Professional Documents
Culture Documents
The Impact of Pressure Ulcers
Uploaded by
Decky AndreaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Impact of Pressure Ulcers
Uploaded by
Decky AndreaCopyright:
Available Formats
THE IMPACT OF PRESSURE ULCERS
Todays term for these lesions is pressure ulcer, because this describes more accurately what has
happened to the skin and underlying structures, and why. In the past, they would have been
called bedsores, decubitus ulcers, decubiti, or pressure sores.
Recent figures indicate that 2.5 million patients are treated annually for pressure ulcers in acute
care facilities in the nited !tates "I#I, 2$$%&. The impact of pressure ulcers is staggering.
'irst and foremost, these wounds are very painful, thus causing patients a great deal of
suffering.
The anatomical location of the ulcer may result in a loss of dignity.
(uality of life is affected as the patient must alter activities to help heal the wound or
may face long)term hospitali*ation.
+ non)healing ulcer is at high risk for infection, which can be life)threatening.
lcer treatments may re,uire surgical procedures such as debridement, colostomies, and
amputations, which the patient would otherwise not have to face.
+n ulcer that heals forms scar tissue, which lacks the strength of the original tissue and is
more easily ulcerated again and again.
-ost importantly, the presence of a pressure ulcer increases the risk of death. .early
/$,$$$ hospital patients in the nited !tates are estimated to die each year from
complications due to hospital)ac,uired pressure ulcers "I#I, 2$$%&.
#ealthcare costs increase dramatically due to pressure ulcers. +n estimated 011 billion are spent
each year to treat pressure ulcers. The inpatient length of stay is 235 times longer for those with a
pressure ulcer. 4atients with either a primary or secondary diagnosis of pressure ulcer are
discharged to long)term care at 2 times the rate of other diagnoses "567., 2$1$&.
The nurses workload increases as now additional time and care must be provided to the patient
to manage and treat the ulcer8more dressing changes, more medications, more documentation.
9itigation may be brought against a hospital and its staff for neglect, malpractice, and elder
abuse if a patient develops a pressure ulcer while in the hospital. +wards can be in the millions
of dollars. +nd the bad publicity that follows will hurt the hospitals reputation and bottom line.
4ressure ulcers are now reportable to state and federal agencies. The information is placed in
databases that can be accessed by the public. These governmental agencies may levy fines
against the hospital for avoidable pressure ulcers. The 7enter for -edicare and -edicaid "7-!&
no longer pays a hospital for the additional care needed for a patient who develops a hospital)
ac,uired pressure ulcer "#+4&, but the hospital must provide the care nonetheless.
In the long)term care setting, the :oint 7ommission has made the prevention of healthcare)
associated pressure ulcers a ;2$11 .ational 4atient !afety <oal= ":oint 7ommission, 2$11&.
Thus, the prevention, assessment, and treatment of pressure ulcers are of ma>or importance to
nurses and other caregivers and to the healthcare facilities at which we practice.
RISK ASSESSMENT
The purpose of assessing the risk for developing pressure ulcers is so that interventions can be
implemented to prevent the formation of these ulcers.
Risk Assessment Schedules
Risk assessment should be performed when a patient is admitted to a healthcare setting. It should
be repeated on a regularly scheduled basis and?or when there is a significant change in the
patients condition, such as surgery or a decline in their health status "@4+4?.4+4, 2$$A&.
+ schedule for reassessing risk should be based on the acuity of the patient and knowledge on
when pressure ulcers are most likely to occur in a clinical setting. @very patient must be assessed
and reassessed, not >ust the ones who seem most likely to develop ulcers. Recommendations are
based on the healthcare setting are included in the boB below. "+ particular facility or setting
may have different regulations.&
In acute care, pressure ulcers usually develop within the first 2 weeks of hospitali*ation. @lderly
patients can develop pressure ulcers within the first week of hospitali*ation. In I7, ulcers can
develop within %2 hours of admission.
In both home health and long)term care settings, most pressure ulcers develop within the first C
weeks. In the hospice setting, most pressure ulcers occur within two weeks of death "567.,
2$1$&.
+!!@!!-@.T !7#@D9@! EF #@+9T#7+R@ !@TTI.<
Acute Care The initial assessment is done on admission and reassessment at least every 2C3CG
hours or whenever the patients condition changes. -ost I7s reassess each shift, while a med)
surg unit may reassess daily.
H!me Health The initial assessment is done on admission, and reassessment is done at
resumption of care, recertification, transfer or discharge, or whenever the patients condition
changes. !ome agencies reassess with each nursing visit.
L!n"#term Care In skilled facilities the initial assessment is done on admission and weekly
thereafter. In nursing homes with long)term patients, the assessment is done on admission,
weekly for the first month, then monthly thereafter, or whenever the patients condition changes.
!ourceH 567., 2$1$.
$eterminin" Risk Le%els
!everal risk assessment tools or scales are available to help predict the risk of a pressure ulcer.
They consist of several categories, with scores that when added together determine the total risk
score. The Eraden and .orton !cales are the most widely used for predicting pressure ulcer risk
in a variety of healthcare settings. These tools are used to help the clinician determine risk so that
interventions can be started promptly.
&RA$EN SCALE
The Eraden !cale consists of siB categories. !ensory perception, moisture, activity, mobility, and
nutrition are rated 13C. 'riction?shear is rated 132. The total score can thus range from /322. The
higher the score, the lower the risk.
-ild RiskH 1531G
-oderate RiskH 1231C
#igh RiskH 1$312
Iery #igh RiskH A or below
It is recommended that if other risk factors are present8such as age, fever, poor protein intact,
or diastolic blood pressure less than /$ mm #g8the risk level should be advanced to the neBt
level.
NORTON SCALE
The .orton !cale consists of five categories8physical condition, mental condition, activity,
mobility, and incontinence8that are rated 13 C, with a possible total score ranging from 5 to 2$.
-ild RiskH 1C
-oderate RiskH 12
#igh RiskH 12
It is important that when the clinician uses these scales, the scale must not be altered in any way,
meaning there cannot be shortcuts or changes to the definitions. +ny changes would alter the
accuracy and usefulness of the scale in predicting the risk of developing pressure ulcers.
Risk Fact!rs
7ertain groups of patients have a higher risk for developing pressure ulcers. These include
geriatrics, spinal cord in>ury, and critical care patients. 4atients over /5 years of age are at high
risk, and those over %5 are at even greater risk. Those who have fractured a hip or live in long)
term care facilities are at an increased risk for heel pressure ulcers. !pinal cord3in>ured patients
are at high risk for development and recurrence of pressure ulcers. !pasticity increases the risk of
skin breakdown, as does the eBtent of the paralysis, a younger age at onset, difficulty in
practicing good skin care, and a delay in seeking treatment or implementing preventive
measures. +s noted earlier, I7 patients can develop pressure ulcers within %2 hours.
+<I.< !JI. +.D 4R@!!R@ 97@R!
6bvious changes in both skin structure and function occur with aging. These changes contribute
to the occurrence of skin and wound problems.
'lattening of the epidermal)dermal >unction decreases the overall strength of the skin,
which increases the risk for skin tears and blistering.
Decrease in the melanocytes and 9angerhans cells increases the risk for allergic reactions
and sensitivity to sunlight.
Decreased blood flow decreases skin temperature.
Decreased production of oil and sweat contributes to dryness and flaking.
Decreased subcutaneous tissue, especially fat, decreases the bodys natural insulation and
padding.
Decline in the reproduction of the outermost layer of the epidermis may lead to the skins
inability to absorb topical medications.
These changes in skin structure and function, together with the risks that occur with a change in
overall health and functional ability, put the aged patient at very high risk for the formation of a
pressure ulcer.
There are other risk factors that may increase the chance of developing a pressure ulcer. -ore
than 1$$ of them have been reported "567., 2$1$&. These includeH
<eneral medical conditions, such as diabetes, stroke, multiple sclerosis, cognitive
impairment, cardiopulmonary disease, cancer, hemodynamic instability, peripheral
vascular disease, malnutrition, and dehydration
!moking
#istory of a previous pressure ulcer
Increased length of stay in a facility
ndergoing a long surgery
!ignificant weight loss
@mergency room stays
4rolonged time on a stretcher
-edications, such as sedatives and analgesics
Refusal of care
@dema
6besity
.ot turning the patient
'or patients in the I7H moisture problems, receiving norepinephrine, anemia, fecal
incontinence, and increased length of stay
'hat t! Assess
4revention of pressure ulcers must begin with fre,uent and routine assessment of the patients
skin and of the risk factors that, if left unmanaged, will contribute to the development of an ulcer.
SKIN
+ head)to)toe inspection of the skin should be done on admission and at least daily "or per
facility regulation&. It should focus on high)risk areas such as bony prominences. The specific
areas to assess are the occiput, sacrum, heels, and trochanters if the patient is bed)bound and the
ischial tuberosities and coccyB if the patient is chair)bound.
The 7enter for -edicare and -edicaid "7-!& recommends five parameters of skin assessmentH
skin temperature, skin color, skin teBture?turgor, skin integrity, and moisture status "567.,
2$1$&.
Elanchable erythema is a reddened area that temporarily turns white or pale when pressure is
applied with a fingertip. This is an early indication of pressure. .onblanchable erythema is
redness that persists when fingertip pressure is applied. It means that tissue damage has already
occurred.
It can be difficult to identify skin problems in patients with dark skin. Redness may not be easy
to see. The clinician needs to compare the at)risk area "such as the coccyB or hip& with skin neBt
to it and look for color differences or changes in temperature or pain.
!pecial garments or devices, such as shoes, heel and elbow protectors, splints, and others, must
be removed and the skin inspected at least daily. 4ressure ulcers have been caused by such
devices.
IMMO&ILIT(
Immobility is the most significant risk factor for pressure ulcer development. 4atients who have
some degree of immobility need more fre,uent monitoring to prevent pressure ulcers and include
those who areH
.onambulatory
7onfined to bed, chairs, wheelchairs, recliners, or couches for long periods of time
#ave paralysis and?or contractures
5ear orthopedic devices that limit function and range of motion
Re,uire assistance to ambulate, reposition themselves, or get out of bed and chairs
FRICTION AN$ SHEARIN)
'riction is the mechanical force of two surfaces moving across each otherK damage includes
blisters or abrasions. 4atients who cannot lift themselves during repositioning and transferring
are at high risk for friction in>uries. !hearing is the mechanical force that is parallel to the skin
and damages deep tissues like muscle. Tissues attached to the bone are pulled in one direction
while surface tissues remain in place. !hearing most commonly occurs when the head of the bed
is elevated and the patient slides downward.
INCONTINENCE
-oisture from incontinence can contribute to pressure ulcer development by macerating the skin
and increasing friction in>uries. 'ecal incontinence is even a greater risk for pressure ulcer
development than urinary incontinence because the stool contains bacteria and en*ymes that are
caustic to the skin. 5hen both urinary and fecal incontinence occur, the fecal en*ymes convert
the urea in the urine to ammonia, which raises the skins p#. 5hen the skin p# is elevated
"alkaline&, the skin is more susceptible to damage. 4ressure ulcers are C times more likely in
incontinent patients than those who are continent "567., 2$1$&.
NUTRITIONAL STATUS
+lthough individual nutrients and their specific role in preventing pressure ulcers have not been
determined, malnutrition is associated with overall morbidity and mortality. + nutritional
assessment should be done on admission and whenever there is a change in the patients
condition that would increase the risk of malnutrition.
HISTOR(
It is important to assess the history of a pressure ulcer or presence of a current ulcer. +ssessment
and regular monitoring of the pressure ulcer must be done on admission and at least weekly for
signs of skin or wound deterioration.
PRESSURE ULCER PRE*ENTION
+s the saying goes, ;an ounce of prevention is worth a pound of cure.= It is more cost efficient to
prevent a pressure ulcer than to cure one. Interventions that will help the clinician prevent
pressure ulcers do so from both an inside and outside approach. 'rom the outside, the clinician
can minimi*e pressure through regular repositioning, the use of a support surface, and managing
incontinence to prevent skin damage from moisture. The inside approach includes the
management of nutrition and hydration to support the body in preventing damage and healing
any damage that has occurred.
Re"ular Re+!siti!nin"
+s previously stated, immobility is the most significant risk for the development of pressure
ulcers. #igh pressures over bony prominences for a short time and low pressures over bony
prominences for a long time are e,ually damaging "@4+4?.4+4, 2$$A&. In order to decrease
the risk, it is important to reduce the time and amount of pressure the patient is eBposed to.
+ll patients must have their positions changed on a regular schedule. #ow often this is done is
determined by their own activity?mobility level, general medical condition, the overall treatment
plan, the condition of the skin, and the support surface being used.
&E$#&OUN$ PATIENTS
'or bed)bound patients, the standard ;turn every 2 hours= may be more than ade,uate for some
and not at all ade,uate for others. + patient needs to be repositioned more often on a standard
mattress than on a pressure)redistributing mattress. If the medical condition is so severe that
repositioning the patient regularly is not possible, then a support surface designed to decrease
pressure must be used.
5hen we think of turning the patient, we often think that the patient must be completely over on
a side. This can be difficult for the clinician?caregiver to do, is uncomfortable for the patient, can
result in cardio)pulmonary compromise, and actually increases pressure on the side of the body.
're,uent small position changes, rather than completely turning the patient, is faster, easier, and
safer for all. +ny change in position is beneficial. The patient need only be tilted to the side, no
more than 2$ degrees, with pillows or wedges to help support and reduce the pressure over bony
prominences. + small pillow behind the shoulder or the hip alters position without having to
move the entire body. Eending the knee alters the pressure on the sacrum and hip. + small pillow
behind the heel will elevate the heel off the surface and prevent pressure.
5hen a patient is moved, it must be done in a way as to prevent friction and shearing, as these
forces will cause skin in>ury as readily as pressure. +lways use a lift sheet or lift e,uipment to
reposition the patient. The patient must be lifted, not dragged, while repositioning, which also
means more than one person may be needed to move the patient. 4ulling or dragging the patient
will cause skin damage due to friction.
-aintain the head of the bed at or below 2$ degrees "or the lowest degree of elevation allowed
based on the medical condition& to prevent the body from sliding down and causing a shear)
related in>ury "567., 2$1$&. 9ower the head of the bed 1 hour after meals or intermittent tube
feedings. If this is not possible, the sacral region will need to be checked even more fre,uently
for possible in>ury.
#ave the patient assist in moving by using overhead trape*e bars. @ven if the patient can only
hold onto the bar, some of the weight will be reduced, making it easier and safer to move. +fter
the patient has been repositioned, be sure that he or she is not lying on a medical device, such as
tubes or drains, and make sure the linens are smoothed.
CHAIR#&OUN$ PATIENTS
+ chair)bound patient must be repositioned as well. 5hen a patient is seated, the weight of the
body causes the greatest amount of pressure to occur over the ischial tuberosities. !ince this area
of the body is relatively small, the amount of pressure will be highK without pressure relief, a
pressure ulcer will occur ,uickly. If the patient cannot sit upright but slouches in the chair, then
the sacral area is at risk as well.
Recommendations for the chair)bound patient includeH
!tand the patient and reseat them in the chair.
@levate the legs or place the feet on a stool if the feet do not reach the floor. This will
prevent sliding forward out of the chair.
@levate the feet and recline the chair by 2$ degrees to reduce pressure.
If the patient can change his?her own position, encourage pressure relief every 15
minutes. This includes chair pushups, leaning forward, leaning side to side, or tilting
backwards. 9eaning forward is the most effective and might be easier than chair push)
ups.
+cutely ill patients at risk for pressure ulcers should not sit for longer than 2 hours at a
time and not return to sitting for at least an hour.
4atients with eBisting pressure ulcers on the ischial areas should limit time sitting up in
the chair to 2 times a day for /$ minutes or less and they must use a cushion "gel or air
cushions are best& that redistributes pressure "567., 2$1$&.
4hysical and occupational therapists are of great importance in assessing and managing the
immobile patients activities and instructing staff, patients, and families in proper techni,ues to
avoid in>ury and prevent ulcers.
Su++!rt Sur,aces
There is no mattress or cushion that will eliminate pressure and relieve the clinician or caregiver
from having to turn the patient. 4atients must still be turned, no matter what surface is used.
!upport surfaces on beds and chairs are used, however, to more evenly distribute body)weight
pressure and to help reduce pressure to any one area of the body.
CHOOSIN) A SURFACE
Determining the appropriate support surface is based on the patients condition and the
healthcare setting. 6verall, if the patient is able to be turned and has at least two intact turning
surfaces, meaning the skin is intact on two sides of the body, then a mattress overlay or an
alternating pressure pad can be used over a regular mattress. If the patient has breakdown on
more than one side of the body, then a low3air loss mattress replacement should be used.
7ost and product availability must be considered in choosing a surface. The healthcare setting
will also determine the product used. 'or instance, in the home setting the weight of the bed, the
structure of the home, the width of the doors, and the availability of uninterrupted electrical
power will have a ma>or impact on the support surface available for use.
In general, an ordinary, standard hospital mattress should not be used with at)risk patients. Ee
sure to contact the medical e,uipment department to determine what is available for pressure
reduction "567., 2$1$&.
Do not use rings, foam cutouts, or donuts under the patient, as these concentrate pressure on
surrounding tissue, causing swelling and decreasing circulation.
TF4@! 6' !446RT !R'+7@!
Re+lacement mattressesH -attresses with pressure)reducing features placed on an
eBisting bed frame in place of at the standard mattress
O%erla-sH + support surface placed on top of a standard mattressK made of foam, water,
gel, air, or a combination
F!amH + thick slab of foam with a teBtured surface placed on top of a standard mattress
to reduce pressure by surrounding the bodyK should be at least 23C inches thick to be
effective at reducing pressure "2 inches is for comfort only&
'aterH + vinyl mattress or overlay with sections filled with water to distribute pressure
more evenly and create a flotation effect
)elH -ade of a thick fluid that conforms to the contours of the body
AirH + vinyl mattress or overlay inflated with a blower to reduce pressureK powered or
dynamic mattresses have a pump that inflates the mattress sections in an alternating cycle
L!./air l!ssH + mattress or overlay with controlled air)flow sections
Air#,luidi0edH ses a high rate of blown air to fluidi*e fine particulate material "such as
silicone beads& to ;float= the patient on the surface
ENSURIN) EFFECTI*ENESS
5ith the use of any support surface, the number of linens and other items used under the patient
must be kept at a minimum or the pressure)reducing ability of the surface will be altered
significantly. !taff, patients, and family members must be instructed to use no more than two
items between the patient and the surface, e.g., one pull sheet and one incontinence pad or
product.
The support surface must also be checked for ade,uate support to prevent ;bottoming out.= To
do this, place a hand "palm up& under the mattress or cushion below the area that is at risk "for
eBample, the sacrum or hip& and push up against the mattress. If less than 1 inch of support
material is felt, or if the body can be felt through the mattress, there is not enough support and
the support surface is either malfunctioning or not ade,uate for the patient and will need to be
replaced.
Regardless of the surface used, the patients heels must be floated off the bed using either a
pillow or a heel)lift device. The recommended position for the pillow is lengthwise under the calf
with the heel suspended in the air. The patient must be turned at regular intervals to promote
pulmonary, renal, and vascular function along with protecting skin integrity. 4added devices
such as synthetic sheepskin, bunny boots, or rigid splints protect the heels from friction and
shearing but do not relieve pressure. Devices such as an II bag, rolled towel, or sheet do not
redistribute pressure and can actually increase pressure "567., 2$1$&.
Mana"in" Inc!ntinence
!kin moisture from incontinence is a risk factor for pressure ulcer development. 5ater saturates
the skin, which increases the risk that friction and shearing will result in erosion of the skin. The
ammonia in urine raises the skins p#, which promotes growth of pathogenic bacteria, disrupts
the protective acid mantle, and activates fecal en*ymes. 'ecal en*ymes damage the skin,
allowing the gastrointestinal bacteria to cause infections. These result in a condition called
inc!ntinence ass!ciated dermatitis "I+D&. In and of itself, I+D is not a pressure ulcer. Eut if
unrelieved pressure is added to I+D, the odds are 5 times higher that a pressure ulcer will
develop. 4roper cleansing and protection of the skin are the basis of prevention of I+D "<ray, et
al, 2$$%&.
7leanse the skin gently at each time of soiling with a p#)balanced cleanser. 4erineal skin
cleansers are more effective for prevention and treatment of I+D than traditional soap and water.
This is because bar soap is alkaline and very drying to the skin, which disrupts its protective
abilities. Iigorous cleaning as well as the use of rough washcloths can also lead to skin erosion.
!oft, disposable cloths are easier on the skin. 7leaning products with fragrance or alcohol should
be avoided, as these are irritants. !ome facilities use no)rinse foams, and these are also a good
option.
+n incontinence skin barrier product should be used to protect the skin after cleansing. 4roducts
such as creams, ointments, pastes, or those that form a film on the skin are all useful. 4rotective
products with dimethicone, petroleum, or *inc oBide are recommended for patients with fecal
incontinence or both urinary and fecal incontinence to protect against I+D. !everal
manufacturers offer products that both clean and protect, which can save time and make perineal
care easier for the caregiver and more likely that it will be done each time.
!elect underpads or incontinence briefs that are absorbent to wick moisture away from the skin
instead of those that trap the moisture against the skin. #owever, all briefs increase moisture at
the perineal region because they are occlusive and do not ;breathe.= This creates warmth near the
skin that, when combined with moisture, ammonia, and en*ymes, increases skin breakdown.
There is an increased risk with the use of briefs because they may not be changed as often as
they should be due to the difficulty in seeing when a patient has voided. Eriefs are not
recommended for fecal incontinence because they can trap stool against the skin.
-any hospitals have moved away from using briefs eBcept when a patient is ambulating or going
off of the ward. Instead, they use underpads that wick and hold fluid away from the skin, do not
trap heat and moisture neBt to the body, and can readily be seen when they need to be changed.
+ toileting program can also decrease incontinence and thus I+D. 'or those patients with
significant fecal output, a pouching system or fecal containment device may be necessary to
protect the skin from the effluent. In situations where the severity of urinary incontinence has
contributed to or may contaminate an eBisting pressure ulcer, an indwelling catheter may be
indicated "567., 2$1$&.
Nutriti!n Mana"ement
-alnutrition is associated with overall morbidity and mortality. Thus, assessing the patients
nutritional status must be part of the total assessment. The assessment should be performed upon
admission to a new healthcare setting and whenever there is a change in the patients condition
which puts them at risk for under)nutrition.
.TRITI6. +!!@!!-@.T 4+R+-@T@R!
7urrent weight and usual weight
#istory of unintentional weight loss or gain "greater than 5L change in 2$ days or greater
than 1$L change in 1G$ days&
Eody mass indeB "E-I&
'ood intake
Dental health
+bility to chew, swallow, and feed oneself
-edical and?or surgical history that influence intake or absorption of nutrients
Drug?food interactions
4sychosocial factors that can affect food intakeH
+bility to obtain and pay for food
'acilities for cooking and eating
'ood preferences
7ultural and lifestyle influences on food selection
+dvanced age
The patient should be monitored for signs of dehydration, such as decreased skin turgor and?or
urine output or elevated serum sodium. !erum protein tests, such as for albumin and pre)
albumin, may be affected by inflammation, renal function, and hydration and so may not
correspond with overall nutritional status. Thus, laboratory tests should be considered as only
one part of the nutritional assessment.
5hile there is evidence that ade,uate nutritional support for stage III and II pressure ulcers is a
strong predictor of pressure ulcer healing and that support with high protein can significantly
reduce the risk of pressure ulcers, there is no evidence to support that specific supplements
promote the healing of ulcers. !tudies that show support are small and more research needs to be
done "567., 2$1$&.
+ny patient with nutritional and pressure ulcer risks, suspected or identified nutritional
deficiencies, or a need for nutritional supplementation to prevent undernutrition should be
referred to a registered dietician. +ny patient with a pressure ulcer should be referred to a
dietician as well "567., 2$1$&.
$EFININ) AN$ STA)IN) PRESSURE ULCERS
6ver the years the definition of a pressure ulcer has been refined, most recently in 2$$A. +
pressure ulcer is now defined as ;a locali*ed in>ury to the skin and?or underlying tissue usually
over a bony prominence, as a result of pressure, or pressure in combination with shear and?or
friction= "@4+4?.4+4, 2$$A&.
7ommon terms for pressure ulcer include bedsore, decubitus ulcer, pressure sore, and pressure
ulcer. The terms bedsore and decubitus ulcer originated from the notion that to develop ulcers a
person needed to be bedridden, which we now know is not the case. lcers can develop when a
patient constantly maintains any positionK conse,uently the term pressure ulcer most accurately
describes an ulcer from pressure.
The compression of soft tissue interferes with the tissue blood supply, leading to vascular
insufficiency, tissue anoBia, and cell death. 4ressure ulcers usually occur over bony prominences
such as the sacrum, ischium, heel, and trochanter, where there is less tissue to compress. 6ther
factors previously mentioned also contribute to the tissue breakdown. 4ressure ulcers can
develop within 2C hours of the initial pressure but take as long as 5 days to present themselves.
Sta"es
4ressure ulcers are staged to classify the degree of tissue damage that is present. The staging
system was originally created in 1A%5 as a means to describe the amount of anatomical tissue
loss in a pressure ulcer. The use of stages in pressure ulcer assessment is a way to classify the
amount and type of tissue destroyed based on anatomic depth. #aving and using a common
classification system allows all clinicians a way of communicating accurately what is wrong. It is
only used to describe pressure ulcers, not other wounds.
The most recent definition of the stages from the .ational 4ressure lcer +dvisory 4anel
"@4+4?.4+4, 2$$A& is as followsH
STA)E I
+ !tage I pressure ulcer is defined as intact skin with nonblanchable redness of a locali*ed area,
usually over a bony prominence. Darkly pigmented skin may not have visible blanchingK its
color may differ from the surrounding area. The area may be painful, firm, soft, warmer, or
cooler as compared to ad>acent tissue.
+ blanchable redness means that when the red area is compressed by the finger, the area turns
white or pale and the redness returns when the pressure is released. .onblanchable redness
means the area under the finger remains red as it is compressed. .onblanchable redness indicates
that tissue damage has already occurred. "!ee figure.&
Sta"e I Pressure Ulcer
"!ourcesH MillustrationN O .ational 4ressure lcer +dvisory 4anel, used with permissionK MphotoN
O 5ound, 6stomy and 7ontinence .urses !ociety "567.&, used with permission.
STA)E II
+ !tage II pressure ulcer refers to partial thickness loss of dermis presenting as a shallow open
ulcer with a red pink wound bed, without slough. It may also present as an intact or
open?ruptured serum)filled blister or as a shiny or dry shallow ulcer without slough or bruising.
"Eruising indicates deeper tissue in>ury.&
This stage should not be used to describe skin tears, tape burns, perineal dermatitis "incontinent
associated dermatitis&, maceration, or eBcoriation. P4artial thicknessP means that the damage is
confined to the epidermis and?or dermis but does not penetrate below the dermis. "!ee figure.&
Sta"e II Pressure Ulcer
"!ourcesH MillustrationN O .ational 4ressure lcer +dvisory 4anel, used with permissionK MphotoN
O 5ound, 6stomy and 7ontinence .urses !ociety "567.&, used with permission.&
STA)E III
+ !tage III pressure ulcer includes full)thickness tissue loss. !ubcutaneous fat may be visible,
but bone, tendon, or muscle are not eBposed. !lough may be present but does not obscure the
depth of tissue loss. It may include undermining and tunneling.
The depth of a !tage III pressure ulcer varies by anatomical location. The bridge of the nose, ear,
occiput, and malleolus do not have subcutaneous tissue, and !tage III ulcers here will be shallow.
In contrast, areas of significant fat deposits can develop eBtremely deep !tage III pressure ulcers.
Eone and?or tendon is not visible or directly palpable. P'ull thicknessP means the damage
eBtends completely through the dermis to the subcutaneous layer. !lough is a soft, moist,
avascular. "!ee figure.&
Sta"e III Pressure Ulcer
"!ourcesH MillustrationN O .ational 4ressure lcer +dvisory 4anel, used with permissionK MphotoN
O 5ound, 6stomy and 7ontinence .urses !ociety, used with permission.&
STA)E I*
+ !tage II pressure ulcer involves full)thickness tissue loss with eBposed bone, tendon, or
muscle. !lough or eschar may be present on some parts of the wound bed. It often includes
undermining and tunneling.
The depth of a !tage II pressure ulcer varies by anatomical location. The bridge of the nose, ear,
occiput, and malleolus do not have subcutaneous tissue, and !tage II ulcers here will be
shallow.
!tage II ulcers can eBtend into muscle and?or supporting structures, such as fascia, tendon, or
>oint capsule, making osteomyelitis possible. @Bposed bone or tendon is visible or directly
palpable. "!ee figure.&
Sta"e I* Pressure Ulcer
"!ourcesH MillustrationN O .ational 4ressure lcer +dvisory 4anel, used with permissionK MphotoN
O +ssociation for the +dvancement of 5ound 7are "++57&, used with permission.&
The .4+4 has also described two additional categories of pressure ulcerH suspected deep tissue
in>ury and unstageable "@4+4?.4+4, 2$$A&.
SUSPECTE$ $EEP TISSUE IN1UR(
Deep tissue in>ury may be indicated by a purple or maroon locali*ed area of discolored intact
skin or a blood)filled blister due to damage to the underlying soft tissue from pressure and?or
shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer, or cooler
as compared to ad>acent tissue. Deep tissue in>ury may be difficult to detect in individuals with
dark skin tones. Its evolution may include a thin blister over a dark wound bed. The wound may
further evolve and become covered by thin eschar. @volution may be rapid, eBposing additional
layers of tissue even with optimal treatment. "!ee figure.&
Sus+ected $ee+ Tissue In2ur-
"!ourcesH MillustrationN O .ational 4ressure lcer +dvisory 4anel, used with permissionK
MphotosN O +ssociation for the +dvancement of 5ound 7are "++57&, used with permission.&
UNSTA)EA&LE
+ pressure ulcer is considered unstageable in the case of full thickness tissue loss in which the
actual depth of the ulcer is completely obscured by slough "yellow, tan, gray, green, or brown
tissue& and?or eschar "tan, brown or black tissue& in the wound bed. ntil enough slough and?or
eschar are removed to eBpose the base of the wound, the true depth cannot be determinedK
however it will be a !tage III or II, as slough and?or eschar do not form in !tage I or II ulcers.
!table eschar "dry, adherent, intact without erythema or fluctuance& on the heels serves as the
bodys natural or biological cover and should not be removed. "!ee figure.&
Unsta"ea3le Pressure Ulcer
"!ourceH MillustrationN O .ational 4ressure lcer +dvisory 4anel, used with permissionK MphotoN
O +ssociation for the +dvancement of 5ound 7are "++57&, used with permission.&
Re%erse Sta"in"
The term reverse staging came about in the 1AG$s as a way of describing improvement in an
ulcer. #owever, this term does not accurately describe what is physiologically occurring in the
ulcer. Eecause staging is used only to describe the amount and type of tissue destroyed based on
anatomic depth, it cannot be used to describe healing.
+s a pressure ulcer heals it does decrease in depth, but the body does not replace the lost bone,
muscle, subcutaneous fat, or dermis. Instead, the full)thickness ulcer is filled with granulation, or
scar tissue, and then covered with new epithelium. @ven a partial)thickness !tage II ulcer does
not return to the nonblanchable redness of a !tage I ulcer. + !tage II pressure ulcer that has
closed should be classified as a closed !tage II pressure ulcer and not as something like a ;!tage
6= pressure ulcer "which does not eBist&.
The progress of healing a pressure ulcer can only be documented using wound characteristics
"decrease in length, width, depth, odor, drainage, pain, etc.& or using a validated pressure ulcer
healing tool. If a pressure ulcer reopens in the same anatomical site, the ulcer resumes the
previous staging diagnosis8once a !tage II, always a !tage II "@4+4?.4+4, 2$$A&.
7urrent federal regulations re,uire long)term care facilities to reverse stage at the present time
for coding the -inimum Data !et "-D!&. ntil the -D! is revised, reverse staging must be
used for completion of the Resident +ssessment Instrument. #owever, clinicians are urged to
document healing using either descriptive characteristics of the wound or a validated tool such as
the .4+4 4ressure lcer !cale for #ealing "4!#& tool to document pressure ulcer healing.
This tool documents pressure ulcer healing that is consistent with the healing process ".4+4,
2$1$&.
PRESSURE ULCER TREATMENT
Treating a pressure ulcer involves all of the activities used in preventing a pressure ulcerH the
proper pressure)reducing surface, repositioning the patient correctly and fre,uently, maintaining
intact skin, and improving nutrition. 5hile these interventions are being put into place, the
treatment of the wound itself begins. There are basic wound care principles that can be used in
deciding which treatments will be the best for the wound and for the patient. 're,uent
reassessment of the wound and its response to the treatment is re,uired, as well as eliminating or
reducing the factors that inhibit wound healing.
Pressure Reducti!n
6f all the interventions that must be done to heal the ulcer, pressure reduction measures are the
most important. !imply put, the wound will not heal unless the pressure is removed. Trying to
heal a pressure ulcer without reducing the pressure is like trying to heal a stab wound with the
knife still in it. Fou might get some improvement, but the wound will never heal because the
primary cause has not been removed.
Repositioning and turning must be done regularly and fre,uently. 'riction and shear must be
prevented or a small ulcer will ,uickly turn into a large one with undermining and tunneling. The
right support surface for the bed or the chair must be obtained and used. -anagement of
incontinence will keep skin from getting worse. 5hile outside impediments to healing are being
managed, the inside impediments can be attended to through proper nutrition and by reducing
other factors that affect healing. Dietician consult is always appropriate when treating a pressure
ulcer.
Uni%ersal Princi+les !, '!und Mana"ement
The ob>ect of treatment is to reproduce "to the best of ones ability& the normal environment of
the eBposed tissue of the wound. The normal environment of all tissue and cells, with the
eBception of the epidermis, is warm, dark, moist, and protected. In order to heal any wound,
including pressure ulcers, some basic principles need to be followed. These areH
Remove necrotic tissue
Treat infection
'ill dead space
-aintain moist wound environment
4rotect the wound from infection, trauma, and cold
!ome of these principles will re,uire medical interventionK others, good clinical care. Ey
following these principles, caregivers will provide the wound with the environment it needs to
heal.
REMO*IN) NECROTIC TISSUE
Removing necrotic tissue is the critical first step when healing the ulcer is the goal. Ey removing
dead tissue, bacteria and the risk for infection are decreased as well as drainage and odor.
Removing these materials may also contribute to the release of available growth factors in the
wound, thus allowing the cells to multiply and heal the wound.
The removal of necrotic tissue is called debridement, of which there are several types. The most
appropriate type of debridement will depend on the patients overall condition and goals of care.
'actors to consider include the status of the ulcerK the type, ,uantity, and location of the necrotic
tissueK the presence or absence of infectionK pain toleranceK the care settingK and professional
accessibility "@4+4?.4+4, 2$$A&.
Sur"ical
4erformed by a surgeon at the bedside or in the operating room, this is the ,uickest way to
remove eBtensive necrotic tissue, undermining, and tunneling. #owever, the benefits of surgical
debridement may outweigh the risks in the presence of advancing cellulitis, crepitus, fluctuance,
and?or sepsis secondary to ulcer)related infection. Relative contraindications would include
anticoagulant therapy, bleeding disorders, and immune incompetence. If the necrotic ulcer is on a
limb, a thorough vascular assessment should be done prior to debridement to rule out arterial
insufficiency. The .4+4 "@4+4?.4+4, 2$$A& recommends against debridement of stable,
hard, dry eschar in ischemic limbs.
!harp debridement, as opposed to surgical debridement, may be performed by specially trained,
competent, ,ualified, and licensed healthcare professionals consistent with local legal and
regulatory statutes. !harp debridement removes only loose, easily identifiable necrotic tissue.
Aut!l-tic
This method allows the body to break down necrotic tissue by using its own en*ymes and
defense mechanisms. This is done with the use of occlusive dressings such as hydrocolloids and
films. These dressings help maintain a moist wound environment, reduce pain, and provide a
barrier to infections. The dressing is left on for a few days, allowing the accumulation of fluids
and en*ymes at the site. The dressing is removed, the wound cleansed, and new dressing applied.
This method takes time but is effective.
Chemical
This method involves the use of en*yme debriding agents. These breakdown necrotic tissue
without affecting viable tissue. The en*yme product is applied daily to the necrotic tissue then
covered by a dressing. @n*ymes are by prescription only, and currently only one is available on
the market.
&i!sur"ical
This method uses sterili*ed bottlefly maggots, which debride the wound by dissolving dead and
infected tissue with their digestive en*ymes "in other words, the maggots eat the dead tissue&.
The maggots also disinfect the wound by killing bacteria. This in turn stimulates the growth of
healthy tissue. "'or further information, see ;Resources= at the end of the course.&
Mechanical
-echanical debridement utili*es physical forces to remove necrotic tissue. The most common
are the use of wet)to)dry dressings and high)pressure wound irrigation. "se of whirlpools has
fallen out of favor due to the difficulty in assuring the e,uipment is free of pathogens before its
use on the neBt patient&. #igh)pressure wound irrigation is done with commercially available
devices such as pulsatile lavage units. + lower)pressure method to debride tissue is to use a 25)
ml syringe with a 1A)g needle, held a few inches from the wound. 7are must be taken to
minimi*e splashing and eBposure to wound drainage, and infection control precautions should be
followed.
The use of wet)to)dry dressings is no longer recommended. In this method, wet gau*e is applied
to the wound, and necrotic tissue is allowed to dry and then forcibly removed without re)wetting.
The gau*e will have stuck to the necrotic tissue, thus removing it when the gau*e is removed.
#owever, this method is nonselective in that healing tissue will also be removed, thus re)
traumati*ing the wound bed and causing significant pain.
TREATIN) INFECTION
Infection is not common is !tage I or II ulcers, so the focus for assessment of infection is on
!tage III and II ulcers. 4ressure ulcers that are infected may eBhibit subtle signs of infection8
such as new or increased pain, delayed healing, poor or friable granulation tissue, discoloration
of wound bed tissue, a change in odor, increased serous drainage, induration, or pocketing8
before the classic signs of infection occur. There should be a high suspicion for the likelihood of
infection in ulcers with necrotic tissue, those that have been present for a long time, those large
in si*e, or those repeatedly contaminated, such as those near the anus.
9ook for local infection in ulcers that have no signs of healing after 2 weeks of treatment. +n
acute infection may be present if there is redness eBtending from the ulcer edge, warmth,
purulent drainage and odor, increase in si*e of the ulcer, and increase in pain. !ystemic
symptoms such as fever and malaise may develop. The elderly may develop confusion and
anoreBia. There must also be a high suspicion for the likelihood of infection in patients who have
diabetes, malnutrition, hypoBia, autoimmune disease, or immunosuppression.
The gold standard method of determining wound infection is a by a culture of tissue obtained by
biopsy. #owever, an acceptable alternative to a tissue culture is a swab culture obtained by the
9evine techni,ue "@4+4?.4+4, 2$$A&.
9@II.@ T@7#.I(@ '6R 56.D 79TR@
7leanse wound with sterile normal salineK blot dry with sterile gau*e
7ulture the healthiest)looking tissue in the wound bed
Do not culture drainage, pus, necrotic tissue, or fibrous tissue
Rotate the end of a sterile alginate)tipped applicator over a 1 cm by 1 cm area for 5
seconds
+pply sufficient pressure with the swab to cause tissue fluid to be eBpressed
!end specimen to the lab
If the culture indicates infection, consider a two)week course of topical anti3i!tics. 7onsider
systemic antibiotics if bacteremia, sepsis, advancing cellulitis, or osteomyelitis has occurred.
!ystemic antibiotics cannot reach necrotic tissue, so topical antibiotics are recommended in
addition to systemic "@4+4?.4+4, 2$$A&.
!ilver) and honey)impregnated dressings are an option for ulcers infected with multiple
organisms because these dressings offer broad antimicrobial coverage. Ee sure the patient is not
allergic to honey or to bees before using a honey dressing.
Topical antise+tics such as providone iodine, Dakins solution, or acetic acid that are properly
diluted may be used for a limited time to control the bacterial burden, clean the ulcer, and reduce
surrounding inflammation. 6nce the wound is clean, these products should be discontinued, as
they can be damaging to healthy tissue. These products can also be used to control bacteria,
drainage, and odor in wounds that are not eBpected to heal, such as in a terminally ill patient
"@4+4?.4+4, 2$$A&.
Cleansin" the wound will also reduce the risk of infection. The ulcer and the surrounding skin
must be cleansed at each dressing change. The cleansing method should provide enough pressure
to removed debris yet not enough to cause trauma to the wound bed. Techni,ues for cleansing
may include irrigation, gently swabbing the wound, or showering. 4ressure ulcers that are
healing may be cleansed with water. It can be tap water, distilled water, cooled boiled water, or
saline. +void using cleansing products that are designed for use on intact skin, and avoid
cleaners that are designed to remove fecal materialK both of these can be toBic to a wound. 5hen
the wound has a lot of drainage or debris, a commercial wound cleanser may be used. Those that
contain surfactants can help remove wound contaminants "567., 2$1$&.
FILLIN) $EA$ SPACE AN$ MAINTAININ) A MOIST EN*IRONMENT
5ound dressings are a central component of pressure ulcer care. The selection of the dressing for
the ulcer is very important and based on many parameters, such as "567., 2$1$&H
4resence of infection or necrosis
!i*e, depth, and presence of undermining or tunneling
9ocation
Drainage
7ondition of the surrounding skin
<oals for healing
Individual or caregiver needs, such as pain reduction or odor control
7ost?reimbursement of the dressing
+vailability
@ase of use
-aintaining a moist wound is a primary factor in dressing selection. If the ulcer is draining a
large amount, then a dressing that will absorb but not dry out the wound is needed. If the ulcer
has minimal drainage, then a dressing that replaces moisture and?or doesnt allow the ulcer to dry
out is needed.
The ;dead= space inside the wound needs to be filled so that the dressing is in contact with the
wound bed, including any tunneling or undermining. Do not stuff the wound with the dressing
materialK stuffing the wound puts pressure on the inside of the wound and will prevent eBudate
from draining out.
Dressings are changed based on the amount of drainageH a heavily draining wound will need to
be changed often, while a minimally draining wound can be changed less than daily. There are
many dressings available today to help maintain the correct environment to allow healing.
'ollow manufacturer recommendations for the use of the product "567., 2$1$K
@4+4?.4+4, 2$$A&.
TF4@! 6' DR@!!I.<!
H-dr!c!ll!id "e.g., Duoderm&H + type of dressing containing gel)forming agents applied
to a foam or a film, which form an absorbent, self)adhesive, waterproof occlusive wafer.
These are used in !tage II ulcers in body areas where they will not roll or melt. They are
also used for autolytic debridement. @Bpect the formation and?or collection of drainage
under the wafer. This does not indicate infection but is a property of the product. Do not
use on infected or heavily draining wounds or wounds in which the dressing needs to be
changed more than 2 times per week. Remove carefully.
Trans+arent FilmH 7an be used to protect body areas at risk for friction in>ury. 7an be
used for autolytic debridement. -ay be used as a secondary dressing to hold in other
dressings. Remove carefully.
H-dr!"elH + water)based, non)adherent gel. !ome hydrogel)based dressings have the
ability to absorb eBcess drainage while providing moisture to dry necrotic tissue or
slough. <enerally, these dressings are used on shallow, minimally draining ulcers. They
are covered with a secondary dressing.
Al"inateH These are used in moderately and heavily draining ulcers. 7over with a
secondary dressing.
F!amsH sed in draining !tage II and shallow !tage III ulcers. They absorb drainage and
protect the wound.
Sil%er#im+re"nated $ressin"sH +n antimicrobial dressing used in ulcers that are infected
or at high risk for infection. The silver is incorporated into foam, alginate, and other
dressings. 7onsider discontinuing use when infection is controlled. 7an turn tissues a
dark color. Do not use in patients allergic to silver.
H!ne-#im+re"nated $ressin"sH -anuka honey is used for antimicrobial effects and can
be effective on antibiotic)resistant bacteria while promoting healing. se in !tage II and
III ulcers. Do not use in patients allergic to bees or honey.
Cade4!mer I!dineH +n antimicrobial dressing that absorbs drainage and matter from the
wound surface, and, as it becomes moist, iodine is released. sed in moderately to highly
draining wounds. Do not use in patients with iodine sensitivity or thyroid disease.
Difficult to use in large cavity wounds.
)au0e $ressin"sH + cotton or synthetic weave that is absorptive and permeable to water,
water vapor, and oBygen. <au*e may be impregnated with petrolatum, antiseptics, or
other agents. <au*e should not be used in clean ulcers, as they are labor)intensive to use,
cause pain when removed if dry, and will dry out a wound. #owever, if no other dressing
is available, the use of gau*e that is kept continually moist is preferable to dry gau*e.
-oist gau*e can be used to loosely fill a cavity wound and one with undermining and
tunneling.
Ne"ati%e Pressure '!und Thera+- 5NP'T6H The use of .45T has been associated
with increased rates of healing in !tage III and II pressure ulcers. .ecrotic tissue must
be debrided prior to using .45T. 'ollow manufacturers guidelines for use.
-any of the advanced dressings do not need to be changed daily, which can reduce pain, time,
and eBpense. 'ollow manufacturer directions.
PROTECTIN) THE 'OUN$ FROM INFECTION7 TRAUMA7 AN$ COL$
4rotecting the wound from infection, trauma, and cold can be done through the proper cleansing
and dressing of the wound. +s a wound heals and the drainage decreases, choose a dressing that
does not have to be changed often. @very time a dressing is removed and the wound cleansed,
the temperature of the wound bed drops to room temperature. The body then must eBpend energy
to bring the wound bed back to body temperature so that cell repair and growth can continue.
This can take several hours. 9ess fre,uent dressing changes aid the wound in healing by giving it
time to do so. 4rotecting the wound from trauma includes the proper support surface, protection
from incontinence, and the use of dressings that do not need to be changed fre,uently.
MONITORIN) RESPONSE
!tage I and II pressure ulcers should show evidence of healing within 132 weeks, and !tage III
and II ulcers should show evidence of healing within 23C weeks. This means that if after 2
weeks of treatment, no healing is detected, then the wound, the patient, and the plan of care need
to be reevaluated.
5ith each dressing change, the ulcer is observed for anything that may indicate the need for a
change in treatment8e.g., improvement or deterioration, more or less drainage, signs of
infection, or other complications. +ny signs of deterioration should be addressed immediately.
The type of dressing may need to be changed based on this assessment.
Healin" Assessment T!!ls
There are tools that have been developed that can be used to assess pressure ulcer healing. The
&ates#1ensen '!und Assessment T!!l "E5+T& is comprised of fifteen items, of which
thirteen are scored from 135. The total scores and dates of assessment can be plotted on a graph,
which provides an indeB of improvement or deterioration of the wound.
+nother tool is the PUSH tool "4ressure lcer !cale for #ealing&, which was developed by
.4+4. +n ulcer is categori*ed using numerical scores of $35 according to surface area "length
times width&, drainage amount, and tissue type. + comparison of the total scores measured over
time provides an indication of improvement or deterioration in the ulcer.
-any computer systems also have programs to monitor ulcer progress. 6f course, the clinician
will also use clinical >udgment to assess signs of healing, such as a decrease in the amount of
drainage, pain, and wound si*e, and an improvement in wound bed tissue. The clinician can also
use photography, comparing baseline and serial photographs to monitor healing over time.
'ollow facility policy on the use of photography.
Fact!rs That A,,ect '!und Healin"
If the choice of wound care is appropriate and pressure is being relieved, then the patient needs
to be reassessed for reasons why the ulcer is not improving. 6ne systematic approach to
determining which factors might be affecting wound healing utili*es the acronym DIDNT
HEAL. sing this acronym and correcting those factors that can be corrected will aid in healing
the ulcer. If factors cannot be corrected, healing the ulcer may not be possible.
DID.T #@+9
Cause $escri+ti!n Additi!nal Fact!rs
!ourceH !tillman, 2$1$.
$iabetes
9ack of diabetic control affects wound
healing by causing diminished cardiac
output, poor peripheral perfusion, and a
decrease in the ability of 5E7s to
function
'asting blood sugar greater than G$3
12$ mg?dl
+17 greater than /.5L
Infection
Increases the destruction of collagen
needed for repair
6verwhelms body defenses
$rugs 7an impair collagen synthesis
!teroids
7hemotherapy "high risk for
infection?malnutrition&
Immunosuppressants "interfere with
healing&
Nutrition
Deficiencies impair normal wound
healing
Diet lacks ade,uate calories,
protein, vitamins
6bese patients not necessarily well)
nourished
Tissue
necrosis
Impairs wound healing due to lack of
oBygen
7ell death as a result of all the
factors
HypoBia Inade,uate tissue oBygenation
6
2
saturation less than A2L
+nemia
4oor circulation
7omorbid conditions such as heart
failure, pneumonia, 7I+
4ain
EBcessive Tension on wound edges leads to local 5hen the patient is moved, wound
DID.T #@+9
Cause $escri+ti!n Additi!nal Fact!rs
tension tissue ischemia and necrosis is pulled
Another
wound
7ompetition for all the factors needed
for wound healing impairs wound
healing at all sites
Increased nutritional needs
Low
temperature
'urther deceases oBygen to the wound
4oor circulation
se of cold cleansing solutions
're,uent dressing changes that
cause wound temperature to drop to
room temperature
$eterminin" the Need ,!r Sur"ical Inter%enti!n
+ patient with a !tage III or II ulcer may be evaluated for the need for operative repair for an
ulcer that has not responded to conservative medical treatment. 4rior to surgery the patient
should be in an optimal state both mentally and physically, and factors that impair healing should
be minimi*ed. The patients ability to tolerate the surgery and participate in the postoperative
rehabilitation must be assessed prior to any surgery. !ome patients may not be surgical
candidates due to malnutrition, immobility, poor compliance with treatment, or other chronic
diseases.
6perative procedures may include skin grafts or flaps "surgical reconstruction&. 5hich option is
available may be limited due to previous surgeries, a shortage of available tissue to use, and
impaired blood supply. Immediately after surgery, the operated region must be totally offloaded.
6nce the surgical incision has healed, the patient will be allowed to gradually apply pressure to
the area.
Rates of surgical complications and recurrence rates are high. 7omplication rates have been
reported as high as CAL. 6steomyelitis is the ma>or cause of breakdown after surgery "567.,
2$1$&.
$!cumentin" the '!und Status
The very basics of documentation are to document what was observed, what was done "including
education provided&, and how the patient responded. Documentation for pressure ulcer
management includes an assessment of the ulcer on admission and at least weekly "or per agency
regulations& for any signs of skin and?or wound deterioration, along with documentation of risk
assessment and patient?family education provided. The following is also documentedH
6nset, course, and duration of the ulcer
Description of the ulcer
4ainH location, intensity, ,uality, onset, duration, alleviating?aggravating factors
4atient?caregivers ability and willingness to adhere to the prevention and treatment
program
The description of the ulcer includes the physical characteristics of the ulcer itself and of at least
C cm of the surrounding tissue "#ess, 2$$5&. The following should be included in the
documentation of any woundH
56.D D@!7RI4TI6.
Cate"!r- $escri+ti!n
+natomic 9ocation
Describe where on the body the wound is, including the
nearest bony prominence or anatomic landmark. Descriptors
such as anterior-posterior, medial-lateral, proximal-distal can
clarify location.
!tage se the staging definitions described above.
Drainage or
@Budate
+mount
9ight or scant
-oderate
#eavy or large
7opious
7olor
!erous "clear, watery plasma&
!anguineous "bloody&
!erosanguineous "plasma and red blood&
4urulent "thick, odorous, possibly yellow, green, or
brown&
6dor
Defines the presence or absence of high bacteria counts in the
ulcer and should be assessed only after cleaning the wound. +
strong or foul odor suggests infection. + mild odor may be due
to the particular wound care products in use.
Description of the
4eriwound !kin
7olor
Redness, pallor, blanchable erythema, nonblanchable
erythema, purple discoloration
Temperature
5armth may indicate further tissue breakdown or underlying
infection.
Induration
+bnormal firmness with a definite margin may indicate
infection.
-aceration
!oftening of tissues may be due to soaking from wound
drainage or contact with urine and?or stool.
Denuded
!uperficial skin loss may be due to drainage or trauma "such
as from tape&. Excoriation refers to linear scratch)like marks,
not to skin loss from trauma or incontinence.
Type of Tissue
@Bposed
Red -ay indicate clean, healthy granulation tissue. <ranulation is a
pink or red moist tissue composed of new blood vessels and
56.D D@!7RI4TI6.
Cate"!r- $escri+ti!n
"appearance of
wound bed&
connective tissue that fills an open wound when it starts to
heal. It usually has an irregular, granular surface. .ot all red
tissue is granulation.
Fellow
-ay indicate the presence of drainage or slough. !lough is a
soft, moist, avascular "lacking blood supply& tissue that may be
yellow, white, tan or green. It may be loose or firmly attached.
!ometimes resembles chicken fat.
Elack
-ay indicate the presence of eschar or necrotic tissue, which
slows healing and allows bacteria to grow. It may be brown or
tan and can be hard or soft, loose or firmly attached. It can
resemble a scab, but there is no healing occurring under it.
5ound
-easurements
+lways use a single)use, metric tape measure. .ever measure using ;coins=
"dime)si*ed, ,uarter)si*ed, etc.&
9ength
9inear distances from wound edge to wound edge. To measure
consistently, look at the wound as if it were a clock faceH the
top of the wound "12 oclock& is toward the patients head. The
bottom of the wound "/ oclock& is toward the patients feet.
9ength is the longest distance measured from 12 to / oclock.
5idth
5idth is longest distance measured from side to side, or from
A to 2 oclock.
Depth
The distance from the visible surface to the deepest point in
the wound base. -easure depth using a cotton)tip applicator,
holding it perpendicular to the wound edge, placing the finger
at the point on the swab that corresponds to the wound edge.
5hile still holding this measurement, remove the swab and
measure it on the tape measure.
ndermining
Tissue destruction to underlying, intact skin along the wound
edges. se a cotton)tip applicator to probe to the deepest part
of the undermining. -ark the depth between the end of the
applicator and the wound edge with the finger and measure it
against the tape measure. Describe the location of the
undermining using the clock face "e.g., ;undermining eBtends
from 12 oclock to 5 oclock and is deepest at 2 oclock at 2
cm=&.
Tunneling or
!inus Tract
+ path of tissue destruction that occurs in any direction from
the surface or edge of the wound. -easure the tract as for
undermining and describe its location using the clock face.
5ound care documentation includes a variety of information that reflects the wound status while
it heals. 4roviding an accurate description of the skin and wound characteristics is critical during
each patient visit. These findings will help the clinician revise the plan of care and treatment
strategies over time, based on the current status of the ulcer.
Minimi0in" the Recurrence !, Ulcers
+chieving a closed wound is the beginning of the struggle to prevent an ulcer from recurring.
7linicians must emphasi*e to patients and caregivers that measures to promote healing and
prevent recurrence are lifelong. Recurrence rates for adults have been reported as high as 5/L,
and 21L develop a new ulcer at a different site "567., 2$1$&. The most common factors
associated with recurrence are related to a lack of compliance with maintaining a healthy
lifestyle, such as stopping smoking, maintaining a normal weight, controlling blood sugars if
diabetic, and offloading the pressure areas. 4atient education regarding these factors is critical.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Lung Disease Is Any Disease or Disorder Where Lung Function Does Not Work ProperlyDocument1 pageLung Disease Is Any Disease or Disorder Where Lung Function Does Not Work ProperlyDecky AndreaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Lung Disease Is Any Disease or Disorder Where Lung Function Does Not Work ProperlyDocument1 pageLung Disease Is Any Disease or Disorder Where Lung Function Does Not Work ProperlyDecky AndreaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Antibiotics For The Common Cold and Acute Purulent RhinitisDocument2 pagesAntibiotics For The Common Cold and Acute Purulent RhinitisDecky AndreaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Scope of The Problem: DefinitionsDocument34 pagesScope of The Problem: DefinitionsDecky AndreaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Vaccines For Preventing Influenza in Healthy ChildrenDocument3 pagesVaccines For Preventing Influenza in Healthy ChildrenDecky AndreaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Presentasi Kasus Glaukoma AkutDocument24 pagesPresentasi Kasus Glaukoma AkutHendrawan Ariwibowo100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- For Printing Grand Case Group1Document37 pagesFor Printing Grand Case Group1Joco Bordeos AripNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Nelson MCQ PDFDocument595 pagesNelson MCQ PDFPavan Kumar100% (5)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- A Day in Occupational Therapy Analice BurdDocument5 pagesA Day in Occupational Therapy Analice Burdapi-518311936No ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Sedentary BehaviourDocument2 pagesSedentary BehaviourRiyuNo ratings yet
- American Dietetic AssociationDocument9 pagesAmerican Dietetic AssociationPatty LopezNo ratings yet
- Why Stomach Acid Is Essential For Our HealthDocument6 pagesWhy Stomach Acid Is Essential For Our HealthGabriel Turlac100% (1)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Fitness or Activity Blair 2001Document21 pagesFitness or Activity Blair 2001AisyahMKNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- NCP OsteoarthritisDocument4 pagesNCP OsteoarthritisKyle Margaret Flores100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- A New Understanding and A Minimalist Approach For.17Document9 pagesA New Understanding and A Minimalist Approach For.17diego.guerra.smithNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Types of Veneers in Dental WorldDocument6 pagesTypes of Veneers in Dental WorldLenutza LenutaNo ratings yet
- Pleural Puncture/thoracentesis: Pretty Laura ListianiDocument21 pagesPleural Puncture/thoracentesis: Pretty Laura ListianirastaNo ratings yet
- Ezetimibe + SimvastatinDocument13 pagesEzetimibe + SimvastatinDavid Raju GollapudiNo ratings yet
- Balance System: by M K SastryDocument33 pagesBalance System: by M K SastryEdison halim100% (3)
- Soapie, Assessment and NCP On PAINDocument7 pagesSoapie, Assessment and NCP On PAINAna100% (2)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Precancerous Lesions of The Gynecologyc Tract - 2016 PDFDocument324 pagesPrecancerous Lesions of The Gynecologyc Tract - 2016 PDFCésar Garavito Quijaite50% (2)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- A Solution-Focused Approach To Rational-Emotive Behavior Therapy - Toward A Theoretical IntegrationDocument22 pagesA Solution-Focused Approach To Rational-Emotive Behavior Therapy - Toward A Theoretical Integrationsolutions4familyNo ratings yet
- Diagnosis of cow milk allergy in infants and childrenDocument2 pagesDiagnosis of cow milk allergy in infants and childrenMaya FikriNo ratings yet
- What Is Love Addiction?Document5 pagesWhat Is Love Addiction?Richard BryanNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hypnotize This!Document342 pagesHypnotize This!Jack DICK100% (1)
- Stop excessive sweating with a safe, affordable at-home solutionDocument2 pagesStop excessive sweating with a safe, affordable at-home solutionJohny AplleasedNo ratings yet
- Analysis of Fruit and Vegetable JuicesDocument3 pagesAnalysis of Fruit and Vegetable JuicesAditya Rajendran50% (2)
- Counselling Module EDU3107 by IDRUL HISHAMDocument209 pagesCounselling Module EDU3107 by IDRUL HISHAMThia SolveNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Strategias DE Prevención E Intervención DEL Burnout EN EL Ámbito EducativoDocument7 pagesStrategias DE Prevención E Intervención DEL Burnout EN EL Ámbito EducativoEuge López RuizNo ratings yet
- Brain DeathDocument25 pagesBrain DeathLili JuniartiNo ratings yet
- UNANSWERED Past Plab 1700 McqsDocument260 pagesUNANSWERED Past Plab 1700 McqsHassaan Imtiaz100% (5)
- Comparison of Three Stretches For The Pectoralis Minor Muscle PDFDocument7 pagesComparison of Three Stretches For The Pectoralis Minor Muscle PDFsebafigueroa94No ratings yet
- Cardiorespiratory Conditioning in The Quality of LifeDocument4 pagesCardiorespiratory Conditioning in The Quality of LifeJani Cleria BezerraNo ratings yet
- SystemOne 60 Series REMstar Auto User ManualDocument28 pagesSystemOne 60 Series REMstar Auto User Manualmanojsingh4allNo ratings yet
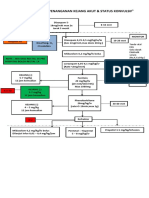
- Algoritma Penanganan Kejang AkutDocument1 pageAlgoritma Penanganan Kejang AkutEwa ClaudiaNo ratings yet
- Homeo TipsDocument124 pagesHomeo TipsAditya uniyal100% (2)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)