Professional Documents
Culture Documents
Migraine Prophylaxis: Pharmacotherapy Perspectives
Uploaded by
jo_jo_maniaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Migraine Prophylaxis: Pharmacotherapy Perspectives
Uploaded by
jo_jo_maniaCopyright:
Available Formats
Berikut ini adalah versi HTML dari berkas http://www.pswi.org/professional/pharmaco/migraine.pdf.
G o o g l e membuat versi HTML dari dokumen tersebut secara otomatis pada saat menelusuri web.
Page 1
Pharmacotherapy Perspectives
20 Nov/Dec 2000 Journal of the Pharmacy Society of Wisconsin
Migraine Prophylaxis
Principles, goals and drug therapy
by Sarah E. Bland, RPh
Column Editor: Lee Vermeulen, MS, RPh,
Director, Center for Drug Policy, University of Wisconsin Hospital and Clinics
The information given and views expressed herein do not necessarily reflect the opinions of PSW, its Board or members.
Goals of treatment
According to the University of Wisconsin Hospital and
Clinics Migraine Treatment Guideline, the goals of treatment
are to reduce the frequency and severity of migraine attacks; a
secondary goal may include improving the responsiveness of
attacks to abortive therapy.7 A good response may be defined
as a 50% reduction in the frequency or severity of the attacks.
The lowest effective dose of medication should be used in
order to minimize side effects. Patients should not expect that
they will become completely free of migraines; rather, they
should expect that they will have less disability. Rescue
medications should still be available to the patient.
Non-pharmacologic measures
All prophylactic treatment plans should include some non-
pharmacologic treatment strategies intended to reduce the
patients exposure to triggers that may cause a migraine attack
to start. Common triggers are missed meals; too little sleep;
excessive heat and humidity; certain foods such as chocolate,
hard cheeses, alcoholic beverages, citrus fruits, nuts, excessive
caffeine, and caffeine withdrawal; medication such as oral
contraceptives, overuse of analgesics, sympathomimetic street
drugs; strong sensory stimuli such as bright lights, glare,
flickering lights, odors, smoke and prolonged exposure to heat
or cold. Patients should be encouraged to keep a headache diary
in an effort to identify triggers.
Introduction
Migraine headache is a chronic condition characterized by
repeated, debilitating attacks of severe, usually unilateral,
pulsatile headaches, often accompanied by nausea, vomiting,
photophobia and a variety of other symptoms. Classical mi-
graine is associated with prodromal symptoms referred to as
aura; common migraine usually lacks these prodromal symp-
toms. It is a disorder with a prevalence of 17.6% in American
females and 5.7% in American males.1 The prevalence of
migraine begins to increase starting at age 12, peaks at about
age 38, and declines thereafter. It is approximately twice as
common in boys as in girls at age 12, becomes 3.3 times as
common in women as men between the ages of 42-44 and
decreases to 2.5 times as common in women by age 70.2
Although there is a common misperception that migraine is
more common in those who have the time and money to seek
treatment, the American Migraine Study has provided docu-
mentation that its incidence actually decreases with higher
socioeconomic status.1
Among the respondents to the American Migraine Study,
25% of the women had four or more severe attacks monthly,
35% had three severe attacks monthly and 40% had one severe
attack per month or less.1 The male respondents reported a
similar frequency of attacks. Over 80% of respondents re-
ported at least some degree of disability with their headaches,
including severe disability or the need for bed rest in one-
fourth of cases. Despite the degree of disability reported, 57%
of males and 68% of females had never consulted a physician
for their headaches.4 Of those who consulted with physicians,
42% reported that they had not received a diagnosis of mi-
graine. Only 13.6% of female migraineurs and 10.4% of males
consulted with a neurologist about their headaches; fewer still,
1.6% of females and 4.7% males, consulted with a pain or
headache specialist.
While the degree of disability experienced by migraineurs
varies widely from patient to patient5, efforts have been made
to estimate the cost of the disability resulting from migraine.
A recently published study estimated that each year in the
United States, 112 million workdays are missed and $13
billion are lost to employers due to absenteeism and reduced
productivity.6 There are also losses experienced in the social
aspects of life that have no means of measurement.
The recent studies of migraine have shown that it is a
common problem, afflicting over 10 million Americans at a
high social and economic cost. At the same time, it appears to
be a medical problem for which patients often do not seek help,
and when they do, the diagnosis is often missed and referrals
to specialists are infrequent. This is unfortunate, because there
are many effective, well-tolerated methods available for the
prevention and treatment of migraine. This article will address
the principles and goals of migraine prophylaxis. The primary
reference for the recommendations made here is the UW
Hospital and Clinics Migraine Assessment and Treatment
Guideline.7
Page 2
Pharmacotherapy Perspectives
Journal of the Pharmacy Society of Wisconsin Nov/Dec 2000 21
Indications for pharmacologic prophylaxis
Any one of the following indications is sufficient to war-
rant a trial of prophylactic medications.7-9 Some published
guidelines may recommend a minimum threshold number of
attacks per month, but such thresholds are in fact arbitrary and
any patient who wishes to reduce the number or intensity of
attacks should be considered as a candidate for prophylactic
therapy.
1. Occurrence of 2-3 attacks/month OR recurring attacks
that patients feel are interfering with their daily ac-
tivities even with acute treatment
2. Attacks lasting 48 hours or more
3. Extreme headache severity or prolonged aura
4. Presence of uncommon migraine conditions such as
hemiplegic migraine, basilar migraine, or migrainous
infarction
5. Inadequate relief from or overuse of acute therapies
6. Contraindication to or intolerable adverse effects
from acute therapies
7. Intolerable cost of acute therapies
8. Patient demand
Guiding principles of drug therapy
There are a number of helpful principles that can be used to
maximize the likelihood of successful results in migraine
prophylaxis.7,8,10 Careful consideration of these principles can
be useful in selecting the appropriate drug with which to begin
a prophylactic trial. Additionally, it is important to explain the
principles relating to commitment, compliance, trial duration
and elimination of confounding medications to patients so they
are able to participate fully in the process. Their input is
essential to successful prophylaxis.
1. Recognize that a plan of prophylactic therapy requires a
major commitment on the part of the patient and the
physician.
2. Educate patients about the importance of compliance.
Once an effective dose is determined, use of a long-
acting, once-daily dosage form may encourage compli-
ance.
3. Give each medication an adequate trial of two to three
months before evaluating its efficacy.
4. Reduce or eliminate the use of medications that exacer-
bate migraine or interfere or interact with the prophylac-
tic drug.
5. Use the lowest effective dose. Start with a very low dose
of the selected medication and titrate upward until a
satisfactory benefit is obtained without side effects or
until the dosage is limited by side effects. The doses
required to effectively treat migraine are often lower
than the doses required to treat other conditions such as
epilepsy, hypertension or depression.
6. While many patients may require combinations of drugs
for effective prophylaxis, it is important to add the drugs
one at a time in order to keep track of their respective
efficacies and to sort out side effect profiles.
7. Consider comorbid conditions when choosing a prophy-
lactic agent. For example, in a patient with hypertension,
it may be possible to choose drugs like beta-blockers or
verapamil that will control hypertension and also reduce
migraine recurrence. Choice of a multifunctional agent
can decrease possible adverse effects, increase compli-
ance and improve cost-effectiveness of therapy. Avoid
medications that could compromise patient care, like
beta-blockers in patients with asthma.
8. Consider also the side effect profile of the prophylactic
drugs and whether some of the side effects might be
beneficial in some patients. For example, the drowsi-
ness caused by the tricyclic antidepressants might be a
beneficial side effect in a patient who is also suffering
from insomnia.
Migraine guidelines
The University of Wisconsin Hospital and Clinics has
developed a Migraine Prophylaxis Guideline (on next page)
based on drugs that have proven efficacy for this indication.7
The guideline is arranged by drug class, with drugs within that
class listed in the second column. Minimum and maximum
dosages are recommended, and contraindications and com-
ments for each drug are included in the third column. The
section immediately following the guideline outlines the clini-
cal evidence for efficacy of each agent listed in the guideline.
Clinical evidence for efficacy
Propranolol has been demonstrated in a number of clinical
trials to be significantly more effective than placebo in reduc-
ing the number of migraine attacks.11-14 In addition, it has been
reported as effective in case series.15,16 Typical doses range
from 80 mg/day up to 320 mg/day. Good results were obtained
with the long-acting formulation which is convenient for
patients, and the drug was well-tolerated by most patients.
Other beta-blockers have been studied for migraine pro-
phylaxis. Metoprolol, in doses of 100-200 mg/day, was signifi-
cantly better than placebo in reducing the number of attacks
and number of migraine days, although its effect on pain
severity scores and analgesic tablet consumption was signifi-
cant only at the higher dose.17,18 Metoprolol has been directly
compared to propranolol in double-blind, cross-over studies;
100-200 mg/day of metoprolol was found to be as effective as
80 mg/day of propranolol in reducing headache frequency,
Page 3
Pharmacotherapy Perspectives
22 Nov/Dec 2000 Journal of the Pharmacy Society of Wisconsin
migraine days, analgesic consumption and ergotamine con-
sumption.19,20 In the Olsson study, 100 mg metoprolol/day was
effective in reducing headache pain severity scores statisti-
cally significantly from baseline.
Atenolol was evaluated in a small trial of 24 patients in a
double-blind, cross-over, placebo-controlled study.21 Doses of
100 mg/day were significantly better than placebo in reducing
migraine frequency and in its effect on headache overall.
Eleven of 20 patients included in the final analysis had a 50%
reduction in headache severity and two patients had no head-
aches during the study period while on atenolol.
A fourth beta-blocker that has been studied for migraine
Beta Blockers
Propranolol 40-240 mg/day PO
Atenolol 50-150 mg/day PO
Metoprolol 100-200 mg/day PO
Nadolol 20-60 mg/day PO
Propranolol and nadolol are contraindicated in bronchial asthma or
COPD
All beta-blockers are contraindicated in overt cardiac failure, 2nd or 3rd
degree AV block or severe sinus bradycardia
Caution in CHF, diabetes mellitus, hyperthyroidism/thyrotoxicosis, pe-
ripheral vascular disease
Do not withdraw abruptly; taper over 1-2 weeks
UWHC Migraine Prophylaxis Recommendations
Drug Class
Drug/Dose
Contraindications/Comments
Calcium Channel
Blockers
Verapamil 240-320 mg/day PO
Diltiazem 90-360 mg/day PO
Nimodipine 120-360 mg/day PO
Diltiazem and verapamil are contraindicated with atrial fibrillation or
flutter, accessory bypass tracts, short PR syndromes, hypotension (<90
mm Hg systolic), 2nd or 3rd degree AV block without functioning artificial
pacemaker, sick sinus syndrome, wide-complex ventricular tachycardia
(QRS>0.12)
Verapamil is contraindicated in CHF, digital ischemia, ulceration or
gangrene, idiopathic hypertrophic cardiomyopathy, severe left ventricu-
lar dysfunction
Diltiazem and verapamil are contraindicated with impaired renal function
Avoid extended-release dosage forms of diltiazem and verapamil with GI
hypermotility or GI obstruction
Serotonin Receptor
Antagonists
Methysergide 2 mg every night,
gradually increased to TID (maximum
8 mg/day if needed); usual dose is 4-8
mg/day
Contraindicated in pregnancy, peripheral vascular or coronary artery
disease, lower limb phlebitis, pulmonary disease, collagen diseases or
fibrotic disease, impaired liver or renal function or valvular disease;
drug holidays of 3-4 weeks every 6 months are needed to prevent
serious drug toxicity
Anti-epileptics
Tricyclic
Antidepressants
Amitriptyline 10-150 mg every night
Nortriptyline 10-150 mg every night
(start with 10 mg and increase as
tolerated until adequate response or
intolerable side effects)
TCAs are contraindicated in the acute recovery phase following myo-
cardial infarction, and with concomitant use of monamine oxidase
inhibitors (MAOIs)
Use with caution in seizure disorders; history of urinary retention,
glaucoma or increased ocular pressure; hyperthyroidism; schizophre-
nia and cardiovascular disease
Nortriptyline should not be used concomitantly with reserpine
Divalproex 500-1500 mg/day
Valproic acid 500-1500 mg/day
Valproic acid and divalproex are contraindicated in pregnancy or with
liver disease
Use with caution with drugs that affect platelet function, or with concomi-
tant use of other CNS depressants
prophylaxis is nadolol. In a study of 80 patients taking 0, 80,
160 or 240 mg/day, patients taking 160 or 240 mg/day had a
reduction in the frequency and severity of their migraines.22
Nadolol 80 and 160 mg/day have also been compared to
propranolol 160 mg/day in migraine prophylaxis.23,24 In the
Sudilovsky study, the higher dose of nadolol produced supe-
rior results to propranolol in headache frequency, intensity,
pain days and use of relief medications by the end of the first
month of treatment. In the Ryan study, the lower dose of
nadolol produced the greatest improvements but the difference
between the groups was not statistically significant.
Verapamil is a calcium channel blocker that has been used
Page 4
Pharmacotherapy Perspectives
Journal of the Pharmacy Society of Wisconsin Nov/Dec 2000 23
prophylactically for migraine, although there has been little
clinical study of it. A review of three double-blind clinical
trials indicates that verapamil, in doses of 240-320 mg/day, is
significantly more effective than placebo in preventing mi-
graine, with the 320 mg dose being more effective than the 240
mg dose.25 Forty-five percent of the 133 patients in the trials
reported greater than 50% improvement in migraine frequency.
Diltiazem has also been used successfully in migraine prophy-
laxis, although it, too, has been little studied.26
Nimodipine has been found to be superior to placebo in
migraine prevention in a double-blind, cross-over trial of 33
patients.27 Statistically significant improvements were attained
in headache frequency, duration and headache index (pain
severity X migraine days/28 days). Studies comparing
nimodipine to flunarizine and pizotifen as well as placebo
found nimodipine to be superior to placebo and equivalent in
efficacy to the comparator drugs.28,29 Two other studies have
shown a strong placebo response in addition to a good response
to nimodipine; a superior benefit from nimodipine could not be
established in these studies.30,31 The usual dose of nimodipine
administered in the studies was 40 mg three times daily.
A fourth calcium channel blocker, nifedipine, was com-
pared to propranolol for migraine prophylaxis.32 In this small,
open-label study, nifedipine was less effective than propra-
nolol and had a much higher incidence of side effects; 45% of
the 20 patients on nifedipine withdrew from the study within
two weeks. A second study found no difference between
nifedipine and placebo in the frequency of headaches, although
side effects were frequent among nifedipine users.33 Based on
the lack of significant benefit and the frequency of side effects,
nifedipine is generally not used for migraine prophylaxis.
Methysergide is a serotonin receptor antagonist that has
been used for migraine prophylaxis for many years. It has
unique and serious toxicities, however, that limit its use to the
most severe and refractory cases and require drug holidays of
3-4 weeks every six months. Its efficacy has been demon-
strated in several clinical trials.34-37 In the Pedersen trial, 60 of
102 patients completed the trial; 57% had a 50% response to
methysergide and methysergide was superior to placebo.34 In
the Whewell trial, 50 of 74 patients completed the trial.
Patients achieved a small decrease in the number of attacks, a
small decline in the duration of attacks and a larger decrease in
the duration of severe headaches.35 Use of methysergide re-
sulted in a statistically significant decline in the number of
attacks per week and in headache index in the Forssman trial;
decreases in duration and intensity were not statistically sig-
nificant.36 In the Lance trial, methysergide produced the best
results among six different serotonin antagonists including
cyproheptadine and methdilazine; 64% of patients on
methysergide had a 50% or greater improvement in their
headaches.37
Amitriptyline has been used widely and effectively for
migraine prophylaxis, although there are not many clinical
trials available. A placebo-controlled trial in 100 patients
found that amitriptyline in doses of up to 100 mg/day was more
effective than placebo in preventing migraine.38 Over 55% of
patients receiving amitriptyline had a 50% improvement in
their headaches, compared to 34% of patients taking placebo.
Amitriptyline was most effective in non-depressed patients
with severe migraine and depressed patients with less severe
migraine; depressed patients with severe migraine did not
respond as well. A second trial compared amitriptyline in
doses of 50 to 150 mg/day to propranolol 80 to 240 mg/day.39
Both drugs were superior to placebo and there was no differ-
ence in efficacy between them. Amitriptyline has been com-
pared to fluvoxamine for migraine prophylaxis in a study of 70
patients.40 Both drugs reduced the headache index to a statis-
tically significant degree. Drowsiness was more common
among patients receiving amitriptyline; a larger number of
patients taking amitriptyline dropped out of the study (9
compared with 2 for fluvoxamine). Nortriptyline is sometimes
used as an alternative to amitriptyline. It is often better toler-
ated than amitriptyline and it appears to be effective, but
clinical trials demonstrating its efficacy are lacking.
Divalproex sodium was evaluated for migraine prophy-
laxis in a placebo-controlled, dose-ranging study.41 Patients
received either placebo, divalproex 500 mg/day, 1000 mg/day
or 1500 mg/day. The three treatment groups had statistically
significant improvements in headache frequency and severity,
although there was no significant difference among the doses
in degree of improvement. A second trial compared divalproex
sodium to placebo in 107 patients.42 Headache frequency and
severity were significantly decreased while patients were
taking divalproex. Side effects, mainly nausea and drowsiness,
were generally mild to moderate. There was no significant
difference between the treatment and placebo groups in the
number of patients withdrawing due to intolerance. A review
of studies of sodium valproate and divalproex sodium for
migraine and chronic daily headache found that patients im-
proved on these drugs in 10 of 11 studies.43 Doses from 500 to
2000 mg/day were evaluated and were well-tolerated.
Divalproex has become one of the mainstays in the treatment
of migraine, although its use is associated with the undesirable
side effect of weight gain. Patients should be counseled about
this effect and monitored for weight gain during treatment.
Emerging treatments
There are a number of drugs that are currently being used
for migraine prophylaxis that have scant published evidence
for efficacy or only anecdotal evidence. For most of these
drugs, there is not yet enough experience with them to offer
firm recommendations for dosing. However, their use may
prove beneficial in refractory patients and are mentioned here
Page 5
Pharmacotherapy Perspectives
24 Nov/Dec 2000 Journal of the Pharmacy Society of Wisconsin
for informational purposes.
Fluoxetine and its s-enantiomer, s-fluoxetine, have been
studied for migraine prophylaxis with mixed results.44-46 A
double-blind, placebo-controlled trial in 32 patients evaluated
fluoxetine over an 8-week period.44 Headache scores in the
active group decreased significantly beginning in the third and
fourth weeks of treatment; no change was observed in the
placebo group. No changes in depression scores were observed
in either group. A second trial evaluated fluoxetine vs. placebo
in 122 patients with migraine or chronic daily headache.45
Fluoxetine was not significantly effective for migraine in this
study but was moderately effective in reducing chronic daily
headache. S-fluoxetine was evaluated in a placebo-controlled
trial in 53 patients.46 The active treatment resulted in a statis-
tically significant decrease in the number of attacks, although
the decreases in secondary efficacy measures, such as mi-
graine days, attack severity and medication use, did not reach
statistical significance.
Lamotrigine is a newer anticonvulsant that has been ex-
plored for migraine prophylaxis. A study in 15 patients found
that lamotrigine reduced the frequency and duration of aura
symptoms to a statistically significant degree, but this study
did not measure the effect on headaches.47 A second study
evaluated lamotrigine for prevention of migraine with aura in
18 patients.48 Doses of 100 mg/day decreased the number of
attacks per month significantly. This study also treated five
patients who had migraine without aura; they had no reduction
in the number of attacks while on lamotrigine. A third study of
lamotrigine in patients with migraine with and without aura
showed a tendency toward reductions in migraine days and
severity scores for the active treatment group, but no statisti-
cally significant benefits were shown.49
A recent case series on the use of gabapentin in centrally
and peripherally mediated pain, migraine and tremor reported
on 14 patients with migraine and cluster headache who were
treated with gabapentin in doses of 900-2700 mg/day. Ten of
the 14 patients reported moderate to excellent reduction in
headache frequency, duration and severity.50
Other agents currently in use or under investigation for
migraine prevention are riboflavin51, magnesium52,
montelukast53 and sumatriptan (taken intermittently for men-
strual migraine).54 The anticonvulsant topiramate has been
used successfully in refractory patients, although there is very
little published data available. Anecdotal reports have indi-
cated excellent response rates with very little toxicity.
Summary
While there are many apparently effective options avail-
able for the preventive treatment of migraine headache, there
is good supporting data for some and relatively little clinical
data supporting the use of others among these agents. Never-
theless, having a wide variety of drug classes to choose from
affords more opportunities to find a drug that will be effective
and well-tolerated in a given patient. It is unfortunate that so
many migraine sufferers are not receiving adequate medical
management of their condition, because substantial relief is
available with prophylactic treatment. Many of the treatments
are very affordable some costing less per month than a
single dose of the migraine abortive agent sumatriptan. Pa-
tients who are frequent users of abortive medications should be
encouraged to ask their physicians about prophylactic treat-
ment, and if they are not seeing a physician with expertise in
this area, they should be encouraged to seek a referral to one.
The potential gains for patients in reduction of migraine
frequency, pain severity and disability are tremendous.
References available on request. n
Costs: Estimated Average Wholesale Prices
for a One-Month Supply
DRUG
DOSE RANGE
AWP/MONTH
Amitriptyline
10-150 mg/day
$2.72-14.64
Propranolol
40-240 mg/day
$3.90-44.55
Nortriptyline
10-150 mg/day
$10.26-35.55
Metoprolol
100-200 mg/day
$18.63-37.27
Atenolol
50-150 mg/day
$21.60-64.80
Nadolol
20-60 mg/day
$25.64-76.94
Valproic acid
500-1500 mg/day
$49.04-147.15
Diltiazem
90-360 mg/day
$35.27-64.20
Verapamil
240-360 mg/day
$36.30-66.60
Divalproex sodium
500-1500 mg/day
$49.04-147.15
Lamotrigine
100 mg/day
$65.60
Methysergide
2-8 mg/day
$69.59-278.35
Fluoxetine
20-40 mg
$81.30-162.60
Gabapentin
900-2700 mg/day
$104.40-313.20
Topiramate
200 mg/day
$177.19
Nimodipine
120-360 mg/day
$803.00-2411.00
www.your.ehealthcenter.com
independent pharmanex medical rep
Nathalie Knowles-Beck
414-961-9162
male, female, family preventative health care
You might also like
- Anti-Aging Therapeutics Volume XIIIFrom EverandAnti-Aging Therapeutics Volume XIIINo ratings yet
- Migraine Prophylaxis: Principles, Goals and Drug TherapyDocument5 pagesMigraine Prophylaxis: Principles, Goals and Drug TherapyAndrew MaragosNo ratings yet
- Schizophrenia Treatment & Management - Approach Considerations, Antipsychotic Pharmacotherapy, Other PharmacotherapyDocument13 pagesSchizophrenia Treatment & Management - Approach Considerations, Antipsychotic Pharmacotherapy, Other PharmacotherapydilaNo ratings yet
- Module 3 Discussion NUR520Document5 pagesModule 3 Discussion NUR52078xh8x8b69No ratings yet
- 2019 Aplicaciones AmericanaDocument18 pages2019 Aplicaciones AmericanaJUAN MANUEL CERON ALVARADONo ratings yet
- The Treatment of Migraine Headaches in Children and AdolescentsDocument11 pagesThe Treatment of Migraine Headaches in Children and Adolescentsdo leeNo ratings yet
- Schizophrenia Treatment & ManagementDocument16 pagesSchizophrenia Treatment & ManagementDimas Januar100% (2)
- Kung Doris Chronic MigraineDocument19 pagesKung Doris Chronic MigraineAnonymous tG35SYROzENo ratings yet
- New Topics in phaRMcology (97-2003)Document18 pagesNew Topics in phaRMcology (97-2003)api-3761895No ratings yet
- Adult Migraine - Choosing Between TherapiesDocument40 pagesAdult Migraine - Choosing Between TherapiesMohan PrasadNo ratings yet
- Medication Overuse Headache - Treatment and Prognosis - UpToDateDocument16 pagesMedication Overuse Headache - Treatment and Prognosis - UpToDateMarcela Garzon O VelezNo ratings yet
- Anti Psychotic MedicationsDocument6 pagesAnti Psychotic MedicationsCandace AngelNo ratings yet
- BPJ64 PolypharmacyDocument11 pagesBPJ64 PolypharmacyLimYouhokNo ratings yet
- Trend Watch: Treatment of Migraine and The Role of Psychiatric MedicationsDocument3 pagesTrend Watch: Treatment of Migraine and The Role of Psychiatric MedicationsCharbel Rodrigo Gonzalez SosaNo ratings yet
- Preventive Treatment of Migraine in AdultsDocument16 pagesPreventive Treatment of Migraine in AdultsRenato Vilas Boas FilhoNo ratings yet
- An Introduction To PrescribingDocument12 pagesAn Introduction To PrescribingNelly AlvaradoNo ratings yet
- AFP MigrañaDocument9 pagesAFP MigrañaJuaan AvilaNo ratings yet
- Research Paper On PolypharmacyDocument5 pagesResearch Paper On Polypharmacyefj02jba100% (1)
- Treatment of Mood DisordersDocument27 pagesTreatment of Mood DisordersCamelutza IsaiNo ratings yet
- gl0087 PDFDocument58 pagesgl0087 PDFNurul HikmahNo ratings yet
- Practice GuidelineDocument3 pagesPractice Guidelineclarajimena25No ratings yet
- NICE Guidelines For The Management of DepressionDocument2 pagesNICE Guidelines For The Management of DepressionstefenandreanNo ratings yet
- Maintenan Bipolar With FarmakoEvid Based Mental Health-2014-Malhi-eb-2014-101948Document7 pagesMaintenan Bipolar With FarmakoEvid Based Mental Health-2014-Malhi-eb-2014-101948amro7190No ratings yet
- Migraine PreventionDocument31 pagesMigraine PreventionMohan PrasadNo ratings yet
- Hospital NursingDocument3 pagesHospital NursingrandolphmanalaNo ratings yet
- Pharmacotherapy Considerations in Palliative Care: Learning ObjectivesDocument19 pagesPharmacotherapy Considerations in Palliative Care: Learning ObjectivesMajed Mubarak Shannan AlzahraniNo ratings yet
- Depresion en GeriatricosDocument6 pagesDepresion en GeriatricosmmsNo ratings yet
- 10 TH Conf Poly PharmacyDocument5 pages10 TH Conf Poly Pharmacytr14niNo ratings yet
- Pi Is 0025712514000893Document32 pagesPi Is 0025712514000893Christoph HockNo ratings yet
- Are There Guidelines For The Responsible Prescription of Benzodiazepines?Document7 pagesAre There Guidelines For The Responsible Prescription of Benzodiazepines?Rian YupitaNo ratings yet
- PN0612 SF MigraineGuidelinesDocument3 pagesPN0612 SF MigraineGuidelinesAlejandra CastilloNo ratings yet
- Group F (Pabellon-Sacramento) - Final ManuscriptDocument35 pagesGroup F (Pabellon-Sacramento) - Final ManuscriptImmah Marie PinedaNo ratings yet
- IkhsanDocument14 pagesIkhsanSilvia Icha RiskiNo ratings yet
- Case Management GuideDocument212 pagesCase Management Guidesheath516100% (2)
- Bpac Polypharmacy Poem 2006 PFDocument20 pagesBpac Polypharmacy Poem 2006 PFJacob Alexander MarpaungNo ratings yet
- Prophylaxis of Migraine Headache: The CaseDocument8 pagesProphylaxis of Migraine Headache: The CaseRo KohnNo ratings yet
- PICOTDocument8 pagesPICOTRaphael Seke OkokoNo ratings yet
- PolypharmacyDocument4 pagesPolypharmacyJeffrey Tan100% (1)
- TP - Tratamiento 2Document17 pagesTP - Tratamiento 2Ilse JuradoNo ratings yet
- Epi Drugs EficaciesDocument18 pagesEpi Drugs EficaciesaandreiiNo ratings yet
- Aripiprazole AugmentationDocument12 pagesAripiprazole AugmentationmissayayayaNo ratings yet
- Geriatric Patient PDFDocument57 pagesGeriatric Patient PDFHasan Al MasudNo ratings yet
- Medication Use in Older Adults by Rose Knapp, MSN, RN, APRN-BC, ANPDocument34 pagesMedication Use in Older Adults by Rose Knapp, MSN, RN, APRN-BC, ANPJose Antonio Tous OlagortaNo ratings yet
- Rational Prescribing & Prescription Writing: IntroductionDocument3 pagesRational Prescribing & Prescription Writing: IntroductionAnmol KudalNo ratings yet
- Practice Parameter: Evidence-Based Guidelines For Migraine Headache (An Evidence-Based Review)Document10 pagesPractice Parameter: Evidence-Based Guidelines For Migraine Headache (An Evidence-Based Review)Arifya Anggoro KasihNo ratings yet
- ManiaDocument2 pagesManiajopet8180No ratings yet
- Clinical Pharmacology (Clark's Clinical Medicine 9th Ed (2017) - 2)Document38 pagesClinical Pharmacology (Clark's Clinical Medicine 9th Ed (2017) - 2)Rosulescu IonNo ratings yet
- Guideline Summary NGC-6824: FDA Warning/Regulatory AlertDocument8 pagesGuideline Summary NGC-6824: FDA Warning/Regulatory AlertÜnal ZağliNo ratings yet
- Discontinuing Antidepressant Medications in AdultsDocument16 pagesDiscontinuing Antidepressant Medications in AdultsOm AracoNo ratings yet
- Artikel 1Document6 pagesArtikel 1dyah novitaningrumNo ratings yet
- T H e C U R B S I D e C o N S U L TDocument7 pagesT H e C U R B S I D e C o N S U L TwaftmoversNo ratings yet
- Non-Pharmacological Treatments For Depression in Primary Care - An OverviewDocument8 pagesNon-Pharmacological Treatments For Depression in Primary Care - An OverviewknowlardNo ratings yet
- The STAR D Study: Treating Depression in The Real World: Interpreting Key TrialsDocument10 pagesThe STAR D Study: Treating Depression in The Real World: Interpreting Key Trials★彡ᏦᏖ彡★No ratings yet
- Anesthesia Books 2019 Bonica's-2001-3000Document1,000 pagesAnesthesia Books 2019 Bonica's-2001-3000rosangelaNo ratings yet
- Best Practice Stopping AntibioticsDocument4 pagesBest Practice Stopping AntibioticsJanine ClaudeNo ratings yet
- Anesthesia Books 2019 Bonica's-2001-3000Document845 pagesAnesthesia Books 2019 Bonica's-2001-3000rosangelaNo ratings yet
- Nejme 2301045Document2 pagesNejme 2301045Billy LamNo ratings yet
- Depresion en El Anciano en APS NejmDocument3 pagesDepresion en El Anciano en APS NejmOscar Alejandro Cardenas QuinteroNo ratings yet
- Clinic 6Document16 pagesClinic 6Renju KuriakoseNo ratings yet
- Wjem 13 01 26 PDFDocument9 pagesWjem 13 01 26 PDFMoises Vega RodriguezNo ratings yet
- Efficacy and Safety of Tigecycline - A Systematic Review and Meta-AnalysisDocument8 pagesEfficacy and Safety of Tigecycline - A Systematic Review and Meta-Analysisjo_jo_maniaNo ratings yet
- Donor DarahDocument1 pageDonor Darahjo_jo_maniaNo ratings yet
- Dystocia SOGCDocument16 pagesDystocia SOGCAdhitia NugrahantoNo ratings yet
- Case Report: Pulmonary Sequestration: A Case Report and Literature ReviewDocument4 pagesCase Report: Pulmonary Sequestration: A Case Report and Literature Reviewjo_jo_maniaNo ratings yet
- Donordarah PDFDocument1 pageDonordarah PDFjo_jo_maniaNo ratings yet
- 111992518Document6 pages111992518jo_jo_maniaNo ratings yet
- Canadian Contraception ConsensusDocument14 pagesCanadian Contraception Consensusjo_jo_maniaNo ratings yet
- AnyelirDocument2 pagesAnyelirjo_jo_maniaNo ratings yet
- Chlamydial Infection Can Cause Disease in Many Organ SystemsDocument22 pagesChlamydial Infection Can Cause Disease in Many Organ Systemsjo_jo_maniaNo ratings yet
- Case Studies Module 1 - A Case of PcosDocument9 pagesCase Studies Module 1 - A Case of PcosBobNo ratings yet
- ContentServer 37.ASPaaaaaDocument6 pagesContentServer 37.ASPaaaaaAchmad Deza FaristaNo ratings yet
- HiResOligonucleoutide ACGH Analysis Under24Hrs AppNote5991-0643ENDocument8 pagesHiResOligonucleoutide ACGH Analysis Under24Hrs AppNote5991-0643ENjo_jo_maniaNo ratings yet
- Bioethic MetaphysicDocument6 pagesBioethic Metaphysicjo_jo_maniaNo ratings yet
- Induction of Labour Versus Expectant Monitoring ForDocument11 pagesInduction of Labour Versus Expectant Monitoring Forjo_jo_maniaNo ratings yet
- Cancer RiskDocument1 pageCancer Riskjo_jo_maniaNo ratings yet
- IBT Q4 03 ReadingonlyDocument1 pageIBT Q4 03 Readingonlyjo_jo_maniaNo ratings yet
- TOEFL Speaking - Question 1&2 TopicsDocument8 pagesTOEFL Speaking - Question 1&2 TopicsSiddharthaSidNo ratings yet
- Yg Belum Masuk IpadDocument1 pageYg Belum Masuk Ipadjo_jo_maniaNo ratings yet
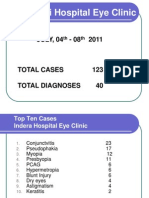
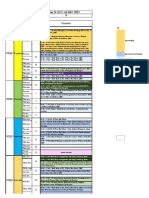
- NEW Weekly Indra 04-08 July 2011Document13 pagesNEW Weekly Indra 04-08 July 2011jo_jo_maniaNo ratings yet
- Structure Content: 1. EXERCISE 1 (Skill 1-2) 2. Toefl Review Exercise (Skill 1-2) 3. Answer KeysDocument3 pagesStructure Content: 1. EXERCISE 1 (Skill 1-2) 2. Toefl Review Exercise (Skill 1-2) 3. Answer Keysjo_jo_mania0% (1)
- BARUPoliklinik Wangaya 4-8 Juli 2011Document14 pagesBARUPoliklinik Wangaya 4-8 Juli 2011jo_jo_maniaNo ratings yet
- Sunday, 26/09 /2010 PT/LN/MG:: Consultant DR Mas Putra SPMDocument6 pagesSunday, 26/09 /2010 PT/LN/MG:: Consultant DR Mas Putra SPMjo_jo_maniaNo ratings yet
- Prediction Reccurence Prostat CADocument9 pagesPrediction Reccurence Prostat CAjo_jo_maniaNo ratings yet
- International Centre For Eye Health Teaching Set 2 The Eye in Primary Health CareDocument25 pagesInternational Centre For Eye Health Teaching Set 2 The Eye in Primary Health Carejo_jo_maniaNo ratings yet
- OrtoDocument61 pagesOrtojo_jo_maniaNo ratings yet
- Laser Iridotomy and GlaucomaDocument2 pagesLaser Iridotomy and Glaucomajo_jo_maniaNo ratings yet
- Arterial Blood Gas: DR - Made Widia, Sp.A (K)Document19 pagesArterial Blood Gas: DR - Made Widia, Sp.A (K)jo_jo_mania100% (1)
- Beyond Wedge: Clinical Physiology and The Swan-Ganz CatheterDocument12 pagesBeyond Wedge: Clinical Physiology and The Swan-Ganz Catheterkromatin9462No ratings yet
- Cataract Case PresentationDocument7 pagesCataract Case PresentationShahbaz AAnsariNo ratings yet
- Best Milking Practices Checklis PDFDocument3 pagesBest Milking Practices Checklis PDFcan_orduNo ratings yet
- Egurukul OrbitDocument8 pagesEgurukul OrbitbetsyNo ratings yet
- Ptisis BulbiDocument6 pagesPtisis Bulbiruditacitrahaha100% (1)
- Main Conference ProgrammeDocument7 pagesMain Conference ProgrammeFaadhilah HussainNo ratings yet
- KN 4@enzl 8 Ha 4 B 6 CC 9 eDocument26 pagesKN 4@enzl 8 Ha 4 B 6 CC 9 eRamzen Raphael DomingoNo ratings yet
- Bipolar Handout 2Document12 pagesBipolar Handout 2hugoi_7No ratings yet
- Congenital Ichthyosis - Collodion Baby Case Report: KeywordsDocument2 pagesCongenital Ichthyosis - Collodion Baby Case Report: KeywordsLidia MdNo ratings yet
- Elite Package Marketing PlanDocument30 pagesElite Package Marketing PlanNiña DyanNo ratings yet
- Safety Seal Certification ChecklistDocument2 pagesSafety Seal Certification ChecklistKathlynn Joy de GuiaNo ratings yet
- Scenar Testimonials (Updated)Document10 pagesScenar Testimonials (Updated)Tom Askew100% (1)
- Screenshot 2022-10-21 at 19.56.24Document3 pagesScreenshot 2022-10-21 at 19.56.24Zafira AkramNo ratings yet
- 2015catalog PDFDocument52 pages2015catalog PDFNegoi Mihai0% (1)
- Cerebral Palsy Brain Paralysis: Complications of Neurodevelopmental DisordersDocument11 pagesCerebral Palsy Brain Paralysis: Complications of Neurodevelopmental DisordersmikayNo ratings yet
- TetanusDocument7 pagesTetanusallah akbarNo ratings yet
- The Well-Being of The EMT: Emergency Medical Technician - BasicDocument30 pagesThe Well-Being of The EMT: Emergency Medical Technician - Basicalsyahrin putraNo ratings yet
- Tugas B.inggrisDocument7 pagesTugas B.inggrisIis setianiNo ratings yet
- Dialog Percakapan Bidan Tugas Bahs Inggris DedeDocument5 pagesDialog Percakapan Bidan Tugas Bahs Inggris DedeSardianto TurnipNo ratings yet
- Spinal InjuryDocument24 pagesSpinal InjuryFuad Ahmad ArdiansyahNo ratings yet
- Experiment #15: Screening Test For Low Titer Group "O" BloodDocument5 pagesExperiment #15: Screening Test For Low Titer Group "O" BloodKriziaNo ratings yet
- Mean Alt Üst SD Range Mean Alt Üst SD Range Mean Alt Üst SD Mean Alt Üst SD FaktörDocument5 pagesMean Alt Üst SD Range Mean Alt Üst SD Range Mean Alt Üst SD Mean Alt Üst SD FaktörZeynep DenizNo ratings yet
- TCM Protocol For ClassicalDocument26 pagesTCM Protocol For ClassicalDrnarendra KumarNo ratings yet
- HTP Visual1Document3 pagesHTP Visual1Queeniecel AlarconNo ratings yet
- Tipos de SuturasDocument5 pagesTipos de SuturasLeandro PeraltaNo ratings yet
- Phase II CurriculumDocument136 pagesPhase II CurriculumNil NilNo ratings yet
- Asbestos Awareness Quiz #1: AnswersDocument2 pagesAsbestos Awareness Quiz #1: AnswersMichael NcubeNo ratings yet
- Prumychild EngDocument12 pagesPrumychild EngAmirol Ariff NazarudinNo ratings yet
- Cyclamen: Chilly PulsatillaDocument10 pagesCyclamen: Chilly Pulsatillaअनुरूपम स्वामीNo ratings yet
- Pe Lesson 1 LifestyleDocument17 pagesPe Lesson 1 LifestyleKeil San PedroNo ratings yet