Professional Documents
Culture Documents
Synthesis of Acetycholine
Uploaded by
Marie Frances Lalican-RingelCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Synthesis of Acetycholine
Uploaded by
Marie Frances Lalican-RingelCopyright:
Available Formats
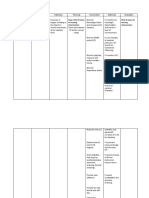
SYNTHESIS OF ACETYLCHOLINE
One-step process:
o AcCoA + Choline produce ACh.
Choline transported into nerve
endings
Acetyl CoA synthesized in the
mitochondria
Ach is transported inside a vesicle via an active pump or
second carrier vesicle-associated transporter (VAT)
o Inhibited by vesamicol
o Peptides (P), adenosine triphosphate (ATP),
and proteoglycan are also stored in the vesicle.
o Vesicles:
Clear vesicles contain more of Ach
(found towards the synaptic
membrane).
Densecored vesicles contain more of
NANC transmitters (located farther
from the synaptic membrane).
o Each vesicle contains 1,000 50,000
molecules of Ach.
Ca2+ stimulates release when levels are increased,
which causes fusion of vesicles with the surface
membrane and exocytotic expulsion of acetylcholine and
cotransmitters into the junctional cleft.
o Can be blocked by botulinum toxin
recordingThe membrane of vesicle joins with the
membrane of the neuron leading to the release of
substances inside the vesicle.
The production, release, and degradation of the
substances are all very rapid
Released ACh are taken up by their respective
cholinoreceptors
Cholinoreceptors produce respective response
Previous transAction of Ach is terminated by:
o Enzymatic degradation by acetylcholinesterase
(AChE) Recording
RecordingAcetylcholinesterase (True/
Specific Cholinesterase) degrade
ACh and its analogs
Butyrylcholinesterase (Plasma/
Nonspecific Cholinesterase) -
degrade all types of esters
Choline is recycled. Previous trans
There are no therapeutic preparations
of Ach as degradation occurs almost
immediately hydrolysis occurs within
a fraction of a second (this is due to
the abundance of AChE in cholinergic
synapses).
AChE can also be found in other
tissues like RBCs.
o Diffusion from the receptor
SYNTHESIS OF NOREPINEPHRINE
Three-step process:
o Conversion of TYOSINE to DOPA
Enzyme: Tyrosine Hydroxylase
Ratelimiting step in catecholamine
synthesis
Inhibited by the drug METYROSINE
(not really given now; previously used
in the Tx of pheochromocytoma)
Tyrosine is transported into the
noradrenergic ending by a
sodiumdependent carrier.
o Conversion of DOPA to DOPAMINE
Enzyme: Dopa decarboxylase
Dopamine is taken up by VMAT
o Synthesis of norepinephrine (NE)
Occurs within the vesicle
Enzyme dopaminehydroxylase
Fusion of vesicles with the synaptic membrane resuls in
the expulsion of NE, cotransmitters, and dopamine-
hydroxylase through exocytosis.
Norepinephrine transporter (NET) carries NE and
similar molecules back into the cell cytoplasm from the
synaptic cleft
o A.k.a. uptake 1 or reuptake 1
o Partially responsible for the termination of
synaptic activity
o Cytoplasmic pool of NE not readily degraded
by MAO (in cytoplasm); in a protective state
o Vesicular pool of NE NE is not degraded and
is instead
o transported into the vesicle
o Inhibited by cocaine and tricyclic antidepressant
(TCA) drugs, resulting in an increase of
transmitter activity in the synaptic cleft
Termination of NE action:
o Neuronal uptake NE is taken back into the
cytoplasm
o Extra-neuronal uptake - degraded by enzymes
like monoamine oxidase (mitochondria) and
catecholOmethyltransferase (liver and other
tissues)
o Diffusion from receptor site
Exam! Presynaptic receptors at the sympathetic nerve
terminal
o Autoreceptor (same) presynaptic alpha-2
receptors
Produce a negative feedback
mechanism
o Heteroreceptor muscarinic receptors
Cocaine, tricyclic, and antidepressants (TCAs)
o inhibit neuronal uptake leading to more
norepinephrine that continuously activate the
receptors
o increase in sympathetic activity
PHYSIOLOGY OF THE AUTONOMIC NERVOUS SYSTEM
The ANS controls smooth muscle
Visceral & vascular
Exocrine (and some endocrine) secretion are increased
o Increased lacrimation, sweating, gastric
secretion
Rate and force of contraction affected by both PNS and
SNS
Certain metabolic processes (e.g. glucose utilization, fat
metabolism)
Innervations
o Single
Pilo erector muscles
Most of the blood vessels are also
subserved by SNS Dual
o Dual
Heart, bronchioles, bladder (also GIT
and ciliary muscle of iris)
Antagonism
o Effects of SNS and PNS are antagonistic
o In those organs that are dually innervated
especially if they are antagonistic to one
another, there is one division that becomes
more dominant.
o Examples:
Heart rate accelerated by SNS and
diminished by PNS
GIT
PNS increase tone or
motility
SNS decrease motility;
relaxation of GIT smooth
muscle
Gut
PNS walls contract; trigone
and sphincter relax
SNS sphincter contraction
Exception salivary glands stimulation
by both PNS and SNS will result in
increase salivation.
Coordination
o When a number of organs are involved to affect
a physiological function in a coordinated way,
the two divisions are called to act in a
coordinated or orchestrated manner.
o Examples:
Vomiting
Male reproductive system
PNS - erection
SNS - ejaculation
Domination
o In an organ that receives dual innervations from
the two opposing divisions, one of them usually
plays a dominant role in controlling the function.
o PNS is generally more dominant because it is
responsible for homeostasis, except in
vasomotor tone (SNS dominant).
o Antagonism of the dominant division produces
effects very similar to stimulation of the other
more submissive division.
Examples:
o PNS dominant in eyes pupillary constriction
(miosis); if PNS is blocked pupillary dilation
(mydriasis), a SNS effect
o PNS dominant in GIT causing increased motility
giving antispasmodic or antimuscarinic
diminishes GIT activity
o PNS dominant in heart (bradycardia)
Atria are more affected than the
ventricles (recording)
blocking will produce tachycardia
Sympathetic activity increases in stress (fight or flight
response), whereas parasympathetic activity
predominates during satiation and repose (maintain body
homeostasis). Both systems exert a continuous
physiological control of specific organs under normal
condition, when the body is at neither extreme.
AUTONOMIC NERVOUS SYSTEM IMPORTANT REFLEX
MECHANISMS (The following comes from the missing ppts that
dean reyes mentioned)*
Barostatic Reflex
ANS activity can be initiated or modified by impulses
from higher centers.
Changes in arterial pressure detected by
baroreceptors in carotid and aortic arch
Impulses from baroreceptors (located in carotid
sinus) via afferents (cranial nerve IX) signal
vasomotor center (VMC) to counteract original
change in BP
Example:
o Increase peripheral resistance (PR)
causes IX nerve firing:
Inhibit VMC decrease firing of
neurons in VMC decrease VMT
blood vessels (relayed thru S ganglia)
decrease BP
Excites vagal nucleus in medulla
reflex bradycardia
If you have orthostatic hypotension,
reflex mechanism is reflex tachycardia.
Spinal Micturition
Accumulation of urine increase in intravesical
tension activates sensory neurons in urinary
bladder wall sends afferents to spinal cord
efferent impulses from spinal cord activate
detrusor muscle and inhibit sphincter
micturition reflex
STEPS IN NEUROHORMONAL TRANSMISSION
Axonal Conduction
Passage of impulse along the axon or muscle fiber
Ca2+ and Na+ dependent opening of Na+ channels
influx of Na+ membrane depolarization response
(e.g. muscle contraction)
Increased permeability to Na+ depolarization
o Synthesis and storage of transmitter
substances in their respective vesicles
o Axonal conduction is produced upon arrival of
an action potential.
o Stimulation of nicotinic receptor muscle
contraction prolonged stimulation
depression of depolarization block leads to
flaccid paralysis
By blocking the Na+ channels, action potential
propagation can be inhibited by:
o Saxitoxin (red tide toxin)
Neurotoxin caused by dinoflagellates
Responsible for paralytic shellfish
poisoning (PSP)
Can block conduction by blocking Na+
channels; causes muscle paralysis
Tetrodotoxin (puffer fish toxin)
Local anesthetics
Transmission across Junctions
Passage of the impulse across synaptic or neuroeffector
junction
Transmitter Release via Exocytosis
Mediated by Ca2+, antagonized by Mg
2
+
o Ca2+ destabilizes vesicles vesicles move
closer to presynaptic membrane fusion of
vesicular membrane and prejunctional
membrane occurs with interaction of specific
membrane proteins (vesicular proteins and
proteins associated with terminal membrane
e.g. VAMP, synaptosomes) release of
transmitters
Certain toxins may inhibit neurotransmitter release (e.g.
botulinum toxin (Botox) inhibits Ach release, causing
muscle relaxation)
NeurotransmitterReceptor Combination and Interaction
Change in permeability of receptor membrane
o Generalized increased permeability to all ions
(e.g. K+, Na+, Ca2+ depolarization)
o Selective permeability to small ions (e.g. K+
causes hyperpolarization)
Change in polarity
o Before transmission, transmitter substances are
synthesized in the synaptic vesicle.
o Arrival of the action potential (AP) destabilizes
synaptic vesicle which causes fusion of the
presynaptic membranes with the synaptic
vesicle release of neurotransmitter (NT)
Generalized increased permeability
depolarization excitatory
postsynaptic potential (EPSP)
increased activity (e.g. muscle
contracts)
Selective permeability
hyperpolarization (opening of K+
channels) inhibitory postsynaptic
potential (IPSP) decreased activity
(e.g. muscle relaxes)
Repolarization return to resting stage
ready for another AP
Enzymatic Destruction
Acetylcholine (Ach)
o Degraded by acetylcholinesterase (major
pathway) also known as true or specific
cholinesterase
o Found in cholinergic nerve synapse, RBC,
platelets, as well as in some vascular tissues
o Plasma/butyryl/pseudo cholinesterase has a
broader function.
NE or noradrenaline
o Degraded by catechol O methyl transferase
(COMT) which is found in liver and muscle, and
monoamine oxidase (MAO) which is found in
the mitochondria, cytoplasm, in the nerve
terminal itself, liver, and intestine
Uptake
UPTAKE 1 neuronal uptake
o Major pathway for termination of NE action
o NE goes back into cytoplasm via an active
pump that requires a carrier and also goes back
into vesicle.
o Also true for Ach choline (product of
degradation) goes back into cytoplasm for
synthesis of Ach
o Site of action of tricyclic antidepressants and
procaine (prevent the uptake of NE back to the
cytoplasmic pool)
UPTAKE 2 extraneuronal uptake
o Transmitter substance diffuses into perisynaptic
glia and into the muscle
o Simple diffusion into receptor sites ultimately
goes back into circulation and is degraded by
enzymes
You might also like
- Preventive Pediatrics 2016Document59 pagesPreventive Pediatrics 2016Marie Frances Lalican-RingelNo ratings yet
- 12Lec-Dermatologic InfectionsDocument69 pages12Lec-Dermatologic InfectionsCarmela MamintaNo ratings yet
- Anatomy Supertable PDFDocument14 pagesAnatomy Supertable PDFAlex Ondevilla100% (1)
- 392 FullDocument7 pages392 FullMarie Frances Lalican-RingelNo ratings yet
- Blood TransfusionDocument5 pagesBlood TransfusionCla67% (3)
- Heat StrokeDocument6 pagesHeat StrokeMarie Frances Lalican-RingelNo ratings yet
- Topnotch Surgery Reviewer PDFDocument81 pagesTopnotch Surgery Reviewer PDFMarie Frances Lalican-Ringel100% (16)
- Cis 2017 PDFDocument3 pagesCis 2017 PDFTheresa IlanoNo ratings yet
- Endo AlterationsDocument8 pagesEndo AlterationsMarie Frances Lalican-RingelNo ratings yet
- Ncm106 Notes 2012 ABCDocument9 pagesNcm106 Notes 2012 ABCMarie Frances Lalican-RingelNo ratings yet
- Dr's OrderDocument3 pagesDr's OrderMarie Frances Lalican-RingelNo ratings yet
- Dr's OrderDocument3 pagesDr's OrderMarie Frances Lalican-RingelNo ratings yet
- Osteoporosis CADocument3 pagesOsteoporosis CAMarie Frances Lalican-RingelNo ratings yet
- Assess and treat pressure ulcer riskDocument2 pagesAssess and treat pressure ulcer riskMarie Frances Lalican-RingelNo ratings yet
- Dr's OrderDocument3 pagesDr's OrderMarie Frances Lalican-RingelNo ratings yet
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue PerfusionMarie Frances Lalican-RingelNo ratings yet
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue PerfusionMarie Frances Lalican-RingelNo ratings yet
- Pancreatic Enzymes Do Not Work in An Acidic Environment The Need For An Alkaline Rich FluidDocument17 pagesPancreatic Enzymes Do Not Work in An Acidic Environment The Need For An Alkaline Rich FluidMarie Frances Lalican-RingelNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Biology Form 3 December Holiday AssignmentDocument38 pagesBiology Form 3 December Holiday Assignmenterastuskamunya1No ratings yet
- Severe PreeclampsiaDocument84 pagesSevere PreeclampsiaJm Bernardo50% (2)
- NPB 100 Midterm 1 Study Guide-1Document4 pagesNPB 100 Midterm 1 Study Guide-1April MartínezNo ratings yet
- Product Assessment Report - K-Othrine SC 25 Family PublicDocument142 pagesProduct Assessment Report - K-Othrine SC 25 Family PublicwibowoNo ratings yet
- Neuromorphic Engineering: From Biological To Spike Based Hardware Nervous SystemsDocument33 pagesNeuromorphic Engineering: From Biological To Spike Based Hardware Nervous SystemsSruthy sureshNo ratings yet
- Analyse Signal EMGDocument12 pagesAnalyse Signal EMGAlfonso Molina RamirezNo ratings yet
- Psych 1101 FinalDocument25 pagesPsych 1101 FinalSimon HagosNo ratings yet
- Understanding SeizuresDocument105 pagesUnderstanding SeizuresvlinkhoeNo ratings yet
- New Test - February 14, 2018: Markscheme Examiners ReportDocument35 pagesNew Test - February 14, 2018: Markscheme Examiners ReportRitika GulguliaNo ratings yet
- Model Muschi 2Document15 pagesModel Muschi 2DanDezideriuIacobNo ratings yet
- Academic Question Paper Test 3 PDFDocument21 pagesAcademic Question Paper Test 3 PDFfarrukhNo ratings yet
- Chaos in The Hodgkin-Huxley Model: John Guckenheimer Ricardo A. OlivaDocument10 pagesChaos in The Hodgkin-Huxley Model: John Guckenheimer Ricardo A. OlivaaldoNo ratings yet
- Psych 111 NotesDocument31 pagesPsych 111 NotesMelodie WrideNo ratings yet
- Electromiografia RevneurolDocument14 pagesElectromiografia RevneurolCelia GodoyNo ratings yet
- Muscular System Outline PDFDocument102 pagesMuscular System Outline PDFAlok Singh100% (1)
- Leeson Plan MemmlersDocument34 pagesLeeson Plan Memmlersj01scott100% (1)
- GERRIG 20e 03 FDocument76 pagesGERRIG 20e 03 FErsin TukenmezNo ratings yet
- Marieb Ch7aDocument31 pagesMarieb Ch7aapi-229554503No ratings yet
- IB QBANK 6.1 - p1-p2Document35 pagesIB QBANK 6.1 - p1-p2Naz Gümüşlüoğlu100% (1)
- Tufts Pharmacology ReviewDocument46 pagesTufts Pharmacology Reviewtesh_sachdeva100% (3)
- SURFING National Biology 4 Maitaing Internal Sample PDFDocument21 pagesSURFING National Biology 4 Maitaing Internal Sample PDFelamNo ratings yet
- Atlas of EEG, Seizure Semiology, and Management 2nd EdDocument384 pagesAtlas of EEG, Seizure Semiology, and Management 2nd Edsolecitodelmar100% (9)
- Bienenstock Cooper MunroDocument7 pagesBienenstock Cooper MunroGülsüm YıldırımNo ratings yet
- Biology Lecture Notes: (Stemer'S Guide)Document28 pagesBiology Lecture Notes: (Stemer'S Guide)Magdy Mohamed Abdallah AbdelkaderNo ratings yet
- Unit 1 Part 3 SignallingDocument32 pagesUnit 1 Part 3 SignallingAnn NguyenNo ratings yet
- Test Bank For The Human Body in Health and Disease 7th Edition by PattonDocument22 pagesTest Bank For The Human Body in Health and Disease 7th Edition by Pattonstephaniemendozagamobckjqf100% (15)
- Neurotransmisson AVSDocument1 pageNeurotransmisson AVSHeliodor van ScriverNo ratings yet
- Chapter 7 Nervous System VocabDocument4 pagesChapter 7 Nervous System VocabfamouspotatoNo ratings yet
- Synaptic Transmission at The Crayfish Superficial Flexor Muscle and Third NerveDocument14 pagesSynaptic Transmission at The Crayfish Superficial Flexor Muscle and Third Nerveapi-340131743No ratings yet
- Presentation Bio502 Hodgkin Huxley Neuron 3 13 17 2Document14 pagesPresentation Bio502 Hodgkin Huxley Neuron 3 13 17 2api-369102829No ratings yet