Professional Documents
Culture Documents
Practicum Manual For Student-Teachers
Uploaded by
Dennis Esik Maligaya0 ratings0% found this document useful (0 votes)
28 views6 pagespracticum manual for student-teachers
Original Title
Practicum manual for student-teachers
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentpracticum manual for student-teachers
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
28 views6 pagesPracticum Manual For Student-Teachers
Uploaded by
Dennis Esik Maligayapracticum manual for student-teachers
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
Development and validation of an instrument
to measure the postgraduate clinical learning
and teaching educational environment for
hospital-based junior doctors in the UK
S. ROFF
1
, S. MCALEER
1
& A. SKINNER
2
1
Centre for Medical Education, Dundee University Medical School, UK;
2
Department of
Paediatrics, City Hospital NHS Trust, Birmingham, UK
SUMMARY This paper describes the development and validation
of a 40-item inventory, the Postgraduate Hospital Educational
Environment Measure (PHEEM), by researchers in Scotland and
the West Midlands using a combination of grounded theory and
Delphi process. The instrument has since returned an alpha
reliability >0.91 in two administrations in England and may be a
useful instrument in the quality assurance process for postgraduate
medical education and training.
Background
Genn (2001) and Harden (2001) have pointed to the
potential of the understanding of learning environments
and sub-environments for managing curriculum develop-
ment and change. Stimulated by their suggestions for action
research in their earlier paper (Genn & Harden, 1986), Roff
et al. (1997) developed the 50-item Dundee Ready Education
Environment Measure with a panel of nearly 100 medical
educators and 1000 students to measure and diagnose
undergraduate educational climates in the health professions.
This instrument has been translated into Spanish,
Portuguese, Arabic, Swedish, Malay and Thai and used in
several settings including the Middle East, Thailand
(Primparyon et al., 2000), Nepal and Nigeria (Roff et al.,
2001) and the West Indies (Bassaw et al., 2003). It is
currently being used in the UK, Canada, Ireland, Thailand,
China, Indonesia, Malaysia, Norway, Sweden, Brazil, the
West Indies and the Yemen.
A similar methodology has been utilized to develop and
validate an inventory to measure the postgraduate clinical
teaching and learning environment for hospital-based junior
doctors. A 40-item inventory was developed.
Methods
A form of grounded theory was used involving focus groups,
nominal groups and a Delphi panel drawn from the target
populations in two phases.
Phase 1
In the first stage of the process, a group of 12 Scottish
Postgraduate Deans, Postgraduate Educational Supervisors,
Educational Advisors and PRHOs met in January 2000 to
agree an initial list of possible items for inclusion in the
inventory based on a literature review (conducted by
McAleer and Roff) of articles retrieved from MEDLINE
and mission statements such as the GMCs The New Doctor,
together with their own observations of significant events/
critical incidents in PRHO training. The literature review had
generated 180 items which the stakeholders reduced to 150
items by eliminating repetitive material and consolidating
some items. These were critiqued by colleagues in the
Educational Development Unit of the Scottish Council for
Postgraduate Medical and Dental Education and the Centre
for Medical Education at the University of Dundee and on
the basis of their feedback concerning repetition and clarity
the inventory was further reduced to 132 items.
In order to validate and prioritize the 132 items into a
more manageable inventory, a random sample of 10% of
the current PRHOs in post in Scotland was sought. Since
direct access to PRHOs in post is difficult due to the
transience of their posts, they were contacted via their
Educational Supervisors. Two copies of the 132-item
preliminary inventory were mailed to the 175 Educational
Supervisors who were each asked to distribute them to one
or two PRHOs who would then return them directly to the
researchers in a return paid envelope which was coded for
the educational centre (hospital where the PRHO was in
post) but were otherwise anonymous. Respondents were
asked to rate the items on a Likert-type scale of 0 (not at all
important) to 4 (highly important) according to how impor-
tant they felt each item was in creating a good learning
environment for PRHOs. One hundred and seventeen
responses were returned which is 17% of the estimated 680
PRHOs in post at the time. Eight of these responses were
returned late, after the analysis had been undertaken.
Responses were received from 88 educational centres
including the four major areas of Glasgow, Edinburgh,
Dundee and Aberdeen as well as smaller centres such as
Oban, Ayr, Inverness and Kirkcaldy. This meant that 50% of
the Educational Supervisors had successfully distributed the
questionnaire to at least one trainee. Several Educational
Supervisors indicated that they did not have PRHOs in this
rotation and returned the questionnaires.
Correspondence: Sue Roff, Centre for Medical Education, Dundee University
Medical School, 484 Perth Road, Dundee DD2 1LR, UK. Email: s.l.roff@
dundee.ac.uk
Medical Teacher, Vol. 27, No. 4, 2005, pp. 326331
326 ISSN 0142159X print/ISSN 1466187X online/00/000326-6 2005 Taylor & Francis Group Ltd
DOI: 10.1080/01421590500150874
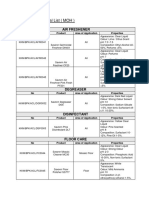
Table 1. The PHEEMitems grouped by sub-scale (negative items in italics).
I. Perceptions of role autonomy:
1 I have a contract of employment that provides information about hours of work
4 I had an informative induction programme
5 I have the appropriate level of responsibility in this post
8 I have to perform inappropriate tasks
9 There is an informative Junior Doctors Handbook
11 I am bleeped inappropriately
14 There are clear clinical protocols in this post
17 My hours conform to the New Deal
18 I have the opportunity to provide continuity of care
29 I feel part of a team working here
30 I have opportunities to acquire the appropriate practical procedures for my grade
32 My workload in this job is fine
34 The training in this post makes me feel ready to be an SpR/Consultant
40 My clinical teachers promote an atmosphere of mutual respect
14 items/max score 56 for this sub-scale
II. Perceptions of teaching:
2 My clinical teachers set clear expectations
3 I have protected educational time in this post
6 I have good clinical supervision at all times
10 My clinical teachers have good communication skills
12 I am able to participate actively in educational events
15 My clinical teachers are enthusiastic
21 There is access to an educational programme relevant to my needs
22 I get regular feedback from seniors
23 My clinical teachers are well organized
27 I have enough clinical learning opportunities for my needs
28 My clinical teachers have good teaching skills
31 My clinical teachers are accessible
33 Senior staff utilize learning opportunities effectively
37 My clinical teachers encourage me to be an independent learner
39 The clinical teachers provide me with good feedback on my strengths and weaknesses
15 items/max score 60 for this sub-scale
III. Perceptions of social support:
7 There is racism in this post
13 There is sex discrimination in this post
16 I have good collaboration with other doctors in my grade
19 I have suitable access to careers advice
20 This hospital has good quality accommodation for junior doctors, especially when on call
24 I feel physically safe within the hospital environment
25 There is a no-blame culture in this post
26 There are adequate catering facilities when I am on call
35 My clinical teachers have good mentoring skills
36 I get a lot of enjoyment out of my present job
38 There are good counselling opportunities for junior doctors who fail to complete their training satisfactorily
11 items/max score 44 for this sub-scale
Interpreting the sub-scales:
I. Perceptions of role autonomy:
014 very poor
1528 a negative view of ones role
2942 a more positive perception of ones job
4356 excellent perception of ones job
II. Perceptions of teaching:
015 very poor quality
1630 in need of some retraining
3145 moving in the right direction
4660 model teachers
(continued )
The postgraduate clinical learning and teaching educational environment
327
One hundred and nine responses were fully completed
and returned in a timely manner. Fifty-eight (53%) were
from males and 51 (47%) were from females. Respondents
were asked to rate the 132 items in terms of how they
perceived the importance for the learning environment of
PRHOs. On a score of 04, 17 items were rated 3.5; 69
were rated 3.00 but 3.49 and the remaining 46 were rated
3.00. Several of the highest ranked items came from the end
of the 132-item list, suggesting that the length of the ques-
tionnaire was not a problem. Eight items received statistically
significant ratings from the males and females, but these
differences did not affect their broad categorization 3.00/
3.00 in the total rank order list. The reliability was high
with an alpha of 0.93.
The top ranking 90 items were retained for the second
version of the inventory.
Phase 2
A focus group (n 10) consisting of a consultant paedi-
atrician/assessor for the Royal College of Paediatrics and
Child Health, five Senior House Officers and four Specialist
Registrars in the Department of Paediatrics at a Birmingham
hospital was convened to review the 90 item inventory.
They were asked to rate the most relevant items in
their perception of a good clinical teaching and learning
environment for hospital-based junior doctors. Items
which three or more members of the focus group considered
least relevant were eliminated from the inventory. This
exercise in checking face validity among the stakeholders
reduced the inventory to 40 items, four of which (nos. 7, 8,
11, 13) are negative statements which have to be reversed for
scoring.
A nominal group of three of the researchers then identified
three sub-scalesPerceptions of role autonomy, Perceptions
of teaching and Perceptions of social support.
Results
The final instrument produced, the Postgraduate Hospital
Educational Environment Measure (PHEEM), is included
as Appendix 2. The items grouped by sub-scale are given
in Table 1. These were grouped into three sections, as
indicated below, together with the maximum score for each
sub-scale:
Perceptions of role autonomy: 14 4 56 max;
Perceptions of teaching: 15 4 60 max; and
Perceptions of social support: 11 4 44 max.
This is made up of the number of items in the sub-scale times
the maximum mark on a Likert scale of 04. The possible
maximum score is 160 and the minimum score is 0.
Information about administering PHEEM and scor-
ing and interpreting the students responses is given in
Appendix 1.
Discussion
The two-phase process of grounded theory research involv-
ing stakeholders from the relevant junior doctor grades
together with educational advisors and senior managers in
Scotland and Birmingham generated a 40-item inventory
with three sub-scales with apparent high face validity both
for the UK and in relation to other studies (Rotem et al.,
1995; Mitchell et al., 1999; Pololi & Price, 2000; Fernald
et al., 2001; Dolmans et al., 2004). Skinner has since
administered this 40-item inventory to 68 Senior House
Officers and 32 Specialist Registrars in Birmingham teach-
ing hospitals from a range of specialties and these results
are reported separately. The Postgraduate Hospital Edu-
cation Environment Measure (PHEEM) had an alpha
reliability of 0.91 in that administration. Clapham et al.
(2005) administered the PHEEM to 134 trainees at
nine Intensive Care Units in England and Scotland. The
Cronbachs alpha for this administration was 0.92 and no
rogue questions were detected by the alpha if item deleted
function in SPSS.
It is hoped that other researchers and managers of
junior doctor teaching and learning in the UK, and perhaps
beyond, will find it a useful quality assessment tool for
both single-use and longitudinal studies of hospital-
based clinical teaching and learning for junior doctors.
Newbury-Birch & Kamali (2001), for instance, have con-
cluded that the level of supervision provided by superiors,
flexibility and freedom in the job and level of participa-
tion in important decision-making are correlated with
levels of stress and anxiety in pre-registration house officers
in the UK.
Acknowledgements
The authors are grateful to Professor Norman Mackay,
Professor Graham Buckley and Dr Gellisse Bagnall for
support for data collection of this project and to Heather
Sutherland, Lynn Bell and Dr Danai Wangsaturaka for help
with data analysis. Funding for Phase 1 was provided by the
Table 1. Continued.
III. Perceptions of social support:
011 non-existent
1222 not a pleasant place
2333 more pros than cons
3444 a good supportive environment
Note: The PHEEM can also be used to pinpoint more specific strengths and weaknesses within the educational climate.
To do this one needs to look at the responses to individual items. Items that have a mean score of 3.5 or over are real
positive points. Any item with a mean of 2 or less should be examined more closely as they indicate problem areas. Items with a
mean between 2 and 3 are aspects of the climate that could be enhanced.
S. Roff et al.
328
Scottish Council for Postgraduate Medical and Dental
Education.
Notes on contributors
SUE ROFF teaches in the Centre for Medical Education, Dundee
University Medical School, UK. She co-developed the Dundee Ready
Education Environment Measure. She is a lay member of the General
Medical Council Fitness to Practice Committee, the Unrelated Live
Transplants Regulatory Authority and the Postgraduate Medical
Education and Training Board.
SEAN MCALEER is Senior Lecturer in the Centre for Medical Education,
University of Dundee. He teaches on the Certificate, Diploma and
Masters Programme in Medical Education. His research interests are in
the areas of assessment, educational climate and learning styles.
ALYSON SKINNER is a Consultant Paediatrician with a special interest in
medical education at undergraduate and postgraduate level.
References
BASSAW, B., ROFF, S., MCALEER, S., ROOPNARINESIGN, S., DE LISLE, J.,
TEELUCKSINGH, S. & GOPAUL, S. (2003) Students perspectives of the
educational environment, Faculty of Medical Sciences, Trinidad,
Medical Teacher, 25, pp. 522526.
CLAPHAM, M., WALL, D. & BATCHELOR, A. (2005) Measuring
the educational climate in intensive care medicine, submitted for
publication.
DOLMANS, D.H.J.M., WOLFHAGEN, H.A.P., GERVER, W.J., DE GRAVE, W.
& SCHERPBIER, A.J.J.A. (2004) Providing physicians with feedback
on how they supervise students during patient contacts, Medical
Teacher, 25, pp. 409414.
FERNALD, D.H., STAUDENMAIER, A.C., TRESSLER, C.J., MAIN, D.S.,
OBRIEN-GONZALES, A. & BARLEY, G.E. (2001) Student perspectives
on primary care preceptorships: enhancing the medical student
preceptorship learning environment, Teaching and Learning in
Medicine, 13, pp. 1320.
GENN, J.M. (2001) AMEE medical education guide No.23 (Part 1):
curriculum, environment, climate, quality and change in medical
educationa unifying perspective, Medical Teacher, 23, pp. 337344.
GENN, J.M. & HARDEN, R.M. (1986) What is medical education here
really like? Suggestions for action research studies of climates of medical
education environments, Medical Teacher, 8, pp. 111124.
HARDEN, R.M. (2001) The learning environment and the curriculum,
Medical Teacher, 23, pp. 335336.
MITCHELL, R., JACK, B. & MCQUADE, W. (1999) Mapping the cognitive
environment of a residency: an exploratory study of a maternal
and child health rotation, Teaching and Learning in Medicine, 11,
pp. 611.
NEWBURY-BIRCH, D. & KAMALI, F. (2001) Psychological stress,
anxiety, depression, job satisfaction, and personality characteristics
in preregistration house officers, Postgraduate Medicine Journal, 77,
pp. 109111.
POLOLI, L. & PRICE, J. (2000) Validation and use of an instrument to
measure the learning environment as perceived by medical students.
Teaching and Learning in Medicine, 12, pp. 201207.
PRIMPARYON, P., ROFF, S., MCALEER, S., POONCHAI, B. & PEMBA, S.
(2000) Educational environment, student approaches to learning
and academic achievement in a Thai nursing school, Medical Teacher,
22, pp. 359365.
ROFF, S., MCALEER, S., HARDEN, R.M., AL-QAHTANI, M., AHMED, A.U.,
DEZA, H., GROENEN, G. & PRIMPARYON, P. (1997) Development
and validation of the Dundee Ready Education Environment
Measure (DREEM), Medical Teacher, 19, pp. 295299.
ROFF, S., MCALEER, S., IFERE, O.S. & BHATTACHARYA, S. (2001) A global
diagnostic tool for measuring educational environment: comparing
Nigeria and Nepal, Medical Teacher, 23, pp. 378382.
ROTEM, A., GOODWIN, P. & DU, J. (1995) Learning in hospital settings.
Teaching and Learning in Medicine, 7, pp. 211217.
Appendix 1: Scoring the Postgraduate Hospital
Educational Environment Measure (PHEEM)
The PHEEM contains 40 statements covering a range of
topics directly relevant to the educational climate of Senior
House Officers (SHOs) and Specialist Registrars (SpRs)
(Appendix 1). The inventory can be administered by postal
or electronic survey or face-to-face. Respondents are asked to
read each statement carefully and to respond using a 5-point
Likert scale ranging from strongly agree to strongly
disagree. It is important that each doctor applies the items
to their own current learning situation and respond to all 40.
Items should be scored: 4 for Strongly Agree (SA), 3
for Agree (A), 2 for Uncertain (U), 1 for Disagree (D) and 0
for Strongly Disagree (SD). However, four of the 40 items
(Numbers 7, 8, 11 and 13) are negative statements
and should be scored: 0 for SA, 1 for A, 2 for U, 3 for D
and 4 for SD.
The 40-item PHEEM has a maximum score of 160
indicating the ideal educational environment as perceived
by the SHO/SpR. A score of 0 is the minimum and would
be a very worrying result for any medical educator.
The following is an approximate guide to interpreting the
overall score:
040 very poor,
4180 plenty of problems,
81120
more positive than negative
but room for improvement, and
121160 excellent.
Interpret a score of 80 as an environment which is viewed
with considerable ambivalence by the SHOs/SpRs and as
such needs to be carefully reviewed.
As well as the total PHEEM score there are three sub-
scales: Perception of role autonomy; Perceptions of teaching;
and Perceptions of social support. Table 1 shows the items
within each sub-scale (negative items are italicized).
The postgraduate clinical learning and teaching educational environment
329
Appendix 2: Postgraduate Hospital Educational Environment Measure
S. Roff et al.
330
The postgraduate clinical learning and teaching educational environment
331
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Uptime Elements Passport: GineerDocument148 pagesUptime Elements Passport: GineerBrian Careel94% (16)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- ALCUCOA StandardsDocument21 pagesALCUCOA StandardsDennis Esik Maligaya100% (6)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Sample CH 4 For Experimental ResearchDocument42 pagesSample CH 4 For Experimental ResearchDennis Esik MaligayaNo ratings yet
- AREA V Entrepreneurship and EmployabilityDocument15 pagesAREA V Entrepreneurship and EmployabilityDennis Esik MaligayaNo ratings yet
- Service and Maintenance Manual AFPX 513 PDFDocument146 pagesService and Maintenance Manual AFPX 513 PDFManuel Amado Montoya AgudeloNo ratings yet
- Role of SupervisorDocument29 pagesRole of SupervisorDennis Esik MaligayaNo ratings yet
- Summary of RA 6713Document25 pagesSummary of RA 6713Dennis Esik MaligayaNo ratings yet
- A. Greenspan C. Panaciio D. Hesse 2.: Servant Leadership QuizDocument1 pageA. Greenspan C. Panaciio D. Hesse 2.: Servant Leadership QuizDennis Esik MaligayaNo ratings yet
- Given The Table Below, Fill Up The Columns Labeled Proportion and Percentage. ADocument9 pagesGiven The Table Below, Fill Up The Columns Labeled Proportion and Percentage. ADennis Esik MaligayaNo ratings yet
- Statistics ExerciseDocument13 pagesStatistics ExerciseDennis Esik MaligayaNo ratings yet
- Financial Management SLCDocument56 pagesFinancial Management SLCDennis Esik MaligayaNo ratings yet
- Nature and Importance of Leadership, Traits and Characteristics of A LeaderDocument18 pagesNature and Importance of Leadership, Traits and Characteristics of A LeaderDennis Esik MaligayaNo ratings yet
- Power and Leadership JLCDocument21 pagesPower and Leadership JLCDennis Esik MaligayaNo ratings yet
- Supervisory Development: by Dr. Dennis E. MaligayaDocument19 pagesSupervisory Development: by Dr. Dennis E. MaligayaDennis Esik MaligayaNo ratings yet
- Logistics Supervision (Ps SLC) : Pssupt. Jesus B. Arceo (Ret) Ed.D., Ph. D. LecturerDocument83 pagesLogistics Supervision (Ps SLC) : Pssupt. Jesus B. Arceo (Ret) Ed.D., Ph. D. LecturerDennis Esik MaligayaNo ratings yet
- Records Management: (For PS SLC)Document59 pagesRecords Management: (For PS SLC)Dennis Esik MaligayaNo ratings yet
- Management Process and EffectivenessDocument12 pagesManagement Process and EffectivenessDennis Esik MaligayaNo ratings yet
- Financial ManagementDocument40 pagesFinancial ManagementDennis Esik MaligayaNo ratings yet
- Govph: Duterte Orders Adoption of Cash Budgeting SystemDocument3 pagesGovph: Duterte Orders Adoption of Cash Budgeting SystemDennis Esik MaligayaNo ratings yet
- Salesmanship: A Form of Leadership: Dr. Dennis E. MaligayaDocument22 pagesSalesmanship: A Form of Leadership: Dr. Dennis E. MaligayaDennis Esik MaligayaNo ratings yet
- Power and Leadership and Leadership Actions TestDocument3 pagesPower and Leadership and Leadership Actions TestDennis Esik MaligayaNo ratings yet
- Leadership Actions: Dr. Dennis E. Maligaya V VN - 9Mu22Ius&Ab - Channel Bluet AlkDocument6 pagesLeadership Actions: Dr. Dennis E. Maligaya V VN - 9Mu22Ius&Ab - Channel Bluet AlkDennis Esik MaligayaNo ratings yet
- Area II FacultyDocument35 pagesArea II FacultyDennis Esik MaligayaNo ratings yet
- Executive Summary 3 Sectors OnlyDocument4 pagesExecutive Summary 3 Sectors OnlyDennis Esik MaligayaNo ratings yet
- Batch 1 ProgrammeDocument15 pagesBatch 1 ProgrammeDennis Esik MaligayaNo ratings yet
- Accounting Presentation COUNTPADocument118 pagesAccounting Presentation COUNTPADennis Esik MaligayaNo ratings yet
- Financial Literacy: Dr. Dennis E. MaligayaDocument65 pagesFinancial Literacy: Dr. Dennis E. MaligayaDennis Esik MaligayaNo ratings yet
- 2023-Tutorial 02Document6 pages2023-Tutorial 02chyhyhyNo ratings yet
- Progressivism Sweeps The NationDocument4 pagesProgressivism Sweeps The NationZach WedelNo ratings yet
- 28Document12 pages28physicsdocsNo ratings yet
- Contents Serbo-Croatian GrammarDocument2 pagesContents Serbo-Croatian GrammarLeo VasilaNo ratings yet
- Brochure - Digital Banking - New DelhiDocument4 pagesBrochure - Digital Banking - New Delhiankitgarg13No ratings yet
- Exercise No.2Document4 pagesExercise No.2Jeane Mae BooNo ratings yet
- 1.quetta Master Plan RFP Draft1Document99 pages1.quetta Master Plan RFP Draft1Munir HussainNo ratings yet
- Yukot,+houkelin 2505 11892735 Final+Paper+Group+41Document17 pagesYukot,+houkelin 2505 11892735 Final+Paper+Group+410191720003 ELIAS ANTONIO BELLO LEON ESTUDIANTE ACTIVONo ratings yet
- Chapter 4 - Risk Assessment ProceduresDocument40 pagesChapter 4 - Risk Assessment ProceduresTeltel BillenaNo ratings yet
- Robot MecanumDocument4 pagesRobot MecanumalienkanibalNo ratings yet
- Annexure 8: Medical Certificate (To Be Issued by A Registered Medical Practitioner) General ExpectationsDocument1 pageAnnexure 8: Medical Certificate (To Be Issued by A Registered Medical Practitioner) General ExpectationsMannepalli RamakrishnaNo ratings yet
- Daud Kamal and Taufiq Rafaqat PoemsDocument9 pagesDaud Kamal and Taufiq Rafaqat PoemsFatima Ismaeel33% (3)
- Win Tensor-UserGuide Optimization FunctionsDocument11 pagesWin Tensor-UserGuide Optimization FunctionsadetriyunitaNo ratings yet
- Simple Future Tense & Future Continuous TenseDocument2 pagesSimple Future Tense & Future Continuous TenseFarris Ab RashidNo ratings yet
- Paediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva SusantiDocument6 pagesPaediatrica Indonesiana: Sumadiono, Cahya Dewi Satria, Nurul Mardhiah, Grace Iva SusantiharnizaNo ratings yet
- 2009 Annual Report - NSCBDocument54 pages2009 Annual Report - NSCBgracegganaNo ratings yet
- Need You Now Lyrics: Charles Scott, HillaryDocument3 pagesNeed You Now Lyrics: Charles Scott, HillaryAl UsadNo ratings yet
- Applied Nutrition: Nutritional Consideration in The Prevention and Management of Renal Disease - VIIDocument28 pagesApplied Nutrition: Nutritional Consideration in The Prevention and Management of Renal Disease - VIIHira KhanNo ratings yet
- KAHOOT - Assignment 4.1 Lesson PlanDocument3 pagesKAHOOT - Assignment 4.1 Lesson PlanJan ZimmermannNo ratings yet
- ESU Mauritius Newsletter Dec 2014Document8 pagesESU Mauritius Newsletter Dec 2014Ashesh RamjeeawonNo ratings yet
- Approved Chemical ListDocument2 pagesApproved Chemical ListSyed Mansur Alyahya100% (1)
- Viva QuestionsDocument3 pagesViva QuestionssanjayshekarncNo ratings yet
- ACCA Advanced Corporate Reporting 2005Document763 pagesACCA Advanced Corporate Reporting 2005Platonic100% (2)
- Prepositions French Worksheet For PracticeDocument37 pagesPrepositions French Worksheet For Practiceangelamonteiro100% (1)
- What Is Folate WPS OfficeDocument4 pagesWhat Is Folate WPS OfficeMerly Grael LigligenNo ratings yet
- Dispersion Compensation FibreDocument16 pagesDispersion Compensation FibreGyana Ranjan MatiNo ratings yet
- Sodium Borate: What Is Boron?Document2 pagesSodium Borate: What Is Boron?Gary WhiteNo ratings yet
- Public International Law Green Notes 2015Document34 pagesPublic International Law Green Notes 2015KrisLarr100% (1)