Professional Documents
Culture Documents
FHS Report 07
Uploaded by
The IIHMR University0 ratings0% found this document useful (0 votes)
41 views67 pagesHealth, Equity and Poverty Exploring the Links in West Bengal, India
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentHealth, Equity and Poverty Exploring the Links in West Bengal, India
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
41 views67 pagesFHS Report 07
Uploaded by
The IIHMR UniversityHealth, Equity and Poverty Exploring the Links in West Bengal, India
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 67
Health, Equity and Poverty
Exploring the Links in West
Bengal, India
Kanjilal B, Mukherjee M, Singh S, Mondal S, Barman D, Mandal A
RESEARCH MONOGRAPH INDIA SERIES
December 2007 www.futurehealthsystems.org
Health, Equity and Poverty
Exploring the Links in West Bengal,
India
FUTUE HE!LTH "#"TE$"
E"E!%H $&'&(!PH
INDIA
Kanjilal B, u!herjee , "ingh ", on#al ", Barman D, an#al A
December 2007
Acknowledgement
We acknowledge and sincerely appreciate the support and inspiration received from the Department of Health and FW,
Government of West Bengal - especially from Dr. Kalyan Bagchi, Additional Chief Secretary (Health & FW). Special thanks
go to Mr. H K Dwivedy, former Special Secretary (Health & FW) for his intense and active interest in the research. The
inspiration received from our colleagues at IIHMR especially from our Director Dr. S D Gupta - is also sincerely appreciated.
Dr. Satish Kumar, Ms. Tannistha Samanta, and Dr. N Ravichandran who were involved at the data collection stage, deserve
special mention.
Primary data from households were collected with active support from Economic Information Technology and KAP two
organizations of Kolkata. The in-charge of various government hospitals fully cooperated with the study team. The key
members of district associations of Rural Medical Practitioners also provided the team with active support.
We also acknowledge the scientific support extended by 'Future Health Systems: Innovations for equity'
( ) a research program consortium of researchers from Johns Hopkins University Bloomberg
School of Public Health (JHSPH), USA; Institute of Development Studies (IDS), UK; Center for Health and Population
Research (ICDDR,B), Bangladesh; Indian Institute of Health Management Research (IIHMR), India; Chinese Health
Economics Institute (CHEI), China; The Institute of Public Health (IPS), Makerere University, Uganda; and University of
Ibadan (UI), College of Medicine, Faculty of Public Health, Nigeria.
We express our appreciation for the financial support (Grant # H050474) provided by the UK Department for International
Development (DFID) for the Future Health Systems research programme consortium. This document is an output from a
project funded by DFID for the benefit of developing countries. The views expressed are not necessarily those of DFID or
Department of Health and FW, Government of West Bengal.
www.futurehealthsystems.org
Health, Equity and Poverty:Exploring the Links in West Bengal, India
i
Abbreviations
BE Budget Estimates
BPHC Block Primary Health Centre
BPL Below Poverty Line
CI Concentration Index
CMOH Chief Medical Officer, Health
DFID Department for International Development
DH District Hospital
DHF District Health Fund
DHFWS District Health and Family Welfare Society (Samity)
DoHFW Department of Health and Family Welfare
EDL Essential Drug List
FHS Future Health System
FW Family Welfare
GoI Government of India
GoWB Government of West Bengal
HSDI Health System Development Initiative
HMIS Health Management Information System
IEC Information, Education, and Communication
IIHMR Institute of Health Management Research
IPD In-patient Department
JSY Janani Suraksha Yojana (Mother's Protection Scheme)
MCH Maternal and Child Health
rd
NFHS-3 National Family Health Survey (3 round)
NGO Non-government Organization
NSDP Net State Domestic Product
NSSO National Sample Survey Organization
OPD Out-patient Department
OOPE Out of Pocket Expenditure
PER Public Expenditure Review
PHC Primary Health Centre
PMGY Prime Minister's Gramodaya Yojana (rural development scheme)
RCH Reproductive and Child Health
RE Revised Estimates
RH Rural Hospital
RMP Rural Medical Practitioners
SDH Sub-divisional Hospital
SHG Self Help Group
SGH State General Hospital
SHSDP-II State Health System Development Project: Phase Ii
STG Standard Treatment Guideline
Health, Equity and Poverty:Exploring the Links in West Bengal, India
ii
Preface
This document presents the key results of a recent research on health care system conducted by Institute of Health
Management Research (IIHMR) in West Bengal, India based on a research grant awarded by the Department for International
Development (DFID), United Kingdom to an International Research Programme Consortium (RPC) in which IIHMR is a
partner. The consortium, titled as Future Health Systems: Innovations for Equity (FHS), will carry out innovative research
programmes in six countries. The three basic themes of FHS can be summarized as follows:
How can the poor be protected from the impoverishing impact of health-related shocks?
What innovations with public and private health sector can work for the poor?
How can policy and research processes be used to meet the needs of the poor?
IIHMR has identified West Bengal as the major focus state for implementing the research programme in India. More
specifically, it proposes to explore the potential of the strategy of decentralization of health care services, as manifested in a
series of initiatives recently being spearheaded by the Department of Health and Family Welfare (DoHFW) in the state to
improve the effectiveness of the health system, in protecting interests of poor people.
The guiding principle of the FHS research initiatives in India is putting the poor first supported by the three research themes
mentioned earlier. Hence, the purpose of research is to generate evidences on the link between health, poverty, and consequent
inequity from demand and supply angles and suggest appropriate interventions to weaken the link. Keeping this in mind, the
research in India was planned as a multi-phases initiative. In the first phase, which just completed, a series of scoping studies
were carried out to prepare a knowledge base on which an appropriate strategy for a more equitable health system would be
developed. Phase II, would be devoted to develop a few major proposals, based on the Phase I research results. The proposals
will approach specific interventions at the district level to help the system (1) track resources and benefits from government
subsidies; and (2) protect the poor from health-related financial shocks.
The principle research questions for the Phase I studies were:
1. How does the link between poverty and health manifest itself in the Indian health care market?
2. How much is the supply side environment oriented towards equitable distribution of resources?
3. Whether and to what extent the existing institutional arrangement at the ground level support
implementation and oversight of pro-poor policies?
The studies were carried out at two levels: (1) national and state level, primarily based on available national survey data (NSSO,
RCH Household Survey, etc.); and (2) district level, exclusively based on primary (quantitative and qualitative) data. The
primary data were sourced from three districts of West Bengal (the state selected for the Phase I studies) through rapid
household survey, assessment of selected institutions (such as, health care providers, Panchayet institutions, health
department, autonomous health societies, civil society bodies, and others), and assessment of a few pro-poor schemes (e.g.,
JSY, Rogi Kalyan Samiti, etc.) about whether and to what extent pro-poor policies are implemented.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
iii
The present monograph summarizes the key findings of Phase-I scoping studies which were conducted during January March,
2007. The purpose of disseminating these results is to initiate dialogue between key stakeholders on how to make the health
care delivery system work more for the poor and vulnerable groups of population and protect them from the impoverishing
effects of poor health and consequent health care. Although the data were sourced from a particular state (West Bengal), most
of the findings are expected to be relevant to other Indian states.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
iv
Table of Contents
Section
Title Page
Acknowledgement
Abbreviations
Preface
Executive Summary
i
ii
iii
vi
1 Background
1.1 Introduction 1
1.2 A brief profile of the state 2
1.3 Data and methods 3
2 Health Sector in West Bengal: An overview
2.1 Health status in West Bengal 7
2.2 Health care system in West Bengal 8
2.3 Public financing of health care in West Bengal : an overview 9
2.4 Private health care spending 10
3 Health, Equity and Poverty: Key issues
3.1 Key issues 13
I. Health Care Utilization
3.2 Good performance in ensuring horizontal equity in inpatient care 13
3.3 Young and older women have less access to hospitalization 16
3.4 Government hospitals play dominant role, but without much targeting
3.5 Outpatient care market is dominated by unqualified providers 18
3.6 Strong barriers against equity in institutional delivery 23
3.7 Inequality in utilization of preventive child health care 26
II. Health Care Financing
3.8 Equity in public spending is questionable 28
3.9 Poor oversight at the district level 30
3.10 Medicines and tests: killing fields 31
3.11 OOPE is progressive in inpatient care but not so in outpatient care 34
3.12 Growing health poverty in a socially unprotected environment 36
4 Towards a More Equitable Future : how can research help?
4.1 How to make the system work more for the poor? 43
4.2 Develop a closer working relation with informal sector 43
4.3 Ensure local oversight for implementing pro-poor strategies 45
4.4 Reduce asymmetric information in drugs market 46
4.5 Develop appropriate risk pooling mechanism 47
4.6 Improve targeting in public subsidies for essential health care. 48
4.7 Address the barriers to preventive care and safe birth delivery 51
4.8 Facilitate and regulate private sector 52
References 53
Health, Equity and Poverty:Exploring the Links in West Bengal, India
v
16
Executive Summary
India is on a fast-track growth path and the health care market is opening up with new opportunities. However,
impressive growth with inadequate social protection may lead to newer vulnerabilities, inequalities, and health
related poverty. The study focused on one Indian state (West Bengal) to explore the link between health, poverty,
and equity against this dynamic backdrop. Primary data - from households and different types of providers - were
collected from three districts of the state.
West Bengal is a middle level achiever in economic front but one of the top rankers (among all major
Indian states) in most of the basic health indicators although the rural areas are significantly behind the urban. The
state has a huge infrastructure of government's health facilities supplemented by an assortment of private health
care providers, which play a minor role in preventive and inpatient care but a major role in ambulatory care.
Despite an impressive growth of public spending on health over the last 15 years, the share of health in total
budget has been declining. Inadequacy of public spending reflects in high out of pocket expenses on health
which is about three times more than the former.
Health, Equity, and Poverty: Key issues
The major findings related to equity and poverty are classified into two groups according to their links to the
following areas: (1) health care utilization, and (2) health care financing.
Health care utilization
Good performance in ensuring horizontal equity in inpatient care: The state has made substantial
progress in ensuring better access and equity in inpatient care. The rate of hospitalization has increased from
1.5% (of total population) in 1995-96 to 4.3% in 2007. The rate is almost uniformly spread across various
socio-economic groups implying a near-perfect horizontal equity in inpatient care.
Young and older women have less access to hospitalization: However, concern remains in gender inequity.
The hospitalization rate was found to be much less for younger and older women than for their corresponding
male counterparts.
Government hospitals play dominant role, but without much targeting: The inpatient care market in
West Bengal is overwhelmingly dominated by public sector an exceptional case since, nationally, private
sector plays the major role. Public hospitals are, however, almost equally used by poor and rich indicating an
uninhibited access to all and missing target mechanism.
Outpatient care market is dominated by unqualified providers: The outpatient care market like other
Indian states is dominated by private providers most of whom practice allopathy without adequate training
(RMPs). The utilization of RMP services in rural areas is almost uniformly spread across various income
groups implying that low cost treatment is not the prime factor to explain people's dependence on RMPs. The
two most important factors, as found, were (1) the average distance to a RMP clinic that was much less than to
a qualified provider; and (2) an attractive packaging of services by RMPs which includes easy availability,
dispensing drugs often on credits, prompt response, and so on.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
vi
Strong barriers against equity in institutional delivery: Perceived benefits (of institutional birth delivery)
are low due to the common belief that birth delivery is a natural process and, hence, it requires no hospitalization.
However, equally important are the barriers (or, cost) to access. Three important barriers are extremely
relevant in this case: (1) long physical distance to the nearest facility, (2) higher out of pocket expenses to seek
birth delivery care from an institution, and (3) poverty. That poverty or economic constraint plays an
important determinant behind choice of place of delivery is evident from the data that 62 percent of all
pregnant mothers in the poorest quintile but only 19 percent of them in the richest quintile delivered at home
clearly implying that barriers get easier as one progresses from poorest to richest quintile.
Inequality in utilization of preventive child health care: There is no significant difference in
immunization rate across gender or rural / urban location, but inequality exists with respect to socio-economic
groups. In other words, poverty is an important dimension to explain the inequity in preventive care. The
scenario is much better in children's curative care where the probability of seeking treatment for a sick child is
more or less same across gender, rural/urban, and socio-economic differential.
Health care financing
Equity in public spending is questionable: During the last few years, the state has made remarkable
progress in pumping additional resources for meeting non-salary and development needs. Yet the
preliminary analysis indicates that there are scopes to improve allocative efficiency of public expenditure.
Major share of public spending goes to urban areas. There are also inequalities in distribution of public
budget across various types of hospitals; for example, the per bed allocation of fund to State General
Hospitals is higher than that to District Hospitals. Demand creation and stewardship two vital functions of
the public sector are allocated little fund. However, despite discrepancies in resource allocation, the state
reflects a reasonably good pro-poor image of policy making on financing. This is quite evident in several
policy decisions improvised during the last few years.
Poor oversight at the district level: It is obvious that for a more effective oversight of public services the
boundary of routine activities should be crossed. However, weak managerial and oversight capacity is one of
the major constraints (at the district level) in this process. The state government has visibly embarked on
several initiatives to arrange more flexible fund and autonomy to the district level. However, there is little
evidence on effective utilization of this autonomy to protect poor from health related financial shock
primarily due to (1) lack of an efficient resource-tracking mechanism, and (2) lack of interest and capacity
among district health administration.
Medicines and test: killing fields: The increase in government's budget on drugs has been significant
especially in the last few years. However, still people spend a substantial amount on drugs even when they
visit government facilities where drugs can be obtained free of cost. The possible reason for this is that about
a half of poor and 70 percent of better-off public clients did not receive some or any drugs from the
government facilities. Dominance of some (i.e., some but not all drugs were available) category offers
several hypotheses about which drugs are not available in government facilities: (1) essential, but prescribed
brands are not available, and (2) non-essential. The hypotheses can be tested only through proper auditing of
Health, Equity and Poverty:Exploring the Links in West Bengal, India
vii
prescriptions. Another key finding is that a large portion of better-off patients (about 56%) also receives drugs
from government facilities implying that a significant part of drug subsidy is absorbed by those who could
possibly pay for it.
Out of pocket payment is progressive in inpatient care but not so in outpatient care: In case of inpatient
care, the impact of out of pocket payment is relatively more severe on higher income groups indicating a
progressive out of pocket financing system. One out of five households from this group is likely to send at
least one member to hospitals (for inpatient care) which will account for one-sixth of their annual household
expenditure three times more than a normal scenario. The poorest households are likely to send fewer
members, and spend proportionately much less. It is interesting to note that the impact somewhat reverses in
case of outpatient care where poorer households spend more in relative terms. While about 4 percent of
poorest households made catastrophic payments for inpatient care, more than 10 percent did so for outpatient
care.
Growing health poverty in a socially unprotected environment: A framework for analyzing health
poverty is introduced which links vulnerability to health poverty with (i) household entitlements, (ii) supply
side environment, and (iii) perceived opportunity cost of health care. Given that the social entitlement is very
weak, all sections of population depend heavily on individual entitlements income, saving, borrowing, sell of
assets, and so on - when they seek health care. Poorer section was found to depend more on extended
entitlements (e.g., borrowing) implying that health care aggravates their poverty. Supply side environment
was found to have no effective procedure for identifying poor and vulnerable. Opportunity cost of health care
was high for example, 70 percent of households, which sent at least one member to a hospital as an inpatient,
had to reduce their food consumption to pay for the hospital cost.
Towards a More Equitable Future: how can research help?
Develop a closer working relation with informal sector: The study recommends internalizing and using the
huge pool of resources (i.e., RMPs) which is being used by the people anyway. Innovative ways to do so is to (1)
empanel selected RMPs at each block as Rural health gate keepers based on several essential quality indicators.
The role of the RMP will be to provide a set of basic curative services and refer cases immediately to formal
providers as and when the patient crosses the identified safe treatment; (2) identify a set of basic curative and
preventive services for which the RMPs will be given franchise right to operate as official gatekeepers; (3)
involve civil societies (Panchayet or NGO) in implementing empanelment and mentoring the RMPs; and (4)
provide intensive training to selected RMPs on simple treatments, identifying potentially complicated cases and
danger mark where they have to refer. Future research in this area should address the following questions: (1)
how safe or unsafe are the current clinical practices of RMPs? (2) What is the net impact of RMP practices on
rural health? (3) How feasible is it to integrate RMPs into existing public health care system?
Ensure local oversight for implementing pro-poor strategies and resource tracking: Are the resources
meant for poor actually reaching them? The answer may be found only when a mechanism for local oversight is
established. The management unit under DHFWS may be strengthened to initiate resource tracking in the
following areas: (1) delivery of drugs and consumables at government facilities, (2) disbursement of untied funds
Health, Equity and Poverty:Exploring the Links in West Bengal, India
viii
for special medical assistance to the poor, (3) program funds flowing through the societies, (4) funds generated
through user charges and retained at the district level, and (5) funds from special schemes, such as JSY or PMGY.
Future research in this area may be initiated in the form of a pilot intervention by which the district management
unit may be oriented and its capacity may be built to help it play oversight role.
Reduce asymmetric information in drugs market to empower the consumers: Protection of people from
health poverty necessarily boils down to protecting them from irrational drug expenses. One of the important
factors influencing the irrational process is high degree of asymmetry of information in the medicines market.
Therefore, the ongoing supply side initiatives should be supplemented by demand side interventions based on the
hypothesis that the out-of-pocket expenditure on medicines could be significantly reduced if the consumers are
adequately empowered with information on (1) cheaper (but equally useful) and generic options of prescribed
branded medicines; and (2) a distinction between essential and non-essential medicines in the context of a specific
disease. The empowerment process could be implemented by involving the local level civil societies and local
self-administration (e.g., Panchayet). The process could be initiated after a scoping study on the degree of
asymmetric information in the market, and how the imperfect agents (i.e., providers and pharmacies) are using
this information gap.
Develop appropriate risk pooling mechanism especially for economically disadvantaged section: A district
based health fund is proposed which will be held by DHFWS and operated by a professional insurer. In addition
to subsidy from the government and donors, the fund will be built on prepayment made by the Self-help Groups
(SHG). Premiums will be determined by community-rated ability to pay. Providers will include selected and
accredited private and government hospitals. Only secondary and tertiary government facilities should be
included in the initial stage. Outpatient care should be included in the benefit package. A Technical Resource
Centre will support the quality assurance mechanism and management of information system. Future research in
this area should also be framed as a pilot intervention in one district.
Improve targeting in public subsidies for essential health care: Targeting poor could be done by equitable
distribution of health care services through some sort of rationing by which the richer (including the government
servants) will be able to access within the limit of a fixed quota of subsidized beds. This should be supplemented
with a policy of total withdrawal of subsidy for those facilities that are accessed by the richer section (for example,
private cabins) and recovery of the cost on 100 percent basis. A more gender-sensitized role of providers is
expected to improve the gender inequity in inpatient care. Future research in this area is expected to focus on two
aspects: (1) generating evidences on various targeting mechanisms and assess their feasibility in the context of the
state's health care system, and (2) assessment of the pro-poor schemes initiated by the Department of Health and
FW at the ground level where it works and where it does not.
Address the barriers to preventive care and safe birth delivery: The strong barriers to meet the goals of
universal immunization and safe birth delivery need to be analyzed. For this purpose, the difficult pockets within
the state and within the districts need to be mapped according to the nature of the barrier. Once the under-served
areas are mapped and their barriers are identified, it is necessary to draw up a set of special strategies to cover these
areas. Future research should meet the acute need for scientific information on what and how the barriers lead to
underperformance. It should also help the decision-makers select a cost-effective option to act against those
barriers and test it as a pilot intervention.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
ix
Health, Equity and Poverty:Exploring the Links in West Bengal, India
x
Facilitate and regulate private sector: Internalization of private sector necessarily implies that the private
sector is to complement, and not just co-exist with, the public sector. The process would require three strategic
steps: (a) Facilitate expansion of private market at those blocks or district headquarters where the government
facilities are over-burdened; (b) minimum standards for its operation need to be maintained and regulated; and (c)
involvement of private sector in district planning process is encouraged. Future research in this area is expected
to provide the policy makers with crucial evidences on the operation of the market and help them design an
effective policy for internalizing the private sector.
1. Background
Health, Equity and Poverty:Exploring the Links in West Bengal, India
1
1.1. Introduction
1.1.1. Indian economy, by all evidences, is on a fast-track growth path. Economic liberalization, triggered in early 1990s has
taken a sharp upward turn with an impressive growth rate. However, despite India's strong growth performance
which has unleashed enormous potential for economic advancement, there is growing concern that economic
liberalization has been less successful in protecting people from the risk of new vulnerabilities, inequalities, and
insecurities especially in the social sector. Health sector in India epitomizes this proposition. Two patterns are clearly
visible: (1) there is a huge discrepancy in health outcome as well as in health care utilization between rich and poor and
between richer and poorer states. Poor people have worse health, are less entitled to public subsidies, and are less
protected against the financial shock generated by health care.; and (2) due to absence of an effective risk-pooling
mechanism, rising demand for health care and galloping inflation in health care market, even not-so-poor groups of
population are quickly slipping into poverty trap. In other words, India reflects a possible future scenario where the
poverty-reducing impact of economic growth will be countered by poverty-enhancing effects of health care if the
system continues to remain inequitable and people remain largely unprotected against financial risks related to health
shock.
1.1.2. The recent government policies related to health and population implicitly acknowledges the need to address the
question of inequities and vulnerabilities in a more effective way. The best instrument at the government's hand is its
spending on health, which is targeted to increase to 2 percent of GDP by the year 2010 from its current level of 0.9
percent. This would require the states' budgetary allocation on health to rise to 8 percent from its current level of 5-6
percent and the center's contribution to rise from 15 percent to 25 percent (NHP, 2002).
1.1.3. Given the fiscal crisis currently being experienced by the state governments, the target may seem a bit ambitious.
However, a more pertinent question is: will the increased public expenditure ensure better health for poor?
Unfortunately, the present scenario fails to offer an unambiguous answer to the question. The primary reason behind
this ambiguity is gross inequity in the distribution of public health resources. Inequity reflects not only in widening
gap of public spending between poor and rich states (Purfield, 2005), but also in substantial absorption of public
subsidies by the richer people within a given state. As shown by a recent study, about Rs. 3 is received by the richest
quintile for every Re 1 of public health subsidy received by the poorest 20 percent (Peters et al., 2002). The
disproportionate absorption of public subsidies reflects poor targeting in the public health care facilities.
1.1.4. Inadequate public expenditure, coupled with its poor targeting, results in uncontrolled proliferation of private
providers and high out of pocket expenditure by the users of health care. Although government-provided health care
is meant to be heavily subsidized and, as such, to benefit the poor, the majority of health care users who go to public
facilities incur significant out-of-pocket costs. For example, a study in one of the Indian states (West Bengal)
demonstrates that users of public sector facilities pay between 18 percent (for birth delivery) and 72 percent (for major
ailments) of what users of qualified private sector facilities pay for similar services. About 75 percent and 87 percent
of out-of-pocket expenditures in case of treatment of major ailments and minor ailments respectively in public
facilities go towards medicine and diagnostic tests. Most of the users of public hospitals are compelled to purchase
drugs and medicines in the private sector due to shortage of prescribed drugs in hospital pharmacy (Kanjilal and
Pearson, 2002).
1.1.5. Weak targeting mechanism also reflects in heavy skewness in choice of providers. According to a recent national
1
This section draws heavily on West Bengal Human Development Report (2004), published by Development
and Planning Department, Government of West Bengal.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
2
survey, about 79 percent of Indians, who were suffering from minor illnesses, sought treatment from private providers
(NSSO, 2004). It is also important to note that a large number of these providers were unqualified medical
practitioners. Clearly, increasing public finance does not match with growing dominance of these unqualified
providers in the health care market.
1.1.6. The above evidences clearly indicate two fundamental problems of Indian health care system: (1) resources flowing
through the public administrative channels do not necessarily benefit the poor; and (2) even if it does, a common
person in general - and a poor in particular - remains significantly unprotected against the unanticipated burden of
treatment of ailments.
1.1.7. How can we make the health care system work more for the poor? How can the growing vulnerabilities be challenged
with effective policy instruments? How can economic growth be made inclusive of health? These and many other
th
questions need to be addressed to achieve what the Indian Planning Commission stated as their vision for the 11 Five-
year plan It must seek to reduce disparities across regions and communities by ensuring access to basic physical
infrastructure as well as health and education services to all. An important step towards this direction is to bridge in
information gap and to generate relevant evidences that could be used as inputs for informed policy decisions. The
present document attempts to do so and diagnose the challenges on the road towards an equitable future health system.
1.2.1. West Bengal, located in the eastern part of India, ranks fourth among all Indian states in population covering less than
3 percent of the total area of India. It is strategically positioned with 3 international frontiers-Bangladesh, Nepal and
Bhutan. Nationally, it borders the state of Bihar, Jharkhand, Orissa, Sikkim and Assam. Southern and eastern plains
of the state are better endowed with sufficient water and huge productive land with a sub-humid climate. Extreme
scarcity of water, adverse climatic conditions, poor quality of soil, and low productivity of land are the characteristic
features of north, western and northwestern dry zone. The state is divided into 18 districts which are grouped into
three administrative divisions.
1.2.2. According to 2001 census, the total population of the state is approximately 80.18 million. It covers 2.7 percent of the
India's land area with 7.8 percent of the total population, thus making it the first ranker in terms of population density
of 904 per square kms. The sex ratio in the state was 934 (females per thousand of males) in 2001 as compared to the
national average of 933. The total fertility rate is lower (2.1) in comparison to the national average (2.4). Recent
estimates show that the Crude Birth Rate (CBR) is 18.8 (2005) and Crude Death Rate is 6.4 (2005). The Crude Death
Rate in urban areas (6.8) is less than that of rural areas (7.2).
1.2.3. The state's economy is rapidly progressing although it is still predominantly agrarian and 72 percent of its population
lives in rural areas. However, agriculture contributes only about 27 percent to State Domestic Product (SDP). The
service sector is the largest contributor to SDP which increased from 41 percent in 1991 to 51 percent in 2002.
Between 1994 and 2004, the economy had grown at an average rate of 8 percent per annum and become the third
largest economy in the country with a Net SDP of $ 21.5 billion. Per capita annual income was $395 in 2004, which
1
1.2. A Brief Profile of West Bengal
Health, Equity and Poverty:Exploring the Links in West Bengal, India
3
Was higher than the national average. The current focus is on rapid industrialization through increasing private
investment.
1.2.4. The state's record in poverty elimination and human development presents a mixed picture. The incidence of poverty
in West Bengal in 1997-2001 was 27 percent of population below the poverty line, marginally higher than the national
average of 26 percent. The performance of West Bengal in terms of household amenities is lower in comparison to
national average. In the late 1990s, only 16 percent of rural households and 68 percent of the urban households had
pucca (concrete) houses compared to 29 percent and 71 percent respectively for all over India. Half the households
have toilet facilities whish is same as of India. In case of access to safe drinking water, 82 percent is getting safe
drinking water vis--vis 62 percent all over India. Electrification has proceeded much slower in the state with only 33
percent having the access, compared to 42 percent all over India. In terms of Human Development Index (HDI), the
th
state ranked 8 among 15 major states indicating an average performance.
1.3.1. The study is largely based on primary data collected from three districts of West Bengal - Malda, Bankura, and North
24 Porgonas (Figure1.1) during November, 2006 through March, 2007. These districts are selected from three
different socio-economic zones of the state. Malda district represents the northern part of the state, which is relatively
backward in term of income, accessibility, literacy status, and other socio-economic indictors. North 24 Porgonas, on
the other hand, is relatively more developed and urbanized and represents the east-central zone of the state which is
also close to the capital city, Kolkata. Bankura district represents the western zone of the state which is historically
backward with more than 10 percent of its populations as tribal.
1.3.2. Primary dataset includes data obtained through following four surveys parallely carried out in the above three
districts:
A households survey covering about 3150 households
An exit interview of 690 out and inpatients in selected government facilities
In-depth interview with 71 Rural Medical Practitioners (RMP) and their associations
In-depth interview with 15 top-level medical officers at selected government hospitals to collect data
on budget, expenditure, collection of user charges, and several other aspects of hospital operations.
Each of the above was executed with a set of structured questionnaire.
1.3. Data and Methods
Health, Equity and Poverty:Exploring the Links in West Bengal, India
4
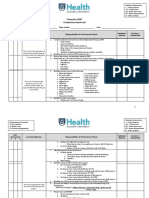
Figure 1.1. West Bengal Map and Study Districts
Household survey
1.3.3. For household survey, the households were selected by two-stage stratified sampling: first, from each of the selected
districts, 35 primary sampling units (PSU) covering both rural and urban areas were selected through PPS (Probability
Proportion to Size) method, and second, by selecting 30 households from each PSU through a systematic random
process. In total, 3152 households were selected.
1.3.4. The household survey was conducted using a structured questionnaire which primarily focused on the health seeking
behaviour, utilization of health care facilities, and out of pocket payments of the selected households. More
specifically, the investigation focused on four types of ailing persons:
(1) those who were hospitalized (for inpatient care) in last 365 days;
(2) those who sought outpatient care in last 90 days, but not hospitalized;
(3) those who were suffering from chronic health problems on the day of the survey. Chronic problems were
defined as (i) the person has been suffering from the problem persistently for at least 90 days, and (ii) the
problem has been diagnosed by a qualified health professional
(4) those women who delivered births during last two years.
In addition to collecting quantitative data, several case studies and focused group discussions were conducted in each
district.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
5
Exit interview
1.3.5. For exit interview, 412 outpatients and 278 inpatients (total 690) were interviewed at selected government facilities
including (a) District and sub-divisional hospitals (DH / SDH); and (b) Block Primary Health Centers (BPHCs). For
outpatients, 10 percent of expected inflow of patients was randomly selected. For inpatients, the same percentage of
sample was randomly drawn from the number of patients who were about to be released. Questions were usually
answered by the attendants (relatives) whenever the patients themselves were unable to do so. The interview focused
primarily on three aspects: (1) patients' background, (2) treatment seeking behavior, and (3) various costs of treatment.
Interview with RMPs
1.3.6. RMPs are not officially recognized; hence, there is no official source of information regarding the number of RMPs
and location of their practice. It is, therefore, extremely difficult to apply standard sampling procedures for selecting a
given number of respondents. Keeping this problem in mind, the following two unofficial sources were tapped to
track a number of practitioners on 'as and when found' basis: (1) every district has at least one association of RMPs
which keeps a list of their members. The association was contacted to locate possible respondents, and (2)
information provided by the clients of government health facilities who were contacted through exit interviews. The
focus of the interview was their background, background of their patients, treatment behaviour, earning, referral
behaviour, and so on. In total, 71 RMPs were interviewed through this process. In addition, in-depth discussions with
the RMPs' district associations were carried out in all the three districts.
Interview with government providers
1.3.7. A set of government facilities was visited by the FHS research team to understand the supply side environment
regarding implementation of pro-poor strategies. The visit started from the office of Chief Medical and Health
Officer (CMOH) of the district and also included: (1) District Hospitals, (2) selected Sub-divisional Hospitals, and (3)
selected BPHC / PHC. In all cases, the facility-in-charge (i.e., the chief medical officer) was met and interviewed.
The interview was guided by a checklist about information on collection and exemption of user fee, availability of
drugs, existing mechanisms for targeting poor users, major problems faced by the providers, and so on. In total, 15
facilities of different levels were visited.
Secondary data
1.3.8. The analysis of primary data is supplemented by national level survey data, wherever necessary. Two major datasets
th
were used: (1) National Sample Survey 60 round data on morbidity, health care and the condition of the aged (NSSO,
2004), and (2) RCH district level household survey (RCH-DLHS, 2004). In addition, the preliminary findings from
the recently held National Family Health Survey (NFHS-3) were also used. NSSO and NFHS data were weighted
while the other data (including the primary data) were un-weighted.
2. Health Sector in West Bengal
An Overview
2.1. Health Status in West Bengal
2.1.1. As is evident from Table 2.1, the status of health in West Bengal is better than that of the national average by almost all
indicators. It is also to be noted that the state can now be grouped with few relatively better performing states in terms
of its some vital statistics. For example, according to the Sample Registration System (SRS) data, the state has the
fourth lowest birth rate after Kerala, Punjab, and Tamil Nadu; the lowest death rate (same as Kerala), and fourth lowest
IMR after Kerala, Maharashtra, and Tamilnadu among the major Indian states. However, a few indicators also show
less-than average status. Special concern is about prevalence of anemia among adult men and women, which seems to
have higher prevalence in the state in comparison to the national average.
2.1.2. Overall health outcomes are quite impressive in the state, but the gap between rural and urban areas (regarding health
outcomes) is also evident (Table 2.1). The gap may be partially explained by the rural/urban inequalities in health
service utilization. Although health care utilization in West Bengal is better than many other states, Table 2.2 shows
that significant problems exist especially in rural areas. For example, only a half of the diarrhea-affected children
were treated in rural in contrast to two-third of the same in urban areas. A little less than half of the pregnant women in
rural areas received no antenatal care compared to only 13 percent of the urban women.
Table 2.1. Health outcomes: West Bengal and India
Indicator Year West Bengal India
Rural Urban Total Total
Birth rate (per 1000 population)
a
2005 21.2 12.6 18.8 23.8
Death rate (per 1000 population)
a
2005 6.3 6.6 6.4 7.6
Infant Mortality Rate (per 1000 live births)
a
2005 40 31 38 58
Neo-natal mortality rates (per 1000 live births)
a
2003 33 16.0 30 27
% of U-5 deaths to total deaths
a
2003 19.5 8.6 17 23.9
% of children aged 6-35 months with any anemia
b
2005-06 71.9 58.2 69.4 79.2
% of children under age 3 under-weight
b
2005-06 46.7 30.0 43.5 45.9
Total Fertility Rate (per 1000 women)
a
2005-06 2.5 1.6 2.27 2.68
% of ever married men age 15-49 anemic
b
2005-06 35.4 26.9 33.1 24.3
% of ever married women age 15-49 anemic
b
2005-06 65.6 59.0 63.8 56.2
Maternal Mortality Ratio (per 100,000 live births)
a
2001-03 NA NA 194 301
a
Source: Sample Registration System
b
National Family Health Survey (2005-06) (NFHS-3);
Table 2.2. Utilisation of selected health services in West Bengal
Source: National Family Health Survey (2005-06) West Bengal (NFHS-3), provisional data
Health service indicator Rural
(Percent)
Urban
(Percent)
Women who received Antenatal care 55.8 87.3
Deliveries in medical facilities 33.8 79.2
Women who received Postnatal care 29.9 67.4
Children received all vaccinations 62.8 70.3
Women who use any modern contraceptive method 49.9 49.9
Children with diarrhea treated in a health facility 50.0 67.6
Health, Equity and Poverty:Exploring the Links in West Bengal, India
7
2.2. Health Care System in West Bengal
2.2.1. The state, like any other Indian state, presents an extremely complex landscape of health care service delivery. Public
sector facilities in West Bengal range from 9 teaching (tertiary) hospitals with highly specialized physicians to more
than 10,000 small sub-centers at the village level staffed by Multi-purpose Workers (MPWs). Within this range there
exist various types of public facilities 15 district hospitals, 79 sub-district / state general hospitals (SDH / SGH), 93
Rural Hospitals (RH), 241 Block Primary
Health Centers (BPHC), and 922 Primary
Health Centers (PHC) - arranged in order
of secondary to primary levels of care.
Despite such an arrangement by levels, the
tertiary and secondary hospitals often
unnecessarily serve as first points of
contact for preventive and basic curative
services the product of a weak referral
system. All these facilities are directly
controlled and financed by the Department
of health and family welfare which
accounts for about 56 percent of total
hospital beds, the rest being provided by
other government departments (14%),
2
and the private sector (30%) (Figure 2.1) .
2.2.2. Services in the private sector, similarly, are delivered by a diverse group of service providers. This assortment includes
about 1700 private (for-profit and not-for-profit) hospitals, modern private practitioners, qualified Indian System of
Medicine (ISM) providers, traditional birth attendants, known as dais, and unqualified quacks. The share of this
sector especially in outpatient care market is much higher than that of public sector, both in terms of utilization and
out-of-pocket expenditure.
2.2.3. Adding to the complexity of the service delivery scenario is the dual role of the government health practitioner.
Although there is hardly any documented evidence, it is commonly accepted that many government practitioners
spend a significant portion of their time in private practice, thus blurring the line between public and private. Hence,
an individual who reports that her source of care is the private sector, may in fact be frequenting the after-hours
practice of a government doctor.
Private
30.0%
Government-
health
55.7%
Government-
Others
14.3%
Figure 2.1. Percent distribution of hospital beds
2
Source: Health on the March (2005-06), SBHIDHS, Government of West Bengal, p-83
Health, Equity and Poverty:Exploring the Links in West Bengal, India
8
2.3. Public Financing of Health Care in West Bengal: An Overview
2.3.1. In 1990, the state spent about Rs. 4600 million on
health which has more than quadrupled over the
next 15 years. Notwithstanding this impressive
hike in investment on health, relative share of
health in total budget, however, declined over the
same period. The decline has its root in growing
fiscal barriers which almost all Indian states have
been subjected to. The increasing fiscal pressure on
the state is quite evident in the fact that the
contribution of Revenue Deficit in Gross Fiscal
Deficit is higher in West Bengal than anywhere else
in the country (RBI, 2006). High and increasing
level of Revenue Deficit indicates a growing
burden of non-plan expenditure in a constrained
revenue-generating environment.
2.3.2. However, despite declining share of public health
expenditure, the government of West Bengal is one
of the top spenders on health on a per capita basis
(Figure 2.3). The per capita expenditure on health
was Rs. 186 (a little less than $5) in 2002-03.
2.3.3. The budget in each department is received and used
3 4
on four major accounts: (1) non-plan , (2) plan , (3)
5
Centrally Sponsored Scheme (CSS) , and (4)
capital account. Among them, non-plan
expenditure remains the major source of public
spending on health in all Indian states. As expected,
the lion's share of this expenditure goes to meet the
salary and wage bill of the staff leaving very
meager resources with the state to spend on
development or non-salary recurrent expenses.
Given the labor-intensity of public health care in
Figure 2.3. Per capita government
expenditure on health, 2003-03 (in Rs.)
86
108
122
147
157
175
176
181
181
186
194
208
210
237
286
0 50 100 150 200 250 300 350
Bihar
Uttar Pradesh
Madhya Pradesh
Orissa
Assam
Rajasthan
Gujarat
Haryana
Maharastra
West Bengal
Andhra Pradesh
Karnataka
Tamil Nadu
Kerala
Punjab
Per cap exp on health (Rs.)
Figure 2.2. Percentage of government health
spend to total budget (1990-2005)
0%
1%
2%
3%
4%
5%
6%
7%
8%
9%
1
9
9
0
-
9
1
1
9
9
1
-
9
2
1
9
9
2
-
9
3
1
9
9
3
-
9
4
1
9
9
4
-
9
5
1
9
9
5
-
9
6
1
9
9
6
-
9
7
1
9
9
7
-
9
8
1
9
9
8
-
9
9
1
9
9
9
-
2
0
0
0
2
0
0
0
-
0
1
2
0
0
1
-
0
2
2
0
0
2
-
0
3
2
0
0
3
-
0
4
2
0
0
4
-
0
5
2
0
0
5
-
0
6
% of health in total budget
Health, Equity and Poverty:Exploring the Links in West Bengal, India
9
3
Non-plan budget is the part of state budget that is spent for continuation of the programs, which were initiated in the previous plan and considered as
committed liabilities of the state. The recurrent part of the plan budget of an activity is usually transferred to the non-plan budget in the next plan period.
The assistance to fill the non-plan resource gap of the State is determined by the Finance Commission appointed by the Central Government.
4
Plan budget is the part of state budget that covers all expenditures, both capital and recurrent, incurred on programs and schemes that have initiated by the
state during the current five-year plan. The size of the total planned expenditure is determined through a negotiation of the state with the Planning
Commission, a non-statutory permanent body appointed by the Central Government.
5
Centrally Sponsored Schemes (CSS) is the central plan grants that directly finance some selected programs, such as Family Welfare program. Except
Family Welfare program, the central grant under this scheme finances only the plan component of the CSS program.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
10
India, the scenario is unlikely to change unless some strategic initiatives are taken to mobilize additional resources for
development.
2.3.4. The present scenario in West Bengal reflects this strategic move additional resources for planned (or, development)
expenditure as well as for non-salary items (such as, drugs) are pumped into the system to jack up non-salary expenses.
Consequently, the share of non-plan expenditure in total outlay reduced to about 71 percent in the recentbudget (2007-
08) from 77 percent in 2000-01. This has been possible due to two most important steps: (1) mobilizing internal
resources under State Plan; and (2) external supports (such as, budgetary support by DFID and the World Bank).
2.3.5. The districts are the basic implementation units of the state's health care programmes. The district health authority is
the ultimate outlet for using the central and state funds. The funds flow on two routes (1) through the district health
authority directly from the state's health department which primarily covers salary, maintenance and drugs, and
constitutes the major share of total fund flow; and (2) through an autonomous body, called District Health and Family
Welfare Samity (DHFWS) which primarily covers direct expenses of various vertical and centrally sponsored
schemes and constitutes less than 20% of total fund flow (excluding in-kind flows).
2.3.6. DHFWS is an extremely significant intervention to improvise decentralization in financing and decision-making at
the district level. It was formed in 2003 to establish a parallel channel of fund inflow to the districts especially in the
context of centrally sponsored public health programmes. Traditionally, the central funds for each of these
programmes used to flow through individual societies, such as District TB Society, District Leprosy Society, and so on.
These societies were autonomous and funds flowing through them were kept in separate accounts outside the
jurisdiction of public treasury. The individual societies were merged in 2003 to form DHFWS and brought under the
common administration of district health system. The underlying principal of fund flow to the society, however,
remained the same, i.e., the funds are primarily additional to the routine non-plan expenditure of the districts (salary,
drugs, administration cost, etc.) and are to be used exclusively on specific programme activities.
2.3.7 The state has a cost-recovery mechanism in terms of users charges levied on different services at higher-level hospitals
(i.e., tertiary hospitals, district hospitals, and sub-district hospitals). Traditionally, the revenues collected through this
process used to be deposited to state's treasury. However, in most recent times two radical steps have been taken to
ensure autonomy at the service delivery point: (1) formation of an autonomous society (Rogi Kalyan Samiti, or RKS))
at all tiers of facilities (from PHCs to teaching hospitals); and (2) facilities, where user fees are charged (e.g., sub-
divisional, district, and teaching hospitals), would be able to retain a pert of the generated revenue and the remaining
part will go to DHFWS. Impacts of these recent interventions are yet to be assessed, but existing evidences point out
that user fee could hardly recover a significant portion of the cost. For example, a study in 2004-05 [Public
Expenditure Review (2005)] on three sub-divisional hospitals (SDH) and three district hospitals (DH) showed that the
SDHs could recover only 1.56 percent of their total and 8.65 percent of their non-salary expenditure. The
corresponding figures for DH are 2.9 percent and 20.9 percent respectively.
2.4.1. There is now substantial evidence that, despite massive investment by the state governments on health care and heavy
subsidy flowing to primary care, the users of services are still spending a huge amount either directly or indirectly to
2.4. Private Health Care Spending
Health, Equity and Poverty:Exploring the Links in West Bengal, India
11
avail the services. For example, according to the estimates of a recent national survey (NSSO, 2004), an inpatient
from rural West Bengal spends Rs. 4582 approximately 16 percent of their annual household expenditure - on
hospitalization (corresponding national average is Rs. 6225).
2.4.2. The household survey carried out for FHS research (in three districts of West Bengal) reconfirms the phenomenon of
high out-of-pocket expenses (see Section 1.3 for methodology). Out of pocket expenses (OOPE) include expenses on
all medical expenses (such as, consultation, drugs, IPD charges, diagnostic tests, etc.) and relevant non-medical
expenses (for example, travel, board and lodging, etc.). Table 2.3 presents the mean OOP estimates for each of the
following categories of health care: (1) hospitalization; (2) outpatient; (3) chronic; and (4) birth delivery for all
districts taken together.
2.4.3. The estimated annual per capita (i.e., based on total population) OOPE for overall health care works out to Rs. 657 in
rural, Rs. 867 in urban areas, and Rs. 703 for overall. Based on the estimated per capita public spending on health in
2007-08 (Rs. 210), this accounts for about 77 percent of total government and households taken together expenditure
on health. On average, a rural household spends Rs. 3248 annually on curative health care and birth delivery which
works out to about 11 percent of its annual total consumption expenditure (the corresponding figures for urban areas
are Rs. 3852 and 8%).
In Rs.
Per household Per affected
household
Per user Per capita
Hospitalization 777 4331 3809 157
Outpatient 1092 1170 497 221
Chronic 1280 2633 1895 259
Birth delivery 99 592 392 20
Total 3248 8726 6593 657
Rural
In Rs.
Per household Per affected
household
Per user Per capita
Hospitalization 932 5141 4540 210
Outpatient 1102 1232 569 248
Chronic 1685 3023 2160 379
Birth delivery 133 1117 1117 30
Total 3852 10513 8386 867
Urban
Table 2.3. Estimated annual out of pocket payments for different categories of health care, 3
districts in West Bengal (in Rs.)
Health, Equity and Poverty:Exploring the Links in West Bengal, India
12
2.4.4. How much does an average household spend on
each of the four categories? Figure 2.4 presents
the distribution of share of each of them in total
medical care expenditure incurred by an average
household (rural and urban taken together).
Hospitalization appears to absorb about a quarter
of a household's medical care expenditure whilst
the expenditure on care for (acute) outpatients
and chronic patients accounts for about 73
percent of the same. The difference between
impacts of inpatient and outpatient care is quite
evident; the financial impact of hospitalization,
which may be disastrous to an affected
household (i.e., the household from where at
least one member was hospitalized) gets
substantially weakened when it is averaged
across all households (since it affects only about
4% of population). In comparison, the impact of
outpatient care is much less on affected
households but more on the whole society since
it affects almost all households.
2.4.5. The results presented in Table 2.3 do not indicate
a significant rural / urban differential with respect to per user OOPE in case of inpatient, outpatient, and chronic care.
For example, an urban resident, when hospitalized, would spend 1.2 times more in comparison to his / her rural
counterpart. The implication is that, on average, rural and urban residents utilize the same level of medical care when
they are hospitalized. The rural-urban differential is more prominent in case of birth deliveries because a large
number of rural women opt for a very cheap option of home delivery.
Figure 2.4. Percentage distribution of
OOPE, by health care categories, 3
districts, West Bengal
Hospitalization
24.0%
OPD
32.3%
Chronic
40.5%
Birth delivery
3.1%
3. Health, Equity and Poverty
Key Issues
3.1. Key issues
I. Health Care utilization
3.2. Good performance in ensuring horizontal equity in inpatient care
The analysis below highlights the following issues that policymakers can address to improve equity in financing, provision,
and use of health care services in West Bengal. These issues are broadly classified into two groups: (1) health care utilization;
and (2) health care financing. The issues are:
I. Health care utilization
Good performance in ensuring horizontal equity in inpatient care
Young and older women have less access to hospitalization
Government hospitals play dominant role, but without much targeting
Outpatient care market is dominated by unqualified providers
Strong barriers against equity in institutional delivery
Inequality in utilization of preventive child health care
II. Health care financing
Equity in public spending is questionable
Poor oversight at the district level
Medicines and test: killing fields
Out of pocket payment is progressive in inpatient care but not so in outpatient care
Growing health poverty in a socially unprotected environment
th
3.2.1. The NSSO 60 round survey in 2004 (NSSO, 2004) estimated total number of hospitalized cases (or, hospital
admissions) in India in a year to be about 2.60 percent of total rural and 3.48 percent of total urban population (Table
3.1). The corresponding estimates for West Bengal (NSSO-2004) are 2.48 percent and 3.94 percent. It is notable that
the estimated rates in 2004 were significantly higher than those in 1995-96 in India as well as in West Bengal (NSSO-
nd
52 round survey).
3.2.2. The last column of Table 3.1 presents the most recent estimates on hospitalization in West Bengal, generated from the
FHS survey in three districts. The estimates are higher than NSSO estimates but closer to the estimates of the
6
Department of Health & FW, Government of West Bengal . It is noteworthy that, overall, the hospitalization rates
have increased in the last 10 years across all socio-economic groups. The rising trend of hospitalization may be
partially explained by the state's persistent efforts to improve the accessibility to hospitals for admissions especially
through State Health System Development Project (SHSDP) implemented in late 1990s through early 2000s.
6
Officially, about 2.6 million cases (i.e., admissions) approximately 3.13% of the state population - were registered in public hospitals (excluding Block
PHCs) in 2005 (estimated from the official website of the Department of Health & FW, Government of West Bengal ). Adding
private hospitals' share and adjusting for average number of admissions per hospitalized person, the most likely estimate would be between 4.0- 4.2%.
- www.wbhealth.gov.in
Health, Equity and Poverty:Exploring the Links in West Bengal, India
13
Health, Equity and Poverty:Exploring the Links in West Bengal, India
14
The project focused on strengthening the secondary care hospitals all across the state through a sizeable investment on
infrastructure. It is, however, to be noted that urban hospitalization rate is higher than that of rural rate, possibly due to
easier access to hospitals and more choices an urban resident usually enjoys.
India West Bengal
NSSO
(1995-96)
NSSO
(2004)
NSSO
(1995-96)
NSSO
(2004)
IHMR
(2007)
Poorest 0.5 1.49 0.4 2.03 3.59
Next 20% 0.9 1.99 0.9 2.30 4.80
Next 20% 1.5 2.41 1.4 2.25 3.65
Next 20% 2.1 3.18 1.5 2.81 3.78
Richest 3.7 4.80 2.7 3.22 5.01
All 1.4 2.60 1.2 2.48 4.13
CI 0.37 0.23 0.30 0.08 0.035
Rural
India West Bengal
NSSO
(1995-96)
NSSO
(2004)
NSSO
(1995-96)
NSSO
(2004)
IHMR
(2007)
Poorest
Next 20%
Next 20%
Next 20%
Richest
All
1. 3
1. 7
2.0
2.7
3.8
2. 1
2. 67
3. 49
3. 68
3. 85
4.26
3.48
1.6
1.7
2.2
2.5
3.9
2. 3
3.55
3. 66
4. 32
3. 67
4. 71
3. 94
4.68
4.48
4.04
5.39
4.57
4.62
CI 0.22 0.08 0.18 0.05 0.012
Total
hospitalization
rate (%)
1.7 2.82 1.5 2.83 4.23
Urban
Table 3.1. Rate of hospitalized cases (% of population) in India and West Bengal
3.2.3. How equitable is the hospitalization rate? Does a poor have equal chance to be hospitalized in comparison to a rich
person when they have equal need for hospitalization? The answer is given in terms of concentration index (CI)
presented in the last row of Table 3.1 (see Box 3.1 for a brief note on CI) and representing the degree of inequity in the
rates. It is evident that CI has been sharply progressing towards 0 a state of horizontal equity in West Bengal over the
last ten years (from 0.3 and 0.18 in 1995-96 to 0.035 and 0.01 in 2007, respectively for rural and urban residents)
while the national figure still indicates a significant pro-rich bias especially for rural cases. In other words, a poor and
a rich person have almost equal access to inpatient care in West Bengal it is neither pro-rich nor pro-poor - while,
nationally, the better-offs tend to use more inpatient care.
Box 3.1. Concentration Index (CI)
Concentration index (CI) is a standard tool universally used by the economists to measure the
degree of inequality in various health system indicators, such as health outcome, health care
utilization, and health care financing [Wagstaff, Van Doorslare, and Paci (1989)]. Its value ranges
from -1 to +1. A negative value of CI implies that the relevant health variable is concentrated
among the poor or disadvantaged people while the opposite is true for its positive values. For
example, if the health indicator were Infant Mortality Rate (IMR), a negative CI would imply that
mortality rate is higher among the poorer infants; if it is immunization and CI is positive, richer
children are proportionately more immunized than their poorer counterparts are. When there is no
inequality, CI will be equal to zero. Typically, a zero CI implies a state of horizontal equity which is
defined as equal treatment for equal needs.
In Table 3.1, rate of hospitalization is the relevant health related indicator. A positive CI means that
persons from the richest group get more hospitalized compared to the poorer groups. A pro-poor
strategy for inpatient care should reduce the CI towards a negative value.
The CI values in Table 3.1 were computed by the following three steps (for details, visit
or contact author).
Step 1
First, the population were ranked according to their monthly per capita consumption expenditure
(MPCE); second, the ranked population were grouped in five ascending quintiles (population in
quintile 1 is the poorest and the same in quintile 5 is the richest); and third, number of hospitalized
cases for each quintile was computed by multiplying number of hospitalized persons in each
quintile in a year with how many times they were hospitalized.
Step 2
First, the cumulative percentage of sample population (from quintile 1 through 5) was calculated
this is denoted as p (t=1,,5). Second, the cumulative percentage of estimated cases (from
t
quintile 1 through 5) was calculated this is denoted as L (t = 1,,5).
t
Step 3
Finally, the concentration index is computed by applying the following formula:
CI = (p L - p L ) + (p L - p L ) + ..+ (p L - p L )
1 2 2 1 2 3 3 2 4 5 5 4
The standard errors of the estimated CI were also computed following the methodology given in
the above reference.
www.worldbank.org/poverty/health/wbact/health_eq.htm
Health, Equity and Poverty:Exploring the Links in West Bengal, India
15
Figure 3.1. Female-male ratio in
hospitalization (3 districts, West Bengal)
0
20
40
60
80
100
120
140
0-14 15-29 30-44 45-59 60 + Total
Age-group
F-M ratio
3.3. Young and older women have less access to hospitalization
3.3.1. Notwithstanding a progress towards more equity in overall hospitalization, one may ask question on gender equity.
For assessing gender perspective in hospitalization, female-male ratio was computed by the following way. First,
female cases per 100 female population and male cases per 100 male population were estimated for each of five broad
age-groups, and second, female rate was divided by male rate and multiplied by 100 to estimate Female-Male (F-M)
ratio. Assuming that need for hospitalization is more or less same between a man and a woman (excluding
hospitalization due to birth deliveries), gender equity is achieved when the ratio is equal or close to 100.
3.3.2. Figure 3.1 presents the F-M ratio for all age groups. It is quite evident that a young girl or an older woman is less likely
to be hospitalized in comparison to their male counterparts. Interestingly and contrarily, the bias against male is quite
prominent in the middle age groups where F-M ratio is significantly greater than 100. Overall, the ratio works out to
be 88 indicating slight bias against females.
3.3.3. Bias against female hospitalization may be explained by the barriers a woman usually faces when she accesses
medical care. These barriers are often prohibitively high especially for inpatient care - treatment is expensive,
inpatient facilities are far away, staying away from home is unaffordable, and so on. Add to this the usually low
perceived severity and high degree of neglect for women's health problem which are not related to childbearing. The
bias against men in their middle age may be partially attributed to their bread-earners' role which often prohibits them
from spending days in hospital.
3.4. Government hospitals play dominant role, but without much targeting
3.4.1 West Bengal is one of the very few states where most people use government hospitals for inpatient care. While
private sector has been expanding its share in the inpatient care market at the national level - from 40 percent of all
hospitalized cases in 1986-87 to about 60 percent in 2004 by NSSO estimates West Bengal remains more like an
exception. According to FHS household survey in three districts, only 18 percent of all hospitalized cases sought
treatment in private hospitals.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
16
Figure 3.2. Share of government and private hospitals in total hospitalized cases, by socio-
economic groups
28
36
43
47
56
72
64
57
53
44
0%
20%
40%
60%
80%
100%
Richest Poorest
Government Private
64
83
88 87
91
36
18
13 13
9
0%
20%
40%
60%
80%
100%
Richest Poorest
Government Private
India West Bengal
Source: NSSO (2004) Source: IIHMR (2007)
3.4.2. Absolute dependence of people on government hospitals in the state may be explained by weak presence of private
hospitals in all districts barring a few pockets. A pertinent question is: does this overwhelming presence of
government (in inpatient care) reflect a better pro-poor strategy? The concern for equity forms a key element in
government interventions in health. It is now well accepted that public provision and funding of health care should
primarily target those who, irrespective of their health status, cannot afford to buy health care or pay the insurance
premiums. In other words, in a resource-scarce environment, the public sector should subsidize the neediest segments
of a population. Consumers who are able to pay for services will do so in the private sector where it exists.
3.4.3. The right panel of Figure 3.2 presents the relative share of government hospitals in West Bengal. For comparison, the
relevant NSSO estimates for India are also presented in the left panel. As expected, almost all of the poorest inpatients
(91%) in West Bengal sought admission in government hospitals, but the data also reveals that about two-third of
patients in the richest group had chosen government hospitals for inpatient care implying that public subsidies also
benefit a large section of high-income population who may not need subsidies.
3.4.4. The evidences in Figure 3.2 indicate a near-perfect horizontal equity in utilization of government hospitals (i.e., equal
treatment for equal needs irrespective of socio-economic differential) in West Bengal whilst the Indian scenario
presents a clear and more desirable pro-poor bias. However, one can also argue that it is neither desirable nor feasible
to prohibit richer section from using government hospitals especially when (1) private hospitals are inadequately
available in most of the districts; and (2) apparently the high utilization by the poorest section remains unaffected
implying that poor's interest is still well-protected even if they are not targeted. The argument, which is apparently
sound, may fall flat if there is any crowding out effect in the public facilities especially in the case of hospitalizations
and birth delivery. In other words, a relevant question would be: is there substantial number of poor patients who
could not get admissions in public hospitals because subsidized beds are already occupied by the better-off patients?
Or, alternatively, did some poorest women have to deliver babies at home because those, who were occupying free
beds despite their higher ability to pay, crowded them out? The anecdotal evidences seem to support this hypothesis,
but, no hard evidence has been produced by the studies carried out so far.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
17
3.5. Outpatient care market is dominated by unqualified providers
3.5.1. Despite a strong infrastructural base of the public health care facilities in many Indian states, the majority of outpatient
services, especially in the rural areas, are provided by private health care providers, most of whom practice modern
allopathy without any formal training. This section of medical practitioners is often identified as Rural Medical
Practitioners (RMPs), unqualified, less than fully qualified (LTFQ) providers, or simply quacks. West Bengal
is no exception, where, according to the National Family Health Survey (NFHS-II) conducted in 1995-96, about 60
percent of the households visited the private medical sector for outpatient care when they fell sick. Although NFHS-II
did not classify private doctors according to their qualification status, researchers and policy makers alike concur
that a large section of them belongs to RMP category.
3.5.2. The evidences collected through FHS research
reconfirm dominance of RMPs in outpatient
care market especially in the rural areas of three
study districts. As Figure 3.3 shows, about 46
percent of outpatient clients sought treatment
from RMPs while government sources were
visited by 21 percent. However, the estimate
regarding utilization of government facilities
(21%) seem a bit underestimated when one
compares it with supply side information (see
Box 3.2).
3.5.3. The FHS research focused on those RMPs who
practiced modern allopathic treatment without
being formally trained to do so. The set
includes those (1) who practice without any
formal training on any stream (allopathy,
homeopathy, ayurvedic, etc.); (2) who graduated in medicine from any unrecognized organization; and (3) who
graduated in a non-allopathy stream but practicing allopathy. Household survey apart, data were collected from two
other sources: (1) exit interviews of selected outpatients and inpatients in selected government health facilities in three
study districts, and (2) in-depth interviews with 71 RMPs. In each case, the interview was conducted by using a
structured questionnaire.
Figure 3.3. Percent distribution of persons
seeking outpatient care, by major sources of
care (3 districts, West Bengal)
22.9
14.7
18.8
13.4
20.9
20.2
53.7
40.3
46.2
0
10
20
30
40
50
60
RMP Govt source Private qualified
Rural Urban Total
Health, Equity and Poverty:Exploring the Links in West Bengal, India
18
Health, Equity and Poverty:Exploring the Links in West Bengal, India
19
Box 3.2. A quick calculation of the share of government facilities in total outpatient
visits, 2005
According to government source ( ) total number of outpatient visits was
about 43 million in the year 2005. A quick back-of-the-envelope computation will be as follows:
(i) Total outpatient visits in a year = 43 million (approx).
(ii) Average annual number of outpatient visits by a person = 1.77 (from FHS survey)
(iii) Hence, total number of OPD visits (including all sources) in the state = Total
population 1.77 = 150 million (approx.) assuming total state population=8.5
million
(iv) Share of government facilities in OPD care = 43 million 150 million = 28.7%
see www.wbhealth.gov.in
3.5.4. Table 3.2 presents data on households' health care seeking behaviour in case of outpatient care. The table is based
on the detailed information on those household members who actually suffered from any type of ailment and
sought outpatient care in the last 90 days preceding the survey.
3.5.5. The strong presence of RMPs is quite evident in Table 3.2. Among the 5284 rural and 1450 urban patients, who
sought treatment for their minor health problems from various sources, about 54 and 19 percents respectively,
were treated by RMPs.
Table 3.2. Percentage of affected persons actually sought
treatment from RMPs, by per capita expenditure quintiles,
3 districts, West Bengal
Rural Urban
3.5.6. There is a common perception that treatment by RMPs is much cheaper than other alternatives; hence, only poor
clients visit them. The evidence, however, stands against this perception, especially in rural areas. As shown in Table
3.2, the utilization of RMP services in rural areas is almost uniformly spread across various socio-economic groups.
Equal distribution (with respect to socio-economic status) in utilization of RMP services in rural areas implies that it is
not only lighter economic burden, but also some other factors, which direct the rural people to RMPs. This is also
evident from Figure 3.4 where the average out-of-pocket payments for treating minor ailments are presented.
3.5.7. Figure 3.4 reveals that visit to a government facility in
the rural area for non-hospitalized treatment would
cost as much as it will to a RMP (about Rs. 75)
although the same can not be said about an urban
government facility where it costs almost double. The
question is: why do rural people across all categories
prefer RMPs to public health care centres if both are
equally cheap (or, expensive)?
3.5.8. The study attempted to identify possible answers to the
above question from the household survey. The three
most important reasons for choosing RMPs (as
identified by the percentage of respondents) are: (1)
close location (74%); (2) always available (65%), and
(3) cheap (61%). The other two reasons, not as
important as the above three, are: (4) availability of
medicines (27%), and (5) scope to pay later or by
installments (25%).
3.5.9. That proximity is one of the most important factors for
the spread of RMPs is also evident from Figure 3.5
where the average distances of various sources of care
from the respondents' residences are plotted. On
average, a rural resident has to travel less than a
kilometre (0.68 km) to visit a RMP; the distance
becomes double (1.48 km) if it is a public health centre
and about ten times more (6 km) if it is a clinic of a
private qualified doctor.
3.5.10. Physical accessibility, however, explains the demand
side only partially. A public facility, even if it is closely
located to a village, may be bypassed due to non-
availability of a regular doctor. All medicines
prescribed by a PHC doctor may not be available
within the facility. Consequently, the patients have to
remain prepared to pay upfront for the medicines they
would purchase from private pharmacies. Moreover, the prescribed medicines, which are purchased from
pharmacies, may not always be of the cheapest brand. RMPs feed on the above weaknesses of the public health care
system. They are usually always available, closely located, and sell medicines as a part of their service often on credit.
Clearly, their operations manifest the simple economic phenomenon that a market, when it fails to deliver, begets a
parallel but efficient alternative.
Figure 3.4. Average out-of-pocket payments
for treatment of minor ailments, by sources
of treatment (in Rs.)
73.5 74.6
339
67.8
137.5
231.9
0
50
100
150
200
250
300
350
KM
Rural Urban
RMP Public Private qualified
Figure 3.5. Average distance to sources
of treatment for outpatient care,
(in Kilometers)
0.68
1.48
6
0.37
0.66
1.34
0
1
2
3
4
5
6
KM
Rural Urban
RMP PHC Private clinic
Health, Equity and Poverty:Exploring the Links in West Bengal, India
20
3.5.11. The in-depth survey of 71 RMPs and their associations in the three districts identified the following characteristics of
the RMPs:
Most of them (58%) were non-graduates.
On an average, a RMP treated about 600 cases per month. About 14% of the users were children (below
5 years)
More than half of them (56%) acquired some sort of degree from unrecognized private institutions.
On an average, an RMP earned around Rs. 3250 per month.
3.5.12. The RMPs usually provided services for minor ailment although a minor fraction (6%) also provided preventive care
(immunization). A majority of them (72%) also did minor surgeries. About one-third of them assisted in birth
deliveries. Almost all of them (90%) responded to house calls. Dispensing drugs with treatment is one of the key
attractive services provided by RMPs. About 90 percent of the sample RMPs were found to follow this practice. A
majority of them (70%) procured drugs from the local chemist shop. The other source was wholesale market from
where one-fifth of them procured drugs.
3.5.13. The most common diseases treated by the RMPs were: diarrhea / gastro-enteric disorders (97%) and common cold /
cough / fever (83%). The typical procedure for treating a child with diarrhoea was to put him / her on saline and give
him / her anti-diarrhea medicine.
3.5.14. Do RMPs refer potentially or actual complicated cases to public facilities or qualified private doctors? The common
perception is that they do it only when cases go completely out of their control. Data collected from the selected
RMPs partially confirm the perception. An RMP would hardly refer a case of common diseases such as diarrhea or
fever, irrespective of its potential complications or chronic nature. This is quite evident from Figure 3.6 where the
sample RMPs' responses (about the status of children after they were treated by them in the last three months) are
presented.
3.5.15. Despite the response bias (since data were
collected from the RMPs), it is worth noting that
only about 10 percent (1668 out of 16842
children) of the children were referred to formal
providers. The children under rest category
were not cured; however, due to data limitations
it can only be assumed, but not confirmed, that
most of them switched over to formal providers
or to another RMP.
Figure 3.6. Distribution of children treated by
the sample RMPs in the last 3 months, by status
after treatment (total 16842 children)
cured
69.50%
died
0.31%
referred
9.90%
rest
20.28%
Health, Equity and Poverty:Exploring the Links in West Bengal, India
21
3.5.16. Do RMPs act as a bunch of thorns in the existing health care system, or do they act as a good balancing factor in
maintaining rural health? The study stops short of drawing any conclusion on this issue due to its limited scope, but
available evidences highlight a few points:
(i) Irrespective of health outcome, RMPs have established a strong network of health care, especially in
rural West Bengal, primarily due to easy accessibility and attractive low-cost packaging. Since there
is no effective barrier to entry into the market, the market share of these providers is likely to increase
in future.
(ii) However, without any effective regulatory mechanism, the quality of care provided by RMPs remains
completely uncontrolled. Consequently, the risk of doing harm is significant, especially in cases
where careful diagnosis or surgical operation is required (see Box 3.3). The risk is further aggravated
particularly because many people do not even know that RMPs are not real doctors.
3.5.17. The household survey informed that more than 80 percent of hospitalized persons sought admission to government
hospitals (see Figure 3.2). However, a different picture emerges when one looks at the pre-admission phase of the
hospitalized persons. About 60 percent of rural hospitalized persons had initiated their treatment with RMPs. They
carried on pre-hospitalization treatment for an average of 33 days and spent Rs. 1400 on average. In other words,
there is a strong indication that a large section of rural patients hang on with the RMPs before they get hospitalized
probably with more complications developed. The implication of this finding is that the burden of disease and cost of
treatment would be substantially reduced for a large number of hospitalized persons if their pre-hospitalization spell
with RMPs could be minimized.
3.5.18. Notwithstanding the risks involved in the spread of RMPs, their positive contributions to rural health can hardly be
exaggerated. This is especially true where the alternative to RMPs' service is no treatment (see Box 3.4).
Health, Equity and Poverty:Exploring the Links in West Bengal, India
22
Box 3.3 A narrow escape
Akhil Pal, a rag-picker, visited Kaliachak
BPHC (Malda district) with a swelling on
his head. The doctor at the BPHC
diagnosed it as a tumor and advised
immediate surgery. Scared of operation
and yet unable to bear the increasing pain,
Akhil went to a local RMP, who is known
to be a multi-therapist, practicing so many
pathies simultaneously and healing
multifold ailments. He guaranteed Akhil
of a prompt cure, administered several
injections around the tumor, and started
operating upon the protruded part. Half-
way in the process, and after the unkindest
cut, he coolly informed that the operation
may eventually end up in cancer, and
called it quits. A frightened Akhil, still
bleeding profusely from 'operated head'
was taken again to the BPHC.
Source: FHS survey, 2007
Box 3.4 An alternative to no care
Sumi t r a Mondal , a r esi dent of
Borosheyana village, was admitted to Taki
Rural Hospital (N 24 Porgona) for birth
delivery. Sumitra complained of severe
abdominal pain and discomfort, but was
not attended to by the hospital staff, who
dismissed her complaints rendering it to be
'normal' in case of delivery patients. With
increasing pain and still being unattended,
Sumitra was taken back towards home.
Back in her village she was attended to by
a local RMP at his dispensary, who
administered injections and medicines to
ease her pain considerably. In the next few
hours, the RMP assisted Sumitra to have a
normal delivery.
Source: FHS survey, 2007
3.6. Strong barriers against equity in institutional birth delivery
3.6.1. There are at least four estimates available on
the current status of institutional delivery in the
state (Figure 3.7). According to the recent
National Family Health Survey (NFHS-3),
about 43 percent of total births in West Bengal
are delivered at government and private
institutions (33.8% in rural and 79.2% in urban
areas). Another household survey conducted
for RCH program (RCH-II DLHS, 2004) also
generated similar estimates (46%). The NSSO
survey (6oth round) conducted in 2004, on the
other hand, came up with a much higher
estimate (56.3%). Finally, the estimates
derived from IIHMR's FHS survey in 2007 are
almost the same as NSSO estimates (55.9%).
3.6.2. Notwithstanding variation in estimates,
increasing institutional delivery is one of the top priorities to the policy makers of the state although NFHS estimates
show only a little progress in this case the rate of institutional delivery just increased by 3 percent points in the last ten
years, from 40.1 percent in 1995-96 (NFHS-2) to 43.1 percent in 2005-06 (NFHS-3). The question, subject to validity
of NFHS estimates, is: why progress in this area is so slow compared to that in other areas?
3.6.3. Conceptually, the answer remains in perceived benefits and various barriers to access an institution for birth delivery.
Perceived benefits (of institutional birth delivery) are low due to the common belief that birth delivery is a natural
process and, hence, it requires no hospitalization. However, equally important are the barriers (or, cost) to access.
Three important barriers are extremely relevant in this case: (1) long physical distance to the nearest facility, (2) higher
out of pocket expenses to seek birth delivery care from an institution, and (3) poverty.
3.6.4. Table 3.3 shows that the above three barriers indeed play important roles in this context. For example, women, who
delivered birth at government hospitals, had to travel 14 km on average to reach the facility whilst women who
delivered at home would have to travel 24 km had they decided to deliver at any institution. In other words, there is
apparently a negative correlation between distance and institutional delivery. Similarly, there is a strong ground for
hypothesizing that higher out of pocket expenses for institutional delivery force many women to deliver births at home
for example, OOPE for home delivery (Rs. 343) was only 40 percent of the same for delivery at a government hospital
(Rs. 848).
3.6.5. That poverty or economic constraint plays an important determinant behind choice of place of delivery is also evident
from the data that 62 percent of all in the poorest quintile but only 19 percent of all in the richest quintile delivered at
home clearly implying that barriers get easier as one progresses from poorest to richest quintile. The above evidence
points out to a glaring dichotomy: while the state has reached a desired level of equity in general inpatient care,
43.1
46.3
56.3
55.9
0 10 20 30 40 50 60
NFHS-3
RCH-II
NSSO
IIHMR
% of inst birth
Figure 3.7. Percentage of institutional birth
deliveries in total births, by different data sources
Health, Equity and Poverty:Exploring the Links in West Bengal, India
23
Table 3.3. Birth delivery and associated information,
by place of delivery (3 districts of West Bengal)
For those who
delivered at
% of total
delivery
Average
distance to
the nearest
facility
(km)
Per user
OOPE (Rs.)
normal
delivery
% of
women in
poorest
quintile
delivering
birth at
% of women
in richest
quintile
delivering
birth at
Institutions
in which
55.9 14.3 1158 38.4 80.7
Government
hospitals
47.4 13.9 848 35.7 56.8
Private hospitals 8.5 20..2 4233 2.7 .23.9
Home 44.1 23.8 343 61.6 19.3
3.6.6. It is also important to note how the targeting principle is totally blurred in case of institutionally delivery. As expected,
almost all women in the poorest quintile who delivered away home used public facilities (35.7%, while total
institutional delivery was 38.4%); but the data also reveals that 70 percent of women in top quintile, who delivered
away home, had chosen public facilities (56.8%, while total institutional delivery was 80.7%) despite the fact that they
could probably afford to pay private market price.
3.6.7. Table 3.3 presents a descriptive picture of the possible barriers to institutional delivery. It is also important to know
their relationship in a more precise term. More specifically, a broader question should be addressed: what factors do
facilitate or impede institutional delivery? Who are more likely to seek institutional care for birth delivery? The
likelihood can be statistically estimated by odds ratio in a multivariate framework (see Box 3.5).
maternity inpatient care remains significantly inequitable. Two plausible explanations for such discrepancy are:
(1) a cheaper option (i.e., home delivery) is available in the latter case while non-maternity inpatient care has no
alternative except accepting death or disability; (2) the perceived risk (or, opportunity cost) of not seeking
institutional care is much less in case of maternity cases.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
24
Health, Equity and Poverty:Exploring the Links in West Bengal, India
25
Box 3.5. Who is more likely to seek institutional care for birth delivery?
Odds ratio is commonly used in binary outcome models (i.e., where the dependent variable is
coded as 1 or 0) to answer a question as asked above. It estimates the odd of occurring an event for
a particular group in comparison to another group (or, reference group). The ratio ranges from 0 to
infinity.
Table 3.4 presents odds ratios with respect to a set of independent variables estimated through a
logistic regression model where dependent variable is institutional birth delivery in three districts
of West Bengal (institutional delivery = 1, non-institutional delivery=0). All independent
variables (except Distance and Age) are grouped with at least one group kept as a reference
variable.
The results may be interpreted in the following way: the odds ratios for Malda and Bankura are
0.46 and 2.76 respectively implying that a woman in Malda district is much less likely and a
woman from Bankura is much more (2.76 times) likely to seek institutional care in comparison to
their counterparts in N. 24 Porgonas. Similarly, a woman from a top income group (Richest
quintile) has odds 2.39:1 in her favor in comparison to a woman in the poorest quintile clearly
indicating a sharp inequity in institutional delivery.
Table 3.4. Estimated Odds ratios for institutional delivery in 3 districts of West Bengal
Variables
Reference
variable
Odds
ratio
District
Malda N.24 Porgonas 0.46
*
Bankura N.24 Porgonas 2.76
*
Economic status
Poorest quintile (quin tile1) Quintiles 2 4 0.47
*
Richest quintile (quintile5) Quintiles 2 4 2.39
*
Social category
Hindu Non-Hindu 3.02
*
SC/ST Non- SC/ST 0.54
*
Residence
Urban Rural 2.75
*
Accessibility
Distance 0.66
*
Individual factors
Age 0.98
Up-to primary education More than
primary
0.57
*
N = 492
p<0.05
The results also show how distance acts as a barrier. The odds ratio for distance is much less than
1 indicating that, all other things remaining the same, an increase in distance would adversely
affect the odd or likelihood of seeking institutional care. As expected, women with no or little
education also are less likely to seek institutional care in comparison to educated women.
However, age of a woman does not have statistically significant link to the probability of
choosing the place of delivery.
3.7. Inequality in utilization of preventive child health care
3.7.1. Preventive health care for the children is still an area where some degree of inequity exists. Table 3.4 shows that there
is no significant difference in immunization rate across gender or rural / urban location, but inequality exists with
respect to socio-economic groups (concentration index is close to 0.1). In other words, poverty is an important
dimension to explain the inequity in preventive care. The scenario is much better in curative care where the
probability of seeking treatment for a sick child is more or less same across gender, rural/urban, and socio-economic
differential (concentration index is close to 0 for male and <0 for female).
Table 3.4. Percent distribution of fully immunized and diarrhea-treated children, by rural /
urban, sex, and socio-economic groups, West Bengal
% of fully immunized children % of diarrhea-affected
children treated
Asset quintiles Male Female Male Female
Poorest 31.75 33.11 68.52 79.41
Next 20% 34.18 32.81 66.67 82.35
Next 20% 34.80 36.25 80.95 70.59
Next 20% 41.27 39.71 70.97 52.94
Richest 51.85 53.23 69.23 76.47
CI 0.098 0.097 0.006 -0.04
Rural
% of fully immunized children % of diarrhea-affected
children treated
Asset quintiles Male Female Male Female
Poorest 35.57 31.61 100 66.67
Next 20% 40.61 39.35 60.00 62.50
Next 20% 50.81 54.70 66.67 66.67
Next 20% 53.40 54.87 66.67 75.00
Richest 58.12 57.43 100 33.33
CI 0.097 0.112 0.007 -0.07
Urban
3.7.2. The link between poverty and lower rate of immunization may have various roots. Achievement in immunization is
directly linked to the strength and effectiveness of outreach services. Barriers to these services include (1) adverse
geographical location, (2) absenteeism and / or inadequacy of grassroots workers, (3) low perceived needs, and so on.
It is a common experience that these barriers are more prohibitive for economically disadvantaged people especially
in rural areas.
3.7.3. West Bengal has demonstrated an impressive record of progress in immunization coverage. For example, by NFHS
estimates, the percentage of fully immunized children in the state has reached about 64 percent in 2005-06 (NFHS-3)
from a mere 34 percent in 1990-91 (NFHS-1), compared to the national progress from 36 percent to 44 percent during
the same period. About three-fourth of all children in the state received measles vaccine in 2005-06 compared to 42
percent in 1990-91 (the corresponding national figures are: 59% and 42%). Despite such progress, the concern
remains among the state's key decision-makers whether and to what extent the barriers (see 3.7.2) act against
Health, Equity and Poverty:Exploring the Links in West Bengal, India
26
Source: RCH-II DLHS, 2004
achieving the goal of universal immunization. It is expected that the FHS research programme would provide
adequate evidences on this issue through its Phase-2 research to help the government draw up an appropriate strategy
for universal immunization. This would be done through (1) mapping un-served and under-served areas; (2)
identifying the major underlying barriers (geographical, or administrative, or other factors); and (3) outlining a
concrete strategy on how to improve the coverage in those areas.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
27
Health, Equity and Poverty:Exploring the Links in West Bengal, India
28
II. Health Care Financing
7
3.8. Equity in public spending is questionable
3.8.1. Apart from out of pocket payments, public finance is the only other major source of health financing in India. The
question is: are public subsidies equitably distributed? An attempt was made to distinguish between spending aimed
at rural and urban areas in West Bengal. The figures probably underestimate the share going to rural areas as it
assumes that teaching facilities spending is in urban areas (it is - but some benefits rural areas) and that hospitals only
serve urban populations (which is nor necessarily true). Based on these simplified assumptions the findings suggest
that rural population (which is a majority) receive about 40 percent of public budget. The distribution of drugs is
considerably biased towards urban population (80 percent against 20 percent going to rural).
Table 3.5. Percentage allocation of government budget by location and use (2005-06),
West Bengal
Salaries and
Wages
Office
Expenses Maintenance Drug Diet Other Total
Rural (%) 43.9 42.1 36.4 20.1 30.5 42.0 41.3
Urban (%) 54.7 57.0 63.5 79.8 69.5 57.2 57.6
National (%) 1.4 0.9 0.1 0.1 0.0 0.8 1.1
Total (%) 100.0 100.0 100.0 100.0 100.0 100.0 100.0
Source: Budget Estimates 2005/6 Demand for Grants No 24
3.8.2. The ways in which resources are used can be described in a number of other ways. Table 3.6 below shows how the key
programmes relate to the main functions of the Department of Health and FW stewardship (the oversight role) the
provision of intermediate goods (such as training medical staff) and the actual delivery of goods as well as efforts to
increase the demand for services.
Table 3.6. Programmes according to functions
Stewardship Provision of
Intermediate Inputs
Delivery of Services Demand
Creation
Government Administration
Direction and Administration
(Central/M&PH/FW)
Direction and Administration
(District)
Grants to Councils/Regulatory
Bodies e.g. Pharmacy Council
Health Statistics and Evaluation
Regulation
Food Adulteration
Drug Control
Public Health Laboratories
Medical/Other Training
Support for Medical
Colleges
Grants to other training
institutions
FW training
Transport
Production of Vaccine
and Sera
Health Facilities
Teaching Hospitals
Hospitals and Dispensaries
Grants to NGOs
Special Programmes for the Poor
Other Hospitals
Medical Stores Dept
Primary Services
PHCs/Dispensaries
U&R FW Services
MCH
Other Systems of Medicine
Tribal/SC
Compensation (demand side
financing)
Health Education - School
Health/Public Education
Health
Education
7
This section draws heavily on Public Expenditure Review (2005).
3.8.3. Table 3.7 suggests that over 80 percent of resources are used to provide services with very little explicitly focused on
demand creation which needs to be considered in the light of low levels of utilization in many primary care facilities.
It also suggests that spending on the provision of inputs is less salary intensive than other forms of support. It also
shows that the 2005-06 budget estimates propose an increase in the share of resources being devoted to the production
of inputs at the expense of service delivery.
Table 3.7. Percentage allocation of Resources by Function, West Bengal
2003/4 Actuals 2004/5 RE 2005/6 BE
Service Delivery
Intermed Inputs
Stewardship
Demand Creation
85.0
9.3
5.6
0.1
83.4
10.6
5.9
0.1
82.0
12.6
5.3
0.1
Source: Public Expenditure Review (2005)
3.8.4 Other distinctions can be made in terms of whether the provider of services is in the public sector or whether there is
contracting with the private sector (e.g. NGOs). It will be important to track this in light of the new policy on public
private partnership to assess whether significant amounts of resources are being transferred to private providers. At
present although Government provides grant to a large number of non-government bodies and institutions together
(excluding Panchayet) such flows only account for around 1% of total spending.
3.8.5. How the public funds are
geographically allocated?
Fi gur e 3. 8 r eveal s no
significant inequality in this
area except in three districts
( Ko l k a t a , Na d i a a n d
Darjeeling). However, it is
also evident that more
backward districts especially
in the northern parts of the
state (Malda, North and
South Dinajpur) reflect a
comparatively lower bed-
population ratio.
3.8.6. Figure 3.9 shows estimated
expenditure for selected
hospital facilities. Here, by
looking at the key budget
lines it would appear that
di s t r i c t hos pi t a l s a r e
relatively underfinanced compared to other types of hospitals. A rather surprising finding is that state general
hospitals seem to receive significantly higher allocations on a per bed basis than district hospitals whose allocations
are comparable with those of much smaller sub divisional hospitals. Moreover, there are significant differences
-
PHC
BPHC
Rural Hospitals
Other Hospitals
State General Hospitals
Sub Divisional Hospitals
Distrcit Hospitals
Medical College and Hospitals
Health Infrastructure:
Beds per Million Population
500
1,000
1,500
2,000
2,500
3,000
B
a
n
k
u
r
a
B
a
r
d
d
h
a
m
a
n
B
ir
b
h
u
m
D
a
k
s
h
in
D
in
a
jp
u
r
D
a
r
jilin
g
H
a
o
r
a
H
u
g
li
J
a
lp
a
ig
u
r
i
K
o
c
h
B
ih
a
r
K
o
lk
a
ta
M
a
ld
a
M
u
r
s
h
id
a
b
a
d
N
a
d
ia
N
o
r
t
h
2
4
-
P
a
r
g
a
n
a
s
M
e
d
in
ip
u
r
P
u
r
u
li
y
a
S
o
u
th
2
4
-
P
a
r
g
a
n
a
s
U
t
ta
r
D
in
a
jp
u
r
T
o
t
a
l
b
e
d
s
p
e
r
m
i
l
l
i
o
n
Figure 3.8. Beds per million population, by districts and
by types of government facilities, West Bengal
Health, Equity and Poverty:Exploring the Links in West Bengal, India
29
between estimated expenditures within
these categories. This would warrant
further investigation. Further analysis
shows that not only is there a significant
difference in terms of allocations to
different types of facility but that are also
significant differences in allocations
between similar types of facility. The fact
that the official bed complement does not
reflect actual practice (i.e., there exists
di screpancy bet ween act ual and
sanctioned number of beds) may account
for part of this but there are still wide
variations which are unexplained.
3.8.7. Despite discrepancies in resource
allocation, the state reflects a reasonably
good pro-poor image of policymaking. This is quite evident in several policy decisions improvised during the last few
years. This includes: (1) strengthening of secondary care facilities all across the state; (2) increasing drug supply; (3)
delegating more autonomy to he districts; (4) allocating untied funds for medical assistance to the poorest; (5)
involving local self-administration (Panchayet) in local decision-making process; and so on. The policies also got
momentum due to recently launched Health System Development Initiative (HSDI) program. The question is:
whether and how these policies are implemented at the district level and below.
3.9.1. Is there any mechanism at the district level by which a poor or a vulnerable could be identified and protected from
impoverishing effect of health care? Apparently, the health functionaries do not have a clear mandate on this issue.
The underlying principal of using funds is to channelize them by line items leaving little scope to improvise local
solutions for protection of poor and vulnerable. The only way a poor receives special attention is his /her exemption
from paying user charges at the hospital. Due to a blurred exemption policy and in absence of a proper identification
mechanism, this policy is often abused to an extent where a government hospital exempts more than 90 percent of its
clients from paying user charges (IIHMR, 2004). Further, the exemption policy does not protect poor from spending
on medicines and diagnostic tests due to their non-availability at the facility level (see Section 3.10).
3.9.2. Obviously, a pro-poor strategy requires an effective oversight mechanism at the local level that could track the
linkages between received funds and the consequent performance of a district in achieving equity goals. Three
important prerequisites for such local oversight are: (1) flexibility in utilizing the funds, (2) an efficient resource-
tracking mechanism, and (3) interest and capacity of local health managers to link performance with budget.
3.9.3. Let us first consider the flexibility issue. It is true that most of the expenditures under non-plan category are
committed (e.g., salary expenses). Also, funds flowing from the central government on various vertical programmes
are usually tied not only to a specific programme, but also to its specific line items. Yet it is notable that the state
3.9. Poor oversight at the district level
Figure 3.9. Estimated expenditure per bed,
by use and types of facility
0.50
1.00
1.50
2.00
2.50
Medical College Hospitals District Hospitals State General Hospital Sub Divisional Hospitals
Other
Drugs
Diet
Office Expenses
Salary
Health, Equity and Poverty:Exploring the Links in West Bengal, India
30
government has recently embarked on a series of innovative initiatives to arrange some additional funds for the
districts which could be used on the top of routine expenses. Important among them are revenue generated from user
charges at hospitals, special medical assistance for poorest patients, increased drug budget, and several other untied or
semi-tied funds. The funds flowing through these routes are small in comparison to routine funds, but large enough to
activate a special financing mechanism for poor and vulnerable.
3.9.4. Is there any efficient way to track down the use of these top-of-the-routine resources? Evidently, no. One reason for
this is the system's complete dependence on and comfort with the existing accounting system which is based on the
principle that money spent (or, disbursed) is equal to money used. Consequently, it becomes difficult to assess
whether and to what extent additional drug budget is actually reducing the burden of a poor patient, how the money
generated through user charges are ploughed back to the system, and so on.
3.9.5. The issues related to interest and capacity are complex. Usually there is a general aversion of district health officials to
financial figures, which creates problem in monitoring the efficiency in funds utilization. Also, interestingly, some of
them avoid or delay in taking decisions regarding flexible funds on various pretexts. For example, discussion with
one of the district offices revealed that not even 1 percent of the medical assistance fund could be spent in a particular
year. A detailed study would provide a clearer and confirmed picture, but in-depth discussions with the health
officials suggest that addressing inequity through available flexible resources is not in their top priority list.
3.9.6. It is obvious that for a more effective oversight of public services the boundary of routine activities should be crossed.
However, weak managerial and oversight capacity is one of the major constraints (at the district level) in this process.
It is encouraging to see that the state has started addressing this problem. A management unit has been established at
each district and a new set of young and skilled non-medical manpower (statistician, accountants, management
graduates, etc.) have been fed into the unit. The potential created by this process needs to be translated and directed
towards an effective oversight role (see Section 4.3 for details).
3.9.7. The District and block level Societies (Samitis) could play an important role in oversight activities (see Section 2.3)
although their primary task is to pull together all programme related funds and transmit it downstream according to
allotments. However, it also could play a stewardship role by
which it could (1) be able to re-allocate the resources among the
programmes on the basis of specific programme-specific needs
or district plan; (2) ask for financing accountability for the funds
spent from each programme manager and assess whether poor
are being benefited; and (3) be able to generate additional
resources at the local level. The current situation reflects poorly
on each of these aspects.
3.10.1. The FHS survey reveals that about two-third of out of pocket
payments in case of inpatient care in government hospitals are
spent on medicines and diagnostic tests (Figure 3.10). On an
average an indoor patient in government hospital would spend
3.10. Medicines and tests: killing fields
Health, Equity and Poverty:Exploring the Links in West Bengal, India
31
Figure 3.10. Out of pocket expenses for
inpatient care in government hospitals
(3 districts of West Bengal)
Tests
13.3%
Drugs
53.5%
Hospital charge
6.7%
Board + Lodging
9.9%
Travel
15.7%
Unofficial
0.9%
Rs. 1428 on these two items while a private client pays about 1.5 times more than that. Since the government facilities
do not charge for the medicines, the above evidence implies that a large section of the users of government hospitals
are compelled to purchase medicines from private pharmacies. Therefore, although public sector users pay for
services, these payments accrue largely to the private sector for medicines and unaccounted ancillary costs. These
revenues do not enter the public health system and, hence, cannot be used to improve the services that clients receive.
3.10.2. Expenditure on medicine in inpatient care is however just a small fraction of what people spend on outpatient care.
According to the recent NSSO results on
consumption expenditure (NSSO(2), 2004), per
capita monthly out of pocket expenses in non-
institutional (i.e., outpatient) care is about 10 times
and 8 times more than institutional (i.e., inpatient)
care respectively in rural and urban areas (Figure
3.11). Not surprisingly, medicines in outpatient care
accounts for more than 80 percent of total out of
pocket payments
3.10.3. Medicines and tests are, therefore, the principal
agents for economic drain in households affected by
health shocks. It is, therefore, expected that the
government would commit more attention and
resources towards this direction. The scenario
prevailing in the last few years reflects that the
government has indeed embarked on a commendable initiative to rationalize drug use. This includes (1) developing
an Essential Drug List (EDL) and a Standard Treatment Guideline (STG); (2) initiating a process of computerizing the
drug procurement and management systems; (3) imparting training in basic store management principle; and last,
significantly increasing the budget on drugs. At the same time, the principle of providing the patients with drugs at no
cost (if available) would remain unchanged.
3.10.4. The increase in budget on drugs is significant especially in the last few years. From a mere 5.5 percent in 1998-99 it
has increased to about 8 percent of non-plan expenditure. According to the providers visited by FHS research team,
the drug supply situation has considerably changed in recent years. There are more varieties of drugs now, compared
to the pre-2000 scenario. About 77 percent and 68 percent of hospital respondents (i.e., providers) felt that the drug
supply was regular and adequate. In general, discussions with hospital officials reflected a scenario where despite its
own deficiencies, the present drug supply status is much better than that in five years ago.
3.10.5. In an ideal situation, according to government policy, all clients of all government facilities will obtain drugs from the
facility (free of cost). As expected, the reality is way apart from the ideal situation. The results from exit interview of
412 outpatients in government facilities shows that about 22 percent of outpatients of government hospitals did not
receive any of the prescribed drugs from the hospital pharmacy. It is, however, also to be noted that the poorer patients
are less likely to return with no drug compared to better-off patients. Figure 3.12 shows that probability of getting no
Health, Equity and Poverty:Exploring the Links in West Bengal, India
32
Figure 3.11. Per capita monthly
OOPE on medicines in institutional
and non-institutional care (in Rs.)
2.95
5.08
21.85
42.73
0
10
20
30
40
50
60
Rural Urban
Institutional Non-inst
drugs directly varies with the economic status of
8
the patients - 44 percent of high-income patients
and 16 percent of low-income patients received
no drugs, indicating a clear pro-rich tilt in the
distribution of those who probably had to buy, or
opted to buy all prescribed drugs from private
pharmacies. Alternatively, as the data reveals,
poorer patients are less deprived from receiving
government's drug subsidy.
3.10.6. Notwithstanding the impressive equitable
distribution of drugs, the fact remains that people
spend a significant amount on drugs even when
they use services of government hospitals. The possible reason for this is that about a half of poor and 70 percent of
better-off patients did not receive some or any drugs from the government facilities (see Figure 3.12). The some
category is crucial since it covers 40 percent of all patients. One way to figure out the proportion of expenses on this
some drugs is to compare the average expense of those who purchased all drugs from private pharmacies with the
same of those who purchased the remaining drugs. The average expenses, as estimated from the exit interview data,
work out to Rs. 156.8 and Rs. 87.35 respectively implying that about 55 percent (87.35 156.8) of the values of total
prescribed drugs are paid by the users who had to buy some drugs from outside.
3.10.7. We can summarize the relevant issues in the following way:
Most of the poorer outpatients (about 85%) in government facilities receive either all or some drugs free of
cost from the facility.
However, a large portion of better-off patients (about 56%) also receive this benefit implying that a significant part
of drug subsidy is absorbed by those who could possibly pay for it .
Dominance of some (i.e., some but not all drugs were available) category offers several hypotheses about which
drugs are not available in government facilities: (1) essential, but prescribed brands are not available, and (2) non-
essential. The hypotheses can be tested only through proper auditing of prescriptions.
There is hardly any monitoring in prescribing behavior; in the absence of monitoring, the prescribing behavior is
often determined by the physicians' subjective assessment of patients' spending capacity (i.e., more expensive
drugs are prescribed if the patient is assessed able to pay).
The drug flow to the hospitals is primarily supply-driven; no objective analysis is done to assess the hospital-
specific needs (which, in turn, would require assessment of local epidemiology).
Health, Equity and Poverty:Exploring the Links in West Bengal, India
33
Figure 3.12. Percentage of outpatients in government
facilities who received all, some, and no drugs from
the government pharmacies, by income categories.
[Exit interview, 412 respondents, 3 districts]
0%
20%
40%
60%
80%
100%
Low Medium High
Income category
None
Some
All
8
The economic status was determined on the basis of reported annual household income: (1) low income less than Rs. 20,000; (2) medium more than Rs.
20,000 but less than Rs. 40,000; and (3) high more than Rs. 40,000. The classification is arbitrary but not incompatible with the argument presented in this
section.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
34
3.11. Out of pocket payment is progressive in inpatient care but not so in outpatient care
3.11.1. The findings in an earlier study strongly suggests that the
users' opportunity cost of accessing health care services
in West Bengal is often very high (Kanjilal and Pearson,
2002). The evidences from the present study also
support this phenomenon. As Figure 3.13 shows, about
28 percent of potential users who could not access
modern outpatient services in rural Bengal were barred
from accessing services only due to economic reasons.
As expected, the barrier is more prohibitive for families
in the poorer groups; around 41 percent of the persons
belonging to the poorest quintile could not access
outpatient services for economic reasons the
corresponding figure for the richest quintile is only 6.5
percent.
3.11.2. What happens to those who access services? Table 3.8 shows that the impact varies not only across rural and urban
areas, but also with respect to the type of care (inpatient and outpatient care) and socio-economic groups. Regarding
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
Poorest 2 3 4 Richest Overall
Figure 3.13. Percentage of rural ailing
persons who could not seek treatment due
to financial constraint, by asset quintiles (3
districts, West Bengal)
Table 3.8. Percentage of annual household expenditure spent on medical care,
by socio-economic groups (3 districts, West Bengal)
Rural
Inpatient care Outpatient care Asset
Quintile % of households
affected (in a
year)
% of their annual
expenditure
spent
% of households
affected (in 3
months)
% of their annual
Expenditure spent
(annually)
16.63 10.41 90.44 4.32
17.67 11.02 92.31 4.48
19.58 10.72 94.58 4.44
16.46 13.02 93.96 3.86
19.38 16.24 95.42 3.59
Urban
Inpatient care Outpatient care Asset
Quintile % of households
affected (in a
year)
% of their annual
expenditure
spent
% of households
affected (in 3
months)
% of their annual
Expenditure spent
(annually)
Poorest
Next 20%
Next 20%
Next 20%
Richest
20.00 4.04 86.67 2.95
17.88 11.41 87.42 2.16
18.12 6.56 91.95 2.82
19.33 8.30 88.67 2.46
15.33 18.18 92.67 2.24
Health, Equity and Poverty:Exploring the Links in West Bengal, India
35
9
Here, progressive out of pocket financing is defined as a state when OOPE as a percentage of total household expenditure increases with respect to
increase in ability to pay. A regressive financing would describe just the opposite scenario.
inpatient care, it is obvious that the impact of out of pocket payment is relatively more severe on higher income groups
9
indicating a progressive out of pocket financing system . One out of five households from this group is likely to send
at least one member to hospitals (for inpatient care) which will account for one-sixth of their annual household
expenditure three times more than a normal scenario. The poorest households are likely to send fewer members
(17%), and spend proportionately much less (10.4%). The implication is clear - hospitalization makes middle and
upper-middle income groups also vulnerable to major health shocks.
3.11.3. It is interesting to note that the impact somewhat reverses in case of outpatient care where poorer households spend
more in relative terms. Almost all households were affected in a quarter (90-95%) and a rural household in the poorest
quintile would spend around 4..3 percent of its annual expenditure (compared to 3.59% spent by the richest quintile).
The severity of economic drain is much less for urban residents primarily due to lower economic barriers to access.
3.11.4. The above analysis raises an important issue from equity angle. While it is universally accepted that hospitalization
implies catastrophe to the economy of an affected household, ambulatory or outpatient care begets no less disaster. It
hits at a much slower rate but erodes the economic base of many more households in a more definite way. As a whole,
it seems to perpetuate chronic poverty more than inpatient care does.
3.11.5. One crude benchmark of such catastrophe is the share of medical expenses in total household expenditure. Roughly
speaking, a payment is catastrophic to a
household if the share is more than 10
percent [Pradhan and Prescott (2002),
Ranson (2002)]. Figure 3.14 shows that
inpatient care is relatively more
catastrophic to the richer households. On
the other hand, it also shows that
outpatient care is more catastrophic than
inpatient care in terms of percentage of
households. While about 4 percent of
poorest households made catastrophic
payments for inpatient care, more than 10
percent did so for outpatient care. It is
also quite evident that the impact is
relatively heavier on the poorer section
indicating a regressive financing for
outpatient care.
3.11.6. Progressivity in OOP financing in case of inpatient care may be explained in terms of near-complete dependence of
poorer people on government hospitals. On the other hand, a significant portion of the richest section about 36
percent (see Figure 3.2) - seeks inpatient care from private hospitals and consequently absorbs heavier economic
burden. Regressivity in outpatient care financing possibly has its roots in two factors: (1) most people seek treatment
0
2
4
6
8
10
12
Inpatient Outpatient
Q1
Q2
Q3
Q4
Q5
Figure 3.14. Percentage of total households spending
more than 10% of their annual total expenditure on
medical care, by quintiles (3 districts, West Bengal)
Health, Equity and Poverty:Exploring the Links in West Bengal, India
36
Household
Endowment
Vulnerability to
Health poverty
Direct Entitlement
(Asset, knowledge,
labor)
Exchange
Entitlement
(Wage, rent, etc.)
Extended
Entitlement
(e.g., borrowing)
Social entitlement
(social protection)
Perceived
Opportunity
Cost of health care
Health Shock
Supply side
environment
Financial Productivity
Source: Adapted from Russell (1996) and Sen (1981)
Figure 3.15. Health and poverty: a conceptual framework
3.12.2. Vulnerability to health poverty, in turn, is determined by three factors:
(i) household entitlements which also define the household endowment at a particular point of time,
(ii) supply side environment, and
(iii) perceived opportunity cost of seeking health care.
from the private market, and (2) even those who visit government facilities obtain many drugs from private sector rich
and poor alike - implying that the financial burden is inequitably distributed among population.
A conceptual framework
3.12.1. Medical care imposes economic burden on households, but how is it related to poverty? The question is especially
relevant in the context of India's health care system where, due to absence of any full-proof risk protection mechanism,
10
the entire burden is more often absorbed by the households. Figure 3.15 presents a conceptual framework to explain
the dynamic relationship between poverty and health shock. The pivot element in this framework is the concept of
health poverty which is defined as a process of immiserisation of a household due to health shock an external shock to
the household. The shock manifests in possible erosion of the economic base of an affected household through two
parallel ways: (1) loss in productivity due to health problem, and (2) financial burden of treatment. The degree of
erosion would depend not only on the frequency and gravity of the shock, but also on the vulnerability of the affected
household to health poverty.
3.12. Growing health poverty in a socially unprotected environment
10
Adapted from Russell (1996) and Sen (1981).
3.12.3. Entitlements, i.e., households' command over alternative bundles of commodities, may be classified into four types:
Direct entitlements or Assets: This includes assets such as land and labor, and own produced crops / livestock
Exchange entitlement: Assets and direct entitlements translated into cash which may be used for saving and
spending on consumption, i.e., regular income and savings.
Extended entitlements:These emerge from social relations and add to household's command over
commodities; for example, access to credit and gift from professional moneylenders and relatives.
Social entitlements: Open access to social security or welfare (e.g., provident fund, social insurance, old age
pension, public distribution system, subsidized public health care system, etc.). These can form an important
component of a household's entitlement set in a welfare economy.
The entitlements act as absorber of health shock. In other words, a household with a piece of saleable land, higher
level of income, higher creditworthiness, and / or access to social security is less vulnerable to health related financial
shock compared to one which has none or less of them.
3.12.4. Vulnerability to health poverty also depends on supply side environment. The typical question to assess this
environment would be whether there is any effective mechanism at service delivery point to identify the poor and
vulnerable, and protect them from impoverishing effect of health care. Open access to public health facilities may
indicate a good environment, but the same coupled with an effective targeting mechanism would be better.
3.12.5. Finally, the opportunity cost perceived by the users of health care plays an important role to define vulnerability. It is
often found that the pattern of response to a particular disease or a ailing household member changes across
households. Consequently, the degree of sacrifice varies across households over a particular health shock leading to
varying levels of vulnerability. For example, a household may sell its assets to pay for an institutional delivery while
another (with same entitlement set) may opt for home delivery and manage it without selling an asset.
Evidences on entitlements
3.12.6. The FHS study made a preliminary attempt to assess the vulnerability through the components mentioned above. The
guiding question was: how do households use their entitlements as a coping strategy when at least one member seeks
inpatient or outpatient care? The answer to this question is expected to indicate the status of vulnerability among the
households.
3.12.7. Table 3.9 shows how the affected households used their entitlements to cope with financial shock for various health
cares. As expected, inpatient care made the affected households draw more upon extended entitlements (23%
borrowed with interest and 36% borrowed without interest) compared to outpatient care (2.8% and 8.5%,
respectively).
Health, Equity and Poverty:Exploring the Links in West Bengal, India
37
Table 3.9. Percentage distribution of households, by sources they used for financing medical
care (3 districts, West Bengal)
Sources of financing (%) Inpatient care Outpatient care Birth delivery
N 644 6303 483
Saving 29 16 31.7
Borrowing with interest 23.1 2.8 10.1
Borrowing without interest 36.3 8.5 21.3
General income 51.5 81.6 60.5
Selling property 3.1 0.4 1
Mortgaging property 0.6 0.1 0
Others 5 1.6 8.1
* Total may not add to 100% due to multiple responses
3.12.8. As mentioned above, health problems act as a shock to the equilibrium of household economy. In a situation where
social entitlement is weak, a household draws upon its other entitlements. It is expected that it would cope with the
shock first on exchange entitlements (i.e, its regular income); it is expected to fall upon extended entitlements (for
example, borrowing) and ultimately to direct entitlements (for example, selling assets) when its exchange entitlement
turns insufficient. Naturally, the graver the shock is, the more a household is expected to resort to extended and direct
entitlements. This, in turn, leads to erosion of the household's economic base and enhances its vulnerability to future
shocks.
3.12.9. Figure 3.16 presents the relative share of various sources of financing to pay for, say Rs. 100, on inpatient care. For
11
this purpose, NSSO data are used since the FHS survey did not collect the amount of financing from each source . It is
quite evident that households in the poorest quintile depended more on borrowing (extended entitlement) in
comparison to the richest quintile especially in urban areas. Relative share of other which includes selling /
mortgaging assets is also conspicuously higher for poorest section. The underlying process reflects their inherent
weakness to counter catastrophic expenses of inpatient care. However, it also reflects that the rural rich are
comparatively more vulnerable than urban rich since the former uses extended entitlements more extensively then the
latter.
Figure 3.16. Percentage share of various sources in total out of pocket payments for inpatient
care, by expenditure quintiles, West Bengal
th
Source: NSSO 60 round, 2004
Rural
Poorest Richest
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Borrowing Income Gifts Others
Urban
0%
10%
20%
30%
40%
50%
60%
70%
80%
90%
100%
Poorest Richest
Borrowing Income Gifts Others
3.12.10.The findings presented above focused on inpatient care. Apparently, the outpatient care does not shake the
entitlement base so brusquely (only 11% resorted to borrowing). The reason for such apparent milder effect remains
in the way the shock manifests. The shock, in this case, acts like a slow poison leading to a gradual erosion of
household's economic base. A snapshot of the effect of one or two episodes (in last three months as asked in the
11
The FHS survey asked which sources (not how much) were used to pay for medical care. The results are given in Table 3.9.
The NSSO survey, on the other hand, asked how much was sourced from each category.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
38
interview) is less likely to capture this dynamic effect. The presents study acknowledges this limitation and proposes
to undertake a research on inter-temporal effect of acute and chronic ailments on vulnerability to health poverty.
The findings presented above raises concern about the social entitlement a typical household in West Bengal have the
benefit of. Is there any social protection instrument by which a household, under duress due to medical care, can be
protected? Table 3.10 demonstrates that the state, like other Indian states, has a long way to go to achieve this goal.
Except ration card (i.e., membership in subsidized public distribution system) and life insurance, no significant
protective mechanism exists. Risk pooling through medical insurance is still far from reality as only a little above 5
percent of households were found to have some sort of health insurance.
3.12.11.
Table 3.10. Percent of households who are covered by various social protection mechanisms
(3 districts, West Bengal)
% of HH who have
the benefits of
Total Rural Urban
Social health Insurance
Other health insurance
3.2
2.2
1.4
1.5
Provident fund 13.9 11.7 21.4
Life insurance 31.3 28.5 40.2
Old-age pension 1.2 1.4 0.4
Crop insurance 0.4 0.5 0.0
Support from Panchayet 16.8 21.7 0.9
Other support from govt. 1.5 1.7 0.8
Ration card 91.7 91.8 91.4
9.3
4.4
Evidences on opportunity costs
3.12.12.Economic stress, caused by medical care, may also be viewed from its opportunity cost to an affected household. For
example, a low-income household, which is already sustaining on subsistence level, may have to delay medical
treatment of one member when another member is hospitalized. Similarly, the children may drop out from schools or
some social event (e.g., marriage) may be delayed. Although no attempt was made to quantify these opportunity costs,
the FHS study tried to understand the nature of such costs. As Figure 3.17 indicates in case of inpatient care most of
the households (70%) compromised food consumption while about 14 percent delayed social obligations (e.g.,
marriage or Puja) and 10 percent had to underspend on children's education.
Evidences on supply side environment
3.12.13.The earlier sections (Section 3.2 3.10) suggest that West Bengal is one of the very few states where open and easy
access to public facilities has led to overwhelming dominance of public facilities in inpatient care market. These
facilities, despite their flaws, often stand as the only resort to poorer sections. However, the state also demonstrates
that subsidized public health care does not provide enough ammunition, or pool the risks enough, to protect people
from the impoverishing effect of health care.
Health, Equity and Poverty:Exploring the Links in West Bengal, India
39
3.12.14.It is a common understanding that an effective targeting and consequent cross-subsidization may help create a
protective shield around those who needs external support for protection. However, the problem remains in
identifying the poor and vulnerable - a crucial prerequisite for targeting. Without a well-defined mechanism for
identification, the existing system follows ad hoc approaches. One glaring example is the existing exemption policy
in collecting user charges at hospitals where any person is exempted if he / she produces an indigent certificate issued
by any elected representative of any level. Consequently, almost everybody gets exempted (see 2.3.7).
3.12.15.In brief, without much social protection, households resort to the natural coping mechanism - a reactive strategy -
which usually implies drastic erosion of household resources. The following two case studies from two districts of the
state demonstrate how a typically poor household gets into poverty trap due to this reactive strategy (Boxes 3.6
and 3.7)
Figure 3.17. Percent of households compromising or postponing consumption
decision after they sought inpatient care (3 districts, West Bengal)
0
10
20
30
40
50
60
70
80
10.8
69.6
13.9
4.6
4.6
3.6
Children Education Food Consumption Daughter Marriage Medical Treatment Social Obligations Other
Health, Equity and Poverty:Exploring the Links in West Bengal, India
40
Box 3.6: How health and poverty are linked: Pratham's story
Pratham Mahato, a 33-year old male, is a marginal farmer in the block of Jhalda II in Purulia district. Since his own land is not
big enough to feed his family for the whole year, he is forced also to work as a daily labourer. At one night in April 2000, he felt an
excruciating pain in his stomach. In the morning, he was admitted to the Kotshila BPHC where he was treated for 3 days. His
family had to buy all medicines from a private pharmacy except the saline, which was given free by the hospital. Next he was
taken to the Purulia district hospital where he received treatment for 7 days, and his stomach was X-rayed free of cost. Except for
a few supplied by the hospital, Pratham's family bought all medicines (for Rs.3000). Seeing no result, his family next consulted
Dr. Das, a general private practitioner of Jhalda. He assured a complete remedy and treated Pratham with a few pain killer tablets
and a bottle of saline and got him again X-rayed, charging Rs.1000 for all this. With no diagnosis and no result, his family finally
admitted him to famous St. Barnabas Hospital at Ranchi where the attending doctor recommended a series of blood tests.
Pratham was then referred for an ultra-sonography test which showed serious problems in his intestines. Surgical intervention
was necessary. After his operation, he spent 14 days at the hospital and received 35 bottles of saline, 42 shots, and varieties of
medicines during the period. The stitches were removed and the patient was discharged on the fifteenth day. Meanwhile his
family had already spent Rs. 26000 on hospital charges, tests, and medicines.
The hospital had prescribed medication for four months; after that period, Pratham went to Ranchi for a check up where he was
diagnosed as fully cured. But, after one year, (in June 2002) the sharp old pain came back and Pratham was forced to go to the
Kotshila BPHC. The medical officer saw his past treatment records and pushed an injection and gave him 12 tablets for 3 days.
He feels easy now, but his past experience haunts him. The expenses in the first treatment made him sell a piece of land at
Rs.18000 though its actual price was Rs. 30000. He also sold 2 buffaloes, 10 goats and even borrowed Rs. 3000 from a local
moneylender at 10% interest per month. He does not find any hope to recover from the loss in his lifetime.
Source: Kanjilal B and M Pearson (2003)
Box 3.7. How health and poverty are linked: Anil's story
In the first week of August, 1997, Anil, a 47 year old farmer in the village of Mornia (Block: Dinhata II), suddenly felt an acute
pain in his chest and lower abdomen. It became difficult for him to eat anything. In the middle of that month, the intensity of the
pain shot up. The local RMP (unqualified allopathic doctor) failed but another RMP gave him a short respite. The pain, however,
returned soon. The next 20 months were lost in futile attempts by consulting one RMP after another. At the long last, one RMP
diagnosed the problem as Gastric Ulcer, and strictly advised him to avoid red meat, heavy-weight fishes, and any spicy food. He
was recommended only pulp-boiled rice, papaya, shuji, and simple fish curry (of Singhi and Magur fish). It was going on all
right, with the spicy-food-loving Anil keeping a vigil on himself, but everything changed when a 10 Kg grass carp was caught in
the pond adjacent to his house. After a verbal dual with his wife, he ate a few pieces of that fish (cooked with generous doses of
spice and oil).
Acute chest pain, inflammation, and asphyxiation followed 4 hours after the intake and he was admitted to the Dinhata SDH on
that night. The doctor attending the emergency immediately administered a few shots and medicines. His stomach was also
pumped out. He was in the general medical ward for 3 days. Another doctor took over and recommended immediate USG which
was done at a private centre in Kochbihar town. It all cost his family Rs.1350 and yet nothing was found in the report. A free X-
ray in the Dinhata SDH also produced nothing even after nine retakes. Another USG this time at Rs.1500. The process continued
for thirty-five days with slight recovery probably due to injections and Medicines (purchased from private outlets) given during
this period. The doctor restricted his diet to rice, easily digestible small fishes (Singhi, Magur, Pona etc.), Papaya and curd.
The problem, however, was not completely solved. In order to totally sort out his ailment, Anil began to consult doctors
randomly. All of them, however, endorsed the past treatment regime. Frustration set in, and, at last, he started finding solace in
alcohol. By April 2002, Anil's condition began to deteriorate rapidly. He has now reached a highly emaciated state, like a
skeleton with skin and is even unable to get up from his bed. Financial resources have dried up and he has now come back to
cheaper option of treatment provider - the local quack (haturey). The quack's treatment is being supplemented by services
rendered by other traditional providers (such as, Ayurvedic, faith healers, etc.).
Anil's struggle with ailments has so far stripped his family off 2 bighas (81.5 decimals) of farmland, 3 milk producing cows, all
gold ornaments, a few big trees and a loan of Rs. 15000. The family now survives on the wages (irregular, approximately
Rs.8000 per annum) of his two kids who work as daily labourer. The only property left is a dilapidated homestead with a small
piece of backyard (15 Kathas).
Source: Kanjilal B and M Pearson (2003)
Health, Equity and Poverty:Exploring the Links in West Bengal, India
41
4. Towards a more equitable future: how
can research help?
Health, Equity and Poverty:Exploring the Links in West Bengal, India
43
4.1. How to make the system work more for the poor?
4.1.1. What can be done now to make the health care system work more for the poor and make a more equitable future? On
the basis of situation analysis presented above we identify the following five broad policy objectives for strengthening
the equity base of the health care system in the state:
The population are protected from the financial consequences of ill health (especially catastrophic ill
health) and are not denied essential health services because of inability to pay.
Public financing of health care is more accountable at the ground level to ensure that maximum benefits
from flow of public subsidies to poor.
Public funds are allocated in ways consistent with national and state health policies and are utilized
efficiently.
Removing the barriers against equitable preventive care and maternal health care.
Private sector is internalized and made to work towards the common vision
4.1.2. The specific options to meet the above objectives are:
Develop a closer working relation with informal sector
Ensure local oversight for implementing pro-poor strategies and resource tracking
Reduce asymmetric information in drugs market to empower the consumers
Develop appropriate risk pooling mechanism especially for economically disadvantaged section.
Improve targeting in public subsidies for essential health care.
Address the barriers to preventive care and safe birth delivery especially in under-served areas.
Facilitate and regulate private sector
4.1.2. How can research help meet these objectives? For a responsive health care system, it is necessary that research results
would not only feed into the policy making process, but also influence the implementation process through innovative
ideas. The future health system, as envisaged by FHS research, would be distinctively marked on this aspect. The
results of scoping studies are expected to help policy makers take informed decision; new ideas will be tested through
well-planned action research; system performance will be assessed through innovative tools; and, evidences will be
regularly generated to oversee the progress towards a more equitable system. The scope of research is, therefore,
indicated at the end of each of the following sections.
4.2. Develop a closer working relation with informal sector
4.2.1. The study highlights the urgent need for addressing the silent but all-pervasive spread of Rural Medical Practitioners
(RMPs) in rural health care market (see Section 3.5). Two clear policy options emerge from the study:
(i) Ensure adequate basic health care facilities with qualified health care providers who would remain available
round-the-clock for basic curative services and birth delivery. The purpose, in this case, is to crowd out
RMPs by government-sponsored competitors.
(ii) The alternative option is to internalize RMPs within the system and feed on their strengths in a guided
manner. For example, a section of RMPs may be empanelled or franchised to help them operate as
gatekeepers of primary health care.
4.2.2. The first option, despite its popularity among public health researchers, is seriously constrained by two factors: (1)
perennial shortage of government doctors in rural areas primarily due to their reluctance to serve there, and (2)
resource crunch in providing adequate infrastructure, drugs, and maintenance inputs to meet the huge need for basic
curative care. Further, supplying doctors and other inputs is not enough to compete with RMPs as long as RMPs excel
formal providers in packaging their services.
4.2.3. The second option has clear advantages on these aspects the option allows the system to use a huge pool of resources
(i.e., RMPs) which is being used by the people anyway. However, the risk, as mentioned earlier, remains in their huge
potential to generate adverse health effects through immature applications of medical science. The additional barriers
are (1) the legal aspects which may bar involving a RMP in formal medical care, and (2) the intrinsic profit motive of
RMPs which may not adjust with the public health goals of the government.
4.2.4. Several experiments at the international and national levels demonstrated that minimizing the risk and overcoming the
barriers is not an impossible task. The study strongly suggests such a strategic experiment, at least at a particular
district as a prototype. The basic components of such an experiment might be:
Empanel selected RMPs at each block as Rural health gate keepers. Empanelment should be based on several
essential quality indicators. The program may be initially started where public system is relatively weak. The
role of the RMP will be to provide a set of basic curative services and refer cases immediately to formal providers
as and when the patient crosses the identified safe treatment.
Identify a set of basic curative and preventive services for which the RMPs will be given franchise right to
operate as official gatekeepers.
Involve civil societies (Panchayet or NGO) in implementing empanelment and mentoring the RMPs.
Provide intensive training to selected RMPs on simple treatments, identifying potentially complicated cases and
danger mark where they have to refer.
It is also important to devise an incentive structure (monetary and otherwise) for adopting franchise right and adhering
to standard protocols.
Research scope
4.2.5. The present study is the first step towards understanding the role and potential of RMPs as a part of huge informal
sector in India's health care market. Several issues emerged from the present study all of which could not be
conclusively addressed due to its limited scope. The limitations in the present study encourages Future Health System
project to embark on exploring further on this issue with a broader canvas. The research questions for future research
in this area could be broadly delineated as:
How safe or unsafe are the current clinical practices of RMPs?
What is the net impact of RMP practices on rural health?
How feasible is it to integrate RMPs into existing public health care system?
Health, Equity and Poverty:Exploring the Links in West Bengal, India
44
4.2.6. The last question would require designing an operational research with a strategic intervention plan with RMPs which
could be implemented in one or two districts of West Bengal. The intervention may be aligned to the steps outlined in
previous section with appropriate modifications.
4.3.1. As discussed earlier, the routine fund flow to the districts, which constitutes the major share of total fund flow, is
channelized through the district health department through its Drawing and Disbursement Officers (DDO). The lion's
share of this fund is earmarked for salary and maintenance leaving little room for maneuver. Tracking resources in
this case implies tracking the performance of human resources which the system has been doing anyway. However,
still there are a few important items for which tracking intervention may be initiated:
(i) Delivery of drugs and consumables at government facilities is it consistent with the standard treatment protocol
and essential drug list? Does a poor have to buy drugs from private pharmacies even when it is not necessary?
(ii) Disbursement of untied funds for special medical assistance to the poor is it really going to the poor?
(iii) Program funds flowing through the societies what is the health outcome?
(iv) Funds generated through user charges and retained at the district level is it really being spent on welfare of
patients (Rogi Kalyan)?
(v) Funds from special schemes, such as JSY or PMGY to what extent they benefit the targeted beneficiaries?
4.3.2. All these questions are difficult to answer at present due to absence of local oversight. In some cases, specialized
studies need to be done (for example, tracking JSY fund). However, the decentralization and devolution strategy of
the state has also created a potentially powerful institution in the form of District and Block level societies (DHFWS
and BHFWS). The societies have recently gained more attention with a clear intention that district management of
health care must be strengthened to reap the benefits of decentralization strategies.
4.3.3. As discussed earlier, the present centre-state relationship in the context of implementation of vertical programmes is
one of the factors which restricts DHFWS to playing a post-office role with respect to management of the mobilized
resources. Each of the programmes requires a separate book-keeping system and restricts the ear-marked fund to be
used towards a predetermined direction. The role of DHFWS is extremely limited in this fund flow mechanism and is
not likely to change in the short run.
4.3.4. Given the constraints, the best a DHFWS can do in this context is to keep track of the resources flowing in through this
mechanism, prepare a consolidated account, and comes up with a performance index of each programme on the basis
of a simplified 'source and use' matrix. The necessary steps to meet this objective would be to (1) calculate total funds
flowing in under the vertical and other programmes; (2) prepare a performance index of each programme based on
their progress in meeting target output within a specific period of time; and (3) estimate expenditure per unit of
performance index. The results are expected to provide the top management of DHFWS with crucial inputs for
monitoring the progress of the programmes.
4.3.5. Financial accountability is one of the major issues related to financing efficiency of the system. The current practice
followed by the societies (and, DHFWS) does not promote better accountability. The approach is often simplified to
expedite the receipt of funds from the central programme units. As a result financial reports on fund utilization from
the district societies are sent upwards based on the amount of fund released to the block level, not on whether and how
they were spent.
4.3. Ensure local oversight for implementing pro-poor strategies
Health, Equity and Poverty:Exploring the Links in West Bengal, India
45
Health, Equity and Poverty:Exploring the Links in West Bengal, India
46
4.3.6. One way to address the problem is to link release of funds to a set of crude performance index (as mentioned above)
prepared for each block. This may be supplemented by random performance audit at the field level. The audit may be
carried out by selected non-government organizations, or, by a separate technical cell of DHFWS.
4.3.7. Increasing flow of untied funds (for example, a part of user charges) has created an excellent opportunity for DHFWS
to rig up innovative ways for protecting poors' interest. There are opportunities to initiate demand side financing at a
small scale for example, subsidized food coupons for poor patients and their attendants, or vouchers for purchasing
drugs to those who can hardly afford to obtain by themselves.
4.3.8. The oversight role may be initiated through establishing an information system which would be regularly fed in by
data collected through patient satisfaction survey, disease surveillance, costing of services, district health accounts,
and forecasting local need for drugs. It would inform how many women received JSY assistance and how many still
need help, and so on.
4.3.9. What is the expected output from this empowered decentralization? Local control allows for management, planning,
and use of resources that responds directly to district needs. Health facilities will be adequately stocked, equipped,
and placed where they are most likely to be accessed by the poor. Retained user fees and centrally provided funds will
be spent on community health concerns, rather than on central priorities. Medical personnel who answer to
communities rather than to supervisors at the state or national level are more likely to treat their clients with respect,
giving them the time they need for quality services.
Research scope
4.3.10. It is quite obvious that the existing level of capacity of the district management team of DHFWS is inadequate to play
such an extended role envisaged above. It is therefore essential that a short-term and a medium-term plan be designed
to build and strengthen the institutional capacity of the team. This should be based on a thorough needs assessment
exercise, and then filling in the appropriate skill gap through rigorous in situ training process. The FHS research
proposes to undertake this exercise in one of the districts on a pilot basis.
4.3.11. The initiative may be framed as a pilot research programme in one district. The guiding research question would be
whether the district health care system, with their scope and capacity extended, can make itself work more for the poor?
More specifically, it would explore whether the ongoing initiatives for decentralization strengthening the DHFWS in
particular could be translated into a platform in the short run for (i) generating evidences through an information
system (see 4.3.8) and (ii) helping channelize the untied resources towards poor users of health care through demand
side financing. In the long run, it could also be tested whether it can generate local resources through risk pooling
mechanism - to establish a fund for protecting poor and vulnerable from health related financial shock (more on this in
Section 4.5).
4.4.1. As discussed earlier (see Section 3.10) expenses on drugs constitute more than 80 percent of out of pocket expenses
especially in outpatient care. One of the fundamental problems in Indian health system is poor accessibility to low-
cost drugs especially by the poorer section of population. The poor clients receiving care from the public or private
sources are often directed by the providers to purchase high-priced or irrational drugs. The pharmacies in public
4.4. Reduce asymmetric information in drugs market to empower the consumers
Health, Equity and Poverty:Exploring the Links in West Bengal, India
47
hospitals, which are supposed to provide the users with free medicines, frequently fail to meet the prescribed needs,
and, thereby pushing them to obtain medicines from private pharmacies. The cheaper alternatives are usually not
mentioned in the prescription making the consumers spend a high proportion of their total out-of-pocket medical
expenditure on medicines.
4.4.2. Protection of people from health poverty thus necessarily boils down to protecting them from irrational drug expenses.
One of the important factors influencing the irrational process is high degree of asymmetry of information in the
medicines market. The clients do not have any bargaining power since they do not have any information on the
cheaper alternatives and that they could be equally useful. The asymmetry is further widened due to common practice
of the providers prescribing branded medicines. The variation in prices of a single medicine across different brands is
quite significant.
Research scope
4.4.3. The interventions so far undertaken are primarily from the supply side. EDL has been prepared, doctors have been
instructed to prescribe generic drugs, standard treatment protocols are now available, and so on. The problem still
remains unresolved. While acknowledging the importance of these interventions, the FHS research forwards the
hypothesis that the out-of-pocket expenditure on medicines could be significantly reduced if the consumers are
adequately empowered with information on (1) cheaper (but equally useful) and generic options of prescribed
branded medicines; and (2) a distinction between essential and non-essential medicines in the context of a specific
disease. The information is expected to generate certain degree of negotiating power when they visit a provider, and,
more importantly, when they visit the private pharmacies for purchasing drugs. The empowerment process could be
implemented by involving the local level civil societies and local self administration (e.g., Panchayet). The process
could be initiated after a scoping study on the degree of asymmetric information in the market and how this is being
used by the imperfect agents (i.e., providers and pharmacies).
4.5.1. The inadequacy of public health care delivery system as a risk pooling mechanism has made people helpless in case of
financially catastrophic illnesses or conditions. Is insurance a solution? Conceptually, insurance is a risk pooling
mechanism which may also be more successful in mobilizing additional private household resources as individuals
are assessed premiums when they are in good health and better able to afford payments. Insurance can be as simple as
community funds to transport women with complicated deliveries to hospitals, or as complicated as health
maintenance funds that reimburse providers for all health needs including preventive and curative functions.
Encouragingly, the state government has recently embarked on a serious initiative to work out a suitable model for risk
pooling in the state.
4.5.2. The products designed by for-profit private health insurers are not a solution to a rural or urban poor person. On the
other hand, it is most unlikely to see the government, which is already financing the public health care, to take the
whole financial burden of a social insurance scheme that would cover the financial risk of the poor. What, then, is the
option? One feasible way to protect the financial risk of the poor would be to focus on a district-based health fund
scheme. In this case, the District Health and Family Welfare Society would be the custodian of all health funds
received from the central, the state and the donors, and the user charges for the secondary care. It would also collect
4.5. Develop appropriate risk pooling mechanism especially for economically disadvantaged section.
Figure 4.1. A conceptual framework on district health fund
District Health
Funds
DHFWS
Households Panchayet
Subsidy from
Govt. and
donors
Contri-
bution
Risk manager
(Insurer)
Providers
Cashless
service
Pooling
Managing
Empanel
reimburse
Technical Resource
Centre
Monitoring &
MIS support
Capacity and
Technical resource
Marketing
Servicing
SHG
Contri-
bution
Contri-
bution
Health, Equity and Poverty:Exploring the Links in West Bengal, India
48
pre-payment from the community according to their ability to pay. A preliminary outline of this framework is given in
12
Figure 4.1 .
4.5.3. The pivot element of this frame work is the District Health Fund (DHF). The main purpose of this fund is to provide
financial protection to those households who need it after receiving a health shock. The fund has two sources: (1)
subsidy (if any) and untied funds from government and donors, and (2) households, through risk premium. The
households' contribution flows through some organized groups, such as Self Help Groups (SHG) to DHF through
established civil society organization, such as Panchayet. The distinctive feature of such an initiative is to consider the
community group (SHG), not an individual or a household, as the base unit of contact.
4.5.4. The second component is the insurer which will underwrite the risk and manage claims with or without Third Party
Administrators (TPA) on the basis of a well-defined contract with the district society (DHFWS). The third component
is the set of providers comprising of selected private and public hospitals. The major problem in this case would be to
define the public providers. The existing model of provision of public health services is clearly a misfit in the
proposed system since, theoretically, it is supposed to provide almost free services to the user at the lower (i.e., PHC)
level. Clearly, the state needs to realign its subsidy policy to match it with the regime of health insurance financing.
Currently the state is playing the dual role a provider as well as a financier. A health insurance paradigm ideally
requires it to assume a single role preferably a provider.
4.5.5. The existing policy environment in the state clearly indicates that subsidy policy at least at the primary level of health
care - is unlikely to change in near future. A pragmatic approach, therefore, is to start reform the financing strategy
from the top layer of the delivery system, i.e., from the secondary and tertiary level of care where already people are
participating in purchase of services (through user charges). In other words, at the initial phase, the services at
secondary / tertiary level may be priced on a full-cost basis. The enrollees will receive fully cash-less services and
12
The framework is a modified version of one proposed to the DHoFW by GTZ (West Bengal) as a part of its proposal on Social protection for
informal sector in West Bengal. The version and views presented here are not necessarily those of GTZ or DHoFW.
Products (IPD, drugs, tests, wage-loss, etc.) in exchange of community-rated premium. The hospitals will be
reimbursed from the district pooled fund.
4.5.6. The proposed mechanism (as shown above) will work at the district level in the following way:
i. The DHFWS will establish a separate wing within itself named as District Health Fund Unit (DHFU). The unit
will hold the (1) premium contributions received from the target beneficiaries; (2) premium subsidies paid by the
government and donors; and (3) any other untied fund meant for poors' health.
ii. DHFU will outsource the management of this fund and underwriting responsibility to a professional insurer, or
any other institution it deems fit. The contracted institution will also do quality accreditation and empanelment,
and 24 hours servicing
iii. For collection of contribution and marketing, DHFU will contract the District Panchayet (Zilla Panchayet) which,
in turn, will contract block and village Panchayets to ensure a steady collection from the SHGs.
iv. DHFU will have a contractual relationship with empanelled providers (public and private) which will include
rate setting, payment contract, and quality assurance. This responsibility may also be outsourced to the
contracted risk manager.
v. DHFU will monitor the process and outcome of HI intervention. For this purpose, it will receive support and
technical assistance from an autonomous resource Centre.
4.5.7. The main entry point at the village level will be the SHGs who will work in close collaboration with the Gram
Panchayet (GP). The expected number of beneficiaries and level of collection will be decided by the Block Panchayet
(BP) and concerned GP. The GP will market the product to SHGs and collect premium from them. The SHGs,
therefore, will collect premium from their members and deposit it to the GP. The GP, in turn, will transfer the fund
directly to DHFU or through Block Panchayet office. It is important to note that the GP and their block counterpart
will be eligible to claim some monetary incentive depending on the degree of enrolment.
4.5.8. The role of a GP is thus crucial. They will not only work as a bridge partner between SHGs (or, beneficiaries) and the
district health fund, but also they will promote HI as a part of their other social security initiatives. Further, it will
directly connect the target beneficiaries where SHG is relatively weak or absent. The incentive structure (for GPs and
BPs) should be adequately rewarding (on performance basis) to help them do so. Given the poor management
capacity of the GPs (and BPs), it is imperative that an intensive capacity building and sensitization process is initiated
with the Panchayet structure even before the HI intervention is launched. The resource centre proposed above may
play a key role in this process.
4.5.9. District Health Fund may therefore be one of the key channels of risk pooling in the future health system. However, a
few points, which emerged from the FHS research, need to be addressed once the final outline of such an initiative is
shaped:
(i) As mentioned earlier (see Section 3.11) catastrophe due to hospitalization is often highlighted since it is
conspicuously visible, but outpatient care also hurts the household economy, albeit in a slow but steady way. The
out of pocket payment for outpatient care is regressive implying that poorer households are more hurt than better-
off households. The bottom-line of this argument is that any mechanism for financial protection or risk pooling
must cover outpatient care. This is, however, challenging since the risk is very evenly spread in this case (hence,
pooling risk is difficult).
Health, Equity and Poverty:Exploring the Links in West Bengal, India
49
Health, Equity and Poverty:Exploring the Links in West Bengal, India
50
(ii) Setting a flat risk premium across various socio-economic groups defeats the principle of equity. However, it is
also true that discriminatory pricing (or, discriminatory subsidy) is extremely difficult since it requires
segmentation of beneficiaries in all villages according to their socio-economic status. The transaction cost of
such an effort is prohibitively high especially when it is done by an external agency. A more cost-effective way
would be to let the SHGs or the community groups rate the ability to pay of their members on a continuous scale
to reach a given target of collection.
(iii) Insurance, as a risk pooling mechanism, should supplement but not substitute the government's fundamental role
in health care, especially in the context of primary health care. The underlying proposition in the above
statement is that the suggestions presented in other parts of this section (4.2 4.4 and 4.6-4.8) are equally relevant
even when DHF or any other risk pooling mechanisms are adopted.
Research scope
4.5.10. The role of research in this area is extremely crucial. More specifically, research may focus on following issues:
(i) Developing a measurement criterion of vulnerability to health poverty by which households in a given area can
be ranked according to their vulnerability. For example, a vulnerability index may be derived on the basis of
evidences on entitlements, supply side environment, and perceived opportunity cost.
(ii) Costing major services in private and public hospitals by using standard costing format.
(iii) Generating evidences on out of pocket expenses to help derive the rate of risk premium.
(iv) Being a part of the Technical Resource Centre and providing all required research support.
4.5.11. The FHS research also likes to mould the proposed initiative in a pilot intervention frame (in a district). The pilot
research, which may go concurrently with other proposed interventions given in other parts of this section (Section 4),
would help DHFWS design and implement the proposed DHF concept in a particular district.
4.6. Improve targeting in public subsidies for essential health care.
4.6.1. The findings presented in Section 3 shows that subsidies flowing to finance public health delivery are not specifically
targeted to poor. It is true that poor people use government facilities, but so do the rich. More pro-poor distribution of
subsidies would require that (i) the richer groups move to private care, or unsubsidized public facilities such as paid
inpatient wards, and (ii) out of pocket costs (especially the travel costs and drug costs) borne by a poor are also reduced.
4.6.2. The key hurdles on the way to meet the above requirements are (1) inadequate private hospitals at the block levels
which leaves hardly any alternative choice for the better-off; and (2) high private cost to access the public facilities
(often due to non-availability of services in the proximate areas). The indirect cost to access public facilities is quite
evident from the FHS study; a public client of inpatient care spent about Rs. 530 about a quarter of his / her total out of
pocket expenses - on travel and associated expenses. Clearly, development of infrastructure at the peripheral level
would help reduce this burden.
4.6.3. However, infrastructure development is not sufficient by itself. Equity in access requires equity in quality of care. It
is a common experience that the richer section has better capacity to jump the queue (to receive better quality of care at
Health, Equity and Poverty:Exploring the Links in West Bengal, India
51
public facilities) and to crowd out the poor. The root of the problem remains in existing user fee mechanisms in which
one is free to opt for subsidized bed irrespective of his/her paying capacity. The solution, therefore, remains in a
more equitable distribution through some sort of rationing by which the richer (including the government servants)
will be able to access within the limit of a fixed quota of subsidized beds. This should be supplemented with a policy
of total withdrawal of subsidy for those facilities that are accessed by the richer section (for example, private cabins)
and recovery of the cost on 100 percent basis.
4.6.4. The analysis presented in Section 3.3 clearly indicates that there is a strong case for targeting younger (0 14 age-
group) and older women (60 and above) who utilize much less inpatient care compared to their male counterparts. It is
primarily a demand side issue (gender inequity within households); however, a more gender-sensitized role of
providers is expected to improve the situation. It is important that the government hospitals seriously take note of this
problem, try to understand the specific local barriers, and improvise innovative methods to address these barriers in
their ongoing IEC campaigns.
Research scope
4.6.5. Future research in this area is expected to focus on two aspects: (1) generating evidences on various targeting
mechanisms followed in other states (and, other developing countries) and assess their feasibility in the context of the
state's health care system, and (2) assessment of the pro-poor schemes initiated by the Department of Health and FW at
the ground level where it works and where it does not. The research may be integrated with the same described in
Section 4.3 (Ensure local oversight).
4.7.1. The analysis presented in Sections 3.6 and 3.7 clearly indicate that there exist a few strong barriers, especially in some
districts and some pockets within a district, to meet two important public health goals: universal immunization and
safe birth delivery. The barriers include: (1) poor accessibility to public health services in some areas due to strong
geographical adversity, (2) administrative weakness (for example, unavailability of outreach workers for various
reasons), (3) economic constraints, and (4) weak demand due to socio- cultural factors. It is obvious that these under-
served areas need special strategies to fight these barriers. Unfortunately, the information currently available with the
Department of Health and FW is inadequate to map out these areas according to the nature of the barrier.
4.7.2. Once the under-served areas are mapped and their barriers are identified, it is necessary to draw up a set of special
strategies to cover these areas. For instance, if an administrative block in a district shows chronic underperformance
in children's immunization due to geographical inaccessibility the outreach services may be reinforced by involving a
local NGO or a local non-government health care provider. Alternatively, mobile health camps may be organized
which would also provide immunization services. Similarly, special initiatives may be undertaken to ensure safer
home delivery in those areas where women do not use institutions for birth delivery for socio-cultural reasons.
However, the actual strategy will ultimately depend on a scientific assessment of the barriers.
Research scope
4.7.3. There is an acute need for scientific information on what and how the barriers lead to underperformance. The first
research step is, therefore, to study their impacts and map the under-served barriers assorted according to particular
4.7. Address the barriers to preventive care and safe birth delivery especially in under-served areas
Health, Equity and Poverty:Exploring the Links in West Bengal, India
52
barriers (in a particular district). The next step would be to assess various sets of options to act against those barriers
and identify the set which is technically feasible and cost-effective. The next step would involve testing the selected
strategies through a bunch of pilot interventions. Finally, the output of interventions would be evaluated in
comparison to a control (no intervention) area. The results of this research process would then be used to design a
comprehensive strategy for the state.
4.8.1. Given the predominant role of the private sector in curative care, the state should internalize it, in both its modern
qualified and traditional forms, into health plans. The public sector is responsible for coordinating, but not necessarily
delivering, affordable health care for all. For many middle- and high-income people, affordable health care exists in
the private sector. When relatively prosperous clients use private sector services, scarce resources are freed up for
higher quality and more accessible public services for the poor.
4.8.2. Internalization of private sector necessarily implies that the private sector is to complement, and not just co-exist with,
the public sector. The process would require three strategic steps:
(i) Facilitate expansion of private market at those blocks or district headquarters where the government facilities are
over-burdened. This would require creating market incentives through tax-subsidies and a collaborative but
profitable arrangement with the existing government facilities. This may be supplemented by disincentive to
further concentration of private hospitals either where government facilities are under-utilized or where it is
over-concentrated.
(ii) Minimum standards for its operation need to be maintained and regulated. The existing process of licensing and
re-licensing of private facilities is grossly ineffective and the legal framework is inadequate. Evidences are
plenty that many private hospitals are taking advantage of this situation and being engaged in malpractices and
violation of consumers' rights especially if the consumer is already in a disadvantaged situation. A complete re-
look into this issue is essential.
(iii) Involvement of private sector in district planning process. This is especially important in the context of the
ongoing process under National Rural Health Mission (NRHM). It is also to be noted that the department has
embarked on an innovative scheme of partnership with the private hospitals regarding institutional delivery.
However, these initiatives often become non-sustainable when the private partners are asked to share a pre-
designed scheme. For sustainability, it is important to involve them from the conception stage of the schemes.
Research scope
4.8.3. Future research in this area should primarily focus on generating evidence on the spread and operation of private
sector in the state. The key research questions that sill remain largely unanswered are: (1) to what extent the growth of
private health care market is related to health poverty? (2) how this market is spread and to what extent it can help
targeting at government facilities? (3) what are the formal mechanisms of quality assurance in private facilities and to
what extent the standard benchmarks are complied? (4) how cost-effective are the ongoing initiatives of public-
private partnerships, and so on. The results of research are expected to provide the policy makers with crucial
evidences on the operation of the market and help them design an effective policy for internalizing the private sector.
4.8. Facilitate and regulate private sector
Health, Equity and Poverty:Exploring the Links in West Bengal, India
53
References
Indian Institute of Health Management Research (IIHMR) 2004. Impact evaluation of West Bengal SHSD project,
Kanjilal B and M Pearson 2002. Health financing in West Bengal: Structure, challenges and options. Unpublished report,
DFID Health System Resource Centre.
National Health Policy (NHP) 2002, Ministry of Health and Family Welfare, Government of India. 2002.
National Sample Survey Organization (NSSO) 2004. Morbidity, health care and the condition of the aged. Report on NSS 60th
round, New Delhi.
National Sample Survey Organization (NSSO-2) 2004. Household consumer expenditure in India, Report on NSS 60th round,
New Delhi.
Peters, D et al. 2002. Better health systems for India's poor: findings, analysis, and options. Washington DC: The World Bank
Pradhan, M. and N. Prescott 2002. Social risk management options for medical care in Indonesia. Health Economics 11:
431-446.
Public Expenditure Review 2005. Unpublished report prepared under the Health Sector Development Initiative, Government
of West Bengal.
Purfield, C 2006. Mind the gap Is economic growth in India leaving some states behind, IMF working paper, Washington
DC:IMF.
Ranson, M. K 2002. Reduction of catastrophic health care expenditures by a community-based health insurance scheme in
Gujarat, India: current experiences and challenges. Bulletin of the World Health Organization 80(8): 613-21.
Reserve Bank of India, 2006. State finances: A study of budgets of 2006-07, Mumbai: RBI Publications.
Russell, S 1996. Ability to pay for health care: concepts and evidences, Health Policy and Planning: 11(3): 219-237.
Sen, A 1981. Poverty and Famines. Oxford: Clarendon
Wagstaff, A., Van Doorslaer, E., Paci, P. 1989. Equity in the finance and delivery of health care: some tentative cross-country
comparisons. Oxford Review of Economic Policy 5(1), 89-112.
You might also like
- Rekharani SethyDocument18 pagesRekharani SethyMahila Pratishtha JournalNo ratings yet
- Assessing the Landscape of Healthcare in India-1Document13 pagesAssessing the Landscape of Healthcare in India-1sumit kumarNo ratings yet
- State Led Innovations For Achieving UnivDocument8 pagesState Led Innovations For Achieving UnivPragyan MonalisaNo ratings yet
- Health Infrastucture in IndiaDocument8 pagesHealth Infrastucture in IndiaBinit kumarNo ratings yet
- Access and Efficiency of Health Services in HaryanaDocument7 pagesAccess and Efficiency of Health Services in HaryanaVAIBHAV VERMANo ratings yet
- Health Infrastructure and Economic Development in IndiaDocument9 pagesHealth Infrastructure and Economic Development in IndiaAkanksha PalNo ratings yet
- India's National Health Policy and National Rural Health MissionDocument4 pagesIndia's National Health Policy and National Rural Health MissionrajatsgrNo ratings yet
- Impact of Pradhan Mantri Jan Arogya Yojnaa On Indian EconomyDocument41 pagesImpact of Pradhan Mantri Jan Arogya Yojnaa On Indian EconomyyashNo ratings yet
- rp (1)Document14 pagesrp (1)Samita ChandalNo ratings yet
- Governance Frameworks for Gender Mainstreaming in Public HealthDocument10 pagesGovernance Frameworks for Gender Mainstreaming in Public HealthFika Nur FadhilahNo ratings yet
- Health Care Industry in IndiaDocument14 pagesHealth Care Industry in IndiaAmit KumarNo ratings yet
- PH.D PROPOSAL BY N SRINU, UNIVERSITY OF HYDERABADDocument9 pagesPH.D PROPOSAL BY N SRINU, UNIVERSITY OF HYDERABADsri_cbmNo ratings yet
- Health Care Delivery System in IndiaDocument11 pagesHealth Care Delivery System in IndiaAnish VeettiyankalNo ratings yet
- A Study On Service Quality and Customer Satisfaction of Selected Private Hospitals of Vadodara CityDocument6 pagesA Study On Service Quality and Customer Satisfaction of Selected Private Hospitals of Vadodara Citymurugan_muruNo ratings yet
- PG Project FinalDocument46 pagesPG Project FinalThomas BabuNo ratings yet
- M2022LSP007 Q2Document3 pagesM2022LSP007 Q2krishna vamsyNo ratings yet
- Public Health Care System in IndiaDocument5 pagesPublic Health Care System in IndiaPela KqbcgrlaNo ratings yet
- India's Country Experience in Addressing Social Exclusion in Maternal and Child HealthDocument28 pagesIndia's Country Experience in Addressing Social Exclusion in Maternal and Child HealthOommen C. KurianNo ratings yet
- Up Health Care DeliveryDocument18 pagesUp Health Care DeliveryAparna KinginiNo ratings yet
- Rural Health in Andhra PradeshDocument5 pagesRural Health in Andhra PradeshInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Pakistan Health CareDocument31 pagesPakistan Health CarenomimasterNo ratings yet
- Innovative Ways To Meet Health Challenges of Urban India - Radhika Arora - Sourav Neogi - Madhavi MisraDocument9 pagesInnovative Ways To Meet Health Challenges of Urban India - Radhika Arora - Sourav Neogi - Madhavi MisraJimmy KatiraNo ratings yet
- Private Health Services in BangladeshDocument37 pagesPrivate Health Services in Bangladeshhornzz0% (1)
- ENG102 ProjectDocument4 pagesENG102 Project2221634No ratings yet
- Comparative Study of Public and Private Health Services in Mumbai RegionDocument18 pagesComparative Study of Public and Private Health Services in Mumbai RegionJobin BabuNo ratings yet
- Chapter - 1 Nature, Scope, Objectives and Methodology of ResearchDocument18 pagesChapter - 1 Nature, Scope, Objectives and Methodology of ResearchJobin BabuNo ratings yet
- Chapter - 1 Nature, Scope, Objectives and Methodology of ResearchDocument18 pagesChapter - 1 Nature, Scope, Objectives and Methodology of ResearchMohammad MudasirNo ratings yet
- Chapter - 1 Nature, Scope, Objectives and Methodology of ResearchDocument18 pagesChapter - 1 Nature, Scope, Objectives and Methodology of ResearchJobin BabuNo ratings yet
- Chapter - 1 Nature, Scope, Objectives and Methodology of ResearchDocument18 pagesChapter - 1 Nature, Scope, Objectives and Methodology of ResearchJobin BabuNo ratings yet
- Health Care Services in India: Problems and Prospects: B. S. Ghuman Akshat MehtaDocument15 pagesHealth Care Services in India: Problems and Prospects: B. S. Ghuman Akshat MehtaPaul PriyarajNo ratings yet
- Category Health Workers PDFDocument37 pagesCategory Health Workers PDFAparna Kingini100% (1)
- Reasons For Development of Health Care in IndiaDocument5 pagesReasons For Development of Health Care in IndiasnehapriyaNo ratings yet
- Lahariya HWCInd JPeds 2020Document15 pagesLahariya HWCInd JPeds 2020YashwanthNo ratings yet
- Public Health Research in India in The New MillennDocument10 pagesPublic Health Research in India in The New Millennatul gusainNo ratings yet
- Healthcare Models in The Era of Medical NeoliberalismDocument9 pagesHealthcare Models in The Era of Medical NeoliberalismmnagashyamNo ratings yet
- A Study On Public Expenditure On Health Sector in IndiaDocument8 pagesA Study On Public Expenditure On Health Sector in IndiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Health Care Delivery Concerns in IndiaDocument43 pagesHealth Care Delivery Concerns in IndiaSaji Sadanandan50% (4)
- Review Jurnal Pembiayaan Kesehatan 2Document5 pagesReview Jurnal Pembiayaan Kesehatan 2SUCI PERMATANo ratings yet
- Healthcare Financing Infrastructure PaperDocument25 pagesHealthcare Financing Infrastructure Papersri_cbmNo ratings yet
- Government's Policy on Public HealthDocument30 pagesGovernment's Policy on Public HealthKrittika PatelNo ratings yet
- 163 696 2 PB PDFDocument15 pages163 696 2 PB PDFHameed AbdulNo ratings yet
- Uzbekistan and Philippines Healthcare Systems ComparedDocument8 pagesUzbekistan and Philippines Healthcare Systems ComparedbnvjNo ratings yet
- Rutuja GarghateDocument10 pagesRutuja GarghateKarel de KlerkNo ratings yet
- Draft National Health Research Policy, DHR, MOHFW (Nov 2021)Document50 pagesDraft National Health Research Policy, DHR, MOHFW (Nov 2021)Harish KiranNo ratings yet
- 09 Chapter 2hhjDocument36 pages09 Chapter 2hhjRizzy PopNo ratings yet
- India: Current State of HealthcareDocument15 pagesIndia: Current State of HealthcareYadav MannuNo ratings yet
- Research ProposalDocument7 pagesResearch ProposalTony DumfehNo ratings yet
- Ngos and Government Partnership For Health Systems Strengthening: A Qualitative Study Presenting Viewpoints of Government, Ngos and Donors in PakistanDocument8 pagesNgos and Government Partnership For Health Systems Strengthening: A Qualitative Study Presenting Viewpoints of Government, Ngos and Donors in PakistanGummie Akalal SugalaNo ratings yet
- Major Challenges in The Health Sector in BangladeshDocument13 pagesMajor Challenges in The Health Sector in BangladeshRaima Ibnat ChoudhuryNo ratings yet
- A Survey Report On Scaling of Public Health Units As Sub Centers, PHC and CHC of Uttar Pradesh State, India.Document71 pagesA Survey Report On Scaling of Public Health Units As Sub Centers, PHC and CHC of Uttar Pradesh State, India.Voice of People100% (1)
- Rural India Final PaperDocument8 pagesRural India Final Paperapi-664194717No ratings yet
- RhciDocument378 pagesRhcivinodshende31No ratings yet
- International Journal For Equity in HealthDocument12 pagesInternational Journal For Equity in HealthjlventiganNo ratings yet
- Material Plan On: Holy Family College of Nursing Delhi UniversityDocument10 pagesMaterial Plan On: Holy Family College of Nursing Delhi UniversityManisha ThakurNo ratings yet
- Equity in Hospital Services Utilisation in India PDFDocument7 pagesEquity in Hospital Services Utilisation in India PDFaditya_2kNo ratings yet
- Health System in India Opportunities AndDocument9 pagesHealth System in India Opportunities AndSarfaraz Samim HaqueNo ratings yet
- Khyber Pakhtunkhwa Health Sector Review: Hospital CareFrom EverandKhyber Pakhtunkhwa Health Sector Review: Hospital CareNo ratings yet
- New Health Systems: Integrated Care and Health Inequalities ReductionFrom EverandNew Health Systems: Integrated Care and Health Inequalities ReductionNo ratings yet
- FAQ - MBA in Rural Management - IIHMR UniversityDocument8 pagesFAQ - MBA in Rural Management - IIHMR UniversityThe IIHMR UniversityNo ratings yet
- DR MK Bhan Speech at Convocation Ceremony 2017 - IIHMR UniversityDocument3 pagesDR MK Bhan Speech at Convocation Ceremony 2017 - IIHMR UniversityThe IIHMR UniversityNo ratings yet
- Pharma Brochure FINALDocument65 pagesPharma Brochure FINALThe IIHMR UniversityNo ratings yet
- Pradanya Broucher 2015Document148 pagesPradanya Broucher 2015The IIHMR UniversityNo ratings yet
- Information Brochure - 2015-2017Document42 pagesInformation Brochure - 2015-2017The IIHMR UniversityNo ratings yet
- Placement Brochure MBA Hospital, Health, HRM, Rural-2016Document125 pagesPlacement Brochure MBA Hospital, Health, HRM, Rural-2016Mukesh GehalotNo ratings yet
- Placement Brochure MBA Hospital, Health, HRM, Rural-2016Document125 pagesPlacement Brochure MBA Hospital, Health, HRM, Rural-2016Mukesh GehalotNo ratings yet
- Gender Health Resource Centre-News LetterDocument16 pagesGender Health Resource Centre-News LetterThe IIHMR UniversityNo ratings yet
- IIHMR University Conduct Pharma MAT For Admission in MBA Pharmaceutical ManagementDocument5 pagesIIHMR University Conduct Pharma MAT For Admission in MBA Pharmaceutical ManagementThe IIHMR UniversityNo ratings yet
- IIHMR University Brochure 2016-18Document40 pagesIIHMR University Brochure 2016-18The IIHMR University100% (1)
- IIHMR-30th State of Institute ReportDocument96 pagesIIHMR-30th State of Institute ReportThe IIHMR UniversityNo ratings yet
- Universal Health Coverage Road Map For 2020-Pradanya 2015 Annual ConferenceDocument1 pageUniversal Health Coverage Road Map For 2020-Pradanya 2015 Annual ConferenceThe IIHMR UniversityNo ratings yet
- IIHMR Pharmaceutical Placements-2014 PDFDocument48 pagesIIHMR Pharmaceutical Placements-2014 PDFThe IIHMR UniversityNo ratings yet
- Information Brochure 2015 2017Document40 pagesInformation Brochure 2015 2017The IIHMR UniversityNo ratings yet
- GHRC News LetterDocument12 pagesGHRC News LetterThe IIHMR UniversityNo ratings yet
- Souvenir (PG 1-82) With CoverDocument83 pagesSouvenir (PG 1-82) With CoverThe IIHMR UniversityNo ratings yet
- 29th SIR Report - 2014Document100 pages29th SIR Report - 2014The IIHMR UniversityNo ratings yet
- MBA - Hospital & Health - IIHMR UniversityDocument1 pageMBA - Hospital & Health - IIHMR UniversityThe IIHMR UniversityNo ratings yet
- MBA PHARMACEUTICAL MANAGEMENT Flyer (Sept 2014)Document2 pagesMBA PHARMACEUTICAL MANAGEMENT Flyer (Sept 2014)The IIHMR UniversityNo ratings yet
- IIHMR Placements-2014 - Hospital and Health ManagementDocument100 pagesIIHMR Placements-2014 - Hospital and Health ManagementThe IIHMR UniversityNo ratings yet
- IIHMR University-MBA PHARMACEUTICAL MANAGEMENTDocument2 pagesIIHMR University-MBA PHARMACEUTICAL MANAGEMENTThe IIHMR UniversityNo ratings yet
- MBA-Rural IIHMR UniversityDocument1 pageMBA-Rural IIHMR UniversityThe IIHMR UniversityNo ratings yet
- Promoting Rational Use of Drugs in The Community November 16-25, 2014Document5 pagesPromoting Rational Use of Drugs in The Community November 16-25, 2014The IIHMR UniversityNo ratings yet
- MBA HOSPITAL AND HEALTH MANAGEMENT Flyer (Sept 2014)Document2 pagesMBA HOSPITAL AND HEALTH MANAGEMENT Flyer (Sept 2014)The IIHMR UniversityNo ratings yet
- PHD Hospital and Health Management Flyer PHD H&HM (Sept 2014)Document2 pagesPHD Hospital and Health Management Flyer PHD H&HM (Sept 2014)The IIHMR UniversityNo ratings yet
- National Workshop On KohaDocument5 pagesNational Workshop On KohaThe IIHMR UniversityNo ratings yet
- MBA RURAL MANAGEMENT Flyer RM (Sept 2014)Document2 pagesMBA RURAL MANAGEMENT Flyer RM (Sept 2014)The IIHMR UniversityNo ratings yet
- IIHMR UNIVERSITY AN EXCLUSIVE HEALTH RESEARCH AND POST GRADUATE UNIVERSITY-FlyerDocument4 pagesIIHMR UNIVERSITY AN EXCLUSIVE HEALTH RESEARCH AND POST GRADUATE UNIVERSITY-FlyerThe IIHMR UniversityNo ratings yet
- Pradanya Broucher 2014Document8 pagesPradanya Broucher 2014The IIHMR UniversityNo ratings yet
- Iihmr 1984-2009Document110 pagesIihmr 1984-2009The IIHMR UniversityNo ratings yet
- Man Against HimselfDocument507 pagesMan Against Himselfalbatros3000No ratings yet
- Golden NumbersDocument89 pagesGolden NumbersjoobazhieNo ratings yet
- WeeFIM Score Sheet (MS Word)Document4 pagesWeeFIM Score Sheet (MS Word)Siti Maryam Rosyidah0% (2)
- 2 Months To LiveDocument26 pages2 Months To LivedtsimonaNo ratings yet
- Medic Alert Short BrochureDocument2 pagesMedic Alert Short BrochureDerek DickersonNo ratings yet
- Dr. Jinitha K.S. - Assorted Essays On Classical and Technical LiteratureDocument137 pagesDr. Jinitha K.S. - Assorted Essays On Classical and Technical LiteratureSasi KadukkappillyNo ratings yet
- Tabel Interaksi Kolom BetonDocument10 pagesTabel Interaksi Kolom BetonEndoGutierrezNo ratings yet
- Jeremy Jones: Dental Hygiene, Associate of Applied Science, Pending 05/17Document3 pagesJeremy Jones: Dental Hygiene, Associate of Applied Science, Pending 05/17Jeremy JonesNo ratings yet
- How Brain Science Can Inform Architectural DesignDocument12 pagesHow Brain Science Can Inform Architectural DesignadrianmoleavinNo ratings yet
- 1536106348Document144 pages1536106348Saman SarKoNo ratings yet
- Spectrophotometric determination of total phenolic content in Gul-e-ZoofaDocument4 pagesSpectrophotometric determination of total phenolic content in Gul-e-Zoofayulyansyah susantoNo ratings yet
- Disorders of Orgasm in Women A LiteraturDocument15 pagesDisorders of Orgasm in Women A Literaturкостя100% (1)
- Yoga y AyurvedaDocument50 pagesYoga y AyurvedaManuel100% (1)
- Plasmid-Mediated Resistance - WikipediaDocument16 pagesPlasmid-Mediated Resistance - WikipediaUbaid AliNo ratings yet
- ACCIDENT REPORTING AND INVESTIGATION PROCEDUREDocument23 pagesACCIDENT REPORTING AND INVESTIGATION PROCEDUREkirandevi1981No ratings yet
- Sodium Polystyrene SulfonateDocument11 pagesSodium Polystyrene SulfonatejanellaNo ratings yet
- 261-Article Text-575-1-10-20180915Document11 pages261-Article Text-575-1-10-20180915hector michel galindo hernandezNo ratings yet
- Thalassemia Report Edited2Document121 pagesThalassemia Report Edited2rjcarlos_05No ratings yet
- Ron Greenspan DDS - Braces 101Document10 pagesRon Greenspan DDS - Braces 101Ron Greenspan DDSNo ratings yet
- The Chapeter That Is TissueDocument36 pagesThe Chapeter That Is TissuereemNo ratings yet
- CPHQ Review Course Nov 28-29 2012Document195 pagesCPHQ Review Course Nov 28-29 2012Khaskheli Nusrat100% (2)
- Brain Implant Victims - MCRAISDocument11 pagesBrain Implant Victims - MCRAISProjekt_-stop-tortureNo ratings yet
- Health and its failure: Causes, Types, and Prevention of DiseasesDocument9 pagesHealth and its failure: Causes, Types, and Prevention of DiseasesAbhimanyu BahreeNo ratings yet
- PHC Conference Agenda 6-13Document5 pagesPHC Conference Agenda 6-13OSUMCNo ratings yet
- Prismaflex CRRT Competency Based Tool PDFDocument5 pagesPrismaflex CRRT Competency Based Tool PDFalex100% (1)
- Genetic Polymorphism of Cyp2d6Document23 pagesGenetic Polymorphism of Cyp2d6Oscar Velasco0% (1)
- Significant Prognostic Impact of Improvement in VeDocument10 pagesSignificant Prognostic Impact of Improvement in VeFIA SlotNo ratings yet
- 1 Gram Positive Bacterial InfectionDocument87 pages1 Gram Positive Bacterial InfectionCoy NuñezNo ratings yet
- UrinalysisDocument16 pagesUrinalysisJestha Parayno De Vera100% (6)
- Risk Management in Medical LaboratoriesDocument32 pagesRisk Management in Medical Laboratoriesapanisile14142No ratings yet