Professional Documents
Culture Documents
Medical Care
Uploaded by
Rusty HoganOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical Care
Uploaded by
Rusty HoganCopyright:
Available Formats
Medical Care
The primary treatment of hemorrhagic shock is to control the source of bleeding as soon as
possible and to replace fluid.
In controlled hemorrhagic shock (CHS), where the source of bleeding has been occluded, fluid
replacement is aimed toward normalization of hemodynamic parameters. In uncontrolled
hemorrhagic shock (UCHS), in which the bleeding has temporarily stopped because of
hypotension, vasoconstriction, and clot formation, fluid treatment is aimed at restoration of
radial pulse or restoration of sensorium or obtaining a blood pressure of 80 mm Hg by aliquots
of 250 mL of lactated Ringer's solution (hypotensive resuscitation).
When evacuation time is shorter than 1 hour (usually urban trauma), immediate evacuation to
a surgical facility is indicated after airway and breathing (A, B) have been secured ("scoop and
run"). Precious time is not wasted by introducing an intravenous line. When expected
evacuation time exceeds 1 hour, an intravenous line is introduced and fluid treatment is started
before evacuation. The resuscitation should occur before, or concurrently with, any diagnostic
studies.
Crystalloid is the first fluid of choice for resuscitation. Immediately administer 2 L of isotonic
sodium chloride solution or lactated Ringers solution in response to shock from blood loss.
Fluid administration should continue until the patient's hemodynamics become stabilized.
Because crystalloids quickly leak from the vascular space, each liter of fluid expands the blood
volume by 20-30%; therefore, 3 L of fluid need to be administered to raise the intravascular
volume by 1 L.
Alternatively, colloids restore volume in a 1:1 ratio. Currently available colloids include human
albumin, hydroxy-ethyl starch products (mixed in either 0.9% isotonic sodium chloride solution
or lactated Ringers solution), or hypertonic saline-dextran combinations. The sole product that
is avoided routinely in large-volume (>1500 mL/d) restoration is the hydroxy-ethyl starch
product mixed in 0.9% isotonic sodium chloride solution because it has been associated with
the induction of coagulopathy. The other products have not been so implicated.
In patients with hemorrhagic shock, hypertonic saline has the theoretical benefit of increasing
intravascular volume with only small amounts of fluid. The combination of dextran and
hypertonic saline may be beneficial in situations where infusion of large volumes of fluid may
be harmful, such as in elderly persons with impaired cardiac activity. Additional trials will be
required before this combination is accepted as standard of care.
PRBCs should be transfused if the patient remains unstable after 2000 mL of crystalloid
resuscitation. For acute situations, O-negative noncrossmatched blood should be administered.
Administer 2 U rapidly, and note the response. For patients with active bleeding, several units
of blood may be necessary.
There are recognized risks associated with the transfusion of large quantities of PRBCs. As a
result, other modalities are being investigated. One such modality is hemoglobin-based oxygen
carriers (HBOC). Clinical application has been limited by its toxic effect profile. However,
research is ongoing on the use of these products.
If at all possible, blood and crystalloid infusions should be delivered through a fluid warmer. A
blood sample for type and cross should be drawn, preferably before blood transfusions are
begun. Start type-specific blood when available. Patients who require large amounts of
transfusion inevitably will become coagulopathic. FFP generally is infused when the patient
shows signs of coagulopathy, usually after 6-8 U of PRBCs. Platelets become depleted with large
blood transfusions. Platelet transfusion is also recommended when a coagulopathy develops.
In a large, comprehensive cohort study by Levi et al, placebo-controlled trials of recombinant
factor VIIIa (rFVIIa) were examined.
[2]
Off-label treatment with high doses of rFVIIa significantly
increased the risk of arterial events but not venous thromboembolic events, especially among
elderly patients.
[3]
Special concern
One situation that may arise is the transfusing of massive amounts of blood products into a
Jehovah's Witness. This error occurs on occasion. Despite acting in the patient's best interest
(prior to knowing that the patient would not want a blood transfusion), this error is a major
incident for the patient. In this situation, honesty with the patient and the family member(s) is
the rule. Involve the hospital's risk manager early. Family conferencing with a clergy member
sometimes is helpful as well.
Sumber : Hemorrhagic Shock Treatment & Management
(Author: John Udeani, MD, FAAEM; Chief Editor: John Geibel, MD, DSc, MA)
Diunduh melalui : http://emedicine.medscape.com/article/432650-treatment
Perawatan Medis
Penanganan utama syok hemoragik adalah untuk mengontrol sumber perdarahan secepat mungkin dan
untuk menggantikan cairan.
Pada syok hemoragik terkontrol (CHS), di mana sumber perdarahan telah tersumbat, penggantian cairan
ditujukan terhadap normalisasi parameter hemodinamik. Pada syok hemoragik tidak terkendali (UCHS),
di mana pendarahan untuk sementara dihentikan karena hipotensi, vasokonstriksi, dan pembentukan
bekuan, pengobatan cairan ditujukan untuk pemulihan denyut nadi radial atau restorasi sensorium atau
mendapatkan tekanan darah 80 mm Hg oleh aliquot 250 mL larutan Laktat Ringer (resusitasi hipotensif).
Ketika waktu evakuasi yang lebih pendek dari 1 jam (biasanya trauma perkotaan), evakuasi segera ke
fasilitas bedah diindikasikan setelah jalan napas dan pernapasan (A, B) telah diamankan ("sendok dan
lari"). Waktu yang berharga tidak terbuang dengan memperkenalkan jalur intravena. Ketika waktu
evakuasi diharapkan melebihi 1 jam, jalur intravena diperkenalkan dan pengobatan cairan dimulai
sebelum evakuasi. Resusitasi harus terjadi sebelum, atau bersamaan dengan, setiap studi diagnostik.
Kristaloid adalah cairan pilihan pertama untuk resusitasi. Segera mengelola 2 L larutan natrium klorida
isotonik atau larutan Ringer laktat dalam menanggapi shock dari kehilangan darah. Pemberian cairan
harus terus sampai hemodinamik pasien menjadi stabil. Karena kristaloid cepat bocor dari ruang
vaskuler, setiap liter cairan memperluas volume darah sebesar 20-30%, karena itu, 3 L cairan perlu
diberikan untuk meningkatkan volume intravaskular oleh 1 L.
Atau, koloid mengembalikan volume dalam rasio 1:1. Koloid Saat ini tersedia meliputi albumin, produk
manusia hidroksi-etil pati (dicampur baik 0,9% isotonik larutan natrium klorida atau larutan Ringer
laktat), atau kombinasi garam hipertonik-dekstran. Satu-satunya produk yang dihindari secara rutin
dalam volume besar (> 1500 mL / d) restorasi merupakan produk pati hidroksi-etil dicampur dalam 0,9%
isotonik larutan natrium klorida karena telah dikaitkan dengan induksi koagulopati. Produk lainnya
belum begitu terlibat.
Pada pasien dengan syok hemoragik, salin hipertonik memiliki manfaat teoritis meningkatkan volume
intravaskular dengan hanya sejumlah kecil cairan. Kombinasi dekstran dan salin hipertonik mungkin
bermanfaat dalam situasi di mana infus volume besar cairan mungkin berbahaya, seperti pada orang tua
dengan aktivitas jantung terganggu. Percobaan tambahan akan diperlukan sebelum kombinasi ini
diterima sebagai standar perawatan.
PRC harus ditransfusikan jika pasien tetap tidak stabil setelah pemberian 2000 mL resusitasi kristaloid.
Untuk situasi akut, darah noncrossmatched O-negatif harus diberikan. Administer 2 U cepat, dan
perhatikan respon. Untuk pasien dengan perdarahan aktif, beberapa unit darah mungkin diperlukan.
Ada risiko yang diakui terkait dengan transfusi dalam jumlah besar PRC. Akibatnya, modalitas lain
sedang diselidiki. Salah satu modalitas tersebut adalah pembawa oksigen berbasis hemoglobin (HBOC).
Aplikasi klinis telah dibatasi oleh profil efek racunnya. Namun, masih dalam tahap penelitian.
Jika memungkinkan, darah dan infus kristaloid harus diberikan melalui cairan hangat. Sampel darah
untuk jenis harus diperiksa, sebaiknya sebelum transfusi darah dimulai. Mulai golongan darah tertentu
bila tersedia. Pasien yang memerlukan sejumlah besar transfusi pasti akan menjadi coagulopathic. FFP
umumnya diresapi ketika pasien menunjukkan tanda-tanda koagulopati, biasanya setelah 6-8 U PRC.
Trombosit menjadi habis dengan transfusi darah besar. Transfusi trombosit juga dianjurkan saat
koagulopati berkembang.
Dalam sebuah studi, besar kohort komprehensif oleh Levi et al, uji coba terkontrol plasebo rekombinan
faktor VIIIA (rFVIIa) diperiksa. Pengobatan dengan dosis tinggi rFVIIa secara signifikan meningkatkan
risiko kejadian trombormboli arteri tetapi tidak pada vena, khususnya di antara pasien lanjut usia.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
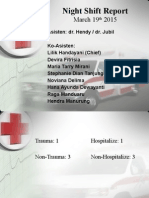
- NIGHT SHIFT REPORT OPTIMIZED TITLEDocument52 pagesNIGHT SHIFT REPORT OPTIMIZED TITLEAnastasia FebriantiNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 3333Document9 pages3333Rusty HoganNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Osteoporosis in AthletesDocument9 pagesOsteoporosis in AthletesRusty HoganNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- 2010 CPR Guidelines Released by The American Heart AssociationDocument2 pages2010 CPR Guidelines Released by The American Heart AssociationRusty HoganNo ratings yet
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Although Shock Has Been Recognised For Over 100 YearsDocument4 pagesAlthough Shock Has Been Recognised For Over 100 YearsRusty HoganNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Bahan Referat Miocardial Stunning 1-s2.0-S0914508710000080-MainDocument8 pagesBahan Referat Miocardial Stunning 1-s2.0-S0914508710000080-MainviniganorNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- 111111111Document12 pages111111111Rusty HoganNo ratings yet
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- 111111111Document12 pages111111111Rusty HoganNo ratings yet
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- 3333Document9 pages3333Rusty HoganNo ratings yet
- 3333Document9 pages3333Rusty HoganNo ratings yet
- 3333Document9 pages3333Rusty HoganNo ratings yet
- RRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRDocument9 pagesRRRRRRR RRRRRRR RRRRRRR RRRRRRR RRRRRRRRusty HoganNo ratings yet
- 1211111111111111111111111112Document9 pages1211111111111111111111111112Rusty HoganNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)