Professional Documents
Culture Documents
Hea DB (Ni) 9904supplement1
Uploaded by
Ver Bautista0 ratings0% found this document useful (0 votes)
56 views28 pagesThe Medical Devices Agency helps safeguard public health by working with users, manufacturers and lawmakers. The key aim of the Northern Ireland adverse incident Centre (NIAIC) is to record and investigate reported adverse incidents. NIAIC also disseminates safety information in northern ireland, including information provided by MDA.
Original Description:
Original Title
Hea Db(Ni)9904supplement1
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe Medical Devices Agency helps safeguard public health by working with users, manufacturers and lawmakers. The key aim of the Northern Ireland adverse incident Centre (NIAIC) is to record and investigate reported adverse incidents. NIAIC also disseminates safety information in northern ireland, including information provided by MDA.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
56 views28 pagesHea DB (Ni) 9904supplement1
Uploaded by
Ver BautistaThe Medical Devices Agency helps safeguard public health by working with users, manufacturers and lawmakers. The key aim of the Northern Ireland adverse incident Centre (NIAIC) is to record and investigate reported adverse incidents. NIAIC also disseminates safety information in northern ireland, including information provided by MDA.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 28
Checks and
tests for newly
delivered medical
devices.
DB 9904 (NI) SUPPLEMENT 1
MARCH 2001
D
E
V
I
C
E
Supplement to Medical device and equipment management
for hospital and community-based organisations DB 9904 (NI)
BULLETIN
(Northern Ireland Version)
An Executive Agency of the Department of
Health, Social Services and Public Safety
isneacht Feidhmeannach don Roinn Slinte,
Serbhs Sisialta agus Sbhilteacht Phoibl
The Medical Devices Agency helps safeguard public health by working with users, manufacturers and
lawmakers to ensure that medical devices meet appropriate standards of safety, quality and performance
and that they comply with the relevant Directives of the European Union.
Our primary responsibility is to ensure that medical devices achieve their fullest potential to help
healthcare professionals give patients and other users the high standard of care they have a right to
expect.
The Medical Devices Agency is an Executive Agency of the Department of Health
The key aim of the Northern Ireland Adverse Incident Centre (NIAIC), part of Health Estates, is to
record and investigate reported adverse incidents involving Medical Devices and equipment used in
Health and Personal Social Services in Northern Ireland and to issue warning notices and guidance to
help prevent recurrence and avert patient or user injury. NIAIC has direct links with MDA who co-
ordinate across the adverse incident centres in England, Scotland, Wales and Northern Ireland. NIAIC
also disseminates safety information in Northern Ireland, including information provided by MDA.
Health Estates is an Executive Agency of the Department of Health, Social Services and Public Safety.
1
CONTENTS
EXECUTIVE SUMMARY..............................................................................3
1 OBJECTIVES.............................................................................................4
1.1 Scope...............................................................................................4
1.2 Introduction.....................................................................................4
2 CHOOSING SUITABLE CHECKS AND TESTS FOR A
PARTICULAR PRODUCT ........................................................................5
2.1 Broad guidelines .............................................................................5
2.2 Building up suitable tests from modules ........................................6
2.3 Training and knowledge which testers need...................................8
2.4 Efficient and record keeping...........................................................8
3 LEGAL REQUIREMENTS FOR ELETRICAL
SAFETY TESTING..................................................................................10
4 SPECIAL CASES.....................................................................................10
4.1 Devices which require commissioning.........................................10
4.2 Devices which might need a local certificate of safety................11
4.3 Devices loaned by manufacturers.................................................13
5 FORMS ....................................................................................................14
5.1 Draft form for bulk-packed products............................................14
5.2 Draft modules for mechanical/electrical devices..........................14
Module A Paperwork....................................................................14
Module B Visual Inspection .........................................................15
Module C Functional check..........................................................15
Module D Electrical safety (basic) ...............................................15
Module E Electrical safety for patient connected devices ...........16
Module F Calibration and measurement ......................................16
ANNEX 1 BACKGROUND - delivery checks .............................................18
ANNEX 2 BACKGROUND - pre-use tests ..................................................19
Acknowledgments
We are grateful to Charing Cross Hospital Department of Clinical Engineering
for their contribution to Section 4.2.
2
3
EXECUTIVE SUMMARY
This guidance document:
replaces HEI 95 Code of practice for acceptance testing of medical
electrical equipment, which is now withdrawn, and extends the
scope of pre-first-use checks and tests to non-electrical medical
devices;
replaces HEI 140 part II Code of practice for acceptance testing of
electrically operated hospital laboratory equipment for in vitro
diagnostic medical devices, pending further guidance in this area;
is designed to minimise the risks associated with using a product
for the first time;
is a supplement to DB9904 (NI) Medical device and equipment
management for hospital and community-based organisations.
User organisations whose procedures require implementation of document
updates should insert it in their DB9904 (NI) folder. However the guidance
is designed to be self-contained, and this supplement can be used as a
stand-alone document.
1. OBJECTIVES
We present a straightforward approach to choosing appropriate pre-first use
checks and tests for most newly-delivered products (see Section 2).
However two exceptional product groups need special treatment:
large, complex products which need installation and commissioning
(see Section 4.1).
products which may need a local certificate of safety - for example
products not manufactured under the Medical Devices Regulations or
supplied second-hand (see Section 4.2).
A risk assessment is needed to ensure that tests and checks are appropriate
for a particular product. Section 2 provides a simple rule-based risk
assessment which leads directly to appropriate lists of checks and tests for
the majority of products. The two exceptional groups involve user
organisations in a local risk assessment to determine an appropriate
procedure.
Chapter 5 of DB9904 (NI): When a new device is delivered is also
relevant. This supplement replaces and extends HEI 95 (Code of practice
for acceptance testing of medical electrical equipment), which is now
withdrawn.
User organisations should check the safety and functionality of newly-
delivered medical devices.
Aims for all devices include:
checking that the correct product, complete with manuals and
accessories, has been supplied;
providing assurance that product items have been delivered in good
condition and (where relevant) in working order;
ensuring that risks associated with using a particular model for the
first time have been minimised.
Additionally, for re-usable devices:
recording the device on a database, so that appropriate maintenance can
be initiated and, in the event of an adverse incident when a new device
is first used, evidence of good practice can be produced.
complying with safety legislation.
These aims are relevant to all medical devices - not just electrically
powered devices. As well as pre-use checks and tests, a procedure for
managing new devices should identify:
any training needs;
appropriate planned preventative maintenance;
technical support needs of users
1
Medical Devices Regulations 1994-SI 1994/3017, see DB9904 (NI) Appendix A1 p. vi. All products covered here are
medical devices under the definition in Article 1 of the regulations intended for the diagnosis, prevention, monitoring,
treatment or alleviation of disease...injury or handicap. Most but not all are therefore subject to the MDR.
4
1.1 Scope
1.2 Introduction
Quality, suitability and conformity to standards must be addressed before
purchase (DB9904 (NI) Chapter 3). There is no sense in buying something and
then deciding that it is not acceptable. The pre-use checks suggested here are the
intended to minimise risks associated with using a newly delivered device, and
not to provide a belated critique of purchasing decisions.
Many of the tests specified in standards are type tests which pose a challenge to
the device, and should only be carried out by the manufacturer or a test house.
Product items subjected to types tests are never put into service, in case the test
has caused some damage. Type tests must never be used as pre-use tests.
2. CHOOSING SUITABLE CHECKS AND
TESTS FOR A PARTICULAR PRODUCT
This section applies to products which are:
brand new;
CE-marked under the MDR (see DB9904 (NI) Section A1.4
CE-marking for purchasers).
Table 1 distinguishes between bulk-pack products, for which there is a single list
of checks (5.1), and products delivered as single items, for which a risk matrix
(Table 2) gives guidance on which of the six modules in section 5.2 are needed.
Every protocol should include checks that:
the delivery is complete;
the product is exactly what was ordered;
there has been no damage in transit.
Category Examples Key issues Draft form
Sterile and non-sterile medical gloves, stock rotation/use Section 5.1
bulk products - checks tongue, by dates
must focus on bulk pack. depressors, tracing lots if there
catheters, is a recall
syringes, circulating instructions
dressings, and safety information
when necessary
faulty packaging
Individual non-active walking frame device is safe to use Assemble from
items modules (see
active infusion pump device functions as sections 2.2
intended and 5.2)
5
2.1 Broad
guidelines
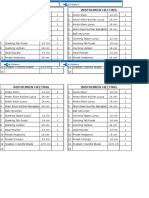
Modules A, B and C are delivery checks. Modules D, E ad F are safety and
calibration test and checks (Table 2).
The appropriate checks and tests for individual product items are chosen
from a set of modules, according to Table 3.
DELIVERY A Paperwork device checks against order and PPQ
CHECKS manuals, compliance and calibration
certificates, test results all included
see Annex 1 for where relevant
background is same model already represented on
database? (if not training/
documentation needed)
is device included in maintenance
system?
B Visual inspection outer packaging intact and undamaged
no damage apparent on inspection
case markings where relevant - CE
marking, notified body number,
electrical class, applied part type
(B/BF/CF)
does the device (or any component
part or accessory) need sterilizing
before the first use?
C Functional check are accessories/parts compatible?
do indicators and displays function
correctly when powered up?*
does it start when you press go?*
action of knobs and switches as
intended*
(see Example 1)
SAFETY AND D Electric - mains leads, plugs, and other
CALIBRATION basic safety connectors undamaged
CHECKS electrical safety test with Portable
Appliance Tester (PAT)
see Annex 2 for E Electric - patient acceptable leakage currents (see p 12)
background connected
F Calibration and Use test device to check
measurement accuracy of physiological measurements
dose delivery*
energy delivery*
accuracy of other outputs*
*only for active devices
6
2.2 Building up
suitable tests
from modules
Lower Risk devices
(typically CE class 1) A.B A,B,C,D
Moderate (typically A,B,C,F A,B,C,D,E,F
classes 2a and 2b) and
High Risk (class 3)
devices
See pp x and xi (DB9904 (NI) Appendix A 1.4) for CE-marking class definitions.
7
Active devices
(Electrical, electronic, gas
pressure powered and
complex mechanical)
Non-active (simple
mechanical devices -
no power source)
Example 1 - Functional test from a dialysis
machine manual
Installation test
The device must not be connected to a patient
during the installation test. Be sure that the test
is conducted using a container of water to
substitute for the patient.
If a malfuncture alarm occurs during the
installation test, the Control Unit has failed the
test. Do not use the control unit.
Call a trained and qualified technician
for service.
Procedure
To perform the installation test, follow the steps
below:
1. Turn on the control unit as described under
start-up in the Operation chapter. The control
unit performs an initialisation test during the
Startup procedure. Verify that the red, yellow,
and green lights are illuminated.
.......
.......
.......
10. Press the STOP softkey, then press the
END TREATMENT softkey and follow
the instructions to unload the set.
Functional tests
Example 1 gives an extract from a
typical manual.
In general such tests check that:
controls operate as expected;
motors and actuators move
freely - device functions
properly;
displays show appropriate
information.
They do not aim to show that
performance conform to any standard,
or exhaustively check every possible
error state. The operations included are
ones normally carried out by a user - the
device is not, for example, placed in
engineering mode, or connected to test
equipment.
For simple electrical devices it will
generally be adequate to simply plug the
device in and switch on. A light source,
for example, ought to light up.
Checks and testers can only be effective if everyone carrying them out has
appropriate training. Table 4 indicates the skills required for the various
modules:
Module Skills Required
(see sections
2.2 and 5.2)
A Familiarity with:
ordering system
inventory system
names and appearances of common medical devices
medical device documentation (manuals, certificates)
serial numbers and model identification codes.
B Knowledge of areas to check for damage.
Familiarity with:
the appearance of product in good condition
common defects.
C Basic electrical safety training - actions to take in cases
where fuse blows or circuit breaker trips. In cases where
manufacturers instructions specify assembly or
manipulation (eg loading a set), familiarity with necessary
components and accessories sufficient to follow
instructions.
D Training in visual electrical safety inspection techniques.
Training in use of simple (go/no go) PAT tester.
E,F Tests which should be carried out by a full-trained technician
Everyone carrying out checks and tests needs to be provided with appropriate
information:
which test modules to apply in a particular case;
where compliance and calibration certificates are necessary;
where to send the device after checking
what to do with manuals and certificates;
what records are needed.
This system is based on a thorough paperwork check and visual
examination carried out by well-trained, but not necessarily technically
qualified staff. Annex 1 gives the background to this policy. Bench tests
need technically qualified staff have been reduced to the minimum
needed to assure safety, on order to increase the time available for work
with users. Annex 2 gives background.
Eliminating duplication
In many cases tests and checks are carried out in stages, by different people.
It is easy to duplicate effort inadvertently, to introduce delays, and to fail to
produce coherent records. Table 5 shows the possible sources of relevant
information, including the data acquired by the manufacturer before
despatch. In many organisations, however, some or all of the functions in this
8
2.3 Training and
knowledge
which testers
need
2.4 Efficient
organisation
and record
keeping
table will be carried out by single department. If clinical staff need to do
checks or tests before first use, they should be alerted - probably best by
attaching a label to the device before it is released for use.
Stage User organisation action Test modules
possibly involved
(see sections 2.2 and
5.2)
Before dispatch - Acquire and assess data C
manufacturer from manufacturer (not for sterile product)
(function, calibration and D,E,F
safety checks which they
have carried out).
Stores/goods inwards Check damage in transit, A,B
order details.
Engineering Perform technical tests, eg D,E,F
departments electrical safety.
Medical physics Check radiation safety, F
calibration of monitoring
equipment.
Before use - Check integrity of pack Bulk pack form (5.1)
clinical staff for sterile devices. C
Perform functional tests (not for sterile product)
where appropriate.
Data from manufacturers
Some user organisations may wish to use data generated by the
manufacturer rather than carry out tests themselves. They must receive
adequate documentation of the tests and their results. It is important to
establish that any tests were carried out on the actual product item in
question, and are not just sample data. Users need to be confident that:
manufacturers are using appropriate test methods;
there has been no damage in transit.
Record Keeping
User organisations should keep records of any safety or functional safety or
functional test. It should always be possible to find out the test result - who
carried it out, when and how:
Health and Safety Inspectors will expect records to be available;
a defence in a negligence if documentation is available for the
particular devices involved.
It is important that all reusable devices are entered onto a device database,
to facilitate efficient equipment management.
9
3. LEGAL REQUIREMENT FOR
ELECTRICAL SAFETY TESTING
The Electricity at Work Regulations Northern Ireland (EWR) 1991 (a
statutory rule SR1991/13, under the Health and Safety at Work Order
(Northern Ireland) 1998 (HASAWO) have regulated electrical safety in the
workplace since March 1991, and form the basis of the programmes used
by hospital estates department for the regular electrical testing of portable
electrical equipment.
HASAWO imposes a duty on employers to provide:
plant and systems of work that are, so far as is reasonably possible,
safe and without risks to health?
such information, instruction, training and supervision as is necessary.
EWR states that no electrical equipment shall be put into use when its
strength and capability may be exceeded... and that all systems shall be
maintained so as to prevent, so far as is reasonably practicable, danger.
Complying with this legislation has led organisations to implement
electrical safety testing programmes, involving pre-use testing of new
devices and periodic subsequent tests. The legislation itself does not spell
out what tests should be done at which intervals. There is no specific legal
obligation - or even guidance - requiring user organisations to do any
particular test, but here is a general duty to take necessary steps to protect
employees from danger.
4. SPECIAL CASES
When a new device model is introduced, or when pre-first-use functional
checks are complicated, technical and clinical staff should work together to
ensure that:
checks are successfully carried out and documented;
users have all the technical information and manuals that they need;
training needs have been identified and acted on;
technical staff are familiar with how the device performs in a clinical
context.
It should be recognised that some single-use products, such as balloon
catheters, are complex (and expensive), and staff training needs should be
taken into account. In most cases a manufacturers representative ought to
be present when a novel product of this type is first used.
Installed devices
When a device needs to be installed, there should be a procedure for
commissioning, worked out in collaboration with the supplier and the
10
4.1 Devices
which require
commissioning
Under the MDR, suppliers must provide instructions for installing a device
and bringing it into use. Where appropriate these instructions will include
specifications for safety and performance checks. A designated member of
staff should have oversight of the commissioning process, and
responsibility of deciding that it has been completed satisfactorily.
The purpose of a local safety certificate is to:
provide assurance that a device is safe and effective;
put appropriate limits on use.
Categories of products which should be subjected to risk assessment are
shown in Table 6.
Some devices fall into more than one category.
Category Examples
Medical devices manufactured outside Manufactured before the regulations
the scope of the MDR came into force.
Purchased by an individual outside EU.
In-house manufacture.
Devices which have (or may have) Bought second-hand.
been previously used. Property of patients or staff.
Lent by another user organisation.
Devices within cope of MDR, but not Custom-made for a named patient.
CE-marked. Under clinical investigation.
Table 7 gives possible outcomes for the risk assessment.
Category Evidence (examples) Outcome
Risk not significantly Custom-made and
greater than for a new clinical investigation Use modular
CE-marked product products with satisfactory tests from
MDR statements. Section 5.2
Previously used devices with
full maintenance history.
Risks significantly Devices of unknown Testing for
greater previous ownership. local safety
Devices manufactured certificate
in house.
In the second case (Risks significantly greater) risk assessment will lead
to a programme of local testing, and the issue of a local safety certificate if
this is successfully completed. If not, risks will outweigh possible benefits,
and the correct decision will be not to use the device in question. Past
history should be taken into account: devices on loan from organisations
with a quality assurance system in place for device maintenance are likely
to be safe and reliable. Example 2 shows a local safety certificate used by
one trust for equipment which needs a comprehensive safety assurance.
11
4.2 Devices
which might
need a local
certificate of
safety
organisation doing the installation. This usually occurs when there is a need
for any of the following:
substantial assembly work on site;
permanent plumbing, electrical and gas pipeline connections;
permanent fixing in place.
Example 2 - Local Certificate of Safety for devices subject to additional investigation.
CERTIFICATE OF ELECTRICAL AND MECHNICAL SAFETY
Applicable only to equipment that has not been commissioned from new
Item No..................... Model/Serial No.....................
VISUAL INSPECTION SECTION
Suitable 13 Amp plug fitted and correctly wired, fitted with a fuse rated at ............. Amp
Mains cable, outer sheath inspected
Mains cable entry / IEC connector, strain relief adequate
Instrument case provides adequate protection from the mains and all fixings are in place
Are the device mountings suitable and properly fitted? If none put na
ELECTRICAL MEASUREMENT SECTION
Earth Leakage Enclosure leakage A Patient Earth leakage A Patient auxiliary
A Only where if protective current A
earth
6 7 8 9 10 11 12 13 14 15 16
Normal supply Normal earth supply Normal earth supply normal earth supply
o/c o/c o/c o/c o/c o/c o/c
QUALITY CONTROL MUST BE COMPLETED BY TEAM LEADER
It was necessary to certificate the equipment because no proof of previous quality checks were available.
either - The equipment has no CE mark, and is not known to conform to BS5724
or - Other, give reason
Indicate what the future planned maintenance will be:
either - On a planned maintenance programme (PM interval..........months)
or - Equipment on fixed term loan. Indicate loan expiry date on licence licence until
Comments
12
Electrical Safety Class:
1B, 1BF, 1CF, 2B, 2BF, 2CF
Ring which is applicable
(3) Insulation resistance ...........MOhms
(4) BF & CF only ...........MOhms
(5) Earth bonding resistance 0...........Ohms
Products being evaluated
Users should check that all devices on loan from manufacturers are subject to
the Regional Supplies Service loan indemnity. This means that the
manufacturer has made suitable arrangements, and that the users exposure to
liability is no different than it would be if they had purchased the device under
normal conditions of sale. Thus pre-use procedures for loan equipment should
be the same as those for purchased equipment.
Products for patients to use at home
Enteral feeding pumps provide a typical example (see DB9904 (NI), page E4).
In cases where ownership and device management remain with the supplier, it
may be satisfactory to accept that manufacturers pre-dispatch tests combined
with simple pre-use checks by those responsible for the care of the patient in
the community (e.g. community nurse of carer) provide an adequate assurance
of safety.
13
4.3 Devices
loaned by
manufacturers
5. FORMS
1. Date/supplier/device type
2. Delivery note checks with order? yes no
3. Outer packaging undamaged? yes no
4. Goods checks with delivery note? yes no
Model/type identification
5. Goods clean, inner packaging intact? yes no
6. Lots or batch number
7. Use by date
8. Stock rotation procedures followed yes no
9. Instructions included yes no
Instructions circulated yes no
Module A Paperwork
1. Date/supplier/device type
2. Delivery note checks with order? yes no
3. Goods checks with delivery note? yes no
Model/type identification
Serial Number
Mains voltage
(where relevant)
Leads supplied yes no
Accessories supplied yes no
User manual supplied yes no
Instructions supplied yes no
Maintenance manual supplied yes no
Warranty document included yes no
Final test certificate supplied yes no
4. Local serial/inventory
5. Device type new to healthcare facility yes no
if yes, instructions circulated appropriately yes no
6. New Device sticker attached yes no
14
5.1 Draft form for
bulk-pack
products
5.2 Draft modules
for mechanical/
electrical devices
Module B Visual Inspection
1. Outer packaging undamaged? yes no
2. Case not dented/broken yes no
3. Panels etc. secure yes no
4. No rattles yes no
Module C Functional check
Plug in, turn on (following instruction manual)
1. Indicator lamps light up yes no
2. Display as described in manual yes no
3. Passes self test routine yes no
4. Moving parts operate properly yes no
5. Knobs and switches act properly yes no
Module D Electrical safety (basic)
1. (Moulded IEC mains connector and mains plug)
Connectors firmly attached yes no
No cores or bare wires visible yes no
Outer insulation intact yes no
Appropriate fuse fitted (see manual) yes no
Fuseholder secure yes no
2. Mains lead permanently attached).
Cord grips satisfactory yes no
3. Fuse value
4. Plugs and sockets mate yes no
5. Clamps and doors hatch yes no
6. Passes PAT test yes no
15
16
Module E Electrical safety for patient connected devices
This set of tests is designed:
to test equipment in normal working order;
not subject to equipment to currents or voltages exceeding those
experienced in normal operating conditions.
Thus no tests involve shorting electrodes together, or applying high voltages
to electrodes.
1. Electrical safety class: 1 2
type: B BF CF
2. Insulation resistance (class 1 only) between mains plug earth and other
two pins (line and neutral) connected together.
Measures at 350 V DC
2
Greater than 20 Megohms
3
yes no
3. Earth continuity (class 1 only) between mains plug earth pin and
accessible conductive parts. Current not more than 1 amp.
Less than 0.2 Ohms. yes no
4. Leakage currents
Setup Mains Mains must be Yes No
normal reversed
Earth (class 1 only) <500 A
Enclosure (tester
connected to <100 A
exposed conductive
part on device case)
Patient (tester 1. <100 A (B and BF)
connected to each 2. <10 A (CF)
electrode in turn 3.
4.
5.
6.
7.
...
2
It is very unlikely that electrical safety analysers operating at 500 V DC will cause any
harm.
3
A measured value less than 20 MQ should be investigated, but does not necessarily mean
that the equipment is unsafe. In some cases what is being measured is not the resistance of
the insulation but the value of an electronic component (a bleed resistor in a mains filter, for
instance), whose inclusion may be desirable and is entirely permissible provided it does not
cause excessive leakage current. If in doubt consult the manufacturer.
Megohms
Ohms
17
Device passes tests in manual Yes
Date
Data
(Insert mearsurements needed from manual, or locally generated
procedure).
No
Module F Calibration and measurement.
18
ANNEX 1 BACKGROUND -
DELIVERY CHECKS
Simple checks on delivery can save time
and avoid trouble - if a device is
discovered to be broken or inappropriate
only when someone tries to use it for the
first time, it can lead to:
delayed or interrupted
treatment;
waste of clinical staff time;
difficulties in returning the
device and establishing
when and where the
problem arose;
invalidation of warranties;
injury to patients and staff.
Other countries have issued similar
guidance (see Example 3)
Delivery checks are plainly cost effective
- they are a necessary part of any device
management system, and also eliminate
unnecessary risks (see Example 4).
These checks are uncontroversial - all
the manufacturers and user organisations
we have consulted agree that they should
be applied to all medical devices,
including single-use and consumable
items.
Example 3 AS/NZS 3551: 1996 Technical
management programs for medical devices
(An Australian/New Zealand standard)
Initial inspection Persons accepting
delivery (e.g. inwards goods staff) shall
check the packaging is undamaged. Any
damage shall be noted.
General acceptance inspection The medical
device shall be inspected as soon as possible
after delivery to establish that it is complete
with specified accessories and that it has not
been damaged in transit.
Example 4 Wrong trolley delivered
A firm supplying a trolley for a transport
incubator supplied a unit slightly modified
from the sample which the hospital had
judged to be satisfactory before purchase.
The model supplied did not have the correct
clamps, and broke loose when mounted in an
ambulance. The error was only discovered
after the adverse incident had occurred, but
could have become apparent during pre-use
testing.
19
ANNEX 2 BACKGROUND -
PRE-USE TESTS
Evidence about risk-levels
MDA/NIAIC receives very few adverse incident reports relating to newly
delivered products. Table 8, for example, gives details of incidents
involving damage in transit.
Category Number of incidents recorded
Wheelchairs and walking aids 54
Single-use devices 10
Nebulisers/oxygen supply 7
Beds and tables 5
Portable electro-medical devices 4
Safety tests.
The over-riding principle here is that pre-use tests should not be outside the
bounds of normal use:
Disassembly should be restricted to what is necessary for normal
use and cleaning;
Currents or voltages applied during tests should not exceed those
occurring in normal use.
Any test which involves an abnormal stress - for example loading a hoist
above its stated maximum working load - carries an unacceptable risk of
causing permanent damage, and may invalidate any warranty.
Failure to follow this advice may lead to dangerous devices being put into
service.
Damage in transit
Although faults can arise during transportation:
adequate packaging should provide any necessary protection;
delivery checks will detect damage to packaging - a good indicator
of possible problems during transport.
Table 8 shows the tiny incidence of damage in transit problems on the
MDA/NIAIC adverse incident data base.
Manufacturers guidance
Maintenance instructions may specify tests on a new device (for example,
in order to generate baseline data for later comparisons). A pragmatic
approach is to avoid duplication - these tests may serve as a functional
check and/or a calibration check.
20
Fig. 1 Incidents involving electric shock as a percentage of all reports
received by MDA.
% of incidents involving electric shock
Year
90 92 94 96 98
0.1
0.15
0.2
0.05
0.25
0
%
Performing extra tests not required by the manufacturer should be avoided.
If a manufacturers instructions seem to be inadequate to ensure continued
safety and adequate performance, this fact should be reported to, MDA and
we will take the appropriate action.
Electrical safety testing
Fig 1 shows all the incidents involving electric shock reported to the MDA
over the last 9 years (a total of 43). These do not exceed 0.25 % of reports
received in any year, and in 40 of these 43 cases injuries are categorised as
none or minor. No deaths by electrocution in the UK are recorded on
the MDA database. reports cover all medical devices in service, so risks for
new devices are very much lower.
21
Example 5 Quotes from speakers at Acceptance
testing for medical devices - the way forward?
meeting, organised by IPEM, ABHI and MDA.
1) John Conely (John Radcliffe Hospital,
Oxford)
The old HEI 95 ... goes into great detail as to what
we should check for electrical safety. Whats the
supreme importance of electrical safety over all
other safety considerations? In my own department
in the last seven years, I can recall two items of
equipment which failed electrical safety tests. One
took out the fuse when plugged in, and the other
had a heater element which caused some high
readings. For over seven years its an awful lot of
effort and not a lot of electrical safety problems.
2) Richard Mellish, (MDA)
I think there are two reasons why we have tended
to concentrated on electrical safety.
Because we know how to do it, and thats
a bad reason.
There is a legal obligation to do safety
testing on electrical equipment in use in
places of work from time to time to make
sure it hasnt become dangerous.
3) Nicholas Abraham (Charing Cross
Hospital)
Electrical safety tests have even less value
(than planned preventative maintenance tests).
Fire risks apart, this is the least of our worries.
Functional failure of equipment is far more
serious, especially for infusion pumps,
defibrillators, anaesthetic machines, etc.
Electrical safety has a place and shouldnt be
ignored but it really isnt the be all and end of
all safety. Weve seen a few cases IEC leads
with failed earth continuity - just enough to
support the testing rule. Weve seen even fewer
failures on patient leakage current - just
enough to support testing. We appreciate that if
youre going to rest either of those things, once
youve got the machine out, the marginal cost
of making all the tests is small enough to make
it really not worth arguing about. So we might
as well do the tests. But remember, its quite
easy for something quite dangerous to pass
electrical safety tests*. I certainly would not be
advocating setting up a whole service from
scratch just to do electrical safety testing.
* eg an intense light source with a faulty fan
will pass an electrical safety test, but overheat
dangerously if operated for any length of time.
Many user organisations have traditionally carried out extensive electrical
safety testing programmes, but evidence that these programmes are
important for maintaining device safety is weak - one hospital clinical
engineering department has told us that it has conducted 13000 electrical
safety tests on new equipment without finding a single electricity unsafe
device. Published data also shows low rates of electrical safety faults.
(Amoore, J.N., Stay, D.G., and Mather, J. Scheduled inspection of
electromedical equipment. Planning and assessment Journal of Medical
Engineering and Technology 19 211-218).
There is thus little evidence that electrically-powered medical devices are a
special hazard and no justification for a disproportionate allocation of
resources to test them - as compared to non-electrical products with similar
risks levels. This document presents a compromise position, recognising
that some electrical testing is legally necessary (see Section 3), and that the
decision to eliminate some of the tests currently in use is a difficult one to
take.
Example 5 has quotes from papers given by senior biomedical engineers
at a meeting organised by IPEM, ABHI and MDA in March 1998.
22
Methods for electrical testing
Role of visual examination
Structured visual inspections involve checks of integrity, compatibility,
correct fusing, and correct labelling. In general, for double-insulated
devices with no accessible metal parts, electrical safety can only be
assessed by a structured visual examination.
Purpose-built appliance testers
A portable tester (PAT) gives a simple pass/fail reading. It requires some
training in its use, though no specialist electronic skills. PAT tests normally
include earth bonding and insulation resistance.
More sophisticated electrical testers such as the Bioteck electrical safety
analyzer print out a list of resistance and current values, and require a
higher competency to operate safely, and not to interpret the findings. Some
of the tests involve operating the device with its safety earth disconnected
and must only be conducted in a suitably equipped workshop. In some
circumstances the testing may constitute live working.
Reducing electrical testing without compromising safety
Table 9 summarises three approaches we considered:
Strategy For all devices Additional tests Additional tests
or devices with for patient
exposed metal connected
parts devices
1 No electrical Structured visual Accept Accept
testing exam + functional manufacturers manufacturers
test assurance assurance
2 Typical estates Structured visual PAT tester Accept
protocol exam + functional manufacturers
test assurance
3 Risk-related Structured visual PAT tester Electrical safety
testing effort exam + functional analyzer
test
Strategy 1 employs a structured visual inspection and simple functional test
for all devices. The functional test will detect electrical faults which cause a
fuse to blow, or the device to fail to operate. Otherwise this strategy relies
on the manufacturers inspection before dispatch for electrical safety. See
Section 3 for legal requirements in this area.
23
Strategy 2 adds a PAT test for any device which is not double-insulated.
This will align medical device practice with procedures used for other
electrical equipment within the same organisation, for example hospital
estates departments testing non-medical devices,
It would seem reasonable for healthcare organisations to adopt a common
safety standard for medical devices:
for use by staff;
supplied to patients to use themselves (or for their carers to use).
Strategy 3. As 2, but with an electrical safety analyser for patient-
connected devices. This reduces a very slight risk of electrocution via leads,
due to an out-of-box failure. Many biomedical engineers have argued
strongly for this option, even if they are persuaded that a full set of
electrical tests on every single device is a waste of time.
The modular approach in section 2 is based on strategy 3, but healthcare
organisations may find that strategy 2 or even strategy 1 proves acceptable
in their particular circumstances, following a risk assessment.
DISTRIBUTION
This Device Bulletin should be brought to the attention of managers and staff in all HPSS
Organisations.
This device bulletin should also be brought to the attention of medical device coordinators, medical
engineering and medical physics staff, IT staff, medical and nursing directorate managers, general
practitioners, dental practitioners, pathology laboratory managers and staff responsible for medical
equipment used in the community.
TECHNICAL ENQUIRIES
General enquiries concerning this Device Bulletin should be addressed to:-
Mr Brian Godfrey
Northern Ireland Adverse Incident Centre
Health Estates
Estate Policy Directorate
Stoney Road
Dundonald
BT16 1US
Tel: 028 9052 3714
Fax: 028 9052 3900
email: brian.godfrey@dhsspsni.gov.uk
FURTHER COPIES
Further copies of this Device Bulletin are free to Health and Social Care providers and may be obtained
on written request from:
Northern Ireland Adverse Incident Centre
Room A7
Health Estates
Estate Policy Directorate
Stoney Road
Dundonald
Belfast
BT16 1US
Tel: 028 9052 3704
Fax: 028 9052 3900
Health Estates
An Executive Agency of the Department of Health, Social Services and Public Safety
isneacht Feidhmeannacdh don Roinn Slinte, Serbhs Sisialta agus Sbhilteacht Phoibl
You might also like
- Guide To Classify of Medical DevicesDocument11 pagesGuide To Classify of Medical DevicesPranav UpadhyayaNo ratings yet
- List Recognized Standards Medical Devices Guidance CanadaDocument35 pagesList Recognized Standards Medical Devices Guidance CanadaRobert SplinterNo ratings yet
- Iba't Ibang Ahensiyang PamahalaanDocument4 pagesIba't Ibang Ahensiyang PamahalaanVer Bautista0% (1)
- Blood Pressure ChartDocument9 pagesBlood Pressure ChartVer BautistaNo ratings yet
- Medical EquipmentDocument48 pagesMedical EquipmentKhalid Khassawneh100% (2)
- EU Guide Medical Device DirectiveDocument112 pagesEU Guide Medical Device DirectiveJoherNo ratings yet
- Managing Medical Devices within a Regulatory FrameworkFrom EverandManaging Medical Devices within a Regulatory FrameworkBeth Ann FiedlerRating: 5 out of 5 stars5/5 (1)
- OGP Standards For Local Medical SupportDocument36 pagesOGP Standards For Local Medical Supportihwan100% (1)
- Unit 2 - Medical Device SafetyDocument27 pagesUnit 2 - Medical Device SafetyBetty MollaNo ratings yet
- How To Design Solar PV SystemDocument53 pagesHow To Design Solar PV SystemVer Bautista100% (2)
- Complaint Handling 60.60 23JUN2020Document11 pagesComplaint Handling 60.60 23JUN2020Abdul RahmanNo ratings yet
- Medical Device GuidanceDocument34 pagesMedical Device GuidanceVanessaNo ratings yet
- Medication Safety PDFDocument95 pagesMedication Safety PDFMangayarkarasi ChandrakasanNo ratings yet
- MED EquDocument9 pagesMED EquAmir100% (1)
- CSDT GMDDocument40 pagesCSDT GMDSyafiqNo ratings yet
- History of Nursing in The Philippines Group 2Document10 pagesHistory of Nursing in The Philippines Group 2Karen Joyce Costales MagtanongNo ratings yet
- International Standard (Iso 11014-1)Document10 pagesInternational Standard (Iso 11014-1)Kanupriya100% (1)
- Electrical & Electronic Testing of EquipmentsDocument52 pagesElectrical & Electronic Testing of EquipmentsPriti BhardwajNo ratings yet
- A Sample of The Completed Essential Principles Conformity Checklist MD CCLDocument12 pagesA Sample of The Completed Essential Principles Conformity Checklist MD CCLAyman Ali100% (1)
- Interview Skills: An RCN Guide For Health Care Assistants and Assistant PractitionersDocument9 pagesInterview Skills: An RCN Guide For Health Care Assistants and Assistant PractitionersWalter AlexandruNo ratings yet
- National Guideline For Patient Safety Incident Reporting and Learning in South Africa Version 2 - Web LayoutDocument82 pagesNational Guideline For Patient Safety Incident Reporting and Learning in South Africa Version 2 - Web LayoutSheena Mabaquiao-PadernalNo ratings yet
- Er Admission PolicyDocument9 pagesEr Admission PolicyIrish Martinez100% (2)
- CSSDDocument43 pagesCSSDMohd SalahuddinNo ratings yet
- IVD GuideDocument23 pagesIVD GuidevolkandemirNo ratings yet
- CE Guidelines Classification Medical DeviceDocument17 pagesCE Guidelines Classification Medical DeviceMehdi100% (4)
- Kitchen LayoutDocument47 pagesKitchen LayoutVer Bautista100% (5)
- Guidelines On Medical Equipment Management in NigeriaDocument8 pagesGuidelines On Medical Equipment Management in NigeriaBALANo ratings yet
- Medical DeviceDocument8 pagesMedical DeviceHarshvardhan ChoudharyNo ratings yet
- Clinical Evaluation Report SampleDocument12 pagesClinical Evaluation Report Sampleibrahim kademogluNo ratings yet
- WHTM 01-01 Part BDocument37 pagesWHTM 01-01 Part BMorcosNo ratings yet
- Manual Fetal Doppler SonolineDocument29 pagesManual Fetal Doppler SonolineOmar del CastilloNo ratings yet
- Define What Is PhysicsDocument6 pagesDefine What Is PhysicsVer BautistaNo ratings yet
- Night NightDocument21 pagesNight Nightapi-402315475No ratings yet
- Medical Devices StandardsDocument135 pagesMedical Devices StandardsGnanasaravanan 2508100% (1)
- Human Factors Medical Devices v2.0Document35 pagesHuman Factors Medical Devices v2.0EKNo ratings yet
- Silay City Watersports and Recreation Park (Chapter VI)Document30 pagesSilay City Watersports and Recreation Park (Chapter VI)Aisa Castro Arguelles100% (1)
- Guide To IEC 62353Document36 pagesGuide To IEC 62353Marco Todde100% (2)
- HIS ADHOC BillStatement STD Rev1Document2 pagesHIS ADHOC BillStatement STD Rev1Quinio ReyNo ratings yet
- Topic 1 Quality Standard Regulations 22Document48 pagesTopic 1 Quality Standard Regulations 22Aiman SyakirinNo ratings yet
- Medical Devices and IVDs: Fit for the new EU-Regulations: Your complete seminar for projekt, study and jobFrom EverandMedical Devices and IVDs: Fit for the new EU-Regulations: Your complete seminar for projekt, study and jobNo ratings yet
- M20 - Chapter 1 - Medical Device Safety Standard PDFDocument80 pagesM20 - Chapter 1 - Medical Device Safety Standard PDFTakIe AdnanNo ratings yet
- Bulletin Healthcare Organisations 03142023Document46 pagesBulletin Healthcare Organisations 03142023dodyNo ratings yet
- SafetyDocument15 pagesSafetyBetty MollaNo ratings yet
- Leitfaden Fuer App Entwickler Def ENDocument53 pagesLeitfaden Fuer App Entwickler Def ENYousra El MeriniNo ratings yet
- GHTF Imdrf Clasificacion de DMDocument30 pagesGHTF Imdrf Clasificacion de DMPieroNo ratings yet
- USA PMS RegulationsDocument42 pagesUSA PMS RegulationsDayaNo ratings yet
- 2010 CLinical Investigations - 2 - 7 - 4 - en PDFDocument10 pages2010 CLinical Investigations - 2 - 7 - 4 - en PDFWillem MuetstegeNo ratings yet
- WHO 2019 NCoV PPE Specifications 2020.1 EngDocument40 pagesWHO 2019 NCoV PPE Specifications 2020.1 EngHervian LanangNo ratings yet
- Clinical Investigations: Serious Adverse Event Reporting Under Directives 90/385/eec and 93/42/eec.Document12 pagesClinical Investigations: Serious Adverse Event Reporting Under Directives 90/385/eec and 93/42/eec.FranciscoNo ratings yet
- GHTF-sg1-n41r9-safety& PerformanceDocument16 pagesGHTF-sg1-n41r9-safety& PerformanceLoganathan SellappanNo ratings yet
- GN 07 r2 2 Guidance On Complaint Handling (2022 Nov) - PubDocument8 pagesGN 07 r2 2 Guidance On Complaint Handling (2022 Nov) - PubJEYA KUMARANNo ratings yet
- Designing Medical Electrical Equipment To Meet Safety Certification and Regulatory RequirementsDocument6 pagesDesigning Medical Electrical Equipment To Meet Safety Certification and Regulatory RequirementsMohamed Abdel FatahNo ratings yet
- Australia Post Market Activity GuidelinesDocument31 pagesAustralia Post Market Activity Guidelinesspenceblack7999No ratings yet
- Final ThesisDocument69 pagesFinal ThesisAswin WSNo ratings yet
- Standard No. CEA/Wellness Centre-018Document21 pagesStandard No. CEA/Wellness Centre-018Gladys MatiraNo ratings yet
- H3 Standares para El Soporte MedicoDocument36 pagesH3 Standares para El Soporte Medicoleo limpiasNo ratings yet
- Benchtop Steam Sterilizers - Guidance On Purchase, Operation and MaintenanceDocument48 pagesBenchtop Steam Sterilizers - Guidance On Purchase, Operation and MaintenanceSigrid MiNo ratings yet
- Medical Device Act 2012Document53 pagesMedical Device Act 2012ram010No ratings yet
- Meddev 2.7 4Document10 pagesMeddev 2.7 4Jug_HustlerNo ratings yet
- ADV-G0004 Guide To The Classification of A Medical Device v2Document11 pagesADV-G0004 Guide To The Classification of A Medical Device v2Putu Gede GandharaNo ratings yet
- Asean MDPWG CSDT - Final - 21 Oct 2010Document12 pagesAsean MDPWG CSDT - Final - 21 Oct 2010Brian WilliamsNo ratings yet
- Spain Product SafetyDocument5 pagesSpain Product SafetySebastian VanderlindenNo ratings yet
- Standard For Equipment in Critical Care: The Intensive Care SocietyDocument15 pagesStandard For Equipment in Critical Care: The Intensive Care SocietyAhmed Sabaa ayounNo ratings yet
- GHTF sg1 n70 2011 Label Instruction Use Medical Devices 110916Document17 pagesGHTF sg1 n70 2011 Label Instruction Use Medical Devices 110916Use EreNo ratings yet
- Bao Duong May Tiet TrungDocument51 pagesBao Duong May Tiet TrungĐức CườngNo ratings yet
- GHTF sg5 n2r8 2007 Clin EvalDocument28 pagesGHTF sg5 n2r8 2007 Clin EvalLoganathan SellappanNo ratings yet
- Planned Preventive MaintenanceDocument4 pagesPlanned Preventive MaintenanceMOHAMMAD AHMADNo ratings yet
- Unistor User and Installation ManualDocument56 pagesUnistor User and Installation ManualIan RamageNo ratings yet
- Medical Devices Handling, Environmental SafetyDocument37 pagesMedical Devices Handling, Environmental SafetyGnanasaravanan 2508No ratings yet
- ProcedureDocument62 pagesProcedureAshok KumarNo ratings yet
- Healthsmart Design Authority: Ihi Pre-Implementation ProjectDocument31 pagesHealthsmart Design Authority: Ihi Pre-Implementation Projectwidayat81No ratings yet
- Emc Emi SystemsDocument2 pagesEmc Emi SystemsVer BautistaNo ratings yet
- UNFPA Technical Requirements For Medical DevicesDocument7 pagesUNFPA Technical Requirements For Medical DevicesVer BautistaNo ratings yet
- Transformation of Energy 8 UnitDocument25 pagesTransformation of Energy 8 UnitVer BautistaNo ratings yet
- Biomed Poster IIDocument1 pageBiomed Poster IIVer BautistaNo ratings yet
- Energy EfficiencyDocument2 pagesEnergy EfficiencyVer BautistaNo ratings yet
- Bachelor of Technical Teacher Education in The PhilippinesDocument14 pagesBachelor of Technical Teacher Education in The PhilippinesVer Bautista0% (1)
- Term Paper 1 Eco Health (Qingwen Kawaji)Document12 pagesTerm Paper 1 Eco Health (Qingwen Kawaji)Ver BautistaNo ratings yet
- Capacitor and Voltage RatingDocument2 pagesCapacitor and Voltage RatingVer BautistaNo ratings yet
- Current Members of SenateDocument3 pagesCurrent Members of SenateVer BautistaNo ratings yet
- Comparison Chart LED CFL ILDocument5 pagesComparison Chart LED CFL ILVer BautistaNo ratings yet
- Mortuary FreezerDocument4 pagesMortuary FreezerVer BautistaNo ratings yet
- ChlorineDocument1 pageChlorineVer BautistaNo ratings yet
- BP Cuff Sizes For Manual SphygmomanometerDocument1 pageBP Cuff Sizes For Manual SphygmomanometerVer BautistaNo ratings yet
- BP Cuff Sizes For Manual SphygmomanometerDocument1 pageBP Cuff Sizes For Manual SphygmomanometerVer BautistaNo ratings yet
- CalibrationDocument25 pagesCalibrationWaqarAhmedButtNo ratings yet
- S.W.G. ChartDocument1 pageS.W.G. ChartVer BautistaNo ratings yet
- Definitions of Acids and Bases0Document15 pagesDefinitions of Acids and Bases0Ver BautistaNo ratings yet
- Etymology of LiteratureDocument28 pagesEtymology of LiteratureVer Bautista50% (2)
- QuotesDocument2 pagesQuotesVer BautistaNo ratings yet
- Biological Safety Cabinet GermfreeDocument3 pagesBiological Safety Cabinet GermfreeVer BautistaNo ratings yet
- Shortcut Keys ReferenceDocument4 pagesShortcut Keys ReferenceVer BautistaNo ratings yet
- An Innovative DesignDocument5 pagesAn Innovative DesignVer BautistaNo ratings yet
- Autodesk Autocad BasicsDocument80 pagesAutodesk Autocad BasicsVer BautistaNo ratings yet
- Temporary Override Keys ReferenceDocument2 pagesTemporary Override Keys ReferenceVer BautistaNo ratings yet
- Alat HectingDocument4 pagesAlat HectingjuliperNo ratings yet
- Case StudiesDocument4 pagesCase StudiesL KennedyNo ratings yet
- Benefits of Preoperative Education For Adult Elective Surgery PatientsDocument6 pagesBenefits of Preoperative Education For Adult Elective Surgery PatientschayankkuNo ratings yet
- SusiDocument32 pagesSusiWebItKpiNo ratings yet
- SIMULATION of EMERGENCY ROOMS USING FLEXSIMDocument10 pagesSIMULATION of EMERGENCY ROOMS USING FLEXSIMBrandon VarnadoreNo ratings yet
- What Service Do You Need? Read The Statements, Look at The Pictures, and Complete The CrosswordDocument2 pagesWhat Service Do You Need? Read The Statements, Look at The Pictures, and Complete The CrosswordOmar GutiérrezNo ratings yet
- Updated CVDocument4 pagesUpdated CVcrazylucarioNo ratings yet
- Nice PrelimDocument2 pagesNice PrelimKaren Mae Santiago AlcantaraNo ratings yet
- Umibilical Cord - ProlapsDocument22 pagesUmibilical Cord - ProlapsAtikah PurnamasariNo ratings yet
- RCPsych Final Forensic Programme 2018at26febDocument8 pagesRCPsych Final Forensic Programme 2018at26febbrunotrancasNo ratings yet
- E-R Diagram Examples Questions PrintDocument9 pagesE-R Diagram Examples Questions PrintGetachew ShambelNo ratings yet
- Assignment Building SystemDocument5 pagesAssignment Building SystemMohd MezlanNo ratings yet
- 1 s2.0 S1879406821000631 MainDocument1 page1 s2.0 S1879406821000631 MainmiNo ratings yet
- ACUTE ABDOMEN Systemic SonographicDocument6 pagesACUTE ABDOMEN Systemic SonographiciwanNo ratings yet
- The Best of Charlie Munger 1994 2011Document12 pagesThe Best of Charlie Munger 1994 2011Vishnu PradeepNo ratings yet
- Hospital ManagementDocument20 pagesHospital ManagementGokulNo ratings yet
- Chap 15Document32 pagesChap 15IngenieroHenryNo ratings yet
- Windshield Survey Nurs340Document10 pagesWindshield Survey Nurs340api-247143627No ratings yet
- Claim Form - IPDDocument2 pagesClaim Form - IPDEswar Kiran ReddyNo ratings yet
- Assessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationDocument3 pagesAssessment Diagnosis Goals and Objectives Planning Intervention Rationale EvaluationCrissa AngelNo ratings yet
- Daftar Pustaka Refrat Bedah PlastikDocument3 pagesDaftar Pustaka Refrat Bedah PlastikAnggita DewiNo ratings yet
- Finaltest Listen SuperGoal11f2Document8 pagesFinaltest Listen SuperGoal11f2yahia222000No ratings yet