Professional Documents
Culture Documents
Pediatric Eye and Vision Examination Reference Guide
Uploaded by
biotech_vidhya0 ratings0% found this document useful (0 votes)
41 views41 pagesscience
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentscience
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
41 views41 pagesPediatric Eye and Vision Examination Reference Guide
Uploaded by
biotech_vidhyascience
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 41
Reference G uide
for O ptom etrists
Optometric Clinical
Practice Guideline
PED IATRIC
EYE A N D VISIO N
EXA M IN ATIO N
Revised edition for the C anadian A ssociation of O ptom etrists printed w ith perm ission of the
A m erican A ssociation of O ptom etrists
A m erican O ptom etric A ssociation 1994, 2002. 243 N . Lindbergh Blvd., St. Louis, M O 63141-7881
First Edition O riginally Prepared by (and Second Edition Review ed by) the A m erican O ptom etric
A ssociation C onsensus Panel on Pediatric Eye and Vision Exam ination:
M itchell M . Scheim an, O .D ., M .S., Principal A uthor
C atherine S. A m os, O .D .
Elise B. C iner, O .D .
W endy M arsh-Tootle, O .D .
Bruce D . M oore, O .D .
M ichael W . Rouse, O .D ., M .S.
Review ed by the A O A C linical G uidelines C oordinating C om m ittee:
John C . Tow nsend, O .D ., C hair (2nd Edition)
John F. A m os, O .D ., M .S. (1st and 2nd Editions)
Kerry L. Beebe, O .D . (1st Edition)
Jerry C avallerano, O .D ., Ph.D . (1st Edition)
John Lahr, O .D . (1st Edition)
W . H ow ard M cA lister, O .D ., M .P.H . (2nd Edition)
Stephen C . M iller, O .D . (2nd Edition)
Richard W allingford, Jr., O .D . (1st Edition)
A pproved by the A O A Board of Trustees June 23, 1994 (1st Edition), Revised Septem ber 1997,
and A pril 25, 2002 (2nd Edition)
Review and revision for C anadian printing:
D eborah Jones, O .D ., FC O ptom , D ipC LP, FA A O
OPTOMETRY: THE PRIMARY EYE CARE PROFESSION
D octors of optom etry are independent prim ary health care providers w ho
exam ine, diagnose, treat, and m anage diseases and disorders of the visual
system , the eye, and associated structures as w ell as diagnose related sys-
tem ic conditions.
O ptom etrists provide m ore than tw o-thirds of the prim ary eye care services
in the U nited States and C anada. They are m ore w idely distributed geo-
graphically than other eye care providers and are readily accessible for the
delivery of eye and vision care services. There are approxim ately 3,500 full-
tim e doctors of optom etry currently in practice in C anada. O ptom etrists
practice in alm ost 900 com m unities across C anada
The m ission of the profession of optom etry is to fulfill the vision and eye
care needs of the public through clinical care, research, and education, all
of w hich enhance the quality of life.
N O TE: C linicians should not rely on this C linical G uideline alone for patient care and
m anagem ent. Refer to the listed references and other sources for a m ore detailed
analysis and discussion of patient care inform ation. The inform ation in the G uideline is
current as of date of publication. It w ill be review ed periodically and revised as needed.
TABLE OF CONTENTS
I. INTRODUCTION ........................................................................ 1
II. STATEMENT OF THE PROBLEM
A . Epidem iology of Eye and Vision D isorders in C hildren ..... 3
B. The Pediatric Eye and Vision Exam ination...................... .. 4
III. CARE PROCESS
A . Exam ination of Infants and Toddlers ......................... 6-12
1. G eneral C onsiderations
2. Early D etection and Prevention
3. Exam ination Sequence
a. Patient H istory
b. Visual A cuity
c. Refraction
d. Binocular Vision and O cular M otility
e. O cular H ealth A ssessm ent and System ic
H ealth Screening
f. A ssessm ent and D iagnosis
B. Exam ination of Preschool C hildren .......................... 12-17
1. G eneral C onsiderations
2. Early D etection and Prevention
3. Exam ination Sequence
a. Patient H istory
b. Visual A cuity
c. Refraction
d. Binocular Vision, A ccom m odation, and
O cular M otility
e. O cular H ealth A ssessm ent and System ic
H ealth Screening
f. Supplem ental Testing
g. A ssessm ent and D iagnosis
C . Exam ination of School-A ge C hildren ....................... 17-20
1. G eneral C onsiderations
2. Early D etection and Prevention
3. Exam ination Sequence
a. Patient H istory
b. Visual A cuity
c. Refraction
d. Binocular Vision, A ccom m odation, and O cular
M otility
e. O cular H ealth A ssessm ent and System ic H ealth
Screening
f. Supplem ental Testing
g. A ssessm ent and D iagnosis
D . M anagem ent of C hildren ...................................... 20-22
1. Patient Education
2. C oordination, Frequency, and Extent of C are
IV. CONCLUSION .......................................................................... 23
V. REFERENCES ...................................................................... 25-30
VI. APPENDICES & RESOURCES............................................... 31-37
Figure 1: Pediatric Eye and Vision Exam ination: A Brief Flow chart
Figure 2: Potential C om ponents of the Eye and Vision Exam ination for Infants and
Toddlers
Figure 3: Potential C om ponents of the Eye and Vision Exam ination for Preschool
C hildren
Figure 4: Potential C om ponents of the Eye and Vision Exam ination for School-A ge
C hildren
A bbreviations of C om m only U sed Term s ................................................ 35
G lossary ................................ ........................................................... 36-37
1.
I. INTRODUCTION
O ptom etrists, through their clinical education, training, experience, and broad geo-
graphic distribution, have the m eans to provide effective prim ary eye and vision
services to children in C anada. Prim ary care has been described as those services
provided to patients by a health care practitioner "w ho know s them , w ho is avail-
able for first contact and continuing care, and w ho offers a portal of entry to spe-
cialists for those conditions w arranting referral."
1
Eye care serves as an im portant
point of entry into the health care system because:
Virtually all people need eye care services at som e tim e in their lives.
By its very nature, eye care provides for the evaluation, assessm ent, and coordi-
nation of a broad spectrum of health care needs.
Eye care is a nonthreatening form of health care, particularly to patients w ho
are reluctant to seek general or preventive m edical care.
2
This O ptom etric C linical Practice G uideline for the Pediatric Eye and Vision
Exam ination describes appropriate exam ination procedures for evaluation of the
eye health and vision status of infants and children to reduce the risk of vision loss
and facilitate norm al visual developm ent. It contains recom m endations for tim ely
diagnosis, intervention, and, w hen necessary, consultation or referral for treatm ent
by another health care provider. This G uideline w ill assist optom etrists in achieving
the follow ing goals:
D evelop an appropriate tim etable for eye and vision exam inations for pediatric
patients
Select appropriate exam ination procedures for all pediatric patients
Exam ine the eye health and visual status of pediatric patients effectively
M inim ize or avoid the adverse effects of eye and vision problem s in children
through early identification, education, treatm ent, and prevention
Inform and educate patients, parents/caregivers, and other health care providers
about the im portance and frequency of pediatric eye and vision exam inations.
II. STATEMENT OF THE PROBLEM
In 2003 the C anadian C ensus Bureau reported that there w ere 7.9 m illion children
under 19 years of age in the C anada (25% of the population).
3
In the U nited
States, vision disorders are the fourth m ost com m on disability and the m ost preva-
lent handicapping condition during childhood.
4
In spite of the high prevalence of
vision disorders in this population, studies show that only about 31 percent of chil-
dren betw een ages 6 and 16 years are likely to have had a com prehensive eye and
vision exam ination w ithin the past year, w hile below the age of 6, only about 14
percent are likely to have had an eye and vision exam ination.
5
In a study of 5,851
children 9 to 15 years of age, nearly 20 percent needed glasses but only 10 percent
of that group already had them .
6
Thus, 90 percent of those children requiring pre-
scription eyeglasses w ere not w earing them . W hy so few children receive profes-
sional eye care is unknow n. Possible explanations include a reliance on pediatri-
2.
cians, other prim ary care physicians, or school screenings, m any uninsured parents'
or caregivers' inability to pay for the needed services, and parents' or caregivers'
lack of know ledge that early professional eye care is needed to prevent unnecessary
loss of vision as w ell as to potentially im prove educational readiness.
U nfortunately, undue reliance on vision screening by pediatricians or other prim ary
care physicians m ay result in the late detection of am blyopia and other vision disor-
ders. O ne study reported that in a sam ple of 102 private pediatric practices , vision
screening w as attem pted on only 38 percent of 3-year-old children and 81 percent
of 5-year-old children. The study also show ed that only 26 percent of children fail-
ing the A m erican A cadem y of Pediatrics vision screening guidelines w ere referred
for a professional eye exam ination.
7
The A m erican Public H ealth A ssociation
adopted a resolution that recognizes the shortcom ings of vision screenings, encour-
ages regular eye exam inations at the ages of 6 m onths, 2 years, and 4 years, and
urges pediatricians to recom m end that all children receive eye exam inations at
these intervals.
8
These recom m endations have been adopted by the C anadian
A ssociation of O ptom etrists and prom oted to the profession and the general public
during C anadian Eye H ealth M onth in O ctober 2003.
The interrelationships betw een vision problem s and learning difficulties and the
cost of undetected vision problem s to society are of concern.
9
Vision problem s
generally are not the direct cause of learning disorders; how ever, they can interfere
w ith children's abilities to perform to their potential. W hen children fail to progress
in school, the cost to the individual and society can be substantial.
A m blyopia is the m ost com m on cause of poor vision in the under 20 age group
(G rounds 1995).
10
Studies have show n the need for earlier eye exam ination and
treatm ent and have resulted in clinical advances that enable m ore effective preven-
tive eye care for infants and preschool children.
11-21
Extensive research has dem on-
strated the im portance of the first few years of life in the developm ent of vision.
W ithin the first 6 m onths of life, rapid changes occur in m ost com ponents of the
visual system including visual acuity,
11,12
accom m odation,
13,14
and binocular vision.
15-
17
Interference w ith developm ent during this very critical phase m ay lead to serious
lifelong effects on vision.
18
Successful treatm ent can be obtained m ore quickly w ith
early intervention.
21-24
A n outgrow th of this research is the developm ent of new clinical procedures appro-
priate for the evaluation of vision in infants and toddlers.
17,25-36
C linicians have
gained a better understanding of both the characteristics and processes of vision
developm ent in infants and the tools necessary to exam ine them . A s a result, it is
now recom m ended that all children receive regular, professional eye care beginning
at 6 m onths of age after an initial eye screening at birth, typically perform ed by the
pediatrician.
8,37
3.
A. EPIDEMIOLOGY OF EYE AND VISION DISORDERS IN CHILDREN
O ne of the largest studies reporting the prevalence of specific vision disorders in
children w as conducted as part of the H ealth Exam ination Surveys of 1963-65.
38
D ata w ere collected from a sam ple of 7,119 non-institutionalized children 6-11
years of age w ho received standardized eye exam inations. O f the children exam -
ined, 9.2 percent had an eye m uscle im balance, a disease condition, or other
abnorm ality in one or both eyes. A pproxim ately 2.4 percent had constant strabis-
m us and 4.3 percent had significant heterophoria. The com bined prevalence of
eyelid conditions (hordeola, conjunctivitis, and blepharitis) w as about 1 percent.
The second phase of that research project determ ined the prevalence of eye disor-
ders in 12- to 17-year-olds.
39
O f the 6,768 children exam ined, 7.9 percent had an
eye m uscle im balance, a disease condition, or other abnorm ality in one or both
eyes; approxim ately 3.4 percent had constant strabism us, and 1.8 percent had sig-
nificant heterophoria. The prevalence of conjunctivitis w as 0.6 percent, and that of
blepharitis, 0.3 percent.
A m ore recent review of the literature found the follow ing prevalence figures for
eye and vision problem s in children: am blyopia, 2-3 percent; strabism us, 3-4 per-
cent; refractive errors, 15-30 percent; and ocular disease, less than 1 percent.
40
A
large-scale prospective study of the prevalence of vision disorders and ocular dis-
ease focused on a clinical population of children betw een the ages of 6 m onths
and 18 years. C om prehensive eye exam inations perform ed on 2,025 consecutive
patients show ed that, in addition to refractive anom alies, the m ost com m on condi-
tions optom etrists are likely to encounter in this population are binocular vision and
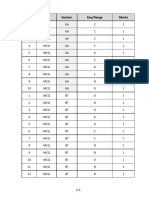
accom m odative disorders (see Table 1).
41
H yperopia 33% 23%
A stigm atism 22.5% 22.5%
M yopia 9.4% 20.2%
N onstrabism ic binocular
disorders
5.0% 16.3%
Strabism us 21.1% 10.0%
A m blyopia 7.9% 7.8%
A ccom m odative disorders 1.0% 6.0%
Peripheral retinal abnorm alities
requiring referral or follow -up care
0.5% 2.0%
VISIO N D ISO RD ERS IN A C LIN IC A L PO PU LATIO N O F C H ILD REN
Disorder Ages 6 months to
5 years 11 months
Ages 6 years
to 18 years
Table 1
4.
B. THE PEDIATRIC EYE AND VISION EXAMINATION
The term "pediatric population" can be applied to patients w ithin a broad age
range, including all those betw een birth and 18 years of age. A lthough the capa-
bilities and needs of children vary significantly, the pediatric population can be
divided into three subcategories:
42-44
Infants and toddlers (birth to 2 years, 11 m onths)
Preschool children (3 years to 5 years, 11 m onths)
School-age children (6 to 18 years).
This subdivision of the pediatric population is based on the developm ental changes
that occur from birth through childhood. C linical experience and research have
show n that at 6 m onths the average child has reached a num ber of critical devel-
opm ental m ilestones, m aking this an appropriate age for the first eye and vision
exam ination. A t this age the average child can sit up w ith support and cognitively
is concerned w ith im m ediate sensory experiences.
45
Visual acuity,
12
accom m oda-
tion,
13,14
stereopsis, and other aspects of the infant's visual system have developed
rapidly, reaching adult levels by the age of 6 m onths (see Table 2, p 5).
15,25
A t about 3 years of age children have achieved adequate receptive and expressive
language skills to begin to cooperate for som e of the traditional eye and vision
tests. H ow ever, the exam iner often needs to m ake m odifications in the testing to
gather useful inform ation. By 6 years of age, the child has m atured to the point
that m any adult tests can be used, w ith m inor procedural m odifications. Because a
child can vary significantly from expected age norm s, it is im portant not to rely
solely upon chronological age w hen choosing testing procedures. A ppropriate test
procedures need to be based on the child's developm ental age and specific capabil-
ity.
The goals of the pediatric eye and vision exam ination are several (see A ppendix
Figure 1):
Evaluate the functional status of the eyes and visual system , taking into
account each child's level of developm ent
A ssess ocular health and related system ic health conditions
Establish a diagnosis and form ulate a treatm ent plan
C ounsel and educate parents/caregivers regarding their child's visual,
ocular, and related health care status, including recom m endations for
treatm ent, m anagem ent, and preventive care.
5.
T
a
b
l
e
2
6.
III. CAREPROCESS
A. EXAMINATION OF INFANTS AND TODDLERS
1. General Considerations
This section of the G uideline describes optom etric procedures for exam ining infants
and toddlers from birth to 2 years, 11 m onths of age. The exam ination com po-
nents are described in general term s and are not intended to be all inclusive.
Professional judgm ent and individual patient sym ptom s, findings, and cooperation
m ay have significant im pact on the nature and course of the exam ination.
C hildren in this age group generally perform best if the exam ination takes place
w hen they are alert. Exam ination early in the m orning or after an infant's nap is
usually m ost effective. Because infants tend to be m ore cooperative and alert
w hen feeding, it is also helpful to suggest that the parent bring a bottle for the
child.
A ge-appropriate exam ination and m anagem ent strategies should be used. M ajor
m odifications include relying m ore on objective exam ination procedures and per-
form ing tests considerably m ore rapidly than w ith older children.
43
2. Early Detection and Prevention
Early detection and treatm ent are essential to preventing vision conditions that
have the potential to cause perm anent loss of vision. Screening by the pediatrician
or other prim ary care physician is im portant at birth and during the first 6 m onths
of life w hen the visual system is highly susceptible to interference. H ow ever,
screening this population has been problem atic, leading to underdetection of stra-
bism us, am blyopia, and significant refractive error.
5,46
N ew er screening techniques
such as photorefraction are available,
36, 47-50
but until they are validated, an eye and
vision exam ination at 6 m onths of age is the best approach for early detection and
prevention of eye and vision problem s in infants and toddlers (see Table 2, p5).
3. Examination Sequence
The eye and vision exam ination of the infant or toddler m ay include, but is not lim -
ited to, the follow ing procedures (see A ppendices Figure 2):
a. Patient History
A com prehensive patient history for infants and toddlers m ay include:
N ature of the presenting problem , including chief com plaint
Visual and ocular history
G eneral health history, including prenatal, perinatal, and postnatal history
and review of system s
Fam ily eye and m edical histories
D evelopm ental history of the child.
7.
The collection of dem ographic data generally precedes the taking of the patient
history. H aving the parent(s) fill out a questionnaire facilitates obtaining the patient
history.
43
Responses to questions related to the m other's pregnancy, birth of the
child, and the child's general and vision developm ent w ill help direct the rem ainder
of the exam ination.
b. Visual Acuity
A ssessm ent of visual acuity for infants and toddlers m ay include these procedures:
Fixation preference tests
Preferential looking visual acuity test.
Estim ation of visual acuity in an infant or toddler can help to confirm or reject cer-
tain hypotheses about the level of binocularity and provides direction for the
rem ainder of the exam ination. Because subjective visual acuity testing requiring
verbal identification of letters or sym bols dem ands sustained attention, this test
cannot be used w ith infants and toddlers. H ow ever, other tests m ay be used to
m ake assum ptions about visual acuity. For exam ple, w hen a unilateral, constant
strabism us is present, visual acuity is presum ed to be reduced in the strabism ic eye.
In the presence of a constant, alternating strabism us, visual acuity is likely to be
norm al in both eyes.
In the absence of strabism us, fixation preference testing w ith a vertical base up or
base dow n 10 prism diopter (PD ) lens to create diplopia has been show n to be
effective in detecting about a three-line visual acuity difference betw een the eyes
and identifying m oderate to severe am blyopia.
51
Specific clinical guidelines have
been developed to estim ate visual acuity on the basis of the strength of fixation
preference.
52, 53
A study of fixation preference testing dem onstrated that the fixa-
tion pattern can be rapidly assessed and confirm ed the usefulness of a graded
assessm ent of the binocular fixation pattern in the detection of am blyopia.
54
Before the advent of behavioral and electrophysiological procedures, indirect m eth-
ods w ere all that w ere available to clinicians for assessing visual acuity in preverbal
children. A s m ore direct assessm ent procedures w ere developed, it becam e evident
that although fixation preference is helpful in detecting am blyopia, it is not alw ays
an accurate predictor of visual acuity. Preferential looking acuity and fixation pref-
erence do not show a strong association.
55,56
C linical use of preferential looking acuity is generally very successful. Teller acuity
cards can be used w ith infants and young children until they are ready for m ore
subjective testing.
33,57 59
H ow ever, underestim ation of visual acuity loss in patients
w ith strabism ic am blyopia on the basis of grating acuity (preferential looking acuity)
lim its the usefulness of this test.
60-65
W hen in doubt, the optom etrist can refer the
child for electrodiagnostic testing, such as visual evoked potentials, w hich has been
show n to be an im portant m ethod for direct assessm ent of visual acuity in
infants.
66-68
8.
If clinical evaluation of an infant or toddler by indirect visual acuity testing, refrac-
tion, and ocular health assessm ent indicates any problem w ith visual acuity, forced-
choice preferential looking w ith the Teller acuity cards or electrodiagnostic testing
should be considered to obtain a m ore precise m easure of baseline visual acuity.
C onsultation w ith an optom etrist or ophthalm ologist w ho has advanced clinical
training or experience w ith preferential looking assessm ent or electrophysiological
evaluation of visual acuity m ay be w arranted.
c. Refraction
Traditional subjective procedures for the assessm ent of refractive error m ay be inef-
fective w ith infants or toddlers because of short attention span and poor fixation.
69
A s a result, the exam iner w ill need to rely on objective m easures of refraction. The
tw o m ost com m only used procedures are:
C ycloplegic retinoscopy
N ear retinoscopy.
It is im portant for the exam iner perform ing cycloplegic retinoscopy in an infant or
toddler to take several precautions:
70
Select the cycloplegic agent carefully (e.g., fair-skinned children w ith blue
eyes m ay exhibit an increased response to drugs and darkly pigm ented
children m ay require m ore frequent or stronger dosages).
Avoid overdosage (e.g., children w ith D ow n syndrom e, cerebral palsy,
trisom y 13 and 18, and other central nervous system disorders in w hom
there m ay be an increased reaction to cycloplegic agents, 1% tropicam ide
m ay be used).
Be aw are of biologic variations in children (e.g., low w eight infants m ay
require a m odified dosage).
C yclopentolate hydrochloride* is the cycloplegic agent of choice. O ne drop should
be instilled tw ice, 5 m inutes apart, in each eye, using a strength of 0.5% for chil-
dren from birth to 1 year and 1% for older children.
71
Spray adm inistration of the
drug appears to be a viable alternative to the use of conventional eye drops for
routine cycloplegic retinoscopy in the pediatric population.
72-74
The child is asked to
keep his or her eyes gently closed w hile the exam iner sprays the cycloplegic agent
on the child's eyelids. A s the child blinks, enough of the drug is delivered to the
eye to provide adequate cycloplegia.
* Every effort has been m ade to ensure that drug dosage recom m endations are accurate at
the tim e of publication of this G uideline. H ow ever, treatm ent recom m endations change due
to continuing research and clinical experience, and clinicians should verify drug dosage
schedules w ith product inform ation sheets. Drugs must be administered in accordance with
provincial regulations.
9.
This technique has tw o advantages: (1) The child has less of an avoidance
response, and it m ay be less traum atic for the child and the parent observing the
procedure. (2) A single application can achieve both cycloplegia and pupillary dila-
tion w hen a m ixture of 0.5% cyclopentolate, 0.5% tropicam ide, and 2.5%
phenylephrine is used. To m aintain sterility, it is best to have this spray m ixture pre-
pared by a pharm acist. Retinoscopy m ay be perform ed 20-30 m inutes after instilla-
tion.
72
The use of loose lenses or a lens rack is recom m ended for retinoscopy.
A study com paring retinoscopy in infants using near retinoscopy, cycloplegia w ith
tropicam ide 1% , and cycloplegia w ith cyclopentolate 1% found that tropicam ide
m ay be a useful alternative in m any healthy, nonstrabism ic infants.
75
N ear retinoscopy is another objective m ethod of estim ating refractive error in
infants and toddlers.30 H ow ever, it has not been found reliable for quantification
of the refractive error.
76-78
N ear retinoscopy m ay have som e clinical value in the follow ing situations:
W hen frequent follow -up is necessary
W hen the child is extrem ely anxious about instillation of cycloplegic agents
W hen the child has had or is at risk for an adverse reaction to cyclopento
late or tropicam ide.
The average refractive error in children from birth to 1 year of age is about 2
diopters (D ) of hyperopia (standard deviation 2 D ).
79
A stigm atism up to 2 D is com -
m on in children under 3 years of age. Studies show that 30-50 percent of infants
less than 12 m onths of age have significant astigm atism , w hich declines over the
first few years of life, becom ing stable by approxim ately 2 to 5 years of age.
80-81
Low am ounts of anisom etropia are com m on and variable in infants. The clinician
m ay choose to m onitor these levels of refractive error rather than prescribe a lens
correction.
d. Binocular Vision and Ocular Motility
The follow ing procedures are useful for assessing binocular function:
C over test
H irschberg test
Krim sky test
Brckner test
Versions
N ear point of convergence.
The cover test is the procedure of choice for evaluation of binocular vision in pre-
verbal children because it is objective and requires little tim e to adm inister. If the
cover test results are unreliable because of the child's resistance to testing, other
m ethods m ay be used. In such cases, use of the H irschberg test is often successful
in infants 6 m onths and younger. Prism s can be used w ith the H irschberg test to
10.
align the corneal reflections (Krim sky test) and determ ine the m agnitude of the
deviation.
The Brckner test is another m eans of objectively assessing binocular vision, as w ell
as providing an indirect evaluation of refractive error. W hen both eyes are sim ulta-
neously illum inated w ith the ophthalm oscope beam at a distance of 100 cm , an
overall w hitening of the red reflex across the entire pupil of one eye indicates stra-
bism us or anisom etropic am blyopia. W hile the absence of a Brckner reflex is not
a good indication of alignm ent, the presence of a Brckner reflex is considered a
positive result, and is a good indication of strabism us, even of sm all am ounts.
O nce detected w ith the Brckner reflex, the deviation should be quantified w ith
the cover test or Krim sky technique.
A dditional binocular testing often can be perform ed successfully w ith infants and
toddlers. For exam ple, preferential looking techniques can be used to assess stere-
opsis w ith som e success.
17, 82,83
A ssessm ent of extraocular m uscle function and concom itancy m ay involve version
testing w ith an appropriate target. If the infant w ill follow a penlight, observation
of the corneal reflections in all cardinal positions of gaze is possible. W hen a prob-
lem is suspected, the cover test procedure should be used for the position of gaze
in question. A fter perform ing version testing, the clinician m ay find it useful to
m ove the penlight or other target tow ard the child to assess objectively the near
point of convergence (N PC ).
If a binocular vision disorder or an ocular m otility problem is suspected, consulta-
tion w ith an optom etrist or ophthalm ologist w ho has advanced clinical training or
experience w ith this population m ay be w arranted.
e. Ocular Health Assessment and Systemic Health Screening
A n evaluation of ocular health m ay include:
Evaluation of the ocular anterior segm ent and adnexa
Evaluation of the ocular posterior segm ent
A ssessm ent of pupillary responses
Visual field screening (confrontation).
The diagnosis of eye disease in infants and toddlers presents som e unique chal-
lenges. Standard procedures such as biom icroscopy, tonom etry, and binocular indi-
rect ophthalm oscopy are considerably m ore difficult in this population.
The cover test and versions, both im portant binocular vision assessm ent proce-
dures, are also im portant for ocular health assessm ent. For exam ple, the presence
of strabism us m ay indicate any num ber of disease entities such as neoplasm , neu-
rom uscular disorder, infection, vascular anom aly, or traum atic dam age.
84
11.
The exam iner perform ing external ocular evaluation should gather as m uch infor-
m ation as possible by gross inspection of the eyes and adnexa. G enerally, children
up to the age of 6-9 m onths are sufficiently attracted to lights to perm it adequate
evaluation using a penlight or transillum inator. W ith the older infant, it is im por-
tant to use a variety of interesting targets that can be attached to the transillum ina-
tor.
84
Pupil function (direct, consensual, and afferent pupil integrity) should also be
evaluated.
A hand-held biom icroscope m ay be used for evaluation of the anterior segm ent or
the parent/caregiver m ay be able to position and hold the infant or toddler in a
standard biom icroscope. If a corneal problem is suspected, but use of the biom i-
croscope is im possible, the optom etrist m ay attem pt an exam ination using sodium
fluorescein and a Burton lam p. A nother sim ple alternative is to use a self-illum inat-
ed, hand-held m agnifying lens, or a 20 D condensing lens w ith a light source.
Thorough evaluation of the ocular m edia and the posterior segm ent generally
requires pupillary dilation. Recom m ended drugs and dosages for pupillary dilation
in infants and toddlers are one drop each of tropicam ide (0.5% ) or cyclopentolate
(0.5% ) and one drop of phenylephrine (2.5% ).
84*
The spray m ixture discussed pre-
viously is effective in achieving both dilation and cycloplegia in the pediatric popu-
lation.
72
Both direct and binocular indirect ophthalm oscopy m ay be perform ed
after the pupil has dilated. A n ideal tim e for evaluation of the posterior segm ent is
w hen the infant is in a calm , relaxed, sedated condition (i.e., being bottle fed or
sound asleep).
44
W hen adequate fundus exam ination is im possible but is indicated
by patient history, exam ination under sedation or anesthesia m ay be w arranted.
M easuring intraocular pressure (IO P) is not a routine part of the eye exam ination of
the infant or toddler. A lthough it is extrem ely rare in this age group, glaucom a
m ay be suspected in the presence of a num ber of signs (e.g., corneal edem a,
increased corneal diam eter, tearing, and m yopia). M easurem ent of IO P is difficult
and the results often are unreliable.
43,85
H ow ever, pressure should be assessed
w hen ocular signs and sym ptom s or risk factors for glaucom a exist. M easurem ent
of IO P in the pediatric population m ay be accom plished w ith hand-held applana-
tion and noncontact tonom eters. If risk factors are present and reliable assessm ent
of IO P under standard clinical conditions is im possible, testing under sedation m ay
be appropriate.
W hen strabism us or other neurological problem s are suspected, confrontation visu-
al fields should be attem pted w ith infants and toddlers using a variation of the tra-
ditional approach.
86
A shift in fixation, head m ovem ent tow ard the target, or
change in facial expression of the infant can indicate that the target has m oved
from an unsighted to a sighted field.
43
The clinician should decide w hen im aging
studies are indicated, independently or in consultation w ith a neurosurgeon or neu-
rologist, on the basis of risk factors and the observation of ocular abnorm alities, or
signs such as nystagm us, developm ental delay, poor grow th, regression of skills,
and seizures.
* Drugs must be administered in accordance with provincial regulations.
12.
D uring the ocular health assessm ent and system ic health screening of infants and
children of any age, it is im portant to rem em ber that health care providers are
responsible for recognizing and reporting signs of child abuse, a significant problem
in the U nited States. Betw een 1990 and 1994 reported child abuse cases increased
27 percent, from 800,000 to 1,012,000, w ith alm ost half of the victim s under the
age of 6 years.
87
O ptom etrists have a uniquely im portant role in diagnosing child abuse including
Shaken Baby Syndrom e (SBS) because external eye traum a, and retinal traum a
(hem orrhages, folds, tears, detachm ents, and schisis) are com m on ocular findings
from child abuse.
88-90
SBS is a specific term used to describe a form of child abuse
in w hich the child is injured secondary to violent shaking, w hich often causes reti-
nal hem orrhaging. M ost often the child is betw een 2 and 18 m onths of age at the
tim e of abuse.
91,92
Suspected cases of child abuse should be reported to the appropriate authority.
This m ay be a social w orker associated w ith the fam ily or the child protection
agency. suspected child abuse or Failure to report a suspected case of child abuse
puts that child, his or her other siblings, and possibly a parent/caregiver in danger
of continued abuse at hom e.
f. Assessment and Diagnosis
U pon com pletion of the exam ination, the optom etrist assesses and evaluates the
data to arrive at one or m ore diagnoses and establishes a m anagem ent plan. In
som e cases, referral for consultation w ith or treatm ent by another optom etrist, the
patient's pediatrician, prim ary care physician, or other health care provider m ay be
indicated.
B. EXAMINATION OF PRESCHOOL CHILDREN
1. General Considerations
This section of the G uideline describes the optom etric exam ination procedures for
preschool children. The exam ination com ponents are discussed in general term s
and are not intended to be all inclusive. Professional judgm ent and individual
patient history, sym ptom s, findings, and cooperation m ay have significant im pact
on the nature and course of the exam ination.
A lthough the vast m ajority of children in this age group can com m unicate verbally,
it is preferable in m ost cases for the parent/caregiver to accom pany the child into
the exam ination room . It is im portant to ensure that the child feels relaxed and at
ease, w hich is often best accom plished by beginning the exam ination w ith proce-
dures that appear less threatening.
A ge-appropriate exam ination and m anagem ent strategies should be used w ith pre-
school children. M ajor m odifications include reliance on objective exam ination
techniques, lim ited use of subjective techniques requiring verbal interaction, and
13.
perform ing testing considerably m ore rapidly than is typically used for older chil-
dren.
2. Early Detection and Prevention
A com m on approach to early detection and prevention of vision problem s in pre-
school children is vision screening by pediatricians or other prim ary care physicians
or lay screeners. Screenings for this population are less problem atic than for
infants and toddlers because som e subjective testing is possible; how ever, screen-
ings are less accurate for preschool children than for older children.
93-95
Reasonably
accurate screening tests are available for the assessm ent of m any visual functions.
The problem w ith m any vision screenings, how ever, is that they are lim ited in
scope. They m ay detect only visual acuity problem s and m ay fail to detect other
im portant vision problem s, leading to parents' or caregivers' false sense of security.
A com prehensive eye exam ination at 3 years of age continues to be the m ost effec-
tive approach to prevention or early detection of eye and vision problem s in the
preschool child.
3. Examination Sequence
The pediatric eye and vision exam ination of the preschool child m ay include, but is
not lim ited to, the follow ing (see A ppendices Figure 3):
a. Patient History
A com prehensive patient history for the preschool child m ay include:
N ature of the presenting problem , including chief com plaint
Visual and ocular history
G eneral health history, including prenatal, perinatal, and postnatal history
and review of system s
Fam ily eye and m edical histories
D evelopm ental history of the child.
The collection of dem ographic data generally precedes the taking of the patient
history. H aving the parent(s) or caregiver(s) com plete a questionnaire in advance of
the exam ination facilitates obtaining the patient history.
43
b. Visual Acuity
A n assessm ent of visual acuity usually includes one of the follow ing procedures:
Lea Sym bols chart
Broken W heel acuity cards
H O TV test.
Kay Picture Test
14.
By 3 years of age, m ost children have the necessary behavioral and psychological
developm ent to allow subjective acuity testing. H ow ever, specially designed tests
are still useful to lim it the am ount of verbal interaction needed. The 3-year-old
child can easily m atch sim ple form s and responds w ell to learning through dem on-
stration and im itation of tasks.
95
Visual acuity tests for this age group ideally
involve a m atching task or a forced-choice task, such as pointing to the correct
response.
U se of the Broken W heel acuity cards is appropriate for this age group. Very little
verbal interaction is necessary, and the cards use a Landolt C target, considered the
optim um type of test for visual acuity.
96
This test has the added advantage of
established norm ative values.
97
The Lea Sym bols chart, w hich consists of four optotypes (circle, square, apple,
house), also can be used w ith great success.
98
The child sim ply has to find a
m atching block or point to the shape that m atches the target presented. This m ini-
m izes verbal interaction and m akes the test very useful for children betw een 30
m onths and 5 years. The Lea Sym bols chart is the first pediatric acuity test based
on the logM A R scale, as recom m ended by the N ational Research C ouncil
C om m ittee on Vision.
99
A study of the Lea Sym bols and H O TV charts found that
the tw o w ere com parable in 4- and 5-year-old children, but that in 3-year-olds, the
Lea Sym bols chart had better testability rates.
100
O nly 8 percent of children w ere
untestable w ith the Lea Sym bols chart. A nother study found that alm ost every
child older than 30 m onths could be tested w ith the Lea Sym bols chart.
101
The
H O TV test can also be com pleted by m any preschoolers.
c. Refraction
M easurem ent of refractive error m ay involve:
Static retinoscopy
C ycloplegic retinoscopy.
W ith tw o im portant m odifications, standard static (distance, non-cycloplegic)
retinoscopy can usually be perform ed in preschool children. A m odern video pro-
jection system is a valuable m eans of controlling accom m odation and fixation at 6
m eters. U sing a lens rack or loose lenses and fogging glasses rather than a
phoropter enables the clinician to see the child's face and observe w hen the child
loses fixation at 6 m eters.
C ycloplegic retinoscopy is a valuable procedure for the first evaluation of preschool-
ers and w hen static retinoscopy yields unreliable results or professional judgm ent
indicates otherw ise. This procedure should also be perform ed w hen strabism us or
significant refractive error is present. C yclopentolate (1% ) is the cycloplegic agent
of choice. Tw o drops should be instilled, one at a tim e, 5 m inutes apart, in each
eye.
71
The use of a spray bottle to adm inister the drug is also effective for this age
group. Retinoscopy m ay be perform ed w ith a lens rack or loose lenses 20 30 m in-
utes after instillation.
72
15.
d. Binocular Vision, Accommodation and Ocular Motility
The follow ing procedures are useful for assessing binocular and accom m odative
function:
C over test
Positive and negative fusional vergences (prism bar/step vergence testing)
N ear point of convergence (N PC )
Stereopsis
M onocular estim ation m ethod (M EM ) retinoscopy
Versions.
The cover test is the prim ary m eans of evaluating binocular vision in the preschool
child. It should be perform ed in the prim ary position and, if necessary, in other car-
dinal positions of gaze to screen for noncom itant deviations. W hen a deviation is
present, estim ation of the m agnitude or use of a prism bar enables m ore precise
m easurem ent. The results of the cover test can also be com bined w ith version test-
ing to rule out the presence of a noncom itant deviation.
If the cover test suggests a potentially significant heterophoria or interm ittent stra-
bism us, fusional vergence testing m ay be used to help determ ine w hether treat-
m ent m ay be indicated. Fusional vergence can be assessed objectively, using the
step vergence procedure.
103,104
To assess fusional vergence objectively, the clinician
uses a hand-held prism bar and carefully observes the patient's eyes, looking for a
loss of bifixation as the am ount of prism is gradually increased.
The N PC is an excellent test to use w ith the preschool child because both the break
and recovery m easurem ents can be determ ined objectively. Instead of asking the
child w hen he sees double, the clinician asks the child to keep looking at the target
as it is m oved closer. The clinician carefully observes the child's eyes and deter-
m ines w hen there is a loss of bifixation. The target is then m oved aw ay from the
child until bifixation is regained. U sing this procedure m akes it easy to determ ine
the N PC in a preschool child.
Stereopsis testing can generally be accom plished in preschool children, using com -
m ercially available stereopsis tests. To increase the ability to m easure stereopsis, it
is w ise to use a m atching procedure, in w hich the exam iner constructs a set of fig-
ures that correspond to the figures in the stereopsis test booklet and sim ply asks
the child to point to the picture he or she sees in the test booklet.
O bjective accom m odative testing can be perform ed in preschool children, using
M EM retinoscopy. M EM retinoscopy is easy to perform w ith children of this age
group and provides inform ation about the accom m odative response.
To assess extraocular m uscle function and concom itancy, it is im portant to perform
version testing in all cardinal positions of gaze, using a high-interest fixation target.
W hen a problem is suspected, the cover test procedure can be used in the relevant
position of gaze.
16.
e. Ocular Health Assessment and Systemic Health Screening
A n evaluation of ocular health m ay include:
Evaluation of the ocular anterior segm ent and adnexa
Evaluation of the ocular posterior segm ent
C olor vision testing
A ssessm ent of pupillary responses
Visual field screening (confrontation).
W ith som e m odification, traditional testing used to assess ocular health in adults
can be used in preschool children. M ost preschool children w ill cooperate, allow ing
the use of the biom icroscope to evaluate the anterior segm ent. Pupillary dilation
facilitates thorough evaluation of the posterior segm ent. W ith encouragem ent and
assistance from the parent, to help control fixation, binocular indirect ophthal-
m oscopy is often successful.
C olor vision testing can generally be done w ith standard pseudoisochrom atic
plates. A n alternative is the D 15 colour vision test w hich is often m anageable by
pre-schoolers w hen presented as a m atching/sorting test. O ther alternatives include
the Pease-A llen C olor Test (PA C T), the M r. C olor Test, or C olor Vision M ade Easy,
w hich do not require the child to identify a num ber. A ll of these tests are easy to
adm inister and have high testability rates in preschool children.
105-107
M easurem ent of IO P is not a routine part of the eye and vision exam ination of pre-
school children, but pressure should be assessed w hen ocular signs and sym ptom s
or risk factors for glaucom a exist. H and-held applanation or noncontact tonom e-
ters are available for the m easurem ent of IO P in this population. If it is not possible
to assess IO P reliably under standard clinical conditions, testing under sedation or
anesthesia m ay be appropriate.
C onfrontation visual fields testing should be attem pted w ith preschool children,
w hen indicated, using the techniques described for infants and toddlers. W hen the
results are equivocal or risk factors are present, the clinician should either retest the
child or consult w ith or refer the child to a pediatric ophthalm ologist or neurologist
for appropriate testing.
f. Supplemental Testing
W hen the preschool child's history indicates a possible developm ental lag or a
learning problem , the optom etrist m ay adm inister a developm ental visual perceptu-
al screening test to help diagnose and m anage visual inform ation-processing prob-
lem s. The testing can help assess developm ental level, detect visual perceptual dys-
function, and enable early identification of children at risk for the developm ent of
learning related vision problem s.
17.
The assessm ent of visual perceptual developm ent m ay include:
D enver D evelopm ental Screening Test (D D ST)
D evelopm ental Test of Visual M otor Integration (D TVM I)
Recom m ended for use in this age group,
108
the D D ST w as designed for use w ith
children from birth through 6 years of age. A nother test that can be used for
screening children as young as 3 years is the D TVM I.
109
W hen visual perceptual
problem s are detected, consultation w ith an optom etrist w ho has advanced clinical
training or experience w ith this population should be considered. Referral for con-
sultation w ith the child's pediatrician or other prim ary care physician or a child psy-
chologist or psychiatrist should also be considered w hen problem s in language and
social developm ent are detected.
g. Assessment and Diagnosis
U pon com pleting exam ination of the preschool-age child, the optom etrist assesses
and evaluates the data to establish the diagnosis and to form ulate a m anagem ent
plan. In som e cases, referral for consultation w ith or treatm ent by another
optom etrist, the patient's pediatrician or other prim ary care physician, or another
health care provider m ay be indicated.
C. EXAMINATION OF SCHOOL-AGE CHILDREN
1. General Considerations
This section of the G uideline describes the optom etric exam ination of the school-
age child. The discussion of exam ination com ponents is presented in general term s
and is not intended to be all inclusive. Professional judgm ent and individual patient
history, sym ptom s, findings, and cooperation m ay have significant im pact on the
nature and course of the exam ination.
Som e of the issues relating to infants, toddlers, and preschool children also apply to
this population, particularly children younger than 8 years old. A ge-appropriate
exam ination and m anagem ent strategies should be used. A lthough m ost of the
exam ination procedures used w ith this age group are identical to those recom -
m ended for adults, age-appropriate m odifications of instructions and targets often
m ay be required.
43
2. Early Detection and Prevention
The value of and need for school-based vision screening have been debated for
decades. O ne concern is that the m ajority of school vision screenings test only
visual acuity. Such testing prim arily detects am blyopia and m yopia, and only high
degrees of astigm atism and hyperopia. A lthough detection of such disorders is cer-
tainly a w orthw hile objective, screening for visual acuity alone generally detects
only about 30 percent of children w ho w ould fail a professional eye exam ination.
110
Visual acuity screening often fails to detect those conditions that w ould be expect-
18.
ed to affect learning. Parents or caregivers of children w ho pass vision screening
m ay incorrectly assum e that their children do not require further professional care.
3. Examination Sequence
The pediatric eye and vision exam ination of the school-age child m ay include, but is
not lim ited to, the follow ing (see A ppendices Figure 4):
a. Patient History
A com prehensive patient history for the school-age child m ay include:
N ature of the presenting problem , including chief com plaint
Visual and ocular history
G eneral health history, including prenatal, perinatal, and postnatal history
and review of system s
Fam ily eye and m edical histories
D evelopm ental history of the child
School perform ance history.
The collection of dem ographic data generally precedes taking the patient history.
H aving the parent(s) or caregiver(s) fill out a questionnaire facilitates obtaining the
patient history. Because of the relationship betw een vision and learning, special
attention needs to be paid to the child's school perform ance. W hen a child is not
perform ing up to potential, the optom etrist should probe for signs and sym ptom s
suggestive of a learning related vision problem .
111
* Q uestions can be designed to
define the specific nature of the learning problem and to distinguish disorders of
visual efficiency from a visual perceptual or nonvisual disorder.
112
b. Visual Acuity
Visual acuity m ay be assessed w ith the Snellen acuity chart (m odified for children 6-
8 years of age). A recom m ended m odification is the isolation of one line, or even
one-half line of letters, rather than projection of a full chart.
c. Refraction
M easurem ent of refractive error m ay involve use of the follow ing procedures:
Static (distance) retinoscopy
C ycloplegic retinoscopy
Subjective refraction.
For children over the age of 8, the clinician can usually use traditional assessm ent
procedures to m easure refractive error. For patients below age 8, static (distance)
retinoscopy m ay be perform ed w ithout a phoroptor, using a lens rack or loose lens-
es and fogging glasses. This procedure allow s the practitioner to m ove w ith the
child and to observe w hether the child is fixating properly. C ycloplegic refraction
19.
m ay be necessary in such conditions as strabism us, am blyopia, or significant hyper-
opia.
d. Binocular Vision, Accommodation, and Ocular Motility
Evaluation of binocular and accom m odative function and ocular m otility m ay
include the follow ing procedures:
C over test
N ear point of convergence (N PC )
Positive and negative fusional vergences
A ccom m odative am plitude and facility
M onocular estim ation m ethod (M EM ) retinoscopy
Stereopsis
Versions.
O ther than refractive errors, the m ost prevalent vision conditions in children fall into
the category of accom m odative and binocular vision anom alies.
41
These conditions
m ay interfere w ith school perform ance, causing a num ber of sym ptom s, including
eyestrain, blurred vision, double vision, loss of place, skipped lines, w ord m ovem ent
on the page, inability to sustain attention w hen reading, and decreased reading
com prehension over tim e.
109,113-119
C areful evaluation of these conditions in the
school-age population is critical.
Evaluation of accom m odation and fusional vergence should involve assessm ent of
both the am plitude and the facility of the response. For accom m odation, the eval-
uation m ay include assessm ent of accom m odative am plitude, accom m odative facili-
ty using +2.00/-2.00 D lenses, and accom m odative response using M EM
retinoscopy.
Binocular evaluation should include the cover test and tests of accom m odative con-
vergence/accom m odation (A C /A ) ratio, fusional vergence am plitude w ith either the
Risley prism s or the prism bar, vergence facility, and stereopsis, using a random dot
stereopsis test. A dditionally, negative relative accom m odation (N RA ) and positive
relative accom m odation (PRA ) tests m ay contribute to an understanding of both
accom m odation and binocular status. In analyzing these tests, it is im portant to
exam ine all data and group findings, rather than depending on any one isolated
finding, to arrive at a diagnosis.
120
Versions can be perform ed to rule out a noncom itant deviation. Q ualitative exam i-
nation of eye m ovem ents involves three distinct steps: assessm ent of stability of
fixation, saccadic function, and pursuit function. Subjective techniques involving
observation of the patient's fixation and eye m ovem ents have been developed,
along w ith rating scales, to probe these three areas.
121
20.
e. Ocular Health Assessment and Systemic Health Screening
A n assessm ent of ocular health m ay include:
Evaluation of the ocular anterior segm ent and adnexa
Evaluation of the ocular posterior segm ent
M easurem ent of intraocular pressure
C olor vision testing
A ssessm ent of pupillary responses
Visual field screening (confrontation).
Traditional testing procedures utilized for the evaluation of ocular health in adults
can be used w ith school-age children. M ost w ill cooperate and allow use of the
biom icroscope to evaluate the anterior segm ent and binocular indirect ophthal-
m oscopy to evaluate the posterior segm ent. Pupillary dilation allow s for thorough
evaluation of the posterior segm ent and m ay be repeated as needed at subsequent
visits.
122
The m easurem ent of IO P in school-age children is generally successful w ith either
applanation or noncontact tonom etry. A lthough the prevalence of glaucom a is low
in this population, a baseline m easurem ent at this age is valuable. Tonom etry m ay
be repeated as needed at subsequent visits.
If color vision testing w as not adm inistered w hen a preschool child, it should be
perform ed at this age. A s children enter school, it is helpful to know w hether a
color vision deficiency exists, because severe color vision deficiency m ay cause m is-
labeling of a child as learning disabled.
123
M oreover, color vision deficiency m ay
indicate an ocular health problem .
124
Evaluation of visual fields can be perform ed in school-age children using confronta-
tion visual field screening.
f. Assessment and Diagnosis
U pon com pletion of the exam ination, the optom etrist should assess and evaluate
the data to establish a diagnosis and to form ulate a m anagem ent plan. In som e
cases, referral for consultation w ith or treatm ent by another optom etrist, the
patient's pediatrician or other prim ary care physician, or another health care
provider m ay be indicated.
D. MANAGEMENT OF CHILDREN
1. Patient Education
D iscussion and com m unication w ith the parents or caregivers and the child should
occur at the end of the eye exam ination to review test findings. The optom etrist's
prim ary responsibility in this area is educating parents or caregivers about any eye
or vision disorders and vision care. M any parents and caregivers believe the screen-
21.
ing perform ed by the child's pediatrician or other prim ary care physician or school
nurse is sufficient to rule out all significant visual disorders. H ow ever, these screen-
ings are lim ited and w ere not intended to replace a com prehensive eye exam ination
The im portance of adhering to an eye and vision exam ination schedule should be
em phasized from a preventive standpoint as w ell. Early detection and preventive
care can help avoid, or m inim ize, the consequences of disorders such as am blyopia
and strabism us.
The optom etrist can also play an im portant role by educating parents/caregivers
and children about eye safety, particularly regarding sports-related eye safety.
Sports and recreational activities accounted for nearly 40,000 of the eye injuries
reported in 1991. Baseball injuries w ere the m ost frequent cause of eye injuries
am ong children 5-14 years of age.
125
A spectacle lens m aterial equivalent or supe-
rior in im pact resistance to that of 2m m polycarbonate or trivex is recom m ended
for use w ith children, except w hen such lenses w ill not fulfill the visual require-
m ents of the patient. For those cases in w hich protective lens m aterials are not
used, the optom etrist should obtain inform ed consent from parents and/or care-
givers.
O ptom etrists should educate parents or caregivers about the im portance of early,
preventive eye care, including exam inations at the age of 6 m onths, at age 3,
before entering first grade, and periodically during the school years. The extent to
w hich a child is at risk for the developm ent of eye and vision problem s determ ines
the appropriate re-evaluation schedule. Individuals w ith ocular signs and sym ptom s
require prom pt exam ination. Furtherm ore, the presence of certain risk factors m ay
necessitate m ore frequent exam inations, based on professional judgm ent (see Table
3).
Patient Age Asymptomatic / risk-
free
At-risk
Birth to 24 m onths A t 6 m onths of age A t 6 m onths of age
or as recom m ended
2 to 5 years A t 3 years of age A t 3 years of age or
as recom m ended
6 to 18 years Before first grade and
every 2 years thereafter
A nnually or as recom -
m ended
Recommended Eye Examiniation Frequency for the Pediatric Patient
Table 3
22.
2. Coordination, Frequency, and Extent of Care
The developing visual system is considered m ost susceptible to interference during
the first few years of life.
51,126-128
In the child of 6 m onths, vision has assum ed the
position of dom inant sense, and it w ill form the basis of later perceptual, cognitive,
and social developm ent.
129
M oreover, in the child of this age, vision has rapidly
developed in m ost crucial areas, including visual acuity, accom m odation, and stere-
opsis.
11-17
Interference during this critical phase of developm ent m ay be deleteri-
ous. For instance, abnorm alities present at birth and shortly thereafter, including
opacities of the ocular m edia (e.g., congenital cataract) and early-onset strabism us,
m ay have profound effects on the developing visual system . Thus, the efforts of
the child's pediatrician or other prim ary care physician are vital in the detection of
ocular abnorm alities that m ay require referral for an eye exam ination and treat-
m ent.
The child's first eye and vision exam ination should be scheduled at 6 m onths of age
(or sooner if signs or sym ptom s w arrant). W hen no abnorm alities are detected at
this age, the next exam ination should be scheduled at age 3.
The child considered at risk for the developm ent of eye and vision problem s m ay
need additional testing or m ore frequent re-evaluation. Factors placing an infant,
toddler, or child at significant risk for visual im pairm ent include:
Prem aturity, low birth w eight, prolonged supplem ental oxygen, or grade III
or IV intraventricular hem orrhage
Fam ily history of retinoblastom a, congenital cataracts, or m etabolic or
genetic disease
Infection of m other during pregnancy (e.g., rubella, toxoplasm osis, venere
al disease, herpes, cytom egalovirus, or hum an im m unodeficiency virus)
D ifficult or assisted labor, w hich m ay be associated w ith fetal distress or
low A pgar scores
H igh refractive error
Strabism us
A nisom etropia
Know n or suspected central nervous system dysfunction evidenced by
developm ental delay, cerebral palsy, dysm orphic features, seizures, or
hydrocephalus.
A n estim ated 17-25 percent of school-age children have vision problem s,
10
m any of
w hich m ay interfere w ith the children's abilities to reach their potential in school. It
is clear that all school-age children should have com prehensive eye and vision
exam inations, before entering the first grade and periodically thereafter. Som e chil-
dren m ay require m ore frequent care, depending on the nature of any diagnosed
eye or vision disorder.
23.
IV. CONCLUSION
C hildren account for a large percentage of the population of C anada. Studies have
dem onstrated that the prevalence of eye and vision disorders is substantial in this
group. Research also indicates that early detection and intervention are particularly
im portant in children because of the rapid developm ent of the visual system in
early childhood and its sensitivity to interference. W hen disorders such as am bly-
opia and strabism us are undetected, the long-term consequences can be serious in
term s of quality of life, com fort, appearance, and career opportunities. In addition,
the cost of providing appropriate treatm ent for longstanding eye and vision disor-
ders m ay be significantly higher than the cost of detecting and treating these prob-
lem s early in life.
25.
V. REFEREN C ES
1. W yngaarden JB. M edicine as a public service. In: W yngaarden JB, Sm ith LH , eds. C ecil's textbook
of m edicine, 18th ed, vol 1. Philadelphia: W B Saunders, 1988:7-8.
2. C atania LJ. Prim ary care. In: N ew com b RD , M arshall EC , eds. Public health and com m unity optom -
etry, 2nd ed. Boston: Butterw orths, 1990:295-310.
3. Statistics C anada. Population C ensus 2003, http://w w w .statcan.ca.
4. G erali P, Flom M C , Raab EL. Report of C hildren's Screening Task Force. Schaum burg, IL: N ational
Society to Prevent Blindness, 1990.
5. Poe G S. Eye care visits and use of eyeglasses or contact lenses. U nited States 1979 and 1980. Vital
and health statistics. Series 10, N o. 145, D H H S Publication (PH S) 84 1573, H yattsville, M D : N ational
C enter for H ealth Statistics, 1984.
6. Pizzarello L, Tilp M , Tiezzi L, et al. A new school-based program to provide glasses: C hildsight. J
A A PO S 1998; 6:372-4.
7. W asserm an RC , C roft C A , Brotherton SE. Preschool vision screening in pediatric practice: a study
from the Pediatric Research in O ffice Setting (PRO S) N etw ork. A m erican A cadem y of Pediatrics.
Pediatrics 1992; 89:834-8.
8. A m erican Public H ealth A ssociation. Im proving early childhood eyecare. Policy Statem ent N o. 20011.
W ashington, D C : A PH A , 2001.
9. A m erican Foundation for Vision Aw areness. C hildren's vision and literacy cam paign position paper.
St. Louis, M O : A FVA , 1993.
10. G rounds. A . Pediatric Eye C are. Blackw ell Science. O xford. 1995
11. D obson V, Teller D Y. Visual acuity in hum an infants: a review and com parison of behavioral and
electrophysiological studies. Vision Res 1978; 17:1469-83.
12. G w iazda J, Brill S, M ohindra I, H eld R. Preferential looking acuity in infants from tw o to fifty-eight
w eeks of age. A m J O ptom Physiol O pt 1980; 57:428-32.
13. Banks M S. The developm ent of visual accom m odation during early infancy. C hild D ev 1980;
51:646-66.
14. Brookm an KE. O cular accom m odation in hum an infants. A m J O ptom Physiol O pt 1983; 60:91-9.
15. Banks M S, A slin RN , Letson RD . Sensitive period for the developm ent of hum an binocular vision.
Science 1975; 190:675-7.
16. H ohm an A , C reutzfeldt O D . Squint and the developm ent of binocularity in hum ans. N ature 1975;
254:613-4.
17. C iner EB, Scheim an M M , Schanel-Klitsch E, W eil L. Stereopsis testing in 18- to 35- m onth-old chil-
dren using operant preferential looking. O ptom Vis Sci 1989; 66:782-7.
18. W iesel T, H ubel D . Effects of visual deprivation of m orphology and physiology of cells in the cat's
lateral geniculate body. J N europhysiol 1963; 26:578-85.
19. W iesel T, H ubel D . Single cell response in striate cortex of kittens deprived of vision in one eye. J
N europhysiol 1963; 26:1003-17.
20. M ohindra I, Jacobson SG , Thom as J, H eld R. D evelopm ent of am blyopia in infants. Trans
O phthalm ol Soc U K 1979; 99:344-6.
21. Epelbaum M , M illeret C , Buisseret P, D ufier JL. The sensitive period for strabism ic am blyopia in
hum ans. O phthalm ology 1993; 100:323-7.
22. A ngi M R, Pucci V, Forattini F, Form entin PA . Results of photorefractom etric screening for am blyo-
genic defects in children aged 20 m onths. Behav Brain Res 1992; 49(1):91 7.
23. N eum ann E, Freidm an Z, A bel-Peleg B. Prevention of strabism ic am blyopia of early onset w ith spe-
cial reference to the optim al age for screening. J Pediatr O phthalm ol Strabism us 1987; 24:106-10.
24. Eibschitz-Tsim honi M , Friedm an T, N aor J, et al. Early screening for am blyogenic risk factors low ers
the prevalence and severity of am blyopia. J A A PO S 2000; 4:194-9.
26.
25. Birch EE, H ale LA . O perant assessm ent of stereoacuity. C lin Vis Sci 1989; 4:295-300.
26. H ow land H C , A tkinson J, Braddick O , French J. Infant astigm atism m easured by photorefraction.
Science 1978; 202:331-3.
27. Fulton A B, D obson V, Salem D , et al. C ycloplegic refractions of infants and young children. A m J
O phthalm ol 1980; 90:239-47.
28. M ohindra I, H eld R. Refraction in hum ans from birth to five years. D oc O phthalm ol Proc 1981;
series 28:19-27.
29. H ow land H C , Sayles N . Photorefractive m easurem ents of astigm atism in infants and young children.
Invest O phthalm ol Vis Sci 1984; 25:93-102.
30. M ohindra I. A technique for infant vision exam ination. A m J O ptom Physiol O pt 1975; 52:867-70.
31. Tongue A C , C ibis G W . Brckner test. O phthalm ology 1981; 88:1041-4.
32. G w iazda J, W olfe JM , Brill S, et al. Q uick assessm ent of preferential looking acuity in infants. A m J
O ptom Physiol O pt 1980; 57:420-7.
33. M cD onald M , D obson V, Sebris SL, et al. The acuity card procedure: a rapid test of infant acuity.
Invest O phthalm ol Vis Sci 1985; 26:1158-62.
34. Birch E, W illiam s C , H unter J, Lapa M C , and the A LSPA C "C hildren in Focus" Study Team . Random
dot stereoacuity of preschool children. J Pediatr O phthalm ol Strabism us 1997; 34:217-22.
35. C iner EB, Schanel-Klitsch E, H erzberg C . Stereoacuity developm ent. 6 m onths to 5 years. A new
tool for testing and screening. O ptom Vis Sci 1996; 73:43-8.
36. O rel-Bixler D , Brodie A . Vision screening of infants and toddlers: photorefraction and stereoacuity.
Invest O phthalm ol Vis Sci 1995; 36(suppl):868.
37. A m erican O ptom etric A ssociation. Position paper: Recom m endations for regular optom etric care.
St. Louis, M O : A O A , 1994.
38. Roberts J. Eye exam ination findings am ong children, U nited States. Vital and health statistics, series
11, no. 115, D H EW publication (H SM ) 72-1057, H yattsville, M D : N ational C enter for H ealth Statistics,
1972.
39. Roberts J. Eye exam ination findings am ong children aged 12-17, U nited States. Vital and health
statistics, series 11, no. 155, D H EW publication (H RA ) 76-1637, H yattsville, M D : N ational C enter for
H ealth Statistics, 1975.
40. C iner EB, Schm idt PP, O rel-Bixler D , et al. Vision screening of preschool children: Evaluating the
past, looking tow ard the future. O ptom Vis Sci. 1998; 75:571 84.
41. Scheim an M , G allaw ay M , C oulter R, et al. Prevalence of vision and ocular disease conditions in a
clinical pediatric population. J A m O ptom A ssoc 1996; 67:193-202.
42. Rosner J, Rosner J. Pediatric optom etry, 2nd ed. Boston: Butterw orths, 1990:47-71.
43. Rouse M W , Ryan JM . The optom etric exam ination and m anagem ent of children. In: Rosenbloom
A A , M organ M W , eds. Principles and practice of pediatric optom etry. Philadelphia: JB Lippincott,
1990:155-91.
44. Press LJ, M oore BD . C linical pediatric optom etry. Boston: Butterw orth-H einem ann, 1993:25-80.
45. W hite BL. The first three years of life. Englew ood C liffs, N J: Prentice-H all, Inc., 1975:77-102.
46. C am pbell LR, C harney E. Factors associated w ith delay in diagnosis of childhood am blyopia.
Pediatrics 1991; 87:178-85.
47. H ow land H , H ow land B. Photorefraction: a technique for study of refractive error at a distance. J
O pt Soc A m 1974; 64:240-9.
48. A tkinson J, Braddick O . The use of isotropic photorefraction for vision screening in infants. A cta
O phthalm ol 1983; 157(suppl):36-45.
49. D uckm an R. U sing photorefraction to evaluate refractive error, ocular alignm ent, and accom m oda-
tion in infants, toddlers, and m ultiple handicapped children. Probl O ptom 1990; 2(3):333-53.
50. Preslan M W , Zim m erm an E. Photorefraction screening in prem ature infants. O phthalm ology 1993;
100:762-8.
27.
51. W right KW , Edelm an PM , W alonker F, Yiu S. Reliability of fixation preference testing in diagnosing
am blyopia. A rch O phthalm ol 1986; 104:549-53.
52. W right KW , W alonker F, Edelm an P. 10-D iopter fixation test for am blyopia. A rch O phthalm ol 1981;
99:1242-6.
53. W hittaker KW , O 'Flynn E, M anners RM . D iagnosis of am blyopia using the 10-diopter fixation test:
a proposed m odification for patients w ith unilateral ptosis. J Pediatr O phthalm ol Strabism us 2000;
37:21-3.
54. Law s D , N oonan C P, W ard A , C handna A . Binocular fixation pattern and visual acuity in children
w ith strabism ic am blyopia. J Pediatr O phthalm ol Strabism us 2000; 37(1):24-8.
55. Birch EE, Stager D R, Berry P, Everett M E. Prospective assessm ent of acuity and stereopsis in am bly-
opic infantile esotropes follow ing early surgery. Invest O phthalm ol Vis Sci 1990; 31:758-65.
56. W ilcox LM Jr, Sokol S. C hanges in binocular fixation patterns and the visually evoked potential in
the treatm ent of esotropia w ith am blyopia. O phthalm ology 1980; 87:1273 81.
57. M ayer D L, Fulton A B, H ansen RM . Preferential looking acuity obtained w ith a staircase procedure in
pediatric patients. Invest O phthalm ol Vis Sci 1982; 23:538-43.
58. Birch EE, N aegele J, Bauer JA , H eld R. Visual acuity of toddlers. Invest O phthalm ol Vis Sci 1980;
20(suppl):210.
59. Spierer A , Royzm an Z, C hetrit A , et al. Vision screening of preverbal children w ith Teller acuity cards.
O phthalm ology 1999; 106:849-54.
60. Birch EE, Stager D R. M onocular acuity and stereopsis in infantile esotropia. Invest O phthalm ol Vis
Sci 1985; 26:1624-30.
61. M ohn G , van H of-van D uin J, Fetter W PF, et al. A cuity assessm ent of non-verbal infants and chil-
dren: clinical experience w ith the acuity card procedure. D ev M ed C hild N eurol 1988; 30(suppl):232-
44.
62. Stager D R, Birch EE. Preferential-looking acuity and stereopsis in infantile esotropia. J Pediatr
O phthalm ol Strabism us 1986; 23:160-5.
63. M ayer D L, Fulton A B, Rodier D . G rating and recognition acuities of pediatric patients.
O phthalm ology 1984; 91:947-53.
64. M ayer D L. A cuity of am blyopic children for sm all field gratings and recognition stim uli. Invest
O phthalm ol Vis Sci 1986; 27:1148-53.
65. Ellis G S Jr., H artm ann EE, Love A , et al. Teller acuity cards versus clinical judgm ent in the diagnosis
of am blyopia w ith strabism us. O phthalm ology 1988; 95:788-91.
66. Sokol S, M oskow itz A . C om parison of pattern VEPs and preferential-looking behavior in 3-m onth-
old infants. Invest O phthalm ol Vis Sci 1985; 26:359-65.
67. Riddell PM , Ladenheim B, M ast J, et al. C om parison of visual acuity in infants: Teller acuity cards
and sw eep visual evoked potentials. O ptom Vis Sci 1997; 74:702-7.
68. Prager TC , Zou YL, Jensen C L, et al. Evaluation of m ethods for assessing visual function of infants.
J A A PO S 1999; 3:275-82.
69. C iner EB. M anagem ent of refractive error in infants, toddlers and preschool children. Probl O ptom
1990; 2:394-419.
70. G ray L. Avoiding adverse effects of cycloplegics in infants and children. J A m O ptom A ssoc 1979;
50:465-70.
71. A m os JF. C ycloplegic refraction. In: Bartlett JD , Jaanus SD , eds. C linical ocular pharm acology, 4th
ed. Boston: Butterw orth-H einem ann, 2001:425-32.
72. Bartlett JD , W esson M D , Sw iatocha J, W oolley T. Efficacy of a pediatric cycloplegic adm inistered as a
spray. J A m O ptom A ssoc 1993; 64:617-21.
73. Ism ail EE, Rouse M W , D e Land PN . A com parison of drop instillation and spray application of 1%
cyclopentolate hydrochloride. O ptom Vis Sci 1994; 71:235-41.
74. H ug T, C ibis G W , Lynd J. The use of spray topical drug delivery system for cycloplegic m edications in
children. Binocular Vis Strabism us Q 1997;12:191-4.
28.
75. Tw elker JD , M utti D O . Retinoscopy in infants using a near noncycloplegic technique, cycloplegia
w ith tropicam ide 1% , and cycloplegia w ith cyclopentolate 1% . O ptom Vis Sci 2001; 78(4):215-22.
76. Saunders KJ, W esthall C A . C om parison betw een near retinoscopy and cycloplegic retinoscopy in the
refraction of infants and children. O ptom Vis Sci 1992; 69:615-22.
77. Borghi RA , Rouse M W . C om parison of refraction obtained by "near retinoscopy" and retinoscopy
under cycloplegia. A m J O ptom Physiol O pt 1985; 62:169-72.
78. W esson M D , M ann KR, Bray N W . A com parison of cycloplegic refraction to near retinoscopy tech-
nique for refractive error determ ination. J A m O ptom A ssoc 1990; 61:680-4.
79. Banks M . Infant refraction and accom m odation. Int O phthalm ol C lin 1980; 20(1):205 32.
80. G w iazda J, M ohindra I, Brill S, H eld R. Infant astigm atism and m eridional am blyopia. Vision Res
1985; 25:1269-76.
81. M ohindra I, H eld R, G w iazda J, Brill S. A stigm atism in infants. Science 1978; 202:329-30.
82. C iner EB, Schanel-Klitsch E, H erzberg C . Stereoacuity developm ent: 6 m onths to 5 years. A new
tool for testing and screening. O ptom Vis Sci 1996; 73:43-8.
83. Birch EE, Salom ao S. Infant random dot stereoacuity cards. J Pediatr O phthalm ol Strabism us 1998;
35:86-90.
84. Frantz K. D iagnosis and m anagem ent of com m on eye disease in infants, toddlers and preschool
children. Probl O ptom 1990; 2:420-37.
85. A m erican A cadem y of O phthalm ology. Preferred practice pattern: com prehensive pediatric eye
evaluation. San Francisco: A A O , 1992.
86. A ppel S, Steciw M , G raboyes M , C ote KS. M anaging the child w ith special needs. J Vision
Rehabil (H ouston) 1985; 1:2-8.
87. Yoo R, Logani S, M ahat M , et al. Vision screening of abused and neglected children by the U C LA
M obile Eye C linic. J A m O ptom A ssoc 1999; 70:461-9.
88. Kivlin JD , Sim ons KB, Lazoritz S, Ruttum M S. Shaken baby syndrom e. O phthalm ology 2000;
107:1246-54.
89. M ills M . Funduscopic lesions associated w ith m ortality in shaken baby syndrom e. J A A PO S 1998;
2:67-71.
90. U .S. D epartm ent of H ealth and H um an Services. C hild M altreatm ent 1994: Reports from the States
for the N ational C enter on C hild A buse and N eglect. W ashington, D C : U .S. G overnm ent Printing O ffice,
1994.
91. Budenz D L, Farber M G , M irchandani H G , et al. O cular and optic nerve hem orrhages in abused
infants w ith intracranial injuries. O phthalm ology 1994; 101:559-65.
92. H an D P, W ilkinson W S. Late ophthalm ic m anifestations of the shaken baby syndrom e. J Pediatr
O phthalm ol Strabism us 1990; 27:299-303.
93. D e Becker I, M acPhearson H J, LaRoche G R, et al. N egative predictive value of a population-based
preschool vision screening program . O phthalm ology 1992; 99:998 1003.
94. Fern KD . A com parison of vision screening techniques in preschool children. Invest O phthalm ol Vis
Sci 1991; 32(4;suppl):962.
95. Richm an JE. A ssessm ent of visual acuity in preschool children. Probl O ptom , 1990; 2:319-32.
96. H ofstetter H W . N ew standards and procedures for m easuring visual acuity. J A m O ptom A ssoc
1981; 52:321-7.
97. M cD onald M , C haudry N M . C om parison of four m ethods of assessing visual acuity in young chil-
dren. O ptom Vis Sci 1989; 66:363-9.
98. H yvrinen L, N snen R, Laurinen P. N ew visual acuity test for pre-school children. A cta O phthalm ol
1980; 58:507-11.
99. A ssem bly of Behavioral and Social Sciences, N ational Research C ouncil, N ational A cadem y of
Sciences. C om m ittee on Vision. Recom m ended standard procedures for the clinical m easurem ent and
specification of visual acuity. Report of W orking G roup 39. A dv O phthalm ol 1980; 41:103-48.
29.
100. H ered R, M urphy S, C lancy M . C om parison of the H O TV and Lea Sym bols charts for preschool
vision screening. J Pediatr O phthalm ol Strabism us 1997; 34:24-8.
101. Becker R, H bsch S, G rf M H , Kaufm ann H . Prelim inary report: exam ination of young children
w ith Lea sym bols. Strabism us 2000; 8:209-13.
102. M oore B. Vision in Preschoolers Study G roup. C om paring the usability of tw o visual acuity tests
w ith preschool age children. O ptom Vis Sci 2000; 77(suppl):280.
103. W esson M D . N orm alization of prism bar vergences. A m J O ptom Physiol O pt 1982; 59: 628 34.
104. Scheim an M , H erzberg H , Frantz K, M argolies M . A norm ative study of step vergence in elem en-
tary schoolchildren. J A m O ptom A ssoc 1989; 60:276 80.
105. Pease PL, A llen J. A new test for screening vision: concurrent validity and utility. A m J O ptom
Physiol O pt 1988; 65:729-38.
106. Ventocilla M , O rel-Bixler D , H aegerstrom -Portnoy G . Pediatric color vision screening: A O H RR vs.
M r. C olor. O ptom Vis Sci 1995; 72(suppl):203.
107. C iner EB. Exam ination procedures for infants and young children. In: M oore BD , ed. Eye care for
infants and young children. Boston: Butterw orth-H einem ann, 1997:85.
108. M iller LJ, Sprong TA . Psychom etric and qualitative com parison of four preschool screening instru-
m ents. J Learn D isabil 1986; 19:480-4.
109. Scheim an M , Rouse M W . O ptom etric m anagem ent of learning related vision disorders. St. Louis,
M O : C V M osby, 1994:321-2.
110. Blum H L, Peters H B, Bettm an JW . Vision screening for elem entary schools. The O rinda Study.
Berkeley: U niversity of C alifornia Press, 1959:36-55.
111. A m erican O ptom etric A ssociation. C linical Practice G uideline on C are of the Patient w ith Learning
Related Vision Problem s. St. Louis, M O : A O A , 2000.
112. C otter S. O ptom etric assessm ent: C ase history. In: Scheim an M M , Rouse M W , eds. O ptom etric
m anagem ent of learning related vision problem s. St. Louis, M O : M osby Year Book, 1994.
113. D uke-Elder S. System of ophthalm ology, vol V. O phthalm ic optics and refraction. St. Louis, M O :
C V M osby, 1970:451-86.
114. D aum KM . A ccom m odative dysfunction. D oc O phthalm ol 1983; 55:177-98.
115. H ennessey D , Iosue R, Rouse M W . Relation of sym ptom s to accom m odative infacility of school
aged children. A m J O ptom Physiol O pt 1984; 61:177-83.
116. H addad H M , Isaacs N S, O nghena K, M azor A . The use of orthoptics in dyslexia. J Learn
D isabil 1984; 17:142-4.
117. Sheedy JE, Saladin JJ. A ssociation of sym ptom s w ith m easures of oculom otor deficiencies. A m J
O ptom Physiol O pt 1987; 55:670-6.
118. Ludlam W M , Ludlam D E. Effects of prism -induced accom m odative convergence stress on reading
com prehension. J A m O ptom A ssoc 1988; 59:440-5.
119. G arzia RP, N icholson SB, G aines C S, et al. Effects of nearpoint visual stress on psycholinguistic pro-
cessing in reading. J A m O ptom A ssoc 1989; 60:38-44.
120. Scheim an M , W ick B. C linical m anagem ent of binocular vision, 2nd ed. Philadelphia: JB
Lippincott, 2002:26-81.
121. M aples W C , A tchley J, Ficklin TW . N ortheastern State U niversity C ollege of O ptom etry's oculom o-
tor norm s. J Behav O ptom 1992; 3:143-50.
122. Parisi M L, Scheim an M , C oulter RS. C om parison of the effectiveness of a nondilated versus dilated
fundus exam ination in the pediatric population. J A m O ptom A ssoc 1996; 67:266-72.
123. G nadt G R, A m os JF. D ichrom acy and its effect on a young m ale. J A m O ptom A ssoc 1992;
63:475-80.
124. H agerstrom -Portnoy G . C olor vision. In: Rosenbloom A A , M organ M W , eds. Principles and prac-
tice of pediatric optom etry. Philadelphia: JB Lippincott, 1990:449 66.
30.
125. N ational Society to Prevent Blindness, N ational C enter for Sight. 1991 eye injuries associated w ith
sports and recreational products. Schaum burg, IL: N SPB, 1992.
126. von N oorden G K, C raw ford M LJ. The sensitive period. Trans O phthalm ol Soc U K 1979; 99:442-6.
127. Petrig B, Julesz B, Kropfl W , et al. D evelopm ent of stereopsis and cortical binocularity in hum an
infants: electrophysiological evidence. Science 1981; 213:1402 5.
128. M ohindra I, Jacobson SG , H eld R. Binocular visual form deprivation in hum an infants. D oc
O phthalm ol 1983; 55:237-49.
129. A tkinson J. H um an visual developm ent over the first 6 m onths of life. A review and a hypothesis.
H um N eurobiol 1984; 3:61-74.
31.
VI. APPENDICES
Figure 1
32.
Figure 2
Potential Components of the Eye and Vision Examination
for Infants and Toddlers
A . Patient H istory
1. N ature of the presenting problem , including chief com plaint
2. Visual and ocular history
3. G eneral health history, including prenatal, perinatal, and postnatal history
and review of system s
4. Fam ily eye and m edical histories
5. D evelopm ental history of the child
B. Visual A cuity
1. Fixation preference tests
2. Preferential looking visual acuity test
C . Refraction
1. C ycloplegic retinoscopy
2. N ear retinoscopy
D . Binocular Vision and O cular M otility
1. C over test
2. H irschberg test
3. Krim sky test
4. Brckner test
5. Versions
6. N ear point of convergence
E. O cular H ealth A ssessm ent and System ic H ealth Screening
1. Evaluation of the ocular anterior segm ent and adnexa
2. Evaluation of the ocular posterior segm ent
3. A ssessm ent of pupillary responses
4. Visual field screening (confrontation)
F. Supplem ental Testing
1. Electrodiagnostic testing
33.
Figure 3
Potential Components of the Eye and Vision Examination
for Preschool Children
A . Patient H istory
1. N ature of the presenting problem , including chief com plaint
2. Visual and ocular history
3. G eneral health history, including prenatal, perinatal, and postnatal history
and review of system s
4. Fam ily eye and m edical histories
5. D evelopm ental history of the child
B. Visual A cuity
1. Lea Sym bols chart
2. Broken W heel acuity cards
3. H O TV test
C . Refraction
1. Static retinoscopy
2. C ycloplegic retinoscopy
D . Binocular Vision, A ccom m odation, and O cular M otility
1. C over test
2. Positive and negative fusional vergences (prism bar/step vergence testing)
3. N ear point of convergence
4. Stereopsis
5. M onocular estim ation m ethod (M EM ) retinoscopy
6. Versions
E. O cular H ealth A ssessm ent and System ic H ealth Screening
1. Evaluation of the ocular anterior segm ent and adnexa
2. Evaluation of the ocular posterior segm ent
3. C olor vision testing
4. A ssessm ent of pupillary responses
5. Visual field screening (confrontation)
F. Supplem ental Testing
1. D enver D evelopm ental Screening Test (D D ST)
2. D evelopm ental Test of Visual M otor Integration (D TVM I)
34.
Figure 4
Potential Components of the Eye and Vision Examination
for School-Age Children
A . Patient H istory
1. N ature of the presenting problem , including chief com plaint
2. Visual and ocular history
3. G eneral health history, including prenatal, perinatal, and postnatal history
and review of system s
4. Fam ily eye and m edical histories
5. D evelopm ental history of the child
6. School perform ance history
B. Visual A cuity
1.Snellen acuity chart (w ith m odification for children 6-8 years of age)
C . Refraction
1. Static retinoscopy
2. Subjective refraction
D . Binocular Vision, A ccom m odation, and O cular M otility
1. C over test
2. N ear point of convergence
3. Positive and negative fusional vergences
4. A ccom m odative am plitude and facility
5. M onocular estim ation m ethod (M EM ) retinoscopy
6. Stereopsis
7. Versions
E. O cular H ealth A ssessm ent and System ic H ealth Screening
1. Evaluation of the ocular anterior segm ent and adnexa
2. Evaluation of the ocular posterior segm ent
3. M easurem ent of intraocular pressure
4. C olor vision testing
5. A ssessm ent of pupillary responses
6. Visual field screening (confrontation)
F. Supplem ental Testing
1. D irectionality
2. Visual m otor integration
Abbreviations of Commonly Used Terms
A C /A - A ccom m odative convergence/accom m odation ratio
D - D iopter
D D ST - D enver D evelopm ental Screening Test
D TVM I - D evelopm ental Test of Visual M otor Integration
IO P - Intraocular pressure
M EM - M onocular estim ation m ethod
N PC - N ear point of convergence
N RA - N egative relative accom m odation
PA C T - Pease-A llen color test
PD - Prism diopter
PRA - Positive relative accom m odation
SBS - Shaken baby syndrom e
35.
Glossary
Accommodation The ability of an eye to focus clearly on objects at various dis-
tances, or through various lens pow ers, resulting from changes in shape of the
crystalline lens.
Adnexa The accessory structures of the eye, including the eyelids, lacrim al appara-
tus, and the extraocular m uscles.
Anterior ocular segment The part of the eye including and anterior to the crys-
talline lens (i.e., cornea, anterior cham ber, iris, ciliary body).
Color vision The ability to perceive differences in color.
Cover test A clinical test to determ ine the ocular alignm ent of the eyes and m eas-
ure the m agnitude of the angle of deviation of the visual axes.
Directionality The ability to understand and identify right and left directions in
external visual space.
Intraocular pressure (IOP) The pressure w ithin the eye relative to the constant
form ation and drainage of aqueous hum or.
Near point of convergence (NPC) The m axim al extent the eyes can be con-
verged, using tonic, accom m odative, fusional, and proxim al convergence.
Negative relative accommodation (NRA) A m easure of the ability to relax
accom m odation w hile m aintaining binocular vision at a fixed distance, usually 40
cm . M easurem ent is m ade w ith plus-lens additions until the patient reports the
first sustained blurring of the target.
Positive relative accommodation (PRA) A m easure of the ability to stim ulate
accom m odation w hile m aintaining binocular vision at a fixed distance, usually 40
cm . M easurem ent is m ade w ith m inus-lens additions until the patient reports the
first sustained blurring of the target.
Posterior ocular segment The part of the eye located posterior to the crystalline
lens (i.e., vitreous, choroid, retina, optic nerve).
Pupillary response The response of the pupils of the eyes to stim ulation by light
or accom m odation.
Refraction C linically, the determ ination of the refractive errors of an eye, or eyes
(e.g., m yopia, hyperopia, astigm atism , anisom etropia).
Refractive status (refractive error) The degree to w hich im ages received by the
eyes are not focused on the retina (e.g., m yopia, hyperopia, astigm atism ).
36.
Stereopsis Binocular visual perception of three-dim ensional space, based on reti-
nal disparity. C linically referred to as depth perception.
Suppression U nder binocular view ing conditions, the inability to perceive all or
part of objects in the field of vision of one eye, attributed to cortical inhibition.
Vergence D isjunctive m ovem ents of the eyes in w hich the visual axes m ove
tow ard each other w ith convergence or aw ay from each other w ith divergence.
Version C onjugate m ovem ent in w hich the tw o eyes m ove in the sam e direction.
Visual acuity The clearness of vision that depends on the sharpness of the retinal
im age and the integrity of the retina and visual pathw ay. It is expressed as the
angle subtended at the anterior focal point of the eye by the detail of the letter or
sym bol recognized.
Visual field The area or extent of space visible to an eye in a given position.
Visual motor integration The ability to integrate visual inform ation w ith fine
m otor m ovem ents.
Sources:
H ofstetter H W , G riffin JR, Berm an M S, Everson RW . D ictionary of visual science
and related clinical term s, 5th ed. Boston: Butterw orth-H einem ann, 2000.
G rosvenor TP. Prim ary care optom etry. A nom alies of refraction and binocular
vision, 4th ed. Boston: Butterw orth-H einem ann, 2002:567-80.
37.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Vision TestDocument93 pagesVision TestAr JayNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Incomitant SquintDocument41 pagesIncomitant Squintshreeja maheshwari100% (3)
- Bab 01 PDFDocument32 pagesBab 01 PDFAbdul Rahman B. NarawiNo ratings yet
- Forensic PhotographyDocument11 pagesForensic Photographyfilibertpatrick_tad-awanNo ratings yet
- Polaroid Onestep Se (AKA Polaroid 1000)Document35 pagesPolaroid Onestep Se (AKA Polaroid 1000)Dominykas BorsakNo ratings yet
- Part and Mold Design GuideDocument170 pagesPart and Mold Design GuideminhtintinNo ratings yet
- Khurana - Review of Ophthalmology-Jaypee Brothers Medical Publishers (2015) PDFDocument178 pagesKhurana - Review of Ophthalmology-Jaypee Brothers Medical Publishers (2015) PDFasdfasdf100% (5)
- Photography Guide Nikon School PDFDocument16 pagesPhotography Guide Nikon School PDFDayanandKambleNo ratings yet
- PANTONE Coated Color Reference: PrinterDocument19 pagesPANTONE Coated Color Reference: PrinterMichel Valentina Escobar TorresNo ratings yet
- Q.No. Type Section Key/Range MarksDocument3 pagesQ.No. Type Section Key/Range Marksbiotech_vidhyaNo ratings yet
- Stripping For ReprobingDocument2 pagesStripping For ReprobingStella SalvatoreNo ratings yet
- BT 2019Document13 pagesBT 2019biotech_vidhyaNo ratings yet
- SDS PageDocument2 pagesSDS Pagebiotech_vidhyaNo ratings yet
- Stripping For ReprobingDocument2 pagesStripping For ReprobingStella SalvatoreNo ratings yet
- Facs ProtocolDocument7 pagesFacs ProtocolmisterxNo ratings yet
- Troubleshooting SDS-PAGE 1Document3 pagesTroubleshooting SDS-PAGE 1biotech_vidhyaNo ratings yet
- Components Reaction MixtureDocument3 pagesComponents Reaction Mixturebiotech_vidhyaNo ratings yet
- TNPSC Group 1 Prelim Book List PDFDocument2 pagesTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaNo ratings yet
- Polymerase Chain Reaction (PCR)Document3 pagesPolymerase Chain Reaction (PCR)biotech_vidhyaNo ratings yet
- Brad FordDocument12 pagesBrad FordQi ChaoNo ratings yet
- Whole Cell ExtractDocument1 pageWhole Cell Extractbiotech_vidhyaNo ratings yet
- Buffer Preparation Guide for DNA/Protein Work (Shi LabDocument6 pagesBuffer Preparation Guide for DNA/Protein Work (Shi Labbiotech_vidhyaNo ratings yet
- Polymerasen GuideDocument16 pagesPolymerasen Guidebiotech_vidhyaNo ratings yet
- Buffer Preparation Guide for DNA/Protein Work (Shi LabDocument6 pagesBuffer Preparation Guide for DNA/Protein Work (Shi Labbiotech_vidhyaNo ratings yet
- Qpaper PondyDocument21 pagesQpaper Pondybiotech_vidhyaNo ratings yet
- Nuclear ExtractsDocument2 pagesNuclear Extractsbiotech_vidhyaNo ratings yet
- TNPSC Group 1 Prelim Book List PDFDocument2 pagesTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaNo ratings yet
- Befcv List PDFDocument22 pagesBefcv List PDFbiotech_vidhyaNo ratings yet
- TNPSC Group 1 Prelim Book List PDFDocument2 pagesTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaNo ratings yet
- Ies 17 Set A Me Q ADocument67 pagesIes 17 Set A Me Q Abiotech_vidhyaNo ratings yet
- Recruitment RulesDocument5 pagesRecruitment Rulesbiotech_vidhyaNo ratings yet
- Mechanical Engineering Code No. 14: Combined Competitive (Preliminary) Examination, 2010Document20 pagesMechanical Engineering Code No. 14: Combined Competitive (Preliminary) Examination, 2010biotech_vidhyaNo ratings yet
- ESE 2017 Mechanical Engineering Prelims Exam Detailed SolutionDocument52 pagesESE 2017 Mechanical Engineering Prelims Exam Detailed SolutionpataNo ratings yet
- Img Word-To PDFDocument3 pagesImg Word-To PDFbiotech_vidhyaNo ratings yet
- TDC 41597 A (Mechanical Engg.) - 2012Document20 pagesTDC 41597 A (Mechanical Engg.) - 2012biotech_vidhyaNo ratings yet
- A.E. (Mechanical Engineering I) 2007Document24 pagesA.E. (Mechanical Engineering I) 2007Mukesh KumarNo ratings yet
- 1 TolerancesDocument1 page1 Tolerancesbiotech_vidhyaNo ratings yet
- Qpaper PondyDocument21 pagesQpaper Pondybiotech_vidhyaNo ratings yet
- Humanoid Robot Industry PowerPoint TemplatesDocument48 pagesHumanoid Robot Industry PowerPoint TemplatesOsman PetitNo ratings yet
- Digital Image Processing LAB MANUAL 6th Sem-FinalDocument20 pagesDigital Image Processing LAB MANUAL 6th Sem-FinalKapil KumarNo ratings yet
- The Art of Photography - Capturing Moments and ExpressionsDocument24 pagesThe Art of Photography - Capturing Moments and ExpressionsMarvin ManaloNo ratings yet
- Detect Faces with Color Segmentation and Template MatchingDocument3 pagesDetect Faces with Color Segmentation and Template MatchingAjith Kumar MNo ratings yet
- CMNHospitals UsageGuide USDocument14 pagesCMNHospitals UsageGuide USanoopots434No ratings yet
- Group B - Sensory PhysiologyDocument25 pagesGroup B - Sensory PhysiologyShane Margauxh AlabastroNo ratings yet
- Nikon D810 Experience-Setup GuideDocument28 pagesNikon D810 Experience-Setup GuidefaisluNo ratings yet
- Photography - December 2023Document16 pagesPhotography - December 2023ArtdataNo ratings yet
- DanilocvDocument4 pagesDanilocvapi-196000379No ratings yet
- Red Cat Reading Level 1 Farm AnimalsDocument19 pagesRed Cat Reading Level 1 Farm Animalssusie wangNo ratings yet
- Panasonic TC-P50GT30 CNET Review Calibration ResultsDocument7 pagesPanasonic TC-P50GT30 CNET Review Calibration ResultsDavid KatzmaierNo ratings yet
- SAYANSDocument6 pagesSAYANSEzekiel LandonNo ratings yet
- Categories of HologramsDocument2 pagesCategories of HologramsChanNo ratings yet
- Lesson Plan in Arts: I. ObjectivesDocument10 pagesLesson Plan in Arts: I. ObjectivesSarmiento JudyNo ratings yet
- NCM 116 Lect Visual PerceptionDocument45 pagesNCM 116 Lect Visual PerceptionMariano MarbellaNo ratings yet
- Eci BVDM Graycon Doc Eng v2Document17 pagesEci BVDM Graycon Doc Eng v2Donato PaceNo ratings yet
- Lesson Plans - VisionDocument5 pagesLesson Plans - VisionZach SanfordNo ratings yet
- Ch00 History of Art Study IntroductionDocument7 pagesCh00 History of Art Study Introductionsadiq anwar hasrutNo ratings yet
- CSS Part 2Document27 pagesCSS Part 2Mariam mariNo ratings yet
- Underwater Image Enhancement Based On Red ChannelDocument10 pagesUnderwater Image Enhancement Based On Red ChannelMustafa Kemal AmbarNo ratings yet
- Anatomi Dan Fisiologi Mata 1Document61 pagesAnatomi Dan Fisiologi Mata 1MAWANNo ratings yet
- Conjunctival-Limbal Autograft Effective for Primary, Recurrent PterygiumDocument3 pagesConjunctival-Limbal Autograft Effective for Primary, Recurrent PterygiumMichael HumiantoNo ratings yet