Professional Documents
Culture Documents
Genomica Del Cáncer
Uploaded by
Daniel PintoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Genomica Del Cáncer
Uploaded by
Daniel PintoCopyright:
Available Formats
Cancer Genomics: Technology, Discovery, and Translation
Ben Tran, Janet E. Dancey, Suzanne Kamel-Reid, John D. McPherson, Philippe L. Bedard,
Andrew M.K. Brown, Tong Zhang, Patricia Shaw, Nicole Onetto, Lincoln Stein, Thomas J. Hudson,
Benjamin G. Neel, and Lillian L. Siu
See accompanying editorial on page 584
Ben Tran, Philippe L. Bedard, and Lillian
L. Siu, Princess Margaret Hospital,
University Health Network, University
of Toronto; Janet E. Dancey, John D.
McPherson, Andrew M.K. Brown,
Nicole Onetto, Lincoln Stein, and
Thomas J. Hudson, Ontario Institute for
Cancer Research; Suzanne Kamel-Reid,
Tong Zhang, and Patricia Shaw, Toronto
General Hospital, University Health
Network, University of Toronto; John D.
McPherson, Nicole Onetto, Lincoln
Stein, Thomas J. Hudson, and Benja-
min G. Neel, University of Toronto; and
Benjamin G. Neel, Campbell Family
Cancer Research Institute, Ontario
Cancer Institute, University Health
Network, University of Toronto,
Toronto, Canada.
Submitted August 29, 2011; accepted
November 16, 2011; published online
ahead of print at www.jco.org on
January 23, 2012.
Terms in blue are dened in the glos-
sary, found at the end of this article
and online at www.jco.org.
Authors disclosures of potential con-
icts of interest and author contribu-
tions are found at the end of this
article.
Corresponding author: Lillian L. Siu,
MD, FRCPC, Princess Margaret Hospi-
tal, Drug Development Program, 610
University Ave, Ste 5-718, Toronto,
Ontario, M5G 2M9, Canada; e-mail:
lillian.siu@uhn.on.ca.
2012 by American Society of Clinical
Oncology
0732-183X/12/3006-647/$20.00
DOI: 10.1200/JCO.2011.39.2316
A B S T R A C T
In recent years, the increasing awareness that somatic mutations and other genetic aberrations drive
human malignancies has led us within reach of personalized cancer medicine (PCM). The implemen-
tation of PCM is based on the following premises: genetic aberrations exist in human malignancies; a
subset of these aberrations drive oncogenesis and tumor biology; these aberrations are actionable
(dened as having the potential to affect management recommendations based on diagnostic,
prognostic, and/or predictive implications); and there are highly specic anticancer agents available that
effectively modulate these targets. This article highlights the technology underlying cancer genomics
and examines the early results of genome sequencing and the challenges met in the discovery of new
genetic aberrations. Finally, drawing fromexperiences gained in a feasibility study of somatic mutation
genotyping and targeted exome sequencing led by Princess Margaret HospitalUniversity Health
Network and the Ontario Institute for Cancer Research, the processes, challenges, and issues involved
in the translation of cancer genomics to the clinic are discussed.
J Clin Oncol 30:647-660. 2012 by American Society of Clinical Oncology
INTRODUCTION
Inrecent years, anincreasing appreciationandiden-
tication of somatic mutations and other genetic
aberrations that drive human malignancies have led
us within reach of personalized cancer medicine
(PCM). The US National Cancer Institute denes
personalized medicine as a form of medicine that
uses information about a persons genes, proteins,
and environment to prevent, diagnose, and treat
disease.
1
The implementation of PCM is based on
the following premises: genetic aberrations exist in
human malignancies; a subset of these aberrations
drives oncogenesis andtumor biology; these aberra-
tions are actionable (have potential to affect man-
agement recommendations based on diagnostic,
prognostic, and/or predictive implications); and
highly specic anticancer agents are available that
effectively modulate these targets. The National
Cancer Institute Ofce of Cancer Genomics, estab-
lished to facilitate PCM through validation of these
key premises, articulates the following mission and
goals
2
: First, enhance the understanding of the mo-
lecular mechanisms of cancer; second, accelerate
genomic science and technology development; and
third, translate genomic data toimprove cancer pre-
vention, early detection, diagnosis, and treatment.
Hence, the focus of this article will revolve around
the three pillars that support cancer genomics: dis-
covery, technology, and translation.
Since the Human Genome Project, the emerg-
ing scientic era of omics has revolutionized the
study of cancer. Although cancer is recognized as a
disease driven fundamentally by genetic changes,
the somatic events that drive the multistep progres-
sionof carcinogenesis are not well understood, even
in the most studied cancer types.
3
The International
Cancer Genome Consortium (ICGC) is coordinat-
ing efforts aimed at identifying all genomic altera-
tions signicantly associated with cancer, including
genomic loss or amplication, mutations in coding
regions, chromosomal rearrangements, aberrant
methylation, and expression proles. Through the
ICGC, the discovery pillar targets the decoding of
cancer genomes. Much of the discovery is depen-
dent on advances in molecular diagnostics, particu-
larly genome sequencing, within the technology
pillar. The improved timeliness and cost associated
with genome sequencing have driven discovery not
only incancer genomics but also inthe nal pillar of
clinical translation. Until now, the majority of the
focus within cancer genomics lay in discovery. As
our molecular understanding of cancer improves,
the prospect of applying genomic knowledge in the
clinic becomes increasingly tangible. However, spe-
cic challenges in the scientic, regulatory, and eth-
ical domains remain to be overcome before PCM
JOURNAL OF CLINICAL ONCOLOGY
S P E C I A L A R T I C L E
VOLUME 30 NUMBER 6 FEBRUARY 20 2012
2012 by American Society of Clinical Oncology 647
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
can become a reality. This article highlights the technology that em-
powers cancer genomics, examines the early results of genome se-
quencing and the challenges met in the discovery of new genetic
aberrations, and discusses the processes involved in the translation of
cancer genomics to the clinic.
TECHNOLOGY
The eld of cancer genomics is growing rapidly as a result of revolu-
tionary advances in DNAsequencing technologies. In this section, we
review the technologic developments that have catalyzed increased
understanding of cancer biology: whole genome sequencing (WGS),
targeted sequencing, genotyping, and bioinformatics.
WGS
WGS is the backbone technology that supports the in-depth
sequencing of cancer genomes. Genome sequencing consists of three
phases: samplepreparation, physical sequencing, andreconstruction.
4
In sample preparation, the target genome is broken into fragments.
4
During physical sequencing, individual bases in each fragment are
identied in order; the number of individual bases identied contig-
uously is denedas the readlength.
4
During reconstruction, bioinfor-
matics softwarealigns overlappingreads fromeachfragment, allowing
the original genome to be constructed; the longer the read length, the
easier the reconstruction.
5
Traditionally, genome sequencinghas been
costlyandtime consuming. However, newtechnologyhas diminished
both of these impediments.
4,5
First-generation sequencing, or Sanger sequencing, has been
the workhorse of DNA sequencing for almost 30 years.
4
Although
signicant improvements in optimization, miniaturization, multi-
plexing, automation, and pipeline integration have occurred, the
fundamental technology has not changed signicantly.
4
Sanger
sequencing can produce read lengths of up to 1,000 bases, consid-
erably longer than second-generation sequencing platforms.
5
It is
an effective method, the long read lengths and high accuracy of
which have resulted in monumental accomplishments, including
completion of the Human Genome Project.
4,6
However, limita-
tions of high cost and low throughput (small amount of data gener-
ated per unit of time) have led to the development of next-generation
sequencing (NGS).
4,5,7
NGS platforms consist of second- and third-generation technol-
ogies, describedindepthbyMetzker.
4
Bothare more economical than
Sanger andhave higher throughput. Second-generationplatforms are
dominated by cyclic array or ush and scanbased sequencing.
Strands of fragmented DNA are amplied, and bases are then added
sequentially using DNA polymerase. Excess reagent is washed out,
imaging then identies the base incorporated, and the process is re-
peated.
8
This repetitive process leads to millions of reads, each of
limitedlength(approximately50to400bases), creatingachallengefor
genome reconstruction.
4,5,7,9
Several second-generationplatforms are
commercially available, each with distinct differences (Table 1). Al-
though NGS has improved cost and throughput, its disadvantages
include short read length, complex sample preparation, need for am-
plication, long time to results, and signicant data storage and inter-
pretation requirements.
5,11
Third-generation sequencing technologies include novel plat-
forms, such as the PacBio RS (Pacic Biosciences, Menlo Park, CA)
and Ion Torrent PGM (Life Technologies, Carlsbad, CA; Table 1).
PacBioRSuses a process calledsingle-molecule, real-time detectionof
biologic processes that results in longer read lengths, averaging 964
bases in published articles,
4,11
and more than 2,000 bases in more
recent applications at our institute. Instead of relying on amplied
DNA, single-molecule sequencing detects the specic sequence of
each individual DNAstrand. Ion Torrent PGMuses nonoptical DNA
sequencing. Rather thandetecting nucleotide incorporationoptically,
PGM uses a semiconductor that senses the ions produced as nucleo-
tides are incorporated. Although read length currently averages fewer
than 200 bases, accuracy is high, and run time is short, potentially
allowing for real-time clinical application.
10,12
The rst humangenome sequence cost more than$2 billionand
tookadecade tocomplete.
20
However, advances incost andtimeliness
gained through these novel platforms bring the $1,000 genome target
of the National Institutes of Healthwithinreach. As genome sequenc-
ing becomes more affordable andaccessible, our understanding of the
molecular basis of cancer is expected to improve exponentially.
Targeted Genome Sequencing
Althoughcheaper thanSanger sequencing, WGSremains expen-
sive on a grand scale, with current costs of $10,000 to $35,000
7
per
human genome, exclusive of labor and other expenses. Targeted se-
quencing refers to strategies that enrich the input for DNAregions of
interest,
7
such as the whole exome or the cancer genome (ie, genes
potentiallyinvolvedintumor biology). Manyof theplatforms usedfor
WGS also are used for targeted sequencing, although polymerase
chain reaction (PCR) amplication of targeted regions or hybridiza-
tionof the test DNAtospecic arrays of oligonucleotides correspond-
ing to the desiredtarget sequences is required. Inadditionto reducing
the cost per sample, these approaches increase coverage of areas of
interest, which may overcome problems of cancer cell cellularity in
tumor specimens and increase accuracy.
7
As WGS costs remain high,
targeted sequencing, particularly exome sequencing, is likely to dom-
inate near-termsequencing strategies.
21
Cancer Genotyping
The increasing number of targeted therapeutics, the antitumor
activity of which is based on the presence of specic biomarkers, has
created a growing need for real-time detection of recognized genetic
aberrations in clinical samples in a cost-effective and timely manner.
Given the observation that some cancer mutations occur at similar
DNA bases in tumors from different patients (so-called recurrent
mutations), it is possible to use assays that test for single bases (a
process referredtoas mutationgenotyping). Giventhat the number of
clinically validated recurrent and predictive mutations are few, meth-
ods suchas PCR-basedrestrictionfragment lengthpolymorphismare
currently being used for somatic mutation genotyping in individual
patients withcancer.
13
However, therepertoireof recurrent mutations
is increasing, and there is interest in testing these to evaluate their role
as predictive mutations for the numerous molecularly targeted agents
in development. This leads to a need for higher-throughput genotyp-
ing methods.
High-throughput genotyping platforms, consisting of multi-
plexed assays and microarrays, have been successfully used for
genotyping clinical samples.
15,22-24
Table 1 details several of these
platforms, including the TaqmanOpenArray Genotyping system(us-
ing Taqman genotyping assays; Applied Biosystems, Carlsbad, CA),
Tran et al
648 2012 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
Table 1. Sequencing and Genotyping Platforms
Platform Method Application Comment
Sequencing
First generation (Sanger sequencing)
Sanger
4
Strands of fragmented DNA are resolved on
gel and distributed in order of length,
with end base labelled
Targeted sequencing; whole
genome sequencing;
genotyping
Despite high accuracy and successes such
as the rst human genome, several
limitations, particularly low throughput,
have led to increased use of NGS
technologies
Second generation (cyclic
arraybased sequencing)
Stands of fragmented DNA are amplied;
then bases are added sequentially using
DNA polymerase; excess reagent is
washed out, imaging identies base
incorporated, and process repeats
Targeted sequencing; whole
genome sequencing
Higher throughput has provided signicant
advantages; however, limitations such as
sample preparation, short read lengths,
and relatively slow run time have limited
clinical use; newer versions (such as
MiSeq Illuminaor 454 Junior Roche)
sacrice genome coverage for faster run
time to become more amenable to
clinical application
454 (Roche, Basel,
Switzerland)
4,5,10
Pyrophosphate released at time of base
incorporation
HiSeq (Illumina, San Diego,
CA)
4,5,9
Fluorescent-labelled nucleotides added
simultaneously
SOLiD 4 (Life Technologies,
Carlsbad, CA)
4,5,10
Driven by DNA ligase instead of DNA
polymerase
Third generation (novel technologies)
PacBio RS (Pacic Biosciences,
Menlo Park, CA)
4,10,11
Single-molecule real-time sequencing;
imaging of dye-labelled nucleotides as
they are incorporated during DNA
synthesis by single DNA polymerase
molecule
Targeted sequencing; whole
genome sequencing
Results in long read lengths, short run time,
and high throughput with simple sample
preparation; potential for clinical
application
Ion Torrent PGM (Life
Technologies)
10,12
Nonoptical DNA sequencing; massively
parallel semiconductor senses ions
produced as nucleotides are incorporated
by DNA polymerase-based synthesis
Targeted sequencing; whole
genome sequencing
Low technology cost and short run time;
potential for clinical application
Genotyping
Restricted fragment length
polymorphism
13,14
Uses restriction enzymes to fragment DNA
in presence of targeted mutation; then
gel electrophoresis separates resulting
fragments, identifying mutation
Single somatic mutation
analysis
Allows detection of low-frequency
mutations ( 4%) but has low
throughput and is dependent upon
subjective visual interpretation; still used
in some centers for KRAS mutation
testing; however, not feasible method for
high-throughput genotyping
Taqman OpenArray Genotyping
System (Applied Biosystems,
Carlsbad, CA)
14,15,16
Uses allele-specic PCR and dye-labelled
probes (Taqman assay) combined with
uorescent readout systems
Somatic mutation analysis;
SNP genotyping
Effective and accurate high-throughput
genotyping platform
MassARRAY (Sequenom, San Diego,
CA)
14,15,16
Uses allele-specic PCR combined with
MALDI-TOF mass spectrometry to detect
mutations/SNPs
Somatic mutation analysis;
SNP genotyping; gene
expression analysis;
methylation analysis
Effective and accurate high-throughput
genotyping platform; able to detect low-
frequency mutations ( 10%); premade
(Oncocarta) and customized mutation
panels available
ABI PRISM 3100 Genetic Analyzer
(Applied Biosystems)
14,17,18
Uses allele-specic PCR with
oligonucleotide primers and labelled
nucleotides for primer extension
(SNaPshot assay) combined with capillary
electrophoresis and optical imaging
Somatic mutation analysis;
SNP genotyping; gene
expression analysis;
methylation analysis
Effective and accurate high-throughput
genotyping platform
iScan (Illumina)
15,16
Uses allele- and locus-specic PCR with
oligonucleotide primers; hybridization of
assay products onto BeadChip; then
imaging of uorescent signals
Somatic mutation analysis;
SNP genotyping; gene
expression analysis;
methylation analysis
Effective and accurate high-throughput
genotyping platform
Gene Titan (Affymetrix, Santa Clara,
CA)
Uses microarray technology and GeneChip
arrays
Somatic mutation analysis;
SNP genotyping
Effective and accurate high-throughput
genotyping platform
aCGH platform (Agilent, Santa Clara,
CA)
19
Uses microarray technology and CGH arrays
(including Agilent and Oxford Gene
Technology Oxford, United Kingdom
arrays) to detect copy number variations
aCGH Effective platform for analysis of copy
number variations with high resolution
and high throughput
Abbreviations: aCGH, array-based CGH; CGH, comparative genomic hybridization; MALDI-TOF, matrix-assisted laser desorption/ionizationtime of ight; NGS,
next-generation sequencing; PCR, polymerase chain reaction; SNP, single nucleotide polymorphism.
Cancer Genomics
www.jco.org 2012 by American Society of Clinical Oncology 649
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
ABI 3730 DNA Analyzer (using SNaPshot assays; Applied Biosys-
tems), iScan platform(using Goldengate assays; Illumina, San Diego,
CA), Affymetrix genotyping arrays (Santa Clara, CA), and MassARRAY
platform(usingmass spectrometrywithmatrix-assistedlaser desorption/
ionizationtime-of-ightanalysis; Sequenom, SanDiego, CA).
14-18
These
high-throughput genotyping platforms can analyze hundreds to mil-
lions of germline and/or somatic variants simultaneously and are
distinctly different from sequencing technologies. Whereas DNA se-
quencing can detect any sequence variant in the gene(s) evaluated,
genotyping detects only known variants that have been selected for
analysis. Because multiplexed assays and microarrays are relatively
inexpensive and provide results rapidly, they are currently the most
common technologies used for both somatic and germline mutation
genotyping in clinical samples.
Simple somatic mutations are only one of several types of
genetic aberrations that have the potential to be predictive bio-
markers. Translocations, DNA amplications, deletions, methyl-
ation, and gene expression also are important, and assaying for
these aberrations also can be performed. In the clinic today, uo-
rescence in situ hybridization (FISH) is the gold standard for iden-
tication of ERBB2 amplication.
25-27
However, like restriction
fragment lengthpolymorphism, FISHhas a lowthroughput. Toiden-
tify and validate gene copy number changes that include deletions,
gains, andamplications (whengene copynumber is greater than10),
ahigher-throughput technologyis required. Array-basedcomparative
genomic hybridization is a molecular-cytogenetic method for detec-
tionof gene copy numbers that has highresolutionandhighthrough-
put. Technologies such as the Agilent array-based comparative
genomic hybridizationplatform(SantaClara, CA) are able toperform
high-throughput genotyping for gene copy number variations inclin-
ical samples.
19,28
Multiplexed assays and microarrays are currently the dominant
technologies in high-throughput genotyping of somatic mutations,
gene copy number variations, and other alterations affecting gene
expression or DNA methylation.
29
However, as costs associated with
targeted or whole-genome sequencing fall, NGS platforms may be-
come the preferred option.
Bioinformatics
Bioinformatics is the application of statistics and computer
science to biology. It includes both information management (eg,
genomic databases and visualization) and algorithm development,
particularly for the assembly, annotation, and comparison of
genomes.
30-33
As detailedinTable 2, these bioinformatic functions are
an essential component of cancer genomics. A detailed discussion of
bioinformatics in the age of NGS is beyond the scope of this review;
instead, the reader is referredtoanexcellent reviewof this topic byPop
et al.
30
DISCOVERY
The discovery of genetic aberrations in human cancers has identied
potential therapeutic targets andprovidedkey insights into the mech-
anisms underlying tumorigenesis,
34-41
as described in an excellent
reviewby Stratton et al.
42
The ICGC, formed in 2008 and incorporat-
ing the Cancer Genome Project of the United Kingdom and the
Cancer Genome Atlas of the United States, coordinates research proj-
ects that aim to comprehensively elucidate genomic changes present
in multiple cancers.
43
Its primary goals are to generate comprehen-
sive catalogues of genomic abnormalities in 500 tumors from each of
50 different cancer types and to accelerate research into the causes
and control of cancer.
43
Whereas ICGC projects aim to develop a molecular map of the
geneticaberrations involvedincancer, genome-wideassociationstud-
ies (GWAS) investigate the inherited basis of cancer by comparing
common DNA variations in a large set of unrelated patient cases and
controls andidentifying genetic variants associatedwithalteredrisk.
44
AlthoughGWASare important inthe larger scheme of cancer genom-
ics, this article focuses predominantly onacquired genetic aberrations
that arise in the genomes of cancer cells.
Results from ICGC studies of glioblastoma multiforme (GBM),
ovarian carcinoma, and chronic lymphocytic leukemia have been
published.
38,45,46
These studies surveyed for gene mutations, DNA
copy number, gene expression, and methylation in large cohorts. The
GBMstudyidentiedasubstantial proportionof tumors withMGMT
promoter methylation, now known to be a predictive biomarker for
Table 2. Role of Bioinformatics in Cancer Genomics
Bioinformatics
Function Background
Genome alignment
and
reconstruction
Alignment and reconstruction requires reads
sufciently long enough to be mapped accurately
onto reference genome sequence
13,15,21
Mapping processes must efciently handle millions of
generated sequences while being robust in
presence of sequencing errors and SNPs
13,21
Existing sequencing alignment tools like BLAST or
BLAT are adequate for long reads produced by
Sanger sequencing, but for short reads produced by
NGS, newer alignment tools are being developed to
allow for mismatches and/or gaps
13,21
SNPs identied through this process must be carefully
analysed to ensure they are real and not a result of
technology-specic errors
13,21
Base calling Base calling is process of converting sequencing
signals into base and is essential for SNP and
somatic variant identication
31
Improvements in base calling accuracy are essential to
reduce false positives and lead to more reliable
identication of germline and somatic variants
31,33
De novo genome
assembly
De novo genome assembly is like solving a large
jigsaw puzzle without knowing the nal picture
Several assembly tools have been adapted or
independently developed for generating assemblies
from short reads
30,31
Genome browsing
and annotation
Genome browsing and annotation enable millions of
sequences to be available to biomedical community
through easily accessible and user-friendly systems;
essential for collaboration and progress in research
Commonly used browsers include EntrezGene
browser, University of California Santa Cruz genome
browser, and European Bioinformatics
Institute/Ensemble browser
31
Commonly used browsers containing cancer mutation
datasets include COSMIC and ICGC
National Centre for Biotechnology Information SNP
database stores millions of SNPs,
31
which can be
useful in classifying mutations into known germline
variants
Abbreviations: BLAST, Basic Local Alignment Search Tool; BLAT, BLAST-Like
Alignment Tool; COSMIC, Catalogue of Somatic Mutations in Cancer; ICGC,
International Cancer Genome Consortium; NGS, next-generation sequencing;
SNP, single nucleotide polymorphism.
Tran et al
650 2012 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
temozolomide sensitivity.
38
The ovarian study identied impaired
homologous recombination in approximately 50% of tumors, a
potential predictor for benet from poly (ADP-ribose) polymerase
inhibitors.
45
The chronic lymphocytic leukemia study demonstrated
that NOTCH1 and MYD88 mutations are associated with distinct
clinical subgroups with specic biologic features.
46
These results vali-
date the role of cancer genomics in achieving PCM.
Sequenced Cancer Genomes
Much of the focus in cancer genomics has centered on sequenc-
ing cancer genomes and identifying potential driver mutations (ie,
mutations that arefunctionallycritical inthetumor). Cancer genomes
from several tumor types have been sequenced and published (Table
3). The earliest comprehensive survey of human genes in cancer by
sequencing methods examined the whole exome (20,661 genes) of 22
human GBM samples, correlating sequencing results with patient
outcome data. This study resulted in the unexpected but important
nding of IDH1 mutations as a potential favorable prognostic bio-
marker.
39
These initial results providedearlyvalidationof the utilityof
genome sequencing in cancer.
Whole genomes (or exomes) of acute myeloid leukemia, mel-
anoma, small-cell lung cancer, prostate cancer, pancreatic cancer,
hepatocellular carcinoma, and multiple myeloma have also been
sequenced. Results from each study illustrate the effectiveness of
cancer genome sequencing in furthering our understanding
of cancer.
35-37,40,47-49
Epigenetics and Gene Expression
Epigenetic aberrations incancer, suchas global hypomethylation
of DNA, hypermethylation of tumor-suppressor genes, and inactiva-
tion of microRNA by DNA methylation, are being systematically
studied, because it is clear they canhave a signicant impact ontumor
biology and treatment outcomes.
50
Using transcriptional proling,
gene expression signatures are also being studied extensively in can-
cer.
51
However, because of challenges associated with reproducibility,
only a fewvalidateddiscoveries have beenmade todate. These include
the novel molecular classicationof breast cancer initially reportedby
Perou et al
52
and the development of validated recurrence scores for
early breast cancer such as OncotypeDX(Genomic Health, Redwood
Table 3. Sequenced Cancer Genomes
Author Tumor
No. of
Samples Tissue Type
Genome
or Exome Novel Mutations
Novel
Mutations in
Coding Regions Comment
Ding et al
34
Basal-like breast
cancer
1 Blood, primary,
metastasis,
xenograft
Genome 27,173, primary;
51,710,
metastasis;
109,078,
xenograft
200, primary;
225,
metastasis;
328,
xenograft
48 validated somatic mutations
present in all three tumor
tissues, with two additional
mutations in metastasis
Mardis et al
35
AML 1 Tumor, skin Genome 20,256 113 Recurrent mutations in IDH1
discovered
Ley et al
41
AML 1 Tumor, skin Genome 31,632 241 Eight newly dened somatic
mutations for AML
Pleasance et al
37
Malignant
melanoma
1 Cell line,
lymphoblastoid
cell line
Genome 33,345 292 Identication of mutation
signature caused by
exposure to ultraviolet light
Pleasance et al
36
Small-cell lung
cancer
1 Cell line,
lymphoblastoid
cell line
Genome 22,190 134 Identication of mutation
signature caused by
exposure to tobacco smoke
Parsons et al
39
GBM 22 Seven tumors; 15
xenograft, blood
Exome
NA 47 (mean) Recurrent mutations in IDH1
discovered
Berger et al
40
Prostate cancer 7 Tumor, blood Genome 3,866 (median) 20 (median) Four of seven patients
harbored events disrupting
PI3K pathway
Jones et al
47
Pancreatic cancer 24 Tumor, normal
duodenum
Exome
NA 63 (mean) Identied 12 pathways,
component genes of which
were most altered in
pancreatic cancer
Chapman et al
48
Multiple myeloma 23 Bone marrow, blood Genome 7,450 (mean) 35 (mean) BRAF mutations identied in
4% of samples
Totoki et al
49
HCC 1 Tumor, blood Genome 12,401 88 Signicant intratumoral
heterogeneity demonstrated
by TSC1 mutation frequency
of 13%; only detected by
whole exome sequencing at
higher sequence depth
Puente et al
46
CLL 4 Tumor, blood Genome 1,038 (mean) 23 (mean) NOTCH1 and MYD88
mutations associated with
distinct clinical subgroups of
CLL
Abbreviations: AML, acute myeloid leukemia; CLL, chronic lymphocytic leukemia; GBM, glioblastoma multiforme; HCC, hepatocellular carcinoma; NA, not
applicable; PI3K, phosphoinositide 3-kinase.
Total of 20,661 protein coding genes were sequenced.
Study also performed whole exome sequencing for 16 patients not reported in Table 3.
Study also performed targeted sequencing for 363 patients not reported in Table 3.
Cancer Genomics
www.jco.org 2012 by American Society of Clinical Oncology 651
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
City, CA) and MammaPrint (Agendia, Irvine, CA).
53,54
Gene expres-
sion signatures can contribute to PCM by being diagnostic, prognos-
tic, and/or predictive, and such proling efforts can be broadened to
encompass other therapeutic strategies including regulation of the
immune system. In cancer immunotherapy, efforts aimed at person-
alizing treatment are investigating the potential insights gained from
transcriptional proling, including the exploration of the prognostic
and predictive impact of immune signatures in the tumor microenvi-
ronment and of potential markers that may be associated with re-
sponse to immunotherapy. These approaches may also provide
potential candidate tumor-associatedantigens for the development of
cancer vaccines.
55-59
Our understanding of cancer is reliant not only on sequencing
the cancer genome but alsoonidentifying epigenetic andgene expres-
sionchanges. Additionally, althoughthe scope of this reviewis limited
primarily to genomics, the potential role of cancer proteomics in
PCM, as described by Hanash et al,
60
must also be recognized.
Conceptual Debates
Debate regarding cancer genomics occurs on multiple levels.
Weinberg
61
raises concerns regarding the enormous amount of re-
sources and researcher energy involved in sequencing entire cancer
genomes with only modest dividends to date; Heng
62
believes the
current concept of cancer needs to be re-examined to ensure ndings
fromICGCprojects are not wasted. Stratton et al
42
note this debate is
not new to genomics and liken it to arguments that occurred before
the human genome was sequenced. They agree that the cost of se-
quencing large numbers of cancer genomes may be astronomical and
that ndings are not entirely predictable; however, given that the
human genome is nite, this is a deliverable project with a scope that
goes beyond identifying cancer genes. For example, as illustrated by
the GBM and ovarian cancer genome projects, comprehensive cata-
loguing of somatic mutations can generate insights into genetic pat-
terns that underlie phenotype, prognosis, and drug response.
42
Challenges and Issues
Aside from the ongoing conceptual debate, we have identied
four major considerations incompletingthe molecular mapof cancer:
sequencing exomes versus whole genomes, differentiating between
driver andpassenger mutations, integratingdataacross platforms, and
nding solutions to problems associated with multiple testing.
Exome versus whole-genome sequencing. Exomes are protein-
coding genomic regions and constitute approximately 1% of the
whole genome.
63
Because of nancial constraints, many cancer ge-
nome projects sequence exomes rather than whole genomes,
21,38,63-65
yet whether this is the best approach remains debatable.
21,64,66
Muta-
tions within exomes are easier to interpret.
66,67
For example, muta-
tions that lead to a change in protein sequence can be easily
distinguished from noncoding variants. By contrast, there is less un-
derstanding of the function of noncoding regions.
42,68
On the other
hand, whole genome sequencing of a lung cancer cell line identied
22,910 point mutations, but only 134 (0.6%) were in exomes.
36
What
do the other 22,776 mutations represent? The answer to this question
is not known, but it can be argued that it will remain unanswered
unless each one is systematically investigated.
42,67
Mardis et al
35
dis-
covered a recurring nongenic mutation in sequencing an acute my-
eloid leukemia genome. They contend that nding mutations in
noncoding regions may greatly improve our understanding of cancer
anduncover newmechanisms of cancer pathogenesis.
69
Theopposing
view is that expending cost and time investigating mutations in non-
coding regions impedes progress inunderstanding the result of muta-
tions withincodingregions, fromwhichdiscovery of cancer genes and
potentially druggable genes will make real differences in can-
cer care.
21,63,64
Drivers versus passengers. Within individual cancer genomes
sequenced thus far, hundreds to thousands of mutations are
present.
34-41
Assigning relevance to each is difcult. Many of these
mutations areprobablypassenger mutations; that is, theywerepresent
but irrelevant in the dominant cancer clone when critical mutations
leading to tumorigenesis were acquired, or they represent de novo
mutations that arose subsequentlyinrapidlydividingcancer cells. The
greatest challenge in cancer genomic discovery is distinguishing be-
nign passenger mutations from those relevant to pathogenesis (ie,
driver mutations). Driver mutations confer growthadvantage and, by
denition, reside in the subset of genes known as cancer genes.
42,70
Knowing whether a mutation is recurrent and being aware of its
frequencyinthe examinedsample canassist indifferentiatingbetween
drivers and passengers. However, the gold standard is functional val-
idation of the mutation in vitro and/or in vivo.
Passenger mutations are generally distributed randomly across
the genome, whereas driver mutations cluster within cancer genes.
42
The likelihood of having identical mutations at the same position in
multiple samples is extremely low; therefore, the vast majority of
mutations recurringinthesamegenomicregions arelikelytobedriver
mutations.
42,69
Because many cancer genes seem to contribute to
cancer development in only a small fraction of tumors (for example,
only approximately 10% of colorectal cancers [CRCs] have a BRAF
mutation
71
), large sample sets must be analyzed to distinguish infre-
quently mutated cancer genes from genes with random clusters of
passenger mutations.
42
To be condent of identifying a cancer gene
that is mutated in 5% of a particular type of cancer, hundreds of
samples need to be sequenced.
42
Mutation frequency refers to the percentage of DNA in which a
mutation is identied and can be used in statistical calculations that
differentiate drivers from passengers.
42
In theory, heterozygous mu-
tations present in all cancer cells should have a frequency of 50%,
whereas homozygous germline variants should have a frequency of
100%.
72
Because tumors are typically contaminated by normal tissue
(tumor stroma), mutational frequencies generated by NGS require a
correctionfactor to determine the actual frequency of the mutation.
35
Although tumor heterogeneity can result in a wide spectrum of mu-
tation frequencies, in general, driver mutations have frequencies at or
lower than 50%.
Functional validationintissue cultures or model organisms is the
gold standard for assessing mutation signicance.
66,69,70,72
This in-
volves assembling multiple mutations into a single cell or model or-
ganism and requires signicant resources and time. Scott et al
73
recently published an example of a complete genomics-to-function
paradigm. They identied a genomic region at 5p13 that was com-
monlyampliedinseveral cancer types, includinglung, ovarian, pros-
tate, and breast cancers and melanoma. An integrated analysis of this
region pinpointed the Golgi-associated protein GOLPH3 for further
study. In vitro and in vivo experiments involving knockdown and
amplication of the GOLPH3 gene led to a linkage between GOLPH3
and the mammalian target of rapamycin, thus establishing GOLPH3
Tran et al
652 2012 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
as a cancer gene.
73
This supports the need for functional studies of
genomic alterations discovered by sequencing.
Integrating data. NGS and the resulting rapid increase in
genome-scale data production have created great challenges in data
integration. Data integrationamong multiple samples andtechniques
is essential for making reliable inferences from genomics data,
31,74,75
because often, an individual technique tells only part of the story. For
example, genomic sequencing can identify structural variations, but
only by adding a technique that assesses RNAlevels, suchas RNA-seq,
can it be determined whether the structural variations affect the tran-
scription levels of a gene. The major hurdles to integration are heter-
ogeneity of the experimental and analytic protocols, varying levels of
data quality, and differences in data representation.
31,74,75
In particu-
lar, boththe frequencyanddistributionof false positives andnegatives
have to be understood for each data set before attempting to integrate
and interpret them. Data integration will remain challenging as more
cancer genomes are sequenced, and innovative bioinformatics strate-
gies are needed to facilitate this process.
Multiple testing. The wealth of data produced by genomic stud-
ies using high-throughput technologies presents a unique set of chal-
lenges relatedtoidenticationof true positives inthe context of a large
number of statistical hypotheses and comparisons, so-called multiple
testing. This is particularly relevant in cancer genomics, where it is
common for hundreds to thousands of genes to be scrutinized in
studies aimed at identifying prognostic, predictive, or diagnostic mo-
lecular biomarkers in selected cancers. Naive application of standard
hypothesis tests without adjustment for multiple testing in these situ-
ations will result in large numbers of nonreproducible false positives.
On the other hand, using multiple testing statistical methods to con-
trol false positives in situations where families of tests are performed
can greatly reduce the power to detect true discoveries.
76
As the
amount of genetic data available increases, so too will problems asso-
ciated with multiple testing.
77,78
TRANSLATION
There is universal expectation that the technologic advances and the
understanding of the molecular basis of cancer gained from studying
cancer genomes will be translated into benets for patients with can-
cer. One of the most valuable translational approaches is to develop
therapeutic agents that target genetic druggable aberrations discov-
ered by studying cancer genomes. Targeted agents that act selectively
on cancer cells harboring these aberrations may provide a greater
therapeutic effect than traditional cytotoxic agents or unmatched tar-
geted agents.
The druggable genome was rst described by Hopkins et al
79
in
Nature in2002. Theydenedaproteinas druggableif asmall molecule
could bind it at the required binding afnity. They noted a protein
may be druggable, but for it to be a potential drug target, it must be
linked to disease.
79
Although these denitions were not made with
cancer in mind, they can be extrapolated. By denition, actionable
aberrations are disease modifying, but not all are druggable.
Currently, several genetic aberrations have been validated as ac-
tionable and druggable. ERBB2 amplication in breast cancer, EGFR
mutations in nonsmall-cell lung cancer (NSCLC), and BRAF muta-
tions in melanoma are actionable and druggable, because they are
prognostic, have their gene products targeted by molecularly targeted
therapies, and are predictive of their benet.
26,80-83
Alternatively, al-
though IDH1 mutations in GBM are actionable as a prognostic bio-
marker, treatments targeting their gene products do not currently
exist, andhence IDH1 mutations are not yet druggable.
39
It is relevant
topoint out that the identicationof actionable anddruggable genetic
aberrations is only one of many means to increase the cancer thera-
peutic armamentarium, and not all actionable and druggable cancer
targets are the products of genetic aberrations. Targets of cancer im-
munotherapy, such as CTLA4 in metastatic melanoma (inhibited by
ipilumumab to improve immune response), CD20 in diffuse large
B-cell lymphoma (targeted by rituximab), or prostatic acid phospha-
tase in prostate cancer (targeted by immune cells induced by
sipuleucel-T), arenot directlytheresults of geneticaberrations inthese
cancers, yet they are druggable by biologic therapeutics andactionable
because suchtargetedtherapeutics canimprove cancer outcomes.
84-86
As the number of potentially actionable and druggable aberra-
tions increases, the repertoire of novel therapeutics studied in early-
phase clinical trials also increases. To validate the predictive value of
genetic aberrations, clinical trials need to be appropriately de-
signed.
87,88
Dancey et al
89
have published guidelines for developing
biomarker studies in early-phase clinical trials. They and others
suggest using molecular targets to guide patient selection for inves-
tigational targeted agents,
90
although this could also apply to inves-
tigational immunotherapeutic agents. Molecular proling (MP) will
enable enrollment onto these studies without the need for individual
tests for each genetic aberration, thus enhancing the efciency of
investigational drug development. For this reason, there is a burgeon-
ing need for MP in the clinic.
MP
Three initial studies examined the feasibility of MP using high-
throughput genotyping (Table 4). Thomas et al,
22
Dias-Santagata et
al,
23
and MacConaill et al
24
collectively examined between 250 and
1,000individual tumor specimens for 120to400mutations in13to33
known oncogenes and tumor suppressor genes. These studies found
at least one mutationin30%to37%of tumor samples andconcluded
that high-throughput genotyping enables sensitive and accurate on-
cogenic mutational proling in human cancer specimens.
More recently, studies have examined the feasibility of real-time
MP of tumors from actual patients and matching of the identied
molecular prole with targeted treatments. Von Hoff et al
91
con-
ducted a study of matching treatment to molecular prole in 86
patients across nine different centers in the United States. Only 66
patients proceeded to MP, wherein 64 targets were examined using a
combination of immunohistochemistry (IHC), FISH, and gene ex-
pression microarrays. Each aberration was matched to a predened
treatment. In 18 of 66 patients, they demonstrated progression-free
survival for matchedtreatment tobe 1.3times greater thanthat for the
treatment patients had received immediately beforehand. Tsimberi-
dou et al
92
performed molecular analysis of 1,283 patients, with suc-
cess in 1,144 (89%). They used PCR, FISH, and IHCin examining for
11 separate aberrations. In their cohort, 40% of patients had at least
one aberration. They matchedeachaberrationtoa targetedtreatment
whenavailable anddemonstratedthat patients whoreceivedmatched
targeted therapy had better response rates and improved time to
treatment failure.
While Von Hoff et al
91
and Tsimberidou et al
92
enrolled patients
with any tumor type, cancer-specic genotyping studies have also
Cancer Genomics
www.jco.org 2012 by American Society of Clinical Oncology 653
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
been performed. Recently, Kim et al
93
published a report on the
BATTLE(Biomarker-IntegratedApproaches of TargetedTherapy for
Lung Cancer Elimination) study, in which 255 patients with pre-
treated metastatic NSCLChad their disease prospectively biopsied for
evaluationof ve biomarkers. They also matched each biomarker to a
predenedtreatment anddemonstrateda 46%8-weekdisease control
rate with this strategy.
Princess Margaret HospitalOntario Institute for
Cancer Research Clinical Genomics Initiatives
The Princess Margaret Hospital (PMH) University HealthNet-
work and the Ontario Institute for Cancer Research (OICR) have
developeda genomic pathwaystrategytosystematicallyevaluate PCM
using NGS and high-throughput genotyping platforms. A feasibility
study is currently enrolling patients. This study will performMPusing
somatic mutation genotyping and targeted exome sequencing of can-
cer genes through the MassARRAY (Sequenom) and PacBio RS (Pa-
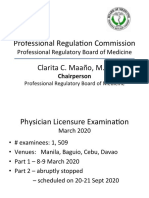
cic Biosciences) platforms. Figure 1 outlines the study design. The
addition of targeted sequencing allows detection of novel and poten-
tially actionable mutations intarget genes, comparedwithgenotyping
methods. Patients are being enrolled from ve cancer centers
throughout Ontario, Canada, andwill beobservedfor 2years, withthe
impact of MP on treatment decisions reassessed at regular intervals.
Indicators of feasibility include a 21-day turnaround fromconsent to
reporting of results and discovering actionable mutations in at least
30% of patients. During the course of this study, several issues and
challenges have beenidentiedintranslatingcancer genomics intothe
clinic, some of which are discussed here.
Candidate gene selection. Candidate genes selected for MP are
inuenced by the aims of MP, technology at hand, and treatment
options available. The majority of MP studies presented in Table 4
performed extensive literature reviews in creating their gene lists,
whereas Tsimberidou et al
92
only selected genetic aberrations with
validatedmolecular diagnostic tests ina Clinical Laboratory Improve-
ment Amendments (CLIA) certied laboratory.
BecauseMPis likelytobeusedfor patient selectioninearly-phase
clinical trials in the near future, it is important that genes selected for
analysis are potential, albeit unvalidated, predictors of efcacy for
existing investigational therapies. The genetic aberration associated
with each selected gene, whether that is mutation, amplication,
methylation, or other, should also be specied. Developmental thera-
peutic agents are evolving constantly, such that any list of candidate
genes and corresponding aberrations can rapidly become out-
dated; thus, any gene list used in MP should be regularly reviewed
and revised.
Gene selection for MP has focused on oncogenes, tumor sup-
pressor genes, and genomic stability genes. However, we believe that
to fully implement PCM, germline genetic aberrations involved in
drug metabolismshouldalsobe examined, because there is increasing
evidence of their role in predicting the efcacy and toxicity of can-
cer therapies.
94-96
The PMH-OICRled feasibility study surveyed 19 experts in
cancer genomics to create a candidate gene list for MP. Experts in-
cluded drug developers and genome scientists. An in-depth literature
search of the PubMed, COSMIC, and Genecard databases led to the
selection of 194 genes with aberrations known to be important in
tumorigenesis or drug metabolism. The survey asked each expert to
assign an importance score to each gene: one, highest; two, interme-
diate; three, lowest; and four, unknown. The mean score assigned to
each gene was calculated, and genes were ranked from most to least
important. This list was used to generate a gene panel for MP. Inter-
estingly, the survey identied signicant differences in the way drug
developers and genome scientists assigned importance to genes (Ap-
pendix Table A1, online only). Drug developers were signicantly
more likely to assign higher importance to genes targeted by estab-
lished or investigational agents.
97
Althoughcancer genomics has been
the domain of genome scientists, this survey demonstrates that in-
volvement of drug developers is crucial to ensure that a clinically
relevant gene panel is created for MP.
Proling archival versus current tumor samples. Most patients
with cancer have archived formalin-xed parafn-embedded (FFPE)
tissue available for MP. However, it is unclear whether archivedtumor
tissue, generally from the primary tumor, accurately represents the
current disease state, particularly if that is metastatic cancer that has
Table 4. Molecular Proling in Clinical Tumor Samples
Author
Total Samples Genes Analyzed
Mutations Detected
Samples
With at
Least One
Mutation
Method No. Tumor Types No. Mutations/Aberrations No. %
Dias-Santagata et al
23
250 26 13 120 100 86 34 Multiplex PCR-based targeted SNP
analysis (SnaPshot; Applied
Biosystems, Carlsbad, CA)
MacConaill et al
24
903 12 33 396 417 335 37 MassARRAY (Sequenom, San Diego,
CA) somatic mutation analysis
Thomas et al
22
1,000 17 17 238 NA 298 30 MassARRAY (Sequenom) somatic
mutation analysis
Von Hoff et al
91
86
25 51 NA 84 98 IHC, FISH, and gene expression
microarray
Tsimberidou et al
92
1,283 NA 11 12 NA NA 40 PCR, FISH, IHC
Abbreviations: IHC, immunohistochemistry; FISH, uorescence in situ hybridization; NA, not applicable; PCR, polymerase chain reaction; SNP, single
nucleotide polymorphism.
Eighty-six evaluable patients.
Thirteen also had protein expression examined by IHC.
Includes signicant change in gene or protein expression.
Tran et al
654 2012 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
progressed through multiple treatments. Molecular discordance be-
tweenprimary andmetastatic disease does occur, but it seems todiffer
between cancer types. In CRC, primary/metastatic concordance is
highfor KRAS andBRAFmutations.
98,99
By contrast, inbreast cancer,
primary/metastatic genotypic differences were observed in a WGS
study, and reported discordance for both ERBB2 amplication and
estrogen receptor expression has not been insignicant.
34,100
It re-
mains unclear whether the future of MP will require archived or
current tumor samples; however, if current tumor samples are re-
quired, a fresh tumor biopsy is needed.
101
Because biopsies are not
without risk, noninvasive strategies are being explored, including cir-
culating tumor cells and circulating DNA.
102
The PMH-OICR feasi-
bility study is using specimens from fresh biopsies to perform MP.
However, archival specimens are also being collected and proled so
that primary/metastatic genotypes can be compared.
Although promising, novel methods of tumor sampling do not
address the problem of tumor heterogeneity. Tumor heterogeneity is
dened as the simultaneous presence of multiple clonal subpopula-
tions of tumor cells within a single neoplasm, and it represents a
signicant barrier to achieving PCM and a possible explanation for
mixed responses to targeted therapies.
103,104
Performing multiple bi-
opsies at different sites is one potential solution to account for tumor
heterogeneity, but this is often impractical. Currently, there is no
solution to this problem.
Process optimization. The usefulness of tissue for MP is inu-
enced signicantly by specimen handling. Crucial components in-
clude optimization of tissue xation and embedding methods. Both
assist in obtaining clear histologic detail and facilitate elucidation of
gene andproteinexpressionproles.
20,105
Snapfreezing andFFPEare
typical processing methods.
105
Although FFPE tissue allows for histo-
logic examination, it does not prioritize preservation of DNA, RNA,
and proteins.
106,107
Traditionally, optimal molecular preservation in
tissue has been achieved through snap freezing.
105
However, many
centers are now comfortable with extracting DNA from FFPE sam-
ples, and studies have shown that this can be done successfully.
108
These advances facilitate MP of archival specimens.
One technical challenge related to proling of clinical samples is
separating tumor from tumor stroma. A good-quality biopsy will
generally ensure that the amount of necrotic tissue is minimal; how-
ever, cellular components fromtumor stroma are sure to be included
if DNAis extracted frombulk tissue. In this situation, extracted DNA
will be representative of both tumor cells and unwanted normal cells.
Laser-capture microdissection is a robust technique that can isolate
tumor cells,
108-111
but the cost and time involved are not amenable to
real-time MP. Although less effective than laser-capture microdissec-
tion for isolating tumor, macrodissection is more commonly used for
MP, because it is more economic and less time consuming. Alterna-
tively, DNAcan be extracted frombulk tumor, with the percentage of
Patient
Consent and
screening
Blood sample
Tumor biopsy
Archived tumor
DNA
extracted
Somatic mutation
genotyping
Targeted exome
sequencing
Mutations
identified
Sanger
sequencing
Expert
panel
Molecular profile
report generated
Clinician
Validated
mutations
Treatment
decisions
Follow-up
Recording of
efficacy and toxicity
of matched
treatments
Recording of
impact of
molecular profile
on treatment
Follow-up
Fig 1. Princess Margaret HospitalOntario Institute for Cancer Research feasibility study of somatic mutation genotyping and targeted exome sequencing.
Patients sign informed consent to enter the study and undergo screening to ensure there are no contraindications to biopsy. A blood sample is collected for
germline DNA, a tumor biopsy is performed, and archived tumor is retrieved. After DNA extraction, somatic mutation genotyping is performed using the
MassARRAY platform (Sequenom, San Diego, CA), and targeted exome sequencing is performed using the PacBio RS platform (Pacic Biosciences, Menlo Park,
CA). If required, identied mutations are conrmed by Sanger or other validated methods in a College of American Pathologists/Clinical Laboratory Improvement
Amendmentscertied laboratory. Validated mutations are reviewed by an expert panel, and a molecular proling report is generated for the clinician. The study
aims to produce a report within 21 days of patient consent. The initial report outlines mutations in the fresh tumor biopsy. Delayed results from analysis of
archived tumor are provided in an amended report. The clinician reviews the report and makes treatment recommendations for the patient. Clinicians are asked
to record the impact of the molecular proling report on their treatment recommendations. Patients are observed every 3 months for 2 years, and efcacy and
toxicity related to matched treatments are recorded.
Cancer Genomics
www.jco.org 2012 by American Society of Clinical Oncology 655
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
tumor cells in the sample considered in evaluating the resultant mo-
lecular prole. Regardless of howthe DNAis acquired, there must be
a sufcient quantity for MP, and this is dependent on the amount of
viable tumor available within the sample. Hence, it is important that
any sample used for MP be reviewed to assess sample quality, provide
histopathologic conrmationof tumor, anddetermine the percentage
of tumor cells present.
Technology validation. Many technologies are available for
high-throughput MP, including microarrays, mass spectrometry,
and NGS platforms. These platforms are able to analyze hundreds
to thousands of targets simultaneously. With every technology
comes the potential for errors and biases, particularly resulting
fromthe long chain of decisions required in sampling, preprocess-
ing, processing, calibration, and analysis.
112
Guidelines have been
published regarding the minimum information needed for an
expression microarray experiment, and these have ensured process
standardization for this technology.
113
For other platforms, there
are no published guidelines at present. Ioannidis
112
has opined that
any molecular prole emerges eventually out of an abyss of exper-
iments and analyses
112(p303)
and suggests that standardizationand
creation of a denitive and xed prole is required before MP is
ready for clinical decision making. The US Food and Drug Admin-
istration has also addressed concerns regarding reliability, preci-
sion, accuracy, and interlaboratory reproducibility of data derived
from MP.
114
The CLIA program sets standards and issues certi-
cates for clinical laboratory testing on human specimens that pro-
vide information for the diagnosis, prevention, and treatment of
disease. Any laboratory that plans to perform MP to affect clinical
decisions should be CLIA certied, ensuring accuracy, reliability,
and timeliness of the test performed. Furthermore, although cur-
rently only medical devices being evaluated in clinical trials are
mandated to have an investigational device exemption by the US
Food and Drug Administration, in the future, platforms used to
identify integral biomarkers that affect clinical decisions on clinical
trials (eg, patient eligibility) are also likely to require this exemp-
tion as well.
115
Once a platform is selected, it requires validation based on ve
performance metrics: sequencing accuracy, variant accuracy, false-
positive rate, false-negative rate, and variant discrepancy rate.
116
Harismendy et al
116
evaluated three NGS platforms against Sanger
sequencing by sequencing a human genome using all four platforms.
Although they demonstrated that NGS identied more than 95% of
variant alleles correctly, they also observed problems with systemic
biases and data variability. Improvements to these technologies have
mitigated these issues, but centers using NGS for MP and clinical
decision making need to ensure that processes are optimized to min-
imize potential problems. Even seemingly simple tests such as FISH
and IHCrequire validation and thorough quality control before their
use in biomarker-based studies, as learned from the lesson in ERCC1
testing, where the antibody used for IHCstaining was found to be not
specicfor this marker after initial publications.
117,118
At PMH-OICR,
somatic mutation genotyping and Sanger sequencing are performed
inaCLIA-certiedlaboratory, andthe PacBioRS(Pacic Biosciences)
and MassARRAY (Sequenom) platforms were tested thoroughly and
cross validated before the feasibility study opening.
Molecular proling reports. Currently, clinicians request testing
for the fewvalidated druggable and actionable genetic aberrations on
anas-neededbasis, andresults frommolecular diagnostic laboratories
are reported back to clinicians in a standardized format. For ERBB2
testing in breast cancer, published guidelines outline required report-
ing elements for both IHC and FISH: identication information,
pathology processes, results, interpretation, and standardized
comment.
119
Furthermore, it is recommended that ERBB2 testing
be performed in a CLIA-certied, College of American Pathologists
accredited laboratory.
119
It remains unclear how MP results will be reported to clini-
cians, because methods for reporting are still in development. At
PMH-OICR, MP reports are generated after an expert panel meeting
in which decisions are made regarding which mutations/aberra-
tions should be reported. The early experience of the PMH-OICR
expert panel (composed of clinical oncologists, pathologists, clin-
ical geneticists, ethicists, bioinformaticians, and genome scientists)
is that discussionemanating frommultiple perspectives is critical, partic-
ularlywhennewgermlineor somatic mutations arediscovered. Attached
to each report is a document based on a literature reviewthat details the
clinical signicance, if any, of the mutation(s) discovered. Documents
suchas this or, alternatively, online resources suchas MyCancerGenome
(a freely available online PCM resource developed by the Vanderbilt
Ingram Cancer Center that provides information regarding several im-
portant genetic aberrations in select cancer types) are essential to ensure
the clinician is fully informed regarding the importance of any discov-
eredmutation.
120
The Data Supplement provides an example of the PMH-OICR
MP report. Several considerations were taken into account in devel-
oping this report, and although some relate to legal aspects, most are
directed at assisting the clinician in interpreting the results (Table 5).
As MP becomes more widespread, guidelines for reporting will be
required. Furthermore, in keeping with guidelines for ERBB2 testing,
such reports should be generated by a CLIA/College of American
Pathologistsapproved molecular diagnostics laboratory.
Table 5. Issues to Be Addressed in Generating a Molecular Proling Report
Category Questions
Legal aspects Disclaimer
Specication that report is for research use only
Process specic Listing of all mutations for which analysis occurred
Listing of analysis failures
Description of platforms and methods used
Details of platform sensitivity and specicity
Laboratory CAP/CLIA certication
Mutation specic Inclusion of all mutations identied or only signicant
mutations
Processes involved in deeming mutations signicant
(eg, expert panel, functional validation)
Mutation nomenclature (chromosome position v
amino acid change)
Inclusion of mutation frequency
Clinical signicance
of mutation
Inclusion of literature-based information regarding
clinical signicance and known frequency of
mutation discovered
Inclusion of preclinical data in addition to clinical data;
evaluation of level of evidence of clinical data
Listing of clinical trials involving novel agents
targeting identied mutation
Listing of only clinical trials conducted in
geographically nearby centers
Abbreviations: CAP, College of American Pathologists; CLIA, Clinical Laboratory
Improvement Amendments.
Tran et al
656 2012 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
Ethics. Privacy, condentiality, and potential for subsequent
discrimination(fromincreased cancer risk identied by GWAS) have
beenidentiedas major considerations incancer genomics. Addition-
ally, three major ethical considerations associated with WGS have
been identied by McGuire et al
121
: identifying circumstances when
research results are disclosed to participants, identifying obligations
that are owedtoparticipants close genetic relatives, anddeciding how
future uses of samples and data taken from WGS are handled. Al-
thoughMcGuireet al address ethical issues associatedwithsequencing
germline DNA, these issues also have implications for MP of tumor
DNA, because germline DNAis usually analyzed simultaneously.
McGuire et al
121
recognize that the volume, complexity, and
clinical uncertainty of data generated from WGS can make commu-
nicationof researchresults challenging andrecommendthat expertise
is needed for interpretation and to ensure adequate understanding of
health and social implications. Two other studies have examined the
ethics behind reporting genetic research results to study participants
and concluded that only results that are associated with sufcient risk
andthat haveestablishedclinical utilityshouldbecommunicatedback
to patients.
122,123
Furthermore, McGuire et al suggest that only vali-
dated data approved by credentialed clinical laboratories be included
inhealthrecords. This approachhas beenadoptedinthe PMH-OICR
feasibility study.
Clinical impact. The presence of ERBB2 amplication in
breast cancer, EGFR mutation in NSCLC, and KRAS mutation in
CRC, to name a few, are genetic aberrations known to inuence
clinical decisions in medical oncology.
26,80-82,124,125
In the near
term, it is unlikely that a more comprehensive molecular prole
will inuence the prescription of regulatory agencyapproved
treatments, given the currently small number of validated predic-
tive biomarkers. However, the evolving nature of novel therapies in
early-phase clinical trials makes it attractive to use MP to select
patients for clinical trials, particularly because matched treatments
seem to provide clinical benet.
91,92
Past studies of MP have demonstrated that approximately 30% of
tumors proled have actionable mutations (Table 4).
22,23,24
Whether
knowledge of these aberrations will have a clinical impact is unknown.
Although many novel agents are in clinical trials, access to these early-
phase studies can be difcult for those who practice outside of large-
volume cancer centers. Thus, for a true clinical impact, MP must lead to
identicationof actionablegeneticaberrationsinasubstantial proportion
of patients, andnovel agents targetingthese aberrations must exist andbe
accessible through clinical trials at a reasonable distance to patients. Fur-
thermore, results of MP should be communicated to clinicians within a
reasonabletimeframe, sopatients remainwell enoughfor clinicians toact
onactionable aberrations. This is particularly important because patients
with advanced cancers can deteriorate rapidly. The PMH-OICR study
timeframe of 21 days from consent to results is consistent with other
genotyping studies, whichhave reportedmedianturnaroundtimes of 20
to30 days.
126,127
The potential impact of MP is not limited to clinical decision
making. MP also provides an opportunity to link pathway deregula-
tion with potential therapeutic strategies through biomarker valida-
tion.
128
For MP to evolve froman interesting scientic concept into a
clinical tool, several issues must be addressed and resolved: impact on
clinical decisionmaking, impact ondrugdevelopment andbiomarker
validation, cost effectiveness, and buy-in from the pharmaceutical
industry, which must accept that its potential market will be reduced
as treatment becomes more personalized.
112,129
DISCUSSION
The potential impact of cancer genomics is enormous. Ongoing
technologic advances and falling costs of genome sequencing are
increasing the rate at which cancer sequencing projects can be
completed. As a result, identication, validation, and functional
investigation of genetic aberrations in cancer are being pursued,
and the list of genes of interest is expanding continually. Driven by
the three pillars of cancer genomicstechnology, discovery, and
translationPCM is now within reach. However, before we are
able to translate the knowledge gained into clinical benet that
enhances patient care, key hurdles must be overcome. Although
bioinformatic analysis and stringent quality control have reduced
errors associated with sequencing and genotyping, the reliability
and accuracy of novel technologies remain potential problems.
From a discovery viewpoint, nding solutions to problems associ-
ated with multiple testing and data integration is crucial to make
reliable inferences fromgenomics data. Finally, although matching
treatments to novel biomarkers is the crux of PCM, key challenges
associated with tissue processing and tumor heterogeneity must be
recognized and addressed. Ultimately, prospective clinical valida-
tion is needed to conrm that PCM provides cost-effective benet
against our current standard approaches.
AUTHORS DISCLOSURES OF POTENTIAL CONFLICTS
OF INTEREST
Although all authors completed the disclosure declaration, the following
author(s) indicated a nancial or other interest that is relevant to the subject
matter under consideration in this article. Certain relationships marked
with a U are those for which no compensation was received; those
relationships marked with a C were compensated. For a detailed
description of the disclosure categories, or for more information about
ASCOs conict of interest policy, please refer to the Author Disclosure
Declaration and the Disclosures of Potential Conicts of Interest section in
Information for Contributors.
Employment or Leadership Position: None Consultant or Advisory
Role: Benjamin G. Neel, Kolltan Pharmaceuticals (C), Novartis (C)
Stock Ownership: Benjamin G. Neel, Kolltan Pharmaceuticals
Honoraria: None Research Funding: None Expert Testimony: None
Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Ben Tran, Janet E. Dancey, Nicole Onetto,
Thomas J. Hudson, Benjamin G. Neel, Lillian L. Siu
Financial support: Thomas J. Hudson, Benjamin G. Neel, Lillian L. Siu
Administrative support: Janet E. Dancey, Lillian L. Siu
Provision of study materials or patients: All authors
Collection and assembly of data: Ben Tran, Suzanne Kamel-Reid,
Andrew M.K. Brown, Tong Zhang, Patricia Shaw, Lillian L. Siu
Data analysis and interpretation: Ben Tran, Suzanne Kamel-Reid, John
D. McPherson, Philippe L. Bedard, Andrew M.K. Brown, Tong Zhang,
Patricia Shaw, Lincoln Stein, Benjamin G. Neel, Lillian L. Siu
Manuscript writing: All authors
Final approval of manuscript: All authors
Cancer Genomics
www.jco.org 2012 by American Society of Clinical Oncology 657
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
REFERENCES
1. National Cancer Institute: Dictionary of can-
cer terms: Personalizedmedicine. http://www.cancer
.gov/dictionary?CdrID561717
2. National Cancer Institute: Ofce of Cancer
Genomics. http://ocg.cancer.gov/
3. Sjo blom T, Jones S, Wood LD, et al: The
consensus coding sequences of human breast and
colorectal cancers. Science 314:268-274, 2006
4. Metzker ML: Sequencing technologies: The
next generation. Nat Rev Genet 11:31-46, 2009
5. Shendure J, Ji H: Next-generation DNA se-
quencing. Nat Biotechnol 26:1135-1145, 2009
6. International Human Genome Consortium:
Finishing the euchromatic sequence of the human
genome. Nature 431:931-945, 1992
7. Robison K: Application of second-generation
sequencing to cancer genomics. Brief Bioinform
11:524-534, 2010
8. Lin J, Li M: Molecular proling in the age of
cancer genomics. Exp Rev Mol Diagn 8:263-276,
2008
9. Ajay SS, Parker SC, Abaan HO, et al: Accu-
rate and comprehensive sequencing of personal
genomes. Genome Res 21:1498-1505, 2011
10. Zhao J, Grant SF: Advances in whole ge-
nome sequencing technology. Curr Pharm Biotech-
nol 12:293-305, 2011
11. Eid J, Fehr A, Gray J, et al: Real-time DNA
sequencing from single polymerase molecules. Sci-
ence 323:133-138, 2009
12. Rohde H, Qin J, Cui Y, et al: Open-source
genomic analysis of shiga-toxin-producing E. coli
O104:H4. N Engl J Med 365:718-724, 2011
13. Twyman RM, Primrose SB: Techniques pat-
ents for SNP genotyping. Pharmacogenomics 4:67-
79, 2003
14. Isler JA, Vesterqvist OE, Burczynski ME:
Analytical validation of genotyping assays in the
biomarker laboratory. Pharmacogenomics 8:353-
368, 2007
15. Brion M, Quintela I, Sobrino B, et al: New
technologies in the genetic approach to sudden
cardiac death in the young. Forensic Sci Int 203:15-
24, 2010
16. Tsuchihashi Z, Dracopoli N: Progress in high
throughput SNP genotyping methods. Biosystems
2:103-110, 2002
17. Pati N, Schowinsky V, Kokanovic O, et al: A
comparison between SNaPshot, pyrosequencing,
and biplex invader SNP genotyping methods: Accu-
racy, cost, and throughput. J Biochem Biophys
Methods 60:1-12, 2004
18. Koumi P, Green HE, Hartley S, et al: Evalua-
tion and validation of the ABI 3700, ABI 3100, and
the MegaBACE 1000 capillary array electrophoresis
instruments for use with short tandem repeat mic-
rosatellite typing in a forensic environment. Electro-
phoresis 25:2227-2241, 2004
19. Curtis C, Lynch AG, Dunning MJ, et al: The
pitfalls of platform comparison: DNA copy number
array technologies assessed. BMC Genomics 10:
588, 2009
20. Voidonikolas G, Kreml SS, Chen C, et al:
Basic principles and technologies for deciphering
the genetic map of cancer. World J Surg 33:615-
629, 2009
21. Teer JK, Mullikin JC: Exome sequencing:
The sweet spot before whole genomes. Hum Mol
Genet 19:145-151, 2010
22. Thomas RK, Baker AC, Debiasi RM, et al:
High-throughput oncogene mutation proling in hu-
man cancer. Nature Genet 39:347-351, 2007
23. Dias-Santagata D, Akhavanfard S, David SS,
et al: Rapid targeted mutational analysis of human
tumours: A clinical platform to guide personalized
cancer medicine. EMBO Mol Med 2:146-158, 2010
24. MacConaill LE, Campbell CD, Kehoe SM, et
al: Proling critical cancer gene mutations in clinical
tumor samples. PloS One 4:e7887, 2009
25. Sauter G, Lee J, Bartlett JM, et al: Guidelines
for human epidermal growth factor receptor 2 test-
ing: Biologic and methodologic considerations.
J Clin Oncol 27:1323-1333, 2009
26. Slamon DJ, Leyland-Jones B, Shak S, et al:
Use of chemotherapy plus a monoclonal antibody
against HER2 for metastatic breast cancer that
overexpresses HER2. N Engl J Med 344:783-792,
2001
27. Bang YJ, Van Cutsem E, Feyereislova A, et
al: Trastuzumab in combination with chemotherapy
versus chemotherapy alone for treatment of HER2-
positive advanced gastric or gastro-oesophageal
junction cancer (ToGA): A phase 3, open-label, ran-
domised controlled trial. Lancet 376:687-697, 2010
28. Davies JJ, Wilson IM, Lam WL: Array CGH
technologies and their applications to cancer ge-
nomes. Chromosome Res 13:237-248, 2005
29. Andrews J, Kennette W, Pilon J, et al: Multi-
platform whole-genome microarray analyses rene
the epigenetic signature of breast cancer metastasis
with gene expression and copy number. PloS One
5:e8665, 2010
30. Pop M, Salzberg SL: Bioinformatics chal-
lenges of new sequencing technology. Trends
Genet 24:142-149, 2008
31. Teufel A, Krupp M, Weinmann A, et al:
Current bioinformatics tools in genomic biomedical
research. Int J Mol Med 17:967-973, 2006
32. Saeys Y, Inza I, Larran aga P: A review of
feature selection techniques in bioinformatics.
Bioinformatics 23:2507-2517, 2007
33. Pandya GA, Holmes MH, Sunkara S, et al: A
bioinformatic lter for improved base-call accuracy
and polymorphism detection using the Affymetrix
GeneChip whole-genome resequencing platform.
Nucleic Acids Res 35:e148, 2007
34. Ding L, Ellis MJ, Li S, et al: Genome remod-
elling in a basal-like breast cancer metastasis and
xenograft. Nature 464:999-1005, 2010
35. Mardis ER, Ding L, Dooling DJ, et al:
Recurring mutations found by sequencing an
acute myeloid leukemia genome. N Engl J Med
361:1058-1066, 2009
36. Pleasance ED, Stephens PJ, OMeara S, et
al: A small-cell lung cancer genome with complex
signatures of tobacco exposure. Nature 463:184-
190, 2010
37. Pleasance ED, Cheetham RK, Stephens PJ,
et al: A comprehensive catalogue of somatic muta-
tions from a human cancer genome. Nature 463:
191-196, 2010
38. Cancer Genome Atlas Research Network:
Comprehensive genomic characterization denes
human glioblastoma genes and core pathways. Na-
ture 455:1061-1068, 2008
39. Parsons DW, Jones S, Zhang X, et al: An
integrated genomic analysis of human glioblastoma
multiforme. Science 321:1807-1812, 2008
40. Berger MF, Lawrence MS, Demichelis F, et
al: The genomic complexity of primary human pros-
tate cancer. Nature 470:214-220, 2011
41. Ley TJ, Mardis ER, Ding L, et al: DNA
sequencing of a cytogenetically normal acute my-
eloid leukaemia genome. Nature 456:66-72, 2008
42. Stratton MR, Campbell PJ, Futreal PA: The
cancer genome. Nature 458:719-724, 2009
43. International Cancer Genome Consortium:
International network of cancer genome projects.
Nature 464:993-998, 2010
44. Hirschhorn JN, Daly MJ: Genome-wide as-
sociation studies for common diseases and complex
traits. Nature Rev Genet 6:95-108, 2005
45. Cancer Genome Atlas Research Network:
Integrated genomic analyses of ovarian carcinoma.
Nature 474:609-615, 2011
46. Puente XS, Pinyol M, Quesada V, et al:
Whole-genome sequencing identies recurrent mu-
tations in chronic lymphocytic leukaemia. Nature
475:101-105, 2011
47. Jones S, Zhang X, Parsons DW, et al: Core
signaling pathways in human pancreatic cancers
revealed by global genomic analyses. Science 321:
1801-1806, 2008
48. Chapman MA, Lawrence MS, Keats JJ, et al:
Initial genome sequencing and analysis of multiple
myeloma. Nature 471:467-472, 2011
49. Totoki Y, Tatsuno K, Yamamoto S, et al:
High-resolution characterization of a hepatocellular
carcinoma genome. Nat Genet 43:464-469, 2011
50. Esteller M: Epigenetics in cancer. N Engl
J Med 358:1148-1159, 2008
51. Kim K, Zakharkin SO, Allison DB: Expecta-
tions, validity, and reality in gene expression prol-
ing. J Clin Epidemiol 63:950-959, 2010
52. Perou CM, Srlie T, Eisen MB, et al: Molec-
ular portraits of human breast tumours. Nature 406:
747-752, 2000
53. Vijver MJ van de, He YD, Veer LJ vant, et al:
A gene-expression signature as a predictor of sur-
vival in breast cancer. N Engl J Med 347:1999-2009,
2002
54. Paik S, Shak S, Tang G, et al: A multigene
assay to predict recurrence of tamoxifen-treated,
node-negative breast cancer. N Engl J Med 351:
2817-2826, 2004
55. Wang E, Panelli MC, Marincola FM: Gene
proling of immune responses against tumors. Cur
Opin Immunol 17:423-427, 2005
56. Pardoll DM: Spinning molecular immunology
into successful immunotherapy. Nature Rev Immu-
nol 2:227-238, 2002
57. Galon J, Costes A, Sanchez-Cabo F, et al:
Type, density, and location of immune cells within
human colorectal tumors predict clinical outcome.
Science 313:1960-1964, 2006
58. Bedognetti D, Wang E, Sertoli MR, et al:
Gene-expression proling in vaccine therapy and
immunotherapy for cancer. Exp Rev Vaccines 9:555-
565, 2010
59. Coppola D, Nebozhyn M, Khalil F, et al:
Unique ectopic lymph node-like structures present
in human primary colorectal carcinoma are identied
by immune gene array proling. Am J Path 179:37-
45, 2011
60. Hanash S, Taguchi A: The grand challenge to
decipher the cancer proteome. Nature Rev Cancer
10:652-660, 2010
61. Weinberg R: Point: Hypotheses rst. Nature
464:678, 2010
62. Heng HH: Cancer genome sequencing: The
challenges ahead. Bioessays 29:783-794, 2007
63. Ng SB, Turner EH, Robertson PD, et al:
Targeted capture and massively parallel sequencing
of 12 human exomes. Nature 461:272-276, 2009
Tran et al
658 2012 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
64. Maher B: Exome sequencing takes centre
stage in cancer proling. Nature 459:146-147, 2009
65. Cirulli ET, Singh A, Shianna KV, et al: Screen-
ing the human exome: A comparison of whole
genome and whole transcriptome sequencing. Ge-
nome Biol 11:R57, 2010
66. Diamandis EP, Hudson T, Kallioniemi O, et al:
Cancer genomes. Clin Chem 56:1660-1664, 2010
67. Strausberg RL, Simpson AJ: Whole-genome
cancer analysis as an approach to deeper under-
standing of tumour biology. Br J Cancer 102:243-
248, 2010
68. Ng PC, Levy S, Huang J, et al: Genetic
variation in an individual human exome. PLoS Genet
4:e1000160, 2008
69. Walter MJ, Graubert TA, Dipersio JF, et al:
Next-generation sequencing of cancer genomes:
Back to the future. Per Med 6:653, 2009
70. Bell DW: Our changing view of the genomic
landscape of cancer. J Path 220:231-243, 2010
71. Tran B, Kopetz S, Tie J, et al: Impact of BRAF
mutation and microsatellite instability on the pattern
of metastatic spread and prognosis in metastatic
colorectal cancer. Cancer [epub ahead of print on
March 31, 2011]
72. Mardis ER, Wilson RK: Cancer genome se-
quencing: A review. Hum Mol Genet 18:R163-R168,
2009
73. Scott KL, Kabbarah O, Liang MC, et al:
GOLPH3 modulates mTOR signalling and rapamycin
sensitivity in cancer. Nature 459:1085-1090, 2009
74. Stein LD: Integrating biological databases.
Nat Rev Genet 4:337-345, 2003
75. Kemmeren P, Holstege FC: Integrating func-
tional genomics data. Biochem Soc Trans 31:1484-
1487, 2003
76. Manly KF, Nettleton D, Hwang JT: Genom-
ics, prior probability, and statistical tests of multiple
hypotheses. Genome Res 14:997-1001, 2004
77. Nadon R, Shoemaker J: Statistical issues
with microarrays: Processing and analysis. Trends
Genet 18:265-271, 2002
78. Martin LJ, Woo JG, Avery CL, et al: Multiple
testing in the genomics era: Findings from Genetic
Analysis Workshop 15, Group 15. Genet Epidemiol
31:124-131, 2007
79. Hopkins AL, Groom CR: The druggable ge-
nome. Nat Rev Drug Discov 1:727-730, 2002
80. Geyer CE, Forster J, Lindquist D, et al:
Lapatinib plus capecitabine for HER2-positive ad-
vanced breast cancer. N Engl J Med 355:2733-2743,
2006
81. Mok TS, Wu YL, Thongprasert S, et al:
Getinib or carboplatin-paclitaxel in pulmonary ade-
nocarcinoma. N Engl J Med 361:947-957, 2011
82. Kim E, Hirsh V, Mok T, et al: Getinib versus
docetaxel in previously treated non-small-cell lung
cancer (INTEREST): A randomised phase III trial.
Lancet 372:1809-1818, 2008
83. Chapman PB, Hauschild A, Robert C, et al:
Improved survival with vemurafenib in melanoma
with BRAF V600E mutation. N Engl J Med 364:
2507-2516, 2011
84. Coifer B, Lepage E, Briere J, et al: CHOP
chemotherapy plus rituximab compared with CHOP
alone in elderly patients with diffuse large-B-cell
lymphoma. N Engl J Med 346:235-242, 2002
85. Hodi FS, ODay SJ, McDermott DF, et al:
Improved survival with ipilimumab in patients with
metastatic melanoma. N Engl J Med 363:711-723,
2010
86. Kantoff PW, Higano CS, Shore ND, et al:
Sipuleucel-T immunotherapy for castration-resistant
prostate cancer. N Engl J Med 363:411-422, 2010
87. Gonzalez-Angulo AM, Hennessy BT, Mills
GB: Future of personalized medicine in oncology: A
systems biology approach. J Clin Oncol 28:2777-
2783, 2010
88. Macconaill LE, Garraway LA: Clinical implica-
tions of the cancer genome. J Clin Oncol 28:5219-
5228, 2010
89. Dancey JE, Dobbin KK, Groshen S, et al:
Guidelines for the development and incorporation of
biomarker studies in early clinical trials of novel
agents. Clin Cancer Res 16:1745-1755, 2010
90. Doroshow JH: Selecting systemic cancer
therapy one patient at a time: Is there a role for
molecular proling of individual patients with ad-
vanced solid tumors? J Clin Oncol 28:4869-4871,
2010
91. Von Hoff DD, Stephenson JJ Jr, Rosen P, et
al: Pilot study using molecular proling of patients
tumors to nd potential targets and select treat-
ments for their refractory cancers. J Clin Oncol
28:4877-4883, 2010
92. Tsimberidou AM, Iskander NG, Hong DS, et
al: Personalized medicine in a phase I clinical trials
program: The M. D. Anderson Cancer Center initia-
tive. J Clin Oncol 29:18s, 2011 (suppl; abstr
CRC2500)
93. Kim ES, Herbst RS, Wistuba II, et al: The
BATTLE Trial: Personalizing Therapy for Lung Can-
cer. Cancer Discov 1:44-53, 2011
94. Ross CJ, Katzov-Eckert H, Dube MP, et al:
Genetic variants in TPMT and COMT are associated
with hearing loss in children receiving cisplatin chem-
otherapy. Nature Genet 41:1345-1349, 2009
95. de Haas EC, Zwart N, Meijer C, et al: Varia-
tion in bleomycin hydrolase gene is associated with
reduced survival after chemotherapy for testicular
germ cell cancer. J Clin Oncol 26:1817-1823, 2008
96. ODwyer PJ, Catalano RB: Uridine diphos-
phate glucuronosyltransferase (UGT) 1A1 and irino-
tecan: Practical pharmacogenomics arrives in cancer
therapy. J Clin Oncol 24:4534-4538, 2006
97. Tran B, Dancey JE, Kamel-Reid S, et al:
Generation of a panel of druggable mutation cancer
genes for molecular proling in a feasibility study of
somatic mutation genotyping and targeted exome
sequencing: OICR-PMH study. Presented at the
European Organisation for Research and Treatment
of CancerNational Cancer InstituteAmerican As-
sociation for Cancer Research Annual Meeting on
Molecular Markers in Cancer, Brussels, Belgium,
October 27-29, 2011
98. Vakiani E, Janakiraman M, Shen R, et al:
Comparative genomic analysis of primary versus
metastasis in colorectal carcinomas. J Clin Oncol
29:15s, 2011 (suppl; abstr 10500)
99. Tie J, Gibbs P, Lipton L, et al: Optimizing
targeted therapeutic development: Analysis of
a colorectal cancer patient population with the
BRAFV600E mutation. Int J Cancer 128:2075-
2084, 2010
100. Amir E, Miller N, Geddie W, et al: Prospec-
tive study evaluating the impact of tissue conrma-
tion of metastatic disease in patients with breast
cancer. J Clin Oncol 30:587-592, 2012
101. Janes CH, Lindor KD: Outcome of patients
hospitalized for complications after outpatient liver
biopsy. Ann Intern Med 118:96-98, 1993
102. Sawyers CL: The cancer biomarker problem.
Nature 452:548-552, 2008
103. Li J, Wang K, Jensen TD, et al: Tumor
heterogeneity in neoplasms of breast, colon, and
skin. BMC Res Notes 3:321, 2010
104. Kopetz S, Desai J, Chan E, et al: PLX4032 in
metastatic colorectal cancer patients with mutant
BRAF tumors. J Clin Oncol 28:15s, 2010 (suppl;
abstr 3534)
105. Leiva IM, Emmert-Buck MR, Gillespie JW:
Handling of clinical tissue specimens for molecular
proling studies. Curr Issues Mol Biol 5:27-35, 2003
106. Klimecki WT, Futscher BW, Dalton WS: Ef-
fects of ethanol and paraformaldehyde on RNA yield
and quality. BioTechniques 16:1021-1023, 1994
107. Ben-Ezra J, Johnson DA, Rossi J, et al: Effect
of xation on the amplication of nucleic acids from
parafn-embedded material by the polymerase
chain reaction. J Histochem Cytochem 39:351-354,
1991
108. Coura R, Prolla JC, Meurer L, et al: An
alternative protocol for DNA extraction from forma-
lin xed and parafn wax embedded tissue. J Clin
Path 58:894-895, 2005
109. Bonner RF: Laser capture microdissection:
Molecular analysis of tissue. Science 278:1481-
1483, 1997
110. Hunt JL, Finkelstein SD: Microdissection
techniques for molecular testing in surgical pathol-
ogy. Arch Path Lab Med 128:1372-1378, 2004
111. Cardoso J, Molenaar L, de Menezes RX, et
al: Genomic proling by DNA amplication of laser
capture microdissected tissues and array CGH. Nu-
cleic Acids Res 32:e146, 2004
112. Ioannidis JP: Is molecular proling ready for
use in clinical decision making? Oncologist 12:301-
311, 2007
113. Brazma A, Hingamp P, Quackenbush J, et al:
Minimum information about a microarray experi-
ment (MIAME): Toward standards for microarray
data. Nat Genet 29:365-371, 2001
114. Ardekani AM, Petricoin EF, Hackett JL: Mo-
lecular diagnostics: An FDA perspective. Expert Rev
Mol Diagn 3:129-140, 2003
115. US Food and Drug Administration: Device
advice: Investigational deviceexemption(IDE). http://
www.fda.gov/MedicalDevices/DeviceRegulationand
Guidance/HowtoMarketYourDevice/Investigational
DeviceExemptionIDE/default.htm
116. Harismendy O, Ng PC, Strausberg RL, et al:
Evaluation of next generation sequencing platforms
for population targeted sequencing studies. Ge-
nome Biol 10:R32, 2009
117. Bhagwat NR, Roginskaya VY, Acquafondata
MB, et al: Immunodetection of DNA repair endonu-
clease ERCC1-XPF in human tissue. Cancer Res
69:6831-6838, 2009
118. Olaussen KA, Fouret P, Kroemer G: ERCC1-
specic immunostaining in non-small-cell lung can-
cer. N Engl J Med 357:1559-1561, 2007
119. Wolff AC, Hammond ME, Schwartz JN, et al:
American Society of Clinical Oncology/College of
American Pathologists guideline recommendations
for human epidermal growth factor receptor 2 test-
ing in breast cancer. J Clin Oncol 25:118-145, 2007
120. My Cancer Genome: Genetically informed
cancer medicine. http://www.mycancergenome.org
121. McGuire AL, Cauleld T, Cho MK: Research
ethics and the challenge of whole-genome sequenc-
ing. Nat Rev Genet 9:152-156, 2008
122. Fabsitz RR, McGuire A, Sharp RR, et al:
Ethical and practical guidelines for reporting genetic
research results to study participants: Updated
guidelines from a National Heart, Lung, and Blood
Institute Working Group. Circ Cardiovasc Genet
3:574-580, 2010
123. Bookman EB, Langehorne AA, Eckfeldt JH,
et al: Reporting genetic results in research studies:
Summary and recommendations of an NHLBI work-
ing group. Am J Med Genet 140:1033-1040, 2006
Cancer Genomics
www.jco.org 2012 by American Society of Clinical Oncology 659
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
124. Amado RG, Wolf M, Peeters M, et al: Wild-
type KRAS is required for panitumumab efcacy in
patients with metastatic colorectal cancer. J Clin
Oncol 26:1626-1634, 2008
125. Karapetis CS, Khambata-Ford S, Jonker DJ, et al:
K-ras mutations and benet fromcetuximab in advanced
colorectal cancer. N Engl J Med 359:1757-1765, 2008
126. Ortiz TM, Joshi VA, Heon S, et al: The
introduction of systematic genomic testing for pa-
tients with non-small cell lung cancer (NSCLC) at
Dana-Farber Cancer Institute (DFCI). J Clin Oncol
29:15s, 2011 (suppl; abstr 7517)
127. Sequist LV, Heist RS, Shaw AT, et al:
SNaPshot genotyping of non-small cell lung cancers
(NSCLC) in clinical practice. J Clin Oncol 29:15s, 2011
(suppl; abstr 7518)
128. Bild AH, Potti A, Nevins JR: Linking onco-
genic pathways with therapeutic opportunities. Na-
ture Rev Cancer 6:735-741, 2006
129. Harris TJ, McCormick F: The molecular pathol-
ogy of cancer. Nat Rev Clin Oncol 7:251-265, 2010
Glossary Terms
Actionable aberrations: Any aberration (germline or so-
matic) that may impact cancer management through diagnostic,
prognostic, and/or predictive implications.
Driver mutation: Driver mutations are those that are caus-
ally implicated in oncogenesis or tumor survival. Such mutations
have been positively selected during carcinogenesis and often
show a recurrent pattern within or across tumor types. This is in
contrast with passenger events, which arise from the background
mutation rate and do not contribute to oncogenesis.
Druggable aberrations: Any actionable aberration that can
be targeted by novel therapeutics and thereby change the natural
history of the disease.
Exome: Part of the genome formed by genes that code for pro-
teins and other functional gene products (known as exons).
Genome: The complete set of genetic material.
Genotyping: The process used for obtaining the genotype of a
given gene. From a somatic point of view (within a tumor), geno-
typing can be used to identify a predetermined genetic aberra-
tion, such as somatic mutations, copy number variations, gene
expression changes, and/or DNA methylation. Genotyping iden-
ties only predetermined aberrations, with all other aberrations
being effectively invisible.
Germline mutation: An inherited variation in the lineage of germ
cells. Germline mutations can be passed on to offspring.
Passenger mutation: A somatic mutation present in cancer with
no bearing on tumor biology.
Sequencing: A laboratory process that determines the nucleotide
sequence of DNA (can involve the whole genome or whole exome or be
targeted to as little as one coding sequence). Unlike somatic mutation
genotyping, sequencing can detect previously unknown somatic
mutations.
SNP (single nucleotide polymorphism): Genetic polymor-
phisms are natural variations in the genomic DNA sequence present in
greater than 1% of the population, with SNP representing DNA varia-
tions in a single nucleotide. SNPs are being widely used to better under-
stand disease processes, thereby paving the way for genetic-based
diagnostics and therapeutics.
Somatic mutation: A change in the genotype of a cancer cell. This
is distinguished from a germline mutation, which is a change in the ge-
notype of all the normal cells in a patients body. Germline mutations
may be passed to offspring, but somatic mutations may not.
Tran et al
660 2012 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Information downloaded from jco.ascopubs.org and provided by at ASCO on March 6, 2014 from 158.232.241.130
Copyright 2012 American Society of Clinical Oncology. All rights reserved.
CORRECTIONS
Author Corrections
The October 10, 2005 editorial by Workman and Johnston, en-
titled, Genomic Proling of Cancer: What Next? (J Clin Oncol
23:7253-7256, 2005) containedanerror.
In the Authors Disclosures of Potential Conicts of Inter-
est section, Almac Diagnostics should have been disclosed for
Patrick G. Johnston in the following two categories: Employ-
ment or Leadership Position (Compensated) and Stock
Ownership.
The authors apologize for the mistake.
DOI: 10.1200/JCO.2012.42.7823; published April 1, 2012
The February 1, 2012 editorial by Paskett, entitled, Cancer
Heath Disparities: Moving From Why They Occur to How
They Can Be Prevented (J Clin Oncol 30:354-356, 2012), con-
tained an error.
The Title should have read:
Cancer Health Disparities: Moving From Why They Occur to
How They Can Be Prevented.
The online version has been corrected in departure from
the print.
The author apologizes for the mistake.
DOI: 10.1200/JCO.2012.42.6379; published April 1, 2012
Journal Corrections
The February 20, 2012 editorial by Pster, entitled, Off-Label
Use of Oncology Drugs: The Need for More Data and Then Some
(J ClinOncol 30:584-586, 2012), containedanerror.
The editorial was linked to an accompanying article on
page 647 of the issue, whereas it should have been the article on
page 661, as follows:
Mullins CD, Montgomery R, Abernethy AP, et al: Recom-
mendations for Clinical Trials of Off-Label Drugs Used to Treat
Advanced-Stage Cancer. J Clin Oncol 30:661-666, 2012.
Journal of Clinical Oncology apologizes for the mistake.
DOI: 10.1200/JCO.2012.42.7831; published April 1, 2012
The February 20, 2012 special article by Tran et al, entitled,
Cancer Genomics: Technology, Discovery, and Translation
(J Clin Oncol 30:647-660, 2012), contained an error.
The article was erroneously linked to an accompanying
editorial on page 584 of the issue and should not have been
linked to any editorial.
Journal of Clinical Oncology apologizes for the mistake.
DOI: 10.1200/JCO.2012.42.7849; published April 1, 2012
2012 by American Society of Clinical Oncology 1149
You might also like
- Targeted Cancer Imaging: Design and Synthesis of Nanoplatforms based on Tumor BiologyFrom EverandTargeted Cancer Imaging: Design and Synthesis of Nanoplatforms based on Tumor BiologyNo ratings yet
- Functional Genomics in HCC 2005Document6 pagesFunctional Genomics in HCC 2005johnyap11No ratings yet
- Pre-Cancer Diagnosis Via Gene Mutations Applied Ensemble AlgorithmsDocument8 pagesPre-Cancer Diagnosis Via Gene Mutations Applied Ensemble AlgorithmsAishwarya ANo ratings yet
- HPV and Cervical Cancer Research PaperDocument8 pagesHPV and Cervical Cancer Research Paperafmcuafnh100% (1)
- Nanotechnology and CancerDocument16 pagesNanotechnology and CancerMarcos LoredoNo ratings yet
- TC Ga BrochureDocument4 pagesTC Ga BrochureroelsmajorNo ratings yet
- Articulo CientificoDocument9 pagesArticulo CientificoHeber Andre Calizaya SánchezNo ratings yet
- Breast Cancer and Biomedical Informatics: The Prognochip ProjectDocument6 pagesBreast Cancer and Biomedical Informatics: The Prognochip ProjectRuanita VeigaNo ratings yet
- 1 s2.0 S0092867413002882 MainDocument21 pages1 s2.0 S0092867413002882 MainDavidf VillabonaNo ratings yet
- 2008 Annurev - Med. Nanotechnology and CancerDocument18 pages2008 Annurev - Med. Nanotechnology and CancerDenise Gonzalez GomezNo ratings yet
- Assignment Applied Genomics and Proteomics: Mtech (Biotechnology) 3 SEM 2014-2016Document14 pagesAssignment Applied Genomics and Proteomics: Mtech (Biotechnology) 3 SEM 2014-2016rawatpooran05No ratings yet
- Roylance 1997Document8 pagesRoylance 1997barti koksNo ratings yet
- Hepatocellular Carcinoma: Clinical Frontiers and PerspectivesDocument13 pagesHepatocellular Carcinoma: Clinical Frontiers and PerspectivesMisnariahIdrusNo ratings yet
- Cancer 1Document16 pagesCancer 1KlitosNo ratings yet
- Chapter 1 - The Cancer GenomeDocument35 pagesChapter 1 - The Cancer GenomeCynthia LopesNo ratings yet
- Mecanisme EpigeneticeDocument13 pagesMecanisme EpigeneticeCelatuchiacNo ratings yet
- Bioinformatics Application: Next-Generation SequencingDocument3 pagesBioinformatics Application: Next-Generation SequencingThiện NguyễnNo ratings yet
- Creatine Phosphokinase Levels in Oral Cancer Patients: Issn 0974-3618 (Print) 0974-360X (Online)Document4 pagesCreatine Phosphokinase Levels in Oral Cancer Patients: Issn 0974-3618 (Print) 0974-360X (Online)Deepak KumarNo ratings yet
- Cancer Biomarkers: Easier Said Than Done: Kenneth P.H. PritzkerDocument4 pagesCancer Biomarkers: Easier Said Than Done: Kenneth P.H. Pritzkerdumboo21No ratings yet
- 2015 The Cancer Genome AtlasTCGADocument11 pages2015 The Cancer Genome AtlasTCGAJoao da Costa100% (1)
- Research Paper On Cancer DetectionDocument8 pagesResearch Paper On Cancer Detectionxsykcbikf100% (1)
- Cancer Genome ProjectDocument6 pagesCancer Genome ProjectDarshil PatelNo ratings yet
- Cancer Total BothDocument33 pagesCancer Total BothUsman AshrafNo ratings yet
- Cancers 13 02067Document15 pagesCancers 13 02067Flaviu Ionuț FaurNo ratings yet
- 655506v1 Full PDFDocument36 pages655506v1 Full PDFgarrobosNo ratings yet
- NGS and Mutational Profile Analysis of Non-Small-Cell Lung Carcinoma (NSCLC)Document7 pagesNGS and Mutational Profile Analysis of Non-Small-Cell Lung Carcinoma (NSCLC)IJRASETPublicationsNo ratings yet
- JPCS 704 1 012011Document12 pagesJPCS 704 1 012011ferNo ratings yet
- Plagiarism1 - ReportDocument8 pagesPlagiarism1 - ReportDeepak GourNo ratings yet
- Genes 12 01539 v2Document14 pagesGenes 12 01539 v2killua0707No ratings yet
- Genetics of Cancer and Its Recent ProgressDocument8 pagesGenetics of Cancer and Its Recent ProgressAaron OsorioNo ratings yet
- Biomedical Nanotechnology For CancerDocument29 pagesBiomedical Nanotechnology For CancervictoriaNo ratings yet
- 2019 Article 858Document13 pages2019 Article 858selcukorkmazNo ratings yet
- Cancer Gene Detection & DiagnosisDocument7 pagesCancer Gene Detection & DiagnosisIJRASETPublicationsNo ratings yet
- Biomarkers For The Lung Cancer Diagnosis and Their Advances in ProteomicsDocument11 pagesBiomarkers For The Lung Cancer Diagnosis and Their Advances in ProteomicsAndi Harmawati NNo ratings yet
- Liquid BiopsyDocument2 pagesLiquid BiopsySalman MajidNo ratings yet
- 723 - Standardization of EUS Imaging and Reporting in High-Risk Individuals of Pancreatic AdenocarcinomaDocument17 pages723 - Standardization of EUS Imaging and Reporting in High-Risk Individuals of Pancreatic AdenocarcinomaJhon Jaime CarvajalNo ratings yet
- Explore Rare Cancer Medicine MutationsDocument6 pagesExplore Rare Cancer Medicine MutationsMikel AngelNo ratings yet
- Biomolecular Detection and Quantification: SciencedirectDocument23 pagesBiomolecular Detection and Quantification: SciencedirectSYED MAAZ TARIQNo ratings yet
- Addressing The Challenges of High Throughput Cancer Tissue Proteomics For Clinical Application - ProCanDocument5 pagesAddressing The Challenges of High Throughput Cancer Tissue Proteomics For Clinical Application - ProCanFarmaceutico RaulNo ratings yet
- Church 2015Document1 pageChurch 2015TrabelsiNo ratings yet
- Hematolrep 03 E2 v2Document3 pagesHematolrep 03 E2 v2772450336No ratings yet
- Research Paper Lung CancerDocument7 pagesResearch Paper Lung Cancerjvfmdjrif100% (1)
- Literature Review of Cervical CancerDocument6 pagesLiterature Review of Cervical Cancerea7e9pm9100% (1)
- Research Paper On Cancer GeneticsDocument7 pagesResearch Paper On Cancer Geneticsrtggklrif100% (1)
- 2023-JTO-Genetic Intratumor Heterogeneity Remodels The Immune Microenvironment and Induces Immune Evasion in Brain Metastasis of Lung CancerDocument21 pages2023-JTO-Genetic Intratumor Heterogeneity Remodels The Immune Microenvironment and Induces Immune Evasion in Brain Metastasis of Lung Cancerzhe zhNo ratings yet
- Development of Prognostic Signatures For Intermediate Risk Papillary Thyroid CancerDocument12 pagesDevelopment of Prognostic Signatures For Intermediate Risk Papillary Thyroid Cancernfp.panjaitanNo ratings yet
- Schwarze 19 Cost Genom SeqDocument10 pagesSchwarze 19 Cost Genom Seqjose vasquezNo ratings yet
- Research Paper Colorectal CancerDocument4 pagesResearch Paper Colorectal Cancerxactrjwgf100% (1)
- MainDocument8 pagesMainIoana CucuNo ratings yet
- Jurnal 1Document11 pagesJurnal 1Dyahsekarayupudak wangiNo ratings yet
- Abeloff Clinical Oncology 2020 (Part 1)Document22 pagesAbeloff Clinical Oncology 2020 (Part 1)Emiliana LarionesiNo ratings yet
- ESMO Recommendations For NGSDocument15 pagesESMO Recommendations For NGSsagarkarvandeNo ratings yet
- Brock Et Al Liquid Biopsy 2015Document11 pagesBrock Et Al Liquid Biopsy 2015Jean BiverNo ratings yet
- JurnalDocument11 pagesJurnalPuput Indah PratiwiNo ratings yet
- Notocias Sobre OncogenesDocument1 pageNotocias Sobre Oncogenesalbertohz1No ratings yet
- Thesis On Breast Cancer DetectionDocument4 pagesThesis On Breast Cancer Detectionafkodkedr100% (2)
- 10b. Diagnosis Journal Review - Colorectal Cancer Screening NEJMDocument11 pages10b. Diagnosis Journal Review - Colorectal Cancer Screening NEJMPPDSNeurologiAgustus 2021No ratings yet
- The Changing Role of Pathology in Breast Cancer Diagnosis and TreatmentDocument17 pagesThe Changing Role of Pathology in Breast Cancer Diagnosis and TreatmentFadli ArchieNo ratings yet
- ch210005954p PDFDocument5 pagesch210005954p PDFJanNo ratings yet
- M2 Economic LandscapeDocument18 pagesM2 Economic LandscapePrincess SilenceNo ratings yet
- 18PGHR11 - MDI - Aditya JainDocument4 pages18PGHR11 - MDI - Aditya JainSamanway BhowmikNo ratings yet
- Building and Other Construction Workers Act 1996Document151 pagesBuilding and Other Construction Workers Act 1996Rajesh KodavatiNo ratings yet
- DC Servo MotorDocument6 pagesDC Servo MotortaindiNo ratings yet
- XgxyDocument22 pagesXgxyLïkïth RäjNo ratings yet
- Extent of The Use of Instructional Materials in The Effective Teaching and Learning of Home Home EconomicsDocument47 pagesExtent of The Use of Instructional Materials in The Effective Teaching and Learning of Home Home Economicschukwu solomon75% (4)
- 450i User ManualDocument54 pages450i User ManualThượng Lê Văn0% (2)
- Experiment On Heat Transfer Through Fins Having Different NotchesDocument4 pagesExperiment On Heat Transfer Through Fins Having Different NotcheskrantiNo ratings yet
- Properties of Moist AirDocument11 pagesProperties of Moist AirKarthik HarithNo ratings yet
- Viceversa Tarot PDF 5Document1 pageViceversa Tarot PDF 5Kimberly Hill100% (1)
- Agricultural Economics 1916Document932 pagesAgricultural Economics 1916OceanNo ratings yet
- 4th Sem Electrical AliiedDocument1 page4th Sem Electrical AliiedSam ChavanNo ratings yet
- 23 Things You Should Know About Excel Pivot Tables - Exceljet PDFDocument21 pages23 Things You Should Know About Excel Pivot Tables - Exceljet PDFRishavKrishna0% (1)
- Newsletter 289Document10 pagesNewsletter 289Henry CitizenNo ratings yet
- Marine Lifting and Lashing HandbookDocument96 pagesMarine Lifting and Lashing HandbookAmrit Raja100% (1)
- Professional Regula/on Commission: Clarita C. Maaño, M.DDocument31 pagesProfessional Regula/on Commission: Clarita C. Maaño, M.Dmiguel triggartNo ratings yet
- Reflections On Free MarketDocument394 pagesReflections On Free MarketGRK MurtyNo ratings yet
- Web Technology PDFDocument3 pagesWeb Technology PDFRahul Sachdeva100% (1)
- RYA-MCA Coastal Skipper-Yachtmaster Offshore Shorebased 2008 AnswersDocument28 pagesRYA-MCA Coastal Skipper-Yachtmaster Offshore Shorebased 2008 AnswersSerban Sebe100% (4)
- HandloomDocument4 pagesHandloomRahulNo ratings yet
- Labstan 1Document2 pagesLabstan 1Samuel WalshNo ratings yet
- 004-PA-16 Technosheet ICP2 LRDocument2 pages004-PA-16 Technosheet ICP2 LRHossam Mostafa100% (1)
- Blade Torrent 110 FPV BNF Basic Sales TrainingDocument4 pagesBlade Torrent 110 FPV BNF Basic Sales TrainingMarcio PisiNo ratings yet
- NOP PortalDocument87 pagesNOP PortalCarlos RicoNo ratings yet
- Profile On Sheep and Goat FarmDocument14 pagesProfile On Sheep and Goat FarmFikirie MogesNo ratings yet
- General Financial RulesDocument9 pagesGeneral Financial RulesmskNo ratings yet
- 4109 CPC For ExamDocument380 pages4109 CPC For ExamMMM-2012No ratings yet
- SILABO 29-MT247-Sensors-and-Signal-ConditioningDocument2 pagesSILABO 29-MT247-Sensors-and-Signal-ConditioningDiego CastilloNo ratings yet
- Supergrowth PDFDocument9 pagesSupergrowth PDFXavier Alexen AseronNo ratings yet
- Hayashi Q Econometica 82Document16 pagesHayashi Q Econometica 82Franco VenesiaNo ratings yet