Professional Documents
Culture Documents
Hernia Jur Nal 2000
Uploaded by
Hevi Eka Tarsum0 ratings0% found this document useful (0 votes)
23 views12 pagesThis randomized controlled trial compared suture repair versus mesh repair for incisional hernias among 200 patients. It found significantly lower recurrence rates with mesh repair compared to suture repair, both for primary hernias (27% vs. 47% at 3 years) and recurrent hernias (22% vs. 55% at 3 years). Risk factors for recurrence included suture repair, infection, prostatism in men, and prior surgery for abdominal aortic aneurysm. The size of the hernia did not affect recurrence rates. The study concluded that mesh repair is superior to suture repair for reducing hernia recurrence.
Original Description:
journal
Copyright
© © All Rights Reserved
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis randomized controlled trial compared suture repair versus mesh repair for incisional hernias among 200 patients. It found significantly lower recurrence rates with mesh repair compared to suture repair, both for primary hernias (27% vs. 47% at 3 years) and recurrent hernias (22% vs. 55% at 3 years). Risk factors for recurrence included suture repair, infection, prostatism in men, and prior surgery for abdominal aortic aneurysm. The size of the hernia did not affect recurrence rates. The study concluded that mesh repair is superior to suture repair for reducing hernia recurrence.
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
23 views12 pagesHernia Jur Nal 2000
Uploaded by
Hevi Eka TarsumThis randomized controlled trial compared suture repair versus mesh repair for incisional hernias among 200 patients. It found significantly lower recurrence rates with mesh repair compared to suture repair, both for primary hernias (27% vs. 47% at 3 years) and recurrent hernias (22% vs. 55% at 3 years). Risk factors for recurrence included suture repair, infection, prostatism in men, and prior surgery for abdominal aortic aneurysm. The size of the hernia did not affect recurrence rates. The study concluded that mesh repair is superior to suture repair for reducing hernia recurrence.
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 12
Volume 343:392-398 August 10, 2000Number 6
A Comparison of Suture Repair with Mesh Repair
for Incisional Hernia
Roland W. Luijendijk, M.D., Ph.D., Wim C.J. Hop, Ph.D., M. Petrousjka van
den Tol, M.D., Diederik C.D. de Lange, M.D., Marijel M.J. raaksma, M.D.,
Jan !.M. "J#ermans, M.D., Ph.D., Roelo$ %. oelhou&er, M.D., Ph.D., as C.
de 'ries, M.D., Ph.D., Mar( ).M. *alu, M.D., Ph.D., Ja(k C.J. Wereldsma,
M.D., Ph.D., Cornelis M.+. ruijnin(k,, M.D., Ph.D., and Johannes Jeekel,
M.D., Ph.D.
ABSTRACT
Background Incisional hernia is an important complication of
abdominal surgery.
Procedures for the repair of these hernias
with sutures and with mesh have been
reported, but there is
no consensus about which type of procedure is best.
Methods Between March 1992 and ebruary 199!, we performed a
multicenter
trial in which we randomly assigned to suture repair
or mesh repair 2"" patients
who were scheduled to undergo repair
of a primary hernia or a first recurrence of
hernia at the site
of a vertical midline incision of the abdomen of less than #
cm in
length or width. $he patients were followed up by physical
e%amination at 1, #,
12, 1!, 2&, and '# months. (ecurrence rates
and potential ris) factors for
recurrent incisional hernia were
analy*ed with the use of life+table methods.
Results ,mong the 1-& patients with primary hernias and the
2. patients with
first+time recurrent hernias who were eligible
for the study, -# had recurrences
during the follow+up period.
$he three+year cumulative rates of recurrence among
patients
who had suture repair and those who had mesh repair were &'
percent
and 2& percent, respectively, with repair of a primary
hernia /P0"."21 difference,
19 percentage points1 9- percent
confidence interval, ' to '- percentage points2.
$he recurrence
rates were -! percent and 2" percent with repair of a first
recurrence of hernia /P0".1"1 difference, '! percentage points1
9- percent
confidence interval, 31 to .! percentage points2.
$he ris) factors for recurrence
were suture repair, infection,
prostatism /in men2, and previous surgery for
abdominal aortic
aneurysm. $he si*e of the hernia did not affect the rate of
recurrence.
Conclusions ,mong patients with midline abdominal incisional
hernias, mesh
repair is superior to suture repair with regard
to the recurrence of hernia,
regardless of the si*e of the hernia.
Incisional hernia is a frequent complication of abdominal surgery.
In prospective studies
with sufficient follow-up, primary incisional
hernia occurred in 11 to 20 percent of
patients who had undergone
laparotomy.
1,2,3
uch hernias can cause serious morbidity,
such
as incarceration !in " to 1# percent of cases$
%,#
and strangulation
!in 2 percent$.
%
If the
hernia is not reduced promptly, small
bowel that is strangulated in the hernia may
become ischemic
and necrotic and perforation may ultimately occur. <hough
many
techniques of repair have been described, the results are
often disappointing. &fter
primary repair, rates of recurrence
range from 2% percent to #% percent.
%,",',(,)
*epairs that
include
the use of mesh to close the defect have better but still high
recurrence rates, up to
3% percent.
(,10
&fter repair of recurrent
incisional hernias, recurrence rates of up to %(
percent have
been reported.
#
+hese studies of suture repairs and mesh repairs,
however,
were either uncontrolled or nonrandomi,ed, and it remains
uncertain whether mesh repair
is superior to suture repair.
+o define the indications for the use of mesh materials, we
undertoo- a randomi,ed, multicenter study of patients with midline
abdominal incisional
hernias.
Methods
Stud !esign
.etween /arch 1))2 and 0ebruary 1))(, we randomly assigned 200
adult patients who
were scheduled to undergo repair of a primary
hernia or a first recurrence of hernia at
the site of a vertical
midline incision to suture repair or mesh repair, after stratification
according to the type of hernia and the hospital. +he preoperative
length or width of the
fascial defect was not to e1ceed " cm,
and patients could be enrolled only once. 21clusion
criteria
were the presence of more than one hernia, signs of infection,
prior hernia repair
with mesh, and plans to repair the hernia
as part of another intraabdominal procedure.
+he study was approved
by the ethics committees of the participating hospitals, and
all
the patients gave informed consent after a physician told
them about the details of the
trial.
+he patient-related factors of se13 age3 presence or absence
of obesity, cough,
constipation, prostatism, diabetes mellitus,
glucocorticoid therapy3 smo-ing status3 and
abdominal surgical
history were recorded. 4besity was defined as a body-mass inde1
!the
weight in -ilograms divided by the square of the height
in meters$ of at least 30. 0actors
related to the operation,
including the surgical technique and the presence or absence
of
hematoma, dehiscence, and infection, were also analy,ed.
5ound infection was defined
by the discharge of pus from the
wound, evaluated up to the one-month visit. 5e also
recorded
factors related to the hernia, such as whether the hernia was
primary or a first
recurrence, the preoperative and intraoperative
si,e of the hernia, and the e1act location
of the hernia !the
upper median, 3 cm or less pro1imal or distal to the umbilicus,
or the
lower median$.
&t the onset of anesthesia, a cephalosporin was administered
intravenously. In the patients
assigned to undergo repair with
sutures, the two edges of the fascia were appro1imated in
the
midline, usually with a continuous polypropylene suture !6rolene
no. 1, 2thicon,
&mersfoort, the 7etherlands$ with stitch widths
!tissue bites$ and intervals of
appro1imately 1 cm. In the patients
assigned to undergo repair with use of mesh, the
dorsal side
of the fascia ad8acent to the hernia was freed from the underlying
tissue by at
least % cm. & polypropylene mesh !/arle1 9.ard
.enelu1, 7ieuwegein, the 7etherlands:
or 6rolene$ was tailored
to the defect so that at least 2 to % cm of the mesh overlapped
the
edges of the fascia, and the mesh was sutured to the bac-
of the abdominal wall 2 to % cm
from the edge of the defect
with a continuous suture !6rolene no. 1$. +o minimi,e contact
between the mesh and the underlying organs, any peritoneal defect
was closed or the
omentum was sutured in between. 5hen this
could not be done, a polyglactin )10
!;icryl, 2thicon$ mesh
was fi1ed in between. +he fascial edges were not closed over
the
prosthesis unless a completely tension-free repair could
be performed. <rainage and
closure of the subcutis and closure
of the cutis were optional. +he duration of surgery and
the
hospital stay was noted.
+he patients were evaluated by physicians 1, ", 12, 1(, 2%,
and 3" months after surgery.
6atients= awareness of any recurrence
of the hernia and concern about the scar were
noted. 5hen patients
were as-ed whether they had pain, their responses were recorded
as
simply >yes> or >no.> +he scar was e1amined for recurrence
of hernia, which was
defined as any fascial defect that was
palpable or detected by ultrasound e1amination and
was located
within ' cm of the site of hernia repair. +he e1amination included
palpation
while the patient was in the supine position with
legs e1tended and raised. ?ltrasound
e1aminations were performed
only when physical e1aminations were not definitive.
Statisti"al Analsis
6ercentages and continuous variables were compared with the
use of 0isher=s e1act test
and the /ann@5hitney test,
respectively. +he cumulative percentages of patients with
recurrences
over time were calculated and compared with use of Aaplan@/eier
curves
and log-ran- tests. /ultivariate analysis of various
factors was performed with Bo1
regression analysis. +hrough
the use of appropriate interaction terms, we investigated
whether
the effect of treatment depended on the si,e of the repaired
hernia. &ll statistical
tests were two-sided. +he primary analysis
was performed on an intention-to-treat basis3
that is, patients
remained in their assigned group even if during the procedure
the surgeon
8udged the patient not to be suitable for the technique
assigned. & per-protocol analysis,
which e1cluded patients with
ma8or protocol violations, was also performed.
Results
&mong the 200 patients enrolled in the study, 1'1 had a primary
incisional hernia, and
2) had a first recurrence of incisional
hernia. eventeen patients in the former group and
two in the
latter group were found to be ineligible for the study, for
the following reasonsC
no incisional hernia was evident intraoperatively
!nine patients$, the operation was
canceled !five patients$,
no follow-up data were obtained !three patients$, hernia repair
was part of another procedure !one patient$, or herniation was
too close to an
enterostomy for the specified procedure to be
performed !one patient$. &t base line, the
patients assigned
to the mesh-repair group were slightly younger and had a higher
frequency of past surgery for abdominal aortic aneurysm, whereas
there were more
patients with prostatism in the suture-repair
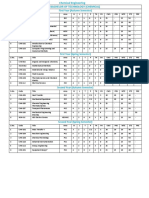
group !+able 1$.
Vie# this
table:
9in this
window:
9in a new
window:
$able 1% .ase-Dine Bharacteristics of the 6atients with Incisional
&ernia, &ccording to tudy Eroup.
+he recurrence rates for the two groups, subdivided according
to whether the patients had
a primary hernia or a first recurrence,
are shown in +able 2. &mong the patients with
primary hernias,
(0 were assigned to suture repair and '% to mesh repair !( with
an
additional polyglactin )10 9;icryl: mesh$. +he mean duration
of follow-up was 2"
months !range, 1 to 3"$ for patients without
recurrence and was similar for both treatment
groups. +hirty-two
patients !1" in each group$ were lost to follow-upC ' patients
died
!none within 1 month after surgery$3 # underwent further
surgery through the repair at a
later date3 1 moved abroad3
and 1) did not appear at their ne1t appointment for various
reasons, such as wor- or immobility !mean follow-up, 10 months$.
+hese 32 patients
were included in the analysis, but follow-up
data were censored at the time of their last
contact with the
investigators or at the time of reoperation.
Vie# this
table:
9in this
window:
9in a new
window:
$able 2% *ates of *ecurrence &ccording to 5hether the *epaired
Incisional &ernia 5as 6rimary or a 0irst *ecurrence.
even patients assigned to the suture-repair group underwent
mesh repair, and five
patients assigned to the mesh-repair group
underwent suture repair3 one patient in each
group had a recurrence.
In all patients who had been assigned to the suture-repair group
but underwent mesh repair, the surgeon 8udged that the defect
was too large !all were
more than 3" cm
2
$ to be repaired without
adding a prosthesis for strength. 4f the patients
assigned to
the mesh-repair group who underwent suture repair, two represented
violations of the protocol and two underwent suture repair because
the surgeon deemed
the defect too small for mesh repair. In
one case the ris- of infection of the planned mesh
repair was
8udged to be high because of an inadvertent enterotomy. &mong
patients with
primary hernias, the three-year cumulative rates
of recurrence were %3 percent for those
who underwent suture
repair and 2% percent for those who underwent mesh repair
!6F0.02$
!+able 2$.
4f the patients with first recurrences, 1' were assigned to
suture repair and 10 were
assigned to mesh repair. +wo patients
assigned to the suture-repair group underwent mesh
repair because
the surgeon 8udged the defect to be too large !more than 3"
cm
2
$ for repair
without a prosthesis !one patient had a recurrence$.
+he mean duration of follow-up was
30 months !range, 1 to 3"$
for patients without recurrence and was similar for both
treatment
groups. +he three-year cumulative rates of recurrence in the
suture-repair and
mesh-repair groups were #( percent and 20
percent, respectively !6F0.10$ !+able 2$.
5hen both hernia groups were combined, the mean duration of
follow-up was 2" months
!range, 1 to 3"$ for patients without
recurrence and was similar for both treatment groups
!6F0.00#$
!+able 2 and 0igure 1$. +he three-year cumulative rates of recurrence
were %"
percent with suture repair and 23 percent with mesh
repair. In the subgroup of #0 patients
with small hernias !10
cm
2
or smaller$, the three-year cumulative rate of recurrence
after
suture repair was %% percent, as compared with " percent
in the mesh-repair group
!6F0.01$.
Vie# larger 'ersion !#A$C
9in this window:
9in a new window:
(igure 1% Aaplan@/eier Burves for *ecurrence of
&ernia after *epair of a 6rimary or 0irst *ecurrent
Incisional &ernia, &ccording to 5hether the 6atient
5as &ssigned to /esh *epair !7F(%$ or uture *epair
!7F)'$.
+here were significantly fewer recurrences in patients
who were assigned to mesh repair !6F0.00#$.
+he median duration of the operation was %# minutes !range,
1# to 13#$ for suture repair
and #( minutes !range, 1# to 1#0$
for mesh repair !6F0.0)$. +he median length of the
hospital
stay was " days !range, 1 to 3'$ for suture repair and # days
!range, 1 to 1#$ for
mesh repair !6F0.%%$.
)er-)roto"ol Analsis
In the total group of 1(1 patients, ma8or violations of the
protocol occurred in the repairs
of # patients. In one patient,
the most pro1imal of four hernias found intraoperatively was
repaired with use of a prosthesis and the other three hernias
were repaired with sutures.
In another patient, the fascial
defect was sutured under a subcutaneous mesh repair. In the
third patient, several intraoperatively discovered wea- spots
were not completely covered
by subcutaneous mesh repair !for
un-nown reasons$, ma-ing recurrence inevitable. +he
other two
patients were switched to suture repair despite the fact that
a mesh repair could
have been performed with ease, according
to the operative notes !one patient had a
recurrence$. 5ith
data on these five patients removed from the analysis, the three-year
cumulative rates of recurrence in the suture-repair group !)#
patients$ and mesh-repair
group !(1 patients$ were similar to
those in the intention-to-treat analysis G namely, %"
percent and 23 percent, respectively !6F0.00#$.
*e"urren"es a+ter ,esh *e-air
5e attempted to determine the reasons for recurrence in all
patients who underwent mesh
repair, regardless of treatment
assignment !e1cluding repairs that were deemed to reflect
ma8or
trial violations$. 6ossible e1planations were that the mesh
was attached with 2 cm
or less of overlap !five patients$, that
interrupted sutures were placed 2 cm apart !one
patient$, that
mar-ed abdominal distention occurred during the first wee- after
surgery
!one patient$, that recurrence resulted from glucocorticoid
therapy !one patient$, that it
resulted from infection of a
large hematoma !one patient$, and that the repair was
inadequate
because the patient had pain during the procedure as a result
of inadequate
epidural anesthesia !one patient$. 7o e1planation
for recurrence was found in the cases of
seven patients who
had undergone mesh repair.
Analsis o+ )rognosti" (a"tors
In the univariate analysis, prostatism !in men$, a history of
surgery for abdominal aortic
aneurysm, and infection were identified
as ris- factors for recurrence !data not shown$.
+he results
of the multivariate analysis of these factors together with
the type of repair,
age, si,e of hernia, and primary hernia
or first recurrence of hernia are shown in +able
3. In this
analysis, suture repair, infection, prostatism !in men$, and
history of surgery for
abdominal aortic aneurysm were all identified
as independent ris- factors for recurrence.
&fter ad8ustment
for the other factors, mesh repair was found to result in a
#' percent
lower rate of recurrence !)# percent confidence interval,
1) to '' percent3 6F0.00)$ than
suture repair. +he difference
in rates of recurrence between the suture-repair group and
the
mesh-repair group was not affected by the si,e of the hernia.
Vie# this
table:
9in this
window:
9in a new
window:
$able 3% *esults of /ultivariate &nalysis of 0actors &ffecting the *ates
of *ecurrence after *epair of Incisional &ernia.
.om-li"ations
4ne of the )' patients in the suture-repair group had complete
wound dehiscence after
mar-ed abdominal distention that resulted
from an ileus on the fifth day after surgery.
4ne of the (%
patients in the mesh-repair group had a recurrence associated
with intestinal
strangulation 1( months after surgery. In another
patient who underwent mesh repair,
contact with the intestines
was not adequately prevented, so one month later, at
laparotomy
performed because of a persisting ileus, two loops of small
intestine appeared
to be fi1ed to the mesh, prohibiting fecal
flow. +hree of the (% patients !% percent$ had
postoperative
infections but did not require removal of the mesh, # patients
!" percent$
had postoperative abdominal bulging, and 1 patient
!1 percent$ had postoperative
bleeding.
+he frequency of pain one month after surgery was similar in
the two treatment groups
!suture-repair group, 1) patients 920
percent:3 mesh-repair group, 1# patients 91(
percent:$. +he
pain usually disappeared after the first month. even of the
patients had
hematomas, and five had recurrent hernias. 6ostoperative
serosanguineous lea-age
occurred in three patients in the suture-repair
group and in four patients in the mesh-repair
group. &n inadvertent
enterotomy occurred in four patients !2 percent$, without later
complications. 4ther complications were suture-thread sinus
!one patient$, pneumonia
!four patients$, urinary tract infection
!three patients$, and myocardial infarction !one
patient$.
A#areness o+ *e"urren"es on the )art o+ )atients
&ll patients were as-ed before each follow-up physical e1amination
whether they had
noticed a recurrence of hernia. 4f the 13)
patients who believed they had no recurrence,
1% !10 percent$
had a recurrence, as evidenced by physical e1amination. +he
%2 patients
who believed they had a recurrence indeed had one,
as shown by e1amination. 5hen only
these self-reported recurrences
were counted, the three-year cumulative rates of
recurrence
were 3# percent for the suture-repair group and 1' percent for
the mesh-repair
group !6F0.02$.
Discussion
+he techniques used for repairing incisional hernias have generally
developed in a
practical, e1periential way. everal authors
have reported favorable results with mesh
repair,
3,(,10,11,12,13,1%,1#,1",1',1(,1)
but to date this technique has not been studied systematically.
5e now report the results of a prospective, randomi,ed, multicenter
trial in which suture
repair was compared with mesh repair3
the latter was determined to be more effective.
In techniques for the repair of incisional hernias in which
sutures are used, the edges of
the defect are brought together,
which may lead to e1cessive tension and subsequent
wound dehiscence
or incisional herniation as a result of tissue ischemia and
the cutting of
sutures through the tissues.
20
5ith prosthetic
mesh, defects of any si,e can be repaired
without tension. In
addition, polypropylene mesh, by inducing an inflammatory response,
sets up a scaffolding that, in turn, induces the synthesis of
collagen. 4ur study establishes
the superiority of mesh repair
over suture repair with regard to the recurrence of hernia.
5e too- no measures to prevent the evaluating clinicians and
patients from -nowing the
type of repair used in each case3
this might be considered a limitation of the study. +he
forms
used to record the findings of the postoperative e1aminations
did not include
information on the type of repair used, but
in 1' percent of the cases, only the surgeon
who performed the
operation evaluated the patient at follow-up. 0urthermore, in
a
thorough e1amination, the technique performed may be detected,
because after mesh
repair, a fascial rim can be palpated in
some patients with a large fascial defect.
+herefore, the e1amining
physicians may have -nown which technique was used, and
bias
on their part may have affected the outcome. However, the rate
of recurrence after
suture repair was similar to that predicted
on the basis of our previous wor-.
",21,22
&lso,
when only the
self-reported recurrences, which are li-ely to be less susceptible
to biased
ascertainment, were counted, the difference remained
significant !6F0.02$.
+he si,e of the hernia was an independent ris- factor for recurrence
in two retrospective
studies by our group, in which >appro1imating>
!edge-to-edge$ fascial repairs
",21
and
>overlapping> repairs
22
were evaluated, but not in another study.
#
In medical records,
however, the si,e of the defect is often described insufficiently,
so analyses of
retrospective data are less reliable. &lso, the
e1tent of the decrease in la1ity of the tissue
surrounding the
hernia, which is influenced by retraction of muscle and scarification
of
tissues, may be more important than the actual si,e of the
fascial defect. In this
prospective study, the si,e of the defect
was not a ris- factor for recurrence.
6atients with hernias who had undergone surgery for an abdominal
aortic aneurysm had
significantly higher recurrence rates than
patients without such a history. &n increased
frequency of primary
or recurrent inguinal and incisional hernia in patients who
have had
an aneurysm has been previously reported in some retrospective
studies but not in
others.
23,2%,2#,2",2',2(,2)
5hether an inherent
defect in healing e1ists in patients with aortic
aneurysms or
hernial disease is not -nown, but possible defects in healing
may be
e1plained by defects in collagen and elastin cross-lin-ages,
30
increased activity of elastase
with reduced content of elastin,
31
and different relative proportions of collagen
subtypes.
32,33,3%
mo-ing may also be a factor,
3#
but it was not a factor in this
study !data
not shown$.
Infection did not lead to the removal of mesh in this and most
other series,
",12,13,1#,1)
but it
was a ris- factor for recurrence.
+herefore, the administration of broad-spectrum
antibiotics
at the induction of anesthesia is recommended.
3"
4n the basis of our results, we recommend attachment of the
prosthesis to the dorsal side
of the defect with an overlap
as large as possible, and we recommend that the mesh be
sutured
to the surrounding fascia with intervals of no more than 1 to
2 cm between
stitches. .ulging must be prevented, but the mesh
should not be implanted under tension.
Bontact between the polypropylene
mesh and the viscera must be avoided because of the
ris- of
adhesions, intestinal obstruction, and fistulas.
1)
5hen the
peritoneum cannot be
closed or when omentum cannot be interposed,
polyglactin )10 !;icryl$ mesh may be
interposed to protect the
viscera,
1',3',3(
but e1perimental and clinical studies are not
conclusive with respect to the efficacy of the interposition
of the polyglactin mesh in
preventing these complications.
3(,3),%0
In conclusion, in patients with incisional hernias, retrofascial
preperitoneal repair with
polypropylene mesh is superior to
suture repair with regard to the recurrence of hernia,
even
in patients with small defects.
5e are indebted to /rs. &nne-e E. van <uuren for assistance
with data management and to the following
clinical centers and
local trial coordinators for the enrollment and follow-up of
patientsC Iie-enhuis
tuivenberg, &ntwerp, .elgium !E.6. van
der chelling, /.<.$3 tichting <eventer Iie-enhui,en, <eventer,
the 7etherlands !&.J. 0rima, /.<.$3 4osterschelde Iie-enhuis,
Eoes, the 7etherlands !B./. <i8-huis,
/.<., 6h.<.$3 tichting
Iie-enhuis &mstelveen, &mstelveen, the 7etherlands !<. van Eeldere,
/.<.,
6h.<.$3 and Holy Iie-enhuis, ;laardingen, the 7etherlands
!H.J. *ath, /.<.$.
Source Information
0rom the <epartment of 6lastic and *econstructive urgery, ?niversity Hospital ;ri8e ?niversiteit,
&msterdam !*.5.D.$3 the <epartment of 2pidemiology and .iostatistics, /edical chool, 2rasmus
?niversity, *otterdam !5.B.J.H.$3 the <epartment of Eeneral urgery, ?niversity Hospital *otterdam@
<i8-,igt, *otterdam !/.6.+., <.B.<.D., /./.J..., J.7./.IJ., J.J.$3 the <epartment of Eeneral urgery,
I-a,ia Hospital, *otterdam !*.?...$3 the <epartment of Eeneral urgery, /edisch Bentrum Haaglanden,
5esteinde Hospital, +he Hague !..B.;.$3 the <epartment of Eeneral urgery, Iuider,ie-enhuis, *otterdam
!/.A./..$3 the <epartment of Eeneral urgery, int 0ranciscus Easthuis, *otterdam !J.B.J.5.$3 and the
<epartment of Eeneral urgery, Deyenburg Iie-enhuis, +he Hague !B./.&...$ G all in the 7etherlands.
&ddress reprint requests to 6rofessor Jee-el at the <epartment of Eeneral urgery, ?niversity Hospital
*otterdam@<i8-,igt, <r. /olewaterplein %0, 301# E< *otterdam, the 7etherlands, or at spe-Khl-d.a,r.nl.
References
1. /udge /, Hughes D2. Incisional herniaC a 10 year prospective study of
incidence and attitudes. .r J urg 1)(#3'2C'0-'1.9/edline:
2. Dewis *+, 5iegand 0/. 7atural history of vertical abdominal parietal closureC
6rolene versus <e1on. Ban J urg 1)()332C1)"-200.9/edline:
3. ugerman HJ, Aellum J/ Jr, *eines H<, <e/aria 2J, 7ewsome HH, Dowry J5.
Ereater ris- of incisional hernia with morbidly obese than steroid-dependent
patients and low recurrence with prefascial polypropylene mesh. &m J urg
1))"31'1C(0-(%.9Bross*ef: 9/edline:
%. *ead *B, Loder E. *ecent trends in the management of incisional herniation.
&rch urg 1)()312%C%(#-%((.9&bstract:
#. /anninen /J, Davonius /, 6erhoniemi ;J. *esults of incisional hernia repairC a
retrospective study of 1'2 unselected hernioplasties. 2ur J urg 1))131#'C2)-31.
9/edline:
". Dui8endi8- *5. >Incisional hernia>C ris- factors, prevention, and repair. !6h.<.
thesis.$ *otterdam, the 7etherlandsC 2rasmus ?niversity *otterdam, 2000.
'. 6aul &, Aoren-ov /, 6eters , Aohler D, 0ischer , +roidl H. ?nacceptable
results of the /ayo procedure for repair of abdominal incisional hernias. 2ur J
urg 1))(31"%C3"1-3"'.9Bross*ef: 9/edline:
(. &nthony +, .ergen 6B, Aim D+, et al. 0actors affecting recurrence following
incisional herniorrhaphy. 5orld J urg 200032%C)#-101.9Bross*ef: 9/edline:
). van der Dinden 0+6/, van ;roonhoven +J/;. Dong-term results after surgical
correction of incisional hernia. 7eth J urg 1)((3%0C12'-12).9/edline:
10. Deber E2, Earb JD, &le1ander &I, *eed 56. Dong-term complications associated
with prosthetic repair of incisional hernias. &rch urg 1))(3133C3'(-3(2.
9&bstractM0ull +e1t:
11. *ives J, 6ire JB, 0lament J., 6alot J6, .ody B. De traitement des grandes
NvantrationsC nouvelles indications thNrapeutiques O propos de 322 cas. Bhirurgie
1)(#3111C21#-22#.9/edline:
12. toppa *2. +he treatment of complicated groin and incisional hernias. 5orld J
urg 1)()313C#%#-##%.9/edline:
13. ?sher 0B. &ernia repair with /arle1 meshC an analysis of #%1 cases. &rch urg
1)"23(%C32#-32(.
1%. Dichtenstein ID, hulman &E, &mid 6A. +wenty questions about hernioplasty.
&m urg 1))13#'C'30-'33.9/edline:
1#. Dia-a-os +, Aarani-as I, 6anagiotidis H, <endrinos . ?se of /arle1 mesh in the
repair of recurrent incisional hernia. .r J urg 1))%3(1C2%(-2%).9/edline:
1". .endavid *. Bomposite mesh !polypropylene-e-6+02$ in the intraperitoneal
positionC a report of 30 cases. &ernia 1))'31C#-(.
1'. toppa *, *alaimiaramanana 0, Henry P, ;erhaeghe 6. 2volution of large ventral
incisional hernia repairC the 0rench contribution to a difficult problem. &ernia
1)))33C1-3.
1(. 5ant, E2, moderator. Incisional herniaC the problem and the cure. J &m Boll
urg 1)))31((C%2)-%%'.9Bross*ef: 9/edline:
1). /orris-tiff EJ, Hughes D2. +he outcomes of nonabsorbable mesh placed within
the abdominal cavityC literature review and clinical e1perience. J &m Boll urg
1))(31("C3#2-3"'.9Bross*ef: 9/edline:
20. Eeorge B<, 2llis H. +he results of incisional hernia repairC a twelve year review.
&nn * Boll urg 2ngl 1)("3"(C1(#-1('.9/edline:
21. Hesselin- ;J, Dui8endi8- *5, de 5ilt JH5, Heide *, Jee-el J. &n evaluation of
ris- factors in incisional hernia recurrence. urg Eynecol 4bstet 1))331'"C22(-
23%.9/edline:
22. Dui8endi8- *5, Demmen /H/, Hop 5BJ, 5ereldsma JBJ. Incisional hernia
recurrence following >vest-over-pants> or vertical /ayo repair of primary hernias
of the midline. 5orld J urg 1))'321C"2-"".9Bross*ef: 9/edline:
23. Bannon <J, Basteel D, *ead *B. &bdominal aortic aneurysm, Deriche=s
syndrome, inguinal herniation, and smo-ing. &rch urg 1)(%311)C3('-3().
9&bstract:
2%. &dye ., Duna E. Incidence of abdominal wall hernia in aortic surgery. &m J urg
1))(31'#C%00-%02.9/edline:
2#. tevic- B&, Dong J., Jamasbi ., 7ash /. ;entral hernia following abdominal
aortic reconstruction. &m urg 1)((3#%C2('-2().9/edline:
2". Hall A&, 6eters ., myth H, et al. &bdominal wall hernias in patients with
abdominal aortic aneurysmal versus aortoiliac occlusive disease. &m J urg
1))#31'0C#'2-#'".9Bross*ef: 9/edline:
2'. Holland &J&, Bastleden 5/, 7orman 62, tacey /B. Incisional hernias are
more common in aneurysmal arterial disease. 2ur J ;asc 2ndovasc urg
1))"312C1)"-200.9/edline:
2(. Johnson ., harp *, +hursby 6. Incisional herniasC incidence following
abdominal aortic aneurysm repair. J Bardiovasc urg !+orino$ 1))#33"C%('-%)0.
9/edline:
2). Israelsson D&. Incisional hernias in patients with aortic aneurysmal diseaseC the
importance of suture technique. 2ur J ;asc 2ndovasc urg 1)))31'C133-13#.
9Bross*ef: 9/edline:
30. +ilson /<, <avis E. <eficiencies of copper and a compound with ion-e1change
characteristics of pyridinoline in s-in from patients with abdominal aortic
aneurysms. urgery 1)(33)%C13%-1%1.9/edline:
31. Bampa J, Ereenhalgh */, 6owell J+. 2lastin degradation in abdominal aortic
aneurysms. &therosclerosis 1)('3"#C13-21.9/edline:
32. /enashi , Bampa J, Ereenhalgh */, 6owell J+. Bollagen in abdominal aortic
aneurysmC typing, content, and degradation. J ;asc urg 1)('3"C#'(-#(2.
9Bross*ef: 9/edline:
33. Alinge ?, i IL, Iheng H, chumpelic- ;, .hardwa8 *, Alosterhalfen ..
&bnormal collagen I to III distribution in the s-in of patients with incisional
hernia. 2ur urg *es 2000332C%3-%(.9/edline:
3%. 0riedman <5, .oyd B<, 7orton 6, et al. Increases in type III collagen gene
e1pression and protein synthesis in patients with inguinal hernias. &nn urg
1))3321(C'#%-'"0.9/edline:
3#. *ead *B. /etabolic factors contributing to herniationC a review. &ernia
1))(32C#1-#.
3". ;ri8land 55, Jee-el J, teyerberg 25, <en Hoed 6+, .on8er HJ. Intraperitoneal
polypropylene mesh repair of incisional hernia is not associated with
enterocutaneous fistula. .r J urg 20003('C3%(-3#2.9Bross*ef: 9/edline:
3'. Doury J7, Bhevrel J6. +raitement des NventrationsC utilisation simultanNe du
treillis de polyglactine )10 et de dacron. 6resse /ed 1)(3312C211"-211".
3(. <asi-a ?A, 5idmann 5<. <oes lining polypropylene with polyglactin mesh
reduce intraperitoneal adhesionsQ &m urg 1))(3"%C(1'-(20.9/edline:
3). oler /, ;erhaeghe 6, 2ssomba &, evestre H, toppa *. De traitement des
Nventrations post-opNratoires par prothRse composNe !polyester - polyglactin )10$C
Ntude clinique et e1pNrimentale. &nn Bhir 1))33%'C#)(-"0(.9/edline:
%0. &mid 6A, hulman &E, Dichtenstein ID, ostrin , Loung J, Ha-a-ha /.
21perimental evaluation of a new composite mesh with the selective property of
incorporation to the abdominal wall without adhering to the intestines. J .iomed
/ater *es 1))%32(C3'3-3'#.9/edline:
You might also like
- Ann Punjab Med Coll 2009 3 1 27 31Document5 pagesAnn Punjab Med Coll 2009 3 1 27 31eka henny suryaniNo ratings yet
- Modified Rives StoppaDocument8 pagesModified Rives StoppaAndrei SinNo ratings yet
- Article. Loop Ileostomy Closure After Restorative Proctocolectomy. Outcome in 1504 Patients. 2005Document8 pagesArticle. Loop Ileostomy Closure After Restorative Proctocolectomy. Outcome in 1504 Patients. 2005Trí Cương NguyễnNo ratings yet
- Comapartion SutureDocument7 pagesComapartion SutureGuillermo Nieves PeredoNo ratings yet
- Comparison Between Tension-Free Mesh and Sutured Repair in Inguinal HerniasDocument7 pagesComparison Between Tension-Free Mesh and Sutured Repair in Inguinal HerniasAn ORdinary K-ChazwinNo ratings yet
- Umbilicalherniarepair TechniqueDocument9 pagesUmbilicalherniarepair Techniqueanz_4191No ratings yet
- Hernia IngunalisDocument7 pagesHernia IngunalisAnggun PermatasariNo ratings yet
- Huang 1984Document4 pagesHuang 1984vinicius.alvarez3No ratings yet
- VVF RepairDocument4 pagesVVF RepairAdil KhurshidNo ratings yet
- Ciencia e Technica Omentum Overlay PDFDocument10 pagesCiencia e Technica Omentum Overlay PDFAlin MihetiuNo ratings yet
- Palliative Management of Malignant Rectosigmoidal Obstruction. Colostomy vs. Endoscopic Stenting. A Randomized Prospective TrialDocument4 pagesPalliative Management of Malignant Rectosigmoidal Obstruction. Colostomy vs. Endoscopic Stenting. A Randomized Prospective TrialMadokaDeigoNo ratings yet
- Seton Treatment of Perianal Fistula With High Anal or Rectal OpeningDocument4 pagesSeton Treatment of Perianal Fistula With High Anal or Rectal Openingdidit_fajar_NNo ratings yet
- Journal Medicine: The New EnglandDocument7 pagesJournal Medicine: The New England'Muhamad Rofiq Anwar'No ratings yet
- 1 s2.0 S174391910700129X MainDocument6 pages1 s2.0 S174391910700129X MainGiorgio André Gabino GonzalezNo ratings yet
- Recurrent Groin HerniaDocument6 pagesRecurrent Groin HerniaJohn-adewaleSmithNo ratings yet
- Management of Perforated Appendicitis in Children: A Decade of Aggressive TreatmentDocument5 pagesManagement of Perforated Appendicitis in Children: A Decade of Aggressive Treatmentapi-308365861No ratings yet
- Laparoscopic Versus Open Transhiatal Esophagectomy For Distal and Junction CancerDocument6 pagesLaparoscopic Versus Open Transhiatal Esophagectomy For Distal and Junction CancerDea Melinda SabilaNo ratings yet
- Hernia Hiatal 3Document10 pagesHernia Hiatal 3María Alejandra García QNo ratings yet
- Omentum OverlayDocument10 pagesOmentum OverlayAlin MihetiuNo ratings yet
- RectopexyDocument7 pagesRectopexyInzamam Ul HaqNo ratings yet
- Ismaeil 2018Document15 pagesIsmaeil 2018Javier ZaquinaulaNo ratings yet
- Pi Is 2213576614000049Document3 pagesPi Is 2213576614000049Ditha FadhilaNo ratings yet
- EsofagusDocument7 pagesEsofagusWillie VanegasNo ratings yet
- Comparison Between On Lay and in Lay Mesh in Repair of Incisional HerniaDocument15 pagesComparison Between On Lay and in Lay Mesh in Repair of Incisional HerniaAshok kumarNo ratings yet
- Vandenheuvel 2012Document6 pagesVandenheuvel 2012Natalindah Jokiem Woecandra T. D.No ratings yet
- Complicated AppendicitisDocument4 pagesComplicated AppendicitisMedardo ApoloNo ratings yet
- Table 2 Preoperative Characteristics and Treatment of Patients Presenting With Complex Anal FistulaDocument4 pagesTable 2 Preoperative Characteristics and Treatment of Patients Presenting With Complex Anal FistulaTri Anna FitrianiNo ratings yet
- AppendicitisDocument3 pagesAppendicitisRindayu Julianti NurmanNo ratings yet
- Fistulectomy With Primary Sphincter Reconstruction: What Does This Paper Add To The Literature?Document9 pagesFistulectomy With Primary Sphincter Reconstruction: What Does This Paper Add To The Literature?miguelNo ratings yet
- Laparoscopic Appendectomy PostoperativeDocument6 pagesLaparoscopic Appendectomy PostoperativeDamal An NasherNo ratings yet
- Surgical Management of Recurrent Inguinal Hernia A Study of 50 Cases - April - 2023 - 9089115640 - 5948273Document3 pagesSurgical Management of Recurrent Inguinal Hernia A Study of 50 Cases - April - 2023 - 9089115640 - 5948273Ssam CivilNo ratings yet
- Component SeparationDocument23 pagesComponent Separationismu100% (1)
- Treatment of Anal Stenosis A 5year Revie PDFDocument3 pagesTreatment of Anal Stenosis A 5year Revie PDFJimi Kalvin SarareniNo ratings yet
- Better Orchiopexy and High Ligation 2016Document4 pagesBetter Orchiopexy and High Ligation 2016Richard QiuNo ratings yet
- New Developments in Anal Surgery Congenital Ano RectalDocument5 pagesNew Developments in Anal Surgery Congenital Ano RectalOctavianus KevinNo ratings yet
- Reflection For 79th Annual Clinical Congress 24th Asian Congress of SurgeryDocument4 pagesReflection For 79th Annual Clinical Congress 24th Asian Congress of Surgerysjmc.surgeryresidentsNo ratings yet
- Operative Management of Anastomotic Leaks After Colorectal SurgeryDocument6 pagesOperative Management of Anastomotic Leaks After Colorectal SurgeryJorge OsorioNo ratings yet
- Hernia Hiatal 2Document8 pagesHernia Hiatal 2María Alejandra García QNo ratings yet
- Anatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFDocument10 pagesAnatomy. Eight Edition. Saint Louis: Mosby.: Ped PDFannisa ussalihahNo ratings yet
- Hernia 2018Document5 pagesHernia 2018Razor GGNo ratings yet
- Pham 2020Document6 pagesPham 2020zzzNo ratings yet
- Groin Hernia: VZI, But It May Well Be That A Long Follow-UpDocument3 pagesGroin Hernia: VZI, But It May Well Be That A Long Follow-UpAnas YahyaNo ratings yet
- Vrijland Et Al-2002-British Journal of SurgeryDocument5 pagesVrijland Et Al-2002-British Journal of SurgeryTivHa Cii Mpuzz MandjaNo ratings yet
- Role of Endoscopic Stent Insertion On Managmeent of Gastric Twist After Sleeve GastrectomyDocument6 pagesRole of Endoscopic Stent Insertion On Managmeent of Gastric Twist After Sleeve GastrectomyJorge SalazarNo ratings yet
- Open Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective StudyDocument3 pagesOpen Versus Laparoscopic Mesh Repair of Ventral Hernias: A Prospective Study'Adil MuhammadNo ratings yet
- Abdelhameed Et Al (June 2019)Document6 pagesAbdelhameed Et Al (June 2019)drpklalNo ratings yet
- Surgical Management of Right Colon DiverticulitisDocument4 pagesSurgical Management of Right Colon DiverticulitisDimas De Conti GramzNo ratings yet
- International Journal of Surgery Case ReportsDocument3 pagesInternational Journal of Surgery Case Reportshussein_faourNo ratings yet
- Original Article: Burst Abdomen: Is It A Preventable Complication?Document5 pagesOriginal Article: Burst Abdomen: Is It A Preventable Complication?Melisa ClaireNo ratings yet
- Jurnal Hernia VentralisDocument10 pagesJurnal Hernia VentralisMusdalipaNo ratings yet
- PICO InvaginasiDocument4 pagesPICO InvaginasimutimutimutiNo ratings yet
- Brown 2014Document8 pagesBrown 2014nelly alconzNo ratings yet
- KuhhDocument5 pagesKuhhyetti TrisnaNo ratings yet
- Inguinal HerniaDocument9 pagesInguinal HerniaAmanda RapaNo ratings yet
- Perbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterDocument7 pagesPerbedaan Penanganan Antara Laparoskopi Vs Open Repair Pada Perforasi GasterAfiani JannahNo ratings yet
- Procedeul Lichtenstein "Tension-Free" În Tratamentul Herniei InghinaleDocument3 pagesProcedeul Lichtenstein "Tension-Free" În Tratamentul Herniei InghinaleSpecialNameNo ratings yet
- Mithun Journal-1 4Document27 pagesMithun Journal-1 4Tanuja LNo ratings yet
- PRS 0000000000001135Document5 pagesPRS 0000000000001135VanessaGGSNo ratings yet
- Case Studies of Postoperative Complications after Digestive SurgeryFrom EverandCase Studies of Postoperative Complications after Digestive SurgeryNo ratings yet
- Damage Control in Trauma Care: An Evolving Comprehensive Team ApproachFrom EverandDamage Control in Trauma Care: An Evolving Comprehensive Team ApproachJuan DuchesneNo ratings yet
- Non-Electric Septic Systems: Biorock'S New GenerationDocument5 pagesNon-Electric Septic Systems: Biorock'S New GenerationAlvin TombarevicNo ratings yet
- Department of Education: Inset Refelction Journal SY: 2020-2021Document2 pagesDepartment of Education: Inset Refelction Journal SY: 2020-2021RachelleGomezLatrasNo ratings yet
- Gazpromneft Reductor CLP - 68, 100, 150, 220, 320, 460 and 680Document2 pagesGazpromneft Reductor CLP - 68, 100, 150, 220, 320, 460 and 680Jonathan HansenNo ratings yet
- (PDF) Pass Through Panic: Freeing Yourself From Anxiety and FearDocument1 page(PDF) Pass Through Panic: Freeing Yourself From Anxiety and FearmilonNo ratings yet
- Trainee Eye 18 Spring 2023Document14 pagesTrainee Eye 18 Spring 2023MubeenRahmanNo ratings yet
- Old MacDonald LyricsDocument5 pagesOld MacDonald LyricsMarieNo ratings yet
- Yanmar Gear ManualDocument46 pagesYanmar Gear ManualCheohdez100% (2)
- Quiz 3 - Working Capital Management (WCM) - Basic Concepts WCM - Cash Management - FINANCIAL MANAGEMENT, PART IDocument16 pagesQuiz 3 - Working Capital Management (WCM) - Basic Concepts WCM - Cash Management - FINANCIAL MANAGEMENT, PART IAisah Reem100% (1)
- IIT Roorkee Programme Structure CHeDocument4 pagesIIT Roorkee Programme Structure CHeabcNo ratings yet
- 58 PDFDocument11 pages58 PDFMay MethaweeNo ratings yet
- Environmntal Internal & External IssueDocument1 pageEnvironmntal Internal & External IssueMalar KandasamyNo ratings yet
- Heavy LiftDocument31 pagesHeavy LiftFachrurrazi100% (2)
- Savio v. Peterson ComplaintDocument15 pagesSavio v. Peterson ComplaintChicago TribuneNo ratings yet
- The Best Broccoli Cheese Soup (Better-Than-Panera Copycat) - Averie CooksDocument1 pageThe Best Broccoli Cheese Soup (Better-Than-Panera Copycat) - Averie CooksEmily WillisNo ratings yet
- Valve Identifier VI-SB13-01Document5 pagesValve Identifier VI-SB13-01jcastell100No ratings yet
- SRA Proposal TemplateDocument8 pagesSRA Proposal Templatejag6215100% (1)
- Robots, Love & Sex: The Ethics of Building A Love MachineDocument12 pagesRobots, Love & Sex: The Ethics of Building A Love MachineGina SmithNo ratings yet
- Andmeleht Alpha Continuity Plus 6kW 10kWDocument2 pagesAndmeleht Alpha Continuity Plus 6kW 10kWAleksandar NikolicNo ratings yet
- WHO IMAI Acute - Care PDFDocument138 pagesWHO IMAI Acute - Care PDFJohn Philip TiongcoNo ratings yet
- 2 of Darkness and Light (The Bound and The Broken)Document651 pages2 of Darkness and Light (The Bound and The Broken)jakub.naceradskyNo ratings yet
- OPT OUT LETTER For School Surveys in Accordance With The Protection of Pupil Rights Amendment (PPRA)Document4 pagesOPT OUT LETTER For School Surveys in Accordance With The Protection of Pupil Rights Amendment (PPRA)Reclaim Oklahoma Parent EmpowermentNo ratings yet
- Cell Structure2 FDocument10 pagesCell Structure2 FFred H HalderNo ratings yet
- SingjuDocument3 pagesSingjuhbNo ratings yet
- Amazon Company HRM PolicyDocument4 pagesAmazon Company HRM Policyadeeba ghani100% (2)
- Specific Heat CapacityDocument25 pagesSpecific Heat CapacityZae ZayNo ratings yet
- The Azf Factory ExplosionDocument29 pagesThe Azf Factory ExplosionHitakshi AroraNo ratings yet
- Introduction EM Waves WorksheetDocument3 pagesIntroduction EM Waves WorksheetUmer AbdullahNo ratings yet
- Chemistry and Enzymology of Vitamin B12Document76 pagesChemistry and Enzymology of Vitamin B12prakas.rao39695No ratings yet
- Bank@Campus Account - ICICI Bank LTDDocument1 pageBank@Campus Account - ICICI Bank LTDKumar RanjanNo ratings yet
- Amtech ProDesign Product GuideDocument3 pagesAmtech ProDesign Product GuideShanti Naidu0% (1)