Professional Documents
Culture Documents
Publication of
Uploaded by
FebniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Publication of
Uploaded by
FebniCopyright:
Available Formats
Publication of IADVL,
WB
Official organ of AADV
IJ
D
Users
online:
76
Hom
e
Editorial
Board
Current
Issue
Archive
s
Comin
g
Soon
Guideline
s
Subscriptio
ns
e-
Alerts
Login
Click here to download free Android Application for this and
other journals Click here to view optimized website for
mobile devices Journal is indexed with PubMed
Share on facebookShare on twitterShare on citeulikeShare on
googleShare on linkedinMore Sharing Services
SPECIAL ARTICLE
Year : 2012 | Volume : 57 | Issue : 6 | Page : 428-433
The Effect of Hypoallergenic Diagnostic Diet in
Adolescents and Adult Patients Suffering from
Atopic Dermatitis
Jarmila Celakovsk
1
, K Ettlerov
2
, K Ettler
1
, J Bukac
3
, M Belobrdek
1
1
Department of Dermatology and Venereology, Faculty Hospital and
Medical Faculty of Charles University, Hradec Krlov, Czech Republic
2
Department of Allergy and Clinical Immunology, Outpatient Clinic,
Hradec Krlov, Czech Republic
3
Department of Medical Biophysics, Medical Faculty of Charles University
in Hradec Krlov, Czech Republic
Date of Web
Publication
1-Nov-
2012
Correspondence Address:
Jarmila Celakovsk
Department of Dermatology and Venereology, Faculty Hospital and
Medical Faculty of Charles University, Hradec Krlov
Czech Republic
Search
GO
Similar in PUBMED
Search Pubmed
for
Celakovsk J
Ettlerov K
Ettler K
Bukac J
Belobrdek M
Search in Google
Scholar for
Celakovsk J
Ettlerov K
Ettler K
Bukac J
Belobrdek M
Related articles
Atopic dermatitis
diagnostic
hypoallergenic
diet
SCORAD system
Article in PDF (593
KB)
Citation Manager
Access Statistics
Reader Comments
Email Alert *
Add to My List *
* Registration required
(free)
DOI: 10.4103/0019-5154.103065
PMID: 23248359
Abstract
Aim: To evaluate the effect of a diagnostic hypoallergenic diet
on the severity of atopic dermatitis in patients over 14 years of
age. Materials and Methods: The diagnostic hypoallergenic
diet was recommended to patients suffering from atopic
dermatitis for a period of 3 weeks. The severity of atopic
dermatitis was evaluated at the beginning and at the end of
this diet (SCORAD I, SCORAD II) and the difference in the
SCORAD over this period was statistically
evaluated. Results: One hundred and forty-nine patients
suffering from atopic dermatitis were included in the study:
108 women and 41 men. The average age of the subjects was
26.03 (SD: 9.6 years), with the ages ranging from a minimum
of 14 years to a maximum of 63 years. The mean SCORAD at
the beginning of the study (SCORAD I) was 32.9 points (SD:
14.1) and the mean SCORAD at the end of the diet (SCORAD
II) was 25.2 points (SD: 9.99). The difference between
SCORAD I and SCORAD II was evaluated with the Wilcoxon
signed-rank test. The average decrease of SCORAD was 7.7
points, which was statistically significant
(P=.00000). Conclusion: Introduction of the diagnostic
hypoallergenic diet may serve as a temporary medical
solution" in patients suffering from moderate or severe forms
of atopic dermatitis. It is recommended that this diet be used
in the diagnostic workup of food allergy.
Keywords: Atopic dermatitis, diagnostic hypoallergenic diet,
SCORAD system
How to cite this article:
Celakovsk J, Ettlerov K, Ettler K, Bukac J, Belobrdek M. The
Effect of Hypoallergenic Diagnostic Diet in Adolescents and Adult
Patients Suffering from Atopic Dermatitis. Indian J Dermatol
2012;57:428-33
Abstract
Introduction
The Aim
Materials and Me...
Results
Discussion
Conclusion
References
Article Figures
Article Tables
Article Access
Statistics
Viewed 661
Printed 14
Emailed 1
PDF
Downloaded
48
Comments [Add]
Cited by
others
2
Gadgets powered
by Google
How to cite this URL:
Celakovsk J, Ettlerov K, Ettler K, Bukac J, Belobrdek M. The
Effect of Hypoallergenic Diagnostic Diet in Adolescents and Adult
Patients Suffering from Atopic Dermatitis. Indian J Dermatol [serial
online] 2012 [cited 2014 May 22];57:428-33. Available
from: http://www.e-ijd.org/text.asp?2012/57/6/428/103065
What was known? The role of food allergy remains controversial in older
children and adult patients suffering from atopic dermatitis, few studies
concerning the food allergy in this group of patients are available.
Introduction
Atopic dermatitis is a chronic, intermittent, inflammatory,
genetically predisposed skin disease that is characterized by
severe pruritus and xerosis. A number of environmental
factors have been implicated in its pathogenesis.
The role of food allergy in atopic dermatitis has been a subject
of controversy in dermatology, but today there is definite
evidence that food allergy has a role in the pathogenesis of the
disease. The importance of food allergy in children with atopic
dermatitis has been confirmed by extensive studies,
[1]
but the
role of food allergy remains controversial in older children and
in adults suffering from this disease.
Many food reactions in people with atopic dermatitis may not
necessarily be mediated through immune reactions.
[2]
As
sensitization to food early in life may be a predisposing
factor,
[3]
it is important to investigate whether the elimination
of dietary triggers can help alleviate the symptoms of atopic
dermatitis. The role of dietary factors in atopic dermatitis-
either as a causative factor or as a treatment measure through
the use of exclusion diets- remains unclear.
[4]
Many
researchers advocate double-blind placebo-controlled food
challenges to establish whether a child has a true food
allergy.
[5]
There is a vast amount of literature claiming that dietary
elimination of specific foodstuffs causes improvement of atopic
dermatitis in some cases. However, much of the evidence fails
to withstand close scrutiny.
[2]
The advantage of dietary
interventions is that they may address one of the primary
causes, as opposed to treatments that merely suppress the
symptoms. However, there can be serious consequences to
any dietary manipulation that leaves the individual deficient in
calories, protein, or minerals such as calcium.
[6],[7]
Avoidance
of multiple foods is potentially hazardous and requires
continuing dietary supervision in the pediatric age-group.
[6]
According to the European Academy of Allergy and Clinical
Immunology (EAACI) position paper, in case of suspected food
allergy (by history and/or specific sensitization), a diagnostic
elimination diet is recommended over a period of up to 4-6
weeks, with the exclusion of the suspected food items. If the
role of food in persistent moderate-to-severe atopic dermatitis
is unclear, the patient should maintain a daily record of
symptoms (including the status of atopic dermatitis, intensity
of itch, and sleep loss) and the intake of specific foods. These
protocols will give an overview of the patient's diet and may
point to a possible relation between the worsening of eczema
and specific food intake. If there is no such association and the
diagnostic procedures outlined above do not provide helpful
information, the introduction of a diagnostic hypoallergenic
diet over a period of at least 3 weeks can be helpful in severe
atopic dermatitis.
[8]
If the condition of atopic dermatitis
remains stable or increases within 4 weeks during the
diagnostic elimination diet, it is unlikely that food allergy is a
relevant trigger factor for the atopic dermatitis, and open food
challenges are then not necessary. It has to be taken into
account that in rare cases a food that was 'allowed' during the
elimination diet may be responsible for persistent symptoms.
The European Task Force on Atopic Dermatitis (ETFAD) has
developed the SCORAD (SCORing AD) index to create a
consensus on assessment methods for atopic dermatitis so
that the results of different trials can be compared.
[9]
The Aim
The aim of our study was to evaluate, using the SCORAD
system, the effect of a diagnostic hypoallergenic diet taken for
a period of at least 3 weeks. This diet was recommended to
patients suffering from atopic dermatitis in the diagnostic
workup of food allergy before open exposure tests with
suspected food allergens.
Materials and Methods
Patients
Patients over 14 years of age with atopic dermatitis who were
examined at the Department of Dermatology and Venereology,
Faculty Hospital and Medical Faculty of Charles University,
Hradec Krlov, Czech Republic, from January 2005 to April
2008 were included in the study. The diagnosis of atopic
dermatitis was made according to the the Hanifin-Rajka
criteria.
[10]
All patients signed informed consent forms prior to inclusion in
the study, and the permission of the local ethics committee
was obtained for conducting this study.
Examinations
Complete dermatological and allergological examination was
performed in all included patients at the allergological
outpatient department, with evaluation of the occurrence of
bronchial asthma and of the occurrence of perenial or seasonal
rhinoconjunctivities.
Personal history
A detailed personal history of possible food allergy was taken
in all included patients. The patients were asked if they
suffered from immediate or late food adverse reactions
affecting the skin (itching, rush, urticaria, worsening of atopic
dermatitis), gastrointestinal tract, or respiratory tract. History
of food-dependent exercise-induced anaphylaxis (FDEIA),
occupational asthma and rhinitis, and contact urticaria was
also elicited.
Examinations
The diagnostic workup of food allergy (including skin prick
tests, atopy patch tests, and measurement of specific serum
IgE) to wheat, cow's milk, peanut, soy, and egg was
performed before the diagnostic hypoallergenic diet was
started. This was done during intervals when the patient had
mild symptoms of atopic dermatitis (as evaluated with
SCORAD).
Open exposure test and double-blind placebo-controlled food
challenge tests with suspected food allergens were performed
after the diagnostic hypoallergenic diet during intervals when
the patient had mild symptoms of atopic dermatitis.
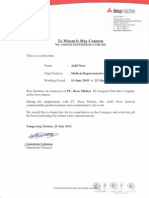
[Figure 1] shows the diagnostic algorithm for the identification
of food allergy in atopic dermatitis patients and the inclusion of
the diagnostic hypoallergenic diet in the diagnostic workup of
food allergy in patients suffering from atopic dermatitis.
[8]
Figure 1: Diagnostic algorithm for the
identification of food allergy in atopic
dermatitis
Click here to view
Scoring of atopic dermatitis
The diagnosis of atopic dermatitis was made using the Hanifin-
Rajka criteria
[10]
at the Department of Dermatology and
Venereology, Faculty Hospital and Medical Faculty of Charles
University, Hradec Krlov, Czech Republic.
Severity of eczema was scored using the SCORAD
index,
[9]
which includes assessment of topography items
(affected skin area), intensity criteria, and subjective
parameters. To measure the extent of atopic dermatitis, the
rule of nines was applied on a front/back drawing of the
patient's body. The extent can be graded on a scale of 0 to
100. The intensity part of the SCORAD index consists of six
items: Erythema, edema/papulation, excoriations,
lichenification, crusts, and dryness. Each of these items can be
graded on a scale of 0 to 3. The subjective items include daily
pruritus and sleeplessness. Both subjective items can be
graded on a 10-cm visual analog scale. The maximum
subjective score is 20. All items were entered in the SCORAD
evaluation form. The SCORAD index was calculated using the
formula: A/5 + 7B/2 + C. In this formula, A represents the
extent (0-100), B represents the intensity (0-18), and C
represents the subjective symptoms (0-20).
The severity of atopic dermatitis as evaluated with SCORAD
was graded as mild (20 points), moderate (20- 50 points), or
severe (>50 points). The severity of atopic dermatitis was
evaluated with the SCORAD system at the beginning of the
diagnostic hypoallergenic diet and at the end of this diet
(before the exposure tests).
The diagnostic hypoallergenic diet
This diet was designed to be free of any additives and
allergens and was suggested to the patient during the
diagnostic workup of food allergy; it was introduced after
obtaining the patient's informed consent.
Over the period of 3 weeks we recommended the following
foods:
Gluten-free foods
Potatoes, rice
Beef, pork, and chicken meat
Vegetable and fruits only after thermal modification;
but parsley, celery, and seasoning were not allowed
The patient was allowed to drink only plain drinking
water, mineral water, or black tea.
No other foods and drinks were allowed during this
period of 3 weeks.
During this diet the patient was allowed to treat himself with a
low-potency topical corticosteroid. Other anti-inflammatory
substances and ultraviolet (UV) therapy were not permitted.
Results
Patients
One hundred and forty-nine persons-108 women and 41 men-
entered the study. The average age was 26.03 years (SD: 9.6
years), with the minimum age being 14 years and the
maximum 63 years. The mean SCORAD was 32.9 points (SD:
14.11) (maximum 79.5 points; minimum 12.5 points) at the
beginning of the study. The mean SCORAD at the end of the
diet was 25.2 (SD: 9.99). These data and the clinical
characteristics of patients are presented in [Table 1].
Table 1: Patient older than 14 years of
age suffering from atopic dermatitis -
characteristics
Click here to view
In all patients a complete allergological examination was
performed. The data about the occurrence of bronchial
asthma, occurrence of seasonal or perennial
rhinoconjunctivitis, the onset of atopic dermatitis, and family
history of atopy were recorded [Table 1].
[Table 2] demostrates the categorization of the 149 patients
according the severity of their atopic eczma at the beginning
of the diet and at the end of the diet. At the beginning of the
diet 32 (22%) patients suffered from the mild form, 97 (65%)
from the moderate form, and 20 (13%) from the severe form
of atopic dermatitis. The mean SCORAD at the start of the
study was 32.9 (SD: 14.1). The mild form of atopic dermatitis
was recorded at the end of the diet in 50 (33%) patients, the
moderate form in 92 (62%) patients, and the severe form in 7
(5%) patients. The mean SCORAD at the end of this diet was
25.2 (SD: 9.99).
Table 2: Patients categorized according
the severity of atopic dermatitis at the
beginning of the diet and at the end of
the diet (with the mean SCORAD)
Click here to view
[Table 3] demonstrates the number of patients with increase
and decrease in SCORAD at the end of the diet. Decrease of
SCORAD was recorded in 119 patients (80%). A decrease of
SCORAD by only about 1 point was recorded in 6 of the 119
patients, while in 113 patients (76%) the decrease of SCORAD
was by more than 1 point. The mean decrease in the SCORAD
was 7.7 points.
Table 3: SCORAD at the end of the diet
Click here to view
Increase of SCORAD was recorded in three patients and in all
of them the increase was by 3 points. No changes during this
diet were recorded in another 27 patients (18%), i.e. the level
of SCORAD at the beginning of the diet and at the end of the
diet were the same.
Statistical evaluation of SCORAD
SCORAD at the beginning and at the end of diagnostic
hypoallergenic diet was evaluated with the Wilcoxon signed-
rank test. We rejected the null hypothesis about the
conformity in SCORAD I and SCORAD II because the average
difference of 7.7 points was substantial and statistically
significant (P = 0.00001).
Discussion
Atopic dermatitis is a chronic, intermittent, inflammatory skin
disease that may be associated in some cases with food
allergies. Numerous other trigger factors for atopic dermatitis
have been identified, including inhalable respiratory allergens,
irritative substances, and infectious microorganisms such as
Staphylococcus aureus. Psychogenic and climatic factors may
also cause exacerbations of atopic dermatitis.
The epidermal barrier plays a crucial role in protecting the
body against infection and other exogenous insults by
minimizing transepidermal water loss and by conferring
immunological protection.
[11]
Filaggrin gene defects
substantially increase the risk of atopic dermatitis. The
increased skin permeability in those with such defects may
increase the risk of sensitization to food and other allergens,
indicating the importance of cutaneous allergen avoidance in
early life to prevent the onset of atopic dermatitis and food
allergy.
[11]
Food allergy appears to be an important factor in the
exacerbation of atopic dermatitis in only a subset of children
(and a much smaller subset of adults). Non- IgE- mediated
mechanisms are sometimes implicated in the atopic dermatitis
flare-ups associated with ingestion of the foods in question,
and food allergy appears to have little or no role in children
with nonatopic dermatitis.
[12],[13],[14]
In a questionnaire survey
of schoolchildrens' perceptions regarding the factors
influencing their atopic dermatitis,
[15]
an extremely small
proportion (8%) of respondents believed that certain foods or
drinks had an effect on their eczema. A survey of adults in
High Wycombe showed that 20% perceived exacerbations of
their atopic dermatitis as adverse reactions to specific foods,
but only 1% had confirmed food allergies.
[16]
According to
Sicherer, both atopic dermatitis and food allergy are, in the
majority of individuals, transitory conditions that improve with
increasing age.
[17]
It is important to determine the severity of atopic dermatitis
for evaluation of disease improvement after and during
therapy. Scoring of the severity of atopic dermatitis is
demanded in clinical trials. The ETFAD has developed the
SCORAD index to create a consensus on assessment methods
for atopic dermatitis so that study results of different trials can
be compared.
[18]
To evaluate the effect of the diagnostic hypoallergenic diet we
calculated the SCORAD index at the beginning and at the end
of this diet in all included 149 patients. This diet was
recommended for 3 weeks and was clearly explained to the
patient at the beginning of the study.
Patients were asked to record the symptoms of atopic
dermatitis (the extent of involved skin, itching, sleep disorder,
etc.) and any other health problems in special forms. In 119
(79.8%) patients there was improvement of atopic dermatitis,
as indicated by the decrease of SCORAD. In 6 of these
patients, the decrease of SCORAD was only by 1 point, while in
113 patients (75%) the decrease of SCORAD was by more
than 1 point. The average level of the SCORAD decrease was
7.7 points. Worsening of atopic dermatitis was recorded during
this diet in three patients, with increase of SCORAD by 3
points in all three cases. No changes in the severity of atopic
dermatitis during this diet were recorded in another 27
patients, with the level of SCORAD at the beginning and at the
end of this diet being the same.
Before the beginning of the diet the majority of patients in our
study suffered from the moderate form of atopic dermatitis (97
patients), 32 from the mild form, and 20 from the severe form
of the disease. At the end of the diet, improvement was
recorded in the 20 patients with the severe form of atopic
dermatitis, with only 7 of these 20 patients continuing to have
severe disease; the SCORAD index was about 45 points in
these patients at the end of 3 weeks, indicating a moderate
form of atopic dermatitis. Although the average decrease in
SCORAD (by 7.7 points) was not very marked from the clinical
point of view, most of the patients evaluated this diet as
having a favorable effect. The majority of the patients
indicated that pruritus of the skin was diminished and that
they could sleep better.
On the basis of our results we can conclude that introduction
of the diagnostic hypoallergenic diet can serve as a temporary
medical solution in adolescents and adult patients suffering
from moderate and severe forms of atopic dermatitis.
After 3 weeks of the diagnostic hypoallergenic diet the patients
were allowed to introduce the suspected food in their meals
and educated about the performance of challenge tests with
the probable food allergen. They were informed about the
possibility of cross-allergy with pollen and about the risk
associated with consuming meals containing aromatic additives
and histaminoliberators. All patients were recommended an
additive-free diet, with a low content of biogenic
amines.Patients with chronic urticaria or atopic dermatitis may
suffer from intolerance to histamine. A diet with a low content
of biogenic amines may improve the condition of these
patients. All patients included in this study evaluated this diet
as having a positive effect on their symptoms.
Because of the uncertainties regarding the benefits and harms
of dietary exclusion in people with atopic dermatitis, Bath-
Hextall et al.
[19]
conducted a systematic review of all relevant
randomized controlled trials. They found some evidence to
support the use of an egg-free diet in infants with suspected
egg allergy and positive specific IgE to eggs in their blood.
Only two of the 11 included studies tested for food
allergy,
[20],[21]
but those studies dealt with comparisons of two
different forms of exclusion diets rather than a comparison of
an exclusion diet vs a normal diet and therefore have not
contributed to the question of whether any form of exclusion
diet is helpful in such people. The other studies included
unselected people with atopic dermatitis did not find any
evidence of benefit for exclusion diets. Elimination diets can be
difficult to follow. The studies reported in the Bath-Hextal et al.
review
[19]
were performed in different populations, with only
one study presenting data on the severity of atopic dermatitis.
The clinical importance of the small changes in severity scores
obtained in many studies is unknown. Although diets excluding
foods such as cow's milk are commonly advised, there is little
evidence in favor of their benefit in unselected people with
atopic dermatitis.
[19]
Future studies should be large enough to answer the questions
posed, and should be reported according to Consolidated
Standards of Reporting Trials (CONSORT)
guidelines.
[22]
Commonsense suggests that food exclusion
studies should be done on people with history suggestive of
food allergy, and positve results should be confirmed by
appropriate allergy testing or challenge tests. A distinction
should be made between young children and adolescents and
adults because food allergy in children tends to improve over
time. Disease severity should be measured using valid
instruments and should include qualityof-life assessments and
patient-centered outcomes that are easy to interpret clinically.
Whereever possible, long-term (>6 months) outcomes should
also be recorded in such studies.
Conclusion
On the basis of our results we recommend the introduction of
this diagnostic hypoallergenic diet as a temporary medical
solution in patients suffering from moderate or severe atopic
dermatitis. This diet can serve as an important diagnostic test
in the workup of food allergy.
References
1. Sampson HA. Update on food allergy. J Allergy Clin
Immunol 2004;113:805-19.
2. Oranje A, De Waard-van der Spek F. Atopic dermatitis and
diet. J Eur Acad Dermatol Venereol 2000;14:437-8.
3. David TJ, Patel L, Ewing CI, Stanton RH. Dietary factors in
established atopic dermatitis. In: Williams H, editor. The
epidemiology, causes and prevention of atopic dermatitis.
Cambridge: Cambridge University Press; 2000. p. 193-
201.
4. Baena-Cagnani C, Teijeiro A. Role of food allergy in asthma
in childhood. Curr Opin Allergy Clin Immunol 2001;1:145-
9.
5. Sampson H. The immunopathogenic role of food
hypersensitivity in atopic dermatitis. Acta Derm Venereol
1992;176:34-7.
6. David TJ, Waddington E, Stanton R. Nutritional hazards of
elimination diets in children with atopic dermatitis. Arch Dis
Child 1984;59:323-5.
7. Devlin J, Stanton RHJ, David TJ. Calcium intake and vows'
milk free diets. Arch Dis Child 1989;64:1183-4.
8. Turjanmaa K. The role of atopy patch tests in the diagnosis
of food allergy in atopic dermatitis. Curr Opin Allergy Clin
Immunol 2005;5:425-8.
[PUBMED]
9. Kunz B, Oranje AP, Labrze L, Stalder JF, Ring J, Taieb A.
Clinical validation and guidelines for the SCORAD index:
consensus report of the European task Force on Atopic
Dermatitis. Dermatology 1997;195:10-9.
10. Hanifin J, Rajka G. Diagnostic features of atopic dermatitis.
Acta Derm Venereol 1980;60:44-7.
11. Worth A, Shaikh A. Food allergy and atopic dermatitis. Curr
Opin Allergy and Clin Immunol 2010;10:226-30.
12. Ranc F, Boguniewicz M, Lau S. New visions for atopic
dermatitis: An iPAC summary and future trends. Pediatr
Allergy Immunol 2008;19 (Suppl 19):17-25.
13. Ranc F. Food allergy in children suffering from atopic
dermatitis. Pediatr Allergy Immunol 2008;19:279-84.
14. Werfel T, Ballmer-Weber B, Eigenmann PA, Niggemann B,
Ranc F, Turjanmaa K, et al. Eczematous reactions to food
in atopic dermatitis: Position paper of the EAACI and
GA2LEN. Allergy 2007;62:723-8.
15. Williams JR, Burr ML, Williams HC. Factors influencing
atopic dermatitis - A questionnaire survey of
schoolchildren's perceptions. Br J Dermatol
2004;150:1154-61.
16. Young E, Stoneham MD, Peetruckevitch A, Barton J, Rona
R. A population study of food intolerance. Lancet
1994;343:1127- 40.
17. Sicherer SH, Sampson HA. Food hypersensitivity and atopic
dermatitis: Pathophysiology, epidemiology, diagnosis and
management. J Allergy Clin Immunol 1999;104:114-22.
18. Oranje AP, Glazenburg EJ, Wolkerstorfer A, De Waard -van
der Speak FB. Practical issues on interpretation of scoring
atopic dermatitis: the SCORAD index, objective SCORAD
and three-item severity score. Br J Dermatol
2007;157:645-8.
19. Bath-Hextall F, Delamere FM, Williams HC. Dieaty
exclusions for improving established atopic dermatitis in
adults and children: systemic review. Allergy 2009;64:258-
64.
20. Niggemann B, Binder C, Dupont C, Hadji S, Arvola T,
Isolauri E. Prospective, controlled, multi-center study on the
effect of an amino-acid-based formula in infants with cow's
milk allergy/intolerance and atopic dermatitis. Pediatr
Allergy Immunol 2001;12:78-82.
21. Isolauri E, Sutas Y, Makinen-Kiljunen S, Oja S, Isosomppi
R, Turjanmaa K. Efficacy and safety of hydrolyzed cow milk
and amino acid-derived formulas in infants with cow milk
allergy. J Pediatr 1995;127:550-7.
22. Moher D, Schulz KF, Altman DG, Lepage L. The CONSORT
statement: Revised recommendations for improving the
quality of reports of parallel group randomised trials. Lancet
2001;357:1191-4.
What is new? The diagnostic hypoallergenic diet can serve as a temporary
medical solution in patients suffering from moderate or severe atopic
dermatitis.
Figures
[Figure 1]
Tables
[Table 1], [Table 2], [Table 3]
This article has been cited by
1 Alimentacin y nutricin: Repercusin en la salud
y belleza de la piel | [Diet and nutrition: Effects on
the skin beauty and health]
Puerto Caballero, L., Tejero Garca, P.
Nutricion Clinica y Dietetica Hospitalaria. 2013;
[Pubmed]
2
Sprvn lba atopick dermatitidy v dtskm
vku | [Treatment of atopic dermatitis in children]
Duchkov, H.
Pediatrie pro Praxi. 2013;
[Pubmed]
About us | Contact us | Sitemap | Advertise | What's New | Feedback | Copyright and Disclaimer
2005 - 2014 Indian Journal of Dermatology | Published by Medknow
Online since 25
th
November '05
ISSN: Print -0019-5154, Online - 1998-3611
V-Bates Shopper
You might also like
- Test-Guided Dietary Exclusions For Treating Established Atopic Dermatitis in Children A Systematic ReviewDocument5 pagesTest-Guided Dietary Exclusions For Treating Established Atopic Dermatitis in Children A Systematic ReviewAlfi RahmatikaNo ratings yet
- Out 4Document3 pagesOut 4Musthafa Afif WardhanaNo ratings yet
- B Celiaca Al Toma PDFDocument31 pagesB Celiaca Al Toma PDFSimona JuncuNo ratings yet
- Jurnal Tugas PDFDocument4 pagesJurnal Tugas PDFIntan Sanditiya AlifNo ratings yet
- Atopic Dermatitis in Infants and Children in IndiaDocument11 pagesAtopic Dermatitis in Infants and Children in IndiaMaris JessicaNo ratings yet
- Thyroid ReviewDocument45 pagesThyroid ReviewSharin K VargheseNo ratings yet
- Food Allergy in EuropeDocument1 pageFood Allergy in EuropehypercyperNo ratings yet
- PIIS1939455119301723Document5 pagesPIIS1939455119301723Yeol LoeyNo ratings yet
- Diagnosis and Management of CowDocument31 pagesDiagnosis and Management of CowSteluta BoroghinaNo ratings yet
- Togias 2017Document16 pagesTogias 2017Jessica LópezNo ratings yet
- 1 s2.0 S1939455122000631 MainDocument25 pages1 s2.0 S1939455122000631 MainWilliam Rolando Miranda ZamoraNo ratings yet
- Nutrients 14 00475 v3Document12 pagesNutrients 14 00475 v3ellafinarsihNo ratings yet
- Coeliac Disease and Gluten-Related DisordersFrom EverandCoeliac Disease and Gluten-Related DisordersAnnalisa SchiepattiNo ratings yet
- Low Vitamin D Levels Are Associated With Atopic Dermatitis, But Not Allergic Rhinitis, Asthma, or Ige Sensitization, in The Adult Korean PopulationDocument15 pagesLow Vitamin D Levels Are Associated With Atopic Dermatitis, But Not Allergic Rhinitis, Asthma, or Ige Sensitization, in The Adult Korean PopulationJundi Agung SamjayaNo ratings yet
- Pediatric Allergy Immunology - 2020 - Foong - Biomarkers of Diagnosis and Resolution of Food AllergyDocument11 pagesPediatric Allergy Immunology - 2020 - Foong - Biomarkers of Diagnosis and Resolution of Food AllergyAlfred AlfredNo ratings yet
- Dhar, 2016 Food Allergy in Atopic DermatitisDocument6 pagesDhar, 2016 Food Allergy in Atopic DermatitisImanuel Far-FarNo ratings yet
- Literature Review On AllergyDocument8 pagesLiterature Review On Allergyogisxnbnd100% (1)
- 1 s2.0 S2213219820303718 MainDocument20 pages1 s2.0 S2213219820303718 Mainrawr rawrNo ratings yet
- Effect of Lactobacillus Sakei Supplementation in Children With Atopic Eczema - Dermatitis SyndromeDocument6 pagesEffect of Lactobacillus Sakei Supplementation in Children With Atopic Eczema - Dermatitis SyndromePutri Halla ShaviraNo ratings yet
- Atopic Dermatitis 2013Document32 pagesAtopic Dermatitis 2013Bagus Maha ParadipaNo ratings yet
- Food Allergy and Atopic Dermatitis: How Are They Connected?Document9 pagesFood Allergy and Atopic Dermatitis: How Are They Connected?Denso Antonius LimNo ratings yet
- Probiotics and Prebiotics in Atopic Dermatitis: Pros and Cons (Review)Document8 pagesProbiotics and Prebiotics in Atopic Dermatitis: Pros and Cons (Review)larissaNo ratings yet
- Challenges in Differential Diagnosis of Coeliac DiDocument10 pagesChallenges in Differential Diagnosis of Coeliac DiNäjlãå SlnNo ratings yet
- Probiotics in Pregnant Women To Prevent Allergic Disease: A Randomized, Double-Blind TrialDocument8 pagesProbiotics in Pregnant Women To Prevent Allergic Disease: A Randomized, Double-Blind TrialarditaNo ratings yet
- The Study of Egg Allergy in Children With Atopic DermatitisDocument5 pagesThe Study of Egg Allergy in Children With Atopic DermatitisranifebNo ratings yet
- Ad 27 355Document9 pagesAd 27 355Hana MitayaniNo ratings yet
- HG 2 PDFDocument5 pagesHG 2 PDFFrandy HuangNo ratings yet
- Nutrition Journal of Parenteral and Enteral: Less or More? Enteral Nutrition in Critically Ill Septic PatientsDocument4 pagesNutrition Journal of Parenteral and Enteral: Less or More? Enteral Nutrition in Critically Ill Septic PatientsMarco Antonio BravoNo ratings yet
- Duration of A Cow-Milk Exclusion Diet Worsens Parents ' Perception of Quality of Life in Children With Food AllergiesDocument7 pagesDuration of A Cow-Milk Exclusion Diet Worsens Parents ' Perception of Quality of Life in Children With Food AllergiesM Aprial DarmawanNo ratings yet
- FK Concetration Is Increase in Children With Celic D....Document6 pagesFK Concetration Is Increase in Children With Celic D....Nejc KovačNo ratings yet
- Interpretation and implementation of the revised European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) guidelines on pediatric celiac disease amongst consultant general pediatricians in Southwest of EnglandDocument8 pagesInterpretation and implementation of the revised European Society for Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) guidelines on pediatric celiac disease amongst consultant general pediatricians in Southwest of EnglandJephte LaputNo ratings yet
- Clinical SpectrumDocument16 pagesClinical SpectrumArga LabuanNo ratings yet
- Fped 10 945212Document8 pagesFped 10 945212Nejc KovačNo ratings yet
- Annals EczemaDocument16 pagesAnnals EczemaewbNo ratings yet
- Clinical Spectrum of Food Allergies: A Comprehensive ReviewDocument16 pagesClinical Spectrum of Food Allergies: A Comprehensive ReviewAmalia Cipta SariNo ratings yet
- Fped 06 00350Document19 pagesFped 06 00350Jake DagupanNo ratings yet
- Nutrients: Personalized Nutrition Approach in Food Allergy: Is It Prime Time Yet?Document16 pagesNutrients: Personalized Nutrition Approach in Food Allergy: Is It Prime Time Yet?Meisya Nur'ainiNo ratings yet
- Atopic DermatitisDocument31 pagesAtopic DermatitisityNo ratings yet
- Medical News in The World of Atopic Dermatitis First Quarter 2016Document5 pagesMedical News in The World of Atopic Dermatitis First Quarter 2016anon_384025255No ratings yet
- Allergic Disease - Probiotics and PrebioticsDocument13 pagesAllergic Disease - Probiotics and PrebioticsMihaela AcasandreiNo ratings yet
- Apical Periodontitis and Diabetes Mellitus Type 2Document11 pagesApical Periodontitis and Diabetes Mellitus Type 2Mihaela TuculinaNo ratings yet
- The Link Between The Clinical Features o PDFDocument2 pagesThe Link Between The Clinical Features o PDFwulanNo ratings yet
- Jurnal DA 9Document8 pagesJurnal DA 9FIFIHNo ratings yet
- Celiac Disease New Approaches To Therapy: A ReviewDocument14 pagesCeliac Disease New Approaches To Therapy: A ReviewCeliacDesiNo ratings yet
- Enteropatia EosinofilicaDocument6 pagesEnteropatia EosinofilicaLuisa Maria LagosNo ratings yet
- Check Unit 555 November Immunology V3 PDFDocument25 pagesCheck Unit 555 November Immunology V3 PDFdragon66No ratings yet
- Allergy - 2014 - Muraro - EAACI Food Allergy and Anaphylaxis Guidelines Diagnosis and Management of Food AllergyDocument18 pagesAllergy - 2014 - Muraro - EAACI Food Allergy and Anaphylaxis Guidelines Diagnosis and Management of Food AllergyCatherinavcuNo ratings yet
- Group 5 Pubmed Accepted Results PDFDocument683 pagesGroup 5 Pubmed Accepted Results PDFDnyanesh LimayeNo ratings yet
- 2011 NIAIDSponsored 2010 Guidelines For Managing Food Allergy Applications in The Pediatric PopulationDocument13 pages2011 NIAIDSponsored 2010 Guidelines For Managing Food Allergy Applications in The Pediatric PopulationLily ChandraNo ratings yet
- Abses PayudaraDocument18 pagesAbses Payudaragastro fkikunibNo ratings yet
- Alergia AlimentariaDocument18 pagesAlergia AlimentariaLUIS PARRANo ratings yet
- Food Allergy - JCDocument20 pagesFood Allergy - JCHani GowaiNo ratings yet
- Alison ReidDocument28 pagesAlison ReidAnonymous KoDfgLZtimNo ratings yet
- HHS Public Access: Food Allergy: Immune Mechanisms, Diagnosis and ImmunotherapyDocument43 pagesHHS Public Access: Food Allergy: Immune Mechanisms, Diagnosis and ImmunotherapyLeonardo AzevedoNo ratings yet
- Atención de Los Niños Con Alergias A FármacosDocument5 pagesAtención de Los Niños Con Alergias A FármacosHugo RoldanNo ratings yet
- Oral Food Challenges in Children With A Diagnosis of Food AllergyDocument7 pagesOral Food Challenges in Children With A Diagnosis of Food Allergyastuti susantiNo ratings yet
- Etanercept Treatment For ChildrenDocument21 pagesEtanercept Treatment For ChildrenSitti Nurdiana DiauddinNo ratings yet
- Lay Prevalence Paper FinalDocument5 pagesLay Prevalence Paper Final강동희No ratings yet
- Abstract 2010 LourençoDocument1 pageAbstract 2010 LourençoAna Cristina SilvaNo ratings yet
- PDF Jurnal Kulit 2 - Oom JhonDocument5 pagesPDF Jurnal Kulit 2 - Oom JhonFebniNo ratings yet
- PhototherapyonPsoriasis-Prof DR Med IsaakEffendyDocument1 pagePhototherapyonPsoriasis-Prof DR Med IsaakEffendyFebniNo ratings yet
- Immunological Aspects of GastrointestinalDocument12 pagesImmunological Aspects of GastrointestinalFebniNo ratings yet
- Appi Ajp 2010 10040541Document9 pagesAppi Ajp 2010 10040541FebniNo ratings yet
- PDF GDocument3 pagesPDF GFebniNo ratings yet
- Jurnal Morbili Lp..Document11 pagesJurnal Morbili Lp..FebniNo ratings yet
- Appi Ajp 2010 09050627Document8 pagesAppi Ajp 2010 09050627FebniNo ratings yet
- Olive Oil: A Good Remedy For Pruritus Senilis: Short CommunicationDocument4 pagesOlive Oil: A Good Remedy For Pruritus Senilis: Short CommunicationFebniNo ratings yet
- Electrocardiograph Changes in Acute Ischemic Cerebral StrokeDocument6 pagesElectrocardiograph Changes in Acute Ischemic Cerebral StrokeFebniNo ratings yet
- Pedoman PenilainDocument4 pagesPedoman PenilainFebniNo ratings yet
- Pi Is 2090074013000790Document3 pagesPi Is 2090074013000790FebniNo ratings yet
- Electrocardiograph Changes in Acute Ischemic Cerebral StrokeDocument6 pagesElectrocardiograph Changes in Acute Ischemic Cerebral StrokeFebniNo ratings yet
- Bacterial Resistance To Antibiotics in Acne Vulgaris: An In: Vitro StudyDocument5 pagesBacterial Resistance To Antibiotics in Acne Vulgaris: An In: Vitro StudyFebniNo ratings yet
- A Comparative Study of The Efficacy of 4% Hydroquinone Vs 0.75% Kojic Acid Cream in The Treatment of Facial MelasmaDocument6 pagesA Comparative Study of The Efficacy of 4% Hydroquinone Vs 0.75% Kojic Acid Cream in The Treatment of Facial MelasmaFebniNo ratings yet
- Efficacy of 2% Metronidazole Gel in Moderate Acne Vulgaris: Therapeutic RoundDocument5 pagesEfficacy of 2% Metronidazole Gel in Moderate Acne Vulgaris: Therapeutic RoundFebniNo ratings yet
- Childhood Vitiligo: Response To Methylprednisolone Oral Minipulse Therapy and Topical Fluticasone CombinationDocument5 pagesChildhood Vitiligo: Response To Methylprednisolone Oral Minipulse Therapy and Topical Fluticasone CombinationFebniNo ratings yet
- Epidemiology RoundDocument13 pagesEpidemiology RoundFebniNo ratings yet
- Therapeutic RoundDocument6 pagesTherapeutic RoundFebniNo ratings yet
- Therapeutic Roun2Document5 pagesTherapeutic Roun2FebniNo ratings yet
- Long Standing Tracheal Foreign Body in ChildrenDocument12 pagesLong Standing Tracheal Foreign Body in ChildrenFebniNo ratings yet
- HTTPDocument6 pagesHTTPFebniNo ratings yet
- Dr. Agustina, SP - An, TenggelamDocument19 pagesDr. Agustina, SP - An, TenggelamrajaalfatihNo ratings yet
- Epidemiology Roun1Document10 pagesEpidemiology Roun1FebniNo ratings yet
- ScanDocument1 pageScanFebniNo ratings yet
- TC AdvisoryDocument1 pageTC AdvisoryJerome DelfinoNo ratings yet
- 9446 - Data Sheets Final PDFDocument17 pages9446 - Data Sheets Final PDFmarounNo ratings yet
- Icpc11 - Thermodynamics and Fluid MechanicsDocument22 pagesIcpc11 - Thermodynamics and Fluid MechanicsAPARNANo ratings yet
- Med Chem Exam 2Document24 pagesMed Chem Exam 2cNo ratings yet
- Stress Management PPT FinalDocument7 pagesStress Management PPT FinalAdarsh Meher100% (1)
- Nano ScienceDocument2 pagesNano ScienceNipun SabharwalNo ratings yet
- Hygiene PassportDocument133 pagesHygiene PassportAsanga MalNo ratings yet
- The Finite Element Method Applied To Agricultural Engineering - A Review - Current Agriculture Research JournalDocument19 pagesThe Finite Element Method Applied To Agricultural Engineering - A Review - Current Agriculture Research Journalsubhamgupta7495No ratings yet
- Transfer Case Electrical RMDocument51 pagesTransfer Case Electrical RMDaniel Canales75% (4)
- Karan AsDocument3 pagesKaran AsHariNo ratings yet
- Acer AIO Z1-752 System DisassemblyDocument10 pagesAcer AIO Z1-752 System DisassemblySERGIORABRNo ratings yet
- Digital Trail Camera: Instruction ManualDocument20 pagesDigital Trail Camera: Instruction Manualdavid churaNo ratings yet
- AC350 Specs UsDocument18 pagesAC350 Specs Uskloic1980100% (1)
- +chapter 6 Binomial CoefficientsDocument34 pages+chapter 6 Binomial CoefficientsArash RastiNo ratings yet
- Logistics Operation PlanningDocument25 pagesLogistics Operation PlanningLeonard AntoniusNo ratings yet
- Mercedez-Benz: The Best or NothingDocument7 pagesMercedez-Benz: The Best or NothingEstefania RenzaNo ratings yet
- Eoi QAMDocument6 pagesEoi QAMPeeyush SachanNo ratings yet
- HBT vs. PHEMT vs. MESFET: What's Best and Why: Dimitris PavlidisDocument4 pagesHBT vs. PHEMT vs. MESFET: What's Best and Why: Dimitris Pavlidissagacious.ali2219No ratings yet
- Aerodrome Advisory Circular: AD AC 04 of 2017Document6 pagesAerodrome Advisory Circular: AD AC 04 of 2017confirm@No ratings yet
- Your Heart: Build Arms Like ThisDocument157 pagesYour Heart: Build Arms Like ThisNightNo ratings yet
- Avionic ArchitectureDocument127 pagesAvionic ArchitectureRohithsai PasupuletiNo ratings yet
- Over Current & Earth Fault RelayDocument2 pagesOver Current & Earth Fault RelayDave Chaudhury67% (6)
- Daoyin Physical Calisthenics in The Internal Arts by Sifu Bob Robert Downey Lavericia CopelandDocument100 pagesDaoyin Physical Calisthenics in The Internal Arts by Sifu Bob Robert Downey Lavericia CopelandDragonfly HeilungNo ratings yet
- General Anaesthesia MCQsDocument5 pagesGeneral Anaesthesia MCQsWasi Khan100% (3)
- Mathematics For Engineers and Scientists 3 PDFDocument89 pagesMathematics For Engineers and Scientists 3 PDFShailin SequeiraNo ratings yet
- Smart Watch User Manual: Please Read The Manual Before UseDocument9 pagesSmart Watch User Manual: Please Read The Manual Before Useeliaszarmi100% (3)
- Notice: Environmental Statements Notice of Intent: Eldorado National Forest, CADocument2 pagesNotice: Environmental Statements Notice of Intent: Eldorado National Forest, CAJustia.comNo ratings yet
- Present Arlypon VPCDocument1 pagePresent Arlypon VPCErcan Ateş100% (1)
- Feature Writing EnglishDocument2 pagesFeature Writing EnglishAldren BababooeyNo ratings yet
- ONGC Buyout GOI's Entire 51.11% Stake in HPCLDocument4 pagesONGC Buyout GOI's Entire 51.11% Stake in HPCLArpan AroraNo ratings yet