Professional Documents
Culture Documents
Histology Exam 2 Review.1
Uploaded by
ashdmb217Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Histology Exam 2 Review.1
Uploaded by
ashdmb217Copyright:
Available Formats
TISSUE AND ORGAN BIOLOGY
CRITERIA FOR SUCCESS: At the conclusion of this course, students should be able to
1) Identify correctly all of the tissues and organs of the human body at the microscopic level;
2) Describe the diagnostic architectural and functional features of the tissues and organs and their specific cells; and
how these features are interrelated;
3) Associate and correlate the important clinical conditions that were presented as examples with their tissues and
organs; and also continue to make these associations as new clinical conditions are encountered.
Tissues can be defined as societies of cells, which together with their associated extracellular matrix (ECM), are
specialized to carry out specific functions.
In mature tissues, there are 4 primary phenotypes:
1) Epithelium;
2) Connective Tissue;
3) Muscle;
4) Nervous Tissue.
In embryonic tissues, there are 2 primary phenotypes:
1) Epithelium;
2) Mesenchyme.
Lecture #1 Cells, Tissues & Organs: Methods of Study
1. Understand the basic principles behind tissue preparation for microscopic
examination.
a. Fixative is typically a chemical agent, which may consist of a simple
solution; e.g., 10% formalin: formaldehyde dissolved in an aqueous or
buffered medium
b. The end result is cross-linking and denaturation of tissue components,
particularly proteins.
c. Dehydration and rehydration steps to move tissue between phases
i. If the fixative is aqueous and the material in which the tissue is to be embedded is
paraffin wax then a dehydration sequence is employed to introduce an organic phase that
will be compatible with the wax embedding medium.
2. Learn and recognize certain specific stains along with their particular characteristics
and shortcomings.
a. Proteins are amphoteric (possess both acidic and basic groups); at the
isoelectric point (pI ), the net charge is zero and minimal dye binding
occurs.
i. However, if staining is performed at a pH below their isoelectric
point
1. Basic groups (primarily amino) are positively charged and
bind dyes that are anionic/acidic, and the substances
stained (proteins) are termed acidophilic (acid-loving).
a. Anionic dye is Eosin (binds Eosinophic proteins)
2. If staining takes place above the isoelectric point, its acidic
groups (phosphate, carboxyl, or sulfate) will be negatively
charged and can combine with a positively charged
cationic dye (such as tolidune blue or methylene blue).
a. Since this type of dye is binding to an acidic (-)
group, it is termed a basic dye (+) and the
substance stained is termed basophilic (base-
loving)
b. Other cellular components that are basophilic: (due
to the phosphate groups in their nucleic acids)
include DNA, RNA, nuclei, nucleoli, and
ribosomes
b. A commonly used combination of dyes is
hematoxylin and eosin (H&E).
i. The hematoxylin (+ dye) can be
considered as a stain for nucleic acids
ii. The eosin (- dye) for proteins
c. Trypan blue and India ink are taken up and
stored by macrophages; form colloidal suspensions in
water. Since these large particulates will not diffuse into cells,
they will be cleared by the phagocytic activity of macrophages, and
are thus excellent markers for members of the mononuclear
phagocyte system (MPS)
i. Euchromatin = transcriptionally active; open &
unfurled; diluted dye
ii. Heterochromatin = not active; compact; darker
dye
d. Lipid colorants such as Sudan black and Oil Red O
are soluble in lipid and are used to demonstrate fat in
tissues if the lipid has not been extracted
e. Periodic acid-Schiff (PAS)
i. This technique is widely used for the
demonstration of certain carbohydrates by first converting side groups to
aldehydes (with periodic acid) and then identifying these aldehyde groups using the
Schiff stain.
f. Silver impregnation methods are employed to
demonstrate the Golgi apparatus, reticular
fibers, neurofibrils
g. Connective tissue stains: the Masson procedure
i. Collagen fibers of connective tissue are stained either
1. Blue (aniline blue), or
2. Green (fast green)
ii. Cytoplasm, in contrast, will be red-orange to red-lilac.
h. Immunohistochemistry (IHC) uses the principles of
immunology to locate and identify specific antigens with labeled antibody
i. Bromodeoxyuridine detection: for analyzing cell proliferation; the
thymidine analog 5-bromodeoxyuridine (BrdU) which is incorporated into nuclear
DNA during S-phase before mitosis - is localized in tissue sections with an antibody and
reveals cells that have recently undergone cell division
4
Hematoxylin = basophilic nuclei ;
Eosin = acidophilic myofibrils
6
Periodic acid Schiff (PAS)
mucins within goblet cells
basement membrane along basal surface of epithelium
SILVER STAIN
Golgi Apparatus
Lecture #2 Connective Tissue
1. Know and be able to identify the types of connective tissues (CTs), and their
functional properties.
a. Classification of a connective tissue is based on its predominant extracellular component
b. Each collagen fibril is composed of numerous (rod-like) collagen molecules that are linearly arranged
with respect to one another in a precisely staggered manner
c. Dense Connective Tissue
i. Dense regular connective tissue:
1. Tightly packed collagen fibers arranged in a parallel fashion.
2. E.g. tendons (which connect muscle to bone), and ligaments
(which connect bone to bone).
3. These structures derive their strength from the regular,
longitudinal arrangement of the bundles of collagen fibril
4. Elongated nuclei
18
Protein Packaged and Modified By
Addition of Sugar Moieties
Pigment of aging
Skin cells (melanin)
Melanin is polarized;
protects from UV with
cap on apical side of
nucleus (where UV is
always pointed)
DENSE REGULAR CONNECTIVE TISSUE (TENDON)
Collagen (fibers/
fibrils)
Fibroblast (nuclei)
ii. Dense irregular connective tissue:
1. Densely packed collagen fibers
2. However these fibers course irregularly through the tissue but
still impart strength to the tissues in which they are found
3. e.g., the dermis of skin
d. Loose/ Areolar Connective Tissue
i. Loose CT is the most common type
of CT
ii. All loose CT is irregular
1. Loose organization of fibers in
a large amount of ground
substance (where hyaluronic
acid & proteoglycans are
localized)
DENSE IRREGULAR CONNECTIVE TISSUE (skin)
Nerve
Nerve
Collagen
Fibroblast (nuclei)
FIBROBLASTS: major cell of both these types of CTs (and also in other CTs).
Synthesize extracellular matrix components (e.g., collagens, elastin, proteoglycans.)
Surfboard nuclei (thin & long from side; wide and flat from top)
Collagen
Fibroblast
(nuclei)
TEM of Collagen fibrils/fibers in longitudinal
(banded) and X-section (round) profiles.
TEM OF FIBROBLASTS AND COLLAGEN FIBRILS/FIBERS
Fibroblast nucleus (1) and cytoplasm (2)
Bundles of collagen fibrils (3)
Ground Substance (4)
LOOSE / AREOLAR CONNECTIVE TISSUE
Collagen fibers/
fibrils
Fibroblast (nuclei)
Blood vessel
iii. Holds organs in place & attaches epithelial tissues to itself and other
underlying tissues
iv. Surrounds blood vessels & nerves
v. Relatively poor in extracellular fibers, but rich in immigrant cells
(such as macrophages, plasma cells, mast cells, leukocytes)
e. Elastic connective tissue
i. Contain a large proportion of extracellular matrix as rubber-like
elastin which is a macromolecule complex able to undergo stretching
and subsequently return to its original length; occurs in two forms:
ii. Lamellar
1. Elastin is predominantly in form of lamellae (sheets/layers) in
large blood vessels (e.g. elastic arteries, rectifying the pulsatile
flow of blood coming from the heart)
iii. Fibrillar
1. Elastin is present in form of branched fibers/fibrils in
nonvascular tissue (e.g. skin)
a. In fibrils, elastin is complexed with a micofibrillar
component (fibrillin) which forms a scaffolding for
deposition of elastin & polymerizes it
f. Basement membranes/ Basal Laminae
i. Generally (but not always) associated with the basal surface of
epithelial tissues and are complex structures with a number of
components
2. Know and be able to identify the cellular constituents and functions of the different
types of CTs.
a. Cellular Components
i. Indigenous cells: arise within the CT itself: (e.g., Mesenchymal cells,
Fibroblasts, Adipocytes (fat cells)
1. Adipose Tissue
a. White
i. Fat (lipid) storage
ELASTIC CONNECTIVE TISSUE (Lamellar) (gives
elasticity to blood vessel)
ELASTIC CONNECTIVE TISSUE (FIBRILS)
(gives elasticity to tissues such as skin)
Branched
Elastic Fibrils
ii. Major cell type is adipocytes (large, fat
storage cells)
b. Brown
i. Heat production
ii. Numerous mitochondria (colored
cytochromes) and large number of blood
vessels
iii. Generally smaller cells than white fat in order
for mitochondria (which is between) to access
fatty droplet
iv. Cells have a large number of lipid droplets of
various sizes
v. Small droplets surrounded by aqueous
environment and mitochondria; nucleus is
usually centrally placed; also much more
vascular than white fat and transfers heat to
the blood in surrounding capillaries
1. Versus white droplet which is large and
surrounded by aqueous environment
White Adipose Tissue
Adipocyte (nucleus)
ADIPOSE TISSUE
Dense irreg. C.T.
Ducts and
Glands
Loose C.T.
Fat droplets
Brown adipose tissue
This photomicrograph shows
brown adipose tissue whose
cells (arrow) have numerous
lipid vacuoles. Also shown are
a small blood vessel(BV), and
white adipose tissue (along the
top).
ii. Immigrant cells: originate from hematopoietic stem cells in bone
marrow, circulate in the blood, and then move into connective tissue where they undergo
differentiation and perform their functions; E.g. Macrophages (derived from monocytes),
Lymphocytes, Plasma Cells (derived from B- Lymphocytes) and Mast cells
1. Macrophages
a. Large cells that phagocytose material such as:
i. Cellular debris (from apoptosis)
ii. Foreign bodies
iii. Air-born particles
b. Also present antigens to lymphocytes & produce cytokines
c. Can fuse with one another, forming large,
multinuclear, giant cells; or become osteoclasts and
function in bone resorption
d. Large eukromatic nuclei
e. Can have multi-nucleated cells lots of transcription
more phagocytic enzymes produced
2. Plasma Cells
a. B lymphocytes that have left circulation
b. Initiate the synthesis of immunoglobulins
c. Characterized by:
i. Oval shape, with one side forming an
apron of basophilic cytoplasm, and the
other side having a nucleus which is eccentric and
whose heterochromatin has a distinctive cartwheel or clock-
face arrangement.
ii. Basophilic staining of the cytoplasm reflects
layers of ER (where the IG proteins are being
synthesized)
Nuclei
Phagosomes
Distinguishing characteristics are large size, large irregularly shaped nuclei,
and cytoplasmic vacuoles (phagosomes) that contain phagocytosed material.
Plasma cells are B- lymphocytes that have left the circulation, and taken up
iii. Between basophilic cytoplasm and the nucleus
is a clear area, indicative of the Golgi (where
glycosylation & further processing of IGs occurs)
3. Mast cells
a. Participate in allergic reactions
b. Characteristics:
i. Presence of numerous small cytoplasmic
granules (generally blue)
ii. Dense central nucleus
c. Medical implications: mast cell granules contain
heparin (an anticoagulant) & histamine (a vasodilator
that renders venules & capillaries leaky- releasing
blood components and cells into surrounding CT)
4. Polymorphonuclear leukocytes: blood cells that (upon
stimulation) migrate from blood stream to CT
a. Includes neutrophils & eosinophils; both have bilobed/
multilobed nuclei & each has its own type of specific
granule
i. Granule of neutrophils are light pink; of
eosinophils are bright red
b. Neutraphils (micophages)
i. Most abundant type of WBC
ii. First cell into connective tissue for
inflammatory response; recruited by cytokines
iii. Phagocytose bacteria, resulting in the
formation of intracellular vacuoles
(phagosomes)
iv. Connective tissue is like the field where the
battle takes place
v. Exocytose genome after an attack which
allows them to use their sticky DNA as a net
for parasites
vi. Results in lobbed nucleus
Plasma Cells
vii. The granules stain the basic dye and the
acid dye, so you have both and they cancel
either out resulting in a lighter dye
viii. Very toxic when they degranulate
c. Eosinophils are recruited if parasites are too big for
neutraphils
i. Prevalent in asthma
1. Have been co-opted because humans dont have
parasitic infections as much anymore; end up
attacking themselves
d. Medical implications:
i. Neutrophils
1. The subsequent killing involves
releasing (from their granules) into the
phagosome antibacterial substances
2. e.g., superoxide anions and hydrogen peroxide,
lysozyme (which cleaves a cell wall component of
certain bacteria), and lactoferrin (that binds iron which
is a crucial component of bacterial nutrition)
ii. Eosinophils
1. Have cytotoxic effects on the parasite
(through the release of peroxidase and
other toxic substances).
2. Involved in mechanisms associated with
allergies
3. e.g., modulating inflamation (by neutralizing histmine
and by phagocytosing antigen-antibody complexes
b. Extracellular Matric Components
i. Fibrous constituents: Collagen fibers, Elastic fibers, Reticular
fibers
1. Reticular Connective Tissues
a. Forms a supportive, flexible network within/around
organs & structures that are subject to changes in form
or volume (e.g. spleen, sinusoids, lymph nodes)
b. Characterized by extremely thin fibers (reticular
fibers) which consist of collagen type III (a fibrillar
collagen) complexed with a large amount of
carbohydrate
Eosinophil
Eosinophil
c. Not visible in H&E preparations but stained black in silver salts
ii. Ground substance (amorphous): non-fibrillar material between
cells
1. Binds tissue components together, mediates metabolite
exchange, lubricates joints, and provides reversible
compressibility
2. Consists of: Proteoglycans, Glycosaminoglycans and
Glycoproteins
a. Proteoglycans are linear polymers of disaccharides [glycosaminoglycans
(GAGs)], covalently linked to a protein core
i. Highly negatively charged (sulfate groups on the sugar
residues)
ii. Can be hydrophilic (attract and bind H
2
O, accounting for the
porous nature of CT that allows diffusion of metabolites and
waste products to traverse to and from blood vessels)
iii. Proteoglycans can range in size from quite small (e.g., the
heparan sulfate proteoglycans) to extremely large complexes
(in cartilage)
b. Glycoproteins are multifuctional proteins that have attached
oligosaccharides
i. Are capable of binding cells to matrix molecules, both for
adhesion and cell-matrix signaling (e.g. fibronectin and
laminin)
3. Know the extracellular (matrix) components of the different types of CTs, and their
properties and functions.
a. The fibrillar collagens (long rod-like)
i. Major structural component of many connective tissues
ii. Comprise ~30% of bodys protein
iii. Different types:
1. Type I: most ubiquitous type
a. Polymerized in different ways to make different
outcomes
b. E.g. bone vs cornea (polymerized so light can pass
through)
2. Type II: the major collagen of cartilage matrix
3. Type III: rich in blood vessels and reticular CT
Sinusoids
Reticular
fibers
iv. Structure: Each collagen is comprised of three chains found into a
triple-helical structure
1. Every 3
rd
residue is glycine (necessary for triple-helix formation)
2. Enzymatic hydroxylation of proline to hydroxyproline stabilizes TH
3. Hydroxylation of lysine is involved in crosslinking
v. Synthesis: Collagen molecules are synthesized as soluble precursors (procollagens) that
have short, non-collagenous peptides (termed propeptides) at both the NH2 and COOH
terminal ends
1. Proteolytic removal of these propeptides by enzymes
termed procollagen peptidases is necessary for the collagen
molecules to associate with one another in a fibrillar
arrangement
a. These caps prevent polymerization until procollagen peptidase cleaves
them; act as a failsafe so collagen synthesis does not occur in fibroblasts
b. Mutation in a procollagen peptidase leads to skin
loss
2. Once the molecules are assembled in the staggered arrangement, the amino groups
on some of the lysines and hydroxylysines are enzymatically converted to reactive
aldehydes by the enzyme lysyl oxidase that then go on to
spontaneously form the intra- and inter- molecular crosslinks
4. Know the pathological conditions discussed.
a. Progressive systemic sclerosis:
i. Results from an over-accumulation of collagen (fibrosis)
ii. Results in hardening and functional impairment that can affect a
number of different organs (e.g., skin, the digestive tract and muscle)
b. Keloids
i. Results from abnormal accumulations of collagen.
ii. Are localized conditions that result in swellings that can be
disfiguring
iii. Occur most often in individuals of black African descent, and be clinically difficult to
correct as their removal is frequently followed by recurrence.
iv. A similar, less severe condition of excessive scar formation is the
hypertrophic scar.
c. Scurvy
i. Deficiency in Vitamin C (ascorbic acid) results in defective collagen
synthesis
ii. Vitamin C is required for activity of prolyl hydroxylase & lysyl
hydroxylase (enzymes responsible for hydroxylation of proline & lysine)
1. These posttranslational modifications stabilize the helical
structure & form the crosslinks that stabilize fibrils
iii. Defective fibrilogenesis causes a general loss of connective tissue
function, including fragile capillaries, resulting in abnormal
bleeding and loss of teeth due to degeneration of the periodontal
ligament
iv. Can result in perifolicular hemorrhage on legs
d. Ehlers-Danlos syndrome
i. Inherited CT disorders caused by variety of defects in CT synthesis
ii. Severity can range from mild to life-threatening
iii. Examples:
1. Aortic and or intestinal rupture (caused by faulty
transcription or translation of collagen type III)
2. Hyperelastic skin
3. Eye fragility
4. Progressive curvature of the spine (scoliosis; caused by faulty
lysine hydroxylation)
5. Hyperextensible joints & dislocations (luxation); caused by
decreased procollagen peptidase activity
iv. Type VII: decreased procollagen peptidase activity
1. Possible defect in triple helix formation
e. Cutis Laxa
i. Involves a number of gene involved with elastin
ii. Clinical features:
1. Skin that is loose, hanging, wrinkled, and lacking in elasticity;
premature aging appearance
2. Joints may be Hyperextensible
3. Can also affect certain internal organs
f. Marfan Syndrome
i. Mutations of the fibrillin gene
ii. Can affects a number of organ systems
iii. Clinical features:
1. Skeletal abnormalities: greater than normal height; long slender
limbs; scoliosis; Hyperextensible joints
2. Cardiovascular system: dilated aorta or an aortic aneurysm (
fatal aortic dissection)
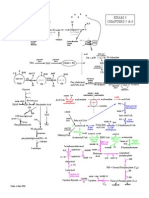
Lectures #3 & #4 Skeletal Tissues: Cartilage and Bone (I and II)
1. The morphological characteristics of the different types/forms of cartilage and bone
a. In the mature, adult skeleton most of the bones are in the form of long bones
i. Consist of a shaft comprised of bone tissue whose ECM has organic and mineral components
ii. Cartilage covering both ends (forming the articular surface)
iii. Bone has blood vessels, but adult cartilage is avascular
iv. Both collagen & the calcium phosphate salts (hydroxy apetite) to make the
bone strong
b. Hyaline Cartilage
i. Two components:
1. Type II cartilage (collagen fibrils)
a. Fibril associated collagen (the darker molecules with a kink)
b. Have a collagen domain and also a bending domain; can
interact with each other and other type II collagens
c. Stabilize matrix through cross-links
d. Only on the surface of the molecule
e. Arthritis may be due to degradation of cross-linked regions
2. Cartilage proteoglycan (give it the resiliency)
a. A protein core with glycosaminoglycan (GAG) side chains that
are predominantly chondroitin sulfate
b. Is also termed aggrecan for the ability of numerous of these proteoglycans to bind to a
hyaluronic acid molecule
c. Highly hydrated, and the side chains, due to their negative
charge, repel one another
d. Are attached through their core protein to linear hyaluronic acid
molecule and form extremely large suppramolecular complexes
ii. The cells (termed chondrocytes) are enclosed within this matrix in regions
termed lacunae (which means lake)
iii. Covers the articular surfaces; found in respiratory tree, nose and transiently
during endochondral bone formation
iv. Resilient (shock absorber) and has a smooth, slippery surface, especially at
joints in conjunction with synovial fluid
c. Cartilage growth
i. INTERSITIAL
1. Isogenic clusters of chondrocytes reflect coordinate cell division
2. After the chondrocytes divide, they deposit matrix between them and
gradually move apart
Hyaline Cartilage (light micrograph)
Cartilage
matrix
Chondrocytes in
lacunae
In mature hyaline cartilage, chondrocytes are largely present as
individuals with a lot of matrix inbetween
RAPIDLY GROWING CARTILAGE undergoing interstitial growth (isogenic clusters of
chondrocytes) and appositional growth (perichondrial cells becoming chondrocytes).
Interstitial growth;
Isogenic clusters of
chondrocytes
Appositional
growth
LIGHT MICROGRAPH (low power) OF HYALINE CARTILAGE WITH THE SURROUNDING
(FIBROBLASTIC) PERICHONDRIUM
Perichondrium
Chondrocytes in lucanae
ii. APPOSITIONAL
1. Occurs at the surface of the cartilage
2. Involves the perichondrium
a. Fibrous CT over the surface of most cartilages (except articulat) which attaches the
cartilage to adjacent tissue
3. Perichondrial cells (which are fibro-blast like) undergo a
progressive transformation to chondrocytes
d. Specialized types of cartilage
i. Intervertebral disc
1. Outer ring of fibrocartilage (the annulus fibrosis), and an inner
gelatinous component (the nucleus pulposus)
2. Fibrocartilage
a. Has features of both a dense connective tissue (type I collagen
fibers), and cartilage matrix (type II collagen fibrils and
cartilage proteoglycan)
3. Elastic cartilage
a. Has cartilage matrix components and also networks of elastic
fibers
b. Provides flexibility; can withstand repeated bending
e. Bone Tissue
i. Extracellular matrix of organic & inorganic components
1. Organic (30%) is type I collagen (large diameter fibrils)
2. Inorganic (65%) is calcium-phosphate in a crystalline form
CHONDROCYTES
IN LUCANAE
ELASTIC FIBERS (within
cartilage matrix)
(hydroxyapatite)
ii. Osteoid: newly synthesized & uncalcified bone; undergoes mineralization
1. Unlike type II, these collagen fibers are long and banded due to the
precise arrangement
iii. Restoration/reconstruction of bone: can be achieved by implanting decalcified
bone matrix
1. bone morphogenic proteins (BMPs)
2. This matrix "induces" cells within the responding tissue to undergo a
complete sequence of endochondral bone formation
2. The molecular composition and the characteristics of bone and cartilage matrix
a.
3. The cell types found in cartilage and bone and their characteristics.
a. Bone cells
i. Osteoblasts (OB)
1. Mesenchymal origin
2. Single layer of cells over the surfaces where the new bone is being
deposited
3. Adopt a cuboidal shape and have an epithelioid (epithelial-like)
arrangement
4. Responsible for the synthesis and secretion of the unmineralized matrix
of bone (called osteoid)
T.E.M. of a region of newly forming bone
ii. Osteocytes (O) are the mature cells of bone tissue
1. Derived from osteoblasts that have become buried within the bone
matrix
2. Reside within lacunae of the bone matrix
3. Canaliculi: small channels that extend from one osteocyte to another;
they all get the same information
a. Osteocyte cell processes grow into the canaliculi and form gap
junctions
iii. Osteoclasts are responsible for bone removal/resorption
1. Monocyte derivatives; monocytes fuse making the osteoclasts multi-
nucleated cells
2. During bone development they are found along the surface of spicules
(pieces) of bone at sites where bone resorption is occurring.
3. Make acid & MMPs to break down the collagen
4. Make a tight connection with the piece of bone where everything will
be done
5. Typically osteoclasts will be making bone in one area while osteoblasts
break down bone in the other area
4. The types of bone development and their salient features
a.
5. The steps involved in the remodeling of mature bone during growth and during fracture
healing.
a.
6. The pathological conditions of cartilage and bone that are discussed
a. Arthritis: irreversible destruction of cartilage matrix (& sometimes adjacent bone)
through production of matrix metalloproteinases and enzymes that degrade cartilage
LIGHT MICROGRAPH OF NEWLY FORMING BONE
Bone with osteocytes
Osteoblasts and osteoid
Mesenchymal cells and blood vessels
proteoglycans (e.g. MMP1 cleaves certain fibrillar collagens, including Type I)
i. Osteoarthritis
1. Acquired from wear & tear
and/or injury
2. Joint pain, swelling, stiffness
3. Diagnosed radiographically by
bony changes (joint space
narrowing)
4. Osteoclasts are breaking down
the bone; all the cartilage is
gone and now even the bone is
being broken down
ii. Rheumatoid arthritis
1. System autoimmune, inflammatory disease
2. Chronic condition characterized by both joint inflammation and
destruction of bone and articular cartilage
3. The synovium is thought to play a major role in the destructive processes whereas in OA its role
is minor
a. Synovial hypertrophy (enlargement) is due to the influx of
monocytes and lymphocytes from the circulation, and from the
local proliferation of fibroblasts
b. In RA, the initial, and main cellular sources of the degradative enzymes are thought
to be the synovial lining cells and macrophages
c. In O.A. cartilage breakdown initially occurs at the articular surface itself
b. Herniated disc
i. Rupture of the annulus fibrosus (the fibrocartilage), which results in expulsion
of the gelatinous nucleus pulposus and a concomitant flattening of the disk
which can compress the nerve
ii. Fusing the vertebrae can help alleviate the pain
c. Osteogenesis Imperfecta
i. Vast majority of individuals with OI have mutations in one of the chains of
type I collagen.
ii. The mild forms are usually caused by mutations that result in a reduced
amount of normal type I collagen.
iii. The more severe forms result from mutations that produce structural defects in
the collagen molecule the most common being disruption of the helical
structure by substitution of a glycine residue every third residue of which
is required for formation of the collagen triple helix
d. Osteoporosis
i. Loss of calcium from the bone due to excessive production of parathyroid
hormone (hyperparathyroidism)
ii. Increased osteoclastic activity which causes an imbalance in skeletal
turnover, so that bone resorption exceeds bone formation
iii. Can be prevalent in post-menopausal women
e. Osteopetrosis
i. A genetic disorder that results from defective osteoclasts and is characterized
by dense, heavy bones.
ii. As bone resorption is defective this results in their overgrowth, thickening,
Histological Section showing cartilage destruction of a knee joint
due to osteoarthritis
and hardening.
iii. Also, the bone marrow cavities can be obliterated, depressing blood cell formation
Lectures #5 & #6 Epithelial Cells II Tissues
1. To learn to classify types of epithelia and to be able to cite examples of where they are
found in the body.
a.
2. To recognize structural specializations present within epithelia:
a. morphologically
b. functionally
c. biochemically
3. To understand how defects in epithelial specializations can affect epithelial integrity and
cause disease
a.
You might also like
- Student Clinical Report SheetDocument2 pagesStudent Clinical Report SheetMike100% (4)
- Brain 3Document3 pagesBrain 3Nurse Betty100% (1)
- Clinical Experience "Tips"Document5 pagesClinical Experience "Tips"ashdmb217No ratings yet
- Room: - Name: - Code Status: - AllergiesDocument2 pagesRoom: - Name: - Code Status: - Allergiesashdmb217No ratings yet
- Maxwell Quick Medical Reference PDFDocument35 pagesMaxwell Quick Medical Reference PDFAnonymous fj68Ms100% (10)
- Room: - Name: - Code Status: - AllergiesDocument2 pagesRoom: - Name: - Code Status: - Allergiesashdmb217No ratings yet
- Information Regarding Family History DocumentDocument9 pagesInformation Regarding Family History Documentashdmb217No ratings yet
- Nursing Management of The Perioperative PatientDocument16 pagesNursing Management of The Perioperative Patientashdmb217No ratings yet
- Nurse Brain Sheet Telemetry Unit SBARDocument1 pageNurse Brain Sheet Telemetry Unit SBARashdmb217No ratings yet
- SymbolsDocument1 pageSymbolsashdmb217No ratings yet
- Useful Spanish Words and PhrasesDocument32 pagesUseful Spanish Words and Phrasesashdmb217No ratings yet
- Exam 3 PathwaysDocument1 pageExam 3 Pathwaysashdmb217No ratings yet
- Adventitious Breath SoundsDocument1 pageAdventitious Breath Soundsashdmb217No ratings yet
- Medical TerminologyDocument13 pagesMedical Terminologyashdmb217No ratings yet
- Histology Exam 3 ReviewDocument7 pagesHistology Exam 3 Reviewashdmb217No ratings yet
- AbbreviationsDocument5 pagesAbbreviationsashdmb217No ratings yet
- HCP FormDocument8 pagesHCP FormMarkNo ratings yet
- Nutrition Review1.2Document12 pagesNutrition Review1.2ashdmb217No ratings yet
- Vitamin Chart.2Document3 pagesVitamin Chart.2ashdmb217No ratings yet
- Critical Care PhysiologyDocument287 pagesCritical Care Physiologyashdmb217100% (7)
- Histology Exam IV Review Part 2Document26 pagesHistology Exam IV Review Part 2ashdmb217No ratings yet
- Histology Exam IV Review Part 1Document36 pagesHistology Exam IV Review Part 1ashdmb217No ratings yet
- Nutrition Review 2.3Document10 pagesNutrition Review 2.3ashdmb217No ratings yet
- Starting Out - New in The ICUDocument30 pagesStarting Out - New in The ICUashdmb217100% (1)
- Exam IV ReviewDocument39 pagesExam IV Reviewashdmb217No ratings yet
- Exam 4 PathwaysDocument1 pageExam 4 Pathwaysashdmb217No ratings yet
- Exam 1 Study Guide.2Document52 pagesExam 1 Study Guide.2ashdmb217No ratings yet
- Biochem Exam 2 Review.2Document31 pagesBiochem Exam 2 Review.2ashdmb217No ratings yet
- Biochem Exam III Review.2Document24 pagesBiochem Exam III Review.2ashdmb217No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
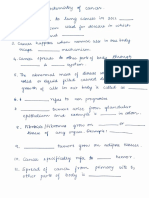
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Metastatic Vertebral Lesion Mimicking An Atypical Hemangioma WithDocument8 pagesMetastatic Vertebral Lesion Mimicking An Atypical Hemangioma Withsica_17_steaua6519No ratings yet
- Neet Wizz Bio Class 12Document89 pagesNeet Wizz Bio Class 12Aarthi T. UNo ratings yet
- Biochemistry of CancerDocument5 pagesBiochemistry of CancerManasa YNo ratings yet
- Blood Cell Morphology TutorialDocument176 pagesBlood Cell Morphology TutorialCharles Jebb Belonio JuanitasNo ratings yet
- Muscular System Study Guide 2015 AnswersDocument16 pagesMuscular System Study Guide 2015 AnswersLinet HuchuNo ratings yet
- HydrocephalusDocument40 pagesHydrocephalusAstrid Sabirin100% (1)
- Assisting A Normal Spontaneous Delivery ChecklistDocument3 pagesAssisting A Normal Spontaneous Delivery ChecklistPia CastilloNo ratings yet
- Bowel Obstruction Case StudyDocument11 pagesBowel Obstruction Case StudyFatimah Batool NawazNo ratings yet
- Medical AstrologyDocument2 pagesMedical Astrologyabhi16No ratings yet
- Glossary For BiologyDocument18 pagesGlossary For BiologyPershernNo ratings yet
- Pharmaceutical Sciences: ArticleinfoDocument8 pagesPharmaceutical Sciences: ArticleinfoMario CastroNo ratings yet
- Tinciones 10.1007@s00436-015-4554-4 PDFDocument6 pagesTinciones 10.1007@s00436-015-4554-4 PDFAxelWarnerNo ratings yet
- Neuroscience: Science of The Brain in NepaliDocument61 pagesNeuroscience: Science of The Brain in NepaliInternational Brain Research Organization100% (1)
- Tissue Repair 2016Document16 pagesTissue Repair 2016Luis AndradeNo ratings yet
- Connective TissueDocument62 pagesConnective Tissuehnm mnhNo ratings yet
- Sean Burke - Online Flatworm WebquestDocument5 pagesSean Burke - Online Flatworm Webquestapi-386190429100% (1)
- Medical NotesDocument421 pagesMedical NotesDanielle100% (7)
- Hemolytic Transfusion ReactionDocument3 pagesHemolytic Transfusion ReactionAinin SofiyaNo ratings yet
- Question Chapter 3 Nerve Fibers and Peripheral InnervationDocument20 pagesQuestion Chapter 3 Nerve Fibers and Peripheral InnervationTrang BuiNo ratings yet
- Transfusion in Emergency Room by DR Prannoy George, Department of Emergency Medicine, Amrita Institute of Medical Sciences, Kochi, KeralaDocument41 pagesTransfusion in Emergency Room by DR Prannoy George, Department of Emergency Medicine, Amrita Institute of Medical Sciences, Kochi, KeralaAETCM Emergency medicineNo ratings yet
- Cells Worksheet 2022Document2 pagesCells Worksheet 2022Mariah CampbellNo ratings yet
- Group No. Date Performed Name Date Submitted Facilitator ScoreDocument7 pagesGroup No. Date Performed Name Date Submitted Facilitator ScoreYancy BagsaoNo ratings yet
- Brain Understanding Interpretation of CT and MriDocument67 pagesBrain Understanding Interpretation of CT and MriStefan StefNo ratings yet
- Transport in HumansDocument1 pageTransport in Humansapi-3714421100% (1)
- Wound Healing: Ziv Peled, M.DDocument8 pagesWound Healing: Ziv Peled, M.Dapi-26007957No ratings yet
- Grade 9 CardioDocument16 pagesGrade 9 CardioJamoi Ray VedastoNo ratings yet
- Gynecology 2020 Copy 2Document620 pagesGynecology 2020 Copy 2school adressNo ratings yet
- Control and CoordinationDocument15 pagesControl and CoordinationHARSH AKSHIT (B15CS018)No ratings yet
- The Radiology Assistant - US of The GI Tract - TechniqueDocument7 pagesThe Radiology Assistant - US of The GI Tract - Techniqueابو عبد الرحمنNo ratings yet