Professional Documents
Culture Documents
Acupuncture or Acupressure For Pain Management in Labour (Review)
Uploaded by
Serbaguna MantapOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acupuncture or Acupressure For Pain Management in Labour (Review)
Uploaded by
Serbaguna MantapCopyright:
Available Formats
Acupuncture or acupressure for pain management in labour
(Review)
Smith CA, Collins CT, Crowther CA, Levett KM
This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library
2011, Issue 8
http://www.thecochranelibrary.com
Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
T A B L E O F C O N T E N T S
1 HEADER . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
1 ABSTRACT . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
2 PLAIN LANGUAGE SUMMARY . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
2 BACKGROUND . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
4 OBJECTIVES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
4 METHODS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
8 RESULTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
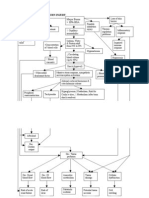
Figure 1. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9
Figure 2. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10
14 DISCUSSION . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
15 AUTHORS CONCLUSIONS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
16 ACKNOWLEDGEMENTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
16 REFERENCES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
19 CHARACTERISTICS OF STUDIES . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
39 DATA AND ANALYSES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Analysis 1.1. Comparison 1 Acupuncture versus control, Outcome 1 Pain intensity. . . . . . . . . . . . . 41
Analysis 1.2. Comparison 1 Acupuncture versus control, Outcome 2 Satisfaction with pain relief in labour. . . . . 42
Analysis 1.3. Comparison 1 Acupuncture versus control, Outcome 3 Use of pharmacological analgesia. . . . . . 43
Analysis 1.4. Comparison 1 Acupuncture versus control, Outcome 4 Caesarean section. . . . . . . . . . . 44
Analysis 1.5. Comparison 1 Acupuncture versus control, Outcome 5 Assisted vaginal birth. . . . . . . . . . 45
Analysis 1.6. Comparison 1 Acupuncture versus control, Outcome 6 Apgar score < 7 at 5 minutes. . . . . . . 46
Analysis 1.7. Comparison 1 Acupuncture versus control, Outcome 7 Spontaneous vaginal delivery. . . . . . . 47
Analysis 1.8. Comparison 1 Acupuncture versus control, Outcome 8 Augmentation with oxytocin. . . . . . . 48
Analysis 1.9. Comparison 1 Acupuncture versus control, Outcome 9 Relaxation. . . . . . . . . . . . . . 49
Analysis 2.1. Comparison 2 Acupressure versus control, Outcome 1 Pain intensity. . . . . . . . . . . . . 50
Analysis 2.2. Comparison 2 Acupressure versus control, Outcome 2 Satisfaction with childbirth. . . . . . . . 50
Analysis 2.3. Comparison 2 Acupressure versus control, Outcome 3 Use of pharmacological analgesia. . . . . . 51
Analysis 2.4. Comparison 2 Acupressure versus control, Outcome 4 Caesarean section. . . . . . . . . . . . 52
Analysis 2.5. Comparison 2 Acupressure versus control, Outcome 5 Assisted vaginal birth. . . . . . . . . . 52
Analysis 2.6. Comparison 2 Acupressure versus control, Outcome 6 Apgar score < 7 at 5 minutes. . . . . . . . 53
Analysis 2.7. Comparison 2 Acupressure versus control, Outcome 7 Augmentation with oxytocin. . . . . . . . 53
Analysis 2.8. Comparison 2 Acupressure versus control, Outcome 8 Length of labour. . . . . . . . . . . . 54
Analysis 2.9. Comparison 2 Acupressure versus control, Outcome 9 Anxiety. . . . . . . . . . . . . . . 54
54 APPENDICES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
57 WHATS NEW . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
57 HISTORY . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
57 CONTRIBUTIONS OF AUTHORS . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
57 DECLARATIONS OF INTEREST . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
57 SOURCES OF SUPPORT . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
57 DIFFERENCES BETWEEN PROTOCOL AND REVIEW . . . . . . . . . . . . . . . . . . . . .
58 NOTES . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
58 INDEX TERMS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
i Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
[Intervention Review]
Acupuncture or acupressure for pain management in labour
Caroline A Smith
1
, Carmel T Collins
2
, Caroline A Crowther
3
, Kate M Levett
4
1
Centre for Complementary Medicine Research, University of WesternSydney, Penrith South DC, Australia.
2
Child NutritionResearch
Centre, Womens and Childrens Health Research Institute, Flinders Medical Centre and Womens and Childrens Hospital; Discipline
of Paediatrics, The University of Adelaide, Bedford Park, Australia.
3
ARCH: Australian Research Centre for Health of Women and
Babies, Discipline of Obstetrics and Gynaecology, The University of Adelaide, Adelaide, Australia.
4
University of Western Sydney,
Sydney, Australia
Contact address: Caroline A Smith, Centre for Complementary Medicine Research, University of Western Sydney, Locked Bag 1797,
Penrith South DC, New South Wales, 2751, Australia. caroline.smith@uws.edu.au.
Editorial group: Cochrane Pregnancy and Childbirth Group.
Publication status and date: Edited (no change to conclusions), published in Issue 8, 2011.
Review content assessed as up-to-date: 1 February 2011.
Citation: Smith CA, Collins CT, Crowther CA, Levett KM. Acupuncture or acupressure for pain management in labour. Cochrane
Database of Systematic Reviews 2011, Issue 7. Art. No.: CD009232. DOI: 10.1002/14651858.CD009232.
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
A B S T R A C T
Background
Many women would like to avoid pharmacological or invasive methods of pain management in labour and this may contribute towards
the popularity of complementary methods of pain management. This review examined evidence supporting the use of acupuncture
and acupressure for pain management in labour.
Objectives
To examine the effects of acupuncture and acupressure for pain management in labour.
Search methods
We searched the Cochrane Pregnancy and Childbirth Groups Trials Register and The Cochrane Complementary Medicine Fields
Trials Register (October 2010), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2010, Issue 4), MEDLINE
(1966 to October 2010), and CINAHL (1980 to October 2010).
Selection criteria
Published and unpublished randomised controlled trials comparing acupuncture and acupressure with placebo, no treatment or other
non-pharmacological forms of pain management in labour. We included all women whether primiparous or multiparous, and in
spontaneous or induced labour.
Data collection and analysis
We performed meta-analysis using risk ratios (RR) for dichotomous outcomes and mean differences (MD) for continuous outcomes.
The outcome measures included pain intensity, satisfaction with pain relief, use of pharmacological pain relief, relaxation, caesarean
section rate, augmentation with oxytocin, length of labour and anxiety.
1 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Main results
We included 13 trials with data reporting on 1986 women. Nine trials reported on acupuncture and four trials reported on acupressure.
Less intense pain was found from acupuncture compared with no intervention (standardised mean difference (SMD) -1.00, 95%
condence interval (CI) -1.33 to -0.67, one trial, 163 women). One trial increased satisfaction with pain relief compared with placebo
control (RR 2.38, 95% CI 1.78 to 3.19, 150 women). Reduced use of pharmacological analgesia was found in one trial of acupuncture
compared with placebo (RR 0.72, 95% CI 0.58 to 0.88, 136 women), and compared with standard care, however, there was signicant
heterogeneity (RR 0.68, 95% CI 0.56 to 0.83, three trials, 704 women). Fewer instrumental deliveries from acupuncture were found
compared with standard care (RR 0.67, 95% CI 0.46, 0.98, three trials, 704 women). Pain intensity was reduced in the acupressure
group compared with a placebo control (SMD -0.55, 95% CI -0.92 to -0.19, one trial, 120 women), and a combined control (SMD -
0.42, 95% CI -0.65 to -0.18, two trials, 322 women). No trial was assessed as being at a low risk of bias for all of the quality domains.
Authors conclusions
Acupuncture and acupressure may have a role with reducing pain, increasing satisfaction with pain management and reduced use of
pharmacological management. However, there is a need for further research.
P L A I N L A N G U A G E S U M M A R Y
Acupunture or acupressure for relieving pain in labour
Acupuncture or acupressure may help relieve pain during labour, but more research is needed.
The pain of labour can be intense, and may be worsened because of a womans tension, anxiety and fear affecting their labour and birth
experience . Many women would like to labour without using drugs or invasive methods of pain management, and turn to alternatives
to manage the pain. The review of 13 trials, with data reporting on 1986 women, found that acupuncture or acupressure may help
relieve labour pain. Single or limited numbers of trials reported less intense pain, increased satisfaction with pain relief and reduced
use of analgesic drugs with acupuncture compared with placebo or usual care. Acupressure also reduced pain intensity. Acupuncture
involves the insertion of ne needles into different parts of the body to correct the imbalance of energy in the body. The intervention
was administered at term as individualised treatment (six trials) or at standardised acupuncture points in the majority of trials but with
wide variation in the mode of stimulation, duration of needling, number of points used, depth of needling and duration of the trial.
B A C K G R O U N D
This review is one in a series of Cochrane reviews examining pain
management in labour. These reviews contribute to an overview
of systematic reviews of pain management for women in labour
(Neilson 2011b), and share a generic protocol (Neilson 2011a).
Description of the condition
Labour presents a physiological and psychological challenge for
women. As labour becomes more imminent, this can be a time of
conicting emotions: fear and apprehension can be coupled with
excitement and happiness. Tension, anxiety and fear are factors
contributing towards womens perception of pain and may also af-
fect their labour and birth experience. Pain associated with labour
has been described as one of the most intense forms of pain that
can be experienced (Melzack 1984). Pain experienced by women
in labour is caused by uterine contractions, the dilatation of the
cervix and, in the late rst stage and second stage, by stretching of
the vagina and pelvic oor to accommodate the baby. However,
the complete removal of pain does not necessarily mean a more
satisfying birth experience for women (Morgan 1982). Effective
and satisfactory pain management need to be individualised for
each woman.
Description of the intervention
The use of complementary and alternative medicine (CM) has
become popular with consumers worldwide. Studies suggest that
between36%and 62%of adults in industrialised nations use some
form of CM to prevent or treat health-related problems (Barnes
2 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
2004). Complementary therapies are more commonly used by
women of reproductive age, with almost half (49%) reporting use
(Eisenberg 1998). It is possible that a signicant proportion of
womenare using these therapies during pregnancy. Arecent review
of 14 studies with large sample sizes (N > 200) on the use of CM
in pregnancy identied a prevalence rate ranging from1%to 87%
(with nine falling between 20% and 60%) (Adams 2009). The
review identied use of various complementary therapies includ-
ing acupuncture and acupressure, aromatherapy, massage, yoga,
homeopathy and chiropractic care. The review also showed many
pregnant womenhad used more thanone complementary product
or service (Adams 2009). Many women would like to avoid phar-
macological or invasive methods of pain relief in labour and this
may contribute towards the popularity of complementary meth-
ods of pain management (Bennett 1999).
The Complementary Medicine Field of The Cochrane Collabora-
tiondenes complementary medicine as practices and ideas which
are outside the domain of conventional medicine in several coun-
tries, which are dened by its users as preventing or treating ill-
ness, or promoting healthand wellbeing (Manheimer 2008). This
denition is deliberately broad, as therapies considered comple-
mentary practices in one country or culture may be conventional
in another. Many therapies and practices are included within the
scope of the Complementary Medicine Field. These include treat-
ments people can administer themselves (e.g. botanicals, nutri-
tional supplements, health food, meditation, magnetic therapy),
treatments providers administer (e.g. acupuncture, massage, re-
exology, chiropractic and osteopathic manipulations), and treat-
ments people can administer under the periodic supervision of a
provider (e.g. yoga, biofeedback, Tai Chi, homoeopathy, Alexan-
der therapy, Ayurveda).
The most commonly cited complementary medicine and practices
associated with providing pain management in labour can be cat-
egorised into mind-body interventions (e.g. yoga, hypnosis, relax-
ation therapies), alternative medical practice (e.g. homoeopathy,
traditional Chinese medicine), manual healing methods (e.g. mas-
sage, reexology), pharmacologic and biological treatments, bio-
electromagnetic applications (e.g. magnets) and herbal medicines.
Acupuncture has a long history of use in Asia, including China,
Korea and Japan. Traditional Chinese medicine (TCM), with
acupuncture as one of the major modalities, describes a state of
health maintained by a balance of energy in the body. Acupunc-
ture performed within the context of TCM is a complex inter-
vention involving not only technical needling skill but develop-
ment of a therapeutic relationship, formulation of a diagnosis,
provision of lifestyle advice, and often administering co-interven-
tions such as gua sha (scrapping), tuina (massage), moxibustion
(a type of Chinese medicine which involves burning a herb close
to the skin) or electrical stimulation. In clinical practice, use of
co-interventions is not uncommon although acupuncture is the
primary focus. Acupuncture involves the insertion of ne needles
into different parts of the body to correct the imbalance of energy
in the body. TCM and Classical acupuncture explain disease and
physiological function based on theoretical concepts of Yin and
Yang and the Five Elements. A westernised medical application of
acupuncture involves the use of acupuncture using trigger points,
segmental points and commonly used formula points. Auricular
therapy, a formof Western acupuncture, involves the use of the ear
to make a diagnosis and subsequent needling to points on the ear.
Medical acupuncture may involve the application of acupuncture
based on the principles of neurophysiology and anatomy, rather
than TCM principles and philosophy. The style and approach of
acupuncture characterises the acupuncture point selection and re-
lated treatment parameters administered in clinical practice and
research.
Acupressure has its origins in early China, and is based on the
same paradigm as described for acupuncture. When acupressure
is applied, the therapist uses their hands and ngers to activate
the same points as applied by acupuncture. Sometimes only a few
points need touch applied to alleviate pain, or bring about a feeling
of relaxation. In other circumstances a combinations of points
will be used to achieve a greater effect. There are several forms of
acupressure, whichdrawonthe same knowledge and philosophical
systemas other forms of traditional Asian medicine. Some of these
systems are applied by trained health professionals and others can
be applied by the individual as a form of self-massage.
How the intervention might work
Acupuncture has been used to treat a number of painful condi-
tions, and several theories have been presented as to howacupunc-
ture may work. It has been proposed that acupuncture may
modify the perception of pain, or alter physiological functions
(Stux 1995). Since the majority of acupuncture points are ei-
ther connected to, or located near, neural structures, this suggests
that acupuncture stimulates the nervous system. From a Western
acupuncture perspective, points selected are based according to
the innervation of the target organ, e.g. the uterus. Activation of
muscle afferents at this segmental level transmits signals in the
spinal cord and in the central nervous system. During needle stim-
ulation of common acupuncture points for pain, signals are trans-
mitted to the spinal cord, and via afferent pathways to the mid-
brain. The perception of pain emerges fromthe resulting ow and
integration of this information among specic brain areas, and
may lead to a change in the perception of pain. Another theory
suggests that acupuncture stimulates the body to produce endor-
phins, which reduce pain (Pomeranz 1989). Other pain-relieving
substances called opioids may be released into the body during
acupuncture treatment (Ng 1992). Both segmental and central
mechanisms of acupuncture are likely to be involved in the total
effect of acupuncture (Stener-Victorin 2006).
3 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Why it is important to do this review
There is interest by women to use additional forms of care to assist
with their pain management in labour. It is important to examine
the efcacy, effectiveness and safety of under-evaluated forms of
treatment to enable women, health providers and policy makers
to make informed decisions about care. A number of clinical tri-
als have been performed to study the efcacy of acupuncture for
pain in labour although it remains uncertain whether the existing
evidence is rigorous enough to reach a denitive conclusion.
This review is one in a series of Cochrane reviews examining pain
relief in labour. These reviews contribute to an overviewof system-
atic reviews of pain relief for women in labour (Neilson 2011b)
and share a generic protocol (Neilson 2011a).
O B J E C T I V E S
To examine the effects of acupuncture and acupressure for pain
management in labour.
M E T H O D S
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) only. (We have planned not
to include results from quasi-RCTs in the analyses but we may be
discuss them in the text if little other evidence is available.)
Types of participants
Women in labour. (This includes women in high-risk groups, e.g.
preterm labour or following induction of labour. We planned to
use subgroup analysis for any possible differences in the effect of
interventions in these groups.)
Types of interventions
This review is one in a series of Cochrane reviews examining pain
management in labour. These reviews contribute to an overviewof
systematic reviews of interventions for pain management in labour
(Neilson 2011b), and share a generic protocol (Neilson 2011a).
To avoid duplication, the different methods of pain management
have been listed in a specic order, from one to 15. Individual
reviews focusing on particular interventions include comparisons
with only the interventions above it on the list. Methods of pain
management identied in the future will be added to the end of
the list. The current list is as follows.
1. Placebo/no treatment
2. Hypnosis
3. Biofeedback (Barragn 2006)
4. Intracutaneous or subcutaneous sterile water injection
(Derry 2011)
5. Immersion in water (Cluett 2009)
6. Aromatherapy (Smith 2011)
7. Relaxation techniques (yoga, music, audio)
8. Acupuncture or acupressure (this review)
9. Manual methods (massage, reexology)
10. Transcutaneous electrical nerve stimulation (TENS)
(Dowswell 2009)
11. Inhaled analgesia
12. Opioids (Ullman 2010)
13. Non-opioid drugs (Othman 2011)
14. Local anaesthetic nerve blocks
15. Epidural (including combined spinal-epidural)
(Anim-Somuah 2005; Simmons 2007)
Accordingly, this review includes comparisons of any type of
acupuncture or acupressure compared with any other type of
acupuncture or acupressure, as well as any type of acupuncture or
acupressure compared with: 1. placebo/no treatment; 2. hypnosis;
3. biofeedback; 4. intracutaneous or subcutaneous sterile water
injection; 5. immersion in water; 6. aromatherapy; 7. relaxation
techniques (yoga, music, audio).
Types of outcome measures
Primary outcomes
Effects of interventions
Pain intensity (as dened by trialists)
Satisfaction with pain relief (as dened by trialists)
Sense of control in labour (as dened by trialists)
Satisfaction with childbirth experience
Use of pharmacological pain relief
Safety of interventions
Effect (negative) on mother/baby interaction
Breastfeeding (at specied time points)
Assisted vaginal birth
Caesarean section
Side effects (for mother and baby; review specic)
Admission to special care baby unit/neonatal intensive care
unit (as dened by trialists)
Apgar score less than seven at ve minutes
Poor infant outcomes at long-term follow-up (as dened by
trialists)
4 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Other outcomes
Cost (as dened by trialists)
Secondary outcomes
Maternal
Length of labour; mode of delivery; need for augmentation with
oxytocin; perineal trauma (dened as episiotomy and incidence
of second- or third-degree tear); maternal blood loss (postpartum
haemorrhage dened as greater than 600 ml); relaxation; anxiety.
Neonatal
Need for mechanical ventilation; neonatal encephalopathy.
Search methods for identication of studies
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Groups Tri-
als Register by contacting the Trials Search Co-ordinator (October
2010).
The Cochrane Pregnancy and Childbirth Groups Trials Register
is maintained by the Trials Search Co-ordinator and contains trials
identied from:
1. quarterly searches of the Cochrane Central Register of
Controlled Trials (CENTRAL);
2. weekly searches of MEDLINE;
3. handsearches of 30 journals and the proceedings of major
conferences;
4. weekly current awareness alerts for a further 44 journals
plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL and MEDLINE,
the list of handsearched journals and conference proceedings, and
the list of journals reviewed via the current awareness service can
be found in the Specialized Register section within the edito-
rial information about the Cochrane Pregnancy and Childbirth
Group.
Trials identied through the searching activities described above
are each assigned to a review topic (or topics). The Trials Search
Co-ordinator searches the register for each review using the topic
list rather than keywords.
We searchedthe Cochrane Complementary Medicine Fields Trials
Register using the terms (labor OR labour).
In addition, we searched the Cochrane Central Register of Con-
trolled Trials (The Cochrane Library 2010, Issue 4), MEDLINE
(1966 to October 2010), and CINAHL (1980 to October 2010)
using a combination of subject headings and text words. See
Appendix 1.
We did not apply any language restrictions.
Data collection and analysis
We used the following methods when assessing any reports iden-
tied by the search.
Selection of studies
C Smith (CS), CT Collins (CTC) or K Levett (KL) screened the
titles and abstracts of articles found in the search, and discarded
trials that were clearly not eligible. Two out of the four review
authors (CS, CTC, KL, CA Crowther (CAC)) undertook trial
selection.
CS, KL or CTC independently assessed whether the trials met the
inclusion criteria, with disagreements resolved by discussion with
the fourth author (CAC). When articles contained insufcient
information to make a decision about eligibility, CS attempted to
contact authors of the original reports to obtain further details.
Data extraction and management
Following an assessment for inclusion CS, KL or CTC indepen-
dently extracteddata using the formdesignedby the ReviewGroup
for this purpose. We resolved discrepancies through discussion or,
if required, we consulted a fourth person. For each included trial,
we collected information regarding the location of the trial, meth-
ods of the trial (as per assessment of risk of bias), the participants
(age range, eligibility criteria), the nature of the interventions, and
data relating to the outcomes specied above. We collected in-
formation on reported benets and adverse effects. When infor-
mation regarding any of the above was unclear, we attempted to
contact authors of the original reports to provide further details.
We entered data into Review Manager software (RevMan 2011)
and checked for accuracy.
Assessment of risk of bias in included studies
Two review authors independently assessed the risk of bias for
each study using the criteria outlined in the Cochrane Handbook
for Systematic Reviews of Interventions (Higgins 2011). We resolved
any disagreement by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible
selection bias)
We described for each included study the method used to generate
the allocation sequence in sufcient detail to allow an assessment
of whether it should produce comparable groups.
We will assessed the method as:
low risk of bias (any truly random process, e.g. random
number table; computer random number generator);
5 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
high risk of bias (any non-random process, e.g. odd or even
date of birth; hospital or clinic record number); or
unclear risk of bias.
(2) Allocation concealment (checking for possible selection
bias)
We described for each included study the method used to con-
ceal allocation to interventions prior to assignment and assessed
whether intervention allocation could have been foreseen in ad-
vance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation;
consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non-
opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3) Blinding (checking for possible performance bias)
We judged that blinding of participants and caregiver would not
be possible due to the type of intervention being assessed. For
this reason we assessed whether the lack of blinding was likely to
have introduced bias in the measure of outcomes of interest. We
assessed blinding for primary outcomes as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition
bias due to the amount, nature and handling of incomplete
outcome data)
We described for each included study, and for each outcome or
class of outcomes, the completeness of data including attrition and
exclusions from the analysis. We stated whether attrition and ex-
clusions were reported and the numbers included in the analysis at
each stage (compared with the total randomised participants), rea-
sons for attrition or exclusion where reported, and whether miss-
ing data were balanced across groups or were related to outcomes.
Where sufcient information is reported, or can be supplied by
the trial authors, we will re-include missing data in the analyses
which we undertake.
We assessed methods as:
low risk of bias (e.g. no missing outcome data; missing
outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data
imbalanced across groups; as treated analysis done with
substantial departure of intervention received from that assigned
at randomisation);
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the
possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the studys pre-
specied outcomes and all expected outcomes of interest to the
review have been reported);
high risk of bias (where not all the studys pre-specied
outcomes have been reported; one or more reported primary
outcomes were not pre-specied; outcomes of interest are
reported incompletely and so cannot be used; study fails to
include results of a key outcome that would have been expected
to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not
covered by 1 to 5 above)
We described for each included study any important concerns we
had about other possible sources of bias.
We assessed whether each study was free of other problems that
could put it at risk of bias:
low risk of other bias;
high risk of other bias;
unclear whether there is risk of other bias.
(7) Overall risk of bias
We made explicit judgements about whether studies are at highrisk
of bias, according to the criteria given in the Handbook (Higgins
2011). With reference to (1) to (6) above, we assessed the likely
magnitude and direction of the bias and whether we considered it
likely to impact on the ndings. We planned to explore the impact
of the level of bias through undertaking sensitivity analyses - see
Sensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio
with 95% condence intervals.
Continuous data
We expressed continuous data as mean differences with 95% con-
dence intervals, or as standardised mean differences if outcomes
were conceptually the same in the different trials but measured in
different ways.
6 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Unit of analysis issues
We planned to include cluster-randomised trials in the analyses
along with individually randomised trials, and adjust their sample
sizes or standard errors using the methods described in the Hand-
book using an estimate of the intra-cluster correlation co-efcient
(ICC) derived from the trial (if possible), from a similar trial or
from a study of a similar population. If we used ICCs from other
sources, we planned to report this and conduct sensitivity analyses
to investigate the effect of variation in the ICC. If we identied
both cluster-randomised trials and individually-randomised trials,
we planned to synthesise the relevant information. We considered
it reasonable to combine the results from both if there was little
heterogeneity between the study designs and the interaction be-
tween the effect of intervention and the choice of randomisation
unit was considered to be unlikely.
We also planned to acknowledge heterogeneity in the randomisa-
tion unit and perform a sensitivity analysis to investigate the ef-
fects of the randomisation unit.
Dealing with missing data
For included studies, we noted levels of attrition. We aimed to
explore the impact of including studies with high levels of missing
data in the overall assessment of treatment effect by using sensi-
tivity analysis.
For all outcomes, we carried out analyses, as far as possible, on
an intention-to-treat basis, i.e. we attempted to include all partic-
ipants randomised to each group in the analyses, and all partici-
pants were analysed in the group to which they were allocated, re-
gardless of whether or not they received the allocated intervention.
The denominator for each outcome in each trial was the number
randomised minus any participants whose outcomes are known
to be missing. We excluded trials with greater than 20% missing
data from the analysis.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta-analysis using
the T, I and Chi statistics. We regarded heterogeneity as sub-
stantial if T was greater than zero and either I was greater than
50% or there was a low P value (less than 0.10) in the Chi test
for heterogeneity.
Assessment of reporting biases
If there were 10 or more studies in the meta-analysis we planned to
investigate reporting biases (such as publication bias) using funnel
plots. We would assess funnel plot asymmetry visually, and would
use formal tests for funnel plot asymmetry. For continuous out-
comes we would use the test proposed by Egger 1997, and for di-
chotomous outcomes we would use the test proposed by Harbord
2006. If we detected asymmetry in any of these tests or by a vi-
sual assessment, we proposed to perform exploratory analyses to
investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager soft-
ware (RevMan 2011). We used xed-effect meta-analysis for com-
bining data where it was reasonable to assume that studies were
estimating the same underlying treatment effect: i.e. where trials
were examining the same intervention, and the trials populations
and methods were judged sufciently similar. If there was clinical
heterogeneity sufcient to expect that the underlying treatment
effects differed between trials, or if substantial statistical hetero-
geneity was detected, we used a random-effects meta-analysis to
produce an overall summary if an average treatment effect across
trials was considered clinically meaningful. We treated the ran-
dom-effects summary as the average range of possible treatment
effects and we planned to discuss the clinical implications of treat-
ment effects differing betweentrials. If the average treatment effect
was not clinically meaningful we would not combine trials.
If we used the random-effects analyses, we have presented the
results as the average treatment effect with its 95% condence
interval, and the estimates of T and I.
Subgroup analysis and investigation of heterogeneity
We investigated substantial heterogeneity using subgroup analyses
and sensitivity analyses. We considered whether an overall sum-
mary was meaningful, and if it was, we undertook a random-ef-
fects analysis.
We planned to carry out the following subgroup analyses.
1. Spontaneous labour versus induced labour.
2. Primiparous versus multiparous
3. Term versus preterm birth
4. Continuous support in labour versus no continuous support
For xed-effect inverse variance meta-analyses we planned to assess
differences between subgroups by interaction tests. For random-
effects and xed-effect meta-analyses using methods other than
inverse variance, we planned to assess differences between sub-
groups by inspection of the subgroups condence intervals; non-
overlapping condence intervals indicate a statistically signicant
difference in treatment effect between the subgroups.
Sensitivity analysis
Where subgroup analysis failed to explain the heterogeneity, we
planned to analyse the data using the random-effects model. A
priori, we planned to performsensitivity analyses on results to look
at the possible contribution of: (1) differences in methodological
quality, with trials of high quality (lowrisk of bias) compared to all
trials; and (2) publication bias by country. If publication bias was
7 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
present we planned to undertake a sensitivity analysis excluding
trials from countries where there was a greater publication bias.
R E S U L T S
Description of studies
See: Characteristics of included studies; Characteristics of
excluded studies; Characteristics of studies awaiting classication;
Characteristics of ongoing studies.
Results of the search
The original review included a range of complementary therapies.
This updated review includes acupuncture and acupressure tri-
als only; we included 13 studies, and excluded nine studies. We
included eight new studies (Borup 2009; Hantoushzadeh 2007;
Hjelmstedt 2010; Huang 2008; Kashanian 2010; Martensson
2008; Qu 2007; Ziaei 2006) and ve studies await further assess-
ment. See Characteristics of included studies, Characteristics of
excluded studies, Characteristics of studies awaiting classication,
and Characteristics of ongoing studies.
Included studies
Study design
All studies were parallel design. Eight studies had two groups
(Hantoushzadeh 2007; Kashanian 2010; Lee 2004; Martensson
2008; Nesheim2003; Qu 2007; Ramnero 2002; Skilnand 2002).
Four studies had three groups (Borup 2009; Chung 2003;
Hjelmstedt 2010; Ziaei 2006) and one study had four arms
(Huang 2008). Comparative and control groups varied. Six studies
used placebo controls (Hantoushzadeh 2007; Hjelmstedt 2010;
Kashanian 2010; Lee 2004; Skilnand 2002; Ziaei 2006). Placebo
techniques varied between invasive and non-invasive techniques.
Comparison with medication was used in two studies (Borup
2009; Huang 2008). Other control groups included standard care;
passive supportive care by the midwife (Chung 2003); or unspeci-
ed care standard care in three studies (Hjelmstedt 2010; Nesheim
2003; Ramnero 2002). Huang 2008 used transcutaneous electri-
cal nerve stimulation and a breathing group; Martensson 2008
used sterile water injections, and no intervention was reported in
two studies (Qu 2007; Ziaei 2006).
Sample sizes
Studies included in the review ranged from 36 (Qu 2007) to 607
(Borup 2009).
Study location and sources of women
Three studies were undertaken in Iran (Hantoushzadeh 2007;
Kashanian 2010; Ziaei 2006), two studies each were undertaken
in China (Huang 2008; Qu 2007), Norway (Nesheim 2003;
Skilnand 2002) and Sweden (Martensson 2008; Ramnero 2002),
and one study each in Denmark (Borup 2009), India (Hjelmstedt
2010), Korea (Lee 2004) and Taiwan (Chung 2003).
Participants
Seven studies recruited both nulliparous and primiparous women
(Borup 2009; Chung 2003; Lee 2004; Martensson 2008; Nesheim
2003; Ramnero 2002; Skilnand 2002). Nulliparous women were
recruitedinthree studies (Hantoushzadeh 2007; Hjelmstedt 2010;
Kashanian 2010). Parous women only were recruited in two stud-
ies (Huang 2008; Qu 2007), and parity was unclear in one study
(Ziaei 2006). Women were recruited in spontaneous labour in
eight studies (Chung 2003; Hantoushzadeh 2007; Martensson
2008; Nesheim 2003; Qu 2007; Ramnero 2002; Skilnand 2002;
Ziaei 2006). Two studies recruited women in both spontaneous
and induced labour (Borup 2009; Hjelmstedt 2010). Reporting
on the onset of labour was unclear in three studies (Huang 2008;
Kashanian 2010; Lee 2004).
The intervention was administered at term for the majority of
trials studies except Huang 2008 where details were not reported.
Types of intervention
Four studies used acupressure (Chung 2003; Hjelmstedt 2010;
Kashanian 2010; Lee 2004) and nine studies used acupuncture
(Borup 2009; Hantoushzadeh 2007; Huang 2008; Martensson
2008; Nesheim 2003; Qu 2007; Ramnero 2002; Skilnand 2002;
Ziaei 2006) (includes manual andelectro-acupuncture). Acupunc-
ture and acupressure varied in point selection, frequency of treat-
ment and number of treatments, with commonly used points in-
cluded SP6, LI4, BL23, BL32, HT7, GB34, LR3, ST36. A xed
set of acupuncture points only were administered in three studies
(Qu 2007; Skilnand 2002; Ziaei 2006). A xed set of acupres-
sure points was used in four studies (Chung 2003; Hjelmstedt
2010; Kashanian 2010; Lee 2004). Individualised treatment was
administered in six studies (Borup 2009; Hantoushzadeh 2007;
Huang 2008; Martensson 2008; Nesheim2003; Ramnero 2002).
See Characteristics of included studies.
Outcome measures
All studies reported on pain. Maternal outcomes (satisfac-
tion, sense of control) were reported in nine studies (Borup
2009; Chung 2003; Hjelmstedt 2010; Huang 2008; Lee 2004;
Martensson 2008; Qu 2007; Ramnero 2002; Ziaei 2006), and
clinical outcomes were reported in the majority of studies ex-
cept for Huang 2008. See details of all outcomes reported within
Characteristics of included studies.
8 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Excluded studies
We excluded nine trials; see Characteristics of excluded studies.
One study did not meet the inclusion criteria based on the criteria
for interventions: for example, the use of point injection therapy
(Zhang 2000). We excluded four studies due to insufcient re-
porting of randomisation, or other aspects of study design, or no
clinically relevant data (Bo 2006; Deen 1985; Li 2006; Ternov
1998) and we were unable to ascertain true randomisation status
from the author. No clinically relevant outcomes were reported in
three trials (Li 1996; Shalev 1991; Shang 1995). One study was
reported as an abstract only with insufcient reporting to deter-
mine inclusion (Park 2003). Further background information on
these trials is presented in Characteristics of excluded studies.
Risk of bias in included studies
See Figure 1 and Figure 2 for a graphical summary of the risk of
bias assessments by authors of the included studies based on the
six risk of bias domains. No study was at a low risk of bias on all
domains.
Figure 1. Methodological quality graph: review authors judgements about each methodological quality
item presented as percentages across all included studies.
9 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Figure 2. Methodological quality summary: review authors judgements about each methodological quality
item for each included study.
10 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Allocation
Method of allocation
Most of the trials (92%) were rated at a low risk of bias for
adequate generation of the randomisation sequence. In 53% of
the trials the sequence was computer generated (Borup 2009;
Hantoushzadeh 2007; Hjelmstedt 2010; Huang 2008; Kashanian
2010; Martensson 2008; Nesheim 2003). The sequence was by
lot drawing in two trials (Qu 2007; Skilnand 2002), coin tossing
in one trial (Chung 2003), randomnumber tables in one trial (Lee
2004), and shufing cards in one trial (Ramnero 2002).
Allocation concealment
Allocation concealment was described as low risk in nine trials
(69%). Sealed envelopes were used in seven trials (Hantoushzadeh
2007; Hjelmstedt 2010; Kashanian 2010; Martensson 2008;
Nesheim2003; Ramnero 2002; Skilnand 2002), central randomi-
sation in one trial (Borup 2009) and sequential numbers in one
trial (Chung 2003).
Blinding
Blinding was assessed at low risk in three trials (Hantoushzadeh
2007; Lee 2004; Skilnand 2002). The risk of blinding was unclear
in ve trials due to poor reporting. The intervention could not be
administered blind.
Incomplete outcome data
Outcome reporting was assessed at a low risk of bias in 69% of
trials.
Selective reporting
The risk of bias from selective reporting was unclear in all trials
due to the absence of a study protocol.
Other potential sources of bias
The risk of bias from other sources of bias was rated as low in
eight trials (Borup 2009; Chung 2003; Kashanian2010; Lee 2004;
Martensson 2008; Nesheim 2003; Qu 2007; Ramnero 2002).
Effects of interventions
We included 12 trials in the meta-analysis with data reporting
on 1950 women using different modalities of pain management.
Data were not reported in a form that could be included in the
meta-analysis from the Qu 2007 study.
1) Acupuncture
Primary outcomes
1.1) Outcome: pain intensity
Data on pain intensity were reported from four trials with 493
women (Analysis 1.1).
1.1.1 Placebo control
There was signicant heterogeneity indicated by the I statistic and
we applied a random-effects model. There was no difference in the
intensity of pain between groups (standardised mean difference
(SMD) 0.04, 95% condence interval (CI) -0.22 to 0.30, two
trials 240 women).
1.1.2 Standard care
There was no difference in pain intensity between groups (SMD
-0.14, 95% CI -0.55 to 0.28, one trial, 90 women).
1.1.3 No treatment
Women receiving acupuncture reported less intense pain com-
pared with women receiving no intervention (SMD -1.00, 95%
CI -1.33 to -0.67, one trial, 163 women). The electro-acupuncture
group reported a lower intensity of pain compared with the con-
trol group (26 participants, one trial Qu 2007 study (P = 0.018)).
1.2) Outcome: satisfaction with pain relief in labour
Data on satisfaction with pain relief in labour were available from
four trials and 784 women (Analysis 1.2).
1.2.1 Placebo control
Acupuncture increased satisfaction with pain relief in labour com-
pared with placebo control (risk ratio (RR) 2.38, 95% CI 1.78 to
3.19, one trial, 150 women).
1.2.2 Standard care
There was no difference in satisfaction between groups (RR 1.08,
95% CI 0.95 to 1.22, one trial, 90 women). Comparative data
between two groups were not available, fromthe Borup 2009 trial,
59% of women receiving acupuncture thought acupuncture gave
some or substantial pain relief.
11 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
1.2.3 Water injection
Continuous data were reported and not included in the meta-
analysis from the Martensson 2008 trial. Women receiving water
injection were more satised with pain relief from water injection
compared with acupuncture (mean difference (MD) 18.60, 95%
CI 11.54 to 25.66, one trial, 128 women).
1.3) Outcome: use of pharmacological analgesia
Five trials, 968 women (Analysis 1.3).
1.3.1 Placebo control
One small trial of acupuncture compared with placebo found a
reduction in the use of pharmacological analgesia (RR 0.72, 95%
CI 0.58 to 0.88, one trial, 136 women).
1.3.2 Standard care
Use of pharmacological analgesia was lower in the acupuncture
group compared with standard care, however there was signicant
heterogeneity (RR 0.68, 95% CI 0.56 to 0.83, three trials, 704
women).
1.3.3 Water injection
There were no differences between groups (RR0.84, 95%CI 0.54
to 1.30, one trial, 128 women).
1.4) Outcome: caesarean section
Data on caesarean delivery were reported in seven trials and 1245
women (Analysis 1.4).
1.4.1 Placebo control
There was no difference between groups with caesarean delivery
(RR 1.39, 95% CI 0.62 to 3.10, three trials, 448 women).
1.4.2 Standard care
There was no difference between groups with caesarean delivery
(RR 0.86, 95% CI 0.47 to 1.60, two trials, 506 women).
1.4.3 No treatment
There was no difference between groups with caesarean delivery
(RR 0.76, 95% CI 0.35 to 1.83, one trial 163 women).
1.4.4 Water injection
There was no difference between groups with caesarean delivery
(RR 1.33, 95% CI 0.37 to 4.73, one trial, 128 women).
1.5) Outcome: assisted vaginal birth
Six trials reported on this outcome, 1203 women (Analysis 1.5).
1.5.1 Placebo control
There was no difference between groups (RR 0.64, 95% CI 0.27
to 1.50, one trial, 208 women).
1.5.2 Standard care
Three trials found a reduction with instrumental delivery favour-
ing acupuncture compared with standard care (RR 0.67, 95% CI
0.46 to 0.98, 704 women).
1.5.3 No treatment
There was no difference between groups (RR 0.49, 95% CI 0.18
to 1.38, one trial, 163 women).
1.5.4 Water injection
There was no difference between groups (RR 1.60, 95% CI 0.47
to 5.39, one trial, 128 women).
1.6) Outcome: Apgar score less than seven at ve minutes
Four trials, 914 women reported on this outcome (Analysis 1.6).
1.6.1 Placebo control
The number of babies with low Apgar scores at ve minutes was
small. There was no difference between groups (RR 0.32, 95% CI
0.01 to 7.79, one trial, 208 women).
1.6.2 Standard care
There were no differences between groups (RR0.60, 95%CI 0.12
to 2.99, three trials, 706 women).
1.7) Outcome: vaginal delivery
Three trials, 415 women reported on this outcome (Analysis 1.7).
1.7.1 Placebo control
There was signicant statistical heterogeneity betweentrials. There
were no differences between groups (RR 1.00, 95% CI 0.87 to
1.14, two trials, 325 women).
1.7.2 Standard care
There were no differences between groups (RR0.98, 95%CI 0.89
to 1.08 women, one trial, 90 women).
12 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
1.8) Outcome: augmentation with oxytocin
Five trials, 710 women reported on this outcome (Analysis 1.8).
1.8.1 Placebo control
There was signicant heterogeneity between trials; there were no
differences between groups (RR 0.62, 95% CI 0.15 to 2.52, two
trials, 358 women).
1.8.2 Standard care
There were no differences between groups (RR0.88, 95%CI 0.72
to 1.08, two trials, 224 women).
1.8.3 Water injection
There were no differences between groups (RR1.16, 95%CI 0.85
to 1.58, one trial, 128 women).
1.9) Outcome: relaxation
Three trials reported on this outcome, 308 women (Analysis 1.9).
1.9.1 Placebo control
There were no differences between groups (SMD -0.27, 95% CI
-0.72 to 0.17, one trial, 90 women).
1.9.2.Standard care
Acupuncture increased relaxation compared with standard care
(SMD -0.51, 95% CI -0.93 to -0.09, one trial, 90 women).
1.9.3 Water injection
Water injection increased womens reported of relaxation com-
pared with acupuncture (SMD 0.55, 95% CI 0.20 to 0.91, one
trial 128 women).
1.10) Outcome: length of labour
Length of labour was reported differently between trials, and not
combined in a meta-analysis.
1.10.1 Placebo control (two trials)
The active phase of labour was shorter in the acupuncture group
compared with control (3.41, 3.06 to 3.77 versus 4.45, 4.06
to 4.83, P < 0.001) (Hantoushzadeh 2007). Length of labour
from the initiation of acupuncture was signicantly in favour of
acupuncture (MD 71 fewer minutes, 95% CI -123.70 to -18.30)
(Skilnand 2002).
1.10.2 Standard care
Ramnero 2002 reported on the duration of labour from less than
4 cm to birth, there was no difference between groups (MD-0.30,
95% CI -1.79 to 1.19, one trial, 100 women).
1.10.3 Water injection
Martensson 2008 reported on the time fromtreatment to delivery
in minutes, there was no difference between groups (MD -90.1,
95% CI -187.02 to 6.82, one trial 300 women).
2) Acupressure
Primary outcomes
2.1) Outcome: pain intensity
Three trials, 462 women reported on this outcome (Analysis 2.1).
2.1.1 Placebo control
Pain intensity was reduced in the acupressure group compared
with the placebo control (SMD -0.55, 95% CI -0.92 to -0.19,
one trial, 120 women).
2.2.2 Combined control (placebo and no treatment)
Pain intensity was reduced in the acupressure group compared
with the combined control (SMD -0.42, 95% CI -0.65 to -0.18,
two trials, 322 women).
2.2) Outcome: satisfaction with childbirth
One trial, 211 women reported on this outcome (Analysis 2.2).
2.2.1 Combined control
There was no difference between groups (MD4.80, 95%CI -2.29
to 11.89, one trial, 211 women).
2.3) Outcome: use of pharmacological analgesia
Two trials, 287 women reported on this outcome (Analysis 2.3).
2.3.1 Placebo control
There was no difference between groups (RR 0.54, 95% CI 0.20
to 1.43, one trial, 75 women).
13 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
2.3.2 Combined control
There was no difference between groups (RR 0.94, 95% CI 0.71
to 1.25, one trial, 145 women).
2.4) Outcome: caesarean section
Two trials, 332 women reported on this outcome (Analysis 2.4).
2.4.1 Placebo control
Caesarean section was reduced in the acupressure group compared
with the placebo control group (RR 0.24, 95% CI 0.11 to 0.54,
one trial, 120 women).
2.4.2 Combined control
Caesarean section was reduced in the acupressure group compared
with the placebo control group (RR 0.48, 95% CI 0.22 to 1.04,
one trial, 222 women).
2.5) Outcome: assisted vaginal birth
One trial, 222 women (Analysis 2.5).
2.5.1 Combined control
There was no difference between groups (RR 0.81, 95% CI 0.39
to 1.67, one trial, 212 women).
2.6) Outcome: Apgar score less than seven at ve minutes
2.6.1 Placebo control
One trial reported on this outcome. No infants met this criteria
(Analysis 2.6).
2.7) Outcome: augmentation with oxytocin
Two trials, 332 women reported on this outcome (Analysis 2.7).
2.7.1 Placebo control
Augmentation was lower in the acupressure group compared with
placebo control (RR 0.66, 95% CI 0.46 to 0.94, one trial, 120
women).
2.7.2 Combined control
There was no difference between groups (RR 1.01, 95% CI 0.77
to 1.31, one trial, 222 women).
2.8) Outcome: length of labour
2.8.1 Placebo control
There was signicant heterogeneity betweentrials; lengthof labour
was lower in the acupressure group compared with placebo control
(SMD -1.06, 95% CI -1.74 to -0.38, two trials, 195 women)
(Analysis 2.8).
2.9) Outcome: anxiety
2.9.1 Placebo control
Acupressure reduced anxiety compared with placebo control (MD
-1.40, 95%CI -2.51 to -0.29, one trial, 75 women) (Analysis 2.9).
Sensitivity analysis
It was proposed to undertake a sensitivity analysis on the results
to look at the possible contribution of: (1) differences in method-
ological quality, with trials of high quality (low risk of bias) com-
pared to all trials; and (2) publication bias by country. This was
not done due to the small number of trials overall. There were no
trials of high quality; there were also too few trials within com-
parisons to make comparisons to examine the inuence of publi-
cation bias. Where there was heterogeneity, we applied a random-
effects model.
Subgroup analysis
We did not undertake subgroup analysis, based on insufcient
reporting of trials with the variables of interest by outcome.
D I S C U S S I O N
Summary of main results
Evidence from 13 trials and 1950 women included in the review
suggest a limited benet from acupuncture and acupressure in re-
lation to the primary outcomes of reduced pharmacological anal-
gesia, less intense pain and increased maternal satisfaction. There
was a reduced use of pharmacological analgesia found in one trial
of acupuncture compared with placebo (risk ratio (RR) 0.72, 95%
condence interval (CI) 0.58 to 0.88), and from three trials com-
pared with standard care; however, there was signicant hetero-
geneity (RR 0.68, 95% CI 0.56 to 0.83). There was a reduction
in pain intensity in one trial of acupuncture compared with no
intervention (standardised mean difference (SMD) -1.00, 95%CI
-1.33 to -0.67). One trial reported increased satisfaction with pain
14 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
relief in labour compared with placebo control (RR 2.38, 95% CI
1.78 to 3.19). There was a reduction with instrumental delivery
from acupuncture compared with standard care (RR 0.67, 95%
CI 0.46 to 0.98). Pain intensity was reduced in the acupressure
group compared with the placebo control (SMD -0.l55, 95% CI
-0.92 to -0.19) and a combined control group (SMD -0.42, 95%
CI -0.65 to -0.18). Currently there are a small number of trials
included within each comparison, and this limits the power of
the review to detect meaningful differences between groups and
analyses, suggesting these limited benets should be interpreted
with caution.
Overall completeness and applicability of
evidence
There remain relatively few trials of acupuncture and acupressure
that assess the role of these interventions in the management of
pain relief in labour. The completeness and applicability of the
evidence is limited from the 13 included trials, with no trial at a
lowrisk of bias on all domains. The inclusion of relevant outcomes
has improved with over 50% of the acupuncture trials reporting
on outcome of safety, and effectiveness. Aweakness of a number of
trials continues to be the inclusion of few outcomes and omission
of safety clinical outcomes.
Trials recruited low-risk nulliparous and primiparous women at
term, mostly in spontaneous labour. Studies were conducted in
different countries and consequently this reects the different
styles of acupuncture administered in the studies.There are many
styles of acupuncture, including individualised traditional Chi-
nese medicine, as illustrated by six trials administering individ-
ualised treatment (Borup 2009; Hantoushzadeh 2007; Huang
2008; Martensson 2008; Nesheim 2003; Ramnero 2002) and
those using standardised acupuncture points as used in the major-
ity of trials in this review. The systematic reviewdocumented wide
variation in the mode of stimulation, duration of needling, num-
ber of points used, depth of needling and duration of the trial. It
is unclear how representative the treatment protocols used in the
research are generalisable to acupuncture as it is usually practiced.
There was insufcient reporting of the rationale of the acupunc-
ture used in the research setting. The variation may also reect the
context in which acupuncture is practiced.
Quality of the evidence
The risk of bias table (Figure 1; Figure 2) demonstrates that
acupuncture has not been consistently subjected to consistent rig-
orous study. The quality of reporting was poor in over 50% of tri-
als. The risk of bias was lowin respect to randomisation (90% and
68%). No one trial was rated at a low risk of bias on all domains.
Rates of follow-up were high in the majority of trials with only a
small number of trials reporting a small loss of participants. For
many studies blinding of participants and the practitioner was not
possible, and reporting indicated that the outcomes could have
been inuenced by a lack of blinding and consequently were rated
at a high risk of bias. The small number of studies within compar-
isons and lack of high-quality trials suggest there remains insuf-
cient evidence of a consistent treatment effect from acupuncture.
The chief investigators of some studies were contacted to provide
additional methodological and statistical information; however,
we obtained only a few responses (Chung 2003; Huang 2008;
Kashanian 2010).
The quality of evidence was affected by unexplained heterogene-
ity in some comparisons arising from both the heterogeneity of
the clinical interventions and study designs. The small number
of studies within comparisons, and lack of high quality trials pre-
vented further investigation of the heterogeneity and the impact
on treatment effects.
Potential biases in the review process
We attempted to minimise publication bias. Our search was com-
prehensive and we included studies identied in languages other
than English. However, we cannot rule out the possibility that
some studies have been missed. The variation in the duration,
frequency and selection of acupuncture points suggests that the
acupuncture may not have been therapeutically effective and in
some cases may not represent best clinical practice.
Agreements and disagreements with other
studies or reviews
There is one other systematic reviews of acupuncture to treat de-
pression (Cho 2010). This review included trials for which we
were unable to ascertain the randomisation details or we excluded
because the trials did not meet the eligibility criteria. Our ndings
and conclusions concerning the role of acupuncture for pain relief
in labour are similar to this review.
A U T H O R S C O N C L U S I O N S
Implications for practice
The data available suggest acupuncture and acupressure may be a
helpful therapy for pain management in labour. However, there
is insufcient evidence to make clinical recommendations. There
are insufcient data to demonstrate whether acupuncture and acu-
pressure are more effective thana placebo control, or whether there
is additional benet fromacupuncture when used in combination
with usual care. The risk of bias was high in the majority of trials
and recommendations for practice cannot be made until further
high quality research has been undertaken.
15 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Implications for research
Further randomised controlled trials of acupuncture and acupres-
sure for pain management in labour are needed. Further ran-
domised trials should be adequately powered and include clinically
relevant outcomes such as those described in this review. There is
a need for improving the quality and reporting of future trials. In
particular, considerationshouldbe giveninthe analysis andreport-
ing on the person providing the intervention: for example, their
training, length of experience and relationship to the woman. In
addition, further research is required which include data measur-
ing neonatal outcomes and the effects on analgesia requirements
in institutions with and without an on demand epidural service.
A cost-benet analysis should be incorporated into the design of
future studies.
Future studies may need to consider the use of both effectiveness
designs using medication, or other forms of standard care, and
efcacy designs using placebo controls.
A C K N O W L E D G E M E N T S
The review authors would like to acknowledge the Pregnancy and
Childbirth teamfor assistance with the preparation of the original
reviewand its update, including the Trials Search Co-ordinator for
assistance in developing the search strategy, the editors, co-editors
and other staff within the team. We also acknowledge the Chinese
to English translation assistance provided by Song Mei Wu, and
thank Huijuan Cao for her assistance with seeking clarication
from authors in China.
As part of the pre-publication editorial process, this review has
been commented on by three peers (an editor and two referees
who are external to the editorial team), and the Groups Statistical
Adviser.
R E F E R E N C E S
References to studies included in this review
Borup 2009 {published data only}
Borup L, Wurlitzer W, Hedegaard M, Kesmodel US,
Hvidman L. Acupuncture as pain relief during delivery: a
randomized controlled trial. Birth 2009;36(1):512.
Chung 2003 {published data only}
Chung UL, Hung LC, Kuo SC, Huang CL. Effects of
LI4 and BL67 acupressure on labor pain and uterine
contractions in the rst stage of labour. Journal of Nursing
Research 2003;11(4):25160.
Hantoushzadeh 2007 {published data only}
Hantoushzadeh S, Alhusseini N, Lebaschi AH. The effects
of acupuncture during labour on nulliparous women: a
randomised controlled trial. Australian and New Zealand
Journal of Obstetrics and Gynaecology 2007;47(1):2630.
Hjelmstedt 2010 {published data only}
Hjelmstedt A, Shenoy S, Stener-Victorin E, Lekander
M, Bhat M, Balakumaran L, et al.Acupressure to reduce
labour pain - a randomized controlled trial. Acta Obstetricia
et Gynecologica Scandinavica 2010;89(11):14539.
Hjelmstedt A, Shenoy S, Stener-Victorin E, Lekander M,
Bhat M, Leena K Kb, et al.Acupressure to reduce labour
pain - a randomized controlled trial. International Journal of
Gynecology & Obstetrics 2009;107(Suppl 2):S201.
Huang 2008 {published data only}
Huang T, Yang Y, Huang X. Selection of acupoints and
opportunity for acupuncture analgesia in delivery. Journal
of Traditional Chinese Medicine 2008;49:6258.
Kashanian 2010 {published data only}
Kashanian M, Shahali S. Effects of acupressure at the
Sanyinjiao point (SP6) on the process of active phase of
labor in nulliparous women. Journal of Maternal-Fetal and
Neonatal Medicine 2010;23(7):63841.
Lee 2004 {published data only}
Lee MK. Effects of San-Yin-Jiao (SP6) acupressure on labor
pain, delivery time in women during labor. Journal of
Korean Academy of Nursing 2003;33(6):75361.
Lee MK, Chang SB, Kang D-H. Effects of SP6 acupressure
on labor pain and length of delivery time in women during
labor. Journal of Alternative and Complementary Medicine
2004;10(6):95965.
Martensson 2008 {published data only}
Martensson L, Stener-Victorin E, Wallin G. Acupuncture
versus subcutaneous injections of sterile water as treatment
for labour pain. Acta Obstetricia et Gynecologica Scandinavica
2008;87(2):1717.
Nesheim 2003 {published data only}
Nesheim BI, Kinge R, Berg B, Alfredsson B, Allgot E, Hove
G, et al.Acupuncture during labor can reduce the use of
meperidine: a controlled clinical study. Clinical Journal of
Pain 2003;19(3):18791.
Qu 2007 {published data only}
Qu F, Zhou J. Electro-acupuncture in relieving labor pain.
Evidence-based Complementary and Alternative Medicine
2007;4(1):12530.
Ramnero 2002 {published data only}
Ramnero A, Hanson U, Kihlgren M. Acupuncture
treatment during labour - a randomised controlled trial.
BJOG: an international journal of obstetrics and gynaecology
2002;109:63744.
16 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Skilnand 2002 {published data only}
Skilnand E, Fossen D, Heiberg E. Acupuncture in
the management of pain in labor. Acta Obstetricia et
Gynecologica Scandinavica 2002;81:9438.
Ziaei 2006 {published data only}
Ziaei S, Hajipour L. Effect of acupuncture on labor.
International Journal of Gynecology & Obstetrics 2006;92(1):
712.
References to studies excluded from this review
Bo 2006 {published data only}
Bo QX, Zhang JX. Observation on therapeutic effect of
scalp acupuncture analgesia on labor. Zhongguo Zhenjiu
2006;26(9):65961.
Deen 1985 {published data only}
Deen P, Yuelam H. Use of acupuncture analgesia during
childbirth. Journal of Traditional Chinese Medicine 1985;5
(4):2535.
Li 2006 {published data only}
Li P, Liu X. Clinical and mechanism study on acupuncture
for relieving the labour pain. Journal of Tianjin University of
Traditional Chinese Medicine 2006;25(2):7476.
Li 1996 {published data only}
Li XH, Ma WZ. Effect of electro-acupuncture Shenmen
(Otopoint) and Hegu (LI4) on uterine contraction
of parturients. Shanghai Journal of Acupuncture and
Moxibustion 1996;15(4):145.
Park 2003 {published data only}
Park Y, Cho J, Kwon J, Ahn E, Lim J, Chang S. The effect
of san-yin-jiao (SP-6) acupressure on labor progression
(abstract). American Journal of Obstetrics and Gynecology
2003;189(6):S209.
Shalev 1991 {published data only}
Shalev E, Yanay N, Peleg D, Yagudin E. Electroacupuncture
during labour and its effect on peripheral plasma beta-
endorphin concentration. American Journal of Acupuncture
1991;19(4):3458.
Shang 1995 {published data only}
Shang LF, Liu JY, Li AX. Puncture the Hegu acupoint
to accelerate the second stage of labor and to reduce the
postpartum hemorrhage. Chinese Journal of Nursing 1995;
30(9):5378.
Ternov 1998 {published data only}
Ternov K, Nilsson M, Lofberg L, Algotsson L, Akeson J.
Acupuncture for pain relief during childbirth. Acupuncture
and Electro-therapeutics 1998;23:1926.
Zhang 2000 {published data only}
Zhang LJ. Point-injection therapy for labor pains. Shanghai
Journal of Acupuncture and Moxibustion 2000;19(2):10.
References to studies awaiting assessment
Fei 1985 {published data only}
Fei DE, Huang YL. Application of acupuncture analgesia in
labor. Chinese Acupuncture & Moxibustion 1985;5(2):167.
Su 2001 {published data only}
Su XJ. Clinical effect with Hans acupoint nerve stimulator
(Hans) for reliving labour pain. Chinese Journal of Pain
Medicine 2001;2:89.
Wang 1994 {published data only}
Wang RY. Application of acupuncture-combined with
hypnotism in painless labor. Acupuncture Research 1994;19
(1):180.
Xu 2000 {published data only}
Xu CP. Combination of Hans and diazepam for labor
analgesia: a basic and clinical study. Chinese Journal of Pain
Medicine 2000;6(1):12.
Zhang 2002 {published data only}
Zhang SY. Hans combined with diazepam for labor pain
control. Chinese Journal of Pain Medicine 2002;8(2):101.
References to ongoing studies
MacKenzie 2005 {published data only}
MacKenzie IZ. Acupuncture for pain relief during
induced labour for nulliparae. Clinical Trials.gov (http:
//clinicaltrials.gov/ct2/show/record/NCT01165099)
(accessed 6.01.2011).
Martensson 2008 {published data only}
Martensson L. Acupuncture to reduce labour pain. Clinical
Trials.gov (http://clinicaltrials.gov/ct2/show/record/
NCT01197950) (accessed 6.01.2011).
Mohamadinia 2008 {published data only}
Mohamadinia N. Comparing Hoku point (LI4) acupressure
and San-Yin-Jiao (SP6) acupressure on labor pain and
length of delivery time in nulliparous women in Iran
hospital 2008-2009. Iranian Registry of Clinical Trials
(IRCT) (http://www.irct.ir/) (accessed 6.01.2011).
Additional references
Adams 2009
Adams J, Lui C-W, Sibbritt D, Broom A, Wardle J, Homer
C, et al.Womens use of complementary and alternative
medicine during pregnancy: a critical review of the
literature. Birth 2009;36(3):23745.
Anim-Somuah 2005
Anim-Somuah M, Smyth Rebecca MD, Howell Charlotte
J. Epidural versus non-epidural or no analgesia in
labour. Cochrane Database of Systematic Reviews 2005,
Issue 4. [DOI: 10.1002/14651858.CD000331.pub2; :
CD000331]
Barnes 2004
Barnes P, Powell-Griner E, McFann K, Nahin R.
Complementary and alternative medicine use among adults:
United States. CDC Advance Data Report 2002:343.
Barragn 2006
Barragn Loayza IM, Gonzales F. Biofeedback for pain
during labour. Cochrane Database of Systematic Reviews
2006, Issue 4. [DOI: 10.1002/14651858.CD006168]
17 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Bennett 1999
Bennett VR, Brown LK. Myles Textbook for Midwives. 13th
Edition. London: Churchill Livingstone, 1999.
Cho 2010
Cho S-H, Lee H, Ernst E. Acupuncture for pain relief in
labour: a systematic review and meta-analysis. BJOG: an
international journal of obstetrics and gynaecology 2010;117:
90720.
Cluett 2009
Cluett ER, Burns E. Immersion in water in labour and
birth. Cochrane Database of Systematic Reviews 2009, Issue
2. [DOI: 10.1002/14651858.CD000111.pub3]
Derry 2011
Derry S, Straube S, Moore RA, Hancock H, Collins SL.
Intracutaneous or subcutaneous sterile water injection
for relieving pain in labour. Cochrane Database of
Systematic Reviews 2011, Issue 5. [DOI: 10.1002/
14651858.CD009107]
Dowswell 2009
Dowswell T, Bedwell C, Lavender T, Neilson James P.
Transcutaneous electrical nerve stimulation (TENS)
for pain relief in labour. Cochrane Database of
Systematic Reviews 2009, Issue 2. [DOI: 10.1002/
14651858.CD007214.pub2]
Egger 1997
Egger M, Davey Smith G, Schneider M, Minder C. Bias
in meta-analysis detected by a simple, graphical test. BMJ
1997;315(7109):62934.
Eisenberg 1998
Eisenberg DA, Davis RB, Ettner SL, Appel S, Wilky S,
Van Rompay M. Trends in alternative medicine use in the
United States, 1990-1997: results of a follow up national
survey. JAMA 1998;280:156975.
Harbord 2006
Harbord RM, Egger M, Sterne JA. A modied test for
small-study effects in meta-analyses of controlled trials
with binary endpoints. Statistics in Medicine 2006;25(20):
344357.
Higgins 2011
Higgins JPT, Green S, editors. Cochrane Handbook for
Systematic Reviews of Interventions Version 5.1.0 [updated
March 2011]. The Cochrane Collaboration, 2011.
Available from www.cochrane-handbook.org.
Manheimer 2008
Manheimer E, Berman B. Cochrane Complementary
Medicine Field. About The Cochrane Collaboration
(Fields) 2008, Issue 2.
Melzack 1984
Melzack R. The myth of painless childbirth. Pain 1984;19:
3317.
Morgan 1982
Morgan BM, Bulpitt CJ, Clifton P, Lewis PJ. Analgesia
and satisfaction in childbirth (the Queen Charlottes 1000
mother survey). Lancet 1982;2(8302):80810.
Neilson 2011a
Jones L, Dou L, Dowswell T, Alrevic Z, Neilson JP.
Pain management for women in labour: generic protocol.
Cochrane Database of Systematic Reviews in press.
Neilson 2011b
Jones L, Othman M, Dowswell T, Alrevic Z, Gates
S, Newburn M, Jordan S, Lavender T, Neilson JP. Pain
management for women in labour: an overview of
systematic reviews. Cochrane Database of Systematic
Reviews in press.
Ng 1992
Ng LKY, Katims JJ, Lee MHM. Acupuncture, a
neuromodulation technique for pain control. In: Aronoff
GM editor(s). Evaluation and Treatment of Chronic Pain.
2nd Edition. Baltimore: Williams & Wilkins, 1992.
Othman 2011
Othman M, Jones L, Neilson JP. Non-opioid drugs for pain
management in labour. Cochrane Database of Systematic
Reviews in press.
Pomeranz 1989
Pomeranz B, Stux G. Scientic Bases of Acupuncture. Berlin:
Springer-Verlag, 1989.
RevMan 2011
The Nordic Cochrane Centre, The Cochrane Collaboration.
Review Manager (RevMan). 5.1. Copenhagen: The Nordic
Cochrane Centre, The Cochrane Collaboration, 2011.
Simmons 2007
Simmons Scott W, Cyna Allan M, Dennis Alicia T, Hughes
D. Combined spinal-epidural versus epidural analgesia in
labour. Cochrane Database of Systematic Reviews 2007,
Issue 3. [DOI: 10.1002/14651858.CD003401.pub2; :
CD003401]
Smith 2011
Smith CA, Collins CT, Crowther CA. Aromatherapy
for pain management in labour. Cochrane Database of
Systematic Reviews in press.
Stener-Victorin 2006
Stener-Victorin E, Fujisawa S, Kurosawa M. Ovarian blood
ow responses to electroacupuncture stimulation depend on
estrous cycle and frequency of stimulation in anesthetized
rates. Journal of Applied Physiology 2006;101:8491.
Stux 1995
Stux G, Pomeranz B. Basics of Acupuncture. Berlin:
Springer-Verlag, 1995.
Ullman 2010
Ullman R, Smith Lesley A, Burns E, Mori R, Dowswell
T. Parenteral opioids for maternal pain relief in labour.
Cochrane Database of Systematic Reviews 2010, Issue
9. [DOI: 10.1002/14651858.CD007396.pub2; :
CD007396]
References to other published versions of this review
Smith 2006
Smith CA, Collins CT, Cyna AM, Crowther CA.
Complementary and alternative therapies for pain
18 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
management in labour. Cochrane Database of
Systematic Reviews 2006, Issue 4. [DOI: 10.1002/
14651858.CD003521.pub2]
Indicates the major publication for the study
19 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
C H A R A C T E R I S T I C S O F S T U D I E S
Characteristics of included studies [ordered by study ID]
Borup 2009
Methods Randomised trial of acupuncture, TENS or traditional analgesics
Participants 607 healthy, Danish-speaking women in labour with a normal singleton pregnancy
who were giving birth at term (37-42 completed weeks) and with a fetus in cephalic
presentationwere eligible for the study. Womenwere recruited froma university hospital.
Women were excluded if they had medical complications, or already received analgesics
in labour
Interventions Acupuncture group: acupuncture was administered by midwives who had completed
a 5-day course in Western techniques of obstetric acupuncture, and received at least 6
months clinical training using acupuncture during labour
Treatment was individualised, according to location of pain and womans mobility, nee-
dles used of 3 depths 0.20 x 15, 0.30 x 30, 0.35 x 50 mm. Duration of needling 30-120
minutes and could be repeated. Needles removed if woman uncomfortable or if obstetric
pathology. Supplementary analgesics provided on request as per control group
Acupuncture points included BL 23, 24, 25, 26, 31-34, 36, 60, CV20 and sishongong,
ear points uterus, shenmen, endocrine, EX-HN3 yintang, LR3, SP6, SP9, ST36, GB34,
HT7, PC6, LI10,11, LU7, LI 4
Control group: traditional analgesics: women randomised to the traditional group could
choose among all analgesic methods available (sterile water papules, nitrous oxide, warm
tub bath, pethidine, and epidural analgesia)
Outcomes Need for pharmacological pain relief, pain intensity, overall experience and satisfac-
tion,duration of labour, use of oxytocin, mode of delivery, postpartum haemorrhage,
Apgar score, umbilical cord pH
Notes Study duration: 1/3/2002- 29/2/2004.
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk Computer-generated sequence, with ran-
domisation in a ratio of 2:1
Allocation concealment (selection bias) Low risk Central randomisation voice response.
Blinding (performance bias and detection
bias)
All outcomes
High risk Women, midwife acupuncturists were not
blind to their group allocation. It was un-
clear if the outcome assessor or analyst was
blind to group allocation
20 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Borup 2009 (Continued)
Incomplete outcome data (attrition bias)
All outcomes
Low risk Data were missing from 8%, with the rea-
sons similar between groups: no project
midwife available, did not want the al-
located treatment, rapid progression of
labour, other reasons
Selective reporting (reporting bias) Unclear risk The study protocol is not available but the
study reports the expected outcomes
Other bias Low risk The study appears free of other biases.
Chung 2003
Methods Single-blind, randomised controlled trial of acupressure, efeurage and a control group.
It was not feasible for the participant and therapist to be blind to their group allocation
Participants 127 women participated in the trial, during their rst stage of labour. Participants needed
to be between 37 and 42 weeks pregnant, a low-risk pregnancy, singleton pregnancy and
able to speak Chinese. Women who were induced with oxytocin, or received an epidural
block or who planned a caesarean section were excluded from the study. The trial was
undertaken in Taiwan; no other details were reported
Interventions Trained midwives administered the acupressure to women. The intervention lasted 20
minutes, consisting of 5 minutes pressure to points LI4 and BL67. 5 cycles of acupressure
were completed in5 minutes, with each cycle comprising 10 seconds of sustained pressure
and 2 seconds of rest without pressure. A protocol was established to control nger
pressure, accuracy of points and accuracy of technique. For the efeurage group, the left
and right upper arms were massaged for 10 minutes. In the control group, the midwife
stayed with the participant for 20 minutes, taking notes or talking with the participant
or family members
Outcomes A VAS scale was used to measure the intensity of labour pain. This was administered
before and after the intervention. Qualitative data were also collected on womens ex-
perience of labour pain 1-2 hours after delivery. The frequency and intensity of uterine
contractions were measured from electronic fetal monitors
Notes There was no power analysis. An intention-to-treat analysis was not performed
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk Coin tossing.
Allocation concealment (selection bias) Low risk Sequentially numbered.
21 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Chung 2003 (Continued)
Blinding (performance bias and detection
bias)
All outcomes
Unclear risk Partial. The outcome assessors were blind
to womens group allocationbut unclear for
analyst
Incomplete outcome data (attrition bias)
All outcomes
Low risk 23 (18%) women withdrew fromthe study
due to a need for a caesarean section, pain
medication. The reason for attrition was
similar across groups and due to the need
for induction or pain relief
Selective reporting (reporting bias) Unclear risk Unclear.
Other bias Low risk No other sources of bias detected.
Hantoushzadeh 2007
Methods Single blind randomised controlled trial of acupuncture versus placebo acupuncture
using sham needling
Duation: February to September 2005.
Setting: government general hospital, Tehran, Iran.
Participants 150 women with a singleton pregnancy, at term (37 weeks), nulliparous, parturient and
in spontaneous active labour. Exclusion criteria: presence of medical or surgical disease,
indication for caesarean section, pace-maker, emphysema, history of anticoagulation,
HIV, HCV or HBV infection, pregnancy-related complications, e.g. chorioamnionitis,
placental abruption, placenta praevia and pre-eclampsia/eclampsia, cervical dilation > 6
cm
Interventions The study group received acupuncture administered by the study investigator, who was
trained to practice acupuncture. Points were selected bilaterally according to parturient
symptoms, and needles were inserted at 45 degree or perpendicularly with a depth that
depended on the thickness of the subcutaneous fat. The selection of points was done
according to acupuncture principles and was subject to variation frompatient to patient.
Needles were manually stimulated until the de chi sensation (sensation of warmth,
numbness, tingling, or heaviness) was achieved. The needles were not taped and were
removed either when delivery occurred or the patient herself asked to do so or when the
effect terminated or there was no effect
The following points and there indication were reported as follows: LI4- analgesia, BL32-
back pain, BL60 back pain, SP6 severe pain during contractions, ST36 general pain,
LR3 analgesia, GB34 cervical rigidity, HT7 anxiety, nervousness
The control group received minimal acupuncture which involved insertion of acupunc-
ture needles away from true acupuncture points. Participants were not asked about de
qi and the needles were manually stimulated for about 20 minutes
Both groups received care from health providers, routine analgesia was not available
Outcomes Pain scores measured using VAS scale, at beginning, 30 minutes, 60 minutes, 120 min-
utes, then every hour until end of labour
Duration of active labour, amount of oxytocin used, vaginal birth, birthweight, Apgar
22 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Hantoushzadeh 2007 (Continued)
score at 1 minute, acceptability of acupuncture
Notes
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk Computer generated.
Allocation concealment (selection bias) Low risk Sealed opaque envelopes.
Blinding (performance bias and detection
bias)
All outcomes
Low risk Partcipants blind to group allocation (as-
sessment of blinding not reported), admin-
istering clinician unblinded, care provider
unclear, outcome assessor blinded
Incomplete outcome data (attrition bias)
All outcomes
Low risk 5 losses in the acupuncture group: 3 cae-
sarean section, 2 labour stopped. 1 loss in
the control group caesarean section. No in-
tention to treat
Selective reporting (reporting bias) Unclear risk Protocol not available.
Other bias High risk Partcipants in the control group had signif-
icantly lower pain scores before interven-
tion commenced
Hjelmstedt 2010
Methods Parallel randomised controlled trial of acupressure compared with light touch or standard
care
Participants Public hospital in Trivandrum, India. 212 women randomised to the trial
Inclusion criteria: nulliparous, transferred to labour room, dilation 3-7 cm, healthy,
uncomplicated pregnancy, term, live fetus, cephalic presentation
Exclusion criteria: hypertensive disorder, pre-eclampsia, diabetes, neuropathic pain, mul-
tiparous, intrauterine death, multiple fetuses, breech presentation, gestation < 38 or >
42 weeks, dilation < 3 or > 7 cm, elective caesarean section, presence of pharmacological
pain relief
Interventions Group 1: acupressure at acu-point Sp6 bilaterally during contractions over a 30-minute
period. Treatment was not repeated after 2 hours if the woman was not in second stage
or had not delivered. Intensity of pressure adapted to each womans pain threshold
Group 2: (TG) receive light touch at SP6 bilaterally during contractions
Group 3: (SCG) standard care.
Acupressure and touch was delivered by same person who had undergone 3 days of
23 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Hjelmstedt 2010 (Continued)
training by a certied acupressure therapist
Outcomes Participants self-assessment of in-labour pain via VAS pain scores, oxytocin augmenta-
tion, pharmacological pain relief, caesarean section, mode of delivery, episiotomy, birth-
weight, birth length, Apgars (5 minutes). Retrospective ratings of labour pain, coping
with labour pain and experience of childbirth
Notes Trial duration: 1/9/2007-30/4/2008.
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk Computer generated.
Allocation concealment (selection bias) Low risk Sealed opaque envelope.
Blinding (performance bias and detection
bias)
All outcomes
Unclear risk It was unclear if the participant was blind to
light touch or acupressure, the clinicianwas
not blind to group allocation, the outcome
assessor was blind to group allocation
Incomplete outcome data (attrition bias)
All outcomes
Low risk 1 women withdrew from the standard care
group.
Selective reporting (reporting bias) Unclear risk Study protocol unavailable.
Other bias High risk Baseline pain scores were signicantly dif-
ferent between APG and SC, and board-
ing on signicance between APG and TG.
Therefore scores were not used for a be-
tween group comparison, but were used for
a within-group comparison over time
Huang 2008
Methods Single blind RCT, 4-arm study: 1) electro-acupuncture group N = 82; TENS group N
= 82; control group (breathing) N = 81; spinal-epidural analgesia group N = 79
Unit of randomisation: 1:1:1:1.
Participants Delivery unit at the Beijing Gynaecolgoy and Obstetrics Hospital, China
Inclusioncriteria: 324 primiparae women aged 22-34 years, vaginal delivery, monocyesis,
not cephalopelvic disproportion, no abnormal fetal position, no serious complications
of pregnancy, agreement to labour analgesia
Exclusion criteria: not explicitly stated.
24 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Huang 2008 (Continued)
Interventions 1) Electro-acupuncture. Shi diagnosis labour pain mainly located in the lumbosacral and
with bearing-down sensation, sturdy body, desiring cold and fearing of warmth, good
appetite, normal or dry stool, normal or less yellowurine, good sleep, normal red tongue
with thin and whitish or slightly thicker tongue coating, wiry, drooling and strong pulse
Xu diagnosis: labour pain mainly located in the lower abdomen and distending, weak
body, seeking warmth and fearing of cold, poor appetite, loose stool, clear abundant
urine, increased nocturnal enuresis, worse sleep, easily waken up in the night, fatty and
whitish tongue with teeth mark, thicken and greasy coating, deep and thin, weak pulse.
Electro-acupuncture group applied self-developed acusector on selected acu-points ac-
cording to syndrome differentiation, and needling and galvanism were combined on
the acu-points. Main acu-points were ST36, CV3 and CV4. Additional points for Shi
were BL32 and LR3) and for Xu were LI4 and SP6. Radio frequency electrodes (self-
developed, putting auricular needle in the centre of electrode plate with thumb-tack
needle) were inserted and connected to Hans acu-point nerve stimulator. Dilatational
wave of 2Hz/100 Hz operated as a stimulator and the strength adjusted to the womans
tolerance level
2) TENS group used Hans acu-point nerve stimulator and stimulated point with 2/100
Hz of dilatational wave.
3) Spinal-epidural analgesia group received combined spinal and epidural block anaes-
thesia
4) Advice on breathing during contraction and local massage during severe pain
Outcomes VAS scores of pain applied at pre-pain, 30 minutes, 60 minutes, 120 minutes after pain
analgesia, at the end of active stage (cervical dilation of 7-8 cm), complete dilation of
cervix, second stage of labour, third stage of labour and 1 day after labour. 0-no pain,
1-mild pain, 10-most severe and intolerable pain
Degree of satisfaction to labour analgesia 2 hours after delivery
Satised: pain completely relieved without evident discomfort
Relatively satised: pain relieved to some extent without evident discomfort
Unsatised: pain not relieved with evident discomfort.
Mode of delivery, maternal and labour complications.
Notes Trial duration: April 2004-February 2005.
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk Computer generated.
Allocation concealment (selection bias) Unclear risk No details reported.
Blinding (performance bias and detection
bias)
All outcomes
Unclear risk Women provided self reported pain and
were not blind, other outcomes unlikely to
be inuenced by lack of blinding, although
status of outcome assessor unclear
25 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Huang 2008 (Continued)
Incomplete outcome data (attrition bias)
All outcomes
Low risk No participant loss.
Selective reporting (reporting bias) Unclear risk Study protocol unavailable.
Other bias Unclear risk Insufcient reporting.
Kashanian 2010
Methods Single blind randomised controlled trial of acupressure at SP6 or light touch control
group
Participants 120 women were recruited from the labour ward at Akbaradi teaching hospital, Iran
Setting: labour ward at Akbarabadi Teaching hospital in Tehran
Inclusion criteria: age: 18-35 years, nulliparous, singleton, cephalic presentation, gesta-
tional age 37-41 weeks, intact membranes, cervical dilation 3-4 cm, established contrac-
tions (> 3:10 minutes 45-60 seconds duration).
Exclusion criteria: any sedation during labour, abnormal or deceased fetus, fetal distress,
meconium passage, previous hysterotomy or uterine scar, any medical or surgical com-
plications of pregnancy, drug use except usual supplements, vaginal bleeding and high-
risk pregnancy
Interventions Acupressure, performed by investigator, at SP6 during contractions for a total acupressure
time of 30 minutes
Control: touch at SP6, performed by same investigator, for same duration of time
Outcomes Severity of pain as measured by VAS, duration of active phase of labour, mode of delivery,
use of oxytocin, neonatal weight, and Apgar scores
Notes Study duration: March to September 2007. The research was supported by Iran Univer-
sity
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk 4 part block randomisation method (seems
to be computer generated)
Allocation concealment (selection bias) Low risk Sealed envelopes.
Blinding (performance bias and detection
bias)
All outcomes
Unclear risk Participant: unclear.
Clinician: no.
Outcome assessor:
yes.
Describe: treatment was known and ad-
ministered by the investigator. Unclear
26 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Kashanian 2010 (Continued)
whether there was an attempt to conceal
that the control treatment of touch was not
the intervention
Incomplete outcome data (attrition bias)
All outcomes
Unclear risk No discussion of loss of participants at data
collection points. No discussion of exclu-
sions after randomisation but exclusion cri-
teria of any sedation during labour or any
sign of fetal distress could indicate exclu-
sion after randomisation
Selective reporting (reporting bias) Unclear risk The study protocol was unavailable.
Other bias Low risk No imbalances at randomisation.
Lee 2004
Methods Single-blind, randomised controlled trial of acupressure or touch control
Participants 89 women were randomly allocated to the trial. Inclusion criteria for the study were:
greater than 37 weeks pregnant, singleton pregnancy, planning a vaginal delivery and
in good health. Women were recruited to the study from publicity materials in the
outpatient department of a general hospital in Korea
Interventions Women allocated to the intervention group received acupressure at SP6, or to the control
group touch at SP6. The acupressure involved pressure at SP6 on both legs during
a contraction during a 30-minute time period during each contraction. The pressure
applied was 2150 mmHg. The control group received touch with no pressure from the
thumbs
Outcomes Pain was measured along a VAS and assessed at entry, before the intervention was ad-
ministered, after the intervention, and 30 and 60 minutes after the intervention. Other
outcomes included duration of labour, use of pain relief, and maternal anxiety
Notes No power analysis was reported. An intention-to-treat analysis was performed
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk The randomisationsequence was generated
from random-number tables
Allocation concealment (selection bias) Unclear risk Unclear.
Blinding (performance bias and detection
bias)
All outcomes
Low risk The participants and outcome assessors
were blind to group allocation
27 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Lee 2004 (Continued)
Incomplete outcome data (attrition bias)
All outcomes
Unclear risk 14 (15%) women did not complete the
study. Reasons given were caesarean sec-
tion, withdrawal or incomplete data. No
information was reported by group alloca-
tion
Selective reporting (reporting bias) Unclear risk Study protocol unavailable. All pre-speci-
ed outcomes were reported
Other bias Low risk No other bias detected.
Martensson 2008
Methods Randomised controlled trial of acupuncture compared with sterile water injections
Participants 128 women admitted to labour ward in Sweden. Inclusion criteria were: 37-42 weeks
gestation, spontaneous onset of labour, frequency of 3 contractions during 10 minutes
and a requirement for pain relief. Exclusion criteria were: no opoid analgesics, acupunc-
ture, TENS, or sterile water injection in the previous 10 hours, or had received paracer-
vical nerve block, epidural or intrathecal analgesia or augmentation of labour
Interventions Acupuncture group: all women were treated at GV20, LI4 and SP6. Local acupunc-
ture points were selected individually depending on where the pain was perceived; the
midwives could choose 4 to 7 points from BL23-24, BL54, EX19, GB25-29 and KI11.
The acupuncture points were chosen both from recommendations in the literature and
in cooperation with the midwives, the latter in an attempt to imitate normal clinical
practice. The needles (Hegu AB, Landsbro, Sweden) were made of stainless steel (0.3030
or 0.3550 mm). After insertion, the needles were stimulated to evoke needle sensation
(De Qi), a feeling of heaviness, numbness and distension, reecting activation of mus-
cle-nerve afferents. The needles were left in place for 40 minutes, and were stimulated
manually, as described, every 10 minutes. The rst assessment after treatment took place
30 minutes after all the needles were in place. The treatment was repeated if necessary
Water injection group was given 48 subcutaneous injections of 0.5 ml sterile water. The
injections were administered in the area where the woman felt pain; the injections could
be repeated if necessary. A 2-ml plastic syringe (B. Braun Omnix) with a thin needle
(B. Braun Omnix; diameter: 0.40 mm, length: 20 mm) was used. The injections were
administered during a contraction. The rst assessment after treatment took place 30
minutes after all the injections were given
40 midwives administered acupuncture and/or injections of sterile water. All midwives
were equally trained in administration of acupuncture and injection of sterile water. All
protocols were thoroughly standardised
Outcomes Pain and relaxation was assessed using a VAS immediately before and 30, 60, 90, 120,
150 and 180 minutes after treatment. The woman was asked to mark her degree of pain
and relaxation on the 100-mm line with the following endpoints: 0 = no pain at all and
100 = worst conceivable pain, and 0 = totally relaxed and 100 = very tense, for pain and
relaxation, respectively. Obstetric outcomes were also assessed. After delivery, the woman
was asked the extent to which the treatment had provided pain relief and relaxation, and
28 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Martensson 2008 (Continued)
if she would accept the same treatment during a future delivery
Notes Stratied by parity, randomisation in blocks of 10.
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk Computer generated.
Allocation concealment (selection bias) Low risk Sealed opaque envelopes.
Blinding (performance bias and detection
bias)
All outcomes
High risk Women and the care providers were not
blind to their group allocation. No other
details reported
Incomplete outcome data (attrition bias)
All outcomes
Low risk Dropouts dened as events after randomi-
sation leading to no treatment or events
after treatment, such as delivery or re-
quirement for other methods of pain re-
lief. Another midwife undertook womens
assessment of pain and relaxation. The
reasons for drop-out were similar be-
tween groups.16 women in the acupunc-
ture group and 11 women in the injection
group dropped out (total 17% drop out)
Selective reporting (reporting bias) Unclear risk Study protocol was not available.
Other bias Low risk There was a slight imbalance in age, there
appears to be no other source of bias
Nesheim 2003
Methods A single-blind, controlled trial of acupuncture versus standard care
Participants 198 women were enrolled into the trial of acupuncture versus standard care, from a
labour ward in a University hospital in Norway. Women were recruited to the trial who
were at term, experiencing regular contractions and had an ability to speak Norwegian.
Women were excluded if their labour was induced, planning a caesarean section, a plan to
request an epidural block, medical reasons for an epidural, or experiencing any infectious
diseases
Interventions 8 midwives were educated and trained to practice acupuncture for the trial. All women
received other analgesics on demand. The acupuncture points used were selected based
on the participants needs and included points BL32, GV20, BL60, BL62, HT7, LR3,
GB34, CV4, LI10, LI11, BL23, BL27, 28, 32, LI4, SP6, PC6,7, ST36. De qi was
29 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Nesheim 2003 (Continued)
obtained. Needles were left in place for 10-20 minutes, or removed after the needling
sensation was obtained, or taped and left in place. Women in the control group received
conventional care
Outcomes Clinical outcomes included use of meperidine, use of other analgesics, duration of labour,
mode of delivery and Apgar score. Participants also rated their pain relief along a VAS
scale and asked to report any side effects from the treatment
Notes A power analysis was undertaken. An intention-to-treat analysis was performed
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk Computer generated.
Allocation concealment (selection bias) Low risk Adequate, sealed opaque envelopes.
Blinding (performance bias and detection
bias)
All outcomes
High risk Participants, the therapist and care givers
were not blind. Blinding of the analyst was
unclear
Incomplete outcome data (attrition bias)
All outcomes
High risk 6 drop outs, 1 drop out from acupuncture.
Selective reporting (reporting bias) Unclear risk Study protocol was unavailable.
Other bias Low risk Demographic baseline characteristics com-
parable between groups
Qu 2007
Methods Randomised controlled trial of electro-acupuncture or control (no pain relief )
Participants Afliated hospital of Heilongjiang University of Chinese Medicine, China
36 study participants.
Inclusioncriteria: primiparous women, witha normal single pregnancy with spontaneous
onset of labour, cephalic presentation, cervical dilation < 6 cm at admission, gestational
age 37-42 completed weeks
Exclusioncriteria:diabetes, pre-eclampsia, hypertension, kidney disease, thrombocytope-
nia, psychological distress or anorexia, infectious blood disease, atopic eczema or psoriasis
Interventions Acupuncture group: bilateral acupuncture points stimulation of points LI4 and SP6.
Treatment started at beginning of active phase of rst stage of labour. When de-Qi
achieved, needles retained for 2 minutes, then connected to electro-acupuncture stimula-
tor, at a frequency of 2-100Hz, current: 14-30mA. Stimulation increased gradually and
needles removed after 20 minutes. When dilation reached 7-8 cm, procedure performed
30 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Qu 2007 (Continued)
again
Control group: no pain relief.
Outcomes Assessment of pain intensity and degree of relaxation throughout the labour. (Assessed
hourly. Assessment tool 11-point scale: 0 = painless and well relaxed; 10 = worst pain
imaginable and very tense.)
Notes Study duration August 2004 to May 2005.
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk Lot drawing.
Allocation concealment (selection bias) Unclear risk Neither the doctors, midwives, nor the
primiparas could predict the group alloca-
tion.
Blinding (performance bias and detection
bias)
All outcomes
High risk Women and the study practitioner was not
blind to the study groups. No other details
reported
Incomplete outcome data (attrition bias)
All outcomes
Low risk 3 women excluded from the analysis, 2
acupuncture (no pain or relaxation data
available), 1 womanfromthe control group
(no spontaneous labour)
Selective reporting (reporting bias) Unclear risk Study protocol not available.
Other bias Low risk No imbalances at baselines, the study ap-
pears free of other biases
Ramnero 2002
Methods Parallel single-blind, randomised controlled trial of acupuncture. The trial was stratied
by parity. Women received acupuncture or no acupuncture
Participants 100 women were recruited from an antenatal clinic in Sweden. Randomisation took
place in the delivery suite following admission. Inclusion criteria: 37+ weeks gestation,
spontaneous labour, cephalic presentation, cervical dilatation < 7 cm at admission. Ex-
clusion criteria: diabetes, pre-eclampsia, kidney disease, thrombocytopenia, psychologi-
cal distress or anorexia, infectious blood disease, atopic eczema or psoriasis
Interventions All women had access to conventional analgesia. Eleven midwives completed a 4-day
course in acupuncture for labour pain. These midwives administered acupuncture to
the treatment group. Acupuncture treatment was individualised with relaxing points
31 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Ramnero 2002 (Continued)
combined with local and distal analgesic points. Needles were inserted at 45 or 90 degrees,
stimulated manually until de qui (needling sensation) was obtained. Needles were left
in situ and removed after 1-3 hours
Outcomes Painintensity and degree of relaxationwas assessed once every hour, prior to any analgesic
and 15 minutes after. Other outcomes included; the use of analgesics, augmentation of
labour with oxytocin, duration of labour, outcome of birth, antepartum haemorrhage,
Apgar scores, and infant birthweight
Notes No sample-size calculation was described. An intention-to-treat analysis was performed
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk Randomisation was generated by shufing
cards.
Allocation concealment (selection bias) Low risk Adequate, concealed in sealed, opaque en-
velopes.
Blinding (performance bias and detection
bias)
All outcomes
High risk The outcome assessor was not blind and
it was unclear if the analyst was blind to
treatment allocation. Women and the prac-
titioner were not blind to group allocation
Incomplete outcome data (attrition bias)
All outcomes
Low risk 10 (10%) were excluded from the analy-
sis after not meeting the inclusion criteria
(breech presentation, not in active labour,
not in spontaneous labour, missing pain
and relaxation data). 5 fromeach group re-
lating to not in active labour, breech pre-
sentation, not inspontaneous labour, emer-
gency caesarean section, no assessment of
pain
Selective reporting (reporting bias) Unclear risk Study protocol unavailable.
Other bias Low risk Baseline characteristics comparable be-
tween groups, no other identiable source
of bias
32 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Skilnand 2002
Methods Single-blind, randomised controlled trial of acupuncture versus minimal acupuncture
Participants 210 women were recruited from the maternity ward of a hospital in Norway. Women
with a singleton pregnancy, cephalic presentation, in spontaneous active labour met the
inclusion criteria. 110 women refused to participate in the trial
Interventions Real acupuncture followed a treatment protocol. The protocol specied obtaining the
de qi sensation, needles were taped and left in place until delivery or until conventional
analgesics were required. Acupuncture points included HT7, LU7, ST30, ST29, GB34,
ST36, SP8, SP6, KI3, GB41, LR3, GV20, BL34, BL32, LI4, BL67, BL60. Minimal
acupuncture involved the same procedure but needles were inserted away fromthe merid-
ians. Some needles were removed after 20 minutes if insufcient pain relief was provided
by the treatment and control interventions. Conventional pain relief was made available.
Midwives providing the intervention had received formal training in acupuncture
Outcomes Pain was assessed along a 10 cm VAS, recorded at 30 minutes, 1 and 2 hours after
treatment, the need for conventional pain relief and use of oxytocin
Notes No power analysis was reported.
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Low risk Randomisation was assigned by drawing
lots.
Allocation concealment (selection bias) Low risk Adequate, randomisation concealed in
sealed in opaque envelopes
Blinding (performance bias and detection
bias)
All outcomes
Low risk Women were blind to their group alloca-
tion and study personnel collecting data
were unaware of womens study group allo-
cation
Incomplete outcome data (attrition bias)
All outcomes
Low risk 2 women were excluded from the control
group because they delivered prior to the
intervention being administered
Selective reporting (reporting bias) Unclear risk Study protocol unavailable.
Other bias High risk There was an imbalance in parity at base-
line.
33 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Ziaei 2006
Methods Randomised controlled trial of acupuncture compared with placebo acupuncture and
no intervention
Participants 90 women were recruited froma hospital in Tehran, Iran. Inclusion criteria: were normal
singleton pregnancy of 37 weeks or longer and a spontaneous onset of labour, cephalic
version, cervical dilatation of 3-6 cm
Interventions Acupuncture (30 women): solid titanium needles GV20, Yingtang, ST36, SP6, LI4,
CV2, 3. Needle insertionbeganwhenpre-treatment painscore of 3or higher was reached.
A feeling of de qi was obtained. Nedles left in place until delivery.
Control group 1 (30 women): pretend acupuncture, solid titanium needles of same type
as intervention, inserted at 6 points normally used for vaccinations and other injections
Control group 2 (30 women): npo intervention.
Outcomes Pain intensity, relaxation, duration of labour, need for augmentation by oxytocin, cae-
sarean delivery
Notes
Risk of bias
Bias Authors judgement Support for judgement
Random sequence generation (selection
bias)
Unclear risk The study was randomised but unclear
methods in the brief communication
Allocation concealment (selection bias) Unclear risk The study was randomised but unclear
methods in the brief communication
Blinding (performance bias and detection
bias)
All outcomes
Unclear risk Women were blind to their group alloca-
tion. The study practitioner was not blind
to group allocation. The status of the out-
come assessor and analyst was unclear
Incomplete outcome data (attrition bias)
All outcomes
Unclear risk Insufcient reporting.
Selective reporting (reporting bias) Unclear risk Insufcient reporting.
Other bias Unclear risk Insufcient reporting.
TENS: transcutaneous electrical nerve stimulation
VAS: visual analogue scale
34 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Characteristics of excluded studies [ordered by study ID]
Study Reason for exclusion
Bo 2006 We were unable to establish study details to determine details of randomisation, blinding and data completeness
Deen 1985 We were unable to establish study details to determine the exact study design
Li 2006 We were unable to conrm if the study was a randomised controlled trial following communication with the authors
Li 1996 This trial evaluated the effect of 2 acupuncture points on the strength and timing of uterine contractions following
acupuncture. It did not report on any primary outcomes relevant to this review by study group
Park 2003 Abstract only published. Insufcient data reported to assess if eligibility criteria met
Shalev 1991 25 women recruited during labour at a maternity hospital in Israel. 13 women randomised to receive electroacupunc-
ture and 12 women received no analgesia at the start of the active phase of labour (cervical dilatation 4 cm, effacement
60%). The study reported on beta endorphin levels and did not report on any measures relevant to this review
Shang 1995 In this trial of 161 women, the effect of acupuncture on Hegu point was examined in relation to the length of the
second stage of labour and the amount of postpartum bleeding. The study was excluded as it did not examine the
effect on pain relief
Ternov 1998 We were unable to establish the study design quasi-random or a controlled clinical trial
Zhang 2000 The evaluation of point injection therapy did not meet our eligibility criteria
Characteristics of studies awaiting assessment [ordered by study ID]
Fei 1985
Methods
Participants
Interventions
Outcomes
Notes Awaiting translation.
35 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Su 2001
Methods
Participants
Interventions
Outcomes
Notes Awaiting translation.
Wang 1994
Methods
Participants
Interventions
Outcomes
Notes Awaiting translation.
Xu 2000
Methods
Participants
Interventions
Outcomes
Notes Awaiting translation.
Zhang 2002
Methods
Participants
Interventions
Outcomes
Notes Awaiting translation.
36 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Characteristics of ongoing studies [ordered by study ID]
MacKenzie 2005
Trial name or title Acupuncture for pain relief during induced labour for nulliparae
Methods Randomised controlled trial, double blind (subject, caregiver, outcome assessor)
Participants 105 women aged 18 years of greater, nulliparous having an induction of labour for prolonged pregnancy or
mild hypertension, no previous experience of acupuncture
Interventions No details reported.
Outcomes Use of epidural.
Starting date August 2005
Contact information IZ MacKenzie, University of Oxford.
Notes Recruitment complete.
Martensson 2008
Trial name or title Acupuncture to reduce labour pain.
Methods Randomised controlled trial of electro-acupuncture compared with manual acupuncture
Participants 300 Swedish women admitted to labour ward in spontaneous labour (latent or active labour phase). Nulli-
parous, singleton pregnancy, cephalic presentation, gestation 37+0 to 41.6 weeks and days, with an expressed
need for pain relief, Swedish speaking. Exclusion criteria: no pharmacological pain relief within 24 hours
prior to inclusion in the study, pre-eclampsia, treatment with oxytocin at the time of randomisation, use of
anticoagulants, pacemaker
Interventions Manual acupuncture compared with electro-acupuncture.
Outcomes Experience of labour pain, use of epidural.
Starting date October 2008.
Contact information Dr Lena Martensson, University of Skovde, lena.martensson@his.se, phone +46500448000
Notes Recruiting.
37 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Mohamadinia 2008
Trial name or title Comparing Hoku point (LI4) acupressure and San-Yin-Jiao (SP6) acupressure on labour pain and length of
delivery time in nulliparous women in Iran hospital 2008-2009
Methods Randomised single blind trial.
Participants 60 Iranian women in active labour, with a gestational age between 38-42 weeks, singleton pregnancy, cephalic
presentation, primiparous, good health, planning a vaginal delivery. Exclusion criteria: psychotic and di-
agnosed anatomic disorder, chronic disease inammation or eczema in the acupressure region, gestational
diabetes, polyhydramnios, reduced fetal movements, intrauterine growth restriction, fetal death, history of
chronic pelvic pain, abnormal fetal heart rate, taking psychotherapeutic medication
Interventions Intervention administered over 20 minutes.
Outcomes Labour pain, duration of labour.
Starting date January 2008.
Contact information Mrs Neda Mohamadina, Midwifery Dept, Iranshahr Faculty of Medical Sciences, Iranshahr, Iran. Phone
00985473310482, email Tahninehslehian@yahoo.com
Notes Recruitment complete.
38 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
D A T A A N D A N A L Y S E S
Comparison 1. Acupuncture versus control
Outcome or subgroup title
No. of
studies
No. of
participants
Statistical method Effect size
1 Pain intensity 4 Std. Mean Difference (IV, Fixed, 95% CI) Subtotals only
1.1 Placebo control 2 240 Std. Mean Difference (IV, Fixed, 95% CI) 0.04 [-0.22, 0.30]
1.2 Standard care 1 90 Std. Mean Difference (IV, Fixed, 95% CI) -0.14 [-0.55, 0.28]
1.3 No treatment 1 163 Std. Mean Difference (IV, Fixed, 95% CI) 1.00 [-1.33, -0.67]
2 Satisfaction with pain relief in
labour
2 Risk Ratio (M-H, Fixed, 95% CI) Subtotals only
2.1 Placebo control 1 150 Risk Ratio (M-H, Fixed, 95% CI) 2.38 [1.78, 3.19]
2.2 Standard care 1 90 Risk Ratio (M-H, Fixed, 95% CI) 1.08 [0.95, 1.22]
3 Use of pharmacological analgesia 5 Risk Ratio (M-H, Random, 95% CI) Subtotals only
3.1 Placebo control 1 208 Risk Ratio (M-H, Random, 95% CI) 0.72 [0.58, 0.88]
3.2 Standard care 3 704 Risk Ratio (M-H, Random, 95% CI) 0.68 [0.56, 0.83]
3.3 Water injection 1 128 Risk Ratio (M-H, Random, 95% CI) 0.84 [0.54, 1.30]
4 Caesarean section 7 Risk Ratio (M-H, Fixed, 95% CI) Subtotals only
4.1 Placebo control 3 448 Risk Ratio (M-H, Fixed, 95% CI) 1.39 [0.62, 3.10]
4.2 Standard care 2 506 Risk Ratio (M-H, Fixed, 95% CI) 0.86 [0.47, 1.60]
4.3 No treatment 1 163 Risk Ratio (M-H, Fixed, 95% CI) 0.76 [0.35, 1.63]
4.4 Water injection 1 128 Risk Ratio (M-H, Fixed, 95% CI) 1.33 [0.37, 4.73]
5 Assisted vaginal birth 6 Risk Ratio (M-H, Fixed, 95% CI) Subtotals only
5.1 Placebo control 1 208 Risk Ratio (M-H, Fixed, 95% CI) 0.64 [0.27, 1.50]
5.2 Standard care 3 704 Risk Ratio (M-H, Fixed, 95% CI) 0.67 [0.46, 0.98]
5.3 No treatment 1 163 Risk Ratio (M-H, Fixed, 95% CI) 0.49 [0.18, 1.38]
5.4 Water injection 1 128 Risk Ratio (M-H, Fixed, 95% CI) 1.60 [0.47, 5.39]
6 Apgar score < 7 at 5 minutes 4 Risk Ratio (M-H, Fixed, 95% CI) Subtotals only
6.1 Placebo control 1 208 Risk Ratio (M-H, Fixed, 95% CI) 0.32 [0.01, 7.79]
6.2 Standard care 3 706 Risk Ratio (M-H, Fixed, 95% CI) 0.60 [0.12, 2.99]
7 Spontaneous vaginal delivery 3 Risk Ratio (M-H, Random, 95% CI) Subtotals only
7.1 Placebo control 2 358 Risk Ratio (M-H, Random, 95% CI) 1.00 [0.87, 1.14]
7.2 Standard care 1 90 Risk Ratio (M-H, Random, 95% CI) 0.98 [0.89, 1.08]
8 Augmentation with oxytocin 5 Risk Ratio (M-H, Random, 95% CI) Subtotals only
8.1 Placebo control 2 358 Risk Ratio (M-H, Random, 95% CI) 0.62 [0.15, 2.52]
8.2 Standard care 2 506 Risk Ratio (M-H, Random, 95% CI) 0.88 [0.72, 1.08]
8.3 Water injection 1 128 Risk Ratio (M-H, Random, 95% CI) 1.16 [0.85, 1.58]
9 Relaxation 3 Std. Mean Difference (IV, Fixed, 95% CI) Subtotals only
9.1 placebo control 1 90 Std. Mean Difference (IV, Fixed, 95% CI) -0.27 [-0.72, 0.17]
9.2 Standard care 1 90 Std. Mean Difference (IV, Fixed, 95% CI) -0.51 [-0.93, -0.09]
9.3 Water injection 1 128 Std. Mean Difference (IV, Fixed, 95% CI) 0.55 [0.20, 0.91]
39 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Comparison 2. Acupressure versus control
Outcome or subgroup title
No. of
studies
No. of
participants
Statistical method Effect size
1 Pain intensity 3 Std. Mean Difference (IV, Random, 95% CI) Subtotals only
1.1 Placebo control 1 120 Std. Mean Difference (IV, Random, 95% CI) -0.55 [-0.92, -0.19]
1.2 Combined control 2 322 Std. Mean Difference (IV, Random, 95% CI) -0.42 [-0.65, -0.18]
2 Satisfaction with childbirth 1 Mean Difference (IV, Fixed, 95% CI) Subtotals only
2.1 Combined control 1 211 Mean Difference (IV, Fixed, 95% CI) 4.80 [-2.29, 11.89]
3 Use of pharmacological analgesia 2 Risk Ratio (M-H, Fixed, 95% CI) Subtotals only
3.1 Placebo control 1 75 Risk Ratio (M-H, Fixed, 95% CI) 0.54 [0.20, 1.43]
3.2 Combined control 1 212 Risk Ratio (M-H, Fixed, 95% CI) 0.94 [0.71, 1.25]
4 Caesarean section 2 Risk Ratio (M-H, Fixed, 95% CI) Subtotals only
4.1 Placebo control 1 120 Risk Ratio (M-H, Fixed, 95% CI) 0.24 [0.11, 0.54]
4.2 Combined control 1 212 Risk Ratio (M-H, Fixed, 95% CI) 0.48 [0.22, 1.04]
5 Assisted vaginal birth 1 Risk Ratio (M-H, Fixed, 95% CI) Subtotals only
5.1 Combined control 1 212 Risk Ratio (M-H, Fixed, 95% CI) 0.81 [0.39, 1.67]
6 Apgar score < 7 at 5 minutes 1 120 Risk Ratio (M-H, Fixed, 95% CI) 0.0 [0.0, 0.0]
6.1 Placebo control 1 120 Risk Ratio (M-H, Fixed, 95% CI) 0.0 [0.0, 0.0]
7 Augmentation with oxytocin 2 Risk Ratio (M-H, Fixed, 95% CI) Subtotals only
7.1 Placebo control 1 120 Risk Ratio (M-H, Fixed, 95% CI) 0.66 [0.46, 0.94]
7.2 Combined control 1 212 Risk Ratio (M-H, Fixed, 95% CI) 1.01 [0.77, 1.31]
8 Length of labour 2 Std. Mean Difference (IV, Random, 95% CI) Subtotals only
8.1 Placebo control 2 195 Std. Mean Difference (IV, Random, 95% CI) -1.06 [-1.74, -0.38]
9 Anxiety 1 Mean Difference (IV, Fixed, 95% CI) Subtotals only
9.1 Placebo control 1 75 Mean Difference (IV, Fixed, 95% CI) -1.40 [-2.51, -0.29]
40 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 1.1. Comparison 1 Acupuncture versus control, Outcome 1 Pain intensity.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 1 Acupuncture versus control
Outcome: 1 Pain intensity
Study or subgroup Acupuncture Control Std. Mean Difference Weight Std. Mean Difference
N Mean(SD) N Mean(SD) IV,Fixed,95% CI IV,Fixed,95% CI
1 Placebo control
Hantoushzadeh 2007 75 52.64 (2.9) 75 52.94 (3.75) 65.4 % -0.09 [ -0.41, 0.23 ]
Ziaei 2006 30 8.52 (1.45) 60 8.05 (1.75) 34.6 % 0.28 [ -0.16, 0.72 ]
Subtotal (95% CI) 105 135 100.0 % 0.04 [ -0.22, 0.30 ]
Heterogeneity: Chi
2
= 1.78, df = 1 (P = 0.18); I
2
=44%
Test for overall effect: Z = 0.30 (P = 0.77)
2 Standard care
Ramnero 2002 46 6.6 (1.51) 44 6.8 (1.4) 100.0 % -0.14 [ -0.55, 0.28 ]
Subtotal (95% CI) 46 44 100.0 % -0.14 [ -0.55, 0.28 ]
Heterogeneity: not applicable
Test for overall effect: Z = 0.64 (P = 0.52)
3 No treatment
Huang 2008 82 6.76 (1.41) 81 7.92 (0.82) 100.0 % -1.00 [ -1.33, -0.67 ]
Subtotal (95% CI) 82 81 100.0 % -1.00 [ -1.33, -0.67 ]
Heterogeneity: not applicable
Test for overall effect: Z = 6.01 (P < 0.00001)
Test for subgroup differences: Chi
2
= 24.82, df = 2 (P = 0.00), I
2
=92%
-10 -5 0 5 10
Favours acupuncture Favours control
41 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 1.2. Comparison 1 Acupuncture versus control, Outcome 2 Satisfaction with pain relief in labour.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 1 Acupuncture versus control
Outcome: 2 Satisfaction with pain relief in labour
Study or subgroup Acupuncture Control Risk Ratio Weight Risk Ratio
n/N n/N M-H,Fixed,95% CI M-H,Fixed,95% CI
1 Placebo control
Hantoushzadeh 2007 69/75 29/75 100.0 % 2.38 [ 1.78, 3.19 ]
Subtotal (95% CI) 75 75 100.0 % 2.38 [ 1.78, 3.19 ]
Total events: 69 (Acupuncture), 29 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 5.80 (P < 0.00001)
2 Standard care
Ramnero 2002 44/46 39/44 100.0 % 1.08 [ 0.95, 1.22 ]
Subtotal (95% CI) 46 44 100.0 % 1.08 [ 0.95, 1.22 ]
Total events: 44 (Acupuncture), 39 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 1.22 (P = 0.22)
0.1 0.2 0.5 1 2 5 10
Favours control Favours acupuncture
42 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 1.3. Comparison 1 Acupuncture versus control, Outcome 3 Use of pharmacological analgesia.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 1 Acupuncture versus control
Outcome: 3 Use of pharmacological analgesia
Study or subgroup Acupuncture Control Risk Ratio Weight Risk Ratio
n/N n/N M-H,Random,95% CI M-H,Random,95% CI
1 Placebo control
Skilnand 2002 58/106 78/102 100.0 % 0.72 [ 0.58, 0.88 ]
Subtotal (95% CI) 106 102 100.0 % 0.72 [ 0.58, 0.88 ]
Total events: 58 (Acupuncture), 78 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 3.22 (P = 0.0013)
2 Standard care
Borup 2009 185/291 124/125 45.7 % 0.64 [ 0.59, 0.70 ]
Nesheim 2003 70/106 75/92 36.5 % 0.81 [ 0.69, 0.96 ]
Ramnero 2002 20/46 34/44 17.8 % 0.56 [ 0.39, 0.81 ]
Subtotal (95% CI) 443 261 100.0 % 0.68 [ 0.56, 0.83 ]
Total events: 275 (Acupuncture), 233 (Control)
Heterogeneity: Tau
2
= 0.02; Chi
2
= 6.90, df = 2 (P = 0.03); I
2
=71%
Test for overall effect: Z = 3.91 (P = 0.000092)
3 Water injection
Martensson 2008 22/62 28/66 100.0 % 0.84 [ 0.54, 1.30 ]
Subtotal (95% CI) 62 66 100.0 % 0.84 [ 0.54, 1.30 ]
Total events: 22 (Acupuncture), 28 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.80 (P = 0.42)
0.1 0.2 0.5 1 2 5 10
Acupuncture lower Control higher
43 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 1.4. Comparison 1 Acupuncture versus control, Outcome 4 Caesarean section.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 1 Acupuncture versus control
Outcome: 4 Caesarean section
Study or subgroup Acupuncture Control Risk Ratio Weight Risk Ratio
n/N n/N M-H,Fixed,95% CI M-H,Fixed,95% CI
1 Placebo control
Hantoushzadeh 2007 3/75 1/75 11.0 % 3.00 [ 0.32, 28.19 ]
Skilnand 2002 3/106 4/102 44.9 % 0.72 [ 0.17, 3.15 ]
Ziaei 2006 5/30 6/60 44.1 % 1.67 [ 0.55, 5.02 ]
Subtotal (95% CI) 211 237 100.0 % 1.39 [ 0.62, 3.10 ]
Total events: 11 (Acupuncture), 11 (Control)
Heterogeneity: Chi
2
= 1.32, df = 2 (P = 0.52); I
2
=0.0%
Test for overall effect: Z = 0.80 (P = 0.42)
2 Standard care
Borup 2009 26/291 13/125 94.7 % 0.86 [ 0.46, 1.62 ]
Ramnero 2002 1/46 1/44 5.3 % 0.96 [ 0.06, 14.83 ]
Subtotal (95% CI) 337 169 100.0 % 0.86 [ 0.47, 1.60 ]
Total events: 27 (Acupuncture), 14 (Control)
Heterogeneity: Chi
2
= 0.01, df = 1 (P = 0.94); I
2
=0.0%
Test for overall effect: Z = 0.46 (P = 0.64)
3 No treatment
Huang 2008 10/82 13/81 100.0 % 0.76 [ 0.35, 1.63 ]
Subtotal (95% CI) 82 81 100.0 % 0.76 [ 0.35, 1.63 ]
Total events: 10 (Acupuncture), 13 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.70 (P = 0.48)
4 Water injection
Martensson 2008 5/62 4/66 100.0 % 1.33 [ 0.37, 4.73 ]
Subtotal (95% CI) 62 66 100.0 % 1.33 [ 0.37, 4.73 ]
Total events: 5 (Acupuncture), 4 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.44 (P = 0.66)
0.1 0.2 0.5 1 2 5 10
Acupuncture lower Control higher
44 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 1.5. Comparison 1 Acupuncture versus control, Outcome 5 Assisted vaginal birth.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 1 Acupuncture versus control
Outcome: 5 Assisted vaginal birth
Study or subgroup Acupuncture Control Risk Ratio Weight Risk Ratio
n/N n/N M-H,Fixed,95% CI M-H,Fixed,95% CI
1 Placebo control
Skilnand 2002 8/106 12/102 100.0 % 0.64 [ 0.27, 1.50 ]
Subtotal (95% CI) 106 102 100.0 % 0.64 [ 0.27, 1.50 ]
Total events: 8 (Acupuncture), 12 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 1.02 (P = 0.31)
2 Standard care
Borup 2009 38/291 28/125 75.4 % 0.58 [ 0.38, 0.91 ]
Nesheim 2003 11/106 11/92 22.7 % 0.87 [ 0.39, 1.91 ]
Ramnero 2002 2/46 1/44 2.0 % 1.91 [ 0.18, 20.35 ]
Subtotal (95% CI) 443 261 100.0 % 0.67 [ 0.46, 0.98 ]
Total events: 51 (Acupuncture), 40 (Control)
Heterogeneity: Chi
2
= 1.56, df = 2 (P = 0.46); I
2
=0.0%
Test for overall effect: Z = 2.05 (P = 0.040)
3 No treatment
Huang 2008 5/82 10/81 100.0 % 0.49 [ 0.18, 1.38 ]
Subtotal (95% CI) 82 81 100.0 % 0.49 [ 0.18, 1.38 ]
Total events: 5 (Acupuncture), 10 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 1.34 (P = 0.18)
4 Water injection
Martensson 2008 6/62 4/66 100.0 % 1.60 [ 0.47, 5.39 ]
Subtotal (95% CI) 62 66 100.0 % 1.60 [ 0.47, 5.39 ]
Total events: 6 (Acupuncture), 4 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.75 (P = 0.45)
0.1 0.2 0.5 1 2 5 10
Acupuncture lower Control higher
45 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 1.6. Comparison 1 Acupuncture versus control, Outcome 6 Apgar score < 7 at 5 minutes.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 1 Acupuncture versus control
Outcome: 6 Apgar score < 7 at 5 minutes
Study or subgroup Acupuncture control Risk Ratio Risk Ratio
n/N n/N M-H,Fixed,95% CI M-H,Fixed,95% CI
1 Placebo control
Skilnand 2002 0/106 1/102 0.32 [ 0.01, 7.79 ]
Subtotal (95% CI) 106 102 0.32 [ 0.01, 7.79 ]
Total events: 0 (Acupuncture), 1 (control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.70 (P = 0.48)
2 Standard care
Borup 2009 1/291 2/125 0.21 [ 0.02, 2.35 ]
Nesheim 2003 1/106 0/92 2.61 [ 0.11, 63.24 ]
Ramnero 2002 0/46 0/46 0.0 [ 0.0, 0.0 ]
Subtotal (95% CI) 443 263 0.60 [ 0.12, 2.99 ]
Total events: 2 (Acupuncture), 2 (control)
Heterogeneity: Chi
2
= 1.52, df = 1 (P = 0.22); I
2
=34%
Test for overall effect: Z = 0.62 (P = 0.53)
0.1 0.2 0.5 1 2 5 10
Acupuncture lower Control higher
46 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 1.7. Comparison 1 Acupuncture versus control, Outcome 7 Spontaneous vaginal delivery.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 1 Acupuncture versus control
Outcome: 7 Spontaneous vaginal delivery
Study or subgroup Acupuncture Control Risk Ratio Weight Risk Ratio
n/N n/N M-H,Random,95% CI M-H,Random,95% CI
1 Placebo control
Hantoushzadeh 2007 70/75 74/75 54.7 % 0.95 [ 0.89, 1.01 ]
Skilnand 2002 95/106 86/102 45.3 % 1.06 [ 0.96, 1.18 ]
Subtotal (95% CI) 181 177 100.0 % 1.00 [ 0.87, 1.14 ]
Total events: 165 (Acupuncture), 160 (Control)
Heterogeneity: Tau
2
= 0.01; Chi
2
= 4.64, df = 1 (P = 0.03); I
2
=78%
Test for overall effect: Z = 0.04 (P = 0.97)
2 Standard care
Ramnero 2002 43/46 42/44 100.0 % 0.98 [ 0.89, 1.08 ]
Subtotal (95% CI) 46 44 100.0 % 0.98 [ 0.89, 1.08 ]
Total events: 43 (Acupuncture), 42 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.41 (P = 0.68)
0.1 0.2 0.5 1 2 5 10
Favours control Favours acupuncture
47 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 1.8. Comparison 1 Acupuncture versus control, Outcome 8 Augmentation with oxytocin.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 1 Acupuncture versus control
Outcome: 8 Augmentation with oxytocin
Study or subgroup Acupuncture Control Risk Ratio Weight Risk Ratio
n/N n/N M-H,Random,95% CI M-H,Random,95% CI
1 Placebo control
Hantoushzadeh 2007 67/75 72/75 51.8 % 0.93 [ 0.85, 1.02 ]
Skilnand 2002 15/106 36/102 48.2 % 0.40 [ 0.23, 0.69 ]
Subtotal (95% CI) 181 177 100.0 % 0.62 [ 0.15, 2.52 ]
Total events: 82 (Acupuncture), 108 (Control)
Heterogeneity: Tau
2
= 0.98; Chi
2
= 26.45, df = 1 (P<0.00001); I
2
=96%
Test for overall effect: Z = 0.67 (P = 0.50)
2 Standard care
Borup 2009 129/291 64/125 87.6 % 0.87 [ 0.70, 1.07 ]
Ramnero 2002 16/46 15/44 12.4 % 1.02 [ 0.58, 1.80 ]
Subtotal (95% CI) 337 169 100.0 % 0.88 [ 0.72, 1.08 ]
Total events: 145 (Acupuncture), 79 (Control)
Heterogeneity: Tau
2
= 0.0; Chi
2
= 0.28, df = 1 (P = 0.60); I
2
=0.0%
Test for overall effect: Z = 1.21 (P = 0.23)
3 Water injection
Martensson 2008 37/62 34/66 100.0 % 1.16 [ 0.85, 1.58 ]
Subtotal (95% CI) 62 66 100.0 % 1.16 [ 0.85, 1.58 ]
Total events: 37 (Acupuncture), 34 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.93 (P = 0.35)
0.1 0.2 0.5 1 2 5 10
Acupuncture lower Control higher
48 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 1.9. Comparison 1 Acupuncture versus control, Outcome 9 Relaxation.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 1 Acupuncture versus control
Outcome: 9 Relaxation
Study or subgroup Favours acupuncture Control Std. Mean Difference Weight Std. Mean Difference
N Mean(SD) N Mean(SD) IV,Fixed,95% CI IV,Fixed,95% CI
1 placebo control
Ziaei 2006 30 3.52 (1.5) 60 3.97 (1.68) 100.0 % -0.27 [ -0.72, 0.17 ]
Subtotal (95% CI) 30 60 100.0 % -0.27 [ -0.72, 0.17 ]
Heterogeneity: not applicable
Test for overall effect: Z = 1.22 (P = 0.22)
2 Standard care
Ramnero 2002 46 4.2 (1.52) 44 5.1 (1.94) 100.0 % -0.51 [ -0.93, -0.09 ]
Subtotal (95% CI) 46 44 100.0 % -0.51 [ -0.93, -0.09 ]
Heterogeneity: not applicable
Test for overall effect: Z = 2.39 (P = 0.017)
3 Water injection
Martensson 2008 62 68.6 (22.7) 66 56 (22.59) 100.0 % 0.55 [ 0.20, 0.91 ]
Subtotal (95% CI) 62 66 100.0 % 0.55 [ 0.20, 0.91 ]
Heterogeneity: not applicable
Test for overall effect: Z = 3.07 (P = 0.0022)
Test for subgroup differences: Chi
2
= 16.64, df = 2 (P = 0.00), I
2
=88%
-10 -5 0 5 10
Favours acupuncture Favours control
49 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 2.1. Comparison 2 Acupressure versus control, Outcome 1 Pain intensity.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 2 Acupressure versus control
Outcome: 1 Pain intensity
Study or subgroup Acupressure Control Std. Mean Difference Weight Std. Mean Difference
N Mean(SD) N Mean(SD) IV,Random,95% CI IV,Random,95% CI
1 Placebo control
Kashanian 2010 60 5.87 (1.77) 60 6.79 (1.52) 100.0 % -0.55 [ -0.92, -0.19 ]
Subtotal (95% CI) 60 60 100.0 % -0.55 [ -0.92, -0.19 ]
Heterogeneity: not applicable
Test for overall effect: Z = 2.98 (P = 0.0029)
2 Combined control
Chung 2003 37 0.17 (1.32) 73 0.74 (1.28) 34.1 % -0.44 [ -0.84, -0.04 ]
Hjelmstedt 2010 71 74 (18.2) 141 81.43 (18.1) 65.9 % -0.41 [ -0.70, -0.12 ]
Subtotal (95% CI) 108 214 100.0 % -0.42 [ -0.65, -0.18 ]
Heterogeneity: Tau
2
= 0.0; Chi
2
= 0.01, df = 1 (P = 0.91); I
2
=0.0%
Test for overall effect: Z = 3.51 (P = 0.00045)
-10 -5 0 5 10
Favours acupressure Favours control
Analysis 2.2. Comparison 2 Acupressure versus control, Outcome 2 Satisfaction with childbirth.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 2 Acupressure versus control
Outcome: 2 Satisfaction with childbirth
Study or subgroup Acupressure Control Mean Difference Weight Mean Difference
N Mean(SD) N Mean(SD) IV,Fixed,95% CI IV,Fixed,95% CI
1 Combined control
Hjelmstedt 2010 70 85 (25) 141 80.2 (24.2) 100.0 % 4.80 [ -2.29, 11.89 ]
Subtotal (95% CI) 70 141 100.0 % 4.80 [ -2.29, 11.89 ]
Heterogeneity: not applicable
Test for overall effect: Z = 1.33 (P = 0.18)
Test for subgroup differences: Not applicable
-10 -5 0 5 10
Favours control Favours acupressure
50 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 2.3. Comparison 2 Acupressure versus control, Outcome 3 Use of pharmacological analgesia.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 2 Acupressure versus control
Outcome: 3 Use of pharmacological analgesia
Study or subgroup Acupressure Control Risk Ratio Weight Risk Ratio
n/N n/N M-H,Fixed,95% CI M-H,Fixed,95% CI
1 Placebo control
Lee 2004 5/36 10/39 100.0 % 0.54 [ 0.20, 1.43 ]
Subtotal (95% CI) 36 39 100.0 % 0.54 [ 0.20, 1.43 ]
Total events: 5 (Acupressure), 10 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 1.23 (P = 0.22)
2 Combined control
Hjelmstedt 2010 35/71 74/141 100.0 % 0.94 [ 0.71, 1.25 ]
Subtotal (95% CI) 71 141 100.0 % 0.94 [ 0.71, 1.25 ]
Total events: 35 (Acupressure), 74 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.43 (P = 0.66)
0.1 0.2 0.5 1 2 5 10
Acupressure lower Control higher
51 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 2.4. Comparison 2 Acupressure versus control, Outcome 4 Caesarean section.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 2 Acupressure versus control
Outcome: 4 Caesarean section
Study or subgroup Acupressure Control Risk Ratio Weight Risk Ratio
n/N n/N M-H,Fixed,95% CI M-H,Fixed,95% CI
1 Placebo control
Kashanian 2010 6/60 25/60 100.0 % 0.24 [ 0.11, 0.54 ]
Subtotal (95% CI) 60 60 100.0 % 0.24 [ 0.11, 0.54 ]
Total events: 6 (Acupressure), 25 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 3.43 (P = 0.00061)
2 Combined control
Hjelmstedt 2010 7/71 29/141 100.0 % 0.48 [ 0.22, 1.04 ]
Subtotal (95% CI) 71 141 100.0 % 0.48 [ 0.22, 1.04 ]
Total events: 7 (Acupressure), 29 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 1.86 (P = 0.063)
0.1 0.2 0.5 1 2 5 10
Acupressure lower Control higher
Analysis 2.5. Comparison 2 Acupressure versus control, Outcome 5 Assisted vaginal birth.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 2 Acupressure versus control
Outcome: 5 Assisted vaginal birth
Study or subgroup Acupressure Control Risk Ratio Weight Risk Ratio
n/N n/N M-H,Fixed,95% CI M-H,Fixed,95% CI
1 Combined control
Hjelmstedt 2010 9/71 22/141 100.0 % 0.81 [ 0.39, 1.67 ]
Subtotal (95% CI) 71 141 100.0 % 0.81 [ 0.39, 1.67 ]
Total events: 9 (Acupressure), 22 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.56 (P = 0.57)
0.1 0.2 0.5 1 2 5 10
Acupressure lower Control higher
52 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 2.6. Comparison 2 Acupressure versus control, Outcome 6 Apgar score < 7 at 5 minutes.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 2 Acupressure versus control
Outcome: 6 Apgar score < 7 at 5 minutes
Study or subgroup Acupressure Control Risk Ratio Risk Ratio
n/N n/N M-H,Fixed,95% CI M-H,Fixed,95% CI
1 Placebo control
Kashanian 2010 0/60 0/60 0.0 [ 0.0, 0.0 ]
Total (95% CI) 60 60 0.0 [ 0.0, 0.0 ]
Total events: 0 (Acupressure), 0 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.0 (P < 0.00001)
Test for subgroup differences: Chi
2
= 0.0, df = -1 (P = 0.0), I
2
=0.0%
0.01 0.1 1 10 100
Favours experimental Favours control
Analysis 2.7. Comparison 2 Acupressure versus control, Outcome 7 Augmentation with oxytocin.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 2 Acupressure versus control
Outcome: 7 Augmentation with oxytocin
Study or subgroup Acupressure Control Risk Ratio Weight Risk Ratio
n/N n/N M-H,Fixed,95% CI M-H,Fixed,95% CI
1 Placebo control
Kashanian 2010 25/60 38/60 100.0 % 0.66 [ 0.46, 0.94 ]
Subtotal (95% CI) 60 60 100.0 % 0.66 [ 0.46, 0.94 ]
Total events: 25 (Acupressure), 38 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 2.31 (P = 0.021)
2 Combined control
Hjelmstedt 2010 38/71 75/141 100.0 % 1.01 [ 0.77, 1.31 ]
Subtotal (95% CI) 71 141 100.0 % 1.01 [ 0.77, 1.31 ]
Total events: 38 (Acupressure), 75 (Control)
Heterogeneity: not applicable
Test for overall effect: Z = 0.05 (P = 0.96)
0.1 0.2 0.5 1 2 5 10
Acupressure lower Control higher
53 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Analysis 2.8. Comparison 2 Acupressure versus control, Outcome 8 Length of labour.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 2 Acupressure versus control
Outcome: 8 Length of labour
Study or subgroup Acupressure Control Std. Mean Difference Weight Std. Mean Difference
N Mean(SD) N Mean(SD) IV,Random,95% CI IV,Random,95% CI
1 Placebo control
Kashanian 2010 60 252.37 (108.5) 60 441.38 (155.88) 51.6 % -1.40 [ -1.80, -1.00 ]
Lee 2004 36 138.6 (62) 39 191.2 (83.7) 48.4 % -0.70 [ -1.17, -0.24 ]
Subtotal (95% CI) 96 99 100.0 % -1.06 [ -1.74, -0.38 ]
Heterogeneity: Tau
2
= 0.19; Chi
2
= 4.91, df = 1 (P = 0.03); I
2
=80%
Test for overall effect: Z = 3.05 (P = 0.0023)
-10 -5 0 5 10
Acupressure less Control higher
Analysis 2.9. Comparison 2 Acupressure versus control, Outcome 9 Anxiety.
Review: Acupuncture or acupressure for pain management in labour
Comparison: 2 Acupressure versus control
Outcome: 9 Anxiety
Study or subgroup Acupressure Control Mean Difference Weight Mean Difference
N Mean(SD) N Mean(SD) IV,Fixed,95% CI IV,Fixed,95% CI
1 Placebo control
Lee 2004 36 4.9 (2.3) 39 6.3 (2.6) 100.0 % -1.40 [ -2.51, -0.29 ]
Subtotal (95% CI) 36 39 100.0 % -1.40 [ -2.51, -0.29 ]
Heterogeneity: not applicable
Test for overall effect: Z = 2.47 (P = 0.013)
Test for subgroup differences: Not applicable
-10 -5 0 5 10
Acupressure less Control higher
54 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
A P P E N D I C E S
Appendix 1. Search strategy
Authors wrote and ran the following searches:
a) Cochrane Central Register of Controlled Trials (The Cochrane Library 2010, Issue 4)
#1 (labor)
#2 (childbirth):ti,ab,kw
#3 (labor):ti,ab,kw or (Childbirth):ti,ab,kw or (pain* manag*):ti,ab,kw or (Pain* labo*r):ti,ab,kw or (contraction*):ti,ab,kw in Clinical
Trials
#4 (#1 OR #2 OR #3)
#5 (Acupuncture):ti,ab,kw or (meridian*):ti,ab,kw and (therapy):au
#6 MeSH descriptor Acupuncture explode all trees
#7 MeSH descriptor Acupressure explode all trees
#8 MeSH descriptor Acupressure, this term only
#9 MeSH descriptor Acupuncture, this term only
#10 MeSH descriptor Acupuncture Analgesia, this term only
#11 MeSH descriptor Acupuncture, Ear, this term only
#12 MeSH descriptor Meridians explode all trees
#13 MeSH descriptor Acupuncture Points, this term only
#14 MeSH descriptor Moxibustion, this term only
#15 needling in Clinical Trials
#16 (needling):ti,ab,kw in Clinical Trials
#17 (acu NEXT point*):ti,ab,kw in Clinical Trials
#18 (shu*):ti,ab,kw in Clinical Trials
#19 (acupoint*):ti,ab,kw in Clinical Trials
#20 (shiatsu):ti,ab,kw or (tui na):ti,ab,kw in Clinical Trials
#21 (acupuncture):ti,ab,kw in Clinical Trials
#22 (acupressure):ti,ab,kw in Clinical Trials
#23 (electro NEXT acupuncture):ti,ab,kw in Clinical Trials
#24 (meridian):ti,ab,kw in Clinical Trials
#25(mox*):ti,ab,kw in Clinical Trials
#26 (#5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #
20 OR #21 OR #22 OR #23 OR #24 OR #25)
#27 (#4 AND #26)
b) MEDLINE (1966 to October 2010)
1. exp Labor, Obstetric/ or labo*r.mp.
2. (childbirth or child birth or child-birth).tw.
3. (labour or labor).ab.
4. pain$.mp.
5. pain manag$.mp. or exp Pain/
6. or/1-5
7. exp Acupuncture/
8. exp Acupuncture Analgesia/ or exp Acupuncture Therapy/ or Acupuncture/ or exp Acupuncture Points/ or exp Acupuncture, Ear/
or acupuncture.mp.
9. acupuncture.tw.
10. exp Acupressure/
11. (electroacupuncture or electro acupuncture or electro-acupuncture).tw.
12. meridian$.tw.
13. mox$.tw.
14. needling.tw.
15. (acup-point$ or acu point$).tw.
16. acupoint$.tw.
55 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
17. shu.tw.
18. (shiatsu or tui na).tw.
19. or/7-18
20. 6 and 19
21. randomized controlled trial.pt.
22. controlled clinical trial.pt.
23. (randomized or randomised).ab.
24. placebo.ab.
25. drug therapy.fs.
26. randomly.ab.
27. trial.ab.
28. groups.ab.
29. or/21-28
30. (animals not (humans and animals)).sh.
31. 29 not 30
32. 20 and 31
c) CINAHL (1980 to October 2010)
S29(((MH Acupuncture+) OR acupuncture OR (MH Acupuncture Analgesia) OR (MH Acupuncture Points) OR (MH
Acupuncture, Ear) OR (MH Acupressure) OR (MH Auriculotherapy) OR (MH Electroacupuncture) OR (MH Meridians)
OR (MH Shiatsu)) and (S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26)) and S8)
S28((MH Acupuncture+) OR acupuncture OR (MH Acupuncture Analgesia) OR (MH Acupuncture Points) OR (MH
Acupuncture, Ear) OR (MH Acupressure) OR (MH Auriculotherapy) OR (MH Electroacupuncture) OR (MH Meridians)
OR (MH Shiatsu)) and (S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26))
S27(MH Acupuncture+) OR acupuncture OR (MH Acupuncture Analgesia) OR (MH Acupuncture Points) OR (MH
Acupuncture, Ear) OR (MH Acupressure) OR (MH Auriculotherapy) OR (MH Electroacupuncture) OR (MH Meridians)
OR (MH Shiatsu)
S26 AB Quantitative studies/
S25 AB placebos/
S24 AB placebo$
S23 AB random$ allocation
S22 AB random assignment
S21 AB randomi?ed control$ trial$
S20 AB randomi?ed controlled trial
S19 AB clinical trial*
S18 AB clinical trials
S17 AB shu*
S16 AB acu point or acu-point
S15 AB acupoint*
S14 AB needling
S13 AB mox*
S12 AB meridian
S11 AB electroacupuncture or electro acupuncture or electro-acupuncture
S10 AB acupressure
S9 AB acupuncture
S8(AB ( pain or labo*r pain )) and (S1 or S2 or S3 or S4 or S5 or S6 or S7)
S7 AB pain or labo*r pain
S6 AB pain manag$
S5 AB pain manag$
S4 AB pain$ manag$
S3 AB childbirth or child birth
S2 AB childbirth or AB obstetric$
S1 AB labor or AB labour
56 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
W H A T S N E W
Last assessed as up-to-date: 1 February 2011.
Date Event Description
1 July 2011 Amended We deleted however, there was signicant heterogeneity from the Results section within the Abstract
because, according to Analysis 1.5, assisted vaginal birth, there was no signicant heterogeneity
H I S T O R Y
Review rst published: Issue 7, 2011
C O N T R I B U T I O N S O F A U T H O R S
Caroline Smith and Carmel Collins conceptualised and wrote the protocol, reviewed trials, performed data extraction and jointly wrote
the review and its update. Caroline Smith is the guarantor of the review. Caroline Crowther commented on each draft of the protocol
and review and its update. Kate Levett performed data extraction and commented on the review.
D E C L A R A T I O N S O F I N T E R E S T
None known.
S O U R C E S O F S U P P O R T
Internal sources
The University of Adelaide, Adelaide, Australia.
Child Health Research Institute, Australia.
Child, Youth and Womens Health Services, Adelaide, Australia.
External sources
No sources of support supplied
57 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
D I F F E R E N C E S B E T W E E N P R O T O C O L A N D R E V I E W
This updated review differs from the previously published Cochrane systematic review Complementary and alternative therapies for
pain management in labour (Smith 2006). This review has now been revised to three separate reviews.
N O T E S
This new review is one of three which, collectively, update the previous review on a range of complementary therapies (Smith 2006).
This review includes only trials of acupuncture or acupressure.
I N D E X T E R M S
Medical Subject Headings (MeSH)
Acupressure [
methods]; Acupuncture Therapy [
methods]; Analgesia, Obstetrical [
methods]; Labor Pain [
therapy]; Randomized
Controlled Trials as Topic
MeSH check words
Female; Humans; Pregnancy
58 Acupuncture or acupressure for pain management in labour (Review)
Copyright 2011 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
You might also like
- Living with Hearing Difficulties: The process of enablementFrom EverandLiving with Hearing Difficulties: The process of enablementNo ratings yet
- Acupuncture For Insomnia (Cochrane)Document107 pagesAcupuncture For Insomnia (Cochrane)JonasMarçaloNo ratings yet
- Diclofenac For Acute Pain in Children (Review) - Cochrane 2009Document63 pagesDiclofenac For Acute Pain in Children (Review) - Cochrane 2009Carlos CuetoNo ratings yet
- Intervensi DomainDocument92 pagesIntervensi DomainSylvia DamayantiNo ratings yet
- Journal Slep Dan Massage 3Document100 pagesJournal Slep Dan Massage 3KarmizaNo ratings yet
- Oa KneeDocument146 pagesOa Kneeesta veta mahardikaNo ratings yet
- 2012 Mirror Therapy For Improving Motor Function After StrokeDocument68 pages2012 Mirror Therapy For Improving Motor Function After StrokeMarcelo Ortiz Valenzuela100% (1)
- Relaxation Techniques For Pain Management in Labour PDFDocument53 pagesRelaxation Techniques For Pain Management in Labour PDFNadia Eka PutriNo ratings yet
- Ivig-Cidp (2013)Document51 pagesIvig-Cidp (2013)Nattawat TeerawattanapongNo ratings yet
- Perineal Techniques During The Second Stage of Labour For Reducing Perineal TraumaDocument88 pagesPerineal Techniques During The Second Stage of Labour For Reducing Perineal TraumaJeferson BarbosaNo ratings yet
- Cochrane Database of Systematic ReviewsInterventions For Congenital Talipes EquinovarusDocument65 pagesCochrane Database of Systematic ReviewsInterventions For Congenital Talipes EquinovarusadynataciayadiNo ratings yet
- Statin As Primary Prevention in CVDDocument60 pagesStatin As Primary Prevention in CVDErvan ZuhriNo ratings yet
- Hysteroscopy For Treating Subfertility Associated WithDocument57 pagesHysteroscopy For Treating Subfertility Associated WithAuliana FENo ratings yet
- Page Et Al-2014-The Cochrane LibraryDocument120 pagesPage Et Al-2014-The Cochrane LibraryLuis UretaNo ratings yet
- Stern Et Al-2017-Cochrane Database of Systematic ReviewsDocument63 pagesStern Et Al-2017-Cochrane Database of Systematic ReviewsAgusAchmadSusiloNo ratings yet
- Guidelines Bronquiolite PDFDocument57 pagesGuidelines Bronquiolite PDFAlexandra MatiasNo ratings yet
- Treatment Antiviral. Bell S ParalysisDocument56 pagesTreatment Antiviral. Bell S ParalysisNayrobi GuillénNo ratings yet
- Intervention To Improve Hand Hygiene Compliance in Patient Care (Review)Document106 pagesIntervention To Improve Hand Hygiene Compliance in Patient Care (Review)Riska IndrianiNo ratings yet
- Ultrasound Versus Liver Function Tests For Diagnosis of Common Bile Duct Stones (Review)Document57 pagesUltrasound Versus Liver Function Tests For Diagnosis of Common Bile Duct Stones (Review)FlipNo ratings yet
- CD005288 StandardDocument92 pagesCD005288 StandardGraziele GuimarãesNo ratings yet
- Tens Chronic Pain 2010Document62 pagesTens Chronic Pain 2010nandhini raguNo ratings yet
- Relaxation Techniques For Pain Management in Labor: Cochrane Database of Systematic Reviews (Online) December 2011Document38 pagesRelaxation Techniques For Pain Management in Labor: Cochrane Database of Systematic Reviews (Online) December 2011Safrina Widya HastutiNo ratings yet
- Neuropsychological Rehabilitation Multiple Sclerosis RostiDocument84 pagesNeuropsychological Rehabilitation Multiple Sclerosis Rostisidney drecotteNo ratings yet
- Cipriani Et Al-2013-Cochrane Database of Systematic ReviewsDocument52 pagesCipriani Et Al-2013-Cochrane Database of Systematic ReviewsfiskaderishaNo ratings yet
- Fabbro Et Al-2016-The Cochrane LibraryDocument108 pagesFabbro Et Al-2016-The Cochrane LibraryAnonymous N6OWzvKNo ratings yet
- Honey As A Topical Treatment For Wounds-Jull - Et - Al-2015Document131 pagesHoney As A Topical Treatment For Wounds-Jull - Et - Al-2015amiralbertoNo ratings yet
- Combination Pharmacotherapy For The Treatment of The Tretatment of Neuropatic Pain in Adults Review Cochrane 2017Document59 pagesCombination Pharmacotherapy For The Treatment of The Tretatment of Neuropatic Pain in Adults Review Cochrane 2017Annie MCHNo ratings yet
- Early Intervention (Mobilization or Active Exercise) For Critically Ill Adults in The Intensive Care Unit (Review) - Doiron2018Document60 pagesEarly Intervention (Mobilization or Active Exercise) For Critically Ill Adults in The Intensive Care Unit (Review) - Doiron2018RodrigoSachiFreitasNo ratings yet
- Buch Binder 2003Document48 pagesBuch Binder 2003Azmi FarhadiNo ratings yet
- Magnesium For Skeletal Muscle CrampsDocument54 pagesMagnesium For Skeletal Muscle CrampsM Mohsin ChowdhuryNo ratings yet
- Medical Interventions For Fungal Keratitis (Review)Document54 pagesMedical Interventions For Fungal Keratitis (Review)Matias BossieNo ratings yet
- Burry 2018Document113 pagesBurry 2018Luis CsrNo ratings yet
- Interprofessional Education: Effects On Professional Practice and Healthcare Outcomes (Update) (Review)Document49 pagesInterprofessional Education: Effects On Professional Practice and Healthcare Outcomes (Update) (Review)idscribddotcomNo ratings yet
- Vagus Nerve Stimulation For Partial SeizuresDocument49 pagesVagus Nerve Stimulation For Partial SeizuresRodrigo CesarNo ratings yet
- Diapo 5Document76 pagesDiapo 5Santiagochz Osuna ChairezNo ratings yet
- School-Based Education Programmes For The Prevention of Child Sexual Abuse (Review)Document123 pagesSchool-Based Education Programmes For The Prevention of Child Sexual Abuse (Review)Regina De SouzaNo ratings yet
- Support Surfaces For Treating Pressure UlcersDocument79 pagesSupport Surfaces For Treating Pressure UlcersANÔNIMONo ratings yet
- 2013 A Kley - Creatine For Treating Muscle Disorders.Document58 pages2013 A Kley - Creatine For Treating Muscle Disorders.Luis VargasNo ratings yet
- Zinc For The Common Cold (Review) : Singh M, Das RRDocument61 pagesZinc For The Common Cold (Review) : Singh M, Das RRDavid HermanNo ratings yet
- Panduan PKMIDocument75 pagesPanduan PKMIAndrew TimantaNo ratings yet
- Joyce Et Al. (2010) Flexible Working Conditions and Their Effects On Employee Health PDFDocument91 pagesJoyce Et Al. (2010) Flexible Working Conditions and Their Effects On Employee Health PDFMarcelo Astorga VelosoNo ratings yet
- Singh 2011Document84 pagesSingh 2011Iuliana NitaNo ratings yet
- Greene Et Al 2016Document76 pagesGreene Et Al 2016Valentina Muñoz OyarzúnNo ratings yet
- Chochrane LibraryDocument83 pagesChochrane LibrarynorizaNo ratings yet
- Salina Hipertonica-2013-The Cochrane LibraryDocument50 pagesSalina Hipertonica-2013-The Cochrane LibraryGerardo MansillaNo ratings yet
- Intervention Pityriasis RoseaDocument36 pagesIntervention Pityriasis RoseaNila SariNo ratings yet
- Ostuzzi 2018Document98 pagesOstuzzi 2018Sol ContrerasNo ratings yet
- Probiotics For Preventing Acute Upper Respiratory Tract InfectionsDocument72 pagesProbiotics For Preventing Acute Upper Respiratory Tract InfectionsChawki MokademNo ratings yet
- Bells Palsy Physio PDFDocument71 pagesBells Palsy Physio PDFडा. सत्यदेव त्यागी आर्यNo ratings yet
- Cody 2012Document86 pagesCody 2012karnelNo ratings yet
- Amylase in Drain Fluid For The Diagnosis of Pancreatic Leak inDocument52 pagesAmylase in Drain Fluid For The Diagnosis of Pancreatic Leak inrhiza may tigasNo ratings yet
- Abbass Et Al Cochrane 2014Document87 pagesAbbass Et Al Cochrane 2014Mario ColliNo ratings yet
- Gaskell 2017Document106 pagesGaskell 2017zhuangemrysNo ratings yet
- Acupunture and Related InterventionsDocument69 pagesAcupunture and Related InterventionsfirdaustheshadowNo ratings yet
- Cochrane para Amitriptilina y Dolor NeuropaticoDocument61 pagesCochrane para Amitriptilina y Dolor Neuropaticoyennifer hoyos mendezNo ratings yet
- Cocrane InglesDocument134 pagesCocrane InglesGuiselle PetrovicNo ratings yet
- Ostuzzi Et Al-2015-The Cochrane Library - Sup-2Document63 pagesOstuzzi Et Al-2015-The Cochrane Library - Sup-2Pepe Serrano RodríguezNo ratings yet
- SA Balneo Vs ExoDocument47 pagesSA Balneo Vs ExoCiana DeseigneNo ratings yet
- CD012669 PDFDocument156 pagesCD012669 PDFnoviNo ratings yet
- Barbato Et Al-2018-Cochrane Database of Systematic ReviewsDocument79 pagesBarbato Et Al-2018-Cochrane Database of Systematic ReviewsfiskaderishaNo ratings yet
- Kleiner Lindsay The Ananga Ranga YesDocument8 pagesKleiner Lindsay The Ananga Ranga YesAsh CarterNo ratings yet
- Psychic Ability DevelopingDocument7 pagesPsychic Ability DevelopingSerbaguna MantapNo ratings yet
- AwakPsy Ebook MaggieAndersonDocument64 pagesAwakPsy Ebook MaggieAndersonizzybjNo ratings yet
- Cheryl's Press KitDocument3 pagesCheryl's Press KitSerbaguna MantapNo ratings yet
- Acupuncture or Acupressure For Pain Management in Labour (Review)Document60 pagesAcupuncture or Acupressure For Pain Management in Labour (Review)Serbaguna Mantap100% (1)
- Sautter Engaging The TabooDocument11 pagesSautter Engaging The TabooSerbaguna MantapNo ratings yet
- Chakra TeksDocument4 pagesChakra TeksSerbaguna MantapNo ratings yet
- How To Attract AbundanceDocument118 pagesHow To Attract Abundanceilya18No ratings yet
- So U Think PsychicDocument212 pagesSo U Think PsychicEileen DoverNo ratings yet
- New Testament Intercessory Prayer List: Nternational Ouse of Rayer WWW Ihopkc COMDocument9 pagesNew Testament Intercessory Prayer List: Nternational Ouse of Rayer WWW Ihopkc COMSerbaguna MantapNo ratings yet
- Gematria - Numbers and LettersDocument13 pagesGematria - Numbers and LettersJames Driscoll100% (1)
- MayimDocument52 pagesMayimSerbaguna MantapNo ratings yet
- AbuBereshit MeditationDocument1 pageAbuBereshit MeditationSerbaguna Mantap50% (2)
- Menorat2fixed20122 PDFDocument3 pagesMenorat2fixed20122 PDFsofonias777No ratings yet
- Power WordsDocument5 pagesPower WordsSerbaguna MantapNo ratings yet
- 2014 August Mount Shasta Inner Divinity RetreatDocument2 pages2014 August Mount Shasta Inner Divinity RetreatSerbaguna MantapNo ratings yet
- Experiences in Spiritualism With D D HomeDocument46 pagesExperiences in Spiritualism With D D HomeftldriveNo ratings yet
- Experiences in Spiritualism With D D HomeDocument46 pagesExperiences in Spiritualism With D D HomeftldriveNo ratings yet
- Krav Maga Pressure Points - Military Hand To Hand Combat GuideDocument27 pagesKrav Maga Pressure Points - Military Hand To Hand Combat Guidebrogan98% (135)
- Great-Pole Boxing: The Theory: Attributed To Wang Zongyue (Wang T'sung-Yeuh) (Late 18th Century)Document3 pagesGreat-Pole Boxing: The Theory: Attributed To Wang Zongyue (Wang T'sung-Yeuh) (Late 18th Century)Miguelin666No ratings yet
- 2014 August Mount Shasta Inner Divinity RetreatDocument2 pages2014 August Mount Shasta Inner Divinity RetreatSerbaguna MantapNo ratings yet
- So U Think PsychicDocument212 pagesSo U Think PsychicEileen DoverNo ratings yet
- So U Think PsychicDocument212 pagesSo U Think PsychicEileen DoverNo ratings yet
- Start of The Class: URBAN X ProgrammeDocument1 pageStart of The Class: URBAN X ProgrammeSerbaguna MantapNo ratings yet
- Start of The Class: URBAN X ProgrammeDocument1 pageStart of The Class: URBAN X ProgrammeSerbaguna MantapNo ratings yet
- The Secrets of Telekinesis RevealedDocument36 pagesThe Secrets of Telekinesis RevealedKlemen Rozman100% (1)
- How To Improve The Energy of The BodyDocument201 pagesHow To Improve The Energy of The BodySerbaguna Mantap100% (9)
- Great-Pole Boxing: The Theory: Attributed To Wang Zongyue (Wang T'sung-Yeuh) (Late 18th Century)Document3 pagesGreat-Pole Boxing: The Theory: Attributed To Wang Zongyue (Wang T'sung-Yeuh) (Late 18th Century)Miguelin666No ratings yet
- Week 9Document1 pageWeek 9Serbaguna MantapNo ratings yet
- NCP2 ConstipationDocument1 pageNCP2 ConstipationGrace_CessNo ratings yet
- Themythofmultitasking Rosen PDFDocument6 pagesThemythofmultitasking Rosen PDFyeni marcela montañaNo ratings yet
- MKQ 019Document6 pagesMKQ 019faisaldanyaniNo ratings yet
- Mustard Oil TestingDocument6 pagesMustard Oil TestingMYUTILITY100% (1)
- Substanceabuseand Trauma: Shannon Simmons,, Liza SuárezDocument12 pagesSubstanceabuseand Trauma: Shannon Simmons,, Liza SuárezEma UrzicaNo ratings yet
- Table of Specifications in Health 10Document3 pagesTable of Specifications in Health 10Rowan ZheeNo ratings yet
- Resilience in Nurses - An Integrative ReviewDocument15 pagesResilience in Nurses - An Integrative ReviewBob SmithNo ratings yet
- A Guide To Radio Frequency Hazards With Electric DetonatorsDocument37 pagesA Guide To Radio Frequency Hazards With Electric Detonatorszix013No ratings yet
- Avoiding The Line of Fire: "For Safety's Sake - Do Something"Document1 pageAvoiding The Line of Fire: "For Safety's Sake - Do Something"Sergio SáezNo ratings yet
- Epilepsy & Behavior: Ethan B. Russo, MDDocument6 pagesEpilepsy & Behavior: Ethan B. Russo, MDJose Carlos Solis SuarezNo ratings yet
- Introduction To Water and Sanitation For Health Facility Improvement Tool "Wash Fit"Document73 pagesIntroduction To Water and Sanitation For Health Facility Improvement Tool "Wash Fit"dalford100% (1)
- Anaphy Instuctural DesignDocument6 pagesAnaphy Instuctural DesignDanielleSarahCacheroNo ratings yet
- Phoenix, Arizona: Principles To Guide Zoning For Community Residences For People With DisabilitiesDocument44 pagesPhoenix, Arizona: Principles To Guide Zoning For Community Residences For People With Disabilitiesdan-304518No ratings yet
- 5SDocument5 pages5SKakek SugionoNo ratings yet
- Method StatementDocument20 pagesMethod StatementCharles IkenyeNo ratings yet
- Couple ReportDocument10 pagesCouple ReportTrey TaylorNo ratings yet
- Rational-Emotive Behaviour Therapy (Rebt)Document11 pagesRational-Emotive Behaviour Therapy (Rebt)Sheralena Mohd RasidNo ratings yet
- Arcadia Reptile 2018Document32 pagesArcadia Reptile 2018marianpcbNo ratings yet
- A Study On Nutritional Status of Kharia Tribal Females of Simdega DistrictDocument7 pagesA Study On Nutritional Status of Kharia Tribal Females of Simdega DistrictMaheshPVNo ratings yet
- PA1 CLASS XI P.edDocument2 pagesPA1 CLASS XI P.edJatin GeraNo ratings yet
- Mapil Civil Engineering ConstructionDocument2 pagesMapil Civil Engineering ConstructionakilaNo ratings yet
- Isolation of Nosocomial Multi-Drug Resistant Gram-Negative Bacteria From Some Benghazi HospitalsDocument18 pagesIsolation of Nosocomial Multi-Drug Resistant Gram-Negative Bacteria From Some Benghazi HospitalsInternational Medical Publisher100% (1)
- Effectiveness of An Anterior Mini-Screw in Achieving Incisor IntrusionDocument10 pagesEffectiveness of An Anterior Mini-Screw in Achieving Incisor IntrusionAbdel Hadi KanjNo ratings yet
- Anatomical Foundations of Chinese MedDocument29 pagesAnatomical Foundations of Chinese Medanattā100% (1)
- No.40 Vocabulary & Structures B/ Stocky C/ PretextDocument5 pagesNo.40 Vocabulary & Structures B/ Stocky C/ PretextMai Phương Nguyễn ThịNo ratings yet
- Pathophys BURNDocument2 pagesPathophys BURNpaupaulala83% (6)
- A Brief About Legal Services Authorities Act, 1987Document3 pagesA Brief About Legal Services Authorities Act, 1987MINNU MINHAZNo ratings yet
- ISSLDocument58 pagesISSLsufiNo ratings yet
- Trends in Maternal Mortality 2000 To 2020Document108 pagesTrends in Maternal Mortality 2000 To 2020shouka.inNo ratings yet
- Nursing 2 4yDocument10 pagesNursing 2 4yGCON KURNOOLNo ratings yet