Professional Documents
Culture Documents
Shock Study Guide Nursing
Uploaded by
Kory Christina100%(2)100% found this document useful (2 votes)
1K views4 pagesNursing Student Study Guide
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentNursing Student Study Guide
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
100%(2)100% found this document useful (2 votes)
1K views4 pagesShock Study Guide Nursing
Uploaded by
Kory ChristinaNursing Student Study Guide
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
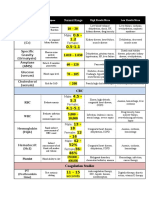
Chapter 6 Shock 107
Name Cause Signs & Symptoms Diagnosis Treatment
Hypovolemic
Shock
(Acute blood
loss from
trauma, fluid
shifts, loss from
surgery or
burns, vomiting
or diarrhea.
Severe
electrolyte
imbalance.)
Decrease in clients circulating
blood volume that leads to
inadequate tissue perfusion.
This can lead to organ damage
& death. Most Common cause
is acute blood loss from
trauma. Burned (massive
evaporation of water from
skin). Vomiting & diarrhea
(fluid loss & electrolyte
imbalance).
**Shock occurs when less than
20% of circulating blood
volume is lost & Severe shock
occurs when the patient has
lost more than 40% of the
blood volume. Most Adults
have a total blood volume of 5
liters, and do not show
symptoms of shock until at
least 500mL is lost. ** Small
children are more susceptible
than adults. ** Teens & Young
adults are high risk because
trauma main death in MVAs.
Early Signs: mild
tachycardia, mild
hypotension (B/P falls
below 90/40).
Anxiety, restlessness,
delayed cap refill,
increased Res Rate.
Kidney function
decreases. Skin cool
clammy & may appear
mottled. If
Hypovolemic is not
corrected patient may
experience
tachycardia,
arrhythmias, & chest
pain. Changes in LOC
with possible
unconsciousness.
** Weak thread pulse.
Diminished urine
output.
ABG, BUN (protein
of metabolism),
Creatine (renal
function),
Osmolality (fluid
status), WBC
(indicator of
immune status and
infection). Blood &
urine specimens.
Treatment based on
correcting circulation
volume & the cause. O2
Administered immediately.
Blood products & IV fluids
may be ordered. **LR is the
common fluid Rx. Diet &
fluids are administer as
tolerated. *Epinephrine &
dopamine. (Tissue damage,
even death, can occur if
these medications esp.
dopamine leak into the
tissue. monitor IV site for
signs of infiltration. Activity
as tolerated. Reposition Q
1-2 hours. Monitor I&O q1-
2 hours (Foley). Monitor
EKG. Signs of fluid
overload. Adequate sleep.
*Monitor changes in mental
status.
Cardiogenic
Shock
(MI, Ventricular
Hypotension, cellular hypoxia
& inadequate tissue perfusion
resulting from decreased
cardiac output.
Cool & clammy skin,
weak thread pulses,
tachycardia, increased
res rate, decreased
ABG, Cardiac
catheterization
(inserted into
femoral artery &
Treatment centered at
restoring pump function &
easing workload of the
heart. ** Cardiac output will
Chapter 6 Shock 107
Rupture,
Cardiac
tamponade.)
**Usually from MI.
Cardiogenic shock occurs in 5-
10% of clients with MIs. Risk
factors: Female, CAD, and
previous MI.
urinary output, lower
extremity edema, EKG
changes, decreased
B/P, anxiety, feelings of
impending doom, chest
pain, shortness of
breathe, hypotension.
threaded into
heart), Chest X-ray,
Echocardiogram
(ejection fraction
50-75%),
Osmolality (fluid
status), Troponin
(indicates MI),
WBC.
be less than 2.2L/min
(normal 4-8L/min). Diet as
tolerated (if critically ill
NPO or TPN). May be on a
ventilator, may need tube
feedings. **Medication is
the First Line of treatment
Dopamine & primacor.
Placed in supine
Trendelenburg position or
passive leg elevation
UNLESS patient is having
respiratory distress and
lower EXR edema.
Reposition q1-2h. Bed rest.
O2 if ordered. Urinary
output q1-2h.
Septic Shock
(Infection from
sources
including bone,
blood, invasive
lines, GI tract,
GU tract,
pulmonary,
cardiac, skin &
CNS.)
Bacteria releases endotoxins
into the bloodstream and
inflammatory cascade if
triggered that causes
inflammation in the entire
body, edema, hypotension,
hypoxia, decreased cellular
perfusion.
*Sepsis has a 40-50%
mortality rate.
Warm flushed skin,
fever above (100.4F),
tachycardia; elevated
res rate above 20/min,
WBC count to low or to
high. Anxiety,
hypotension, hypoxia,
mental status change.
*Tachycardia worsens
metabolic acidosis can
occur. Septic shock can
lead to organ damage
to the brain, heart,
*Risk increases
with age.
ABG, Blood
culture, BUN, CBC,
Creatine, EKG,
LDH, PTT, PT,
urinalysis with
culture.
Finding & treating cause is
essential. 1
st
line of
treatment is IV antibiotics,
fluid resuscitation,
vasopressors & O2. Usually
a central line is used for
multiple line access.
Monitor B/P,
Glucocorticoids used as
anti-inflammatory, Solu-
medrol is the steroid of
choice administered IV Q6-
8H. Bed REST. *Proper
Chapter 6 Shock 107
lungs, liver, and
kidneys. DEATH.
Foley cath care.
Neurogenic
Shock
(Spinal cord
injury, or
permanent
paralysis.)
Interruption of the
sympathetic Nervous System
response. NS is more severe
form of spinal shock
(sympathetic innervation of
the spinal cord is lost but the
parasympathetic function
continues).
Flaccidity & paralysis
can result in loss of
motor & sensory
function. Hypotension,
bradycardia, low B/P,
Weak thread pulse,
cool clammy skin,
decreased urinary
output, cyanosis,
increased Res Rate.
Symptoms can last 4-6
weeks. Complication:
Organ failure, MI,
stress ulcers.
ABG, BUN, CBC,
Creatine, EKG,
LDH, Urine specific
gravity.
Correction of hypotension,
IV fluid, vasopressors, O2,
Respiratory support PRN.
No dietary restrictions.
Vasopressors are the first
line of treatment. Maintain
flat position. Monitor EKG.
Monitor BS. Asses level of
anxiety.
Anaphylactic
Shock
(Type 1
hypersensitivity
reaction caused
when allergen
comes in
contact with
body)
Body reacts to foreign
substance with a misdirected
immune response. IGE
antibodies.
**Common allergies: milk &
eggs (esp. infants), peanuts,
chocolate, strawberries,
tomatoes & seafood (common
in adults. **Physiological
changes within the body in
response to anaphylactic
reactions include
bronchoconstriction,
hypotension, tachycardia,
Can occur within
minutes-hours. Itching,
hives, nasal congestion,
headache, nausea,
vomiting, or diarrhea.
Hypotension,
tachycardia, wheezing,
tachypnea, cyanosis,
chest pain,
arrhythmias, seizures,
and Rare symptoms:
pelvic pain, vaginal
bleeding, and urinary
incontinence.
ABG. BUN, CBC,
Creatine (renal
function), EKG
(electrical activity
of the heart), LDH
(tissue ischemia,
necrosis, or
acidosis), Urine
specific gravity
(fluid status).
No dietary restrictions,
except avoid food allergens.
Epinephrine. Epi-Pen Rx.
(do NOT inject Epi-pen IV
or into buttocks). Benadryl
(antihistamine),
Corticosteroids
(inflammatory mediators).
Trendelenburg position or
supine position. O2 prn. IV
NS or LR.
**Most severe complication
is DEATH.
Chapter 6 Shock 107
hypovolemic & febrile
response.
******************************************************************************************************************************
Blood: Bacteremia Pulmonary: Pneumonia Surgical wounds
Bone: Osteomyelitis Invasive Lines: Caths, IVs UTIS
Cardiovascular: endocarditis, pericarditis Soft tissue: Cellulitis & Wound
CNS: meningitis Intra-abdominal: diverticulitis, Appendicitis
You might also like
- Fluid and Electrolytes for Nursing StudentsFrom EverandFluid and Electrolytes for Nursing StudentsRating: 5 out of 5 stars5/5 (12)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Chart of Neuro DisordersDocument1 pageChart of Neuro DisordersNursingSchoolNotes100% (2)
- EKG Crash Course NuRsing 390 SMC - 4Document57 pagesEKG Crash Course NuRsing 390 SMC - 4m1k0e100% (2)
- Week 2 Case StudyDocument8 pagesWeek 2 Case StudyMelissa Cerny100% (3)
- Med Surg Respiration-Cardiac NotesDocument11 pagesMed Surg Respiration-Cardiac Notesorganictallgirl50% (2)
- Fluid and Electrolytes - 24 Hours or Less To Absolutely Crush The NCLEX Exam!Document45 pagesFluid and Electrolytes - 24 Hours or Less To Absolutely Crush The NCLEX Exam!KingBlack Canarsie100% (2)
- Neurology Nursing Study GuideDocument19 pagesNeurology Nursing Study GuideHayleyLangley100% (5)
- Shock Comparison ChartDocument2 pagesShock Comparison Chartlinnaete88% (8)
- Med Surge 2 Mod 1 CardiacDocument13 pagesMed Surge 2 Mod 1 CardiacDirk Buckner100% (2)
- 1430 Drug CardsfinalDocument7 pages1430 Drug CardsfinalLizSherman100% (1)
- Testing - 2 NclexDocument12 pagesTesting - 2 NclexYoke W KhooNo ratings yet
- Capstone Final ExamDocument19 pagesCapstone Final ExamEileen Arboleda100% (3)
- Ekg Chart PDF 01Document5 pagesEkg Chart PDF 01YukiMaedaNo ratings yet
- Fluids and Electrolytes ConceptDocument31 pagesFluids and Electrolytes ConceptDarwin AndalNo ratings yet
- Med-Surg HESI Study GuideDocument13 pagesMed-Surg HESI Study GuideTravis Hargett93% (14)
- Nursing Pharmacology Drug Study GuideDocument15 pagesNursing Pharmacology Drug Study GuideChelsea SmithNo ratings yet
- 50 Most Commonly Prescribed MedicationsDocument2 pages50 Most Commonly Prescribed MedicationsGloryJane67% (3)
- Study Guide For Fluid and Electrolyte ImbalancesDocument5 pagesStudy Guide For Fluid and Electrolyte ImbalancesMandi Goetz HarmonNo ratings yet
- Priority Nursing ActionsDocument4 pagesPriority Nursing ActionsAnn ChenNo ratings yet
- CardioDocument7 pagesCardioGerald AndrinNo ratings yet
- Nclex NotesDocument18 pagesNclex Notesmaane1005No ratings yet
- Med Surg ATI1Document97 pagesMed Surg ATI12Ghzchapter88% (17)
- Cardiac DrugsDocument35 pagesCardiac DrugsCristina Centurion100% (3)
- DYSRHYTHMIASDocument15 pagesDYSRHYTHMIASKristine CastilloNo ratings yet
- Med Surge 2 Mod 3 Study Guide2Document21 pagesMed Surge 2 Mod 3 Study Guide2Dirk Buckner100% (4)
- Med Surg Study GuideDocument98 pagesMed Surg Study Guideprogramgrabber100% (2)
- Ati #3Document8 pagesAti #3Leah Elizabeth100% (8)
- Nero Drugs To KnowDocument14 pagesNero Drugs To KnowGina Giammalvo100% (2)
- Cardiac Study GuideDocument9 pagesCardiac Study GuideJane DiazNo ratings yet
- AntidotesDocument2 pagesAntidotesYemaya84No ratings yet
- NR 325 Endocrine System-StudentDocument41 pagesNR 325 Endocrine System-StudentJohn Mixer100% (1)
- Med Surg Final Exam MapDocument42 pagesMed Surg Final Exam MapAnais Hall-Garrison100% (1)
- A. Maternity and Newborn Medications: (MINT) MDocument4 pagesA. Maternity and Newborn Medications: (MINT) MErica Williams0% (1)
- Lab ValuesDocument3 pagesLab Valuessurviving nursing school100% (1)
- Study Guide Med Surg #1Document22 pagesStudy Guide Med Surg #1cfunk929No ratings yet
- Electrolyte ChartDocument2 pagesElectrolyte ChartJenny Varghese100% (4)
- Compressive Ati PDFDocument9 pagesCompressive Ati PDFsarahjaimeeNo ratings yet
- Rounding Rules11!3!11Document1 pageRounding Rules11!3!11Sheldon SloanNo ratings yet
- Med Surg Study GuideDocument27 pagesMed Surg Study Guidetrifecta31No ratings yet
- Med Surg Study GuideDocument24 pagesMed Surg Study Guidekylie100% (4)
- MED ATI RemediationDocument8 pagesMED ATI RemediationLarry Oliver82% (17)
- Cardiac DisordersDocument38 pagesCardiac Disordersprototypeallhell100% (1)
- Shock With Hemodynamic ChangesDocument2 pagesShock With Hemodynamic ChangesBNA_RN100% (1)
- RN Intense Remedial Packet AnswersDocument53 pagesRN Intense Remedial Packet AnswersAli Resendiz50% (4)
- Medication Work Sheet For MedSurgDocument5 pagesMedication Work Sheet For MedSurgRyanMitchell100% (2)
- ABGs Respiratory/MetabolicDocument3 pagesABGs Respiratory/MetabolicJoe B100% (1)
- Nursing NotesDocument6 pagesNursing NotesLinguumNo ratings yet
- Med Surge 2 - RESP SYSTEM NOTESDocument26 pagesMed Surge 2 - RESP SYSTEM NOTESlorrainenxumalo75% (4)
- Handout Medical-Surgical Nursing Fluid and ElectrolyteDocument13 pagesHandout Medical-Surgical Nursing Fluid and ElectrolytePaul Christian P. Santos, RN100% (10)
- OB NRSNG - Com BrainsheetsDocument4 pagesOB NRSNG - Com BrainsheetsD SchwartzlerNo ratings yet
- Chapter 35 - Ignatavicius Medical Surgical NursingDocument6 pagesChapter 35 - Ignatavicius Medical Surgical Nursinggrkpanygiri100% (4)
- Medical-Surgical Nursing 1Document28 pagesMedical-Surgical Nursing 1Maui Ting100% (1)
- A-T-I Endocrine NotesDocument3 pagesA-T-I Endocrine NotesKelseyAnnBarnesNo ratings yet
- The Nclex-Pn Cram Sheet: General Test Information Normal Lab ValuesDocument2 pagesThe Nclex-Pn Cram Sheet: General Test Information Normal Lab Valuesroboat96No ratings yet
- Hesi Test PDFDocument35 pagesHesi Test PDFAnonymous s3TzBvwS1100% (2)
- Ati Leadership Proctored Focus ReviewDocument4 pagesAti Leadership Proctored Focus ReviewVin Lorenzo Campbell100% (3)
- SDL: Common Cardiac Drugs: Deala, Donna Marie Toledo Advanced Diploma in Medical Surgical-Group 1Document13 pagesSDL: Common Cardiac Drugs: Deala, Donna Marie Toledo Advanced Diploma in Medical Surgical-Group 1Donna Deala100% (2)
- Occlusive Disorders and HFDocument4 pagesOcclusive Disorders and HFKory ChristinaNo ratings yet
- Inflammatory Cardiac DisordersDocument3 pagesInflammatory Cardiac DisordersKory ChristinaNo ratings yet
- Bio TerrismDocument4 pagesBio TerrismKory ChristinaNo ratings yet
- BurnsDocument4 pagesBurnsKory ChristinaNo ratings yet
- EARDocument6 pagesEARKory ChristinaNo ratings yet
- EYEDocument7 pagesEYEKory ChristinaNo ratings yet
- Sensory DisordersDocument2 pagesSensory DisordersKory ChristinaNo ratings yet
- Aero - 2013q2 Apu On DemandDocument32 pagesAero - 2013q2 Apu On DemandIvan MilosevicNo ratings yet
- DMSCO Log Book Vol.25 1947Document49 pagesDMSCO Log Book Vol.25 1947Des Moines University Archives and Rare Book RoomNo ratings yet
- Adverbs Before AdjectivesDocument2 pagesAdverbs Before AdjectivesJuan Sanchez PrietoNo ratings yet
- Matthew DeCossas SuitDocument31 pagesMatthew DeCossas SuitJeff NowakNo ratings yet
- Q3 Lesson 5 MolalityDocument16 pagesQ3 Lesson 5 MolalityAly SaNo ratings yet
- Jaimini Astrology and MarriageDocument3 pagesJaimini Astrology and MarriageTushar Kumar Bhowmik100% (1)
- Crystek Technology Co.,LtdDocument35 pagesCrystek Technology Co.,LtdCésar MarinNo ratings yet
- MC Donald'sDocument30 pagesMC Donald'sAbdullahWaliNo ratings yet
- What Is A Designer Norman PotterDocument27 pagesWhat Is A Designer Norman PotterJoana Sebastião0% (1)
- CAPE Env. Science 2012 U1 P2Document9 pagesCAPE Env. Science 2012 U1 P2Christina FrancisNo ratings yet
- Sample Behavioral Interview QuestionsDocument3 pagesSample Behavioral Interview QuestionssanthoshvNo ratings yet
- PCI Bank V CA, G.R. No. 121413, January 29, 2001Document10 pagesPCI Bank V CA, G.R. No. 121413, January 29, 2001ademarNo ratings yet
- Hypnosis ScriptDocument3 pagesHypnosis ScriptLuca BaroniNo ratings yet
- KBC Autumn Regatta 2023 Saturday Race ScheduleDocument2 pagesKBC Autumn Regatta 2023 Saturday Race SchedulezainNo ratings yet
- Formal Letter Format Sample To Whom It May ConcernDocument6 pagesFormal Letter Format Sample To Whom It May Concernoyutlormd100% (1)
- ED Tox PGS.2021Document4 pagesED Tox PGS.2021Jm uniteNo ratings yet
- Faiths of Eberron PDFDocument2 pagesFaiths of Eberron PDFCarrieNo ratings yet
- Pa Print Isang Beses LangDocument11 pagesPa Print Isang Beses LangGilbert JohnNo ratings yet
- Thomas Noochan Pokemon Review Final DraftDocument6 pagesThomas Noochan Pokemon Review Final Draftapi-608717016No ratings yet
- Kofax Cross Product Compatibility MatrixDocument93 pagesKofax Cross Product Compatibility MatrixArsh RashaNo ratings yet
- GE 110HP DC Trolley MotorDocument10 pagesGE 110HP DC Trolley MotorAnthony PetersNo ratings yet
- Nandurbar District S.E. (CGPA) Nov 2013Document336 pagesNandurbar District S.E. (CGPA) Nov 2013Digitaladda IndiaNo ratings yet
- 15.597 B CAT en AccessoriesDocument60 pages15.597 B CAT en AccessoriesMohamed Choukri Azzoula100% (1)
- Panera Bread Company: Case AnalysisDocument9 pagesPanera Bread Company: Case AnalysisJaclyn Novak FreemanNo ratings yet
- Chapter 15 (Partnerships Formation, Operation and Ownership Changes) PDFDocument58 pagesChapter 15 (Partnerships Formation, Operation and Ownership Changes) PDFAbdul Rahman SholehNo ratings yet
- SEW Products OverviewDocument24 pagesSEW Products OverviewSerdar Aksoy100% (1)
- QTP Common FunctionsDocument55 pagesQTP Common FunctionsAnkur TiwariNo ratings yet
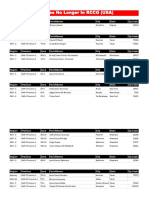
- Churches That Have Left RCCG 0722 PDFDocument2 pagesChurches That Have Left RCCG 0722 PDFKadiri JohnNo ratings yet
- BirdLife South Africa Checklist of Birds 2023 ExcelDocument96 pagesBirdLife South Africa Checklist of Birds 2023 ExcelAkash AnandrajNo ratings yet
- Purposeful Activity in Psychiatric Rehabilitation: Is Neurogenesis A Key Player?Document6 pagesPurposeful Activity in Psychiatric Rehabilitation: Is Neurogenesis A Key Player?Utiru UtiruNo ratings yet