Professional Documents
Culture Documents
Joint Commission Sentinel Event Alert 8 8 12
Uploaded by
api-2442306640 ratings0% found this document useful (0 votes)
87 views5 pagesOriginal Title
joint commission sentinel event alert 8 8 12
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
87 views5 pagesJoint Commission Sentinel Event Alert 8 8 12
Uploaded by
api-244230664Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
AoD nr e-*rlai
Published for Joint
Commission accredited
organizations and interested
health care professionals,
Senti nel Event Al ert identif ies
specific types of sentinel
events, describes their
common underlying causes,
and suggests steps to prevent
occurrences in the future.
Accredited organizations
should consider information in
an Alert when designing or
redesigning relevant
processes and consider
implementing relevant
suggestions contained in the
Alert or reasonable
alternatives.
Please route this issue to
appropriate staff within your
organization. Sentinel Event
Alert may only be reproduced
in its entirety and credited to
The Joint Commission. To
receive by e-mail, or to view
past issues, visit
www jointcomm
ission.org.
Y7
/IFThe
Joint Commission
A complimentary publication of
TheJoint Commission
Issue 49, August 8,2012
Safe use of opioids in hospitals
while opioid use is gener{]v sa[e,[or most patients,ryld4analge.s.i.cF.rjlg-y,qe
ffila+ed with adverse effects, ''''" the most,serious effect being rddpir-aiory
,&FBss'ilgrl;.which
is.gener:alS_nre.csded,by.sdatiorxa'5'6
Other common adverse
effects associated with opioid therapy include dizziness, nausea, vomiting,
constipation, pedation, delirium, hallucinations, falls, hypotension, and aspiration
pneumonia.a'7 Adverse events can occur with the ,se oi any opioid; among these
are fentanyl, hydrocodone, hydromorphone, methadone, morphine, oxycodone,
and sufentanil. while there are numerous problems associated with opioid use,
including underprescribing, overprescribing, tolerance, dependence, and drug
abuse;tftis Abrt'wiLlfo,eus on the -safe lse.of
.opioids,that are,prescribed and-
administered within the inpatient hospitalsgtting.iThe Joint Commission recognizes
that the emergency department presents unique challenges that should also be
addressed by the hospital, but may not be direcfly addressed in this Alert. This
Alert will provide a number of actions that can be taken to avoid the unintended
consequences of opioid use among hospital inpatients.
Opioid analgesics rank among the drugs most frequently associated with adverse
drug events. The literature provides numerous studies of the adverse events
associated with opioids. one study found that most adverse drug events were due
to drug-drug interactions, most commonly involving opioids, benzodiazepines, or
cardiac medications.8 tn addition, a British stuoy oia,'osS inpatient adveise drug
reactions found thatr.L6,gersent,ivreFe,:attr.ihrtable.too&kk,
making opioids one of
the most frequently implicated drugs in adverse reactions.TcT&ingider&
d
EW{{@i&PrreFsisn..@atsj+rryer{ed.toaver-ageaboqt
'O;5"Frer*
Some of the causes for adverse events associated with opioid use are:
o
Lack of knowledge about potency differences among opioids.
.
lmproper prescribing
and administration of multiple opioids and modalities of
opioid administration (i.e., oral, parenteral and transdermal patches).
.
lnadequate monitoring of patients on opioids.e,10
of the opioid-related adverse drug events
-
including deaths
-
that occurred in
hospitals and were reported to The Joint commission's sentinel Event database
(200 4 -20 1 1
) ;,4.&
pefggnJ.lryere,,yvrong
dose,:,nredieatkrfi rrors; 2g pereent were
qela-tgd"t,orimpr,sper.rglryx,t@ring,.q{,lhe.p3lhot,
andJX.,gerqent were,+elated.to otter
.f 8.@.q including excessive dosing, medication interactions and adverse drug
reactions.* These reports underscore the need for the
judicious
and safe
prescribing and administration of opioids, and the need for appropriate monitoring
of patients. when opioids are administered, the potential for opioid-induced
respiratory depression should always be considered because:
o
The risk may be greater with higher opioid doses
o
The occurrence may actually be higher than reported
o
There is a higher incidence observed in clinical trialsll
o
=\4ariqug,,pA.1jents,
afe at
hgler.risk{see- elSnr);:mc}udiqg.patien-ts,witt+ sleep
-,ffial@*entswho,are.merbidly,obese;,who are,very,yqffigF,J&hg."Ie elder:$,
.sthcare
very ill, and who:.eoneunently,receive:oIhe+.drugs
that.ar: entml
=nefvor*s,system
and,respirato,ry.depres,saBts,(e.g.r.anxioty.Jics,
sedatives).5,11,12
*
The reporting of most sentinel events to The Joint Commission is voluntary and represents only a
small proportion of actual events. Therefore these data are not an epidemioiogic daia set and no
conclusions should be drawn about the actual relative frequency of events or irends in events over time.
www.jointcommission.org
Sentinel Event Aleft, lssue 49
Page2
The need for assessing and managing
pain to
help avoid accidental opioid overdose
The safe use of opioids in hospital settings relies
have increased awareness of the importance of
safe and effective pain management.'' lnstituted in
2001, these standards have made a significant
difference in appropriate
pain management. Before
the standards, there were continuing reports of
inadequate
pain control for postoperative and
traumatic
pain, cancer pain, and many other acute
and chronic
pain challenges.'" ln addition,
compliance with the standards leads to better
clinical outcomes, such as improved wound
healing, and helps to prevent untoward
consequences of inadequate.pain relief, such as
impaired immune response.la The importance of
both assessing and managing pain is criticalto
patients who otherwise would suffer debilitating
pain. Notwithstanding the need for appropriate
pain
management, organizations should make staff
aware of the following factors and activities that
can help avoid accidental opioid overuse:
Screen
patients for respiratory depression risk
factors (see sidebar).
5'11'12
Assess the patient's previous history of
analgesic use or abuse, duration and possible
side effects to identify potential opioid
tolerance or intolerance.
Conduct a full body skin assessment of
patients prior to administering a new opioid to
rule out the possibility that the patient has an
applied fentanyl patch or implanted drug
delivery system or infusion
PumP.
Use an individualized, multimodal treatment
plan to manage pain.6'15 A multimodal
approach combines strategies such as
psychosocial support, coordination of care, the
promotion of healthful behaviors,
nonpharmacologic approqqf e-s, and non-
opioid pain medications.ls'l6'17 Upon
assessment, the
with a non-n
(e.g., level thrge_gn a 10-point sga!e,),
ffiftffiYTfr"S6
precautions shou ld i ncl ude
siarting the patient with a short-term trialls of
carefully titrated opioids at the lowest effective
dose to achieve satisfactory
pain control'18
Sufficient time should be allowed to assess the
patient's response to an initial dose before
increasing the dosage or prescribing opioids
for long-term use.
Consult a pharmacist or pain management
expert (when available)when converting from
one opioid to another, or changing the route of
administration
(from oral to lV or transdermal).
Consider that the patient may be less tolerant
of the new drug (incomplete cross tolerance)
or that the new drug may be more potent.
Note: While there are numerous dose
conversion sca/es and othertools available,
each organization should determine the tool(s)
that will be used and assess sfaff's
understanding of the selected tool(s)- Sentinel
events have been reported to The Joint
Commission related to misuse or
misunderstanding of these tools.
Avoid rapid dose escalation of opioid
analgesia above routine dose levels in opioid-
tolerant patients.
Take extra
precautions when transferring
patients between care units and facilities, and
Sentinel Event Nert, lssue 49
Page 3
when discharging patients to their home.
Consider that drug levels may reach peak
concentrations during transport.
r
Avoid using opioids to meet an arbitrary pain
rating or a planned discharge date. Dosing
should be based on the individual patient's
need and condition.
Actions suggested by The Joint Gommission
Hospitals can take the following evidence-based
actions to help avoid adverse events associated
with the use of opioids.
See relevant Joint Commission requirements:
LD.04.01.07 element of performance 1,
1D.04.04.05, PC.0'1 .02.01,
pC.01.02.03
Ep 2 and
3, Pr.01.01.01, Pt.02.01.01,
pt.03.01.01,
MM.07.01.03
Safe
4. lf available,
into e-prescribing
systems for all opioids. The red flags can be
either for dosing limits or alerts, or for
verifications.
Separate sound-alike and look-alike opioids,
and use tall man lettering and other techniques
to reduce the risk of error.
Use conversion support systems to calculate
correct doses of opioids to help prevent
problems with conversions from oral, lV and
by Proxy," for strategies for eliminating risk
related to PCA by proxy.) The use of smart
infusion pump technology with dosage error
reduction software can add another layer of
safety.
See relevant Joint Commission requirement:
MM.01.01.03
Appropriate education and training
agents, antidepressants, anticonvulsants (e.9.,
gabapentin and pregabalin), and muscle relaxants
(e.9., baclofen, tizanidine), can be used before
prescribing an opioid. ln addition, when used in
combination with opioids, these non-narcotics may
reduce the dose of opioids required to effectively
manage pain.27'28'2e
3d
and oxygenation, and technological and clinical
monitoring. Staff training should emphasize how to
assess patients for adverse drug reactions, how to
recognize advancing sedation, and the importance
of making timely adjustments to the plan of care
assessments should take place and define the
period of time that is appropriate to adequately
observe trends.o Monitoring should be
management plans that include high-risk opioids,
such as methadon-e, fentanyl, lV hydromorphone
and meperidine.2u''6
te oxygen saturation in patients
who are actively experiencing respiratory
depression, especially when supplemental oxygen
is being used
-
thus the value of using
capnography to monitor ventilation.6 When pulse
oximetry or capnography is used, it should be used
continuously rather than intermittently.6'1e'24
Sentinel
individuali7gd according to the patient's
Sentinel Event Aleft, lssue 49
Page 4
based on the patient's risk.5'6 For example, a
comprehensive pain management program can
help to educate clinicians, endorse best practices,
and improve safety.
o The various generic and brand names,
formulations, and routes of administration of
opioids in order to prevent confusion and
reduce the accidental duplication of opioid
Screening lnstrument for Substance Abuse
Potential (SISAP).5'6'15
See relevant Joint Commission requirement:
PC.01.02.07 EP 2
Contributing to this alert were Judith A. Paice,
Ph.D., R.N., director of the Cancer Pain Program at
Northwestern University's Feinberg School of
Medicine, Chicago, lll.; Debra B. Gordon, R.N.,
University of Wisconsin Hospital and Clinics,
Madison, Wis.; Jose Contreras, M.D., Pain and
Palliative Medicine, Hackensack University Medical
Center, Hackensack, N.J.; and Donna Jarzyna,
R.N., University Medical Center, Tucson, Ariz.
Resources
The Food and Drug Administration provides a
"Blueprint for Prescriber Education for Extended-
Release and Lonq-Actinq Opioid Analqesics,"
which includes information about the specific
characteristics of the ER/LA opioid analgesic
products.
References
1
Vila H Jr, Smith RA, Augustyniak MJ: The efficacy and
safety of pain management before and after
implementation of hospital-wide pain management
standards t
Anesthesia and
An al gesia, 2005;101 :47 4-80
2
Emergency department visits involving nonmedical use
of selected prescription drugs
-
United States, 2004-
20Q8. Morbidity and Mortality Weekly Repoft 2010,
59:705-709
3
Office of Applied Studies, Substance Abuse and Mental
Health Services Administration. Substance abuse
treatment admissions involving abuse of pain relievers:
1998 and 2008,
http://oas:samhsa.qov/2k1 0/230/230PainRelvr2k1 0.cfm
(accessed October 28, 201 1)
o
McPherson ML: Strategies for the management of
opioid-induced adverse iffects. Advanced Studies in
P h a rm acy, 2008;5(2):52-57
5
Jarzyna D, et al: American Society for Pain
Management Nursing guidelines on monitoring for opioid-
induced sedation and respiratory depression. Parn
M an agement N u rsing, 201 1 ;12(3): 1 1 8-1 45.e1 0
6
Pasero C, M McCaffery: Pain assessment and
pharmacologic management. Chapter 12
-
Key Concepts
in Analgesic Therapy, and Chapter 19
-
Management of
opioid-induced adverse effects. St. Louis, Mosby
Elseveir, 2011
7
Davies EC, et al: Adverse Drug Reactions in Hospital
ln-Patients: A Prospective Analysis of 3695 Patient-
Episodes, PLos ONE, February 2009:4(2):e4439
8
Wright A, et al: Preventability of adverse drug events
involving multiple drugs using publicly available clinical
decision support tools. Ameican Journal of Health-
Sysfem Pharmacy, 2012; 69:221 -7
s
U.S. Food and Drug Administration: Public Health
Advisories (Drugs), Fentanyl Transdermal Patch,
lmportant lnformation for the Safe Use of Fentanyl
t's
I
I
I
I
{
{
The potential risks of tolerance, addiction,
physical dependency, and withdrawal
symptoms associated with opioid therapy.l5
The specific dangers as a result of the
potentiating
effectg_when opioids are used in
l+-l_'+
combinationlEuch as oral and transdermal
(fentanyl patches).
.
The safe and secure storaoe of ooioid
anargesrcs ,n rne nomF
When providing this information at discharge, also
include phone numbers for a contact person to call
with questions.
See relevant Joint Commission requirements:
HR.01.04.01 EP 4, HR.01.05.03, HR.01.06.01,
MS.03.01.03 EP 2
acute care setting are the Pasero Opioid-lnduced
Sedation Scale (POSS)and the Richmond
Agitation-Sedation Scale (RASS). Tools that can
be used after discharge to help prevent opioid
misuse include the Screener and Opioid
Assessment for Patients with Pain (SOAPP and
SOAPP-R), the Opioid Risk Tool (ORT), and the
The impact of opioid tnerapy o6lBq),qhemo'tor
qlcr,
eoonitive function (wnici m6lifrEEi-
onvrng ano worK sarely);
Il::f$:tx"lffrffi :dHrff Lffi]x
depressants;
ilEfm-n6[tfulmdentifyi n g knowledge gaps and
in developing improvement strategies to reduce
Sentinel Event Alefi, lssue 49
Page 5
Transdermal System (Patch). December 21
,2007,
http ://www.fda.
qov/Druqs/DruqSafetv/PostmarketDruq
Sa
fetvl nformationforPatientsand Providers/DruoSafetvl nform
ationforHeathcareProfessionalsi PublicHealthAdvisories/u
cm051257.htm?utm campaion=Gooqle2&utm source=fd
aSearch&utm medium=website&utm term=fentanvl&utm
content=g (accessed May 21,2012)
m
l.J-S. Food and Drug Administration: FDA Reminds the
Public about the Potential for Life-Threatening Harm from
Accidental Exposure to Fentanyl Transdermal Systems
("Patches"). April 18, 2012,
http://www.fda. gov/Drugs/DrugSafety/ucm300747.
htm?ut
m_cam pai g n
=Google2&utm_sou rce=fdaSearch&utm_me
d ium=website&utm_term=20 1 2 fentanyl&utm_content=4
(accessed May21,2012\
"
Dahan A, et al: lncidence, reversal and prevention of
opioid-induced respiratory depression. Anesthesiology,
2010;112:226-38
12
American Geriatrics Society Panel on the
Pharmacological Management of Persistent Pain in Older
Persons: Pharmacologic Management of Persistent Pain
in Older Persons. Journal of the American Geiatrics
Society. 2009:57 :1331 -46
'3
Dahl JL, Gordon DB: Joint Commission pain
standards: a progress report. APS Bulletin,2002;12(6)
1a
Wells N, et al: Patient Safety and Quality: An
Evidence-Based Handbook for Nurses. Chapter 1 7
-
lmproving the quality of care through pain assessment
and management. AHRQ Publication No. 08-0043, April
2008. Agency for Healthcare Research and Quality,
Rockville, Md., http://www.ahrq.qov/qual/nurseshdbld
'u
Chou R, et at ty -
American Academy of Pain Medicine Opioids Guidelines
Panel: Clinical guidelines for the use of chronic opioid
therapy in chronic noncancer pain. The Journal of Pain,
2009;10(2):113-'130
16
Harvard Health Publications: Painkillers fuel growth in
drug addiction. Harvard Reviews of Health News,
January 2011:4-5,
http://harvardpartnersinternational.stavwel lsolutionsonlin
,eocom/69,M01
1 1 b (accessed October 28, 201 1)
17
Streltzer J, Johansen L: Prescription drug dependence
and evolving beliefs about chronic pain management.
Ame i can J ou m al of Psy ch i atry, 2006 ; 1 63(4): 594-597
'o Pasero C, et al: Using continuous infusion with PCA.
American Joumal of Nursing, 1 999;99(2)
1e
Overdyk FJ: Postoperative respiratory depression and
opioids. lnitiatives in Safe Patient Care, Saxe Healthcare
Communications, 2009, http://initiatives-
patientsafetv.orq/l
nitiativesl %20.pdf (accessed October
28,2011)
20
Cepeda MS, et al: Side effects of opioids during short-
term administration: effect of age, gender and race.
Clinical Pharmacology and Therapeutics, 2003;74:102-
112
21
Dunn KM, et al: Opioid prescriptions for chronic pain
and overdose: a cohort study. Annals of lnternal
Medi cine, 201 0;1 52:85-92
22
Hagle ME, et al: Respiratory depression in adult
patients with intravenous patient-controlled analgesia.
O rth opaed i c N u rsi ng, 2004;23(1)): I 8-27
23
Ozdilekcan C, et al: Risk factors associated with
postoperative pulmonary complications following
oncolog i cal s u rgery. T u b e rk To ra ks, 2004;52(3):248-55
" Stoelting RK, Weinger MB: Dangers of postoperative
opioids
-
is there a cure? Anesthesia Patient Safety
F_oundation Newsletter, Summer 2009;24(2):25-26
25
The Truax Group: Long-acting and extended-release
opioid dangers. Patient Safety Tip of the Week, June 28,
2011,
http://patientsafetvsolutions.com/docs/June 28 201 1 Lo
nq Actinq and Extended Release Opioid Danqers.htm
(accessed July 19, 2011)
26
lnstitute For Safe Medication Practices: Ongoing,
preventable fatal events with fentanyl transdermal
patches are alarming! Medication Safety Aleft, June 28,
2007,
http://www. ismp.oroinewsletters/acutecare/articles/20070
628.asp (accessed October 28, 201 1)
27
Svenson JE, Meyer, TD: Effectiveness of nonnarcotic
protocol for the treatment of acute exacerbations of
chronic nonmalignant pain. Ihe American Journal of
Emergency Med ic i ne, 2007
;25:445-449
"
Schug SA, Manopas A: Update on the role of non-
opioids for postoperative pain treatment. Best Practice &
Re se a rc h C I i n i c a I An ae sthe s i o I ogy, 2007
;21
(1
):
1 5-30
2e
Munir MA, et al: Nonopioid analgesics. Anesthesiology
Clinics, 2007
;25:7 61 -77 4
to
White PF: The changing role of non-opioid analgesic
techniques in the management of postoperative pain.
Anesthesia & Analgesia, 2005;'101 :S5-S22
Patient Safety Advisory Group
The Patient Safety Advisory Group informs The Joint
Commission on patient safety issues and, with other
sources, advises on topics and content for Sentinel
Event Alert. Members: James P. Bagian, M.D., P.E.
(chair); Michael Cohen, R.Ph., M.S., Sc.D. (vice chair);
Jane H. Barnsteiner, R.N., Ph.D., FMN; Jim B. Battles,
Ph.D.; William H. Beeson, M.D.; Patrick J. Brennan,
M.D.; Martin H. Diamond, FACHE; Cindy Dougherty,
R.N., CPHQ; Frank Federico, B.S., R.Ph.; Marilyn Flack;
Steven S. Fountain, M.D.; Suzanne Graham, R.N.,
Ph.D.; Martin J. Hatlie, Esq.; Jennifer Jackson, B.S.N.,
J.D.; Paul Kelley, CBET; Henri R. Manasse, Jr., Ph.D.,
Sc.D.; Jane McCaffrey, MHSA, DFASHRM; Mark W.
Milner, R.N., MBA, CPHQ, FACHE; Jeanine Arden Ornt,
J.D.; Grena Porto, R.N., M,S., ARM, CPHRM; Matthew
Scanlon, M.D.; Ronni P. Solomon, J.D.; Dana Swenson,
P.E., MBA
You might also like
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceFrom EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceRating: 3 out of 5 stars3/5 (1)
- Anderson & Townsend Preventing High-Alert Medication Errors in Hospitalized PatientsDocument6 pagesAnderson & Townsend Preventing High-Alert Medication Errors in Hospitalized PatientsCG0% (1)
- Drug Errors: Consequences, Mechanisms, and Avoidance: Key PointsDocument7 pagesDrug Errors: Consequences, Mechanisms, and Avoidance: Key PointsRavikiran SuryanarayanamurthyNo ratings yet
- PharmacovigilanceDocument45 pagesPharmacovigilancepavani valluriNo ratings yet
- Adverse Drug ReactionDocument3 pagesAdverse Drug ReactionTin SagmonNo ratings yet
- Interview Questions-PVDocument9 pagesInterview Questions-PVtausif100% (1)
- Introduction To Pharmacovigilance & Its Current Perspectives in PunjabDocument35 pagesIntroduction To Pharmacovigilance & Its Current Perspectives in PunjabAshar NasirNo ratings yet
- Moore RDocument7 pagesMoore RElaine IllescasNo ratings yet
- National Patient Safety GoalsDocument7 pagesNational Patient Safety GoalsyaniNo ratings yet
- Incidence, Characteristics, and Predictive Factors For Medication Errors in Paediatric Anaesthesia: A Prospective Incident Monitoring StudyDocument8 pagesIncidence, Characteristics, and Predictive Factors For Medication Errors in Paediatric Anaesthesia: A Prospective Incident Monitoring StudyShaikh ZarinNo ratings yet
- Pharmacovigilance Ensuring The Safe Use of MedicinesDocument18 pagesPharmacovigilance Ensuring The Safe Use of MedicinespopadrianionutzNo ratings yet
- JCI-Sentinel Event AlertDocument3 pagesJCI-Sentinel Event AlertDewi Ratna SariNo ratings yet
- Art 09Document9 pagesArt 09Francisca DonosoNo ratings yet
- PHARMACOVIGILANCEDocument28 pagesPHARMACOVIGILANCENosheen JavedNo ratings yet
- Impact of Pharmacist Interventions On Clinical Outcome and Cost Avoidance in A University Teaching HospitalDocument8 pagesImpact of Pharmacist Interventions On Clinical Outcome and Cost Avoidance in A University Teaching HospitalErick De La RosaNo ratings yet
- PV DefinitionsDocument6 pagesPV DefinitionsJhansi ReddyNo ratings yet
- International Patient Safety GoalsDocument30 pagesInternational Patient Safety GoalsMuvenn Kannan50% (2)
- Drug Incompatibilities in Intravenous Therapy Evaluation and Proposition of Preventive Tools in Intensive Care and Hematology UnitsDocument9 pagesDrug Incompatibilities in Intravenous Therapy Evaluation and Proposition of Preventive Tools in Intensive Care and Hematology UnitsGlory Claudia KarundengNo ratings yet
- Consumer ReportingDocument36 pagesConsumer ReportingJai RamNo ratings yet
- Journa Generall AneshesiaDocument7 pagesJourna Generall AneshesiaNadya NovianiNo ratings yet
- Aims and Applications: Aims: The Three Aims of Pharmacoepidemiology AreDocument10 pagesAims and Applications: Aims: The Three Aims of Pharmacoepidemiology Aregowtham0% (1)
- Emergency Drug Therapy DoneDocument4 pagesEmergency Drug Therapy DonelsshgriffinNo ratings yet
- Adverse Drug Reaction Monitoring Reporting PDFDocument3 pagesAdverse Drug Reaction Monitoring Reporting PDFRossana Rizqita PutriNo ratings yet
- Medication Error PDFDocument61 pagesMedication Error PDFChelsea Ritz MendozaNo ratings yet
- Med Errors OldDocument1 pageMed Errors OldAnonymous XvwKtnSrMRNo ratings yet
- Brief Notes On PharmacovigilanceDocument78 pagesBrief Notes On Pharmacovigilancejay100% (1)
- Introduction To PharmacovigillanceDocument93 pagesIntroduction To PharmacovigillanceRanjan Kumar MajhiNo ratings yet
- Introduction To Pharmacovigilance UNIT - 1Document58 pagesIntroduction To Pharmacovigilance UNIT - 1meghana vasNo ratings yet
- Day Care Anaesthesia With Ketamine V S Fentanyl A Comparative Study in Short Surgical ProceduresDocument9 pagesDay Care Anaesthesia With Ketamine V S Fentanyl A Comparative Study in Short Surgical ProceduresFuchsia ZeinNo ratings yet
- Introduction To PharmacovigillanceDocument93 pagesIntroduction To Pharmacovigillancefunnymemesworld2023No ratings yet
- Abhijath Documents Those Who Are Preparing For Interview 1664876843Document36 pagesAbhijath Documents Those Who Are Preparing For Interview 1664876843naidujNo ratings yet
- 4 High Alert Medication FinalDocument4 pages4 High Alert Medication Finalrini setyawatiNo ratings yet
- 2000-WHO Drug Information Vol. 14 - No. 4 PDFDocument79 pages2000-WHO Drug Information Vol. 14 - No. 4 PDFAngela Castro RNo ratings yet
- Evidenced Based (Bernardo, BSN - 3C)Document8 pagesEvidenced Based (Bernardo, BSN - 3C)Jerico CunananNo ratings yet
- Pharmacovigilance - Dr. Ganesh UchitDocument58 pagesPharmacovigilance - Dr. Ganesh UchitSshan ChaturvediNo ratings yet
- SMB5401Document288 pagesSMB5401funnymemesworld2023No ratings yet
- I Hi Trigger Tool For Measuring Adverse Drug EventsDocument16 pagesI Hi Trigger Tool For Measuring Adverse Drug EventsGaby ValenzuelaNo ratings yet
- Ad Hoc Data SourcesDocument11 pagesAd Hoc Data SourcesVINAY KUMARNo ratings yet
- Notes To PharmacovigilanceDocument58 pagesNotes To Pharmacovigilancejay100% (1)
- Ipsg # 2017 PDFDocument30 pagesIpsg # 2017 PDFDARRYLARANHA100% (1)
- Week2 Submitter PaperDocument3 pagesWeek2 Submitter Paperapi-299189797No ratings yet
- Spontenious Reporting SystemDocument3 pagesSpontenious Reporting SystemAyanNo ratings yet
- Adverse Reactions SlideshowDocument40 pagesAdverse Reactions SlideshowGary MaoNo ratings yet
- Farmacovigilancia RevisionDocument16 pagesFarmacovigilancia RevisionOfelia RomeroNo ratings yet
- For Partial Fulfilment of The Requirement For TheDocument45 pagesFor Partial Fulfilment of The Requirement For ThesalmanNo ratings yet
- Write - Up - Adhoc Data SourcesDocument12 pagesWrite - Up - Adhoc Data SourcesRaju BaiNo ratings yet
- P109primary Care For Persons Who Inject DrugsDocument8 pagesP109primary Care For Persons Who Inject Drugshossein kasiriNo ratings yet
- Irrational Use of DrugDocument9 pagesIrrational Use of Drugsreedam100% (2)
- Ro-Ils 1Document3 pagesRo-Ils 1api-529438966No ratings yet
- HPCP Assignment 2Document8 pagesHPCP Assignment 2mokshmshah492001No ratings yet
- Radiation Oncology Incident Learning System (ROILS) Cast StudyDocument4 pagesRadiation Oncology Incident Learning System (ROILS) Cast Studyapi-481226212No ratings yet
- Medication Errors: What They Are, How They Happen, and How To Avoid ThemDocument9 pagesMedication Errors: What They Are, How They Happen, and How To Avoid ThemMoisesNo ratings yet
- Pharma CO VigilanceDocument33 pagesPharma CO VigilanceSravani ReddyNo ratings yet
- Medication Safety: Improving Public HealthDocument6 pagesMedication Safety: Improving Public HealthViee Nie SfarmNo ratings yet
- Practices: in Patient CareDocument5 pagesPractices: in Patient Careahmad nuril hidayatNo ratings yet
- Pharmacovigilance - An Overview: Dr. Sukanta Sen MD, DNB, DM (Clin Pharmacology)Document31 pagesPharmacovigilance - An Overview: Dr. Sukanta Sen MD, DNB, DM (Clin Pharmacology)FranchescaAmoréBrodithe100% (1)
- Immunization Safety SurveillanceDocument14 pagesImmunization Safety SurveillanceHIRA DASNo ratings yet
- The Prevention of Intrathecal Medictionl Errors Woods K Department of Health UK 2001 PDFDocument24 pagesThe Prevention of Intrathecal Medictionl Errors Woods K Department of Health UK 2001 PDFArturo RuizNo ratings yet
- Recs 071317 OpioidsDocument4 pagesRecs 071317 OpioidsKuzivakwasheNo ratings yet
- Search BMJ GroupDocument23 pagesSearch BMJ GroupCharles BrooksNo ratings yet
- Recommendation From Renee AbdellaDocument2 pagesRecommendation From Renee Abdellaapi-244230664No ratings yet
- PPPPC Meeting Minutes 071614Document5 pagesPPPPC Meeting Minutes 071614api-244230664No ratings yet
- Signed Final Evaluation 2014Document3 pagesSigned Final Evaluation 2014api-244230664No ratings yet
- Recommendation From Jamie NordhagenDocument1 pageRecommendation From Jamie Nordhagenapi-244230664No ratings yet
- Thank You Patient 1Document2 pagesThank You Patient 1api-244230664No ratings yet
- Kudos Email 8 25 13Document2 pagesKudos Email 8 25 13api-244230664No ratings yet
- Focuspdca 7 26 14Document2 pagesFocuspdca 7 26 14api-244230664No ratings yet
- Kudos Email 1 13 14Document1 pageKudos Email 1 13 14api-244230664No ratings yet
- Pain Severity Satisfaction With Pain ManagementDocument10 pagesPain Severity Satisfaction With Pain Managementapi-244230664No ratings yet
- Kudos Email 8 2 14Document1 pageKudos Email 8 2 14api-244230664No ratings yet
- Ce Record 2014 Aurora Davis v2Document1 pageCe Record 2014 Aurora Davis v2api-244230664No ratings yet
- Advisor Checklist CompletedDocument7 pagesAdvisor Checklist Completedapi-244230664No ratings yet
- Kudos Email 10 11 13Document1 pageKudos Email 10 11 13api-244230664No ratings yet
- Kudos Email 3 29 14Document1 pageKudos Email 3 29 14api-244230664No ratings yet
- Thank You New Grad 1Document2 pagesThank You New Grad 1api-244230664No ratings yet
- Preceptor Council AttendanceDocument2 pagesPreceptor Council Attendanceapi-244230664No ratings yet
- Lo6 FeedbackDocument2 pagesLo6 Feedbackapi-244230664No ratings yet
- January Staff Meeting MinutesDocument3 pagesJanuary Staff Meeting Minutesapi-244230664No ratings yet
- Preceptor Council AttendanceDocument2 pagesPreceptor Council Attendanceapi-244230664No ratings yet
- Cancer Patients Barriers To Pain ManagementDocument12 pagesCancer Patients Barriers To Pain Managementapi-244230664No ratings yet
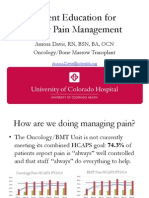
- Presentation of Pain Patient Education ToolDocument10 pagesPresentation of Pain Patient Education Toolapi-244230664No ratings yet
- PSC Meeting Agenda 4 2014Document1 pagePSC Meeting Agenda 4 2014api-244230664No ratings yet
- Do Patients Beliefs Act As BarriersDocument13 pagesDo Patients Beliefs Act As Barriersapi-244230664No ratings yet
- Pain Minutes 031914Document2 pagesPain Minutes 031914api-244230664No ratings yet
- Email From Mandy 7 14 14Document1 pageEmail From Mandy 7 14 14api-244230664No ratings yet
- A Pain Education ProgrammeDocument13 pagesA Pain Education Programmeapi-244230664No ratings yet
- Cancer Pain Part 2Document7 pagesCancer Pain Part 2api-244230664No ratings yet
- Hcahps Omg Data BeforeDocument1 pageHcahps Omg Data Beforeapi-244230664No ratings yet
- Hcahps BMT Data BeforeDocument1 pageHcahps BMT Data Beforeapi-244230664No ratings yet
- Daisy Nomination Bill ValentineDocument2 pagesDaisy Nomination Bill Valentineapi-244230664No ratings yet
- Cryptosporidiosis in ChickensDocument7 pagesCryptosporidiosis in ChickensŠhâh NawazNo ratings yet
- PDEA S Register 2-14 FormDocument12 pagesPDEA S Register 2-14 FormAngelito BALUYOT JRNo ratings yet
- Desi Elage: High Cholestrol Level in Blood (Khoon Main Cholesterol Ka Level Barh Jae)Document7 pagesDesi Elage: High Cholestrol Level in Blood (Khoon Main Cholesterol Ka Level Barh Jae)Irshad HussainNo ratings yet
- Health PromotionDocument10 pagesHealth PromotionReyta NoorNo ratings yet
- Basic Life Support (BLS)Document49 pagesBasic Life Support (BLS)Sukhbir KaurNo ratings yet
- Felix Widal TestDocument9 pagesFelix Widal TestGaluhAlvianaNo ratings yet
- CPG Management of Hypertension (4th Edition)Document98 pagesCPG Management of Hypertension (4th Edition)ssfdsNo ratings yet
- Radiotherapy NursingDocument35 pagesRadiotherapy NursingMarlon Rey AnacletoNo ratings yet
- MAPEH 7 Q4 Week 4Document9 pagesMAPEH 7 Q4 Week 4Maricris ArsibalNo ratings yet
- Chapter37 Assessment and Management of Patients With Allergic DisordersDocument40 pagesChapter37 Assessment and Management of Patients With Allergic Disordersjericho dinglasanNo ratings yet
- EC Certificate - Production Quality Assurance EC Certificate - Production Quality AssuranceDocument6 pagesEC Certificate - Production Quality Assurance EC Certificate - Production Quality AssuranceEngr Hamid AliNo ratings yet
- Post-Operative Fever EditDocument52 pagesPost-Operative Fever EditDebsNo ratings yet
- Chagrin Factor - Feinstein1985Document3 pagesChagrin Factor - Feinstein1985Rafael MartinsNo ratings yet
- Preoperative Physiology, Imaging, andDocument13 pagesPreoperative Physiology, Imaging, andSiLfia SahrinNo ratings yet
- Teaching Students With Autism Spectrum DisordersDocument155 pagesTeaching Students With Autism Spectrum DisordersAnonymous Pj6Odj0% (1)
- General HospitaDocument273 pagesGeneral HospitaAbcdNo ratings yet
- Active and Passive Euthanasia Thesis StatementDocument7 pagesActive and Passive Euthanasia Thesis StatementDoMyPaperForMeSingapore100% (2)
- Risk Factors For Venous and Arterial ThrombosisDocument19 pagesRisk Factors For Venous and Arterial ThrombosisM Buyung MusliminNo ratings yet
- Comparative Study of Episiotomy Repair Absorbable Synthetic Versus Chromic Catgut Suture MaterialDocument5 pagesComparative Study of Episiotomy Repair Absorbable Synthetic Versus Chromic Catgut Suture MaterialamilyapraditaNo ratings yet
- AllianzDocument27 pagesAllianzHariz SyahmiNo ratings yet
- PhysioEx9,1: Exercise 7 Activity 2: PEX-07-02Document8 pagesPhysioEx9,1: Exercise 7 Activity 2: PEX-07-02mishael_baig100% (11)
- DialysisDocument21 pagesDialysisReygie MarsadaNo ratings yet
- Discharge PlanDocument1 pageDischarge PlanGail GenturalezNo ratings yet
- A3 ReportDocument4 pagesA3 ReportmfernandNo ratings yet
- Evaluation of The R One Robotic System For Percutaneous Coronary Intervention THDocument11 pagesEvaluation of The R One Robotic System For Percutaneous Coronary Intervention THNeranga SamaratungeNo ratings yet
- Name of Drug Dosage, Route, Frequency and Timing Mechanism of Action Indication Adverse Reactions Special Precautions Nursing ResponsibilitiesDocument2 pagesName of Drug Dosage, Route, Frequency and Timing Mechanism of Action Indication Adverse Reactions Special Precautions Nursing ResponsibilitiesKarl Lourenz DeysolongNo ratings yet
- NUTRILITE Apple Jujube WheatPeptide enDocument27 pagesNUTRILITE Apple Jujube WheatPeptide enNoris Eka Raudzah IshakNo ratings yet
- Hospital Management System: By, C.Arun Kumar S.Dinesh V.Dinesh S.Gowtham S.HarijayanthDocument16 pagesHospital Management System: By, C.Arun Kumar S.Dinesh V.Dinesh S.Gowtham S.Harijayanthneeraj-singh-6543No ratings yet
- AnswersDocument47 pagesAnswersOriyomi OdekunleNo ratings yet
- Mortality Incidence Sociodemographic and Clinical Data in COVID19 PatientsDocument1,365 pagesMortality Incidence Sociodemographic and Clinical Data in COVID19 PatientsSoumodeep SenNo ratings yet
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDFrom EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDRating: 4.5 out of 5 stars4.5/5 (167)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryFrom EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryRating: 4.5 out of 5 stars4.5/5 (157)
- An Autobiography of Trauma: A Healing JourneyFrom EverandAn Autobiography of Trauma: A Healing JourneyRating: 5 out of 5 stars5/5 (2)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreFrom EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreRating: 5 out of 5 stars5/5 (17)
- The Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItFrom EverandThe Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItRating: 4.5 out of 5 stars4.5/5 (107)
- Don't Panic: Taking Control of Anxiety AttacksFrom EverandDon't Panic: Taking Control of Anxiety AttacksRating: 4 out of 5 stars4/5 (12)
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeFrom EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeRating: 4.5 out of 5 stars4.5/5 (140)
- Redefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackFrom EverandRedefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackRating: 4.5 out of 5 stars4.5/5 (152)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeFrom EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeRating: 4.5 out of 5 stars4.5/5 (49)
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionFrom EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionNo ratings yet
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisFrom EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (5)
- A Profession Without Reason: The Crisis of Contemporary Psychiatry—Untangled and Solved by Spinoza, Freethinking, and Radical EnlightenmentFrom EverandA Profession Without Reason: The Crisis of Contemporary Psychiatry—Untangled and Solved by Spinoza, Freethinking, and Radical EnlightenmentNo ratings yet
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeFrom EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeRating: 5 out of 5 stars5/5 (559)
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesFrom EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesRating: 5 out of 5 stars5/5 (70)
- Feel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveFrom EverandFeel the Fear… and Do It Anyway: Dynamic Techniques for Turning Fear, Indecision, and Anger into Power, Action, and LoveRating: 4 out of 5 stars4/5 (250)
- Anxious for Nothing: Finding Calm in a Chaotic WorldFrom EverandAnxious for Nothing: Finding Calm in a Chaotic WorldRating: 4.5 out of 5 stars4.5/5 (1245)
- Insecure in Love: How Anxious Attachment Can Make You Feel Jealous, Needy, and Worried and What You Can Do About ItFrom EverandInsecure in Love: How Anxious Attachment Can Make You Feel Jealous, Needy, and Worried and What You Can Do About ItRating: 4.5 out of 5 stars4.5/5 (84)
- How to Be Miserable: 40 Strategies You Already UseFrom EverandHow to Be Miserable: 40 Strategies You Already UseRating: 4.5 out of 5 stars4.5/5 (57)
- The Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouFrom EverandThe Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouNo ratings yet
- The Anatomy of Loneliness: How to Find Your Way Back to ConnectionFrom EverandThe Anatomy of Loneliness: How to Find Your Way Back to ConnectionRating: 4.5 out of 5 stars4.5/5 (162)
- Heal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaFrom EverandHeal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaRating: 4.5 out of 5 stars4.5/5 (56)
- 50 Ways to Rewire Your Anxious Brain: Simple Skills to Soothe Anxiety and Create New Neural Pathways to CalmFrom Everand50 Ways to Rewire Your Anxious Brain: Simple Skills to Soothe Anxiety and Create New Neural Pathways to CalmNo ratings yet