Professional Documents
Culture Documents
Cyclothymia English
Uploaded by
Desi Lestari NingsihOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cyclothymia English
Uploaded by
Desi Lestari NingsihCopyright:
Available Formats
Cyclothymia (cyclothymic disorder)
Definition
By Mayo Clinic Staff
Cyclothymia (si-klo-THIGH-me-uh), also called cyclothymic disorder, is a mood disorder. Cyclothymia
causes emotional ups and downs, but they're not as extreme as in bipolar disorder type I or II.
With cyclothymia, you experience periods when your mood noticeably shifts up and down from your
baseline. You may feel on top of the world for a time, followed by a low period when you feel somewhat
blue. Between these cyclothymic highs and lows, you may feel stable and fine.
Compared with bipolar disorder I or II, the highs and lows of cyclothymia are less extreme. Still, it's critical
to seek help managing these symptoms because they increase your risk of bipolar disorder I or II.
Treatment options for cyclothymia include talk therapy (psychotherapy), medications and close, ongoing
follow-up with your doctor.
Symptoms
By Mayo Clinic Staff
Cyclothymia symptoms alternate between emotional highs and lows. The highs of cyclothymia are
characterized by symptoms of an elevated mood (hypomanic symptoms), which resemble those of mania
but are less severe. The lows consist of mild or moderate depressive symptoms.
Cyclothymia symptoms are similar to those of bipolar disorder I or II, but they're less severe. When you
have cyclothymia, you can typically function in your daily life, though not always well. The unpredictable
nature of your mood shifts may significantly disrupt your life because you never know how you're going to
feel.
Hypomanic phase of cyclothymia
The highs (hypomania) of cyclothymia meet the same diagnostic definition of hypomania for type II
bipolar disorder. Signs and symptoms may include:
An exaggerated feeling of happiness or well-being (euphoria)
Extreme optimism
Inflated self-esteem
Poor judgment
Rapid speech
Racing thoughts
Aggressive or hostile behavior
Being inconsiderate of others
Agitation
Excessive physical activity
Risky behavior
Spending sprees
Increased drive to perform or achieve goals
Increased sexual drive
Decreased need for sleep
Tendency to be easily distracted
Inability to concentrate
Depressive phase of cyclothymia
Depressive episodes of cyclothymia may include a combination of these signs and symptoms:
Sadness
Hopelessness
Suicidal thoughts or behavior
Anxiety
Guilt
Sleep problems
Appetite problems
Fatigue
Loss of interest in activities once considered enjoyable
Decreased sex drive
Problems concentrating
Irritability
Chronic pain without a known cause
For the first two years after symptoms begin, the highs and lows of cyclothymia are less extreme. After
that time, your highs and lows may become more pronounced. You may have depressive episodes that
meet the criteria for full-blown major depressive episodes. Or you could experience full manic episodes.
When to see a doctor
If you have any symptoms of cyclothymia, seek medical help as soon as possible. Cyclothymia generally
doesn't get better on its own. If you're reluctant to seek treatment, work up the courage to confide in
someone who can help you take the first steps.
If a loved one has symptoms of cyclothymia, talk openly and honestly with that person about your
concerns. You can't force someone to seek professional help, but you can offer support and help find a
qualified doctor or mental health provider.
Suicidal thoughts
Although suicidal thoughts might occur with cyclothymia, they're more likely to occur if you have bipolar
disorder I or II. If you're considering suicide right now:
Call 911 or your local emergency services number, or go to a hospital emergency department.
Call a local crisis center or suicide hotline number in the United States, you can call the National
Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255) to reach a trained counselor. Use
that same number and press 1 to reach the Veterans Crisis Line.
If you just can't make that call, reach out to someone else immediately such as your doctor, mental
health provider, family member, friend or someone in your faith community.
Causes
By Mayo Clinic Staff
It's not known specifically what causes cyclothymia. As with many mental health disorders, research
shows that it may result from a combination of:
Heredity cyclothymia tends to run in families
Your body's biochemical processes, such as changes in brain chemistry
Environment
Risk factors
By Mayo Clinic Staff
Cyclothymia is thought to be relatively rare. But true estimates are hard to pin down because people may
be undiagnosed or misdiagnosed as having other mood disorders, such as depression.
Cyclothymia typically starts during teenage years or young adulthood. The condition affects about the
same number of males and females.
Complications
By Mayo Clinic Staff
Left untreated, cyclothymia can result in significant emotional problems that
affect every area of your life and it might develop into bipolar disorder I or
II, based on worsening or more-extreme signs and symptoms.
Preparing for your appointment
By Mayo Clinic Staff
If you have signs and symptoms common to cyclothymia, call your doctor.
After your initial appointment, your doctor may refer you to a mental health
provider who can help make a firm diagnosis and create the right treatment
plan for you.
Here's some information on how to prepare for your appointment and what to
expect from your doctor.
What you can do
Write down any symptoms you've been experiencing, and for how
long.
Write down your medical information, including other physical or mental
health conditions with which you've been diagnosed.
Make a list of any medications you're taking, including over-the-counter
medications, vitamins and supplements.
Ask a trusted family member or friend to come to your appointment, if
possible. Someone close to you may provide additional insight about your
condition and can help you remember what's discussed during your
appointment.
Write down questions to ask your doctor.
Questions to ask at your first appointment
What do you believe is causing my symptoms?
Are there any other possible causes?
How will you determine my diagnosis?
Should I see a mental health specialist?
Questions to ask if you're referred to a specialist
What is my diagnosis?
What treatments are likely to be helpful in my case?
How much do you expect my symptoms to improve with treatment?
Will I need to be treated for the rest of my life?
What lifestyle changes can help me manage my symptoms?
How often should I be seen for follow-up visits?
Am I at increased risk of other mental health problems?
Do you have printed material that I can take home with me? What
websites do you recommend?
Don't hesitate to ask for more information if you don't understand something.
What to expect from your doctor
A doctor or mental health provider may ask:
What prompted you to seek treatment?
How would you describe your symptoms?
How have the people close to you described your symptoms?
When did you or your loved ones first notice these symptoms?
Have your symptoms been getting better or worse over time?
If you have intense high and low periods, how long do these periods
generally last?
Do you also have periods where your mood feels relatively stable?
How would you describe your mental and emotional state during high
versus low periods? How would your loved ones answer this question
about you?
How would you say your choices and behaviors change during high versus
low periods? How would your loved ones answer this question about you?
Do your physical needs change during high versus low periods, such as
your need for sleep, food or sex?
How are these cycles affecting your life, including work, school and
relationships?
Have any of your close relatives had similar symptoms?
Have you been diagnosed with any medical conditions?
Have you been treated for other psychiatric symptoms or mental illness in
the past? If yes, what type of therapy was most beneficial?
Have you ever thought about harming yourself or others?
Do you drink alcohol or use illegal drugs? If so, how often?
Tests and diagnosis
By Mayo Clinic Staff
Your doctor or other health care provider must determine if you have cyclothymia, bipolar disorder I or II,
depression or another condition that may be causing your symptoms. To help pinpoint a diagnosis for
your symptoms, you'll likely have several exams and tests, which generally include:
General medical exam. During this exam, your doctor measures your blood pressure and listens to
your heart and lungs, among other things or reviews results of recent physical exams to
determine if there could be any medical reasons for your symptoms.
Lab tests. These may include a complete blood count as well as thyroid tests and other blood tests.
You may also have a urinalysis or tests for drug and alcohol use.
Psychological evaluation. A doctor or mental health provider will talk to you about your thoughts,
feelings and behavior patterns. You may also fill out psychological self-assessments and
questionnaires. You may be asked about substance or alcohol abuse. And with your permission,
family members or close friends may be asked to provide information about your symptoms and
possible episodes of mania or depression.
Diagnostic criteria for cyclothymia
To be diagnosed with cyclothymia, you must meet the criteria spelled out in the Diagnostic and Statistical
Manual of Mental Disorders (DSM). This manual is published by the American Psychiatric Association
and is used by mental health providers to diagnose mental conditions and by insurance companies to
reimburse for treatment.
Diagnostic criteria for cyclothymia include those below.
You've had numerous periods of elevated mood (hypomania) and many periods of depressive
symptoms for at least two years.
Your periods of stable moods usually last less than two months.
Your symptoms significantly affect you socially, at work, at school or in other important functions.
You don't have manic episodes, major depression or schizoaffective disorder a combination of
schizophrenia symptoms, such as hallucinations or delusions, and mood disorder symptoms, such as
mania or depression.
Your symptoms aren't caused by substance abuse or a medical condition.
Treatments and drugs
By Mayo Clinic Staff
Cyclothymia requires lifelong treatment even during periods when you feel better usually guided by
a mental health provider skilled in treating the condition.
To treat cyclothymia, your doctor or mental health provider aims to:
Decrease your risk of bipolar disorder I or II, since cyclothymia carries a high risk of developing
into more severe bipolar disorder
Reduce the frequency and severity of your symptoms,allowing you to live a more balanced and
enjoyable life
Prevent a relapse of symptoms, through continued treatment during periods of remission
(maintenance treatment)
Treat alcohol or other substance abuse problems, since they can worsen cyclothymia symptoms
The main treatments for cyclothymia are medications and psychotherapy.
Medications
Medications may help control cyclothymia symptoms and prevent episodes of hypomania and
depression. Medications used to treat cyclothymia include:
Mood stabilizers. Mood stabilizers help regulate and stabilize mood so that you don't swing between
depression and hypomania. Lithium (Lithobid) has been widely used as a mood stabilizer. Anti-seizure
medications, also known as anticonvulsants, are also used to prevent mood swings. Examples include
valproic acid (Depakene), divalproex sodium (Depakote), carbamazepine (Tegretol, Equetro, others)
and lamotrigine (Lamictal). Your doctor may recommend that you take mood stabilizers for the rest of
your life to prevent and treat hypomanic episodes.
Antipsychotics. Certain antipsychotic medications such as olanzapine (Zyprexa), quetiapine
(Seroquel) and risperidone (Risperdal) may help people who don't benefit from the mood-stabilizing
effects of anti-seizure medications.
Anti-anxiety medications. Anti-anxiety medications, such as benzodiazepines, may help improve
sleep.
Antidepressants. Use of antidepressants for cyclothymia is typically not recommended, unless
they're combined with a mood stabilizer or antipsychotic. As with bipolar disorder I or II, taking
antidepressants alone can trigger potentially dangerous manic episodes. Before taking
antidepressants, carefully weigh the pros and cons with your doctor.
If one medication doesn't work well for you, there are many others to consider. Keep trying until you find
one that works well for you. Your doctor may advise combining certain medications for maximum effect. It
can take several weeks after first starting a medication to notice an improvement in your cyclothymia
symptoms.
All medications have side effects and possible health risks. Talk to your doctor about the benefits and
risks.
Medications such as mood stabilizers may harm a developing fetus or nursing infant. Women with
cyclothymic disorder who want to become pregnant or do become pregnant must fully explore with their
health care providers the benefits and risks of medications.
Psychotherapy
Psychotherapy, also called counseling or talk therapy, can help you understand what cyclothymia is and
how it's treated.
Types of therapy that may help cyclothymia include:
Cognitive behavioral therapy. Cognitive behavioral therapy helps you identify unhealthy, negative
beliefs and behaviors and replace them with healthy, positive ones. In addition, you can explore what
triggers your hypomanic or depressive episodes and learn how to manage stress and cope with
upsetting situations.
Family therapy. Family therapy helps you and your family members learn how to communicate, solve
problems and resolve conflicts with each other. Family therapy helps identify stressors within the
family that may contribute to unhealthy behavior patterns. Your family may also gain a better
understanding of your condition and why you think and behave the way you do.
Group therapy. Group therapy provides a forum to communicate with and learn from others in a
similar situation. It may also help build better relationship skills.
Interpersonal social rhythm therapy. This type of therapy helps you manage your daily routines
(including your sleep schedule), improve your relationships and develop better communication skills
so that interpersonal problems don't disrupt your routines.
Lifestyle and home remedies
By Mayo Clinic Staff
You can do some things for yourself that will build on your treatment plan. In addition to professional
treatment, follow these lifestyle and self-care steps for cyclothymia:
Take your medications as directed. Even if you're feeling well, resist any temptation to skip your
medications. If you stop, cyclothymia signs and symptoms are likely to come back.
Pay attention to warning signs. You may have identified a pattern to your cyclothymia episodes and
what triggers them. Call your doctor if you feel you're facing an episode. Involve family members or
friends in watching for warning signs. Addressing symptoms early on can prevent episodes from
becoming full-blown.
Quit drinking or using illegal drugs. Alcohol and illegal drugs may trigger mood changes. Get help if
you have trouble quitting on your own.
Check first before taking other medications. Call the doctor who's treating you for cyclothymia
before you take medications prescribed by another doctor. Sometimes other medications trigger
episodes of cyclothymia or may interfere with medications you're already taking.
Keep a record. Track your moods, daily routines and significant life events. These records may help
you and your mental health provider understand the effect of treatments and identify thinking patterns
and behaviors associated with cyclothymic symptoms.
Coping and support
By Mayo Clinic Staff
Coping with cyclothymia can be difficult. Medications can have unwanted side
effects, and you may feel angry or resentful about having a serious condition
that requires lifelong treatment. During periods when you feel better, or during
hypomanic episodes, you may be tempted to stop your cyclothymia treatment.
Here are some ways to cope with cyclothymia:
Learn about the disorder. Learning about cyclothymia and its possible
complications can empower you and motivate you to stick to your
treatment plan.
Join a support group. Support groups for people with cyclothymia can
help you reach out to others facing similar challenges.
Stay focused on your goals. Successfully managing cyclothymia can
take time. Stay motivated by keeping your goals in mind.
Find healthy outlets. Explore healthy ways to channel your energy, such
as hobbies, exercise and recreational activities.
Learn relaxation and stress management. Try stress-reduction
techniques such as meditation, yoga or tai chi.
Prevention
By Mayo Clinic Staff
There's no sure way to prevent cyclothymia. However, treatment at the
earliest indication of a mental health disorder can help prevent cyclothymia
from worsening. Long-term preventive treatment also can help prevent minor
episodes from becoming full-blown episodes of mania or depression.
http://www.mayoclinic.org/search/search-results?q=cyclotemia
You might also like
- Stress Less, Live More: Everyday Stress, Everyday SolutionsFrom EverandStress Less, Live More: Everyday Stress, Everyday SolutionsNo ratings yet
- Surviving Anxiety: How to Reduce Stress, Overcome Anxiety, and Stop Anxiety AttacksFrom EverandSurviving Anxiety: How to Reduce Stress, Overcome Anxiety, and Stop Anxiety AttacksNo ratings yet
- Schizoaffective - Disorder - FactsheetDocument9 pagesSchizoaffective - Disorder - FactsheetGeraldVal100% (1)
- Understanding: Schizoaffective DisorderDocument24 pagesUnderstanding: Schizoaffective DisorderGemma GarciaNo ratings yet
- Delusional DisorderDocument4 pagesDelusional DisorderBarunansu SarkarNo ratings yet
- Edith Packer - The Art of Introspection Intro PDFDocument4 pagesEdith Packer - The Art of Introspection Intro PDFmabesninaNo ratings yet
- Bipolar Disorder: Download PDF Download Epub Order A Free Hardcopy en EspañolDocument50 pagesBipolar Disorder: Download PDF Download Epub Order A Free Hardcopy en EspañolMark Anthony Bueno AsuncionNo ratings yet
- Psychology AssignmentDocument3 pagesPsychology AssignmentDavid HoangNo ratings yet
- Chakras & SoundDocument7 pagesChakras & Soundacme2000usNo ratings yet
- He Drove Me Mad. An Investigation Into The Relationship Between Domestic Violence and Mental Illness - Debbie Hager PDFDocument184 pagesHe Drove Me Mad. An Investigation Into The Relationship Between Domestic Violence and Mental Illness - Debbie Hager PDFJaneNo ratings yet
- Mind Leaflet - How-To-Cope-With-Sleep-Problems-2014Document24 pagesMind Leaflet - How-To-Cope-With-Sleep-Problems-2014api-273164510No ratings yet
- Abnormal BehaviorDocument22 pagesAbnormal BehaviorKieth DagondongNo ratings yet
- Depression During PregnancyDocument17 pagesDepression During PregnancySellymarlinaleeNo ratings yet
- Biblio TherapyDocument8 pagesBiblio TherapyRobert Jan FiestaNo ratings yet
- Chapter 16 - Psychological Disorders NotesDocument5 pagesChapter 16 - Psychological Disorders NotesManan JainNo ratings yet
- Young Adulthood Presentation 1Document32 pagesYoung Adulthood Presentation 1Johan bioreNo ratings yet
- Glossary of Psychotic Disorders FinalDocument16 pagesGlossary of Psychotic Disorders FinalYuridiana SánchezNo ratings yet
- Prelim PsychologyDocument3 pagesPrelim PsychologyRamon Jr. MontesorNo ratings yet
- Abnormal Psychology DisordersDocument34 pagesAbnormal Psychology DisordersannaNo ratings yet
- Mindfulness Glossary of TermsDocument2 pagesMindfulness Glossary of TermsmykolayovychNo ratings yet
- Unit - 6 - Stress Copying StrategiesDocument20 pagesUnit - 6 - Stress Copying Strategiespallavi tripathyNo ratings yet
- Anxiety PDFDocument2 pagesAnxiety PDFHussain OtlaNo ratings yet
- ConversionPsychiatric Symptoms and Dissociation in Conversion, Somatization and Dissociative Disorders15Document7 pagesConversionPsychiatric Symptoms and Dissociation in Conversion, Somatization and Dissociative Disorders15Amir MirzaNo ratings yet
- Ten Ways To Like Yourself BetterDocument3 pagesTen Ways To Like Yourself BetterpvarillasNo ratings yet
- Axis I Clinical Psychiatric Disorders - LMM-1Document11 pagesAxis I Clinical Psychiatric Disorders - LMM-1richhuangNo ratings yet
- US Veterans Administration Geropsychology Bibliotherapy Resource GuideDocument47 pagesUS Veterans Administration Geropsychology Bibliotherapy Resource GuideAnonymous Ax12P2srNo ratings yet
- Loss, Grief and DyingDocument18 pagesLoss, Grief and DyingLliryc Sotnas OleusnocNo ratings yet
- Mental Disorder: Ega Saphira Talitha Ilma Sabrina Fildzah Nadhilah Nurul AnggrainiDocument13 pagesMental Disorder: Ega Saphira Talitha Ilma Sabrina Fildzah Nadhilah Nurul AnggrainiCharissa ArdhinaNo ratings yet
- Conversion Disorder The Modern HysteriaDocument6 pagesConversion Disorder The Modern HysteriaGiiszs AlvarezNo ratings yet
- A Relational Toolbox / BestDocument10 pagesA Relational Toolbox / BestPetar LukicNo ratings yet
- Interpersonal and Social Rhythm Therapy For Bipolar Disorder: Strategies and TechniquesDocument54 pagesInterpersonal and Social Rhythm Therapy For Bipolar Disorder: Strategies and TechniquesGiselle M. SuarezNo ratings yet
- Psychology ReviewerDocument103 pagesPsychology ReviewerRachel AlmiaNo ratings yet
- Bruna MartinuzziDocument27 pagesBruna MartinuzzicruxymirthNo ratings yet
- Autism: Catatonia: The Ultimate Yet Treatable Motor Reaction To Fear in AutismDocument5 pagesAutism: Catatonia: The Ultimate Yet Treatable Motor Reaction To Fear in AutismMariano OutesNo ratings yet
- Redefining Our Perceptions of What Constitutes Psychological DisordersDocument21 pagesRedefining Our Perceptions of What Constitutes Psychological DisordersaKmaL100% (1)
- Chapter 14Document54 pagesChapter 14muhibNo ratings yet
- Anxiety Disorders: TreatmentDocument23 pagesAnxiety Disorders: TreatmentSónia AlvesNo ratings yet
- Week 1: Store Managers/ Supervisors Training GuideDocument3 pagesWeek 1: Store Managers/ Supervisors Training GuideAron SulitNo ratings yet
- Dysthymia and CyclothymiaDocument9 pagesDysthymia and CyclothymiaNatnael0% (1)
- The Bipolar SpectrumDocument104 pagesThe Bipolar SpectrumjklugmnNo ratings yet
- Guía de TOCDocument96 pagesGuía de TOCkarlunchoNo ratings yet
- Communication Skills (09av 12av201,2) LTBVY W1-15Document123 pagesCommunication Skills (09av 12av201,2) LTBVY W1-15space24No ratings yet
- Behavioral Developmental Effects TraumaDocument7 pagesBehavioral Developmental Effects TraumaAdidelys ColonNo ratings yet
- Excoriation FaqDocument1 pageExcoriation FaqaladininsaneNo ratings yet
- Dissociation and Dissociative DisordersDocument20 pagesDissociation and Dissociative DisordersRicky DNo ratings yet
- Psychological Disorders BookletDocument16 pagesPsychological Disorders BookletKaraLyn Hatcher100% (1)
- 1 The Effects of Sleep DeprivationDocument15 pages1 The Effects of Sleep DeprivationShenel OrtegaNo ratings yet
- Dissociative Identity Disorder in ArtDocument5 pagesDissociative Identity Disorder in ArtsiancampbellNo ratings yet
- The Importance of Beliefs and Values Cheatsheet PDFDocument5 pagesThe Importance of Beliefs and Values Cheatsheet PDFHelen RyleNo ratings yet
- APA - (2011) DSM-5 Development. Personality and Personality DisordersDocument16 pagesAPA - (2011) DSM-5 Development. Personality and Personality DisordersRodrigo Middleton InfanteNo ratings yet
- Comorbidity: Addiction and Other Mental IllnessesDocument12 pagesComorbidity: Addiction and Other Mental IllnessesnidaebooksNo ratings yet
- Mental Disorders: Sub Ject: Clinical Psychology Presented By: PHD - Mariana CernitanuDocument34 pagesMental Disorders: Sub Ject: Clinical Psychology Presented By: PHD - Mariana CernitanuAlbert PruteanuNo ratings yet
- Anxiety: Cognitive Fusion & WillingnessDocument47 pagesAnxiety: Cognitive Fusion & WillingnessMonika MalikNo ratings yet
- 57 Psychopathology OCD 2007PDFDocument4 pages57 Psychopathology OCD 2007PDFLIDIYA MOL P VNo ratings yet
- Selfless Love Lesson EbookDocument19 pagesSelfless Love Lesson EbookChris PearsonNo ratings yet
- Bipolar Check in PDFDocument2 pagesBipolar Check in PDFAnonymous 830d2u2UNo ratings yet
- Cognitive Behavioral Therapy PDFDocument1 pageCognitive Behavioral Therapy PDFmofasorgNo ratings yet
- The Student-Athlete & StressDocument6 pagesThe Student-Athlete & StresssadepressionscreenNo ratings yet
- Sleeping Difficulties: Harrow Mental Health Information Directory FactsheetDocument4 pagesSleeping Difficulties: Harrow Mental Health Information Directory FactsheetjmaurpNo ratings yet
- Crohn's DiseaseDocument46 pagesCrohn's Diseaseuttarasingh100% (3)
- List of MedicinesDocument32 pagesList of Medicinescarleen_almiraNo ratings yet
- Script For Gradderall XVDocument4 pagesScript For Gradderall XVapi-273399286No ratings yet
- Kumpulan Diagnosas Klinik/poliklinikDocument10 pagesKumpulan Diagnosas Klinik/poliklinikHadiyasa JatmikaNo ratings yet
- Soal Latihan Bahasa InggrisDocument8 pagesSoal Latihan Bahasa InggrisFransiska TanNo ratings yet
- Worm Infestations 1Document18 pagesWorm Infestations 1Beta UserNo ratings yet
- Andrés Felipe Cardona: Eduardo Obando)Document3 pagesAndrés Felipe Cardona: Eduardo Obando)Zarit Diseños CaliNo ratings yet
- Republic of The Philippines DOH Regional Office XIII Butuan City Midwife Ii Narrative ReportDocument1 pageRepublic of The Philippines DOH Regional Office XIII Butuan City Midwife Ii Narrative ReportLAURENCE ALBIOSNo ratings yet
- Malaria Rapid Diagnostic Tests (RDTS)Document37 pagesMalaria Rapid Diagnostic Tests (RDTS)MegbaruNo ratings yet
- Mendelian Disorders Class 12Document22 pagesMendelian Disorders Class 12Harith KumarNo ratings yet
- Clinical Fact Sheet PNDocument2 pagesClinical Fact Sheet PNapi-360120287No ratings yet
- 2017 PTMAZEiftDocument4 pages2017 PTMAZEiftAnindya DeNo ratings yet
- Skin AssessmentDocument45 pagesSkin AssessmentAbdurehman AyeleNo ratings yet
- 1 AnalgesicsDocument10 pages1 Analgesicsalhesham141No ratings yet
- Neurological Disorders - SIMCLEXDocument10 pagesNeurological Disorders - SIMCLEXLLLJJJNo ratings yet
- Avishek Recent RecallsDocument43 pagesAvishek Recent RecallsPritam RoyNo ratings yet
- LV Systolic FunctionDocument36 pagesLV Systolic Functionsruthimeena6891No ratings yet
- Acute Necrotizing Ulcerative GingivitisDocument4 pagesAcute Necrotizing Ulcerative GingivitisNeira N SakinahNo ratings yet
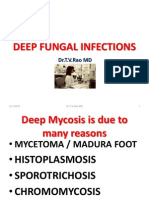
- Deep Fungal InfectionsDocument33 pagesDeep Fungal Infectionstummalapalli venkateswara raoNo ratings yet
- 4.17 Tighe Mitral Valve Prostheses PDFDocument60 pages4.17 Tighe Mitral Valve Prostheses PDFBrie DanielNo ratings yet
- DashBoard Health SampleDocument1 pageDashBoard Health SampleAliChana1No ratings yet
- Pediatric Respiratory EmergencyDocument35 pagesPediatric Respiratory EmergencyImran FaisalNo ratings yet
- Seamless Care - DR SH LeungDocument38 pagesSeamless Care - DR SH Leungmalaysianhospicecouncil6240No ratings yet
- Schistosomiasis Control Program - Department of Health WebsiteDocument2 pagesSchistosomiasis Control Program - Department of Health WebsiteDud AccNo ratings yet
- Colonic Carcinoma Case StudyDocument23 pagesColonic Carcinoma Case StudyGlaiza Claire Am-amlan OlayanNo ratings yet
- Kapita Selekta Epidemiologi - HO PDFDocument42 pagesKapita Selekta Epidemiologi - HO PDFDyandri YogiNo ratings yet
- Alcohol Withdrawal Syndrome by AAFPDocument8 pagesAlcohol Withdrawal Syndrome by AAFPWayTernMahNo ratings yet
- Case Study About Type II Diabetes MellitusDocument82 pagesCase Study About Type II Diabetes MellitusKristine YoungNo ratings yet
- 0043 PDFDocument12 pages0043 PDFZuhdan AnnajmutstsaqibNo ratings yet
- Chapter 43 - Pituitary and Adrenocortical HormonesDocument10 pagesChapter 43 - Pituitary and Adrenocortical HormonesHannaNo ratings yet