Professional Documents
Culture Documents
Clinical Features and Pathology of Phthisis Bulbi
Uploaded by
ruditacitrahahaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Features and Pathology of Phthisis Bulbi
Uploaded by
ruditacitrahahaCopyright:
Available Formats
1.
Clinical background
Key symptoms and signs
Phthisis bulbi represents an ocular end-stage disease of various causes and
is defined by atrophy, shrinkage, and disorganization of the eyeball and intraocular
contents (Box 54.1).[1,2] Subjective complaints depend on the etiology and severity
of phthisis bulbi. Typical clinical symptoms and signs include chronic ocular
hypotension (5 mmHg), a shrunken globe, pseudoenophthalmos, intraocular tissue
fibrosis and scarring, vision loss, and recurrent episodes of intraocular irritation and
pain.[3]
Definitionphthisis bulbi
Phthisis bulbi represents an ocular end-stage disease characterized by:
Atrophy
Shrinkage
Disorganization of the eyeball and its intraocular contents
2. Historical development
The term phthisis bulbi derives from the Greek word phthiein or phthinein, meaning
shrinkage or consuming, and was first used by Galen.[3] Over the last 200 years, the
clinical interpretation of phthisis bulbi has often been modified according to the
underlying disease and structural changes; a clear distinction from ocular atrophy
was often difficult and controversial.[4] Hogan and Zimmerman[1] were the first ones
who stated that both terms atrophy and phthisis bulbi refer to consecutive stages
in the degeneration process of a severely damaged eye. Their descriptive
classification system including three different stages (1) ocular atrophy without
shrinkage; (2) with shrinkage; and (3) with shrinkage and disorganization has been
further modified by Yanoff and Fine[2] (Table 54.1).
3. Epidemiology
Epidemiological data on phthisis bulbi are mainly based on retrospective
clinicopathological studies on enucleated eyes.[510] Enucleations are usually the
result of failed ocular treatment or end-stage diseases (i.e., phthisis bulbi) associated
with blind, painful, or cosmetically unacceptable eyes. The incidence of enucleation
in general has slightly decreased during the last decades because of improved
diagnostic and therapeutic approaches, and the trend towards globe-preserving
procedures; however, information on the incidence of phthisis bulbi is limited.[10,11]
In contrast, the prevalence of phthisis bulbi in enucleated eyes is well documented,
ranging from 11.2% to 18.7% with an average of 13.7%, and has remained fairly
stable over the last 60 years (Table 54.2).[59] However, statistical evaluations
indicate a slight increase in the number of enucleations for phthisis bulbi during the
last two decades
4. Genetics
A possible relationship between myotonic dystrophy and ocular hypotony has
been described by Kuechle and co-workers.[14] The examined eyes displayed a
diminished bloodaqueous barrier (BAB) function and diffuse choroidal edema,
presumably due to elevated follicle-stimulating hormone and luteal hormone serum
levels.
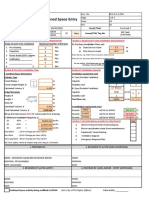
5. Diagnostic workup
Phthisical eyes are usually easily accessible for slit-lamp examination, which
allows evaluation of the periocular region and structures of the anterior segment. In
less advanced stages of the disease with a lack of significant corneal opacification,
intraocular fibrosis (i.e., cyclitic membranes) or cataractous changes of crystalline
lens, gonioscopy, direct and indirect ophthalmoscopy, fluorescein angiography, and
optical coherence tomography may be useful for evaluation of the anterior-chamber
angle, choroid, and retina.[15] Once optical visualization of the intraocular structures
is obscured, ultrasound biomicroscopy and other noninvasive diagnostic imaging
techniques such as computed tomography (CT) and magnetic resonance imaging
(MRI) may be applied to validate morphologic abnormalities of the anterior chamber
and ciliary body as well as to exclude intraocular ossification, or possibly foreign
bodies (Box 54.2).[16,17]However, the differential diagnostic utility of
6. Differential diagnosis
Although the underlying diseases and the clinical course of phthisis bulbi are quite
variable, the end-stage disease is rarely missed because of characteristic clinical
features (i.e., small, soft, atrophic eyes), which are often associated with decreased
or lost vision. However, clinicians should be aware of any potential disease entity
which, if not treated properly, may result in a blind, often painful phthisical eye.
Intraocular malignancies (i.e., retinoblastoma, malignant uveal melanoma) should be
taken into consideration if the ocular history is limited and an obvious cause for
phthisis is missing.[6] In addition, congenital abnormalities like microphthalmos and
microcornea should be kept in the differential diagnosis of phthisis bulbi.
7. Treatment
Therapeutic approaches are very limited in phthisical eyes; symptomatic treatment
(i.e., artificial tears, ointments, topical corticosteroids, nonsteroidal eye drops, anti-
infectious agents) may be recommended in patients with mild ocular symptoms (i.e.,
irritation, pain). Contact lenses or scleral shells can be used for cosmetic purposes.
Once phthisical eyes become chronically irritated and painful, enucleation or
evisceration with implantation of an intraocular or orbital implant should be
performed, especially with regard to potential long-term complications (i.e.,
sympathetic ophthalmia, ulceration, perforation) and to exclude intraocular
malignancies.[19,20]
8. Prognosis and complications
The diagnosis of phthisical eyes implies a frustrating clinical situation demonstrating
the result of failed previous ocular therapy in which restoration of the morphologic
and functional integrity of the eye is not possible. Most phthisical eyes eventually
become blind, painful, and cosmetically unacceptable for the patient. Potential
harmful complications include corneal ulceration and perforation with the risk of
ocular and periocular inflammation (i.e., panophthalmitis), sympathetic ophthalmia,
and malignant transformation
9. Pathology
Clinical and pathologic findings of phthisical eyes are variable and depend on the
underlying disease and time interval between primary lesion and enucleation. The
following section describes the main clinicopathological ocular features commonly
seen phthisis bulbi
10. Clinical features
Phthisical eyes are usually easy to detect by inspection of the patient's face and are
summarized in Table 54.3. The diagnosis is simplified due to the unilaterality of the
disease with asymmetry of the eyeballs and interpalpebral fissures. Additional
indirect clinical signs include narrow lid fissures (pseudoptosis), lagophthalmos,
pseudoenophthalmos, small-sized and soft, hypotonic (IOP 5 mmHg) eyes (Figure
54.1A; Box 54.3). Axial displacement in relation to the surrounding structures may
occur in advanced stages, which are often associated with vision loss. The
conjunctiva may be swollen (chemotic) and hyperemic. The appearance of cornea is
variable displaying corneal haze, scarred, vascularization, and dystrophic
calcification (Figure 54.1B). The anterior chamber is usually shallow, demonstrating
a narrow to closed chamber angle. Synechia (peripheral, posterior),
neovascularization of the iris surface and chamber angle (rubeosis iridis), fibrotic or
fibrovascular
11. Macroscopic and microscopic features
A. Gross pathology of the external eye
External examination of enucleated phthisical eyes typically shows a soft and
partially collapsed globe. The shape and size of the eyes may vary depending on the
nature and duration of the underlying disease as well as the age of the patient at the
initial event. Phthisical eyes usually demonstrate a squared-off shape with scleral
buckling behind the insertion line of the horizontal and vertical extrinsic rectus
muscles. Other specimens seem to maintain their normal spherical shape despite
marked shrinkage and decreased volume. On average, phthisical eyes are about
20% smaller in dimension compared to normal-sized adult eyes (24 24
24 mm).
[3]
The cornea is usually flattened, smaller in diameter (20%), and hazy due
to edema, scarring, or dystrophic calcification.
[3]
B. Gross pathology of the internal eye
The cornea and sclera are usually markedly thickened, on average by 80% (cornea)
to 50% (sclera) (Figure 54.2).
[3]
The anterior chamber is often shallow or collapsed;
iris defects (partial, complete) from previous trauma or surgery may be present. The
lens is usually thickened and cataractous. The ciliary body and retina are often
detached and displayed anteriorly by a retrolenticular or epiretinal fibrotic tissue; the
optic nerve head may be pulled into the vitreous cavity. Intraocular hemorrhages
may be present in the anterior chamber, vitreous, or choroid.
12. Histopathology
All intraocular structures may be involved in phthisical eyes (Table 54.3). The cornea
is usually thickened, edematous, scarred, and vascularized (57%); a fibrovascular
tissue and areas of dystrophic calcification may be present in the anterior stroma
next to the epithelium.[3] The posterior stroma and Descemet membrane are thrown
into folds by a fibrous tissue proliferation at the inner surface of Descemet
membrane (stromal downgrowth) (Figure 54.3A). The endothelium, if present, may
display cystic changes of its cytoplasm. Additional pathologic findings of the anterior
chamber may include epithelialization and vascularization of the chamber angle and
iris surface (24%), peripheral and posterior synechia with secondary angle closure,
and fibrous or fibrovascular cyclitic membranes at the pupillary margin (Figure
54.3A).[3] The lens usually displays epithelial proliferation, differential staining of
nucleus and cortex, and clefting of the lens fibrils. Occasionally,
13. Etiology
Phthisis bulbi cannot be understood as a specific clinical entity; rather, it is
considered the endpoint of a number of ocular diseases with various stimuli.
Potential risk factors contributing to phthisis bulbi include failed surgical procedures
(i.e., cataract, glaucoma, retina surgery), infections and inflammation (i.e., keratitis,
uveitis, endophthalmitis), intraocular malignancies (i.e., choroidal melanoma,
retinoblastoma) as well as systemic cardiovascular diseases (i.e., diabetes,
hypertension) (Table 54.1).[3,19,28,29] Although it is not known how long an
individual eye will tolerate a specific ocular damage, virtually all diseased eyes will
finally become atrophic if therapeutic treatment fails.
14. Pathophysiology
A. Aqueous humor dynamics and bloodocular barrier functions
The aqueous humor that fills the anterior and posterior chambers is important
in the physiology of the mammalian eye. It provides oxygen and nutrients for the
avascular tissues of the anterior segment such as cornea, trabecular meshwork, and
lens and subsequently removes metabolic waste products. In addition, it maintains
an IOP of about 15 mmHg that is required for the functional and morphological
integrity of the eye. The aqueous humor is derived from the blood plasma and
secreted in an energy-consuming process (approximately 23 l/min) by a
monolayer of nonpigmented epithelial cells at the inner surface of the ciliary body.
Compared to the plasma, the aqueous has a low protein level (about 0.02 g/ml
compared to 7 g/ml), mainly composed of albumin and transferrin.[30]Other
components include various growth and neurotrophic factors such as transforming
growth factor- (TGF-), acidic and basic fibroblastic growth
B. Ocular hypotony and phthisis bulbi
Ocular hypotony, a key feature of phthisical eyes, is defined as IOP of 5
mmHg at consecutive measurements in an individual eye.[28] While clinical signs
and symptoms are usually reversible in acute and transient stages, chronically
decreased IOP can have deleterious effects on intraocular tissue morphology and
function, eventually leading to phthisis bulbi (Table 54.2).[28,33,34] Although the
underlying pathologies and mechanisms of ocular hypotony may be quite variable,
they all work together, inducing an imbalance of aqueous production and outflow
(trabecular, uveoscleral) (Figure 54.4).[21,28,35,36]Subsequent alterations of
aqueous flow dynamics associated with compromised oxygen supply, nutrition, and
metabolic exchange within the anterior chamber are main points of concern. In
particular, intraocular hypoxia has been shown to contribute to BAB breakdown
associated with invasion of serum components (i.e., proteins, growth factors),
inflammatory cells,
C. Ocular wound healing in phthisis bulbi
Fibrovascular and fibrous tissue proliferation can also be observed after
trauma (i.e., concussion, perforation) or complicated vitreoretinal surgery. Similar to
proliferative vitreoretinopathy (PVR), it represents a specific ocular wound-healing
response, which, if not treated properly, contributes to ocular hypotony and
subsequent atrophy of the globe (Figure 54.4).[25,4244] Potent predisposing risk
factors include long-standing retinal detachment and retinal breaks with release of
RPE cells into the vitreous. Briefly, ocular injury results in breakdown of the blood
ocular barrier with release of serum components and chemotactic factors such as
fibronectin (FN), TGF-, and platelet-derived growth factor (PDGF) into the anterior
chamber and vitreous cavity. These factors accelerate migration, proliferation, and
transformation of inflammatory cells and RPE.[31]Later cells are able to secrete
additional growth factors and cytokines like interleukins
D. Dystrophic calcification and heterotopic ossification in phthisis bulbi
Calcification and ossification are frequent end-stage changes of degenerating
tissues. Both can be observed in phthisical eyes, often associated with chronic
inflammation, multiple traumas, long-standing retinal detachment, or
PVR.[23,24,48,49] Intraocular calcium deposits are mainly composed of calcium
phosphate and carbonate and typically occur in the cornea (band keratopathy), lens,
RPE (drusen), and retina, depending on low carbon dioxide tension due to
metabolic inactivity.[50] In contrast, bone formation usually involves the choroid and
fibrovascular or fibrocellular cyclitic membranes external to the neurosensory retina.
The time between original insult and bone formation is quite variable, ranging from a
few months to several years, with an average of approximately 20
years.[23,48]While trauma seems to be more common in young patients with
formation of compact bone tissue, inflammation is often associated with an
15. Conclusion
Phthisis bulbi represents an ocular end-stage disease that results from wound
healing secondary to various causes such as severe trauma, inflammation,
necrotizing tumors, and/or vascular diseases. It results in vision loss and continues
to be an important cause of blindness. The clinical diagnosis of phthisis bulbi, which
is characterized by atrophy, shrinkage, and disorganization of the globe, is a
frustrating situation since therapeutic approaches are limited to symptomatic or
cosmetic treatment options. Prophylactic procedures and close follow-up visits are
required in patients at high risk for the development of phthisis bulbi.
You might also like
- Adler - Individual PsychologyDocument51 pagesAdler - Individual PsychologySafira YulfaNo ratings yet
- Retinal DetachmentDocument8 pagesRetinal DetachmentJohanLazuardiNo ratings yet
- Iritis 8Document14 pagesIritis 8Alvis KurniawanNo ratings yet
- Elements of Exercise ProgramDocument4 pagesElements of Exercise ProgramMariam Gamos100% (1)
- Feline UveitesDocument9 pagesFeline UveitesErick ConfickeerzNo ratings yet
- Take One Nursing Final Coaching Ms CriticalDocument29 pagesTake One Nursing Final Coaching Ms Criticalnot your medz duranNo ratings yet
- Hemodialysis, Phosphorus and Calcium, Peritoneal DialysisDocument29 pagesHemodialysis, Phosphorus and Calcium, Peritoneal DialysisTrizha MaeNo ratings yet
- Medical Management of BlepharitisDocument6 pagesMedical Management of BlepharitisAl NaifNo ratings yet
- Ventilation Plan For Confined Space EntryDocument9 pagesVentilation Plan For Confined Space EntryMohamad Nazmi Mohamad Rafian100% (1)
- A Case Study On The Improper Waste Disposal in General Santos CityDocument22 pagesA Case Study On The Improper Waste Disposal in General Santos CityJino Onij BolandoNo ratings yet
- Catalog Snibe Maglumi 800 English PDFDocument7 pagesCatalog Snibe Maglumi 800 English PDFAniket DubeyNo ratings yet
- Nursing Theory of Ramona T. Mercer MaterDocument8 pagesNursing Theory of Ramona T. Mercer MaterMark Norriel Cajandab100% (1)
- Thyroid Ophthalmopathy: Yash ShahDocument6 pagesThyroid Ophthalmopathy: Yash ShahCATALINMARCUNo ratings yet
- Nightingale Institute of Nursing: AssignmentDocument18 pagesNightingale Institute of Nursing: AssignmentDhAiRyA ArOrANo ratings yet
- Blepharitis - UpToDateDocument22 pagesBlepharitis - UpToDateanisa maria ulfaNo ratings yet
- Differential Diagnosis of The Swollen Red Eyelid - AAFPDocument16 pagesDifferential Diagnosis of The Swollen Red Eyelid - AAFPtorome4979No ratings yet
- Yanoff DukerDocument8 pagesYanoff DukerFerdinando BaehaNo ratings yet
- Approach To The Adult With Acute Persistent Visual LossDocument17 pagesApproach To The Adult With Acute Persistent Visual LossMauricio SvNo ratings yet
- How to take an eye exam historyDocument5 pagesHow to take an eye exam historyChris KingNo ratings yet
- Retinoblastoma PDFDocument5 pagesRetinoblastoma PDFRiska PermatasariNo ratings yet
- Blepharitis - UpToDateDocument38 pagesBlepharitis - UpToDatecamiloedaza1977No ratings yet
- New 5-FU option for epithelial downgrowthDocument4 pagesNew 5-FU option for epithelial downgrowthDelila MaharaniNo ratings yet
- Red Eye Clinical Presentation: History and Physical ExaminationDocument11 pagesRed Eye Clinical Presentation: History and Physical ExaminationLaiba KhanNo ratings yet
- 1-8 Eyelid DisordersDocument6 pages1-8 Eyelid Disorderssien99100% (1)
- OpthaDocument5 pagesOpthavarun2k6No ratings yet
- Uveitis GlaukomaDocument13 pagesUveitis GlaukomaDede FatmawatiNo ratings yet
- Referat Cystoid Macular Edema Periode 17 Juni - 20 Juli 2019Document25 pagesReferat Cystoid Macular Edema Periode 17 Juni - 20 Juli 2019CharlotteGraceNusiferaNo ratings yet
- Overlooked Complication ofDocument9 pagesOverlooked Complication ofdoctorbanNo ratings yet
- Chronic Closed Angle Glaucoma - StatPearls - NCBI BookshelfDocument6 pagesChronic Closed Angle Glaucoma - StatPearls - NCBI BookshelfAngel LimNo ratings yet
- Damage Control Surgery Ocular Traumatology (Injury)Document7 pagesDamage Control Surgery Ocular Traumatology (Injury)Shirakawa AlmiraNo ratings yet
- Review ArticleDocument10 pagesReview ArticleAnonymous Hic7yE7I8INo ratings yet
- Protrusion OjoDocument16 pagesProtrusion OjoAntonio ReaNo ratings yet
- Dry Eye Syndrome - StatPearls - NCBI Bookshelf PDFDocument7 pagesDry Eye Syndrome - StatPearls - NCBI Bookshelf PDFnum padNo ratings yet
- 1 SMDocument7 pages1 SMAriNo ratings yet
- Graves 508Document6 pagesGraves 508VellaNo ratings yet
- Keratoconus: Picture 1Document6 pagesKeratoconus: Picture 1BuiyiWongNo ratings yet
- Keratoconus: Picture 1Document6 pagesKeratoconus: Picture 1BuiyiWongNo ratings yet
- Silo - Tips - How To Take An Ophthalmic HistoryDocument5 pagesSilo - Tips - How To Take An Ophthalmic HistorySumon SarkarNo ratings yet
- Ptosis (Wiki)Document6 pagesPtosis (Wiki)lochnezNo ratings yet
- Corneal DystrophyDocument5 pagesCorneal DystrophyDejan JanevNo ratings yet
- Dry Eye Disease GuideDocument25 pagesDry Eye Disease Guide215045 zulfa laili aNo ratings yet
- Oftalmitis SimpatikaDocument12 pagesOftalmitis SimpatikaKarina HelsaNo ratings yet
- Treating Epithelial Downgrowth with 5-Fluorouracil InjectionsDocument5 pagesTreating Epithelial Downgrowth with 5-Fluorouracil Injectionsaghnia jolandaNo ratings yet
- Congenital Ptosis CaseDocument8 pagesCongenital Ptosis CaseHitesh Sharma67% (3)
- Equine Recurrent Uveitis: U.S.A.M.V. Cluj-Napoca Facultatea de Medicină Veterinară Disciplina: OftalmologieDocument9 pagesEquine Recurrent Uveitis: U.S.A.M.V. Cluj-Napoca Facultatea de Medicină Veterinară Disciplina: OftalmologiePatricia PopNo ratings yet
- Blowoutfractures PresentationDocument38 pagesBlowoutfractures PresentationVISHAKHANo ratings yet
- Fundoscopy Guide for OSCE ExamsDocument19 pagesFundoscopy Guide for OSCE ExamsMohamed Anas SayedNo ratings yet
- Congenital PtosisDocument15 pagesCongenital PtosisRobiniskandarNo ratings yet
- Ptosis (Eyelid) - WikipediaDocument26 pagesPtosis (Eyelid) - WikipediaRishabh ParakhNo ratings yet
- Seasonal Monthly Variation Amongst Reported Cataract Surgeries in IndiaDocument92 pagesSeasonal Monthly Variation Amongst Reported Cataract Surgeries in IndiafriendsofindiaNo ratings yet
- Exposure KeratopathyDocument12 pagesExposure KeratopathyFahyuniNo ratings yet
- Eye & ENTDocument12 pagesEye & ENTShandar SadafNo ratings yet
- Pan Uveitis (Causes and MGT of Sympathetic Ophthalmitis)Document21 pagesPan Uveitis (Causes and MGT of Sympathetic Ophthalmitis)Edoga Chima EmmanuelNo ratings yet
- MyopiaDocument11 pagesMyopiablueiceNo ratings yet
- Congenital Ptosis - GenetikaDocument28 pagesCongenital Ptosis - GenetikaJohanes Arie SetiawanNo ratings yet
- Internuclear OphthalmoplegiaDocument7 pagesInternuclear OphthalmoplegiaGrozaAlinaNo ratings yet
- Treatment of Blepharitis Recent Clinical TrialsDocument12 pagesTreatment of Blepharitis Recent Clinical TrialsSandra PeñuelaNo ratings yet
- MiddleEastAfrJOphthalmol19113-4844325 132723Document9 pagesMiddleEastAfrJOphthalmol19113-4844325 132723Vincent LivandyNo ratings yet
- The Association of Carotid Cavernous Fistula With Graves' Ophthalmopathy Brief CommunicationsDocument3 pagesThe Association of Carotid Cavernous Fistula With Graves' Ophthalmopathy Brief CommunicationsRiris SihotangNo ratings yet
- Primary vs. Secondary Angle Closure Glaucoma: DiseaseDocument1 pagePrimary vs. Secondary Angle Closure Glaucoma: Diseasefarah azizahNo ratings yet
- Blepharitis - UpToDateDocument37 pagesBlepharitis - UpToDateJorge Leonardo BedoyaNo ratings yet
- Diagnosis and Management of Pseudoexfoliation Glaucoma - American Academy of Ophthalmology PDFDocument7 pagesDiagnosis and Management of Pseudoexfoliation Glaucoma - American Academy of Ophthalmology PDFnoviaNo ratings yet
- Eye Trauma: Brief IntroductionDocument16 pagesEye Trauma: Brief IntroductionOchi D. GreenNo ratings yet
- MR 180 EditedDocument6 pagesMR 180 EditedfatmadianaNo ratings yet
- Miopi X Katarak 4Document5 pagesMiopi X Katarak 4Melati Nurul UtamiNo ratings yet
- Fundus Autofluorescence and Optical Coherence TomoDocument4 pagesFundus Autofluorescence and Optical Coherence TomoAndi Tiara S. AdamNo ratings yet
- Complications in UveitisFrom EverandComplications in UveitisFrancesco PichiNo ratings yet
- Skin Manifestations Associated With COVID-19: Current Knowledge and Future PerspectivesDocument12 pagesSkin Manifestations Associated With COVID-19: Current Knowledge and Future PerspectivesruditacitrahahaNo ratings yet
- Skin Manifestations Associated With COVID-19: Current Knowledge and Future PerspectivesDocument12 pagesSkin Manifestations Associated With COVID-19: Current Knowledge and Future PerspectivesruditacitrahahaNo ratings yet
- Bahan PanuveitisDocument28 pagesBahan PanuveitisruditacitrahahaNo ratings yet
- Daftar PustakaDocument1 pageDaftar PustakaruditacitrahahaNo ratings yet
- Peters AnomalyDocument7 pagesPeters AnomalyruditacitrahahaNo ratings yet
- TOEFLDocument3 pagesTOEFLruditacitrahahaNo ratings yet
- Jurnal1 PDFDocument6 pagesJurnal1 PDFruditacitrahahaNo ratings yet
- Ge 5 Lesson 5Document29 pagesGe 5 Lesson 5Lea MendarosNo ratings yet
- Daily Time Record Daily Time Record: Hazel Mae A. Monterde, RN Hazel Mae A. Monterde, RNDocument1 pageDaily Time Record Daily Time Record: Hazel Mae A. Monterde, RN Hazel Mae A. Monterde, RNTyler BertNo ratings yet
- MSC114 LessonsDocument54 pagesMSC114 Lessonsgrashew maanNo ratings yet
- Vasa Praevia RCOG GTGDocument13 pagesVasa Praevia RCOG GTGMariaBrincatNo ratings yet
- Obesity Obesity OverviewDocument6 pagesObesity Obesity OverviewLorena IbarrolaNo ratings yet
- Orthodontics & Dentofacial Orthopaedics: Page 1 of 24Document24 pagesOrthodontics & Dentofacial Orthopaedics: Page 1 of 24Abdul MohaiminNo ratings yet
- Taklimat Akademik Program MSC Counselling, MSW, MSC Correctional Science 6 September 2020 PDFDocument30 pagesTaklimat Akademik Program MSC Counselling, MSW, MSC Correctional Science 6 September 2020 PDFNCNNo ratings yet
- ANNEX DQAC Member List 29 OctDocument29 pagesANNEX DQAC Member List 29 OctSpace HR100% (1)
- Special Release 3 - Women and Men in Western Visayas PDFDocument8 pagesSpecial Release 3 - Women and Men in Western Visayas PDFJing PanganibanNo ratings yet
- Nevada CTE Recommended Equipment for Foods and Nutrition ProgramsDocument2 pagesNevada CTE Recommended Equipment for Foods and Nutrition Programsnithya nithyaNo ratings yet
- 1.principles of Business EthicsDocument7 pages1.principles of Business Ethicslegacy guptaNo ratings yet
- ® Whitening Fluoride Toothpaste: Product Overview Frequently Asked QuestionsDocument2 pages® Whitening Fluoride Toothpaste: Product Overview Frequently Asked QuestionsDina TrinidadNo ratings yet
- Preliminary Findings From RULER Approach in Spanish Teachers' Emotional Intelligence and Work EngagementDocument24 pagesPreliminary Findings From RULER Approach in Spanish Teachers' Emotional Intelligence and Work EngagementDaniela MendozaNo ratings yet
- Lisa Maley: Elementary School Teacher 4 Or5 GradeDocument2 pagesLisa Maley: Elementary School Teacher 4 Or5 Gradeapi-279892655No ratings yet
- IO ScriptDocument2 pagesIO ScriptShreya SagaonkarNo ratings yet
- 293 871 3 PBDocument7 pages293 871 3 PBDiana PertiwiNo ratings yet
- Inspection Checklist of Fishery Enterprises Handling Live FishDocument4 pagesInspection Checklist of Fishery Enterprises Handling Live FishBong PerezNo ratings yet
- Strength For Runners by Phily Bowden CoachingDocument7 pagesStrength For Runners by Phily Bowden CoachingKiranNo ratings yet
- Aug. 10, 2013Document10 pagesAug. 10, 2013The Delphos HeraldNo ratings yet
- ERROR DETECTION (New pattern) for Upcoming Mains ExamDocument31 pagesERROR DETECTION (New pattern) for Upcoming Mains Examishky manoharNo ratings yet
- AISD - Dental - Cigna - PPO & HMO Plan Information - 2019-2020Document1 pageAISD - Dental - Cigna - PPO & HMO Plan Information - 2019-2020Jordin TumlinsonNo ratings yet