Professional Documents
Culture Documents
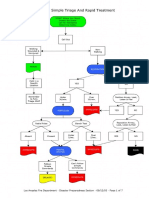
Triage
Uploaded by
Putra EkaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Triage
Uploaded by
Putra EkaCopyright:
Available Formats
Original Contribution
Use of the Triage Stroke Panel in a neurologic
emergency service
Igor Sibon MD, PhD
, Franois Rouanet MD,
Wassilios Meissner MD, PhD, Jean Marc Orgogozo MD
Department of Clinical Neurosciences, Bordeaux University Hospital, France
Received 31 October 2007; revised 9 May 2008; accepted 13 May 2008
Abstract
Background: Acute stroke is associated with serum elevations of numerous markers. We evaluated the
additive accuracy of the Triage Stroke Panel (D-dimer, B-natriuretic peptide, matrix metalloproteinase 9,
and S-100) to the triaging nurse for acute stroke diagnosis.
Methods: Consecutive patients with suspected stroke were included in this prospective, controlled,
single-center study. A well-trained stroke center triage nurse assigned a probability that the patient had
experienced a stroke (certain, very probable, probable, not likely, doubtful, or other); then, the Triage
Stroke Panel testing was performed. Patients' diagnosis was based on clinical and imaging data by a
neurologist blinded to the test results.
Results: Two hundred four patients were evaluated. Confirmed strokes and transient ischemic attacks
(TIAs) were observed in 131 patients. When considering an experienced stroke nurse's assessment of
other, doubtful, or not likely to be negative for stroke and categorizing TIAwith stroke, the stroke
panel's Multimarker Index (MMX) value had identical accuracy (70%) and equivalent sensitivity
(94%) and specificity (24%) for stroke diagnosis to that of the nurse. Combining nurse assessment
with the MMX result significantly improved the specificity of diagnosing mimic vs stroke + TIA from
25.4% (nurse assessment only) to 46.0% (nurse assessment + MMX; P b .001).
Conclusions: The Triage Stroke Panel provides objective information that complements a triage nurse in
the assessment of a suspected stroke patient. Its performance compares favorably with that of a well-
trained stroke center triage nurse, suggesting potential use in nonexpert centers for improving the
accuracy of stroke diagnosis.
2009 Elsevier Inc. All rights reserved.
1. Introduction
In patients suspected of having an acute cerebrovascular
insult, time to diagnosis and accuracy of diagnosis are the 2
main parameters for successful therapy. In the last 15 years,
the introduction of thrombolytic agents for the treatment of
acute ischemic stroke has resulted in a transition in stroke
care from supportive medical therapy to that of an acute
medical emergency [1]. However, the time-window for
thrombolytic therapy remains narrow and requires rapid,
accurate, and well-organized prehospital and in-hospital
systems [2,3]. Several obstacles preclude early administra-
tion of thrombolytic therapy in acute stroke patients such as
Corresponding author. Dpartement de Neurologie, CHU Pellegrin,
Universit de Bordeaux II, Place Amlie Raba-Lon, 33076 Bordeaux
Cedex France. Tel.: +33 5 56 79 55 20; fax: +33 5 56 79 87 02.
E-mail address: igor.sibon@chu-bordeaux.fr (I. Sibon).
www.elsevier.com/locate/ajem
0735-6757/$ see front matter 2009 Elsevier Inc. All rights reserved.
doi:10.1016/j.ajem.2008.05.001
American Journal of Emergency Medicine (2009) 27, 558562
the following: (1) the lack of awareness of stroke symptoms
by the patient or the patient's family, (2) the nonurgent triage
of stroke patients in the emergency department (ED), or (3)
the physician's uncertainty regarding administration of
thrombolytic medication [4]. To overcome these short-
comings, different awareness campaigns have disseminated
stroke warning signs to the general population and have
promoted thrombolysis to health professionals [5-7].
Furthermore, the competences of paramedics have been
improved by specific stroke education programs [8-10].
However, only 2% to 10% of acute stroke patients receive
intravenous thrombolysis [11-13], suggesting the need for
additional efforts to increase the number of treated patients.
In most hospitals, stroke patients are commonly triaged by
nurses responsible for the management of all acute medical
conditions. Several studies have clearly demonstrated the
effectiveness of acute stroke triage protocols in reducing
door-tocomputed tomography (CT) and door-to-needle
times in patients presenting directly to the ED[14]. Moreover,
Lindsberg, et al [15] reported a favorable increase in the
number of patients eligible for thrombolytic therapy after a
reorganization of the ED. Improved triage of stroke patients
was achieved using a nursing team that was trained in stroke
symptom recognition and exclusively dedicated to the care of
neurologic patients in the ED [15,16]. However, in the
preadmission setting and in nonspecialized centers where
specifically trained stroke nurses are unavailable, the
accuracy of clinical and paraclinical tools is critical to reduce
the risk of misdiagnosing stroke and its medicolegal
implications [17]. In this case, a rapid and sensitive diagnostic
assay for detecting acute stroke would be highly beneficial for
the triage of stroke patients during preadmission and in the
ED of nonspecialized centers. The Triage Stroke Panel
(Biosite Incorporated, San Diego, Calif) is a rapid point-of-
care test that measures plasma levels of B-type natriuretic
peptide (BNP), D-dimer, matrix metalloproteinase 9 (MMP-
9), and S-100 and provides the test results as a Multimarker
Index (MMX) value. The MMXvalue can be used as an aid in
the assessment and diagnosis of stroke. Here, we assessed the
accuracy of a trained stroke nurse and the Triage Stroke Panel
for identifying stroke patients in the ED.
2. Materials and methods
Two hundred four consecutive patients with suspected
stroke or transient ischemic attack (TIA, defined as
spontaneous disappearance of neurologic symptoms within
the 24 hours after stroke onset) presenting during autumn
2005 to the ED of the Hospital Pellegrin, Bordeaux, were
included in this study. Patients with coma or traumatic injury
were excluded.
A well-trained stroke center triage nurse considered a
diagnosis of stroke when a patient presented with sudden
onset of limb weakness, difficulties in speech/language,
vision, mobility, or balance, or when a physician referred the
patient for suspected stroke or TIA. The nurse assigned a
stroke probability for each patient (certain, very probable,
probable, not likely, doubtful, or other diagnosis).
During the assessment, the patient's blood was drawn for
Triage Stroke Panel testing. The EDTA-anticoagulated
whole blood was used for this purpose. The Triage Stroke
Panel is a point-of-care fluorescence immunoassay for the
rapid quantitative measurement of BNP and fibrin degrada-
tion products containing D-dimer, MMP-9, and S-100 in
EDTA-anticoagulated whole blood or plasma specimens. In
addition to the values for the individual markers, a
proprietary algorithm for the automatic calculation of a
single MMX result is obtained to simplify the assessment
and diagnosis of stroke (Triage Stroke Panel). The MMX
ranges from 0 to 10. If the MMX is less than or equal to 1.3,
the likelihood of a stroke is low. An index greater than 5.9
indicates a strong likelihood of stroke. A value between 1.3
and 5.9 is abnormal and suggests the need for further
evaluation [18]. Nurses were blinded to the MMX results.
All patients underwent a clinical evaluation by a neurologist,
and brain imaging was performed (brain CT scan and/or
magnetic resonance imaging) within 24 hours after admis-
sion. The final diagnosis was based on clinical and imaging
data and was performed 1 day after admission by a senior
neurologist blinded to the test results. Strokes were
subclassified as infarctions, TIAs, and hemorrhages.
All other diagnoses were grouped as mimics.
Descriptive statistics were summarized for patient demo-
graphic variables and final diagnosis. Patients with missing
data (MMX or nurse assessment) were excluded from the
statistical analyses. The clinical performance parameters of
sensitivity, specificity, positive predictive value (PPV), and
negative predictive value (NPV) were calculated based on
the final diagnosis of the patients for the MMX result and the
stroke nurse's assessment. The accuracy for identifying
stroke patients by the MMX result (value, N1.3), the trained
nurse's assessment, or their combination was defined by the
Fig. 1 Disease probability based upon single MMX cutoff.
Percentages of mimic (gray), stroke (black), and TIA (white)
diagnoses depending on the MMX cutoff. Mimic was significantly
less probable when MMX value was higher than 1.3. Stroke was
significantly more probable when MMX value was higher than 1.3
( corresponds to P b .001).
559 Triage Stroke Panel in a neurologic emergency service
sensitivity, specificity, NPV and PPV, and the validity was
supported by the percent of true positives (ie, MMX
validity = Number of positive MMX (N1.3) results / Total
number of strokes confirmed by the neurologist).
NcNemar tests were used to compare the clinical
performance parameters between the MMX result, the stroke
nurse's assessment, and the combination of the MMX result
with the stroke nurse's assessment. Results with P values
less than .05 were considered to be statistically significant.
3. Results
Two hundred four patients with a suspected stroke were
evaluated (104 men and 92 women), 8 patients were excluded
because of technical failure. Mean age was 70.11 15.6 years
(67.69 14.29 years for men and 72.85 15.6 years for
women). The diagnosis of stroke was confirmed in 131 cases
with the following subtypes: 85 infarction, 33 TIA, and 13
hemorrhages. The remaining 65 patients received hetero-
geneous diagnoses including epilepsy, encephalitis, or
tumors. These patients received the diagnosis of stroke
mimic. For 7 patients (5 patients with stroke and 2 patients
with mimic), the nurse-assigned stroke probability was
unavailable. Therefore, statistical analyses were performed
for 189 patients (126 patients with stroke and 63 patients
with mimic).
In patients whose MMX value was greater than 1.3, the
probability of stroke was greater than 50%, whereas in
patients whose MMX value was less than or equal to 1.3, the
probability of a stroke mimic or TIA was 80% (Fig. 1). The
probability of stroke increased with the MMX value and was
76.1% in patients whose MMX value was greater than 5.9.
When considering an experienced stroke nurse assess-
ment of other, doubtful, or not likely to be negative for
stroke, and categorizing TIA with stroke, the MMX result
and the nurse assessment had identical accuracy (agreement
with the final diagnosis) (71.4% nurse vs 69.8% MMX) and
equivalent sensitivity (94.4% nurse vs 92.9% MMX) and
specificity (25.4% nurse vs 23.8% MMX) as well as NPV
and PPV for the diagnosis of stroke compared with the
diagnosis suggested by the nurse (Fig. 2, Table 1). Ninety-
nine percent of strokes were identified if any positive nurse
assessment or a positive Triage Stroke Panel MMX was
considered. Combining nurse assessment with the MMX
significantly improved the specificity of diagnosing mimic
vs stroke + TIA from 25.4% (nurse assessment only) to
46.0% (nurse assessment + MMX; P b.001) (Table 2).
4. Discussion
The present study demonstrates that the measurement of a
combination of biomarkers that are included in the Triage
Stroke Panel candetect cerebral infarct withthe same accuracy
and specificity as a nurse trained in stroke management.
The diagnosis of acute ischemic stroke in most hospitals
is only made on clinical grounds after exclusion of an
intracranial hemorrhage or a mass lesion by CT. However,
other potential causes of an acute focal neurologic deficit,
including complex migraine, postictal paresis, tumors,
demyelinating disorders, or even metabolic disturbances
such as hypoglycemia, may be difficult to differentiate from
stroke. Here, we demonstrate that the MMX might assist in
differentiating these mimics from real stroke patients, mainly
in centers without an experienced triage nurse and in the
prehospital setting.
Acute stroke is associated with serum elevations of
numerous inflammatory and anti-inflammatory mediators
such as interleukin 6 and MMP-9 [19-23], markers of
impaired hemostasis and thrombosis such as D-dimer [24,25]
and markers of glial activation such as S-100 [26,27].
Several of these markers are elevated within hours after
ischemia and correlate with infarct volume [28,29]. How-
Fig. 2 Nurse assessment and MMX result comparison in stroke
diagnosis. Comparison of MMX (gray) and nurse (black)
performance for patients with a diagnosis of stroke mimic vs
patients with a cerebrovascular event (TIA and stroke).
Table 1 Sensitivity and specificity of nurse and MMX stroke
assessment (TIA included)
n = 189 Mimic All strokes (+TIA)
Nurse+
MMX+
n 34 111
% 17.99 59
MMX
n 13 8
% 6.88 4.23
Nurse
MMX+
n 14 6
% 7.41 3.17
MMX
n 2 1
% 1.06 0.53
Nurse: sensitivity, 94.4%; specificity, 25.4%; and accuracy, 71.4%.
MMX: sensitivity, 92.9%; specificity, 23.8%; and accuracy, 69.8%.
Nurse is negative if assigned stroke probability is other, doubtful, or
not likely.
MMX is negative if equivalent to 1.3 or lesser.
560 I. Sibon et al.
ever, although highly correlated with cerebral ischemia, no
individual biochemical marker has the necessary sensitivity
and specificity to be used as a clinically independent
diagnostic marker [30-32]. Given the absence of a single
peripheral diagnostic marker of stroke, an alternative
approach is the creation of a panel of several serum
biomarkers [30,33,34].
Among the biochemical markers that are involved in the
pathogenesis of stroke and neuronal injury, Lynch et al [30]
identified 4 markers as highly correlated with stroke: 1
marker of glial activation (S-100), 2 markers of inflamma-
tion (matrix metalloproteinase 9 and vascular cell adhesion
molecule), and 1 marker of thrombosis (von Willebrand
factor). S-100, MMP-9, and von Willebrand factor were
also identified by Reynolds et al [34] as highly correlated
with the diagnosis of stroke as well as B-type neurotrophic
growth factor and monocyte chemoattractant protein-1.
Moreover, they demonstrated the ability of these different
biomarkers as a marker panel to diagnose hemorrhagic and
ischemic stroke and, in particular, acute ischemic stroke
within the first 6 hours of onset [34]. The Triage Stroke Panel
was designed according to the results of these different
biomarker studies in stroke patients. In a recent study,
Grifoni et al [35] found the MMX result to have an accuracy
for stroke diagnosis of 74%, a result close to the 69.8%
observed in the present study. Grifoni et al [35] also reported
the ability of the Triage stroke panel to contribute to the
diagnosis of stroke when clinical data are doubtful and when
the values of a prehospital stroke scale are normal. Together
with the present study, these results suggest that the Triage
Stroke Panel is an attractive tool to improve the accuracy of
rapid stroke diagnosis. Two cutoffs associated with a high and
low probability of stroke have been defined. In the present
study, we only used the lower cutoff (1.3). This provided the
opportunity to identify the benefit of combining the MMX
with the nurse assessment, suggesting that a single cutoff
should be used in the clinical practice.
The ideal biomarker (or panel) should be able to identify
acute stroke, differentiate ischemic from hemorrhagic stroke,
correlate with infarct volume, relate to stroke mechanism,
and predict the long-term outcome. To date, no single
biomarker meets these criteria, but studies have demon-
strated that a combination of biomarkers, including D-dimer
and BNP, might be more specific of cardioembolic stroke and
that D-dimer or MMP-9 could be linked to infarct volume or
stroke outcome [21,34]. Further studies are necessary to
confirm these data.
In conclusion, the use of the Triage Stroke Panel provides
objective information that complements a triage nurse in the
assessment of a suspected stroke patient. Its performance
compares favorably with that of a well-trained stroke center
triage nurse, suggesting potential use in nonexpert centers for
improving the accuracy of stroke diagnosis. Moreover,
experienced EDs might also benefit from use of the Triage
Stroke Panel because the specificity for the diagnosis of a
mimic was increased, and 99% of stroke patients could be
identified when combining the nurse assessment with the
MMX result. However, the interaction of the nursing
assessment and the Triage Stroke Panel result was not
investigated and is a limitation to this study. Because the
nurses were blinded to the results of the Triage Stroke Panel,
a 99% rate of stroke identification (by a positive nurse
assessment or a positive Triage Stroke Panel) may over-
estimate the actual rate of stroke identification. Further
research will be needed to investigate the interaction of the
nurse assessment and the Triage Stroke Panel result.
References
[1] Citerio G, Galli D, Cadore B, et al. How to improve ischemic stroke
treatment in the fibrinolysis era. Minerva Anestesiol 2006;72:407-12.
[2] Hacke W, Brott T, Caplan L, et al. Thrombolysis in acute ischemic
stroke: controlled trials and clinical experience. Neurology 1999;53:
S3-S14.
Table 2 Statistical comparison between MMX, nurse and Nurse + MMX in stroke diagnosis
MMX Nurse Nurse + MMX Fisher exact or
2
test
a
Sensitivity 0.929 (0.870-0.962) 0.944 (0.890-0.973) 0.992 (0.956-0.999) 0.06598 NS
b
TP 117 119 125
FN 9 7 1
Specificity 0.238 (0.149-0.356) 0.254 (0.163-0.373) 0.460 (0.343-0.582) 0.025148
b
TP 15 16 29
FN 48 47 34
Likelihood ratio+ 1.2 1.3 1.8
Likelihood ratio 3.3 4.6 58.0
PPV 0.709 (0.636-0.773) 0.717 (0.644-0.779) 0.786 (0.715-0.843) 0.5682 NS
c
NPV 0.625 (0.427-0.788) 0.696 (0.491-0.844) 0.967 (0.833-0.994) 0.1605 NS
c
Accuracy 0.698 (0.630-0.759) 0.714 (0.646-0.774) 0.815 (0.753-0.864) 0.5454 NS
c
Parenthetical values are 95% confidence interval.
NS indicates nonstatistically significant; TP, true positive; FN, false negative.
a
Comparison between nurse vs nurse + MMX (n = 189).
b
Fisher exact.
c
2
561 Triage Stroke Panel in a neurologic emergency service
[3] Wardlaw JM, Zoppo G, Yamaguchi T, et al. Thrombolysis for
acute ischaemic stroke. Cochrane Database Syst Rev 2003:
CD000213.
[4] Kwan J, Hand P, Sandercock P. A systematic review of barriers to
delivery of thrombolysis for acute stroke. Age Ageing 2004;33:
116-21.
[5] Kwan J, Hand P, Sandercock P. Improving the efficiency of delivery of
thrombolysis for acute stroke: a systematic review. QJM 2004;97:
273-9.
[6] Alberts MJ, Perry A, Dawson DV, et al. Effects of public and
professional education on reducing the delay in presentation and
referral of stroke patients. Stroke 1992;23:352-6.
[7] Morgenstern LB, Staub L, Chan W, et al. Improving delivery of acute
stroke therapy: the TLL Temple Foundation Stroke Project. Stroke
2002;33:160-6.
[8] Sandercock P, Berge E, Dennis M, et al. A systematic review of the
effectiveness, cost-effectiveness and barriers to implementation of
thrombolytic and neuroprotective therapy for acute ischaemic stroke in
the NHS. Health Technol Assess 2002;6:1-112.
[9] Bray JE, Martin J, Cooper G, et al. An interventional study to
improve paramedic diagnosis of stroke. Prehosp Emerg Care 2005;9:
297-302.
[10] Bray JE, Martin J, Cooper G, et al. Paramedic identification of stroke:
community validation of the Melbourne ambulance stroke screen.
Cerebrovasc Dis 2005;20:28-33.
[11] Rosamond W, Flegal K, Friday G. Heart disease and stroke statistics
2007 update. http://circahajournalsorg/cgi/content/full/115/5/e69#
TBL5179743; 2007.
[12] Katzan IL, Furlan AJ, Lloyd LE, et al. Use of tissue-type plasminogen
activator for acute ischemic stroke: the Cleveland area experience.
JAMA 2000;283:1151-8.
[13] Wang DZ, Rose JA, Honings DS, et al. Treating acute stroke patients
with intravenous tPA. The OSF stroke network experience. Stroke
2000;31:77-81.
[14] Mehdiratta M, Woolfenden AR, Chapman KM, et al. Reduction in IV
t-PA door to needle times using an Acute Stroke Triage Pathway. Can J
Neurol Sci 2006;33:214-6.
[15] Lindsberg PJ, Happola O, Kallela M, et al. Door to thrombolysis: ER
reorganization and reduced delays to acute stroke treatment.
Neurology 2006;67:334-6.
[16] Ornstein SM. Translating research into practice using electronic
medical records the PPRNet-TRIP project: primary and secondary
prevention of coronary heart disease and stroke. Top Health Inf
Manage 2001;22:52-8.
[17] Brous E. A patient with an undetected evolving stroke: legal lessons
learned. J Emerg Nurs 2005;31:580-2.
[18] Laskowitz D. A point of care diagnostic for acute stroke. 14th Annual
European Stroke Conference, Bologna, Italy; 2005.
[19] Kim JS, Yoon SS, Kim YH, et al. Serial measurement of interleukin-6,
transforming growth factorbeta, and S-100 protein in patients with
acute stroke. Stroke 1996;27:1553-7.
[20] Dziedzic T, Bartus S, Klimkowicz A, et al. Intracerebral hemorrhage
triggers interleukin-6 and interleukin-10 release in blood. Stroke 2002;
33:2334-5.
[21] Montaner J, Alvarez-Sabin J, Molina C, et al. Matrix metalloproteinase
expression after human cardioembolic stroke: temporal profile and
relation to neurological impairment. Stroke 2001;32:1759-66.
[22] Perini F, Morra M, Alecci M, Galloni E, et al. Temporal profile of
serum anti-inflammatory and pro-inflammatory interleukins in acute
ischemic stroke patients. Neurol Sci 2001;22:289-96.
[23] Vila N, Castillo J, Davalos A, Chamorro A. Proinflammatory
cytokines and early neurological worsening in ischemic stroke. Stroke
2000;31:2325-9.
[24] Fon EA, Mackey A, Cote R, et al. Hemostatic markers in acute
transient ischemic attacks. Stroke 1994;25:282-6.
[25] Takano K, Yamaguchi T, Uchida K. Markers of a hypercoagulable
state following acute ischemic stroke. Stroke 1992;23:194-8.
[26] Buttner T, Weyers S, Postert T, et al. S-100 protein: serum marker of
focal brain damage after ischemic territorial MCA infarction. Stroke
1997;28:1961-5.
[27] Martens P, Raabe A, Johnsson P. Serum S-100 and neuron-specific
enolase for prediction of regaining consciousness after global cerebral
ischemia. Stroke 1998;29:2363-6.
[28] Tarkowski E, Rosengren L, Blomstrand C, et al. Early intrathecal
production of interleukin-6 predicts the size of brain lesion in stroke.
Stroke 1995;26:1393-8.
[29] Fassbender K, Rossol S, Kammer T, et al. Proinflammatory cytokines
in serum of patients with acute cerebral ischemia: kinetics of secretion
and relation to the extent of brain damage and outcome of disease.
J Neurol Sci 1994;122:135-9.
[30] Lynch JR, Blessing R, White WD, et al. Novel diagnostic test for acute
stroke. Stroke 2004;35:57-63.
[31] Jauch EC, Lindsell C, Broderick J, et al. Association of serial
biochemical markers with acute ischemic stroke: the National Institute
of Neurological Disorders and Stroke recombinant tissue plasminogen
activator stroke study. Stroke 2006;37:2508-13.
[32] Rainer TH, Lam NY, Man CY, et al. Plasma beta-globin DNA as a
prognostic marker in chest pain patients. Clin Chim Acta 2006;368:
110-3.
[33] Dambinova SA, Khounteev GA, Skoromets AA. Multiple panel of
biomarkers for TIA/stroke evaluation. Stroke 2002;33:1181-2.
[34] Reynolds MA, Kirchick HJ, Dahlen JR, et al. Early biomarkers of
stroke. Clin Chem 2003;49:1733-9.
[35] Grifoni S, Vanni S, Caini R, et al. Biochemical markers for the
diagnosis of stroke: do they work in the real world. Conferenza
nationale dell ictus cerebrale, Firenze, Italy; 2006.
562 I. Sibon et al.
Reproducedwith permission of thecopyright owner. Further reproductionprohibited without permission.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Vaksin VarelaDocument8 pagesVaksin VarelaPutra EkaNo ratings yet
- KemoDocument11 pagesKemoPutra EkaNo ratings yet
- NutritionsDocument9 pagesNutritionsPutra EkaNo ratings yet
- Acute Pulmonary Edema Algorithm: Consider ConsultationDocument1 pageAcute Pulmonary Edema Algorithm: Consider ConsultationPutra EkaNo ratings yet
- Sample WordDocument1 pageSample WordNuno AlvesNo ratings yet
- Jurnal FixDocument6 pagesJurnal FixPutra EkaNo ratings yet
- Causes and Treatment of Pulmonary EdemaDocument1 pageCauses and Treatment of Pulmonary EdemaShila Wisnasari100% (2)
- Hominid EvolutionDocument2 pagesHominid EvolutionJosephine TorresNo ratings yet
- Maternitas JurnalDocument12 pagesMaternitas JurnalPutra EkaNo ratings yet
- APARQ QuestionnaireDocument6 pagesAPARQ QuestionnairehumanismeNo ratings yet
- Jurnal FixDocument6 pagesJurnal FixPutra EkaNo ratings yet
- Clean Vs Sterile Dressing Techniques For.7Document5 pagesClean Vs Sterile Dressing Techniques For.7Putra EkaNo ratings yet
- Emergency Severity IndexDocument114 pagesEmergency Severity Indexpafin100% (3)
- Start TriageDocument7 pagesStart TriagePutra EkaNo ratings yet
- Effectiveness of Biofeedback As A Tool To Reduce The Perception of Labour Pain Among Primigravidas: Pilot StudyDocument4 pagesEffectiveness of Biofeedback As A Tool To Reduce The Perception of Labour Pain Among Primigravidas: Pilot StudyPutra EkaNo ratings yet
- BasicDocument8 pagesBasicPutra EkaNo ratings yet
- Ipi 107451Document5 pagesIpi 107451Ade Churie TanjayaNo ratings yet
- BasicDocument8 pagesBasicPutra EkaNo ratings yet
- 4686216Document3 pages4686216Putra EkaNo ratings yet
- RoleDocument8 pagesRolePutra EkaNo ratings yet
- BasicDocument8 pagesBasicPutra EkaNo ratings yet
- 4686216Document3 pages4686216Putra EkaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Daftar Seminar Q SIPDocument2 pagesDaftar Seminar Q SIPririn widyaNo ratings yet
- UT Trauma HandbookDocument49 pagesUT Trauma Handbooksgod34No ratings yet
- Certificate and Duties and ResponsibilitiesDocument2 pagesCertificate and Duties and ResponsibilitiesShiredan Rose BagarinaoNo ratings yet
- Case Study On SEPSIS 2' ACP PneumoniaDocument7 pagesCase Study On SEPSIS 2' ACP Pneumoniajcarysuitos100% (2)
- Karyotype ProjectDocument4 pagesKaryotype ProjectShreya DharmaNo ratings yet
- Sample Operative ReportsDocument24 pagesSample Operative ReportsIta Farica100% (1)
- Neonatal Resuscitation DrugsDocument4 pagesNeonatal Resuscitation Drugsblast2111No ratings yet
- Elated QuotesDocument28 pagesElated Quotesshasha001No ratings yet
- History of shingles rehabilitationDocument1 pageHistory of shingles rehabilitationTrixter GarciaNo ratings yet
- IMNCI Students Handbook PDFDocument93 pagesIMNCI Students Handbook PDFAamira Qureshi100% (4)
- AbstractDocument23 pagesAbstractaashish21081986No ratings yet
- FERRIC CARBOXYMALTOSE IMPROVES SYMPTOMS IN HEART FAILURE PATIENTS WITH IRON DEFICIENCYDocument31 pagesFERRIC CARBOXYMALTOSE IMPROVES SYMPTOMS IN HEART FAILURE PATIENTS WITH IRON DEFICIENCYDanar Fahmi SudarsonoNo ratings yet
- Hospital Outdoor Spaces - Therapeutic Benefits and Design ConsiderationsDocument15 pagesHospital Outdoor Spaces - Therapeutic Benefits and Design Considerationsmimk2014No ratings yet
- Arjun Pts Orem - Sumitra DeviDocument13 pagesArjun Pts Orem - Sumitra DeviChandan PradhanNo ratings yet
- Ultrasound in Critical CareDocument4 pagesUltrasound in Critical CareFranz MiguelNo ratings yet
- Manipulative BehaviorDocument27 pagesManipulative BehaviorPC NNo ratings yet
- StrabismusDocument9 pagesStrabismuspandejuniartaNo ratings yet
- 500-Bed Hospital General Specification and Design ConceptDocument5 pages500-Bed Hospital General Specification and Design ConceptShahnawaz ShaikhNo ratings yet
- Prescription Writing: Perfecto B. Soriano, MD, DPPS, Fpscep, MSCDocument27 pagesPrescription Writing: Perfecto B. Soriano, MD, DPPS, Fpscep, MSCJm Casupang100% (3)
- TB Screening in Pregnancy 1Document32 pagesTB Screening in Pregnancy 1nurfitriwidiNo ratings yet
- Maternal and fetal responses to laborDocument27 pagesMaternal and fetal responses to laborBeatrice ChenNo ratings yet
- Eob2 Drug PDFDocument2 pagesEob2 Drug PDFBayu PrabowoNo ratings yet
- CARDIOVASCULAR CHAPTER 6Document10 pagesCARDIOVASCULAR CHAPTER 6Marie Charmaine100% (1)
- Acute Flaccid ParalysisDocument4 pagesAcute Flaccid ParalysisZharah RuzNo ratings yet
- Antidepressants For The Treatment of InsomniaDocument8 pagesAntidepressants For The Treatment of Insomniaapi-19853437No ratings yet
- Gi Case 11 Crohns DiseaseDocument16 pagesGi Case 11 Crohns Diseaseapi-262963527No ratings yet
- Resme Rahul GuptaDocument5 pagesResme Rahul Guptarahul guptaNo ratings yet
- Abc of Burns: Kanwal Khan Lecturer ZCPTDocument35 pagesAbc of Burns: Kanwal Khan Lecturer ZCPTKanwal KhanNo ratings yet
- Foreign and Local Literature Fatigue Among NursesDocument5 pagesForeign and Local Literature Fatigue Among NursesMay Therese B. BoriborNo ratings yet
- Contoh CV Untuk Nursing MalaysiaDocument4 pagesContoh CV Untuk Nursing MalaysiaWahyudin Aziz100% (1)