Professional Documents
Culture Documents
Pourguideline 1 ST
Uploaded by
api-2456727840 ratings0% found this document useful (0 votes)
120 views3 pagesOriginal Title
pourguideline1st
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
120 views3 pagesPourguideline 1 ST
Uploaded by
api-245672784Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
University of Colorado Health-Central, Unit-Based Guideline: Perioperative Services
Voiding Algorithm for Preventing Postoperative Urinary Retention (POUR)
in Phase II Patients
Approved by:
Owner: AIP PACU
Submitted by: Raelyn Nicholson, RN, BSN, PCCN
Date updated/reviewed: 4/2/2014
Perioperative Guideline Task Force review date: (PGTF will review every
two years following PPPPC)
Purpose: The purpose of this unit based guideline (UBG) is to provide the post
anesthesia nurse with clear and concise direction on preventing postoperative urinary
retention (POUR) in Phase II patients by utilizing an evidence based algorithm.
Sources:
Baldini, G., Bagry, H., Aprikian, A., & Carli, F. (2009). Postoperative urinary retention: anesthetic and
perioperative considerations. Anesthesiology, 110(5), 1139-1157.
Beatty, A.M., Martin, D.E., Couch, M., & Long, N. (1997). Relevance of oral intake an necessity to void as
ambulatory surgical discharge criteria. Journal of PeriAnesthesia Nursing, 12(6), 413-421.
Buchko, B.L. & Robinson, L.E. (2012). An evidence-based approach to decrease early post-operative
urinary retention following urogynecologic surgery. Urologic Nursing, 32(5), 260-273.
Buchko, B.L., Robinson, L.E., & Bell, T.D. (2013). Translating an evidence-based algorithm to decrease
early post-operative urinary retention after urogynecologic surgery. Urologic Nursing, 33(1), 24-32. doi:
10.7257/1053-816X2013.33.1.24
DiBlasi, S.M. (2013). Planned cesarean delivery and urinary retention associated with spinal morphine.
Journal of PeriAnesthesia Nursing, 28(3), 128-135. doi: 10.1016/j.jopan.2012.07.012
Dreijer, B., Moller, M.H., & Bartholdy, J. (2011). Post-operative urinary retention in a general surgical
population. European Journal of Anaesthesiology, 28(3), 190-194. doi: 10.1097/EJA.0b013e328341ac3b
Hansen, B.S., Soreide, E., Warland, A.M., & Nilsen, O.B. (2011). Risk factors of post-operative urinary
retention in hospitalised patients. Acta Anaesthesiologica Scandinavica, 55, 545-548. doi: 10.1111/j.1399-
6576.2011.02416.x
Feliciano, T., Montero, J., McCarthy, M., & Priester, M. (2008). A retrospective, descriptive, exploratory
study evaluating incidence of postoperative urinary retention after spinal anesthesia and its effect on PACU
discharge. Journal of PeriAnesthesia Nursing, 23(6), 394-400. doi: 10.1016/j.jopan.2008.09.006
McLeod, L., Southerland, K., & Bond, J. (2013). A clinical audit of postoperative urinary retention in the
postanesthesia care unit. Journal of PeriAnesthesia Nursing, 28(4), 210-216. doi:
10.1016/j.jopan.2013.10.0006
Warner, A.J., Phillips, S., Riske, K., Haubert, M., & Lash, N. (2000). Postoperative bladder distension:
Measurement with bladder ultrasonography. Journal of PeriAnesthesia Nursing, 15(1), 20-25.
University of Colorado Health-Central, Unit-Based Guideline: Perioperative Services
Guideline:
Postoperative urinary retention (POUR) is defined as a bladder volume greater than 400
ml and the inability to void. Signs and symptoms include: restlessness, confusion,
anxiety, hypertension, tachycardia or bradycardia, and tachypnea. The patient may also
be asymptomatic.
Risk factors for POUR include:
Spinal Blocks: Depresses ability to sense bladder fullness and lack of voluntary
muscle coordination to consciously initiate voiding. Once the dermatome is L5 or
lower, detrusor contractions return, meaning patient
should be able to void.
Gynecologic, urologic, rectal (hemorrhoidectomies), and pelvic procedures
(inguinal hernia repairs). Patients receive local anesthetic in these procedures
which can lead to a lack of voluntary muscle coordination to consciously initiate
voiding. These procedures also have the potential to inflame the perineum,
obstructing the urethra or damaging nerves that innervate the bladder
Medications:
o Opioids decrease the urge sensation, which increases bladder capacity.
o Anticholinergics (glycopyrrolate, atropine, ditropan) block detrusor
contractions causing bladder hypotonia
o Sympathomimetics increase urethral resistance.
o Beta blockers reduce sphincter tone; blocking that may cause retention
Length of procedure greater than 60 minutes.
Intraoperative fluid greater than 1000 ml.
History of BPH and/or urinary retention.
65 years or greater due to neuronal degeneration leading to bladder dysfuntion.
To reduce the incidences of POUR in the Phase II patient, the post anesthesia nurse uses
an algorithm. Using the algorithm decreases urinary retention, frequency of
catheterization, duration of Foley catheter, in addition to improving patient safety,
satisfaction, and outcomes.
1. The post anesthesia nurse identifies outpatients with a high risk for developing
POUR.
2. Outpatients with no risk factors are discharged and advised to call if they are
unable to void within 8 hours of last void.
3. Outpatients with risk factors must void at least 150 ml.
4. If the patient is unable to void or voids less than 150 ml, the PACU nurse assesses
the patients volume by bladder scan.
5. For bladder volumes greater than 400 ml, the nurse calls the surgical team for
further orders.
6. For bladder volumes less than 400 ml, the PACU nurse may discharge the patient
if appropriate.
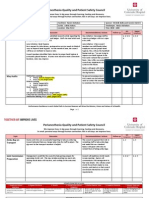
See below for the guideline:
University of Colorado Health-Central, Unit-Based Guideline: Perioperative Services
Is patient at risk
for POUR?
Outpatient with
no risk factors
for POUR
Discharge
Outpatient with
risk factors
for POUR
Unable
to void
Assess volume by
bladder scan
Bladder volume
> 400 ml
Call MD for
catheterization
order
Bladder volume
< 400 ml
Discharge
Advise patient
to seek medical
assistance if
unable to void
within 8 hours
Void
< 150 ml > 150 ml
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Build Size and Aesthetics with the 6-Week Hype Gains Hypertrophy ProgramDocument21 pagesBuild Size and Aesthetics with the 6-Week Hype Gains Hypertrophy ProgramDanCurtis100% (1)
- Lines WorksheetDocument3 pagesLines WorksheetJuzef StaljinNo ratings yet
- Keys To Biblical CounselingDocument7 pagesKeys To Biblical CounselingDavid Salazar100% (6)
- Piaggio MP3 300 Ibrido LT MY 2010 (En)Document412 pagesPiaggio MP3 300 Ibrido LT MY 2010 (En)Manualles100% (3)
- Diploma Pharmacy First Year - Hap - MCQSDocument13 pagesDiploma Pharmacy First Year - Hap - MCQSAnitha Mary Dambale91% (33)
- Conder Separator Brochure NewDocument8 pagesConder Separator Brochure Newednavilod100% (1)
- Pour Pretest GraphsDocument10 pagesPour Pretest Graphsapi-245672784No ratings yet
- CnaannualcompetencyDocument3 pagesCnaannualcompetencyapi-245672784No ratings yet
- Focuspdca Pour1Document5 pagesFocuspdca Pour1api-245672784No ratings yet
- Ekg EmailsDocument5 pagesEkg Emailsapi-245672784No ratings yet
- Jcaho EmailsDocument8 pagesJcaho Emailsapi-245672784No ratings yet
- PscannualcompetencyDocument2 pagesPscannualcompetencyapi-245672784No ratings yet
- RnannualcompetencyDocument3 pagesRnannualcompetencyapi-245672784No ratings yet
- Ekg DefibrhythmstemplateDocument1 pageEkg Defibrhythmstemplateapi-245672784No ratings yet
- Joint Commission Compliance Powerpoint Post-TestDocument2 pagesJoint Commission Compliance Powerpoint Post-Testapi-245672784No ratings yet
- Code BlueDocument5 pagesCode Blueapi-245672784No ratings yet
- CompetencyemailsDocument3 pagesCompetencyemailsapi-245672784No ratings yet
- PACU Joint Commission Compliance Outcomes Board - PEER REVIEWDocument1 pagePACU Joint Commission Compliance Outcomes Board - PEER REVIEWapi-245672784No ratings yet
- JcahosynopsistemplateDocument1 pageJcahosynopsistemplateapi-245672784No ratings yet
- TimelineDocument1 pageTimelineapi-245672784No ratings yet
- JcahopreparationtemplateDocument1 pageJcahopreparationtemplateapi-245672784No ratings yet
- Ekg Ulearn ClasstemplateDocument1 pageEkg Ulearn Classtemplateapi-245672784No ratings yet
- JcahomockvisittemplateDocument1 pageJcahomockvisittemplateapi-245672784No ratings yet
- JointcommissionDocument27 pagesJointcommissionapi-245672784No ratings yet
- CatchabugDocument1 pageCatchabugapi-245672784No ratings yet
- 2015 Yearly Joint Commission Compliance CompetencyDocument1 page2015 Yearly Joint Commission Compliance Competencyapi-245672784No ratings yet
- Ekg Scenario TemplateDocument2 pagesEkg Scenario Templateapi-245672784No ratings yet
- Stroke Alert Powerpoint EmailsDocument5 pagesStroke Alert Powerpoint Emailsapi-245672784No ratings yet
- Qps Min 5-28Document2 pagesQps Min 5-28api-245672784No ratings yet
- Ekg Share Point TesttemplateDocument2 pagesEkg Share Point Testtemplateapi-245672784No ratings yet
- Ekg NursedysrhythmiatesttemplateDocument1 pageEkg Nursedysrhythmiatesttemplateapi-245672784No ratings yet
- Ekg InterpretationDocument1 pageEkg Interpretationapi-245672784No ratings yet
- Perianesthesia Quality and Patient Safety Council CharterDocument2 pagesPerianesthesia Quality and Patient Safety Council Charterapi-245672784No ratings yet
- Pour GuidelineDocument4 pagesPour Guidelineapi-245672784No ratings yet
- StrokecontributionDocument3 pagesStrokecontributionapi-245672784No ratings yet
- BOD FormatDocument4 pagesBOD FormatSkill IndiaNo ratings yet
- Radiol 2020201473Document37 pagesRadiol 2020201473M Victoria SalazarNo ratings yet
- Marital Satisfaction in Dual Earner FamilyDocument4 pagesMarital Satisfaction in Dual Earner FamilyInternational Organization of Scientific Research (IOSR)No ratings yet
- Reflective Essay Assignment #8 - Managing Emotions and Coping With StressDocument2 pagesReflective Essay Assignment #8 - Managing Emotions and Coping With StressRej GarbosaNo ratings yet
- Preferensi Konsumen &strategi Pemasaran Produk Bayem Organik Di CVDocument8 pagesPreferensi Konsumen &strategi Pemasaran Produk Bayem Organik Di CVsendang mNo ratings yet
- Easy and Successful Plumbing Methods You Can Now Applyhslhj PDFDocument2 pagesEasy and Successful Plumbing Methods You Can Now Applyhslhj PDFbeartea84No ratings yet
- CASR Part 830 Amdt. 2 - Notification & Reporting of Aircraft Accidents, Incidents, or Overdue Acft & Investigation OCRDocument17 pagesCASR Part 830 Amdt. 2 - Notification & Reporting of Aircraft Accidents, Incidents, or Overdue Acft & Investigation OCRHarry NuryantoNo ratings yet
- Sugar Reseach in AustraliaDocument16 pagesSugar Reseach in AustraliaJhonattanIsaacNo ratings yet
- Test Units and Accessories: Sinteso™Document22 pagesTest Units and Accessories: Sinteso™Imad QsnNo ratings yet
- Abdul Khaliq - Good Governance (GG)Document15 pagesAbdul Khaliq - Good Governance (GG)Toorialai AminNo ratings yet
- Bandong 3is Q4M6Document6 pagesBandong 3is Q4M6Kento RyuNo ratings yet
- Arecaceae or Palmaceae (Palm Family) : Reported By: Kerlyn Kaye I. AsuncionDocument23 pagesArecaceae or Palmaceae (Palm Family) : Reported By: Kerlyn Kaye I. AsuncionNamae BacalNo ratings yet
- Causes of DyspneaDocument9 pagesCauses of DyspneaHanis Afiqah Violet MeowNo ratings yet
- Jaimin PatelDocument3 pagesJaimin PatelSanjay SinghNo ratings yet
- Understanding Anxiety Disorders and Abnormal PsychologyDocument7 pagesUnderstanding Anxiety Disorders and Abnormal PsychologyLeonardo YsaiahNo ratings yet
- Kootenay Lake Pennywise October 17, 2017Document40 pagesKootenay Lake Pennywise October 17, 2017Pennywise PublishingNo ratings yet
- Health Programs Activities Timeframe Expected Output Child CareDocument3 pagesHealth Programs Activities Timeframe Expected Output Child CareC SamNo ratings yet
- Stepan Formulation 943Document2 pagesStepan Formulation 943Mohamed AdelNo ratings yet
- Mimosa-by-Airspan-C5c Hoja de EspecificacionesDocument2 pagesMimosa-by-Airspan-C5c Hoja de EspecificacionesJuan atzinNo ratings yet
- Jamec Air FittingsDocument18 pagesJamec Air Fittingsgoeez1No ratings yet
- Multiple Sentences and Service of PenaltyDocument5 pagesMultiple Sentences and Service of PenaltyAngelNo ratings yet
- Experiment 4 (Group 1)Document4 pagesExperiment 4 (Group 1)Webster Kevin John Dela CruzNo ratings yet
- Honda PCX150Document137 pagesHonda PCX150Akchu KadNo ratings yet
- Regional Ecology Test ScoringDocument14 pagesRegional Ecology Test Scoringaisyah Wardah201No ratings yet