Professional Documents
Culture Documents
Transient Ischemic Attacks: Part I. Diagnosis and Evaluation
Uploaded by
Andi Saputra0 ratings0% found this document useful (0 votes)
27 views10 pagesA TIA presents as a syndrome rather than any one sign or symptom. There is no reliable way to determine if the abrupt onset of neurologic deficits represents reversible ischemia without subsequent brain damage. Transient ischemic attack is no longer considered a benign event but a critical harbinger of impending stroke.
Original Description:
Original Title
p1665
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentA TIA presents as a syndrome rather than any one sign or symptom. There is no reliable way to determine if the abrupt onset of neurologic deficits represents reversible ischemia without subsequent brain damage. Transient ischemic attack is no longer considered a benign event but a critical harbinger of impending stroke.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
27 views10 pagesTransient Ischemic Attacks: Part I. Diagnosis and Evaluation
Uploaded by
Andi SaputraA TIA presents as a syndrome rather than any one sign or symptom. There is no reliable way to determine if the abrupt onset of neurologic deficits represents reversible ischemia without subsequent brain damage. Transient ischemic attack is no longer considered a benign event but a critical harbinger of impending stroke.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 10
than 50 percent of all adverse events
occurred within the first four days after
the TIA. Notably, of the patients with TIA
who returned to the emergency depart-
ment with stroke (10.5 percent), approxi-
mately one half had the stroke within
the first 48 hours after the initial TIA. In
2.6 percent of patients with TIA, hospi-
talization was required for cardiac events,
including congestive heart failure, unsta-
ble angina, cardiac arrest, and ventricular
arrhythmia.
Clinical Presentation
The more common clinical presenta-
tions of TIA are described in Table 1. In
general, a TIA presents as a syndrome
rather than any one sign or symptom.
Pre-emergency Department Care
There is no reliable way to determine
if the abrupt onset of neurologic deficits
represents reversible ischemia without
subsequent brain damage or if ischemia
will result in permanent damage to the
brain (e.g., stroke). Therefore, all patients
B
ased on an increased under-
standing of brain ischemia
and the introduction of new
treatment options, a working
group has proposed rede-
fining transient ischemic attack (TIA) as
a brief episode of neurological dysfunc-
tion caused by focal brain or retinal isch-
emia, with clinical symptoms typically
lasting less than one hour, and without
evidence of acute infarction.
1(p1715)
This
definition underscores the urgency of rec-
ognizing TIA as an important warning of
impending stroke and facilitating rapid
evaluation and treatment of TIA to pre-
vent permanent brain ischemia.
Epidemiology
An estimated 200,000 to 500,000 TIAs
occur annually in the United States.
2
One study
2
found that 25 percent of
patients who presented to an emergency
department with TIA had adverse events
within 90 days; 10 percent of the events
were strokes, and the vast majority of
the strokes were fatal or disabling.
3
More
Transient ischemic attack is no longer considered a benign event but, rather, a critical
harbinger of impending stroke. Failure to quickly recognize and evaluate this warning
sign could mean missing an opportunity to prevent permanent disability or death. The
90-day risk of stroke after a transient ischemic attack has been estimated to be approxi-
mately 10 percent, with one half of strokes occurring within the first two days of the
attack. The 90-day stroke risk is even higher when a transient ischemic attack results
from internal carotid artery stenosis. Most patients reporting symptoms of transient
ischemic attack should be sent to an emergency department. Patients who arrive at
the emergency department within 180 minutes of symptom onset should undergo an
expedited history and physical examination, as well as selected laboratory tests, to
determine if they are candidates for thrombolytic therapy. Initial testing should include
complete blood count with platelet count, prothrombin time, International Normalized
Ratio, partial thromboplastin time, and electrolyte and glucose levels. Computed tomo-
graphic scanning of the head should be performed immediately to ensure that there
is no evidence of brain hemorrhage or mass. A transient ischemic attack can be mis-
diagnosed as migraine, seizure, peripheral neuropathy, or anxiety. (Am Fam Physician
2004;69:1665-74,1679-80. Copyright 2004 American Academy of Family Physicians.)
Transient Ischemic Attacks:
Part I. Diagnosis and Evaluation
NINA J. SOLENSKI, M.D., University of Virginia Health Sciences Center, Charlottesville, Virginia
O A patient infor-
mation handout on
strokes and TIAs, writ-
ten by the author of
this article, is provided
on page 1679.
See page 1591 for defi-
nitions of strength-of-
recommendation labels.
COVER ARTICLE
This article
exemplifies the
AAFP 2004 Annual
Clinical Focus on caring
for Americas aging
population.
This is part I of a two-
part article on transient
ischemic attacks. Part
II, Treatment, will
appear in this issue on
page 1681.
Downloaded from the American Family Physician Web site at www.aafp.org/afp. Copyright 2004 American Academy of Family Physicians. For the private, noncommercial
use of one individual user of the Web site. All other rights reserved. Contact copyrights@aafp.org for copyright questions and/or permission requests.
with symptoms of TIA should receive an
expedited evaluation.
Office staff should be trained to inform
the family physician immediately if a patient
calls or presents with symptoms that could
represent a TIA. Neurologic symptoms that
crescendo with increasing frequency, dura-
tion, or severity are particularly ominous signs
of impending stroke.
Most patients with possible TIA should be
sent immediately to the nearest emergency
department. If they have had symptoms
for fewer than 180 minutes, they should be
sent to an emergency department that offers
acute thrombolytic therapy. Patients should
not drive themselves to the hospital. To
speed evaluation, it is appropriate to activate
the 9-1-1 Emergency Medical Service system
for transport.
2,3
On presentation to the emergency depart-
ment, patients who have had symptoms for
fewer than 180 minutes might be candidates
1666-AMERICAN FAMILY PHYSICIAN www.aafp.org/afp VOLUME 69, NUMBER 7 / APRIL 1, 2004
The proposed redefinition of transient ischemic attack is a
brief episode of neurological dysfunction caused by focal
brain or retinal ischemia, with clinical symptoms typically
lasting less than one hour, and without evidence of acute
TABLE 1
Common Clinical Presentations of TIA
Affected area Signs and symptoms Implications
Cranial nerves Visual loss in one or both eyes Bilateral loss may indicate more ominous onset of brainstem
ischemia.
Double vision If double vision is subtle, the patient may describe it as
blurry vision.
Vestibular dysfunction True vertigo is likely to be described as a spinning sensation
rather than nonspecific lightheadedness.
Difficulty swallowing Trouble swallowing may indicate brainstem involvement; if the
swallowing problem is severe, there may be an increased risk
of aspiration.
Motor function Unilateral or bilateral weakness affecting Bilateral signs may indicate more ominous onset of brainstem
the face, arm, or leg ischemia.
Sensory function Unilateral or bilateral: either decreased If sensory dysfunction occurs without other signs or symptoms,
sensation (numbness) or increased the prognosis may be more benign, but recurrence is high.
sensation (tingling, pain) in the face,
arm, leg, or trunk
Speech and Slurring of words or reduced verbal output; If speech is severely slurred or facial drooling is excessive, there
language difficulty pronouncing, comprehending, is an increased risk of aspiration.
or finding words Writing and reading also may be impaired.
Coordination Clumsy arms, legs, or trunk; loss of balance Incoordination of limbs, trunk, or gait may indicate cerebellar
or falling (particularly to one side) with or brainstem ischemia.
standing or walking
Psychiatric or Apathy or inappropriate behavior These symptoms can indicate frontal lobe involvement and
cognitive frequently are misinterpreted as poor volitional cooperation.
function
Excessive somnolence This symptom may indicate bilateral hemispheric or brainstem
involvement.
Agitation or psychosis Rarely, these symptoms may indicate brainstem ischemia,
particularly if they occur in association with cranial nerve
or motor dysfunction.
Confusion or memory changes These rarely are isolated symptoms; more frequently, they are
associated with language, motor, sensory, or visual changes.
Inattention to surrounding environment, Depending on the severity of neglect, the physician may
particularly to one side; if severe, patient need to lift the patients arm to check for strength,
may deny deficit or even his or her own rather than rely on the patient to perform this task.
body parts.
TIA = transient ischemic attack.
for treatment with tissue-type plasminogen
activator (tPA).
4,5
If a patient is not a candi-
date for tPA treatment, antiplatelet therapy
should be initiated as soon as it can be deter-
mined that there are no contraindications.
4-6
[Reference 6: SOR A, rating of benefits]
Inpatient or Outpatient Evaluation
Guidelines issued by the National Stroke
Association
7
recommend evaluation within
hours of the onset of TIA symptoms, prefer-
ably in an emergency department. If appro-
priate imaging studies are not immediately
available in the emergency department or out-
patient setting, the patient should be hospital-
ized for observation.
7
[SOR C, expert opin-
ion] Relative indications for more extended
inpatient evaluation for TIA or stroke are
listed in Table 2.
Patients with symptoms of acute TIA for
fewer than 24 to 48 hours should undergo
diagnostic testing in the emergency depart-
ment.
8
[SOR C, expert opinion] Patients
whose symptoms have resolved for more than
48 hours should receive urgent inpatient or
outpatient evaluation.
Initial Work-Up for Suspected TIA
The first step in evaluating a patient with
symptoms of TIA is to confirm the diagnosis
(Figure 1).
DIFFERENTIAL DIAGNOSIS
The most common imitators of TIA are
glucose derangement, migraine, seizure, post-
ictal states, and tumors (especially with acute
hemorrhage).
TIA typically has a rapid onset, and maxi-
mal intensity usually is reached within min-
utes. Fleeting episodes lasting one or two sec-
onds or nonspecific symptoms such as fatigue,
lightheadedness (in the absence of other cer-
ebellar or brainstem symptoms), and bilateral
rhythmic shaking of the limbs are less likely
presentations of acute cerebral ischemia.
Distinguishing TIA from migraine aura
can be difficult. Younger age, previous his-
tory of migraine (with or without aura), and
associated headache, nausea, or photophobia
are more suggestive of migraine than TIA. In
general, migraine aura tends to have a march-
ing quality; for example, symptoms such as
tingling may progress from the fingers to
the forearm to the face. Migraine aura also is
APRIL 1, 2004 / VOLUME 69, NUMBER 7 www.aafp.org/afp AMERICAN FAMILY PHYSICIAN-1667
Neurologic symptoms that crescendo with increasing fre-
quency, duration, or severity are particularly ominous signs of
impending stroke.
TABLE 2
Relative Indications for Inpatient Evaluation of Possible TIA or Stroke*
Condition Implications
High-risk cardioembolic source: acute myocardial infarction Consider anticoagulation.
(especially if large and significant wall-motion abnormality
is present), mural thrombi, new-onset atrial fibrillation
TIAs manifested by major symptoms such as dense paralysis Possible evolving large hemispheric stroke with increased risk of
or severe language disorder brain swelling
Increasing frequency or severity of TIAs (crescendo pattern) Possible evolving thromboembolic stroke
Evidence of high-grade carotid artery stenosis Carotid artery evaluation for possible emergency intervention (surgery,
stent, or angioplasty)
Drooling, imbalance, decreased alertness, difficulty Increased risk of falling, or of aspiration and other pulmonary
swallowing complications
Severe headache, photophobia, stiff neck, recent syncope Possible subarachnoid hemorrhage: obtain emergency computed
tomographic scan of the head; if the scan is negative but clinical
suspicion remains high, cerebrospinal fluid evaluation or possible
cerebral angiography is needed.
TIA = transient ischemic attack.
*May require more than 23 hours of observation in the emergency department, or hospitalization for observation.
more likely to have a more gradual onset and
resolution, with a longer duration of symp-
toms than in a typical TIA.
If a patient has explosive onset of a severe
headache, with or without photophobia, stiff
neck, or syncope, acute subarachnoid hemor-
rhage is a possibility. Rarely, TIA is mistaken
for the first presentation of multiple sclerosis
in young patients or for amyotrophic lateral
sclerosis in older patients.
HISTORY
A general medical history should be
obtained in all patients with suspected TIA.
Special emphasis should be given to pos-
sible symptoms of TIA (Table 1), and stroke
risk factors should be identified to determine
the likelihood that the symptoms are caused
by TIA. Modifiable risk factors for stroke
include hypertension, diabetes, cardiac dis-
ease, elevated blood lipid levels, carotid artery
stenosis, smoking, sickle cell anemia, excessive
alcohol use, obesity, and physical inactivity.
7
Whether hypercholesterolemia is an inde-
pendent primary risk factor for stroke remains
uncertain.
9
However, hypercholesterolemia is
a significant risk factor for coronary heart dis-
ease (CHD) and therefore can be considered
1668-AMERICAN FAMILY PHYSICIAN www.aafp.org/afp VOLUME 69, NUMBER 7 / APRIL 1, 2004
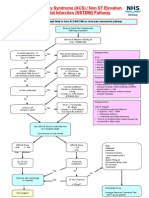
Initial Work-Up for Suspected TIA
FIGURE 1. Initial work-up for the patient with possible transient ischemic attack (TIA). (IV =
intravenous; tPA = tissue-type plasminogen activator; CT = computed tomography; ECG = elec-
trocardiography; PT = prothrombin time; aPTT = activated partial thromboplastin time; INR =
International Normalized Ratio; MRI = magnetic resonance imaging; MRA = magnetic resonance
angiography)
Frequent vital signs, with attention to blood pressure* and heart rhythm
Head CT*
Cardiac monitoring: ECG
Medical and neurologic examination*
Initial laboratory tests: complete blood count with platelet count*; electrolyte,
glucose,* and renal function measurements; PT,* aPTT,* and INR*
Carotid artery evaluation
Head MRI and MRA of intracranial and neck vessels, if available and appropriate
Further testing in selected patients (see Table 3)
Is patient a candidate for
thrombolytic therapy?
Initiate aspirin therapy
within 24 to 48 hours
(if no contraindications).
Perform certain tests (*) within 25 minutes of
patients arrival in emergency department; screen
for inclusion/exclusion criteria for IV tPA therapy.
Send patient to hospital emergency
department for evaluation.
Urgent outpatient evaluation to identify
cause of TIA; if imaging studies are not
available in a timely fashion, admit patient.
Identify and treat stroke risk factors.
Begin medical therapy, including antiplatelet
therapy, as soon as possible.
Acute (did transient symptoms occur <24 to 48 hours ago)?
Confirm TIA history.
Yes No
No Yes
an important risk factor for ischemic stroke.
There appears to be a stronger data relationship
between total and low-density lipoprotein cho-
lesterol levels, as well as a protective influence
of high-density lipoprotein cholesterol levels, in
cervical carotid artery atherosclerosis.
10
Other important information includes a
family history of stroke (including cerebral
aneurysm or hypercoagulable state), the use
of over-the-counter or illicit drugs, a history
of migraine or severe headaches, recent
head trauma, previous systemic clots and,
in a woman of childbearing age, a history of
spontaneous abortion. Certain findings may
indicate the need for special diagnostic tests
(Table 3).
PHYSICAL EXAMINATION
Vital signs should be evaluated, includ-
ing blood pressures in both arms, to rule
out stenosis of the subclavian artery, which
may manifest as grossly asymmetric pressures.
Auscultation of the heart and neck also should
be performed. Carotid bruits, when present,
are neither highly specific nor highly sensitive
for carotid artery stenosis.
All patients with possible TIA should
receive a detailed, documented neurologic
examination, with emphasis on cognitive and
language function, cranial nerve function,
facial and limb strength, sensory function,
deep tendon reflex symmetry, and coordi-
nation. This examination can be helpful in
determining whether a patient previously had
an unrecognized stroke. It also can serve as a
baseline examination if the patients neuro-
logic status worsens or neurologic symptoms
recur. Occasionally, the neurologic examina-
tion may identify a nonischemic cause for
an acute neurologic deficit (e.g., acute radial
nerve palsy, isolated third-nerve palsy in a
patient with diabetes mellitus).
DIAGNOSTIC TESTS
Brain Imaging. Computed tomographic
(CT) scanning of the head without contrast
medium should be performed to identify
subarachnoid hemorrhage, intracranial hem-
orrhage, or subdural hematoma. Urgent iden-
tification of these conditions is critical because
neurosurgical intervention or special manage-
ment may be required.
If hemorrhage is present, treatment with tPA
or anticoagulants that may worsen central ner-
vous system bleeding should be avoided. Spe-
cial measures may be needed to manage blood
pressure if the patient is found to have hyper-
tension-mediated intracranial hematoma, and
further testing may be required if the patient is
found to have subarachnoid hemorrhage (e.g.,
cerebral angiography to rule out aneurysm).
CT scanning also can identify conditions
that mimic TIA, including tumors and other
masses (especially if hemorrhage occurs
acutely within a mass), as well as conditions
that are associated with seizures or auras.
A head CT scan can identify signs of early
brain damage or evidence of old strokes.
11,12
Finally, CT scanning of the head with contrast
medium should be performed in the febrile
patient to rule out an infectious cause or in the
patient with a suspected mass (e.g., metastatic
carcinoma, abscess).
Because of increased bony artifact in the
posterior fossa, CT scanning is not sensitive
for evaluating disease in the brainstem or
cerebellum. In these instances, magnetic reso-
nance imaging (MRI) is the preferred study.
Electrophysiologic Testing. All patients should
have a baseline electrocardiogram (ECG) with
rhythm strip.
6,12,13
If the ECG is abnormal or the
patient has a history of cardiac disease, echocar-
diography should be performed. Atrial fibrilla-
tion and left ventricular hypertrophy (suggest-
ing unrecognized chronic hypertension) are
important risk factors for stroke. Recent data
suggest that the 90-day risk for a cardiac event
TIA
APRIL 1, 2004 / VOLUME 69, NUMBER 7 www.aafp.org/afp AMERICAN FAMILY PHYSICIAN-1669
Conditions that may mimic TIA include glucose derangement,
migraine, seizure, postictal states, tumors or, rarely, multiple
sclerosis and amyotrophic lateral sclerosis.
is seven times higher in patients with TIA and
abnormal ECG findings than in those with a
normal ECG (4.2 versus 0.6 percent).
13
If the ECG is unrevealing, cardiac moni-
toring in selected patients could help diag-
nose paroxysmal atrial fibrillation (or other
arrhythmias in patients with syncope or pal-
pitations). In patients with untreated atrial
fibrillation, echocardiography may identify
a thromboembolic source or left ventricular
systolic dysfunction, both of which are com-
mon predictors of ischemic stroke.
14
Transesophageal echocardiography is super-
ior to transthoracic echocardiography for eval-
uating possible dysfunction of the left atrium
(including thrombus) or a patent foramen
ovale (an etiology for paradoxical emboli),
atrial septal defects (including aneurysm), and
aortic plaque. Recent clinical trials
15,16
suggest
that transesophageal echocardiography should
be considered in patients without an identifi-
able cause of TIA or known cardiac disease,
because it may detect a condition requiring
therapeutic intervention (e.g., anticoagulation
for thrombus). Aortic plaque, which has been
associated with stroke, can be visualized well on
transesophageal echocardiography.
Laboratory Tests. A complete blood count
with platelet count should be obtained to rule
out polycythemia, thrombocytopenia, and
thrombocytosis. It is helpful to know the pro-
thrombin time (PT), activated partial throm-
boplastin time (aPTT), and International
Normalized Ratio (INR) before antiplatelet or
anticoagulation therapy is administered; the
PT, aPTT, and INR can be elevated in some
hypercoagulable states.
The glucose level should be determined to
1670-AMERICAN FAMILY PHYSICIAN www.aafp.org/afp VOLUME 69, NUMBER 7 / APRIL 1, 2004
TABLE 3
Further Diagnostic Testing Based on the History in Patients Undergoing Evaluation for Possible TIA*
History Implications Tests
Headache in postpartum Venous thrombosis MRI with venography or cerebral angiography
or dehydration setting
Fever Subacute or acute bacterial Blood cultures, head CT scan with and without contrast medium;
endocarditis in selected patients with confirmed bacterial endocarditis,
perform cerebral angiography to rule out a mycotic aneurysm.
Confusion, headache, CNS vasculitis Cerebral angiography, ESR, lumbar puncture (to look for elevation of
seizure white blood cell counts in particular)
Hypertensive encephalopathy Careful blood pressure monitoring in intensive care setting; consider
MRI.
Rheumatologic disease, CNS vasculitis Consider cerebral angiography, ESR, lumbar puncture (to look for
sympathomimetic drug use elevation of white blood cell counts in particular).
Recent myocardial infarction Cardioembolic source Transthoracic or esophageal echocardiography
Head, neck, jaw pain, Carotid or vertebral dissection Consider cerebral angiography or other neck neuroimaging studies
especially after trauma (see text).
Abrupt onset of severe Subarachnoid hemorrhage Emergency head CT scan; if the scan is negative, evaluate
headache with cerebrospinal fluid for elevated red blood cell count or perform
photophobia, or cerebral angiography to rule out aneurysm or arteriovenous
recent syncope malformation.
Confusion, stupor, coma, Vertebrobasilar ischemia Consider intracranial magnetic resonance angiography or cerebral
other brainstem symptoms angiography; if basilar artery is significantly thrombosed, consider
(poor prognosis) intra-arterial thrombolytic therapy (if available).
Brain swelling, impending Immediate head CT scan; if the scan is positive, emergency
herniation neurosurgical intervention may be required.
No obvious risk factors Cryptogenic stroke, patent Consider cerebral angiography, transesophageal echocardiography,
for stroke foramen ovale, intra-atrial and work-up for hypercoagulable state.
septal aneurysm, valvular
or aortic arch disease
TIA = transient ischemic attack; MRI = magnetic resonance imaging; CT = computed tomography; CNS = central nervous system;
ESR = erythrocyte sedimentation rate.
*The initial work-up for the patient with possible TIA is outlined in Figure 1.
rule out hypoglycemia or hyperglycemia and to
help diagnose occult diabetes. Blood urea nitro-
gen and creatinine levels are important, because
poor renal status may prohibit the use of con-
trast media in imaging studies. An erythrocyte
sedimentation rate (ESR) should be obtained to
potentially rule out vasculitis. Finally, a drug of
abuse screen, a pregnancy test, a homocystine
level determination, or a blood alcohol level
measurement should be performed in selected
patients.
Follow-Up Evaluation
LIPID PROFILE
After the initial more abbreviated evalua-
tion in the emergency department, risk factors
for stroke can be reassessed thoroughly later
in the evaluation. Recent data indicate that
treatment with statins (3-hydroxy-3-methyl-
glutaryl coenzyme A reductase inhibitors)
reduces the risk of stroke by about 30 percent
in patients with CHD.
17,18
Therefore, a fasting
lipid profile reflective of the patients normal
eating habits should be obtained, and statin
therapy should be initiated if indicated.
HYPERCOAGULABLE STATES
Patients with known risk factors for stroke
and those with a history of migraine, sponta-
neous abortion, pulmonary emboli, or deep
venous thrombosis, or a family history of any
of these conditions, should be evaluated for
hypercoagulable states. Initial tests include
ESR, antinuclear antibody test, rapid plasma
reagent test, and antiphospholipid antibody
tests. Referral to a hematologist or neurolo-
gist can ensure cost-effective evaluation of
the multiple coagulation-factor abnormalities
and conditions that can cause embolic stroke.
TESTING FOR ARTERIAL PATENCY
AND BLOOD FLOW
Carotid duplex ultrasonography should be
performed in a reliable laboratory, preferably
one with validation against the results of cere-
bral angiography. Alternatively, cerebral and
cervical vessels can be evaluated by magnetic
resonance angiography (MRA) with contrast
medium or by CT angiography. If the work-
up demonstrates carotid or other large-vessel
atherosclerotic disease in the patient with TIA
and unrecognized CHD, coronary artery test-
ing is recommended.
19
MRI. Clear advantages of MRI of the brain
over CT scanning of the head include better
imaging of tissues (i.e., greater sensitivity for
early edema), superior imaging within the
posterior fossa (including the brainstem and
cerebellum), additional planes of imaging
(sagittal, coronal, and oblique), and no expo-
sure to radiation.
A clear disadvantage of brain MRI is that it
may or may not identify hemorrhage. For this
reason, although MRI can be helpful, it should
not replace urgent CT scanning of the head in
the initial work-up of patients with possible
TIA. When cerebrovascular malformation,
aneurysm, cerebral venous thrombosis, or arte-
ritis is suspected, MRI or MRA is preferred.
Diffusion-weighted imaging detects cellular
edema as early as 10 to 15 minutes after symp-
tom onset. However, this technique is not yet
widely available.
MRA. This imaging modality is a noninva-
sive means of assessing intra- and extracranial
vessels. Current MRA techniques use intrave-
nously administered contrast medium (gado-
linium) to visualize the vessels.
MRA with the administration of con-
trast medium also is effective in identify-
ing vertebrobasilar stenosis, although recent
data suggest that intracranial vertebral artery
disease can be missed.
20
Depending on the
MRA acquisition technique, the percent-
age of intracranial vessel stenosis can be
overestimated (sensitivity of approximately
85 percent compared with cerebral angiog-
raphy).
21
Therefore, if accuracy is therapeu-
tically important, cerebral angiography is
necessary.
When near occlusion of the carotid artery
cannot be distinguished from complete occlu-
sion on MRA or carotid Doppler ultrasound
studies, cerebral angiography should be con-
TIA
APRIL 1, 2004 / VOLUME 69, NUMBER 7 www.aafp.org/afp AMERICAN FAMILY PHYSICIAN-1671
sidered. Surgery generally cannot be per-
formed on completely occluded vessels.
Special consideration should be given to
patients who present with a history or symp-
toms that suggest arterial dissection. This con-
dition can be diagnosed using neck MRI scans
in certain sequences that can identify hemor-
rhage within the vessel wall (T
1
-weighted
images with fat suppression).
Patients with carotid artery dissection can
present with acute or subacute unilateral
neck, head, or jaw pain. These symptoms may
be associated with visual or language deficits,
or with sensorimotor deficits, particularly in
the opposite arm. More typically, patients
with carotid artery dissection present with
only some of these features, such as temporal
headache with lateral neck pain and, possi-
bly, transient visual obscuration (amaurosis
fugax) because of thromboemboli in the oph-
thalmic artery.
Both carotid and vertebral artery dis-
sections have been described after trauma,
although spontaneous dissection also is com-
mon. Patients should be evaluated for con-
nective tissue disease because of the associated
increased risk of dissection.
If the MRI or MRA study is inconclusive,
cerebral angiography should be used to rule
out arterial dissection or better define the
percentage of vessel narrowing.
CT Angiography. This modality is another
state-of-the-art technique for detecting
blood flow to the brain. CT angiography also
is becoming a useful imaging modality for
identifying carotid or vertebral artery dissec-
tion. Because the technique requires venous
injection of contrast dye, the patients renal
status should be considered before the test is
performed.
Conventional CT scanning in combination
with CT angiography currently is being evalu-
ated as an addition to the diagnostic imaging
tools for use in patients with TIA or stroke.
This combination can provide useful infor-
mation about vascular anatomy (in the form
of three-dimensional reconstructions) and
the extent and location of infarction. It may
allow rapid evaluation of patients with TIA or
stroke in hospitals or institutions that do not
have MRI capability.
Cerebral Angiography. This technique con-
tinues to be the gold standard for complete
evaluation of intracranial and extracranial ves-
sels. With cerebral angiography, both arterial
and venous phases of cerebral blood flow can
be visualized (dynamic study). However, cere-
bral angiography is an invasive technique that
can result in neurologic complications (total
incidence rate: 1.3 to 4.6 percent),
22,23
includ-
ing major stroke or death in 0.1 to 1.3 percent
of patients, depending on the study.
24,25
Relative indications for cerebral angiog-
raphy include suspected carotid dissection
unconfirmed on a noninvasive neuroimaging
study, subarachnoid hemorrhage (to identify
bleeding source), intracerebral hemorrhage in
the absence of hypertension, and vasculitis. If
one of these conditions is suspected, referral
to a neurologist can be helpful in obtaining
and interpreting the angiogram.
Special Considerations
VERTEBROBASILAR ISCHEMIA
Typical signs and symptoms of ischemic
syndromes involving the anterior and pos-
terior circulations are listed in Table 4. The
brainstem and cerebellum are confined within
the posterior fossa, a bony cavity with poor
tolerance of brain swelling or mass effects
(e.g., from hemorrhage). Because brainstem
structures are essential for preserving criti-
cal respiratory function and arousal states,
1672-AMERICAN FAMILY PHYSICIAN www.aafp.org/afp VOLUME 69, NUMBER 7 / APRIL 1, 2004
The Author
NINA J. SOLENSKI, M.D., is associate professor of neurology and a staff member of the
Stroke Center at the University of Virginia Health Sciences Center, Charlottesville. Dr.
Solenski received her medical degree from Jefferson Medical College of Thomas Jeffer-
son University, Philadelphia, and completed a neurology residency and cerebrovascular
fellowship at the University of Virginia Health Sciences Center.
Address correspondence to Nina J. Solenski, M.D., Stroke Center, Department of
Neurology, P.O. Box 800394, University of Virginia Health Sciences Center, Hospital
Dr., McKim Hall, Room 2055, Charlottesville, VA 22908 (e-mail: njs2j@virginia.edu).
Reprints are not available from the author.
patients with vertebrobasilar ischemia should
be monitored closely. It also is crucial to search
for life-threatening cerebrovascular disease,
such as basilar artery stenosis or thrombosis
or disease affecting multiple large vessels (e.g.,
bilateral, vertebral, or carotid artery stenosis).
TIA IN A YOUNG PATIENT
When a TIA occurs in a patient younger
than 45 years, particularly if there are no clear
risk factors for stroke, it is advisable to refer
the patient to a neurologist for consideration
of specialized testing. For example, it may be
necessary to determine the utility of cerebral
angiography to rule out vasculitis, carotid
artery dissection, and other forms of nonath-
erosclerotic vasculopathy, or lumbar spinal
puncture with cerebrospinal fluid evaluation
may be required to rule out chronic infection
or inflammation.
Because cardiac abnormalities are among
the most common causes of TIA in young
patients, a baseline ECG with rhythm strip
should be obtained, and transthoracic and
transesophageal echocardiography should be
considered. A toxicology screen for drugs
of abuse (especially sympathomimetic com-
pounds) usually is performed.
Several newly identified, genetically based
metabolic and hematologic syndromes have
been found to be associated with stroke. With
some of these syndromes, initial symptoms
occur in the younger years (late childhood,
adolescence, or early adulthood). Diagnosis
of these syndromes may require specialized
tests. Such testing could be important to bet-
ter define treatment options and prognosis, as
well as to identify family members who may
APRIL 1, 2004 / VOLUME 69, NUMBER 7 www.aafp.org/afp AMERICAN FAMILY PHYSICIAN-1673
TABLE 4
Typical Characteristics of Ischemic Syndromes Involving the Anterior and Posterior Circulations
Ischemic syndrome:
circulation involved Signs Symptoms
Anterior circulation* Visual-field cut Inability to see well (i.e., difficulty reading or driving
Language dysfunction (left hemisphere most Difficulty finding or understanding words, inability to read,
often affected): aphasia garbled or slurred speech
Motor dysfunction: contralateral face, arm, Dropping objects; depending on severity, inability to lift
or leg weakness or move a body part or objects
Sensory dysfunction: contralateral increased Tingling (paresthesias), numbness, or pain
or decreased sensation to pain, heat, or cold
Behavior dysfunction (right hemisphere): The patient usually reports no symptoms, but family
inattention to surrounding environment, members or others report that the patient has difficulty
particularly to one side; if severe, patient dressing, ignores half of food on a plate, or has poor
may deny deficits or even his or her own attention to one side of the room or to someone speaking
body parts to the patient on one side versus the other (most often,
the left side is ignored).
Posterior circulation Nystagmus Vertigo (spinning sensation)
Disconjugate gaze If subtle, blurry or double vision
Homonymous visual-field cut Inability to see well, especially to one side
Contralateral weakness Dropping objects, inability to fully lift or move the limb
Incoordination of trunk or limbs (ataxia) Clumsiness, falling, inability to coordinate an action
(e.g., drink from a cup without spilling contents)
Motor or sensory dysfunction on opposite For example, the patient may report double vision,
side of cranial nerve deficits (crossed signs droopiness on the left side of the face, and dragging
suggest brainstem involvement) of the right leg (because of weakness).
Bilateral signs Abrupt weakness of both legs, falling
Decreased mentation; stupor or coma Family members or others report that the patient has poor
responsiveness or that they are unable to arouse the patient.
*Includes the internal carotid artery, middle cerebral artery, and anterior cerebral artery, as well as the branches of these arteries.
Includes the vertebral arteries, basilar artery, and posterior cerebral artery, as well as the branches of these arteries.
TIA
be at risk for TIA or stroke.
The author indicates that she does not have any con-
flicts of interest. Sources of funding: none reported.
REFERENCES
1. Albers GW, Caplan LR, Easton JD, Fayad PB, Mohr
JP, Saver JL, et al. Transient ischemic attackpro-
posal for a new definition. N Engl J Med 2002;
347:1713-6.
2. Johnston CS, Gress DR, Browner WS, Sidney S.
Short-term prognosis after emergency department
diagnosis of TIA. JAMA 2000;284:2901-6.
3. Johnston CS. Transient ischemic attack. N Engl J
Med 2002;347:1687-92.
4. Warburton E. Stroke management. Clin Evid 2003;
(9):206-20.
5. Sudlow C, Gubitz G, Sandercock P, Lip G. Stroke
prevention. Clin Evid 2003;(9):221-45.
6. Adams HP Jr, Adams RJ, Brott T, del Zoppo GJ,
Furlan A, Goldstein LB, et al. Guidelines for
the early management of patients with ischemic
stroke: a scientific statement from the Stroke
Council of the American Stroke Association. Stroke
2003;34:1056-83.
7. Gorelick PB, Sacco RL, Smith DB, Alberts M, Mus-
tone-Alexander L, Rader D, et al. Prevention of a
first stroke: a review of guidelines and a multidis-
ciplinary consensus statement from the National
Stroke Association. JAMA 1999;281:1112-20.
8. Diagnosis and initial treatment of ischemic stroke.
Released October 2003. Accessed online February
20, 2004, at http://www.icsi.org/knowledge/detail.
asp?catID=29&itemID=166.
9. Sacco RL, Wolf PA, Gorelick PB. Risk factors and
their management for stroke prevention: outlook
for 1999 and beyond. Neurology 1999;53(7 suppl
4):S15-24.
10. Reed DM, Resch JA, Hayaski T, MacLean C, Yano
K. A prospective study of cerebral atherosclerosis.
Stroke 1988;19:820-5.
11. Albers GW, Hart RG, Lutsep HL, Newell DW,
Sacco RL. AHA scientific statement. Supplement
to the guidelines for the management of transient
ischemic attacks: a statement from the Ad Hoc
Committee on Guidelines for the Management of
Transient Ischemic Attacks, Stroke Council, Ameri-
can Heart Association. Stroke 1999;30:2502-11.
12. Culebras A, Kase CS, Masdeu JC, Fox AJ, Bryan RN,
Grossman CB, et al. Practice guidelines for the use
of imaging in transient ischemic attacks and acute
stroke. A report of the Stroke Council, American
Heart Association. Stroke 1997;28:1480-97.
13. Elkins JS, Sidney S, Gress DR, Go AS, Bernstein AL,
Johnston SC. Electrocardiographic findings predict
short-term cardiac morbidity after transient isch-
emic attack. Arch Neurol 2002;59:1437-41.
14. Echocardiographic predictors of stroke in patients
with atrial fibrillation: a prospective study of 1066
patients from 3 clinical trials. Arch Intern Med
1998;158:1316-20.
15. OBrien PJ, Thiemann DR, McNamara RL, Roberts
JW, Raska K, Oppenheimer SM, et al. Usefulness
of transesophageal echocardiography in predicting
mortality and morbidity in stroke patients without
clinically known cardiac sources of embolus. Am J
Cardiol 1998;81:1144-51.
16. Labovitz AJ. Transesophageal echocardiography
and unexplained cerebral ischemia: a multicenter
follow-up study. The STEPS Investigators. Signifi-
cance of Transesophageal Echocardiography in the
Prevention of Recurrent Stroke. Am Heart J 1999;
137:1082-7.
17. Randomised trial of cholesterol lowering in 4444
patients with coronary heart disease: the Scan-
dinavian Simvastatin Survival Study (4S). Lancet
1994;344:1383-9.
18. Plehn JF, Davis BR, Sacks FM, Rouleau JL, Pfeffer
MA, Bernstein V, et al. Reduction of stroke inci-
dence after myocardial infarction with pravastatin:
the Cholesterol and Recurrent Events (CARE)
study. The CARE Investigators. Circulation 1999;
99:216-23.
19. Adams RJ, Chimowitz MI, Alpert JS, Awad IA,
Cerqueria MD, Fayad P, et al. Coronary risk evalua-
tion in patients with transient ischemic attack and
ischemic stroke: a scientific statement for health-
care professionals from the Stroke Council and the
Council on Clinical Cardiology of the American
Heart Association/American Stroke Association.
Circulation 2003;108:1278-90.
20. Bhadelia RA, Bengoa R, Gesner L, Patel SK, Uzun
G, Wolpert SM, et al. Efficacy of MR angiography
in the detection and characterization of occlusive
disease in the vertebrobasilar system. J Comput
Assist Tomogr 2001;25:458-65.
21. Korogi Y, Takahashi M, Nakagawa T, Mabuchi N,
Watabe T, Shiokawa Y, et al. Intracranial vascular
stenosis and occlusion: MR angiographic findings.
AJNR Am J Neuroradiol 1997;18:135-43.
22. Hankey GJ, Warlow CP, Sellar RJ. Cerebral angio-
graphic risk in mild cerebrovascular disease. Stroke
1990;21:209-22.
23. Willinsky RA, Taylor SM, Ter Brugge K, Farb RI,
Tomlinson G, Montanera W. Neurologic complica-
tions of cerebral angiography: prospective analysis
of 2,899 procedures and review of the literature.
Radiology 2003;227:522-8.
24. Dion JE, Gates PC, Fox AJ, Barnett HJ, Blom RJ.
Clinical events following neuroangiography: a pro-
spective study. Stroke 1987;18:997-1004.
25. Young N, Chi KK, Ajaka J, McKay L, ONeill D, Wong
1674-AMERICAN FAMILY PHYSICIAN www.aafp.org/afp VOLUME 69, NUMBER 7 / APRIL 1, 2004
You might also like
- Transient Ischemic AttacksDocument10 pagesTransient Ischemic AttacksfabianounifenasNo ratings yet
- Transient Ischemic Attack: Clinical PracticeDocument9 pagesTransient Ischemic Attack: Clinical PracticeJuanita MesaNo ratings yet
- Ait Nejm 2020Document9 pagesAit Nejm 2020Ahmed JallouliNo ratings yet
- Ischemic Stroke Management by The Nurse PR - 2019 - The Journal For Nurse PractDocument9 pagesIschemic Stroke Management by The Nurse PR - 2019 - The Journal For Nurse PractLina SafitriNo ratings yet
- Activating A Stroke Alert - A Neurological Emergency - CE591Document7 pagesActivating A Stroke Alert - A Neurological Emergency - CE591Czar Julius Malasaga100% (1)
- Sumber 9Document18 pagesSumber 9Ali Laksana SuryaNo ratings yet
- Seizure Induced by Traumatic Brain Injury Case FileDocument7 pagesSeizure Induced by Traumatic Brain Injury Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Hypertensive CrisisDocument7 pagesHypertensive CrisisAbdul Hannan Ali100% (1)
- Nanda, A, Niranjan NS, Transient Ischemic Attack. Medscape. 2013Document6 pagesNanda, A, Niranjan NS, Transient Ischemic Attack. Medscape. 2013rahmatNo ratings yet
- A. Severe Migraine Attack B. Cluster Headache C. Subarachnoid Hemorrhage D. Hypertensive Encephalopathy E. EncephalitisDocument4 pagesA. Severe Migraine Attack B. Cluster Headache C. Subarachnoid Hemorrhage D. Hypertensive Encephalopathy E. EncephalitisVgdgNo ratings yet
- SBR 4Document16 pagesSBR 4YuhuNo ratings yet
- Drug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansDocument0 pagesDrug Treatment For Hypertensive Emergencies: New Concepts and Emerging Technologies For Emergency PhysiciansRajihah JihahNo ratings yet
- Yncope Earning Bjectives: EfinitionDocument5 pagesYncope Earning Bjectives: EfinitionmuhammadridhwanNo ratings yet
- TIA NeneDocument13 pagesTIA NenekenNo ratings yet
- Evaluation of SyncopeDocument11 pagesEvaluation of Syncopebluecrush1No ratings yet
- Syncope - Electrocardiographic and Clinical CorrelationDocument16 pagesSyncope - Electrocardiographic and Clinical CorrelationNANDY LUZ FERIA DIAZNo ratings yet
- Cerebro-Vascular Disease & Stroke: Faizan Zaffar KashooDocument57 pagesCerebro-Vascular Disease & Stroke: Faizan Zaffar KashooDrGasnasNo ratings yet
- HSA Controversias 2016Document9 pagesHSA Controversias 2016Ellys Macías PeraltaNo ratings yet
- Stroke 1. Disease/DisorderDocument11 pagesStroke 1. Disease/DisorderBiandaNo ratings yet
- Article Acute Stroke PDFDocument10 pagesArticle Acute Stroke PDFHeather PorterNo ratings yet
- Cardiovascular Emergencies SyncopeDocument10 pagesCardiovascular Emergencies SyncopeilltekneexzNo ratings yet
- Post Stroke ComplicationsDocument33 pagesPost Stroke Complicationsdiijah678100% (1)
- Nursing Care Management 103 Related Learning Experience Health TeachingDocument10 pagesNursing Care Management 103 Related Learning Experience Health Teachingkarenfaye00No ratings yet
- 3390-Article Text-1555-3802-10-20200606Document12 pages3390-Article Text-1555-3802-10-20200606Mayara Bongestab ParteliNo ratings yet
- Neurological EmergenciesDocument11 pagesNeurological Emergenciespunit lakraNo ratings yet
- Guide To ECT 2015Document25 pagesGuide To ECT 2015Diana CalderónNo ratings yet
- Cerebrovascular DisordersDocument20 pagesCerebrovascular DisordersPrimas Shahibba RidhwanaNo ratings yet
- 8 StrokeDocument8 pages8 StrokeAhmed aljumailiNo ratings yet
- Guidelines & Protocols: Stroke and Transient Ischemic Attack - Management and Prevention Advisory CommitteeDocument13 pagesGuidelines & Protocols: Stroke and Transient Ischemic Attack - Management and Prevention Advisory CommitteeAndi SaputraNo ratings yet
- Jamieson 2009Document7 pagesJamieson 2009JovitaNo ratings yet
- Neurologic EmergenciesDocument11 pagesNeurologic EmergenciesRoberto López MataNo ratings yet
- Askep StrokeDocument46 pagesAskep Strokesybilla17No ratings yet
- Ischemic StrokeDocument13 pagesIschemic StrokearthurbaidoodouglasNo ratings yet
- The Pathophysiology of Ischemic Strokes Is Widely Known. Ischemic Strokes Are TheDocument7 pagesThe Pathophysiology of Ischemic Strokes Is Widely Known. Ischemic Strokes Are Theprnczb13No ratings yet
- Rapid Focused Neurological Assessment in The Emergency Department and ICUDocument16 pagesRapid Focused Neurological Assessment in The Emergency Department and ICUAnnie RicoNo ratings yet
- AISDocument40 pagesAISMohamed AbdoNo ratings yet
- Seizure Versus SyncopeDocument10 pagesSeizure Versus SyncopeArmando Diaz PerezNo ratings yet
- Emergency Neurological Life Support - Subarachnoid HemorrhageDocument9 pagesEmergency Neurological Life Support - Subarachnoid HemorrhageIsabel VillalobosNo ratings yet
- 2014 CCM Review NotesDocument241 pages2014 CCM Review NotesAndres SimsNo ratings yet
- An Approach To The Evaluation of A Patient For Seizures and EpilepsyDocument8 pagesAn Approach To The Evaluation of A Patient For Seizures and EpilepsyGaneshRajaratenamNo ratings yet
- Clinical Presentation of Cerebrovascular Disease: David Griesemer, MDDocument47 pagesClinical Presentation of Cerebrovascular Disease: David Griesemer, MDPedro CedeñoNo ratings yet
- Hypertensive Emergencies in The Emergency DepartmentDocument13 pagesHypertensive Emergencies in The Emergency DepartmentLuis Lopez RevelesNo ratings yet
- Cec Post Fall Assess and Man June 2013Document3 pagesCec Post Fall Assess and Man June 2013Vicente TurasNo ratings yet
- Acute Stroke Management by Carlos L ChuaDocument61 pagesAcute Stroke Management by Carlos L ChuaRemaica Hernadez100% (1)
- TIA: Transient Ischemic Attack Key PointsDocument2 pagesTIA: Transient Ischemic Attack Key PointsAlmahira Az ZahraNo ratings yet
- Syncope 3Document19 pagesSyncope 3Pratyush PrateekNo ratings yet
- Cardiac Arrhythmia ThesisDocument5 pagesCardiac Arrhythmia Thesiselizabethallencambridge100% (2)
- 1228 HFStroke Altered Neuro 2011Document74 pages1228 HFStroke Altered Neuro 2011Cyndy EnterlineNo ratings yet
- In-Hospital Stroke Recurrence and Stroke After Transient Ischemic AttackDocument15 pagesIn-Hospital Stroke Recurrence and Stroke After Transient Ischemic AttackferrevNo ratings yet
- CVADocument4 pagesCVACloyd Marvin Pajas SegundoNo ratings yet
- Dent Clin N Am 50 (2006) 625-633Document9 pagesDent Clin N Am 50 (2006) 625-633lalajanNo ratings yet
- Case-Based Device Therapy for Heart FailureFrom EverandCase-Based Device Therapy for Heart FailureUlrika Birgersdotter-GreenNo ratings yet
- Patient Management Problem Preferred Responses.27Document12 pagesPatient Management Problem Preferred Responses.27mhd.mamdohNo ratings yet
- ABC Emergency Differential DiagnDocument3 pagesABC Emergency Differential Diagnsharu4291No ratings yet
- Hypertensive Encephalopathy: Presentation DDX Workup Treatment MedicationDocument8 pagesHypertensive Encephalopathy: Presentation DDX Workup Treatment MedicationMoh SuriyawalNo ratings yet
- Neurology 5Document5 pagesNeurology 5Loyla RoseNo ratings yet
- Emergency Medicine Survival Guide: Emergency Medicine Survival Guide for New DoctorsFrom EverandEmergency Medicine Survival Guide: Emergency Medicine Survival Guide for New DoctorsNo ratings yet
- The Code Stroke Handbook: Approach to the Acute Stroke PatientFrom EverandThe Code Stroke Handbook: Approach to the Acute Stroke PatientNo ratings yet
- Eur J of Neuroscience - 2021 - Gorman Sandler - The Forced Swim Test Giving Up On Behavioral Despair Commentary OnDocument4 pagesEur J of Neuroscience - 2021 - Gorman Sandler - The Forced Swim Test Giving Up On Behavioral Despair Commentary OnAndi SaputraNo ratings yet
- 10 1002@0471141755 ph0508s38Document11 pages10 1002@0471141755 ph0508s38Andi SaputraNo ratings yet
- Gastroesophageal Reflux Disease Questionnaire Gerd Q Score in Gerd Patients Treated With dlbs2411 Compared To Omeprazole 2skpDocument1 pageGastroesophageal Reflux Disease Questionnaire Gerd Q Score in Gerd Patients Treated With dlbs2411 Compared To Omeprazole 2skpAndi SaputraNo ratings yet
- The Forced Swim Test For Depression-Like Behavior in RodentsDocument6 pagesThe Forced Swim Test For Depression-Like Behavior in RodentsAndi SaputraNo ratings yet
- Animal Models As Tools To Study The PathophysiologDocument10 pagesAnimal Models As Tools To Study The PathophysiologAndi SaputraNo ratings yet
- Warden Nature 2012 SuppDocument22 pagesWarden Nature 2012 SuppAndi SaputraNo ratings yet
- Anticancer Activity of Phyllanthus Niruri Linn Extract in Colorectal Cancer Patients A Phase II Clinical TrialDocument5 pagesAnticancer Activity of Phyllanthus Niruri Linn Extract in Colorectal Cancer Patients A Phase II Clinical TrialAndi SaputraNo ratings yet
- Mitochondrial Dynamics in Cardiovascular Medicine: Gaetano Santulli EditorDocument644 pagesMitochondrial Dynamics in Cardiovascular Medicine: Gaetano Santulli EditorAndi SaputraNo ratings yet
- Efficacy and Safety of The mRNA-1273 SARS-CoV-2 VaccineDocument14 pagesEfficacy and Safety of The mRNA-1273 SARS-CoV-2 Vaccinejuan carlos monasterio saezNo ratings yet
- Anti-Collagen VII Antibody (LH7.2) Ab6312 Anti-Collagen VII Antibody (LH7.2) Ab6312Document3 pagesAnti-Collagen VII Antibody (LH7.2) Ab6312 Anti-Collagen VII Antibody (LH7.2) Ab6312Andi SaputraNo ratings yet
- Conductivity Standard MSDSDocument4 pagesConductivity Standard MSDSAndi SaputraNo ratings yet
- Pengantar Ilmu Biomedik Dan BiokimiaDocument27 pagesPengantar Ilmu Biomedik Dan BiokimiaAndi SaputraNo ratings yet
- Bahan Kuliah Id-1-2020Document63 pagesBahan Kuliah Id-1-2020Andi SaputraNo ratings yet
- Lampiran VIII - Daftar Riwayat Hidup PDFDocument1 pageLampiran VIII - Daftar Riwayat Hidup PDFAndi SaputraNo ratings yet
- Acute Stroke DiagnosisDocument8 pagesAcute Stroke Diagnosisvivek_win95No ratings yet
- General Aspects of Protein StructureDocument19 pagesGeneral Aspects of Protein StructureAndi SaputraNo ratings yet
- Medical Aspects 2014Document154 pagesMedical Aspects 2014Andi SaputraNo ratings yet
- Hazard Analysis Critical Control Point: Health Practices On Cruise Ships: Training For Employees TranscriptDocument7 pagesHazard Analysis Critical Control Point: Health Practices On Cruise Ships: Training For Employees TranscriptAndi SaputraNo ratings yet
- Acute Stroke DiagnosisDocument8 pagesAcute Stroke Diagnosisvivek_win95No ratings yet
- SCAT Systematic Cause Analysis Technique PDFDocument36 pagesSCAT Systematic Cause Analysis Technique PDFAndi Saputra100% (1)
- The Epilepsy Prescriber's Guide To Antiepileptic Drugs 2010Document333 pagesThe Epilepsy Prescriber's Guide To Antiepileptic Drugs 2010Andi SaputraNo ratings yet
- NICE Guidelines PDFDocument37 pagesNICE Guidelines PDFKahubbi Fatimah Wa'aliyNo ratings yet
- Guidelines & Protocols: Stroke and Transient Ischemic Attack - Management and Prevention Advisory CommitteeDocument13 pagesGuidelines & Protocols: Stroke and Transient Ischemic Attack - Management and Prevention Advisory CommitteeAndi SaputraNo ratings yet
- Ot Guidelines Stroke RehabDocument87 pagesOt Guidelines Stroke Rehab健康生活園Healthy Life GardenNo ratings yet
- Transient Ischemic Attacks: Part I. Diagnosis and EvaluationDocument10 pagesTransient Ischemic Attacks: Part I. Diagnosis and EvaluationAndi SaputraNo ratings yet
- Guidelines For Stroke 2010 KoreaDocument68 pagesGuidelines For Stroke 2010 KoreaNain EmberspiritNo ratings yet
- NICE Guidelines PDFDocument37 pagesNICE Guidelines PDFKahubbi Fatimah Wa'aliyNo ratings yet
- CPG Management of StrokeDocument51 pagesCPG Management of Strokeapalaginih0% (1)
- CPG Management of StrokeDocument51 pagesCPG Management of Strokeapalaginih0% (1)
- Acs Nstemi PathwayDocument3 pagesAcs Nstemi PathwayAliey's SKeplek NgeNersNo ratings yet
- ICU Liberation ABCDEF Bundle Implementation Both Spontaneous Awakening Breathing Trials SBT SATDocument63 pagesICU Liberation ABCDEF Bundle Implementation Both Spontaneous Awakening Breathing Trials SBT SATbejoNo ratings yet
- Laser Retinopexy PDFDocument4 pagesLaser Retinopexy PDFveerroxxNo ratings yet
- Vestibular Exercise For Patient - Guideline Vestibular ExerciseDocument4 pagesVestibular Exercise For Patient - Guideline Vestibular ExerciseResi Lystianto PutraNo ratings yet
- Body Mechanics and Patient CareDocument79 pagesBody Mechanics and Patient CareChristian DioNo ratings yet
- Stress Management PPT FinalDocument7 pagesStress Management PPT FinalAdarsh Meher100% (1)
- Pages From First Aid For The USMLE Step 1 2015, 25 Edition-2Document7 pagesPages From First Aid For The USMLE Step 1 2015, 25 Edition-2Mahmoud MohsenNo ratings yet
- Not GlaucomaDocument5 pagesNot GlaucomaFabio LuccheseNo ratings yet
- Essential Elements of Clinical TrialDocument39 pagesEssential Elements of Clinical TrialmisganaNo ratings yet
- Medical Claim Form - FLEX StaffDocument1 pageMedical Claim Form - FLEX StaffHerawaty Syaiful GusmentaNo ratings yet
- Resistance Training Utilization For Patients With Transverse MyelitisDocument10 pagesResistance Training Utilization For Patients With Transverse Myelitisapi-414772091No ratings yet
- 3 Intraoperative PhaseDocument28 pages3 Intraoperative Phaseada_beer100% (2)
- Trigeminal NeuralgiaDocument3 pagesTrigeminal NeuralgiaKiara PeoplesNo ratings yet
- Nutrisi EnteralDocument51 pagesNutrisi EnteralIsma Awalia Habibah14No ratings yet
- Medication, Toxic, and Vitamin-Related NeuropathiesDocument22 pagesMedication, Toxic, and Vitamin-Related Neuropathiessatyagraha84No ratings yet
- Ophthalmology PDFDocument28 pagesOphthalmology PDFKukuh Rizwido PrasetyoNo ratings yet
- Laboratory Medicine Quality IndicatorsDocument14 pagesLaboratory Medicine Quality IndicatorskinnusaraiNo ratings yet
- Surgical SafetyDocument23 pagesSurgical SafetyNimi BatuboNo ratings yet
- Reliability and Validity of The Turkish Version of The Job Performance Scale InstrumentDocument9 pagesReliability and Validity of The Turkish Version of The Job Performance Scale InstrumentsatmayaniNo ratings yet
- Guia Tiva 2018Document14 pagesGuia Tiva 2018John Bryan Herrera DelgadoNo ratings yet
- Tuberculosis (The Disease)Document24 pagesTuberculosis (The Disease)DiLahNo ratings yet
- VIDATOX ® 30 CH EnglishDocument17 pagesVIDATOX ® 30 CH EnglishmusicaNo ratings yet
- Chronic Myeloid Leukemia Presenting With Priapism 2329 6917 1000171Document5 pagesChronic Myeloid Leukemia Presenting With Priapism 2329 6917 1000171SalwiyadiNo ratings yet
- An Implantable Bioartificial Kidney For Treating Kidney FailureDocument2 pagesAn Implantable Bioartificial Kidney For Treating Kidney FailureAnugrah Pangeran100% (1)
- Tendon TransferDocument1 pageTendon TransferPandi Smart VjNo ratings yet
- Indian Ethos and Values in ManagementDocument23 pagesIndian Ethos and Values in ManagementDinesh Babu PugalenthiNo ratings yet
- Chapter 3 PsychDocument12 pagesChapter 3 Psychred_gyrl9282No ratings yet
- Merci Ships Annual Report Cpr-31Document32 pagesMerci Ships Annual Report Cpr-31larryfoleNo ratings yet
- Total Patient Care Nursing or Case Method NursingDocument3 pagesTotal Patient Care Nursing or Case Method Nursingkint manlangitNo ratings yet
- Pub104 WorkbookDocument16 pagesPub104 Workbooksyang9No ratings yet