportSue MengNo ratings yet
- Criminology ResearchDocument5 pagesCriminology ResearchMaritess ViernesNo ratings yet
- Indian Institutes of Technology Joint Entrance Examination (Advanced) 2021 Online Admit CardDocument4 pagesIndian Institutes of Technology Joint Entrance Examination (Advanced) 2021 Online Admit CardKrishna MeenaNo ratings yet
- (6. Functions of Inspectors: Section 5 - Chief Inspector and InspectorsDocument4 pages(6. Functions of Inspectors: Section 5 - Chief Inspector and InspectorsUmakant KumarNo ratings yet
- Report To The Secretary of The Department of Veterans Affairs On The Association Between Adverse Health Effects and Exposure To Agent OrangeDocument33 pagesReport To The Secretary of The Department of Veterans Affairs On The Association Between Adverse Health Effects and Exposure To Agent OrangeChildren Of Vietnam Veterans Health Alliance100% (2)
- Reading The Proclamation of The Philippine IndependenceDocument11 pagesReading The Proclamation of The Philippine IndependenceGlecil JoyNo ratings yet
- Special Power of Attorney - Bus. RegDocument4 pagesSpecial Power of Attorney - Bus. RegSharon GenitaNo ratings yet
- 1-Personal Fitness Trainer License Application FormDocument5 pages1-Personal Fitness Trainer License Application FormSathish KumarNo ratings yet
- Entrepreneurship & InnovationDocument31 pagesEntrepreneurship & InnovationSamruddhi KudalkarNo ratings yet
- Narrative On NEUDocument2 pagesNarrative On NEUJoey OcampoNo ratings yet