Professional Documents
Culture Documents
Eyelidreconstruction 130801074705 Phpapp02
Uploaded by
Otávio AragãoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Eyelidreconstruction 130801074705 Phpapp02
Uploaded by
Otávio AragãoCopyright:
Available Formats
www.PRSJournal.
com 288e
R
econstruction of the eyelids remains one of
the most challenging areas in reconstruc-
tive plastic surgery. Perhaps no other area
of the human body provides such a delicate inter-
play among anatomy, aesthetics, and function.
1
In
order to protect the underlying globe and vision,
the eyelids require restoration of both function
and appearance following eyelid repair.
When presented with an eyelid defect, the
surgeon should analyze the missing lamellar com-
ponents and whether canthal support is com-
promised. Special attention should be paid to
the integrity of the lacrimal apparatus when the
resection involves the medial canthal region. The
reconstructive plan will be determined mainly by
the size of the defect and the status of the sur-
rounding periorbital tissue, particularly the oppos-
ing lid if eyelid sharing is deemed necessary. Our
reconstructive strategy favors a progression from
direct closure, when possible, to using local aps
in combination with grafts for bilamellar recon-
struction, to lid-sharing procedures. A single-stage
reconstruction should be the goal without com-
promising the aesthetic and functional results.
This article provides a comprehensive review of
eyelid anatomy and various reconstructive tech-
niques in order to provide the reader with a vari-
ety of options.
SURGICAL ANATOMY OF THE EYELID
Both the upper and lower eyelids are bilamel-
lar structures, consisting of the anterior and poste-
rior lamellae.
2
The anterior lamella consists of skin
and the underlying orbicularis oculi muscle. The
eyelid skin is the thinnest in the body and transi-
tions into a thicker eyebrow and cheek skin in the
upper and lower eyelids, respectively. The orbicu-
laris oculi muscle is loosely adherent to the skin and
is divided into pretarsal, preseptal, and orbital seg-
ments.
3
Functionally, the medial inner canthal orbi-
cularis, which is innervated by the buccal branch of
the facial nerve, contributes to blinking, lower lid
tone, and the pumping mechanism for the lacrimal
apparatus. The extracanthal orbicularis, which is
innervated by the zygomatic branches of the facial
nerve, is responsible for eyelid closure, voluntary
squinting, and animation.
4
The pretarsal orbicularis
Disclosure: Drs. Alghoul and McClellan have no
commercial associations, nancial interests, or con-
icts of interest. Dr. Pacella is on the speakers bu-
reau for Lifecell Corporation. Dr. Codner receives -
nances for research and consulting from Mentor and
Syneron corporations and receives royalties for books
published by Quality Medical Publishing and Else-
vier. All conicts have been reviewed and managed
by accreditation volunteers.
Copyright 2013 by the American Society of Plastic Surgeons
DOI: 10.1097/PRS.0b013e3182958e6b
Mohammed Alghoul, M.D.
Salvatore J. Pacella, M.D.,
M.B.A.
W. Thomas McClellan, M.D.
Mark A. Codner, M.D.
Atlanta, Ga.; La Jolla, Calif.; and
Morgantown, W.Va.
Learning Objectives: After reading this article, the participant should be able
to: 1. Demonstrate an anatomic approach to eyelid reconstruction. 2. Man-
age common and complex eyelid defects by utilizing a reconstructive strategy
outlined in the article.
Summary: Reconstruction of the eyelids after excision of skin cancer can be
challenging. Knowledge of surgical eyelid anatomy and appropriate preopera-
tive planning are critical in order to perform eyelid reconstruction and mini-
mize complications and the need for reoperation. The fundamental principle
for full-thickness eyelid reconstruction is based on reconstructing the subunits
of the eyelid, including the anterior and posterior lamellae as well as the tar-
soligamentous sling. (Plast. Reconstr. Surg. 132: 288e, 2013.)
From private practice; the Division of Plastic and Recon-
structive Surgery, Scripps Clinic and Research Institute; the
Division of Plastic Surgery, West Virginia University; and
Emory University.
Received for publication May 16, 2012; accepted May 23,
2012.
Eyelid Reconstruction
Related Video content is available for this ar-
ticle. The videos can be found under the Re-
lated Videos section of the full-text article, or,
for Ovid users, using the URL citations pub-
lished in the article.
CME
Volume 132, Number 2 Eyelid Reconstruction
289e
muscle is densely xed to the anterior surface of the
tarsus in both the upper and lower eyelids.
The tarsal plate and conjunctiva form the pos-
terior lamella. The tarsal plate is a unique compo-
nent of the eyelid that provides structural support
and should be replaced during reconstruction. It
measures 1 mm in thickness and 25 mm horizon-
tally by approximately 7 to 10 mm vertically in the
upper eyelid and 3.8 mm in the lower eyelid.
5
The
lower lid inserts medially and laterally to the canthi,
creating the tarsoligamentous sling. In the authors
opinion, the tarsoligamentous sling is one of the
most critical structures to reconstruct, representing
the support structure of the lower eyelid (Fig. 1).
The posterior reection of the lateral canthal liga-
ment inserts on Whitnalls tubercle, which is found
posterior to the lateral orbital rim.
6
This posterior
vector allows the eyelid to follow the convex curve
of the globe. Disruption of the lateral lid and globe
interface can lead to widening of the lateral scleral
triangle, reactive conjunctival irritation, and lid
malposition. The medial canthal ligament attaches
to the anterior and posterior lacrimal crest. Disrup-
tion of its attachments can lead to medial ectro-
pion, epiphora, or telecanthus.
7
The conjunctiva is
composed of nonkeratinizing, stratied squamous
epithelium and forms the posterior-most layer of
the eyelid.
3
The upper and lower eyelid retractor
muscles are located immediately anterior to the
conjunctiva. Of importance in upper eyelid recon-
struction, the levator aponeurosis inserts on the
anterior superior surface of the upper eyelid tarsus
and sends bers through the preseptal orbicularis
to insert onto the dermis and form the upper eye-
lid crease, 8 to 9 mm from the margin.
3,5
The ophthalmic artery provides the majority
of blood supply to the upper and lower eyelids,
with contribution from the external carotid artery.
Distal branches of the medial and lateral palpe-
bral arteries (the latter are branches of the lac-
rimal artery) coalesce to form the tarsal arcades.
The upper lid has two arterial arcades; the mar-
ginal arcade is located on the anterior tarsal sur-
face 2 to 3 mm from the eyelid margin, while the
peripheral arcade is on the upper border of the
tarsus between Muellers muscle and the levator
aponeurosis.
3,5
Inferiorly, the marginal arcade
(also called the inferior arcade) is located 3.8 mm
inferior to the lower eyelid margin anterior to the
tarsus. The lower eyelid does not have a periph-
eral arcade
3
(Fig. 2). The excretory component of
the lacrimal system is located in the medial can-
thal region. The puncta are the openings of the
lacrimal drainage system and are located 6 mm
from the inner canthus on the upper and lower
eyelids. Tears pass through the puncta and drain
into the vertically oriented ampulla, to the upper
and lower canaliculi (oriented horizontally). Both
canaliculi extend nasally and join to form a com-
mon canaliculus in more than 90 percent of peo-
ple, which connects with the lacrimal sac located
in the lacrimal fossa. The lacrimal sac empties
into the nasolacrimal duct, which opens endona-
sally underneath the inferior turbinate
8
(Fig. 3).
PHYSICAL EXAMINATION AND
SURGICAL PLANNING
A thorough preoperative history and physi-
cal examination are critical to a successful
Fig. 1. The tarsoligamentous sling. Reprinted with permission from McCord CD Jr, Codner MA.
Eyelid & Periorbital Surgery. St. Louis: Quality Medical Publishing; 2008.
290e
Plastic and Reconstructive Surgery August 2013
reconstructive outcome. Preoperative history
should include a discussion of any ophthalmic
medication, visual acuity, dry eyes, Bells palsy,
thyroid eye disease, and other ocular pathology.
History of prior facial radiation and prior peri-
orbital surgery should be obtained. A margin-
controlled excision should be the goal to ensure
adequate excision prior to a complex reconstruc-
tion.
9
Analysis of the defect should address the
bilamellar structure of the eyelid, the tarsoliga-
mentous sling, and the lacrimal drainage system.
The surrounding periorbital tissue should be
evaluated for vascularity, scarring, radiation dam-
age, severe actinic damage, and overall laxity.
Traumatic defects must be carefully assessed
for peripheral zone of injury. Lower eyelid avul-
sions can often create axial stretch injury on
the canalicular mechanism, making intubation
or cannulation extremely challenging. These
injuries often require secondary lacrimal recon-
struction. The size of the defect is estimated by
gently approximating the edges with two forceps
(Fig. 4). Full-thickness lower eyelid defects com-
promising both lamellae can be categorized by
the percentage of lid length affected. Although
commonly published categories of eyelid defects
range from less than 25 percent, 25 to 50 per-
cent, and greater than 50 percent of the lid,
10
this
should be determined on individualized bases
before a reconstructive technique is selected.
Fig. 2. Arterial anatomy of the eyelid and periorbital area. Reprinted with permission from
McCord CD Jr, Codner MA. Eyelid & Periorbital Surgery. St. Louis: Quality Medical Publishing; 2008.
Fig. 3. Anatomy of the lacrimal apparatus. Reprinted with per-
mission from McCord CD Jr, Codner MA. Eyelid & Periorbital Sur-
gery. St. Louis: Quality Medical Publishing; 2008.
Fig. 4. Eyelid wound edges are gently approximated with for-
ceps to accurately estimate the size of the defect.
Volume 132, Number 2 Eyelid Reconstruction
291e
GRAFTS IN EYELID RECONSTRUCTION
As a basic principle in plastic surgery, grafts
should be used when there is an adequate vas-
cular bed to enhance their survival. Therefore,
combining a nonvascularized graft for one
lamella with a vascularized ap for the other
should be the rule. Both bilamellar reconstruc-
tions can be done with grafts if orbicularis mobili-
zation between the grafted areas (sandwich ap)
can be achieved.
11
The orbicularis muscle has an
excellent blood supply and enhances the mobil-
ity of the reconstructed lid.
12,13
Anterior lamellar
defects can be reconstructed with a full-thickness
skin graft.
14
Ideal donor sites include excess
upper and lower eyelid skin and posterior auricu-
lar, preauricular, or supraclavicular skin.
11,15
Split-
thickness skin grafts should not be used except in
situations of extensive burns when the donor site
is limited. Tarsoconjunctival grafts are an excel-
lent choice for posterior lamellar reconstruction,
since they possess the features of a normal eyelid
(Therapeutic: Level III Evidence).
1620
They are
harvested from the upper eyelid, leaving at least
3 to 4 mm of inferior tarsus to avoid upper lid
deformity. The donor site heals spontaneously
by secondary intention. Excellent results have
been reported using tarsoconjunctival grafts for
repairing defects of up to 75 percent of the eyelid
length (Therapeutic: Level III Evidence).
20
Over-
sizing the graft should be avoided to prevent lax-
ity, especially in lower lid reconstruction. Leaving
a 2-mm conjunctival edge on the superior bor-
der of the graft is useful in forming the margin
of the reconstructed lid (Therapeutic: Level III
Evidence).
20
Hard-palate mucoperiosteal grafts
can be used to replace the posterior lamella due
to their ability to provide structural support and
mucosal lining. They have been shown to pro-
duce reliable results; however, donor-site mor-
bidity can be problematic.
21
Their use in upper
Fig. 5. (Left) Upper eyelid defect with perpendicular markings on either side for planned vertical
trimming of the tarsal plate prior to closure. The dog-ear is excised horizontally along the upper
lid crease. (Right) Direct lid closure is illustrated with a gray line-suture to line up the edges and
interrupted partial-thickness tarsal plate sutures. Reprinted with permission from McCord CD Jr,
Codner MA. Eyelid & Periorbital Surgery. St. Louis: Quality Medical Publishing; 2008.
Fig. 6. Direct closure of lower eyelid defect. (Left) A shallow full-thickness defect involving 15 percent of the lower eyelid. (Center)
Direct closure of the defect directed laterally in the skin tension line. (Right) Immediate intraoperative result after closure.
292e
Plastic and Reconstructive Surgery August 2013
eyelid reconstruction is controversial due to
the fact that hard-palate mucosa is composed
of keratinized, stratied squamous epithelium,
which can irritate the cornea. Despite this, excel-
lent results were reported for its use in upper
eyelid posterior lamellar reconstruction, without
complications.
22,23
Other posterior lamellar graft
options include nasal chondromucosa and auric-
ular cartilage. The cartilage can be crosshatched
if necessary to conform to the eyelid shape. Buc-
cal mucosa is a good lining option; however, it
lacks structural integrity and should be used in
combination with cartilage. Finally, a tarsomar-
ginal graft (composite eyelid graft) is composed
of tarsus, conjunctiva, and the lid margin includ-
ing the eyelashes. It can be used to reconstruct
shallow defects (mainly of the upper lid). It is
harvested as a full-thickness wedge from either
the upper or lower eyelid and before insetting;
the anterior lamella skin and muscle are excised,
leaving only the margin with the eyelashes. The
graft is usually 7 to 8 mm wide, and sequential
grafts can be used for bigger defects. The ante-
rior lamella is usually covered with a myocuta-
neous ap. Survival of the eyelashes, however, is
unpredictable, despite survival of the graft.
11,25,26
DIRECT CLOSURE OF AN EYELID
DEFECT
Upper eyelid defects that are up to 20 percent
of the lid in young patients and up to 30 percent
in older patients can be repaired with direct clo-
sure.
24
When combined with cantholysis, defects
of up to 50 percent of the upper lid can often be
closed directly in the elderly. Excessive tension
should be avoided because it can lead to postop-
erative mechanical ptosis, which tends to improve
in elderly patients.
25
Smaller lower eyelid defects
can be closed directly to avoid postoperative lid
malposition and ectropion, which can result from
excessive tension.
11,26
The tarsal edges should be
Fig. 7. (Left) An upper eyelid anterior lamellar defect involving the skin and orbicularis oculi muscle. (Center) The defect is recon-
structed with a V-Y advancement orbicularis-skin fap. (Right) Postoperative view of the upper eyelid 6 weeks later.
Video 1. Supplemental Digital Content 1, demonstrating lower lid
reconstruction with a Tenzel semicircular fap and a periosteal fap,
is available in the Related Videos section of the full-text article on
PRSJournal.com or, for Ovid users, at http://links.lww.com/PRS/
A774.)
Volume 132, Number 2 Eyelid Reconstruction
293e
trimmed in a perpendicular fashion to the lid
margin to facilitate approximation and to prevent
postoperative tarsal buckling and upper lid con-
tour deformity. A precise gray line 7-0 silk suture
is placed to assess the amount of tension and
line up the edges. When satisfactory alignment is
achieved, the tarsal edges are approximated using
interrupted 6-0 Vicryl sutures, making sure not to
go through the conjunctiva (Fig. 5). Finally, the
skin/muscle layer is closed with interrupted 7-0 silk
sutures. Any excess skin superiorly forming a dog-
ear is trimmed and closed horizontally along the
upper lid crease. The same steps are followed for
the lower eyelid, except that the incision should be
directed laterally in the skin tension line (Fig. 6).
26
(See Video, Supplemental Digital Content 1,
which demonstrates lower lid reconstruction with
a Tenzel semicircular ap and a periosteal ap,
available in the Related Videos section of the
full-text article on PRSJournal.com or, for Ovid
users, at http://links.lww.com/PRS/A774.)
LOCAL FLAPS
The use of orbicularis myocutaneous aps in
their various designs (advancement, V-Y, rotational)
has a better aesthetic result compared with full-
thickness skin grafts for anterior lamellar recon-
struction
27
(Fig. 7). They can also be combined
with posterior lamellar grafts and aps for full-
thickness reconstruction. For medium upper
and lower eyelid defects ranging from 40 to 60
percent of the lid, the Tenzel semicircular ap is
preferred as a workhorse ap.
28,29
The ap is dis-
sected in a suborbicularis plane, beginning at the
lateral canthus and then extending superiorly or
inferiorly in a semicircular pattern with a gentle
slope. A lateral canthotomy is performed, fol-
lowed by upper or lower cantholysis (depending
on the eyelid being reconstructed), and the eyelid
and ap are advanced medially to directly close
the defect
28,29
(Fig. 8). (See Video, Supplemental
Digital Content 1, which demonstrates lower lid
reconstruction with a Tenzel semicircular ap and
a periosteal ap, available in the Related Videos
section of the full-text article on PRSJournal.com
or, for Ovid users, at http://links.lww.com/PRS/
A774.) Closure is performed using the same prin-
ciples mentioned above. A 4-0 Vicryl suture can be
used between the cut edge of the Tenzel ap and
the periosteum of the lateral canthus to recreate
the lateral canthal angle. When this ap is used
to repair a medial defect, a lateral tarsoligamen-
tous reconstruction in the form of a lateral orbital
rim periosteal ap or ear cartilage may be needed
(Fig. 9). The McGregor ap has a similar concept
to the Tenzel ap, but instead of a semicircle,
Fig. 9. An illustration showing a Tenzel semicircular fap com-
bined with a periosteal fap for both posterior lamellar recon-
struction and lateral canthal support. Reprinted with permission
from McCord CD Jr, Codner MA. Eyelid & Periorbital Surgery. St.
Louis: Quality Medical Publishing; 2008.
Fig. 8. (Left) A full-thickness shallow defect involving 40 percent of the lower eyelid. (Center) The defect is reconstructed with a
Tenzel semicircular fap. (Right) Postoperative view of the lower eyelid 6 weeks later.
294e
Plastic and Reconstructive Surgery August 2013
the ap extends directly posteriorly after an ini-
tial slope, which makes it more of a transposition
advancement ap.
30
A Z-plasty is added laterally to
reduce the tension and improve the scar appear-
ance (Fig. 10). This ap is usually used for large
V-shaped defects of the lower eyelid. Other local
periorbital aps used for anterior lamellar recon-
struction include Blasius (Fig. 11), Imre (Fig. 12),
Fricke (temporal forehead ap) (Fig. 13), and
Tripier aps (Fig. 14). (See Video, Supplemental
Digital Content 2, which demonstrates total lower
lid and medial canthus reconstruction with a tar-
soconjunctival ap, a Tripier orbicularis myocuta-
neous ap, and a rhomboid ap, available in the
Related Videos section of the full-text article on
PRSJournal.com or, for Ovid users, at http://links.
lww.com/PRS/A775.)
The Mustard ap can be used for large anterior
lamellar defects and total lower eyelid reconstruc-
tion. This ap is a good option for reconstruction
of deep vertical defects and complete lower lid cov-
erage in a single procedure.
31
A semicircular sub-
orbicularis ap is developed at the lateral canthus
and then extended laterally to the preauricular
sulcus and elevated in a subsupercial musculo-
aponeurotic system or subcutaneous plane. The
posterior lamella must be reconstructed separately
with a graft, such as a tarsoconjunctival graft, ear
cartilage, or acellular dermal matrix, followed by
lateral periosteal xation and medial advance-
ment to close the defect (Fig. 15). It is the authors
Fig. 10. (Left) Intraoperative view of McGregors transposition advancement fap with Z-plasty to reconstruct a deep
V-shaped lower eyelid defect. (Right) Postoperative view 6 weeks later.
Fig. 11. An illustration of the Blasius fap used for lower lid reconstruction. (Left)
Preoperative design of a vertically oriented skin muscle fap with the base at the
medial canthus. (Right) The skin-muscle fap is transposed superiorly and com-
bined with a posterior lamellar graft for full-thickness lower eyelid reconstruction.
Reprinted with permission from McCord CD Jr, Codner MA. Eyelid & Periorbital Sur-
gery. St. Louis: Quality Medical Publishing; 2008.
Volume 132, Number 2 Eyelid Reconstruction
295e
preference, however, to use the Mustard ap for
reconstructing the cheek component of the defect
and combine it with another ap (Tripier ap, for
example) to reconstruct the lower lid component
to preserve the aesthetic units.
LID-SHARING PROCEDURES
With the exception of the transposition tar-
soconjunctival ap (Hewes ap), all lid-sharing
procedures are two-stage procedures that are
mainly used to reconstruct large, full-thickness
eyelid defects (>60 percent). The Hughes tarso-
conjunctival ap advances the tarsal plate and
conjunctiva from the ipsilateral upper eyelid to
repair a defect in the lower eyelid as a two-stage
approach.
32,33
This ap delivers vascularized poste-
rior lamellae and is divided after 14 days.
32
Little
donor morbidity occurs if 3 to 4 mm of superior
tarsal plate remains in the upper lid. To recon-
struct the anterior lamella, a semicircular ap,
vertical skin-muscle advancement, or full-thick-
ness skin graft can be used (Therapeutic: Level
IV Evidence).
34
(See Video, Supplemental Digital
Content 3, which demonstrates lower lid poste-
rior lamellar reconstruction with a Hughes tar-
soconjunctival advancement ap, available in the
Related Videos section of the full-text article on
PRSJournal.com or, for Ovid users, at http://links.
lww.com/PRS/A776.) A Cutler-Beard ap, on the
other hand, advances a full-thickness ap (exclud-
ing the tarsus) from the ipsilateral lower eyelid to
repair a defect in the upper eyelid, also in a two-
stage approach.
35,36
When designing the ap, it
is critical to leave at least 5 mm of full-thickness
lower lid margin to maintain blood supply to the
remaining bridge through the inferior arcade. A
graft of ear cartilage is placed between the con-
junctiva and the skin/muscle layers of the ap,
and is sutured superiorly to the levator aponeu-
rosis and medially and laterally to the residual tar-
sus of the upper eyelid. The ap is divided and
inset in 2 weeks (Fig. 16). A Mustard lid-sharing
pedicle ap is used in special situations where
a patient who has a wide, shallow upper eyelid
defect desires to maintain a lash line. The ap is
rectangular in design, 5 mm in vertical width, and
is taken from the center of the lower eyelid and
rotated based on the inferior medial palpebral
artery. The distal cut end of the ap is inset by
Fig. 12. An illustration of the Imre fap used for lower lid reconstruction. (Left) Preoperative
design of a rotational skin-muscle fap based laterally and inferiorly. A Burow's triangle is
cut to eliminate the dog-ear. (Right) The fnal postoperative appearance. Reprinted with
permission from McCord CD Jr, Codner MA. Eyelid & Periorbital Surgery. St. Louis: Quality
Medical Publishing; 2008.
Fig. 13. An illustration of the Fricke temporal forehead fap.
Reprinted with permission from McCord CD Jr, Codner MA. Eyelid
& Periorbital Surgery. St. Louis: Quality Medical Publishing; 2008.
296e
Plastic and Reconstructive Surgery August 2013
suturing it to the medial edge of the defect. Divi-
sion and inset are done in a second stage 2 weeks
later.
37
The Hewes transposition tarsoconjunctival
ap is useful for isolated defects of the lateral can-
thal area of the lower eyelid. It is harvested from
the lateral aspect of the upper eyelid using the
same principles of tarsoconjunctival graft/ap
harvest. However, unlike the Hughes ap, which
is based on blood supply from the superior fornix
and advanced inferiorly, the Hewes ap is based
on the peripheral arcade laterally and is trans-
posed to the lateral defect of the lower eyelid in
a one-stage approach
38
(Fig. 17). (See Video, Sup-
plemental Digital Content 2, which demonstrates
total lower lid and medial canthus reconstruction
with a tarsoconjunctival ap, Tripier orbicularis
myocutaneous ap, and rhomboid ap, available
in the Related Videos section of the full-text
article on PRSJournal.com or, for Ovid users, at
http://links.lww.com/PRS/A775.) The tarsal plate
is sutured to the lower eyelid tarsus medially and
secured to the lateral canthal tendon laterally. If
the lateral canthal tendon is unavailable, then a
periosteal ap can be utilized as discussed below.
The anterior lamella is reconstructed in a manner
similar to used for the Hughes ap.
MEDIAL CANTHAL DEFECTS
The medial canthal area poses a reconstruc-
tive challenge due to the complexity of its various
components. When planning reconstruction, the
surgeon should determine the involvement of the
following structures, from deep to supercial: (1)
bone and sinus, (2) medial canthal tendon, (3)
lacrimal drainage apparatus, and (4) soft tissue,
Fig. 14. (Left) An intraoperative view of a right anterior lamellar defect involving 70 percent of the entire lower eyelid. (Center) The
defect is reconstructed with a unipedicled Tripier fap, which is a skin-muscle transposition fap. (Right) Postoperative view of the
lower lid 6 weeks later.
Video 2. Supplemental Digital Content 2, demonstrating total lower
lid and medial canthus reconstruction with a tarsoconjunctival fap,
Tripier orbicularis myocutaneous fap, and rhomboid fap, is avail-
able in the Related Videos section of the full-text article on PRS-
Journal.com or, for Ovid users, at http://links.lww.com/PRS/A775.)
Volume 132, Number 2 Eyelid Reconstruction
297e
including the bilamellar medial eyelid. Exposed
sinuses should be obliterated with pericranial aps,
especially if postoperative radiation is planned,
to prevent the development of postoperative s-
tulae and infection.
9
Bone grafts can be used as
needed, particularly if they are deemed necessary
for medial canthal support. A posterior anchor-
ing point for the medial canthal tendon should be
established.
9,39
When the lacrimal system has been
compromised following injury or cancer resec-
tion, silicone tubes (e.g., Crawford tubes) may
be placed to stent the ducts to prevent closure.
4,9
Crawford tubes are used when either the superior
or inferior canaliculi are involved but still have at
least an intact portion that can be intubated. In
instances where either canaliculi cannot be intu-
bated or the lacrimal sac is involved, Jones tubes
may be placed bypassing the lacrimal system.
40
(See Video, Supplemental Digital Content 4,
which demonstrates lacrimal system bypass with a
Jones tube, available in the Related Videos sec-
tion of the full-text article on PRSJournal.com or,
for Ovid users, at http://links.lww.com/PRS/A777.)
A sliding tarsoconjunctival ap from the upper lid
is an excellent choice for posterior lamellar recon-
struction of either the medial or lateral canthi, if
Fig. 15. The Mustard fap for anterior lamellar reconstruction of the lower eye-
lid. (Above, left) A young patient with lower lid malposition after anterior lamel-
lar reconstruction with a full-thickness skin graft. (Above, right) The skin graft is
excised and the anterior lamellar defect is reconstructed with a Mustard cheek
fap mobilized with wide undermining. (Below, left) The fap is rotated into the
defect. (Below, right) Postoperative results 6 weeks later.
298e
Plastic and Reconstructive Surgery August 2013
adequate upper eyelid tissue is available.
9
This ap
can be used to reconstruct both the upper and
lower lid components of the medial canthus at the
same time.
39
The anterior lamella can be recon-
structed with a full-thickness skin graft or a variety
of local aps, including a rhomboid glabellar ap
41
(Fig. 18) and a medially based upper eyelid myo-
cutaneous ap (Therapeutic: Level V Evidence).
42
(See Video, Supplemental Digital Content 2, which
demonstrates total lower lid and medial canthus
reconstruction with a tarsoconjunctival ap, Trip-
ier orbicularis myocutaneous ap, and rhomboid
ap, available in the Related Videos section of
the full-text article on PRSJournal.com or, for Ovid
users, at http://links.lww.com/PRS/A775.) Soft-tissue
defects can also be reconstructed with a combi-
nation of pericranial aps and full-thickness skin
grafts.
43
Healing by spontaneous granulation is
also acceptable and well established in medial can-
thal reconstruction.
9
Key sutures should be placed
to direct the medial canthal tissue to oppose the
globe during healing by secondary intention.
TARSOLIGAMENTOUS SLING
RECONSTRUCTION
Addressing the lateral canthus is a critical step
in eyelid reconstruction. Laxity in xation will
lead to a misdirection of the vectors of orbicularis
pull, thereby predisposing to lagophthalmos on
eyelid closure or ectropion in repose. Further-
more, disruption of the lower lid/globe interface
can lead to conjunctival irritation, chemosis, or
canthal phimosis. Methods to address support
include primary suturing to the inner lateral
orbital periosteum, a drill hole xation with can-
thoplasty, or a periosteal bone ap.
The technique of lateral canthal xation is
similar to that used in cosmetic blepharoplasty and
has previously been described.
44
It is useful in lower
eyelids that possess minimal laxity with intact peri-
osteal tissue of the orbital rim. Drill-hole xation
is utilized in revisional procedures where lateral
periosteal tissue is diminutive.
45
When directing
the drill bit, it is important to direct a slight inward
tilt, in an effort to optimize lateral lid/globe con-
tact. A suture passer is often used to direct free
suture from the inner rim to the outer rim.
The periosteal bone ap is also a very reliable
technique, not only for providing xation at the
lateral canthus but also for resurfacing the lat-
eral posterior lamella when extended.
46,47
In its
design, a strip of periosteum is harvested from the
external lateral orbital rim.
.
This ap consists of a
strong layer that can be used to secure the lid to
the lateral orbital rim, providing excellent appo-
sition of tissue for canthal support to the globe.
(See Video, Supplemental Digital Content 1,
which demonstrates lower lid reconstruction with
a Tenzel semicircular ap and a periosteal ap,
available in the Related Videos section of the
full-text article on PRSJournal.com or, for Ovid
users, at http://links.lww.com/PRS/A774.) [See
Video, Supplemental Digital Content 5, which
demonstrates lower eyelid reconstruction with a
periosteal ap, Tripier orbicularis myocutaneous
ap, and Enduragen spacer (Tissue Science Labo-
ratories, Aldershot, United Kingdom), available
in the Related Videos section of the full-text
Video 3. Supplemental Digital Content 3, demonstrating lower lid
posterior lamellar reconstruction with a Hughes tarsoconjunctival
advancement fap, is available in the Related Videos section of the
full-text article on PRSJournal.com or, for Ovid users, at http://links.
lww.com/PRS/A776.)
Volume 132, Number 2 Eyelid Reconstruction
299e
Fig. 17. (Left) Illustration showing a Hughes tarsoconjunctival fap for posterior lamellar recon-
struction of a full-thickness lateral canthal defect involving both the upper and lower lids. (Right) A
Hewes transposition tarsoconjunctival fap based laterally for posterior lamellar reconstruction of a
full-thickness lateral lower eyelid defect. Reprinted with permission from McCord CD Jr, Codner MA.
Eyelid & Periorbital Surgery. St. Louis: Quality Medical Publishing; 2008.
Fig. 16. Total upper lid reconstruction with a Cutler-Beard fap. (Above, left) Full-thickness, nearly total upper eyelid defect.
(Above, right) Cutler-Beard bridge fap is designed from the opposing lower eyelid. (Below, left) A full-thickness incision is
made in the lower eyelid as shown, preserving at least 5mm of full-thickness lower eyelid margin. (Below, right) The fap is
advanced to the upper eyelid defect and sewn to the residual levator aponeurosis superiorly and the tarsal plate remnant
medially and laterally. A forehead rhomboid fap is planned for medial canthal reconstruction.
300e
Plastic and Reconstructive Surgery August 2013
article on PRSJournal.com or, for Ovid users, at
http://links.lww.com/PRS/A778.]
The authors prefer the use of a permanent
suture, as absorbable sutures may dehisce over time.
If the tarsoligamentous sling is detached from
the medial wall, the medial canthal tissue must be
anchored posteriorly to the posterior reection of
the medial canthal tendon. This can be achieved
by suturing it either to the stump of the posterior
limb of the medial canthal tendon or to the peri-
osteum (or periosteal ap) of the medial orbital
wall. If there is no available periosteum, a suture
anchor can be used to secure the medial canthal
tissue to the posterior lacrimal crest. Other avail-
able options include anchoring to a titanium
miniplate and unilateral transnasal wiring.
In situations where the entire posterior
lamella of the upper or lower lid is absent, the
retinacular attachments to the lateral and medial
orbital rim must be reconstructed indepen-
dently from lamellar reconstruction. This is also
the case in disorders involving loss of lid tone,
such as involutional or paralytic ectropion.
48
Fas-
cia lata and palmaris tendon grafts have been
well described for the design of frontalis slings
in treating congenital ptosis and can be utilized
as a suspension grafts to reconstruct the tarsolig-
amentous sling.
49
Disadvantages include morbid-
ity of the donor site, extended harvest time, and
the structure of the fascia, which can fray when
passed through a small, narrow opening. The
palmaris longus tendon has also been described
Fig. 18. (Left) An extensive full-thickness eyelid and periorbital defect involving the medial canthus along with 50 percent
of the medial upper and lower eyelids and the lateral canthus. (Right) Use of a forehead fap for reconstruction of both
the medial canthus and upper eyelid. Both residual lateral eyelids are advanced medially with superior and inferior semi-
circular faps.
Video 4. Supplemental Digital Content 4, demonstrating lacrimal
system bypass with a Jones tube, is available in the Related Videos
section of the full-text article on PRSJournal.com or, for Ovid users,
at http://links.lww.com/PRS/A777.
Volume 132, Number 2 Eyelid Reconstruction
301e
for use in ptosis surgery, and the authors prefer
its use for lower lid tarsoligamentous sling recon-
struction.
50,51
It is exceptionally easy to harvest as
a full or longitudinally split graft and has mini-
mal donor-site morbidity. Its narrow diameter is
optimal for securing it as a loop graft around
the medial canthal tendon, and it can be passed
through a small drill hole for xation in the lat-
eral orbital rim. Furthermore, it is ideal for en
bloc reconstruction of the Y-shaped component
of the upper and lower lateral canthus.
52
CONCLUSIONS
When approaching eyelid reconstruction, a thor-
ough understanding of surgical anatomy is impor-
tant in planning a successful surgical approach. For
the upper and lower eyelids, the anterior lamella,
posterior lamella, and tarsoligamentous sling often
require separate approaches for optimal functional
reconstruction. The principles of when to use a
graft, direct closure, a distant ap, or lid-sharing
procedures are fundamentally sound.
Mark A. Codner, M.D.
Mark Codner Plastic Surgery
1800 Howell Mill Road, Suite 140
Atlanta, Ga. 30318
macodner@aol.com
ACKNOWLEDGMENT
The authors acknowledge Dr. Clinton McCord for
his contribution of ideas and gures taken from the Eye-
lid and Periorbital Surgery textbook.
REFERENCES
1. McCord CD, Codner MA. Approach to eyelid recon-
struction. In: McCord CD, Codner MA, eds. Eyelid and
Periorbital Surgery. St. Louis: Quality Medical Publishing;
2008:495508.
2. Codner MA, Hanna MK. Applied anatomy of the eyelids and
orbit. In: Nahai F, eds. The Art of Aesthetic Surgery: Principles
and Techniques. St. Louis: Quality Medical Publishing;
2005:625650.
3. Amato MM, Monheit B, Shone JW. Eyelid anatomy. In:
Tasman W, Jaeger EA, eds. Duanes Anatomy. Philadelphia:
Lippincott Williams & Wilkins; 2011.
4. McCord CD, Groessl SA. Lower-lid dynamics: Inuence on
blepharoplasty and management of lower-lid retraction. Oper
Tech Plast Reconstr Surg. 1998;5:99108.
5. McCord CD, Codner MA. Classical surgical eyelid anatomy.
In: McCord CD, Codner MA, eds. Eyelid and Periorbital Surgery.
St. Louis: Quality Medical Publishing; 2008:346.
6. Codner MA, McCord CD, Hester TR. The lateral cantho-
plasty. Oper Tech Plast Reconstr Surg. 1998;5:9098.
7. Leibsohn JM, Hahn F. Medial canthal tendon reconstruc-
tion with nasal periosteum. Ophthal Plast Reconstr Surg.
1992;8:3540.
8. Tanenbaum M, McCord CD. Lacrimal drainage system. In:
Tasman W, Jaeger EA, eds. Duanes Anatomy. Philadelphia:
Lippincott Williams & Wilkins; 2011.
9. Madge SN, Malhotra R, Thaller VT, et al. A systematic
approach to the oculoplastic reconstruction of the eyelid
medial canthal region after cancer excision. Int Ophthalmol
Clin. 2009;49:173194.
10. Gndz K, Demirel S, Gnalp I, Polat B. Surgical
approaches used in the reconstruction of the eyelids after
excision of malignant tumors. Ann Ophthalmol (Skokie)
2006;38:207212.
11. Kakizaki H, Madge SN, Mannor G, Selva D, Malhotra R.
Oculoplastic surgery for lower eyelid reconstruction after
periocular cutaneous carcinoma. Int Ophthalmol Clin.
2009;49:143155.
12. Doxanas MT. Orbicularis muscle mobilization in eyelid
reconstruction. Arch Ophthalmol. 1986;104:910914.
13. Sa HS, Woo KI, Kim YD. Reverse modied Hughes proce-
dure for upper eyelid reconstruction. Ophthal Plast Reconstr
Surg. 2010;26:155160.
14. Shorr N, Goldberg RA, McCann JD, Hoenig JA, Li TG.
Upper eyelid skin grafting: An effective treatment for lag-
ophthalmos following blepharoplasty. Plast Reconstr Surg.
2003;112:14441448.
15. Khan JA. Sub-cilial sliding skin-muscle ap repair of ante-
rior lamella lower eyelid defects. J Dermatol Surg Oncol.
1991;17:167170.
16. Leone CR Jr, Hand SI Jr. Reconstruction of the medial eye-
lid. Am J Ophthalmol. 1979;87:797801.
17. Beyer CK, Bathrick ME. One-stage lower eyelid reconstruc-
tion. Ophthalmic Surg. 1982;13:551554.
18. Stephenson CM, Brown BZ. The use of tarsus as a free autog-
enous graft in eyelid surgery. Ophthal Plast Reconstr Surg.
1985;1:4350.
19. Hawes MJ. Free autogenous grafts in eyelid tarsoconjunctival
reconstruction. Ophthalmic Surg. 1987;18:3741.
20. Hawes MJ, Grove AS Jr, Hink EM. Comparison of free tar-
soconjunctival grafts and Hughes tarsoconjunctival grafts
for lower eyelid reconstruction. Ophthal Plast Reconstr Surg.
2011;27:219223.
21. Li TG, Shorr N, Goldberg RA. Comparison of the efcacy
of hard palate grafts with acellular human dermis grafts in
Video 5. Supplemental Digital Content 5, demonstrating lower
eyelid reconstruction with a periosteal fap, Tripier orbicularis
myocutaneous fap, and Enduragen spacer, is available in the
Related Videos section of the full-text article on PRSJournal.
com or, for Ovid users, at http://links.lww.com/PRS/A778.
302e
Plastic and Reconstructive Surgery August 2013
lower eyelid surgery. Plast Reconstr Surg. 2005;116:873878;
discussion 879.
22. Lalonde DH, Osei-Tutu KB. Functional reconstruction of
unilateral, subtotal, full-thickness upper and lower eyelid
defects with a single hard palate graft covered with advance-
ment orbicularis myocutaneous aps. Plast Reconstr Surg.
2005;115:16961700.
23. Cohen MS, Shorr N. Eyelid reconstruction with hard
palate mucosa grafts. Ophthal Plast Reconstr Surg. 1992;8:
183195.
24. McCord CD, Codner MA. Upper eyelid reconstruction. In:
McCord CD, Codner MA, eds. Eyelid and Periorbital Surgery.
St. Louis: Quality Medical Publishing; 2008:509541.
25. ODonnell BA, Mannor GE. Oculoplastic surgery for
upper eyelid reconstruction after cutaneous carcinoma. Int
Ophthalmol Clin. 2009;49:157172.
26. McCord CD, Codner MA. Lower eyelid reconstruction. In:
McCord CD, Codner MA, eds. Eyelid and Periorbital Surgery.
St. Louis: Quality Medical Publishing; 2008:543575.
27. Marchac D, de Lange A, Bine-bine H. A horizontal
V-Y advancement lower eyelid ap. Plast Reconstr Surg.
2009;124:11331141.
28. Tenzel RR. Reconstruction of the central one half of an eye-
lid. Arch Ophthalmol. 1975;93:125126.
29. Tenzel RR, Stewart WB. Eyelid reconstruction by the semi-
circle ap technique. Ophthalmology 1978;85:11641169.
30. McGregor IA. Eyelid reconstruction following subtotal resec-
tion of upper or lower lid. Br J Plast Surg. 1973;26:346354.
31. Sullivan SA, Dailey RA. Graft contraction: A comparison of
acellular dermis versus hard palate mucosa in lower eyelid
surgery. Ophthal Plast Reconstr Surg. 2003;19:1424.
32. Hughes WL. A new method for rebuilding a lower lid: Report
of a case. Arch Ophthalmol. 1937;17:1008.
33. Hughes WL. Reconstruction of the eyelids. Trans Am
Ophthalmol Soc. 1941;39:437.
34. Paridaens D, van den Bosch WA. Orbicularis muscle
advancement ap combined with free posterior and ante-
rior lamellar grafts: A 1-stage sandwich technique for eyelid
reconstruction. Ophthalmology 2008;115:189194.
35. Cutler NL, Beard C. A method for partial and total upper lid
reconstruction. Am J Ophthalmol. 1955;39:17.
36. Fischer T, Noever G, Langer M, Kammer E. Experience in
upper eyelid reconstruction with the Cutler-Beard tech-
nique. Ann Plast Surg. 2001;47:338342.
37. Mustard JC. New horizons in eyelid reconstruction. Int
Ophthalmol Clin. 1989;29:237246.
38. Hewes EH, Sullivan JH, Beard C. Lower eyelid reconstruction
by tarsal transposition. Am J Ophthalmol. 1976;81:512514.
39. McCord CD, Codner MA. Medial and lateral canthal recon-
struction. In: McCord CD, Codner MA, eds. Eyelid and Periorbital
Surgery. St. Louis: Quality Medical Publishing; 2008:577604.
40. Weber R.K. Atlas of lacrimal surgery. In: Keerl R, Schaefer
SD, Della Rocca RC, eds. Nasolacrimal Probing and Intubation.
1st Ed. Heidelberg: Springer; 2007:5359, 87103.
41. Ng SG, Inkster CF, Leatherbarrow B. The rhomboid
ap in medial canthal reconstruction. Br J Ophthalmol.
2001;85:556559.
42. Jelks GW, Glat PM, Jelks EB, Longaker MT. Medial canthal
reconstruction using a medially based upper eyelid myocuta-
neous ap. Plast Reconstr Surg. 2002;110:16361643.
43. Leatherbarrow B, Watson A, Wilcsek G. Use of the pericra-
nial ap in medial canthal reconstruction: Another appli-
cation for this versatile ap. Ophthal Plast Reconstr Surg.
2006;22:414419.
44. Codner MA, Woli JN, Anzarut A. Primary transcutane-
ous lower blepharoplasty with routine lateral canthal sup-
port: A comprehensive 10-year review. Plast Reconstr Surg.
2008;121:241250.
45. McCord CD, Boswell CB, Hester TR. Lateral canthal anchor-
ing. Plast Reconstr Surg. 2003;112:222237; discussion 238.
46. Weinstein GS, Anderson RL, Tse DT, Kersten RC. The use of
a periosteal strip for eyelid reconstruction. Arch Ophthalmol.
1985;103:357359.
47. McClellan WT, McCord CD, Neusch R. Optimizing the peri-
osteal ap for lateral eyelid reconstruction (Abstract). Plast
Reconstr Surg. 2010;126 (Supplement 4S):121122.
48. Terzis JK, Kyere SA. Minitendon graft transfer for suspension
of the paralyzed lower eyelid: Our experience. Plast Reconstr
Surg. 2008;121:12061216.
49. Qiu SS, Hontanilla B. Congenital ptosis of the upper eye-
lid corrected by a modied frontalis suspension technique
using autogenous tendons. Ann Plast Surg. 2011;67:129133.
50. Lam DS, Lam TP, Chen IN, Tsang GH, Gandhi SR. Palmaris
longus tendon as a new autogenous material for fronta-
lis suspension surgery in adults. Eye (Lond). 1996;10(Pt
1):3842.
51. Park S, Shin Y. Results of long-term follow-up observations of
blepharoptosis correction using the palmaris longus tendon.
Aesthetic Plast Surg. 2008;32:614619.
52. Bachelor EP, Jobe RP. The absent lateral canthal tendon:
Reconstruction using a Y graft of palmaris longus tendon.
Ann Plast Surg. 1980;5:362368.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- With 650 Bed-Capacity: Staff Nurse Progressive Care Unit-PulmonaryDocument3 pagesWith 650 Bed-Capacity: Staff Nurse Progressive Care Unit-PulmonaryMersalynNo ratings yet
- Ss1 Family Planning EssayDocument1 pageSs1 Family Planning EssayIrish BarcelonNo ratings yet
- MCN II PostpartumDocument16 pagesMCN II PostpartumJharaNo ratings yet
- GlomerulonephritisDocument1 pageGlomerulonephritismaleskunNo ratings yet
- Apgar ScoreDocument2 pagesApgar Scorejulialeo100% (3)
- November Staff Meeting MinutesDocument2 pagesNovember Staff Meeting Minutesapi-304790946No ratings yet
- Ocular Prosthesis: Custom Devices for Eye DisfigurementDocument11 pagesOcular Prosthesis: Custom Devices for Eye DisfigurementManjeevNo ratings yet
- ISAPS News Letter 2018Document52 pagesISAPS News Letter 2018Man Koon Suh, M.D.No ratings yet
- UNAN-Leon students explore orthopedicsDocument5 pagesUNAN-Leon students explore orthopedicsTriana CanalesNo ratings yet
- Philippine Medical Association Study Indicates That Women Were Injected With Contaminated Tetanus VaccineDocument2 pagesPhilippine Medical Association Study Indicates That Women Were Injected With Contaminated Tetanus VaccineJonathan Robert Kraus (OutofMudProductions)No ratings yet
- HRC Meeting Transfer ProposalsDocument24 pagesHRC Meeting Transfer ProposalsUgyen DorjiNo ratings yet
- Ccs Postings DetailDocument5 pagesCcs Postings DetailBrunoNo ratings yet
- Dental Handpieces and AccessoriesDocument23 pagesDental Handpieces and AccessoriesLokender YadavNo ratings yet
- PhobiaDocument4 pagesPhobiaAmudha MonyNo ratings yet
- Direx - Three New Tools To Compare The Effectiveness of Shock Wave LithotriptersDocument7 pagesDirex - Three New Tools To Compare The Effectiveness of Shock Wave LithotriptershamsiNo ratings yet
- Diastema Closure PDFDocument5 pagesDiastema Closure PDFsimon yonathanNo ratings yet
- Need For More Evidence in The Prevention and Management of PerinatalDocument10 pagesNeed For More Evidence in The Prevention and Management of PerinatalNATALY HASTAMORY VANEGASNo ratings yet
- Ferrer, Dalisay de Los Reyes: Career ObjectiveDocument3 pagesFerrer, Dalisay de Los Reyes: Career ObjectiveIshay FerrerNo ratings yet
- Trimodality Therapy in Bladder CancerDocument12 pagesTrimodality Therapy in Bladder CancerStirNo ratings yet
- Rguhs Thesis Topics in AnesthesiaDocument5 pagesRguhs Thesis Topics in AnesthesiaDltkCustomWritingPaperMurfreesboro100% (2)
- A Maternal and Child's Nurses Quest Towards ExcellenceDocument78 pagesA Maternal and Child's Nurses Quest Towards Excellencedecsag06No ratings yet
- Assessing the Development of eHealth in the Philippines from 1997 to 2020Document12 pagesAssessing the Development of eHealth in the Philippines from 1997 to 2020Nathan MielNo ratings yet
- P AlfonsiDocument5 pagesP Alfonsididik2rslavNo ratings yet
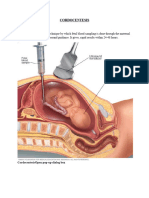
- CORDOCENTESISDocument6 pagesCORDOCENTESISSagar HanamasagarNo ratings yet
- IU Health LawsuitDocument40 pagesIU Health LawsuitIndiana Public Media News100% (1)
- Abnormalities of Labour and Delivery and Their Management: Joó József GáborDocument44 pagesAbnormalities of Labour and Delivery and Their Management: Joó József GáborAnnisa Mutiara InsaniNo ratings yet
- Nursing Exam Papers from Rajiv Gandhi UniversityDocument10 pagesNursing Exam Papers from Rajiv Gandhi UniversityVantrigaru Veeresh Bangi100% (4)
- Panik Poli Obgyn RS USU Mei 9 - 15.Document43 pagesPanik Poli Obgyn RS USU Mei 9 - 15.Zulfindra Arifin93No ratings yet
- Cek List BiomedicDocument159 pagesCek List BiomedicIboedIstina100% (1)
- Volvulus Characterization in Radiology: A Review: Poster No.: Congress: Type: Topic: AuthorsDocument21 pagesVolvulus Characterization in Radiology: A Review: Poster No.: Congress: Type: Topic: AuthorsAgunkRestuMaulanaNo ratings yet