Professional Documents
Culture Documents
Bactec Vs LJ
Uploaded by
Meenachi Chidambaram100%(1)100% found this document useful (1 vote)
79 views4 pagesBACTEC / Mycobacteria Growth Indicator Tube (MGIT) system alone could supplant the use of a supplemental lowenstein-jensen slant for routine recovery of Mycobacterium species from clinical specimens. Overall sensitivities of the MGIT and LJ media were 86.5% and 59.7%, respectively.
Original Description:
Original Title
Bactec vs LJ
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentBACTEC / Mycobacteria Growth Indicator Tube (MGIT) system alone could supplant the use of a supplemental lowenstein-jensen slant for routine recovery of Mycobacterium species from clinical specimens. Overall sensitivities of the MGIT and LJ media were 86.5% and 59.7%, respectively.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
100%(1)100% found this document useful (1 vote)
79 views4 pagesBactec Vs LJ
Uploaded by
Meenachi ChidambaramBACTEC / Mycobacteria Growth Indicator Tube (MGIT) system alone could supplant the use of a supplemental lowenstein-jensen slant for routine recovery of Mycobacterium species from clinical specimens. Overall sensitivities of the MGIT and LJ media were 86.5% and 59.7%, respectively.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
Microbiology and Infectious Disease / RECOVERY OF MYCOBACTERIA FROM CLINICAL SPECIMENS
542 Am J Clin Pathol 2002;118:542-545 American Society for Clinical Pathology
Comparison of the Automated Mycobacteria Growth
Indicator Tube System (BACTEC 960/MGIT)
With Lwenstein-Jensen Medium for Recovery
of Mycobacteria From Clinical Specimens
Dongsi Lu, MD, PhD,
1,2
Bobbi Heeren, MT(ASCP),
2
and W. Michael Dunne, PhD
1
Key Words: Mycobacteria; Lwenstein-Jensen (LJ) slant; MGIT; BACTEC 960
A b s t r a c t
We examined whether the BACTEC/Mycobacteria
Growth Indicator Tube (MGIT) system alone could
supplant the use of a supplemental Lwenstein-Jensen
(LJ) slant for routine recovery of Mycobacterium
species from clinical specimens. A total of 6,062
specimens were included in the study. Of these, 273
specimens were positive for 278 mycobacterial isolates
while 15 specimens were smear positive but culture
negative using both media. Further analysis showed
that 143 (51.4%) of the 278 total isolates were
recovered from both the MGIT and LJ media. An
additional 106 isolates (38.1%) were recovered from
the MGIT only, while 29 (10.4%) isolates grew only on
the LJ slant. The overall sensitivities of the MGIT and
LJ media were 86.5% and 59.7%, respectively, for the
recovery of mycobacteria from clinical materials. This
study shows that although the MGIT system
demonstrates better sensitivity for the recovery of
mycobacteria from clinical specimens, both media types
are necessary to maximize the sensitivity of detection.
The clinical microbiology laboratory has a critical role
in the detection and control of infection caused by clinically
significant Mycobacterium species, such as Mycobacterium
tuberculosis complex and Mycobacterium avium complex
(MAC) organisms. Rapid, sensitive, and accurate detection
of these organisms in clinical specimens can hasten the
administration of appropriate antimycobacterial therapy and
prevent the spread of infection to susceptible contacts
through the use of effective infection control practices.
1
Conventional solid media, such as the egg-based Lwen-
stein-Jensen (LJ) and agar-based Middlebrook 7H10 media,
traditionally have been used for the recovery of mycobac-
teria from clinical materials
2,3
; however, the slow rate of
growth of many pathogenic Mycobacterium species on solid
media can substantially delay the identification process.
Broth media such as Middlebrook 7H9 have been developed
to speed the growth and recovery rate of mycobacteria in
the laboratory.
4
A variety of manual and automated systems have been
developed specifically to reduce the time to detect and iden-
tify mycobacteria in clinical specimens. Examples of the
manual approach include the biphasic Septi-Chek AFB
(Becton Dickinson, Sparks, MD) and the MB-Redox (Biotest
AG, Dreieich, Germany) systems. Advances in automation
and novel growth detection methods have led to the develop-
ment of the radiometric BACTEC 460TB (Becton Dick-
inson), the fluorometric BACTEC MB9000 and BACTEC
MGIT (Mycobacteria Growth Indicator Tube) 960 systems
(Becton Dickinson), the carbon dioxidesensing MB/BacT
ALERT 3D System (Organon Teknika, Durham, NC), and
the pressure-sensing ESP Culture System II (Trek Diagnostic
Systems, Westlake, OH).
Microbiology and Infectious Disease / ORIGINAL ARTICLE
Am J Clin Pathol 2002;118:542-545 543 American Society for Clinical Pathology
The BACTEC MGIT 960 system is one of the more
recent automated detection systems designed for the rapid
detection of mycobacteria in all types of clinical specimens
except blood. The system consists of a culture tube
containing modified Middlebrook 7H9 medium with a fluo-
rescent growth indicator embedded in silicone on the bottom
of each tube. This compound is sensitive to the presence of
dissolved oxygen in the broth medium. Clinical specimens
are processed and inoculated into the MGIT tube. As
microorganisms grow, the oxygen in the medium is depleted
with a subsequent increase in the fluorescence of the indi-
cator. The enhanced fluorescence in tubes can be monitored
automatically over time using the BACTEC 960 detection
module. The difference between the BACTEC MB9000
system and the BACTEC MGIT 960 system is mainly in
total specimen capacity.
Recently, Sharp et al
5
reported that mycobacterial
cultures using the BACTEC MB9000 system alone provided
for the recovery of more than 99.7% of clinically relevant
isolates without the need for supplemental solid media such
as LJ media. The present study was initiated to determine
whether the BACTEC MGIT 960 system was equally sensi-
tive for the recovery of mycobacteria from clinical samples,
thereby eliminating the need for supplemental solid medium.
Materials and Methods
All clinical specimens submitted to Barnes-Jewish
Hospital Microbiology Laboratory (St Louis, MO) for
culture of mycobacteria from December 1999 through
January 2001 were included in the study. All contaminated
specimens, such as sputum, bronchial washings, and
bronchial alveolar lavages, were digested and decontami-
nated within 24 hours of receipt. Tissue specimens (unless
from a sterile site) were homogenized before decontamina-
tion and digestion. Other specimens from presumed sterile
sites were inoculated directly to growth media after concen-
tration by centrifugation. All specimens were examined for
the presence of acid-fast bacilli using the auramine-
rhodamine stain.
6
Processing Specimens With Bacterial Contamination
Decontamination and digestion of contaminated speci-
mens was performed essentially as previously described.
7
Briefly, an equal volume of MycoPrep reagent (BBL, Cock-
eysville, MD) containing N-acetyl-L-cysteine and sodium
hydroxide was added to each specimen in a 50-mL conical
centrifuge tube. The suspension then was mixed for 20
seconds and permitted to stand for 15 minutes. If the spec-
imen was on a swab, it was removed at this point. Phosphate
buffer (0.067-mol/L concentration, pH 6.8) was added to
make a final volume of 40 mL with adequate mixing to stop
the digestion process. The tubes were centrifuged for 20
minutes at 3,000g. The supernatant fluid was decanted care-
fully, and the sediment was retained. The sediment was
suspended in 1 to 3 mL of sterile phosphate buffer, pH 6.8.
Media Inoculation and Smear Preparation
Before inoculation, each MGIT tube was supplemented
with the PANTA (polymyxin B, amphotericin B, nalidixic
acid, trimethoprim, and azlocillin) antibiotic mixture and
OADC (oleic acid-albumin-dextrose-catalase) enrichment
(Becton Dickinson). Exactly 0.5 mL of the digested, decon-
taminated, concentrated suspension was inoculated into the
MGIT tube. The tube was recapped tightly, mixed well by
inversion, and placed into the BACTEC 960 detection
module. MGIT cultures were incubated for a total of 6 weeks
before being reported as negative. Approximately 0.1 mL of
the specimen then was inoculated onto the LJ slant. The
inoculated LJ slants were incubated in carbon dioxide at
37C for a total of 8 weeks. For skin, superficial abscesses,
ulcers, extremities, or other superficial wounds or tissues, a
second set of media was inoculated (LJ, MGIT tube, and
chocolate slant) and incubated at 30C in 8% to 10% carbon
dioxide with humidity. The LJ tubes were examined twice
weekly for 6 weeks and then at 8 weeks before discarding.
When growth was detected, smears were prepared and
stained using the Kinyoun carbolfuchsin stain
6
to determine
the presence or absence of acid-fast bacilli.
Cultures positive for acid-fast bacilli isolates were eval-
uated for the presence of M tuberculosis complex or MAC-
specific sequences by probe hybridization (AccuProbe, Gen-
Probe, San Diego, CA). Mycobacterium species other than M
tuberculosis complex or MAC were forwarded to the
Missouri Department of Health Mycobacteriology Labora-
tory (Mt Vernon, MO) for identification.
Statistical Analysis and Recovery Comparison
Exact McNemar P values were calculated using STATA
release 7.0 statistical software (College Station, TX). For the
purpose of this study, the sensitivity of a culture method was
defined as the percentage of total mycobacterial isolates
(MGIT and LJ slants) recovered by a single culture method
(MGIT or LJ slants).
Results
During the study period, a total of 302 of 6,062 speci-
mens were positive for acid-fast organisms by smear, culture,
or both. The majority (78.1%) of specimens were from respi-
ratory tract sources, including sputum, bronchial washings,
tracheal aspirates, bronchoalveolar lavages, and transbronchial
Lu et al / RECOVERY OF MYCOBACTERIA FROM CLINICAL SPECIMENS
544 Am J Clin Pathol 2002;118:542-545 American Society for Clinical Pathology
biopsies. Nonrespiratory tract specimens included tissue
(lymph node, lung, liver, skin and soft tissue, bone, bone
marrow, and wound; n = 42), urine (n = 4), stool (n = 7),
blood (n = 9), drainage from the chest wall and an unspeci-
fied site (n = 2), and pleural fluid (n = 2). Fourteen speci-
mens were contaminated by bacterial overgrowth (4 MGIT
and 10 LJ slant) and were excluded from the study. Of the
remaining 288 positive specimens, 273 produced 278
mycobacterial isolates in one or both media, while 15 speci-
mens were smear-positive only.
Of the 278 mycobacterial isolates, 143 (51.4%) were
recovered from both MGIT and LJ media, while an addi-
tional 106 (38.1%) and 29 (10.4%) were recovered only
from MGIT or LJ medium, respectively. The overall sensi-
tivity for recovery of mycobacteria from clinical specimens
was 86.5% for the MGIT and 59.7% for LJ medium (P <
.0001) Table 1. Of the 278 positive cultures, 65 (23.4%)
and 105 (37.8%) were identified as M tuberculosis complex
and MAC, respectively, by probe hybridization (Gen-Probe).
M tuberculosis complex was recovered from both MGIT and
LJ media in 44 (68%) of 65 positive cultures, while 17
(26%) and 4 (6%) of the 65 cultures positive for M tubercu-
losis complex were recovered from MGIT or LJ medium
alone, respectively. The calculated sensitivities of MGIT and
LJ media for the recovery of M tuberculosis complex were
94% and 74%, respectively (P = .0072). MAC was isolated
from 56 (53.5%) of 105 positive cultures from both MGIT
and LJ media, while 36 (34.3%) and 13 (12.4%) of the 105
positive cultures were obtained only from MGIT or LJ
medium, respectively. The calculated sensitivities of MGIT
and LJ media for the recovery of MAC were 87.6% and
65.7%, respectively (P = .0014) Table 2.
The remainder of the 108 mycobacterial isolates
included Mycobacterium kansasii (n = 31), Mycobacterium
gordonae (n = 27), Mycobacterium fortuitum (n = 18),
Mycobacterium mucogenicum (n = 13), Mycobacterium
chelonae (n = 12), Mycobacterium lentiflavum (n = 2),
Mycobacterium xenopi (n = 1), Mycobacterium marinum (n
= 2), Mycobacterium terrae (n = 1), and Mycobacterium
flavescens (n = 1) species. Of these, 43 were recovered from
both MGIT and LJ media, while 53 and 12 isolates were
recovered from MGIT or LJ medium alone, respectively. The
overall sensitivities for the recovery of Mycobacterium
species other than M tuberculosis complex and MAC were
89% and 51% for MGIT and LJ, respectively (P < .0001).
Discussion
The results of this study demonstrated that the MGIT
system consistently provided better recovery of all Mycobac-
terium species from a variety of clinical specimens than did
the traditional LJ slant. This observation is consistent with
the findings of previous studies regarding the performance of
the MGIT system.
8-15
Indeed, the MGIT system provided a
20% or greater improvement in total recovery rate for all
mycobacteria (249 vs 172 of 278), M tuberculosis complex
(61 vs 48 of 65), MAC (92 vs 69 of 105), and miscellaneous
Mycobacterium species (96 vs 55 of 108) over a traditional
LJ slant.
However, the MGIT system did not achieve 100% sensi-
tivity for the isolation of M tuberculosis complex and MAC
organisms. Six percent of total M tuberculosis complex
isolates and 12% of total MAC isolates were recovered only
from the LJ slant, while the MGIT remained negative for
growth after 6 weeks of incubation. Of the 13 MAC isolates
detected by LJ medium alone, 6 (46%) were isolated from
patients with a primary diagnosis of MAC disease. If the LJ
slant had been eliminated from the mycobacterial culture
Table 1
Comparison of Mycobacteria Recovery From the BACTEC
960 Mycobacteria Growth Indicator Tube System
*
and Lwenstein-Jensen Culture Medium
Mycobacteria Growth Indicator Tube
Positive Negative Total Isolates
Lwenstein-Jensen
Positive 143 29 172
Negative 106 15 106
Total isolates 249 29 278
*
For proprietary information, see the text.
Table 2
Mycobacterial Isolates Detected by the BACTEC 960 Mycobacteria Growth Indicator Tube (MGIT)
*
and Lwenstein-Jensen
(LJ) Methods
Organism Total No. of Isolates MGIT and LJ MGIT Alone LJ Alone P (MGIT vs LJ)
Mycobacterium tuberculosis complex 65 44 (68) 17 (26) 4 (6) .0072
Mycobacterium avium complex 105 56 (53.3) 36 (34.3) 13 (12.4) .0014
Other 108 43 (39.8) 53 (49.1) 12 (11.1) <.0001
Total 278 143 (51.4) 106 (38.1) 29 (10.4) <.0001
*
For proprietary information, see the text.
Microbiology and Infectious Disease / ORIGINAL ARTICLE
Am J Clin Pathol 2002;118:542-545 545 American Society for Clinical Pathology
procedure, the diagnosis of 17 cases of M tuberculosis
complex or MAC would have been missed.
In this study, 15 specimens were smear-positive and
culture-negative in either MGIT or LJ media. Nine of these
specimens were obtained from patients with previous posi-
tive cultures who were currently receiving antimycobacte-
rial therapy, presumably explaining the false-negative
culture results.
Although the automated MGIT system demonstrated
better sensitivity than the traditional LJ slant for the recovery
of mycobacteria from clinical specimens, our study indicated
that approximately 10% of clinically significant Mycobac-
terium species would be missed by the use of this system
alone. The MGIT system is not yet sufficiently sensitive to
warrant the elimination of supplemental solid media.
From the
1
Division of Laboratory Medicine, Department of
Pathology and Immunology, Washington University School of
Medicine; and
2
Barnes-Jewish Hospital, St Louis, MO.
Presented in part at the 21st Annual Meeting of the Academy
of Clinical Laboratory Physicians and Scientists, Seattle, WA,
June 14-16, 2001.
Address reprint requests to Dr Dunne: Division of
Laboratory Medicine, Box 8118, Washington University School of
Medicine, 660 S Euclid Ave, St Louis, MO 63110.
References
1. Subcommittee of the Joint Tuberculosis Committee of the
British Thoracic Society. Management of opportunist
mycobacterial infections: Joint Tuberculosis Committee
Guidelines 1999. Thorax. 2000;55:210-218.
2. Metchock BJ, Nolte FS, Wallace RJ Jr. Mycobacterium. In:
Murray PR, Baron EJ, Pfaller MA, et al, eds. Manual of Clinical
Microbiology. 7th ed. Washington, DC: ASM Press; 1999:399-
437.
3. Murray PR, Rosenthal KS, Kobayashi GS, et al.
Mycobacterium. In: Brown M, ed. Medical Microbiology. 3rd
ed. St Louis, MO: Mosby; 1998:319-330.
4. Stager CE, Libonati JP, Siddiqi SH, et al. Role of solid media
when used in conjunction with the BACTEC system for
mycobacterial isolation and identification. J Clin Microbiol.
1991;29:154-157.
5. Sharp SE, Lemes M, Sierra SG, et al. Lwenstein-Jensen
media: no longer necessary for mycobacterial isolation. Am J
Clin Pathol. 2000;113:770-773.
6. Ebersole LL. Acid-fast stain procedures. In: Isenberg HD, ed.
Clinical Microbiology Procedure Handbook. Washington, DC:
ASM Press; 1992:3.5.1-3.5.10.
7. Gullans CR Sr. Digestion-decontamination procedures. In:
Isenberg HD, ed. Clinical Microbiology Procedure Handbook.
Washington, DC: ASM Press; 1992:3.4.1-3.4.14.
8. Ardito F, Sanguinetti M, Sechi L, et al. Comparison of the
mycobacteria growth indicator tube with radiometric and
solid culture for isolation of mycobacteria from clinical
specimens and susceptibility testing of Mycobacterium
tuberculosis. New Microbiol. 2000;23:151-158.
9. Casal M, Gutierrez J, Vaquero M. Comparative evaluation of
the Mycobacteria Growth Indicator Tube with the BACTEC
460 TB system and Lwenstein-Jensen medium for isolation
of mycobacteria from clinical specimens. Int J Tuberc Lung
Dis. 1997;1:81-84.
10. Chew WK, Lasaitis RM, Schio FA, et al. Clinical evaluation
of the Mycobacteria Growth Indicator Tube (MGIT)
compared with radiometric (BACTEC) and solid media for
isolation of Mycobacterium species. J Med Microbiol.
1998;47:821-827.
11. Chien HP, Yu MC, Wu MH, et al. Comparison of the
BACTEC MGIT 960 with Lwenstein-Jensen medium for
recovery of mycobacteria from clinical specimens. Int J Tuberc
Lung Dis. 2000;4:866-870.
12. Somoskovi A, Kodmon C, Lantos A, et al. Comparison of
recoveries of Mycobacterium tuberculosis using the automated
BACTEC MGIT 960 system, the BACTEC 460 TB system,
and Lwenstein-Jensen medium. J Clin Microbiol.
2000;38:2395-2397.
13. van Griethuysen AJ, Jansz AR, Buiting AG. Comparison of
fluorescent BACTEC 9000 MB system, Septi-Chek AFB
system, and Lwenstein-Jensen medium for detection of
mycobacteria. J Clin Microbiol. 1996;34:2391-2394.
14. Leitritz L, Schubert S, Bucherl B, et al. Evaluation of
BACTEC MGIT 960 and BACTEC 460TB systems for
recovery of mycobacteria from clinical specimens of a
university hospital with low incidence of tuberculosis. J Clin
Microbiol. 2001;39:3764-3767.
15. Wilson ML, Stone BL, Hildred MV, et al. Comparison of
recovery rates for mycobacteria from BACTEC 12B vials,
Middlebrook 7H11-selective 7H11 biplates, and Lwenstein
Jensen slants in a public health mycobacteriology laboratory.
J Clin Microbiol. 1995;33:2516-2518.
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- 34 Catalase Test FinDocument5 pages34 Catalase Test FinMeenachi ChidambaramNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Identicifation of Hookworm Species in Stool by Harada Mori CultureDocument2 pagesIdenticifation of Hookworm Species in Stool by Harada Mori CultureMeenachi ChidambaramNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Plasma Heme Oxygenase-1 Levels Distinguish Latent or Successfully Treated Human Tuberculosis From Active DiseaseDocument6 pagesPlasma Heme Oxygenase-1 Levels Distinguish Latent or Successfully Treated Human Tuberculosis From Active DiseaseMeenachi ChidambaramNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- 3.0 Drug ResistanceDocument18 pages3.0 Drug ResistanceMeenachi ChidambaramNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- ImmunoregulationDocument19 pagesImmunoregulationMeenachi ChidambaramNo ratings yet
- Prevalence of Hookworm Infection Among Patients Attending Aminu Kano Teaching Hospital Kano, NigeriaDocument3 pagesPrevalence of Hookworm Infection Among Patients Attending Aminu Kano Teaching Hospital Kano, NigeriaMeenachi ChidambaramNo ratings yet
- Immunoglobulin: Isotypes, Allotypes and IdiotypesDocument18 pagesImmunoglobulin: Isotypes, Allotypes and IdiotypesMeenachi ChidambaramNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Dracunculus Medinensis Onchocerca Loa LoaDocument45 pagesDracunculus Medinensis Onchocerca Loa LoaMeenachi Chidambaram100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Catalase Test - Principle, Procedure and Interpretations - HowMedDocument3 pagesCatalase Test - Principle, Procedure and Interpretations - HowMedMeenachi ChidambaramNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Ziehl Neelsen Staining - Principle, Procedure and Interpretations - HowMedDocument4 pagesZiehl Neelsen Staining - Principle, Procedure and Interpretations - HowMedMeenachi ChidambaramNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- 54 Not Eng Stat Comp2k12Document10 pages54 Not Eng Stat Comp2k12Meenachi ChidambaramNo ratings yet
- Mayangukiral Oru MaathuDocument126 pagesMayangukiral Oru MaathuMeenachi ChidambaramNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- InilabDocument94 pagesInilabCarlos Gene QuirozNo ratings yet
- HANDOUT - Pathogen Most Wanted Poster - 2016Document2 pagesHANDOUT - Pathogen Most Wanted Poster - 2016Mazanda YalinduaNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Vaccination Programs in Poultry - Poultry - Merck Veterinary MaDocument9 pagesVaccination Programs in Poultry - Poultry - Merck Veterinary MaSamapanNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- References: Bachoon, D.S. Dustman, W.A. (2008) - Exercise 8: Selective and Differential Media ForDocument4 pagesReferences: Bachoon, D.S. Dustman, W.A. (2008) - Exercise 8: Selective and Differential Media Forlyn-lynNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- B.SC - Microbiology CBCS Syllabus Sem 1 2Document18 pagesB.SC - Microbiology CBCS Syllabus Sem 1 2vivek pattani0% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Polansky SKRRT PDFDocument619 pagesPolansky SKRRT PDFAstrud Labrador100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- JAT - CHT 13Document68 pagesJAT - CHT 13j_smith24No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Introduction To MicrobiologyDocument55 pagesIntroduction To MicrobiologyAngelica Valdez BalmesNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Christopher WalshDocument47 pagesChristopher WalshFernando J. Correa DelgadoNo ratings yet
- Blood Groups, Blood Typing and Blood TransfusionsDocument4 pagesBlood Groups, Blood Typing and Blood TransfusionsShahnawaz KhanNo ratings yet
- UV Dose TableDocument5 pagesUV Dose TablemajortayNo ratings yet
- 0 - Review of Post Graduate Medical Entrance Examination (PGMEE) (AAA) (PDFDrive - Com) Export PDFDocument39 pages0 - Review of Post Graduate Medical Entrance Examination (PGMEE) (AAA) (PDFDrive - Com) Export PDFAbu ÂwŞmž100% (2)
- Algoritmo de Transfusion en Pacientes CardiologicosDocument8 pagesAlgoritmo de Transfusion en Pacientes CardiologicosLyonTrioréNo ratings yet
- Blood Bottle GuideDocument12 pagesBlood Bottle GuideHYTITNo ratings yet
- Forensic BiologyDocument5 pagesForensic BiologyNurul HaziqahNo ratings yet
- Stateboard CLASS 12 BIO ZOOLOGY TM CHAPTER 4 PRINCIPLES OF INHERITANCE AND VARIATION PPT 146 PAGEDocument146 pagesStateboard CLASS 12 BIO ZOOLOGY TM CHAPTER 4 PRINCIPLES OF INHERITANCE AND VARIATION PPT 146 PAGEG. VigneshNo ratings yet
- Tatalaksana PneumoniaDocument37 pagesTatalaksana PneumoniaAnindya AgrasidiNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Mic Bro004 Urine Culture 28-06-17 en Urine CultureDocument2 pagesMic Bro004 Urine Culture 28-06-17 en Urine Culturebilal gayretliNo ratings yet
- Evan Syndrome A Case ReportDocument3 pagesEvan Syndrome A Case ReportEditor IJTSRDNo ratings yet
- AFP/PNP Housing, San Isidro, Rodriguez, RizalDocument1 pageAFP/PNP Housing, San Isidro, Rodriguez, RizalChristine ApoloNo ratings yet
- Revision Test of Chapter 1 ScienceDocument4 pagesRevision Test of Chapter 1 ScienceYasoktaran AnanthanNo ratings yet
- Lab 1 - Asepsis and Infection Control QuestionsDocument3 pagesLab 1 - Asepsis and Infection Control QuestionsmlomiguenNo ratings yet
- Universal PrecautionsDocument3 pagesUniversal PrecautionsRatha VilanirashiyaNo ratings yet
- Eastern Health 30 Minute 4 Hour Rule 2017 PDFDocument1 pageEastern Health 30 Minute 4 Hour Rule 2017 PDFprastiaNo ratings yet
- Pathologist Laboratory Medical Director in Denver CO Resume Joseph EastmanDocument5 pagesPathologist Laboratory Medical Director in Denver CO Resume Joseph EastmanJosephEastmanNo ratings yet
- Phlebotomy Update: Aspek TeknisDocument30 pagesPhlebotomy Update: Aspek TeknisTinik 29No ratings yet
- Blood Group Test ProcedureDocument5 pagesBlood Group Test ProcedureNIRANJANA SHALININo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 344-Malt Extract Agar-105398 PDFDocument1 page344-Malt Extract Agar-105398 PDFAlejandro Canaza JorgesNo ratings yet
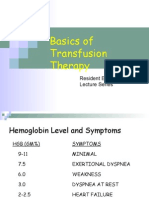
- Basics of Transfusion TherapyDocument43 pagesBasics of Transfusion TherapyMuhammad Afyudin DjumhuriNo ratings yet
- VITEK2 CardsDocument4 pagesVITEK2 CardsNidia MaradiagaNo ratings yet