Professional Documents
Culture Documents
Age Related in Stroke
Uploaded by
AlpascaFirdaus0 ratings0% found this document useful (0 votes)
33 views9 pagesStroke
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentStroke
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
33 views9 pagesAge Related in Stroke
Uploaded by
AlpascaFirdausStroke
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 9
Journal of Clinical Epidemiology 56 (2003) 479486
Age-related changes in risk factor effects on the incidence of
thromboembolic and hemorrhagic stroke
Robert D. Abbott
a,b,c,e,
*
, J. David Curb
b,c,e
, Beatriz L. Rodriguez
b,c,e
, Kamal H. Masaki
b,c,e
,
Jordan S. Popper
b,e
, G. Webster Ross
b,c,d,e
, Helen Petrovitch
b,c,d,e
a
Division of Biostatistics and Epidemiology, University of Virginia School of Medicine, Charlottesville, Virginia 22908, USA
b
Pacic Health Research Institute, 846 S. Hotel Street, Suite 303, Honolulu, Hawaii 96813, USA
c
Department of Medicine, John A. Burns School of Medicine, University of Hawaii, 1356 Lusitana Street, 7th Floor, Honolulu, Hawaii 96813, USA
d
Department of Veterans Affairs, PO Box 50188, Honolulu, Hawaii 96850, USA
e
The Honolulu Heart Program and the HonoluluAsia Aging Study, Kuakini Medical Center, 347 N. Kuakini Street, Honolulu, Hawaii 96817, USA
Received 27 November 2001; received in revised form 9 May 2002; accepted 18 November 2002
Abstract
We examined the changes in risk factor effects on the incidence of thromboembolic and hemorrhagic stroke as they may occur with
age. Findings were based on repeated risk factor measurements at four examinations over a 26-year period in 7589 men in the Honolulu
Heart Program. After each examination, 6 years of follow-up were available to assess risk factor effects on the incidence of stroke over
a broad range of ages (4593 years). As compared with normotensive men, the risk of thromboembolic stroke in the presence of hypertension
declined from a 7-fold excess in men aged 45 to 54 years to a 1.4-fold excess in men aged 75 (P .001). Adverse effects of diabetes
and atrial brillation seemed to be equally important across all ages, whereas a protective effect of physical activity increased with age.
Except for men with atrial brillation, the incidence of thromboembolic stroke increased signicantly with age regardless of risk factor
status, including men with normal blood pressure (P .001). Although hemorrhagic events were less common, positive relations with
cigarette smoking seemed to strengthen with age, whereas those with hypertension tended to decline. Our ndings suggest that strategies
for the prevention of stroke may need to account for changes in risk factor effects as they occur with age. Control of diabetes and the
encouragement of active lifestyles in the elderly seem to be especially important.
2003 Elsevier Inc. All rights reserved.
Keywords: Stroke; Thromboembolic; Hemorrhagic; Risk factors; Aging
1. Introduction
Rapid increases in the risk of stroke and changes in
the prevalence and distribution of important risk factors
are known to occur with advancing age [111]. Whether
these age-related effects alter the association between a risk
factor and stroke is not clear. It may be that the association
between stroke and some risk factors remains constant re-
gardless of age, whereas the importance of other risk factors
declines or increases from middle adulthood to late life. In
addition, if stroke risk factors become sufciently pervasive
in the elderly population, the identication of independent
effects on the risk of stroke could become difcult. The
purpose of this report is to examine the way in which risk
factor effects on the incidence of thromboembolic and
* Corresponding author. University of Virginia Health System, Depart-
ment of Health Evaluation Sciences, P.O. Box 800717, Charlottesville, VA
22908-0717. Tel.: 434-924-1687; fax: 434-924-8437.
E-mail address: rda3e@virginia.edu (R.D. Abbott).
0895-4356/03/$ see front matter
2003 Elsevier Inc. All rights reserved.
doi: 10.1016/S0895-4356(02)00611-X
hemorrhagic stroke can change over a broad range of ages
from middle adulthood to late life in men enrolled in the
Honolulu Heart Program.
2. Methods
2.1. Study background
From 1965 to 1968, the Honolulu Heart Program began
following 8006 men of Japanese ancestry living on the island
of Oahu, Hawaii for the development of coronary heart
disease and stroke [12,13]. At the time of study enroll-
ment, participants received a complete physical examination
when they were aged 45 to 68 years. Procedures were
in accordance with institutional guidelines and approved by
an institutional review committee. Informed consent was
obtained from the study participants.
Information on cardiovascular events that occurred after
the baseline examination was obtained through a comprehen-
sive system of surveillance of hospital discharges, death
R.D. Abbott et al. / Journal of Clinical Epidemiology 56 (2003) 479486 480
certicates, autopsy records, and at repeat examinations
given in the course of follow-up. For this report, subjects were
followed for the rst occurrence of a thromboembolic or
hemorrhagic stroke.
2.2. Diagnosis of stroke
A diagnosis of stroke was made when a neurologic decit
was accompanied by blood in the cerebrospinal uid or by
evidence of an infarct or hemorrhage. Subjects were fol-
lowed for the rst occurrence of a fatal or nonfatal thrombo-
embolic or hemorrhagic stroke. Possible strokes (neurologic
decits lasting at least 24 hours but less than 2 weeks or of
unknown duration) were not included among the stroke
events because of a lack of diagnostic certainty. Subjects who
experienced focal neurologic episodes attributed to other
conditions (e.g., blood dyscrasias, neoplastic disease, head
injury, surgical accident, meningoencephalitis, fat embolism,
epilepsy, or cardiac arrest) were not included among the
victims of stroke.
A stroke was considered thromboembolic if the focal
neurologic decit occurred usually without prolonged un-
consciousness, nuchal rigidity, fever, pronounced leukocyto-
sis, or blood in the spinal uid. Identication of hemorrhagic
stroke was based on a focal neurologic decit accompanied
by loss of consciousness, headache, and blood present in
the spinal uid obtained by an atraumatic lumbar puncture
or on the basis of computerized tomography or surgical
ndings. All diagnoses were reviewed and conrmed by a
study neurologist and the Honolulu Heart Program Morbid-
ity and Mortality Review Committee.
Only men who were free from coronary heart disease
and stroke at the time of study enrollment were considered
for follow-up for a future stroke event. Prevalent coronary
heart disease was dened to include angina pectoris, coro-
nary insufciency, and unequivocal ndings of a myocardial
infarction. The nal sample size included 7589 men. Further
details on the diagnosis of coronary heart disease and stroke
are provided in earlier publications [1315].
2.3. Collection of risk factor information
Risk factor information included hypertensive status, total
cholesterol level, diabetes, body mass index (BMI) (kg/
m
2
), cigarette smoking status, alcohol intake (oz/mo), and
physical activity. Risk factor measurements were made at
the time of study enrollment (19651968) and updated
at physical examinations that occurred at 6 (19711974),
15 (19801982), and 26 (19911993) years into follow-up.
Approximately 90% and 80% of the surviving members of
the original Honolulu Heart Program cohort participated in
the 6th and 26th year anniversary examinations, respectively.
The examination that occurred 15 years into follow-up in-
cluded a randomsample of men who were selected to partici-
pate in the Cooperative Lipoprotein Phenotyping Study [16].
Among the risk factors considered in this report, hyper-
tension was dened as systolic or diastolic blood pressures
160 and 95 mm Hg, respectively, or based on the use of
antihypertensive medication. To be considered normoten-
sive, systolic and diastolic blood pressures needed to be
140 and 90 mm Hg, respectively. Men who were neither
normotensive nor hypertensive were classied as having
borderline hypertension. Study participants were also classi-
ed as having diabetes on the basis of a medical history
(physician-diagnosed or based on the reported use of insulin
or the receipt of oral hypoglycemic therapy).
Assessment of overall metabolic output during a typical
24-hour period used the physical activity index, which is a
weighted average of the number of hours spent per day in
ve different activity levels (basal, sedentary, slight, moder-
ate, and heavy). In addition to the Honolulu Heart Program
[17,18], the same index has been usedin the Framingham[19]
and Puerto Rico [20] heart studies and is known to be in-
versely related to the risk of coronary heart disease and
stroke. The physical activity index was derived at all exami-
nations except the examination that occurred 6 years into
follow-up (19711974). Removing physical activity in this
report does not change the associations that were observed
between the other factors and the risk of stroke. High-density
lipoprotein cholesterol, serum glucose, triglycerides, and
other risk factors were not examined because they were
measured too infrequently during the course of follow-up
to enable an assessment of their effects across a broad range
of ages. Further description of the risk factors is provided
elsewhere [2123].
2.4. Statistical methods
To assess the effects of a risk factor on the incidence of
stroke, proportional hazards regression models were used
[24]. Although such models allow for the adjustment of
other factors, they also allow for the effect of a risk factor
to vary with time as risk factors become updated with age.
Risk factors were also compared across 10-year age ranges
based on standard analysis of covariance methods [25]. All
reported P values were based on two-sided tests of sig-
nicance.
In general, the examination cycles used in this report
were undertaken at least 6 years apart. As a result, four
6-year, non-overlapping and conditionally independent
[26,27] follow-up periods could be created after each risk
factor update. No subjects were followed for longer than 6
years, nor was there overlap with subsequent periods of
follow-up. Follow-up for the last period (which began from
19911993) was available to 1998. For this latter period,
follow-up was available for nearly 6 years. Curtailing follow-
up to shorter 5-year periods had only negligible effects on
the reported ndings.
Follow-up was further restricted to men who were free
of knowncoronaryheart diseaseandstroke at the beginningof
each period. With each risk factor modeled as a time-varying
covariate, subjects could contribute up to four 6-year person
intervals. The intervals of follow-up were pooled to enable
R.D. Abbott et al. / Journal of Clinical Epidemiology 56 (2003) 479486 481
the calculationof 6-year incidence rates of stroke accordingto
an updated age. This allowed for the calculation of incidence
rates across a broad range of ages (4593 years) as age was
updated from the time of study enrollment (19651968) to
the examination that occurred 26 years later (19911993).
Such pooling permitted an assessment of risk factor effects
on stroke as they might change with increasing age. Here,
cross-product terms between a risk factor and age as a contin-
uous variable were modeled. Tests for interaction between a
risk factor and age on the risk of stroke as both variables
were updated with time were then based on the estimated
regression coefcients and standard errors that were associ-
ated with these terms.
3. Results
Among the 7589 men free of stroke and coronary heart
disease at the time of study enrollment, there were 18,070
6-year person intervals of follow-up. The overall average
age at the beginning of the follow-up intervals was 61
10 years (range 4593 years). Across the combined person
intervals, 396 strokes were observed (21.9/1000 in 18,070
intervals at risk of disease). The average time to a stroke
event was 3.0 1.7 years (range 0.16 years). Among
the strokes, 276 were thromboembolic (15.3/1000), 96 were
hemorrhagic (5.3/1000), and the remaining 24 were of un-
known origin.
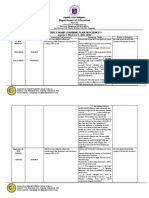
Table 1 further describes the 6-year incidence of each
stroke subtype and all strokes combined according to age.
For each event, the 6-year incidence increased consistently
with age (P .001). For all strokes combined, the incidence
observed in men aged 45 to 54 years (9.0/1000) was doubled
at ages 55to64years (17.8/1000) andmorethantripledat ages
65 to 74 (33.4/1000). For men aged 75 to 93 years, there
was more thana 5-foldexcess of stroke (48.1/1000) relative to
the youngest men. Similar magnitudes of increase occurred
for thromboembolic and hemorrhagic events.
Table 2 provides data on average risk factor values that
were observed at the beginning of the 6-year intervals of
follow-up, also according to age when such data were mea-
sured. Signicant associations were observed between the
Table 1
Six-year incidence (rate/1000) of thromboembolic and hemorrhagic
stroke according to age
Six-year incidence of stroke (rate/1000)
a
Six-year
person
intervals Thromboembolic Hemorrhagic All
Age, y at risk stroke stroke strokes
4554 5430 6.6 (36)
b
2.4 (13) 9.0 (49)
5564 6972 11.5 (80) 5.0 (35) 17.8 (124)
6574 3358 24.1 (81) 7.4 (25) 33.4 (112)
7593 2310 34.2 (79) 10.0 (23) 48.1 (111)
Overall 18,070 15.3 (276) 5.3 (96) 21.9 (396)
a
Incidence of each stroke event increased signicantly with advancing
age (P .001).
b
Number of events.
risk factor levels and age. The strongest associations seemed
to occur for men who were hypertensive when follow-up
began. Of those men who were aged 45 to 54 years, 20.6%
were hypertensive, whereas in the oldest group of men,
the percentage was more than doubled (53.1%, P .001).
Although atrial fibrillation was less common in this cohort
of Japanese-American men, the percentage of men with atrial
brillation increased consistently with age (P .001).
Although the frequency of diabetes seemed to increase with
age as well (P .001), the greatest increase occurred after
age 54. Differences in alcohol consumption were modest in
men 75 years of age and increased in those who were
older. Risk factors that declined with age included total
cholesterol, BMI, cigarette smoking, and the physical activ-
ity index. The latter changes occurred consistently with
advancing age (P .001).
The crude 6-year incidence of thromboembolic stroke
(rate/1000) is given in Table 3 within risk factor and selected
age stratum. Tests of signicance were based on proportional
hazards regression models. Except for men with atrial -
brillation, stroke incidence increased signicantly with age
within each risk factor stratum. Further adjustment for
the other risk factors (including BMI) failed to alter these
ndings.
Although the risk of stroke tended to rise with increasing
hypertension severity within each age stratum, associations
weakened signicantly with advancing age (P .001). The
effects of cigarette smoking on the risk of stroke also seemed
to weaken with age. In contrast, the effect of atrial brillation
on the risk of stroke seemed to be strongest in men 65 years
versus men who were younger. The interaction between
age and atrial brillation was not statistically signicant
(P .404); however, this could be the consequence of lim-
ited statistical power due to the infrequency of atrial brilla-
tion that was observed within all age strata (Table 2).
Although a protective effect of physical activity on the risk
of stroke seemed unclear or modest within each age group,
when modeled as a continuous risk factor, inverse associa-
tions increased signicantly with age (P .046). The protec-
tive effect of physical activity on the risk of stroke became
statistically signicant in men 75 years (P .032).
The adverse effect of total cholesterol on the risk of stroke
was strongest inmenaged55to74years where large increases
in morbidity and mortality from stroke begin to occur. By
age 75, the relation was absent. For diabetes, whereas associ-
ations with stroke were signicant for men 55 years, the
risk of stroke was fairly constant across all age strata. Men
with diabetes tended to have twice the risk of stroke as
compared with men without diabetes.
Similar data on the effect of age, hypertension, total cho-
lesterol, cigarette smoking, and alcohol intake on the risk
of hemorrhagic stroke are described in Table 4. Within all
risk factor strata, except for hypertensive men and men
with total cholesterol levels 200 mg/dL, stroke incidence
increased signicantly with age. After adjusting for the other
R.D. Abbott et al. / Journal of Clinical Epidemiology 56 (2003) 479486 482
Table 2
Average cardiovascular risk factors according to age
Age, y
Risk factor 4554 5564 6574 7593
Borderline hypertensive, %
a
17.3 18.4 21.2 19.4
Hypertensive, %
a
20.6 29.9 41.4 53.1
Total cholesterol, mg/dL
b
219 38
c
216 38 207 35 190 34
Diabetes, %
a
8.5 13.0 14.5 12.2
Atrial brillation, %
a
0.3 0.5 1.3 2.8
Body mass index, kg/m
2
24.1 3.1 23.7 3.1 23.4 3.1 23.1 3.2
Cigarette smoker, %
b
47.8 38.2 23.2 7.4
Alcohol intake, oz/mo
a
14.9 25.3 14.1 24.9 14.6 30.6 18.3 37.6
Physical activity index
b
32.9 4.8 32.6 4.3 31.6 4.1 30.6 4.4
a
Signicant increase with advancing age (P .001).
b
Signicant decline with advancing age (P .001).
c
Mean standard deviation.
risk factors (including diabetes, BMI, and the physical activ-
ity index), the effects of age on the risk of hemorrhagic
stroke remained statistically signicant only for men with
borderline hypertension (P .008) and for consumers of
alcohol (P .048).
As with thromboembolic stroke, the positive relation be-
tween hypertension and hemorrhagic events seemed to
weaken with age (P .040). In contrast to thromboembolic
events, elevated total cholesterol seemed to be protective
against hemorrhagic stroke up until age 75. Assessments
of interactions and quadratic effects were not statistically
signicant. In addition, the association between cigarette
smoking and hemorrhagic stroke seemed to strengthen with
advancing age. In men aged 75 to 93, there was nearly a
4-fold excess of hemorrhagic events in men who smoked
cigarettes (P .006). Men who drank alcohol were also at
an increased risk of hemorrhagic stroke versus nondrinkers
at all ages, but in men 75 years of age, the effects
became insignicant.
Figs. 1and2 tendtoconrmthe reported ndings in Tables
3 and 4 after risk factor adjustment. The relative risk of
thromboembolic stroke in hypertensive versus normotensive
men declined with advancing age (P .001), whereas the
protective effect of physical activity tended to increase
(P .027) (Fig. 1). Although the positive effect of diabetes
on promoting stroke seemed to be strongest in men aged 75
to 93, relative risks were similar across all ages. Declines
in the association between cigarette smoking and the risk
of thromboembolic stroke were modest (P .591).
For hemorrhagic stroke (Fig. 2), additional risk factor
adjustment removedanyapparent interactioneffect betweena
risk factor and age on the risk of a hemorrhagic event. Upper
condence limits for hypertension and alcohol intake are
not provided in instances where they are quite high and
their contribution to the patterns of association in Fig. 2 are
inconsequential. For all age ranges up to 75 years, hyperten-
sion continued to be signicantly associated with an
increased risk of hemorrhagic stroke. At 75 years, it was
not. Cigarette smoking in men 75 to 93 of age also was
signicantly related to an increased risk of stroke, whereas it
was weak in younger men (75). Only for men aged 65 to
74 years was alcohol drinking related to an increased risk
of hemorrhagic stroke (P .047).
4. Discussion
Common risk factors for cardiovascular disease undergo
rapid changes in frequency and distribution with advancing
age. Diabetes may be one of the most important risk factors
that continue to have a consistent relation with the risk of
thromboembolic stroke throughout life. Attention to the risk
of an embolic event due to atrial brillation is also critical
because of the large increases in stroke incidence that can be
attributed to this condition [28,29]. As noted in an earlier
report from the Honolulu Heart Program (and based on
longer follow-up), physically active lifestyles in older middle
age seem to be protective against stroke, and current ndings
suggest that this effect extends to the elderly population
[18]. Cigarette smoking has also long been known to promote
thromboembolic and hemorrhagic events, and although it
becomes a less common habit with advancing age, its effects
on hemorrhagic events persists [30].
In contrast, rates of hypertension increase rapidly with
age, although its effect on stroke seems to decline. This does
not imply that treating hypertension to reduce the risk of
stroke in the elderly population is less important than in
those who are younger. Rather, it is the more powerful effect
of age on promoting disease in normotensive individuals
that seems to diminish the perception that treating hyperten-
sion has health benets with advancing age. In conjunc-
tion with the low percentage of normotensive elderly men
and the increased risk of stroke that occurs naturally with
advancing age, demonstration that hypertension has an effect
on the risk of stroke becomes more difcult in older men than
in those who are younger. In the Honolulu Heart Program,
for men aged 75 to 93 years, nearly 75% were borderline
hypertensive or hypertensive. Over half had hypertension.
Unfortunately, the effects of other important risk factors
on cardiovascular disease could also become harder to mea-
sure in the elderly population because of the pervasiveness
R.D. Abbott et al. / Journal of Clinical Epidemiology 56 (2003) 479486 483
Table 3
Six-year incidence (rate/1000) of thromboembolic stroke according
to age and risk factor status
Age, y
Test for
Risk factor 4554 5564 6574 7593 trend
Hypertension
Normotensive 2.7 4.7 19.1 28.4 0.001
a
Borderline 5.3 17.2 15.5 26.8 0.002
Hypertensive 19.7 19.7 33.1 40.0 0.001
Test for trend 0.001
b
0.001 0.017 0.195 0.001
c
Total cholesterol
200 mg/dL 6.0 10.3 16.4 38.3 0.001
200239 mg/dL 7.1 11.4 27.0 29.5 0.001
240 mg/dL 6.8 13.9 37.0 32.7 0.001
Test for trend 0.425 0.030 0.003 0.287 0.591
Diabetes
Absent 6.2 10.2 22.0 29.1 0.001
Present 10.8 19.8 36.9 71.2 0.001
Test for risk 0.250 0.012 0.042 0.001 0.584
factor effect
Atrial brillation
Absent 6.5 11.4 22.5 31.5 0.001
Present 71.4 27.8 139.5 114.8 0.165
Test for risk 0.015 0.839 0.001 0.001 0.404
factor effect
Cigarette smoker
Nonsmoker 3.2 7.9 18.5 32.1 0.001
Smoker 10.4 17.3 40.3 31.8 0.001
Test for risk 0.002 0.001 0.001 0.915 0.470
factor effect
Physical activity
index
30 8.1 13.3 29.4 40.5 0.001
3033 5.1 13.6 20.6 17.1 0.004
33 7.0 14.4 24.4 28.3 0.001
Test for trend 0.363 0.782 0.211 0.032 0.046
a
P value for testing changes in the risk of stroke with increasing age.
b
Pvalue for testing changes in the risk of stroke across risk factor strata.
c
P value for testing differences in risk factor effects on the risk of
stroke with increasing age.
of the risk factor. It may be that in such situations, experience
from studies of therapies and risk factors in younger cohorts
could have relevance in older individuals where the absence
of a risk factor is uncommon.
Findings fromthe FraminghamStudy and an earlier report
from Honolulu further indicate that, although the percentage
of thromboembolic strokes that are attributed to hypertension
declines with age, the percentage attributed to atrial brilla-
tion increases with age [28,29]. Although hypertension and
atrial brillation increase in prevalence with advancing age,
the strength of the association between atrial brillation and
a thromboembolic event seems to be stronger than it does
for hypertension. Although screening and treatment for hy-
pertension and atrial brillation is important, the impact of
each on the risk of stroke undergoes important changes with
age, largely due to increases in prevalence that are excessive
for hypertension but relatively modest for atrial brillation.
In the Honolulu sample, the effect of age on the risk of
stroke was least apparent when atrial brillation was present
(as compared with other risk factors), which is a possible
consequence of more direct mechanisms that link atrial -
brillation to embolic outcomes.
Such ndings are difcult to interpret because stroke
susceptibility could still reect a dynamic process with
changing vulnerabilities to changes in risk factor exposures
that occur with age or with the risk factors themselves. Com-
plex associations between hypertension and cardiovascular
morbidity and mortality with advancing age have also been
described elsewhere [3138]. Effects of hypertension could
be operating in competition with other inuences that un-
dergo rapid gains in frequency as aging occurs. Stroke sus-
ceptibility in the elderly population may be a sign of
accumulated vascular damage or weakening that has accrued
throughout middle and later adulthood. Others have sug-
gested that mid-life risk factors that promote atherosclerosis
may have lasting importance with advancing age. Investiga-
tors from the Atherosclerotic Risk in Communities Study
suggest that hypercholesterolemia, hypertension, and the use
of cigarettes in middle adulthood may have residual effects on
the development of subclinical atherosclerosis in later life
[39]. In the Framingham Study, carotid stenosis in men
whose average age was 75 years had less of an associa-
tion with late-life cholesterol levels as compared with con-
centrations measured earlier [40]. Recent data from the
Honolulu Heart Program further question the need to lower
cholesterol to excessively low concentrations in the elderly
population [41]. With regard to coronary heart disease, data
from Hawaii suggest that desirable cholesterol levels in the
elderly population may not be a marker of a healthy risk
Table 4
Six-year incidence (rate/1000) of hemorrhagic stroke according to
age and risk factor status
Age, y
Test for
Risk factor 4554 5564 6574 7593 trend
Hypertension
Normotensive 1.2 0.8 2.4 6.3 0.005
a
Borderline 1.1 5.5 5.6 11.2 0.006
Hypertensive 7.2 12.0 12.9 11.4 0.379
Test for trend 0.003
b
0.001 0.003 0.357 0.040
c
Total cholesterol
200 mg/dL 4.2 6.6 10.3 12.8 0.002
200239 mg/dL 1.3 2.9 6.2 3.1 0.080
240 mg/dL 2.0 5.8 1.8 13.1 0.072
Test for trend 0.047 0.074 0.036 0.373 0.226
Cigarette smoker
Nonsmoker 1.8 3.3 5.9 8.2 0.001
Smoker 3.1 7.9 11.7 31.8 0.001
Test for risk 0.326 0.009 0.093 0.006 0.412
factor effect
Alcohol drinker
Nondrinker 1.7 2.2 3.2 6.7 0.039
Drinker 2.7 6.4 9.7 12.6 0.001
Test for trend 0.005 0.001 0.014 0.975 0.030
a
P value for testing changes in the risk of stroke with increasing age.
b
Pvalue for testing changes in the risk of stroke across risk factor strata.
c
P value for testing differences in risk factor effects on the risk of
stroke with increasing age.
R.D. Abbott et al. / Journal of Clinical Epidemiology 56 (2003) 479486 484
Fig. 1. Estimated relative risk of thromboembolic stroke with advancing age comparing hypertensive men with normotensive men, diabetic men with
nondiabetic men, cigarette smokers with nonsmokers, and men in the top versus bottom tertiles of the physical activity index. Relative risk estimates have
been adjusted for each of the other risk factors, including BMI and alcohol intake.
factor prole, particularly if past cholesterol levels were
high [42].
Risk factors that increase rapidly in frequency with ad-
vancing age, such as lowankle/brachial blood pressure index
(ABI) (0.9), could be one sign of an accumulation of a
lifetime of generalized vascular damage. As opposed to an
isolated single risk factor effect that might be more important
in younger years and where vascular disease may be less
apparent, a lowABI in late life could reect systemic damage
from a variety of sources that include hypertension, diabetes,
and past cigarette smoking [43]. In the elderly population,
carry-over effects from past cigarette smoking and adverse
lipid proles may be harder to measure by screening for
risk factors that exist in late life, particularly in subjects who
were once heavy smokers or in those who experienced
large reductions in total cholesterol with advancing age. In
the Honolulu Heart Program, the prevalence of an ABI 0.9
was observed in 6.3% of men aged 71 to 74 years and in
more than 25% in men older than 85 years [43]. Low ABI
was also signicantly related to the risk of stroke in men
without hypertension or diabetes and in noncigarette smok-
ers [43].
Although hypertension is thought to be the primary risk
factor for stroke, data from the Honolulu Heart Program
R.D. Abbott et al. / Journal of Clinical Epidemiology 56 (2003) 479486 485
Fig. 2. Estimated relative risk of hemorrhagic stroke with advancing age comparing hypertensive men with normotensive men, men with total cholesterol
levels at 240 versus 200 mg/dL, smokers with nonsmokers, and alcohol drinkers with nondrinkers. Relative risk estimates have been adjusted for each of
the other risk factors, including diabetes, BMI, and the physical activity index.
suggest that its role as a marker for disease may become
less clear as an independent risk factor with advancingage but
no less important as a condition in need of prevention and
treatment. Consistent risk factor effects on the risk of stroke
include the effects of diabetes and atrial brillation, but
these and other classic risk factors do not seem to account for
the increasing incidence of thromboembolic stroke that
occurs with advancing age in men with normal blood pres-
sures. Other factors not available in the current study could
gain in importance and may eventually equal or exceed the
impact that hypertensionhas onthe riskof stroke inthe elderly
population. The current ndings that active lifestyles are
associated with a reduced risk of stroke in the elderly popula-
tion, combined with earlier reports that describe the health
benets of walking in nonsmoking retired men, suggest that
encouraging active lifestyles in older individuals warrants
special emphasis [44,45].
Acknowledgments
This study was supported by the National Heart, Lung,
and Blood Institute (contract NO1-HC-05102 and grant
U01-HL-56274), the National Institute on Aging (contract
R.D. Abbott et al. / Journal of Clinical Epidemiology 56 (2003) 479486 486
NO1-AG-4-2149), and by the American Heart Association
of Hawaii (grant HIGS-16-97).
References
[1] American Heart Association. Heart and stroke facts. Dallas: American
Heart Association National Center; 1992.
[2] Burt VL, Cutler JA, Higgins M, et al. Trends in the prevalence,
awareness, treatment and control of hypertension in the adult US
population: data from the health examination surveys, 1960 to 1991.
Hypertension 1995;26:609.
[3] Joint National Committee on Prevention. Detection, evaluation and
treatment of high blood pressure. Arch Intern Med 1997;157:241346.
[4] Harris MI, Flegal KM, Cowie CC, et al. Prevalence of diabetes,
impaired fasting glucose, and impaired glucose tolerance in U.S.
adults: the Third National health and Nutrition Examination Survey,
19881994. Diabetes Care 1998;21:51824.
[5] Cornoni-Huntley JC, Harris TB, Everett DF, et al. An overview of
body weight of older persons, including the impact on mortality: The
National Health and Nutrition Examination Survey I: epidemiologic
follow-up study. J Clin Epidemiol 1991;44:74353.
[6] Ferrara A, Barrett-Conner E, Shan J. Total, LDL, and HDL cholesterol
decrease with age in older men and women: the Rancho Bernardo
Study 19841994. Circulation 1997;96:3743.
[7] Wilson PWF, Anderson KM, Harris T, et al. Determinants of change
in total cholesterol and HDL-C with age: the Framingham Study. J
Gerontol Med Sci 1994;49:2527.
[8] Wilson PWF, Hoeg JM, DAgostino RB, et al. Cumulative effects of
high cholesterol levels, high blood pressure, and cigarette smoking
on carotid stenosis. N Engl J Med 1997;337:51622.
[9] Hershcopf RJ, Elahi D, Andes R, et al. Longitudinal study in serum
cholesterol in man: an epidemiologic search for an etiology. J Chron
Dis 1982;35:10114.
[10] Weijenberg MP, Feskens EJM, Kromhout D. Age-related changes in
total and high-density-lipoprotein cholesterol in elderly Dutch men.
Am J Public Health 1996;86:798803.
[11] Abbott RD, Yano K, Hakim AA, et al. Changes in total and high-
density lipoprotein cholesterol over 10- and 20-year periods (The
Honolulu Heart Program). Am J Cardiol 1998;82:1728.
[12] Kagan A, Harris BR, Winkelstein Jr W, et al. Epidemiologic studies
of coronary heart disease and stroke in Japanese men living in Japan,
Hawaii and California: demographic, physical, dietary, and biochemi-
cal characteristics. J Chron Dis 1974;27:34564.
[13] Yano K, Reed DM, McGee DL. Ten-year incidence of coronary heart
disease in the Honolulu Heart Program: relationship to biologic and
lifestyle characteristics. Am J Epidemiol 1984;119:65366.
[14] Kagan A, Popper JS, Rhoads GG. Factors related to stroke incidence
in Japanese men: the Honolulu Heart Study. Stroke 1980;11:1421.
[15] Kagan A, Popper J, Reed DM, et al. Trends in stroke incidence and
mortality in Hawaiian Japanese men. Stroke 1994;25:11705.
[16] Castelli WP, Cooper GR, Doyle JT, et al. Distribution of triglyceride
and total LDLand HDLcholesterol in several populations: the Coopera-
tive Lipoprotein Phenotyping Study. J Chron Dis 1977;30:14769.
[17] Donahue RP, Abbott RD, Reed DM, et al. Physical activity and
coronary heart disease in middle-aged and elderly men: the Honolulu
Heart Program. Am J Public Health 1988;78:6835.
[18] Abbott RD, Rodriguez BL, Burchel CM, et al. Physical activity in
older middle-aged men and reduced risk of stroke: the Honolulu Heart
Program. Am J Epidemiol 1994;139:88193.
[19] Kannel WB, Sorlie PD. Some health benets of physical activity: the
Framingham Study. Arch Intern Med 1979;139:85761.
[20] Garcia-Palmieri MR, Costas R, Cruz-Vidal M, et al. Increased physi-
cal activity: a protective factor against heart attack in Puerto Rico.
Am J Cardiol 1982;50:74955.
[21] Yano K, Reed DM, Curb JD, et al. Biological and dietary correlates
of plasma lipids in elderly Japanese men in Hawaii. Arteriosclerosis
1986;6:42233.
[22] Roberston TL, Kato H, Rhoads GG, et al. Epidemiologic studies of
coronary heart disease and stroke in Japanese men living in Japan,
Hawaii, and California: incidence of myocardial infarction and death
from coronary heart disease. Am J Cardiol 1977;39:23943.
[23] Knutsen R, Knutsen SF, Curb JD, et al. The incidence of coronary
heart disease in the Honolulu Heart Program. J Clin Epidemiol
1988;41:293302.
[24] Cox DR. Regression models and life tables. J R Stat Soc 1972;
34:187202.
[25] Lane PW, Nelder JA. Analysis of covariance and standardization as
instances of prediction. Biometrics 1982;38:61321.
[26] Wu M, Ware J. On the use of repeated measurements in regression
analysis with dichotomous responses. Biometrics 1979;35:51321.
[27] Abbott RD. Logistic regression in survival analysis. Am J Epide-
miol 1985;121:46571.
[28] Wolf PA, Abbott RD, Kannel WB. Atrial brillation as an independent
risk factor for stroke: the Framingham Study. Stroke 1991;22:9837.
[29] Curb JD, Abbott RD, MacLean CJ, et al. Age-related changes in
stroke risk in men with hypertension and normal blood pressure.
Stroke 1996;27:81924.
[30] Abbott RD, Yin Y, Reed DM, et al. Risk of stroke in male cigarette
smokers. N Engl J Med 1986;315:71720.
[31] Taylor JO, Cornoni-Huntley J, Curb JD, et al. Blood pressure and
mortality in the elderly. Am J Epidemiol 1991;134:489501.
[32] Mattila K, Haavisto M, Rajala S, et al. Blood pressure and survival
in the very old. BMJ 1988;296:8879.
[33] Langer RD, Ganiats TG, Barrett-Connor E. Paradoxical survival of
elderly men with high blood pressure. BMJ 1989;298:13568.
[34] Staessen J, Bulpitt C, Clement D, et al. Relation between mortality
and treated blood pressure in elderly patients with hypertension: report
of the European Working Party on High Blood Pressure in the Elderly.
BMJ 1989;298:15526.
[35] Coope J, Warrender TS, McPherson K. The prognostic signicance
of blood pressure in the elderly. J Hum Hypertens 1988;2:7988.
[36] Siegel D, Kuller L, Lazarus NB, et al. Predictors of cardiovascular
events and mortality in the Systolic Hypertension in the Elderly Pilot
Project. Am J Epidemiol 1987;126:38599.
[37] Lindholm L, Lanke J, Bengtsson B. U-shaped association between
mortality and blood pressure in a thirteen year prospective study. Fam
Pract 1986;3:38.
[38] Abbott RD, Curb JD, Rodriguez BL, et al. Age-related changes
in risk factor effects on the incidence of coronary heart disease. Ann
Epidemiol 2002;12:17381.
[39] Nieto FJ, Diez-Roux A, Szklo M, et al. Short- and long-term predic-
tion of clinical and subclinical atherosclerosis by traditional risk
factors. J Clin Epidemiol 1999;52:55967.
[40] Wilson PWF, Hoeg JM, DAgostino RB, et al. Cumulative effects of
high cholesterol levels, high blood pressure, and cigarette smoking
on carotid stenosis. N Engl J Med 1997;337:51622.
[41] Schatz IJ, Masaki K, Yano K, et al. Cholesterol and all-cause mortality
in elderly people from the Honolulu Heart Program: a cohort study.
Lancet 2001;358:3515.
[42] Hakim AA, Curb JD, Burchel CM, et al. Screening for coronary
heart disease in elderly men based on current and past cholesterol
levels. J Clin Epidemiol 1999;52:125765.
[43] Abbott RD, Rodriguez BL, Petrovitch H, et al. Ankle/brachial blood
pressure in elderly men and the risk of stroke: the Honolulu Heart
Program. J Clin Epidemiol 2001;54:538.
[44] Hakim AA, Petrovitch H, Burchel CM, et al. Effects of walking on
mortality among nonsmoking retired men. N Engl J Med 1998;
338:949.
[45] Hakim AA, Curb JD, Petrovitch H, et al. Effects of walking on
coronary heart disease in elderly men: the Honolulu Heart Program.
Circulation 1999;100:913.
Reproducedwith permission of thecopyright owner. Further reproductionprohibited without permission.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hypertension in 2017-What Is The Right Target JAMA 2017Document2 pagesHypertension in 2017-What Is The Right Target JAMA 2017JulianNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Dexa On PneumoniaDocument9 pagesDexa On PneumoniaAlpascaFirdausNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Otolaryngology - Head and Neck Surgery-2015 - Rhinitis AllergicDocument43 pagesOtolaryngology - Head and Neck Surgery-2015 - Rhinitis AllergicAlpascaFirdausNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Sinonasal CADocument9 pagesSinonasal CAAlpascaFirdausNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Forensic ToxicologyDocument11 pagesForensic ToxicologySeptiandry Ade PutraNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- KuesionerDocument121 pagesKuesionerAlpascaFirdaus100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Food Poison ColoradoDocument4 pagesFood Poison ColoradoAlpascaFirdausNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- 2014 AHA-ACC-HRS Guidelines For The Management of Patients With Atrial Fibrillation PDFDocument76 pages2014 AHA-ACC-HRS Guidelines For The Management of Patients With Atrial Fibrillation PDFEvi Furi AmaliaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Food Poisoning Fact FileDocument8 pagesFood Poisoning Fact FileAlpascaFirdausNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- FoodPoisoning HealthsafetyDocument4 pagesFoodPoisoning HealthsafetyMerlinda Juwita SimanjuntakNo ratings yet
- Pat Tho GenesisDocument22 pagesPat Tho GenesisAlpascaFirdausNo ratings yet
- Book Chapter1 - Singh and Pandey 2011Document18 pagesBook Chapter1 - Singh and Pandey 2011AlpascaFirdausNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Who Water Distribution Guideline PDFDocument157 pagesWho Water Distribution Guideline PDFmukundisoNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Sinonasal CarcinomaDocument14 pagesSinonasal CarcinomaAlpascaFirdausNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- APS & ThrombosisDocument4 pagesAPS & ThrombosisAlpascaFirdausNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- HRS-D Depression Scale AssessmentDocument0 pagesHRS-D Depression Scale AssessmentMohsin YounisNo ratings yet
- Uterine Fibroid PDFDocument12 pagesUterine Fibroid PDFAlpascaFirdausNo ratings yet
- Pharmaceuticals 02 00082Document12 pagesPharmaceuticals 02 00082AlpascaFirdausNo ratings yet
- APS & ThrombosisDocument4 pagesAPS & ThrombosisAlpascaFirdausNo ratings yet
- Antiphospholipid SyndromeDocument12 pagesAntiphospholipid SyndromebebekbebekNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Drug-Induced Liver Injury (DILI) : Lana L. Pauls, MPH John R. Senior, MDDocument45 pagesDrug-Induced Liver Injury (DILI) : Lana L. Pauls, MPH John R. Senior, MDAnonymous 7Zz526No ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Arterial Stiffness High Risk CV Patient Habitual Carbo IntakeDocument8 pagesArterial Stiffness High Risk CV Patient Habitual Carbo IntakeAlpascaFirdausNo ratings yet
- Lexicon Psychiatric & Mental Helath TermsDocument112 pagesLexicon Psychiatric & Mental Helath TermsAlpascaFirdausNo ratings yet
- Laboratory Tests For Respiratory ModifDocument23 pagesLaboratory Tests For Respiratory ModifAlpascaFirdausNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Fluids & Electrolytes GuideDocument37 pagesFluids & Electrolytes GuideAlpascaFirdausNo ratings yet
- Terapia Insulinica en Pacientes Criticos.Document9 pagesTerapia Insulinica en Pacientes Criticos.pagra7128No ratings yet
- ElectrolyteDocument8 pagesElectrolyteAlpascaFirdausNo ratings yet
- JURNAL Penyalahgunaan InhalanDocument9 pagesJURNAL Penyalahgunaan InhalanAlpascaFirdausNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- 2011 WHO Progress Report On MDRTB and XDRTBDocument127 pages2011 WHO Progress Report On MDRTB and XDRTBChikezie OnwukweNo ratings yet
- DVTDocument4 pagesDVTAli AlisonNo ratings yet
- Oup Accepted Manuscript 2020Document6 pagesOup Accepted Manuscript 2020JuniorMartinsNo ratings yet
- Soya BeanDocument10 pagesSoya BeanPoonga KNo ratings yet
- Qneibi Unr 0139M 11521Document88 pagesQneibi Unr 0139M 11521Hazem AlmasryNo ratings yet
- LMS - Well Cardio Activ Presentation PDFDocument7 pagesLMS - Well Cardio Activ Presentation PDFRanjit MeenaNo ratings yet
- Jiang 2022 J. Phys. Conf. Ser. 2181 012055Document5 pagesJiang 2022 J. Phys. Conf. Ser. 2181 012055محمد عبدالحميد القرشيNo ratings yet
- CPG Management of Ischaemic Stroke 3rd Edition 2020 v20210228Document156 pagesCPG Management of Ischaemic Stroke 3rd Edition 2020 v20210228Nabilah HariffNo ratings yet
- PRIME Nitric Oxide Activator - QivanaDocument12 pagesPRIME Nitric Oxide Activator - QivanaNikolas SeveridtNo ratings yet
- Curier Med Pag 51 PDFDocument80 pagesCurier Med Pag 51 PDFJardan TatianaNo ratings yet
- The Feasibility of MalunggayDocument31 pagesThe Feasibility of MalunggayRohi100% (2)
- ULANGANDocument2 pagesULANGANari phalosaNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Natural PharmacyDocument1,681 pagesThe Natural Pharmacypragerspole100% (5)
- What Is Saturated FatDocument12 pagesWhat Is Saturated FatAbhi kashyapNo ratings yet
- Two-Day Meal Plan For Type II Diabetic and Cardiovascular PatientDocument11 pagesTwo-Day Meal Plan For Type II Diabetic and Cardiovascular Patientapi-301376054No ratings yet
- 5 PGDMLT McqsDocument7 pages5 PGDMLT McqsTeamGGxKick EsportsNo ratings yet
- NOAA Medical Standards Procedures ManualDocument70 pagesNOAA Medical Standards Procedures ManualPatricio Toledo FuenzalidaNo ratings yet
- New England Journal Medicine: The ofDocument12 pagesNew England Journal Medicine: The ofPabellón 4No ratings yet
- Sag 47 3 42 1503 90Document6 pagesSag 47 3 42 1503 90TanveerNo ratings yet
- sb5 End of Unit Test-HigherDocument8 pagessb5 End of Unit Test-HigherDelosh T0% (2)
- Journal of Advanced Research: Usama A.A. Sharaf El Din, Mona M. Salem, Dina O. AbdulazimDocument12 pagesJournal of Advanced Research: Usama A.A. Sharaf El Din, Mona M. Salem, Dina O. AbdulazimNorman RiyadiNo ratings yet
- Part B Responding To Cooccurring ConditionsDocument231 pagesPart B Responding To Cooccurring ConditionsGiorilliNo ratings yet
- Avtand Lcstudent Sleep and Its Association With Physical ActivityDocument18 pagesAvtand Lcstudent Sleep and Its Association With Physical Activityapi-271276388No ratings yet
- 16 Vascular Diseases of Nervous System-QDocument24 pages16 Vascular Diseases of Nervous System-QAdi PomeranzNo ratings yet
- HAADStatisticsEng2013 PDFDocument91 pagesHAADStatisticsEng2013 PDFHitesh MotwaniiNo ratings yet
- February Health Programs CalendarDocument29 pagesFebruary Health Programs CalendarTeanu Jose Gabrillo TamayoNo ratings yet
- Gestational Hypertension - UTD PDFDocument21 pagesGestational Hypertension - UTD PDFShahar Perea ArizaNo ratings yet
- Merck Geriatrics 3rd Ed PDFDocument603 pagesMerck Geriatrics 3rd Ed PDFMihaela Cosmina Niculescu100% (1)
- Why Animals Dont Get Heart Attacks Book Matthias Rath PDF (Pauling-Rath Therapy Protocol Vitamin C / Lysine)Document320 pagesWhy Animals Dont Get Heart Attacks Book Matthias Rath PDF (Pauling-Rath Therapy Protocol Vitamin C / Lysine)Anonymous Jap77xvqPKNo ratings yet
- Science9 Reyes, J, P Q1.W2Document12 pagesScience9 Reyes, J, P Q1.W2Jeane Pineda ReyesNo ratings yet
- Health Related Fitness: Bunggo National High SchoolDocument19 pagesHealth Related Fitness: Bunggo National High SchoolJeslie Madrigal SagsagatNo ratings yet
- Organisational Structure StudyDocument46 pagesOrganisational Structure StudyChing SantiagoNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyFrom EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyRating: 5 out of 5 stars5/5 (1)
- Power Souping: 3-Day Detox, 3-Week Weight-Loss PlanFrom EverandPower Souping: 3-Day Detox, 3-Week Weight-Loss PlanRating: 3.5 out of 5 stars3.5/5 (3)
- Ultrametabolism: The Simple Plan for Automatic Weight LossFrom EverandUltrametabolism: The Simple Plan for Automatic Weight LossRating: 4.5 out of 5 stars4.5/5 (28)
- Your Health Destiny: How to Unlock Your Natural Ability to Overcome Illness, Feel Better, and Live LongerFrom EverandYour Health Destiny: How to Unlock Your Natural Ability to Overcome Illness, Feel Better, and Live LongerNo ratings yet
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeFrom EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNo ratings yet
- The Fast800 Diet: Discover the Ideal Fasting Formula to Shed Pounds, Fight Disease, and Boost Your Overall HealthFrom EverandThe Fast800 Diet: Discover the Ideal Fasting Formula to Shed Pounds, Fight Disease, and Boost Your Overall HealthRating: 5 out of 5 stars5/5 (37)
- Allen Carr's Easy Way for Women to Lose Weight: The original Easyway methodFrom EverandAllen Carr's Easy Way for Women to Lose Weight: The original Easyway methodRating: 4.5 out of 5 stars4.5/5 (18)
- Glucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingFrom EverandGlucose Goddess Method: A 4-Week Guide to Cutting Cravings, Getting Your Energy Back, and Feeling AmazingRating: 5 out of 5 stars5/5 (59)