Professional Documents
Culture Documents
Asian Cardiovascular and Thoracic Annals 2011 Wakahara 228 31
Uploaded by
Paola Méndez Neciosup0 ratings0% found this document useful (0 votes)
28 views5 pagesDescending necrotizing mediastinitis is a critical infection and the mortality rate remains high. Early aggressive surgical drainage and antibiotic therapy are essential for treatment. A right-side minithoracotomy with thoracoscopic assistance was performed in 11 cases between May 2002 and March 2008.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDescending necrotizing mediastinitis is a critical infection and the mortality rate remains high. Early aggressive surgical drainage and antibiotic therapy are essential for treatment. A right-side minithoracotomy with thoracoscopic assistance was performed in 11 cases between May 2002 and March 2008.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
28 views5 pagesAsian Cardiovascular and Thoracic Annals 2011 Wakahara 228 31
Uploaded by
Paola Méndez NeciosupDescending necrotizing mediastinitis is a critical infection and the mortality rate remains high. Early aggressive surgical drainage and antibiotic therapy are essential for treatment. A right-side minithoracotomy with thoracoscopic assistance was performed in 11 cases between May 2002 and March 2008.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
http://aan.sagepub.
com/
Asian Cardiovascular and Thoracic Annals
http://aan.sagepub.com/content/19/3-4/228
The online version of this article can be found at:
DOI: 10.1177/0218492311408641
2011 19: 228 Asian Cardiovascular and Thoracic Annals
Teppei Wakahara, Yugo Tanaka, Yoshimasa Maniwa, Wataru Nishio and Masahiro Yoshimura
Successful management of descending necrotizing mediastinitis
Published by:
http://www.sagepublications.com
On behalf of:
The Asian Society for Cardiovascular Surgery
can be found at: Asian Cardiovascular and Thoracic Annals Additional services and information for
http://aan.sagepub.com/cgi/alerts Email Alerts:
http://aan.sagepub.com/subscriptions Subscriptions:
http://www.sagepub.com/journalsReprints.nav Reprints:
http://www.sagepub.com/journalsPermissions.nav Permissions:
What is This?
- Jun 1, 2011 Version of Record >>
by guest on May 29, 2014 aan.sagepub.com Downloaded from by guest on May 29, 2014 aan.sagepub.com Downloaded from
Original Article
Successful management of descending
necrotizing mediastinitis
Teppei Wakahara, Yugo Tanaka, Yoshimasa Maniwa,
Wataru Nishio and Masahiro Yoshimura
Abstract
Descending necrotizing mediastinitis is a critical infection and the mortality rate remains high. Early aggressive surgical
drainage and antibiotic therapy are essential for treatment. We evaluated the efficiency of transthoracic drainage using a
minimally invasive technique in 11 cases of descending necrotizing mediastinitis between May 2002 and March 2008.
We performed a right-side minithoracotomy with thoracoscopic assistance, and the mediastinum was thoroughly
drained. The length of hospitalization ranged from 30 to 117 days. The postoperative course was good in all patients,
and the outcome was favorable. All patients were discharged without major complications. We recommend employing a
minithoracotomy with thoracoscopic assistance for aggressive treatment of descending necrotizing mediastinitis.
Keywords
bacterial infections, drainage, mediastinitis, otorhinolaryngologic diseases, thoracoscopy
Introduction
Descending necrotizing mediastinitis (DNM) is a criti-
cal infection that develops when an infection arises in
the neck region, such as the mouth or pharynx, and
descends to the mediastinum because of the anatomical
connection. Although the mortality rate has improved
in recent years, it still remains high at 14%23%.
1,2
We
treated 11 cases of DNM, and all were healed without
major complications. Herein, we describe our proce-
dures and discuss their advantages.
Patients and methods
From May 2002 to March 2008, we treated 11 consecu-
tive patients with DNM in Kobe University Hospital.
All patients underwent preoperative cervicothoracic
computed tomography (CT). Inclusion criteria for the
study population were those previously dened by
Estrera and colleagues:
3
clinical manifestations of a
severe infection, establishment of a relationship between
an oropharyngeal or cervical infection and subsequent
mediastinitis, radiographic features characteristic of
DNM (Figures 1 and 2), and documentation of a necro-
tizing mediastinal infection at the time of operative
debridement.
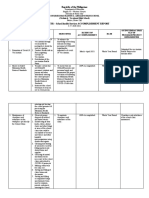
For entry into the thoracic cavity, a minithoracot-
omy with the assistance of thoracoscopy was performed
in all cases. Ten patients had a thoracotomy thorough
the right triangle of auscultation, and one had a right
para-mediastinal incision.
4
At the same time, cervical
open drainage was carried out by an otolaryngologist in
10 patients, and 9 underwent a tracheotomy in antici-
pation of laryngeal edema. The mediastinal pleura were
opened widely longitudinally in 3 areas: the anterior
mediastinum, paratracheal space, and posterior space
of the trachea including the subcarinal space (Figure 3).
Drainage of pus was followed by debridement of necro-
tic tissues. Silicon drains and tubes for postoperative
irrigation were positioned at all opened areas, and an
additional drain was placed in the inferior thoracic
cavity, just above the diaphragm (Figure 4).
Asian Cardiovascular & Thoracic Annals
19(3/4) 228231
The Author(s) 2011
Reprints and permissions:
sagepub.co.uk/journalsPermissions.nav
DOI: 10.1177/0218492311408641
aan.sagepub.com
Division of Thoracic Surgery, Kobe University Graduate School of
Medicine, Kobe, Japan.
Corresponding author:
Yoshimasa Maniwa, Division of Thoracic Surgery, Kobe University
Graduate School of Medicine, 7-5-2 Kusunoki-cho, Chuo-ku, Kobe
650-001, Japan
Email: maniwa@med.kobe-u.ac.jp
by guest on May 29, 2014 aan.sagepub.com Downloaded from
Postoperatively, we irrigated the mediastinum and
thoracic cavity continuously with warm physiologic
saline at 100 mLh
1
for 24 h. Subsequently, we per-
formed the irrigation with 1 L of physiologic saline
for 1 h twice daily. The duration of drainage and irri-
gation was dependent on clinical ndings and the
results of bacterial culture.
Results
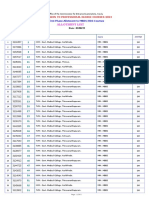
The characteristics of each patient are shown in
Table 1. Their mean age was 65.9 years (range, 54
78), and 6 were male. Diabetes was observed in 4
patients. Two patients had injury to the pharynx as a
result of urgent tracheal intubation. No cases were
caused by odontogenic infection. The period from
detection of neck infection to thoracotomy for medias-
tinal drainage ranged from 3 to 22 days (mean, 7.7
days). In 3 cases (nos. 1, 2, 6), surgical treatment was
performed more than 10 days after the diagnosis of
cervical infection. In these patients, antibiotic therapy
had been given initially by general practitioners, but the
symptoms became worse, and they consulted us.
Bacteriological examination was carried out in all 11
patients, which revealed aerobic Streptococci in 6, aer-
obic Propionibacterium acnes in 1, and mixed aerobic
Figure 1. Chest radiograph showing enlargement
of the mediastinum.
Figure 3. The mediastinal pleura were opened wide,
longitudinally, in at least 3 areas: anterior mediastinum,
paratracheal space, and posterior space of the trachea to the
space of the subcarina. SVC=superior vena cava.
Figure 4. Postoperative chest radiograph showing thoracic
drains positioned in all opened areas, and an additional drain in
the inferior thoracic cavity, just above the diaphragm.
Figure 2. Chest computed tomography showing an abscess
extending from the upper mediastinum, with gas collections.
Wakahara et al. 229
by guest on May 29, 2014 aan.sagepub.com Downloaded from
and anaerobic organisms (Streptococcus and Prevotella)
in 1; the pathogens could not be identied in the other 3
cases. The postoperative duration of mediastinal irri-
gation ranged from 5 to 30 days (mean, 12.3 days),
and the duration of drainage ranged from 9 to 56 days
(mean, 21.3 days). CT gave useful information on any
remaining abscess cavities. In one case, thoracotomy
was repeated to manage residual abscess cavities.
Duration of hospitalization ranged from 30 to 117
days (mean, 67.6 days). The mediastinitis resolved
well postoperatively in all patients, and the outcome
was favorable: all patients were discharged without
major complications.
Discussion
Because the cervical space contains loose areolar tissue
and continues into the pericardium, parietal pleura, and
mediastinum, any oropharyngeal or cervical infection
can easily move into the chest. Generally, the spread of
infection is very rapid. For example, it is said that infec-
tion from a cervical abscess can often progress to the
mediastinum within 48 h, and may result in pyothorax
and pericarditis as well as sepsis, disseminated intravas-
cular coagulation, and multiple organ failure.
3
In the
1980 s, the mortality from DNM was reported to be as
high as 30%40%. Although, early diagnosis by
improved CT imaging and the availability of broad-
spectrum antibiotics has reduced the mortality rate to
14%23%, it is still high compared to other infectious
diseases. Delay of treatment is one reason for the high
mortality rate in DNM; therefore, early aggressive
surgical drainage and antibiotic therapy are essential.
4
The therapeutic principle in our institution is to
perform emergency surgery soon after the diagnosis
of DNM.
It is very dicult to select the optimal antibiotic
therapy because identication of bacteria and antibiotic
sensitivity takes time. It is reported that mixed infec-
tions including both aerobic and anaerobic bacteria
were detected in >50% of DNM patients, and polymi-
crobial infections in 88%.
5,6
In our cases, aerobic bac-
teria in 7 patients and mixed aerobic and anaerobic
bacteria in one were detected by bacteriological exam-
ination, but no bacterium was detected in 3 because
previous medication masked the responsible bacteria.
We consider that intravenous broad-spectrum antibi-
otic therapy is essential in the primary treatment of
DNM because various bacteria may be responsible,
and the spread of infection is very rapid.
The indication for transthoracic drainage of the
mediastinum in patients with DNM is controversial.
Estrera and colleagues
3
stated that open drainage
should be performed when the abscess cannot be con-
trolled by transcervical mediastinal drainage. Kruyt
and colleagues
7
argued that transcervical drainage is
adequate for draining the mediastinum in patients
who do not have septic conditions. Endo and col-
leagues
8
classied DNM into 3 types, according to
the degree of spread of DNM diagnosed by CT, and
proposed dierent surgical management strategies
according to this classication. On the other hand, sev-
eral reports demonstrated that aggressive mediastinal
drainage by a thoracotomy approach is required for
treatment of DNM, regardless of the level of mediasti-
nal involvement.
9,10
Marty-Ane and colleagues
11
rec-
ommended the thoracotomy approach because it
allows comprehensive access to a hemithorax including
the ipsilateral mediastinum and pericardium. Corsten
and colleagues
12
noted that the mortality rate in cases
of transcervical drainage only was 47%, whereas it was
19% after thoracotomy drainage.
Table 1. Characteristics of 11 patients with descending necrotizing mediastinitis
Case Age (years)/ Underlying Duration* Drainage Hospital
No. Sex Disease Source of infection (days) Time (days) Stay (days) Outcome
1 57/M AF Retropharyngeal abscess 22 Unknown 62 Discharged
2 60/F - Unknown 11 11 64 Discharged
3 67/F AMI Pharyngeal intubation injury 5 56 64 Discharged
4 58/M DM/gout Acute epiglottitis 3 15 30 Discharged
5 74/F Dementia Acute epiglottitis 5 12 103 Discharged
6 63/M Basedow disease Cervical cellulitis 13 23 30 Discharged
7 74/M AMI Pharyngeal intubation injury 5 16 60 Discharged
8 78/M RA/DM Unknown 6 17 117 Discharged
9 54/M - Cervical cellulitis 5 40 110 Discharged
10 69/F - Pharyngeal injury 7 14 61 Discharged
11 71/F DM Unknown 3 9 43 Discharged
*From onset of primary infection to operation. AF =atrial fibrillation, AM=acute myocardial infarction, DM=diabetes mellitus,
RA=rheumatoid arthritis.
230 Asian Cardiovascular & Thoracic Annals 19(3/4)
by guest on May 29, 2014 aan.sagepub.com Downloaded from
It seems that previous debate concerned whether the
adequacy of drainage or avoidance of the stress of
surgery was given priority in the treatment of DNM.
We consider that minimally invasive surgery and accu-
rate drainage are both important. Therefore, we
performed a minithoracotomy with thoracoscopic assis-
tance in all 11 cases, to achieve minimally invasive and
ecient drainage. Compared to the conventional thora-
cotomy, our approach provided a smaller surgical
wound and less invasive treatment. Moreover, with the
aid of thoracoscopy, we were able to get good visualiza-
tion of the entire thoracic cavity and ensure ecient
drainage. Although we recognize that some of our
cases might have been controllable by a transcervical
approach only, avoidance of the transthoracic approach
might have resulted in failure of treatment in some cases.
Furthermore, emergency cervical and mediastinal drain-
age was performed at the same time in all cases, even
if the patients condition was poor, because prompt
treatment is also necessary for DNM. Our treatment
approach was successful in all 11 patients. In recent
case reports, mediastinal drainage using video-assisted
thoracoscopic surgery has been described as a much less
invasive approach.
13,14
The progress in thoracoscopic
techniques has reduced the degree of surgical stress,
and transthoracic drainage can be employed without
constraint. It is expected that treatment for DNM will
develop with less invasive and more ecient drainage.
The prophylactic indication for postoperative tra-
cheotomy is controversial. We consider that tracheot-
omy should be performed in patients whose
preoperative respiratory condition is severe, because
pharyngeal edema and airway constriction are frequent
symptoms of DNM. In 9 of our 11 patients, strict respi-
ratory care was needed for long periods because the
preoperative respiratory condition was severe. Thus
we performed tracheotomy without hesitation in these
cases, and obtained good results. Because the tracheot-
omy site is near the cervical drainage wound, cervical
infection could spread to the tracheotomy wound,
resulting in a longer hospital stay. However, we con-
sider that airway management is more important than
wound infections. We recommend that a minithoracot-
omy with thoracoscopic assistance should be employed
for aggressive treatment of patients with DNM.
Funding
This research received no specic grant from any funding
agency in the public, commercial, or not-for-prot sectors.
Conflict of interest statement
None declared.
References
1. Sancho LM, Minamoto H, Fernandez A, Sennes LU and
Jatene FB. Descending necrotizing mediastinitis: a
retrospective surgical experience. Eur J Cardiothorac
Surg 1999; 16: 200205.
2. Papalia E, Rena O, Oliaro A, Cavallo A, Giobbe R,
Casadio C, et al. Descending necrotizing mediastinitis:
surgical management. Eur J Cardiothorac Surg 2001;
20: 739742.
3. Estrera AS, Landay MJ, Grisham JM, Sinn DP and Platt
MR. Descending necrotizing mediastinitis. Surg Gynecol
Obstet 1983; 157: 545552.
4. Tanaka Y, Maniwa Y, Yoshimura M and Okita Y.
Successful treatment of descending necrotizing mediasti-
nitis. Gen Thorac Cardiovasc Surg 2007; 55: 366369.
5. Wheatley MJ, Stirling MC, Kirsh MM, Gago O and
Orringer MB. Descending necrotizing mediastinitis:
transcervical drainage is not enough. Ann Thorac Surg
1990; 49: 780784.
6. Chow AW, Roser SM and Brady FA. Orofacial odonto-
genic infections [Review]. Ann Intern Med 1978; 88:
392402.
7. Kruyt PM, Boonstra A, Fockens P, Reeders JW and van
Lanschot JJ. Descending necrotizing mediastinitis caus-
ing pleuroesophageal fistula: successful treatment by
combined transcervical and pleural drainage. Chest
1996; 109: 14041407.
8. Endo S, Murayama F, Hasegawa T, Yamamoto S,
Yamaguchi T, Sohara Y, et al. Guideline of surgical man-
agement based on diffusion of descending necrotizing
mediastinitis. Jpn J Thorac Cardiovasc Surg 1999; 47:
1419.
9. Marty-Ane CH, Alauzen M, Alric P, Serres-Cousine O
and Mary H. Descending necrotizing mediastinitis:
advantage of mediastinal drainage with thoracotomy.
J Thorac Cardiovasc Surg 1994; 107: 5561.
10. Freeman RK, Vallieres E, Verrier ED, Karmy-Jones R
and Wood DE. Descending necrotizing mediastinitis: an
analysis of the effects of serial surgical debridement on
patient mortality. J Thorac Cardiovasc Surg 2000; 119:
260267.
11. Marty-Ane CH, Berthet JP, Alric P, Pegis JD, Rouvie` re P
and Mary H. Management of descending necrotizing
mediastinitis: an aggressive treatment for an aggressive
disease. Ann Thorac Surg 1999; 68: 212217.
12. Corsten MJ, Shamji FM, Odell PF, Frederico JA,
Laframboise GG, Reid KR, et al. Optimal treatment of
descending necrotizing mediastinitis. Thorax 1997; 52:
702708.
13. Roberts JR, Smythe WR, Weber RW, Lanutti M,
Rosengard BR and Kaiser LR. Thoracoscopic manage-
ment of descending necrotizing mediastinitis. Chest 1997;
112: 850854.
14. Nagayasu T, Akamine S, Oka T and Muraoka M.
Thoracoscopic drainage with wound edge protector for
descending necrotizing mediastinitis. Interact Cardiovasc
Thorac Surg 2003; 2: 5860.
Wakahara et al. 231
by guest on May 29, 2014 aan.sagepub.com Downloaded from
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Joy Wanjiru Midwifery Case StudyDocument17 pagesJoy Wanjiru Midwifery Case StudyJimmy MainaNo ratings yet
- Q2 2023 PFE Earnings ReleaseDocument33 pagesQ2 2023 PFE Earnings ReleaseJuan PeNo ratings yet
- Suicide Assessment Five-Step Evaluation and Triage SMA09-4432Document2 pagesSuicide Assessment Five-Step Evaluation and Triage SMA09-4432Pam RojasNo ratings yet
- NPI NCMH StephDocument12 pagesNPI NCMH StephAnonymous 2fUBWme6wNo ratings yet
- Sep 15 Final Cpsa LetterDocument19 pagesSep 15 Final Cpsa LetterFatima Berriah CamposNo ratings yet
- Chapters 1 3Document29 pagesChapters 1 3marlonNo ratings yet
- Conversation 2Document17 pagesConversation 2JenNo ratings yet
- Heal-Lom A Proposed PJG Hospital Extension in Talavera, Nueva EcijaDocument10 pagesHeal-Lom A Proposed PJG Hospital Extension in Talavera, Nueva EcijaPhilip PinedaNo ratings yet
- (PSYCH) 4.01 Forensic Psychiatry - Dr. Cruz PDFDocument6 pages(PSYCH) 4.01 Forensic Psychiatry - Dr. Cruz PDFMon Kristoper CastilloNo ratings yet
- Vaccine Hesitancy Among Healthcare WorkersDocument33 pagesVaccine Hesitancy Among Healthcare WorkersFitz Jaminit100% (1)
- Biodata March 19Document81 pagesBiodata March 19ULAGANATHAN MNo ratings yet
- Pediatric Pain Assessment in TDocument6 pagesPediatric Pain Assessment in TnurtiNo ratings yet
- Allotlist p2Document182 pagesAllotlist p2Salman SAYYADNo ratings yet
- Shoulder DystociaDocument3 pagesShoulder DystociaNicole Genevie MallariNo ratings yet
- IMDocument5 pagesIMChimboy BartolomeNo ratings yet
- Diabetic Foot Classifications: Review of Literature: Amit Kumar C Jain, Sunil JoshiDocument7 pagesDiabetic Foot Classifications: Review of Literature: Amit Kumar C Jain, Sunil JoshiPutriPasaribuNo ratings yet
- Course Schedule 2019 PDFDocument30 pagesCourse Schedule 2019 PDFcassindromeNo ratings yet
- Case StudyDocument2 pagesCase StudyNetanya AlfadNo ratings yet
- Control of Acute Respiratory Infections 2Document6 pagesControl of Acute Respiratory Infections 2إحسان ماجد محمدNo ratings yet
- Assessment of Patient's Knowledge, Attitude and Practice Regarding HypertensionDocument6 pagesAssessment of Patient's Knowledge, Attitude and Practice Regarding HypertensionScintya NasutionNo ratings yet
- Use of The Glidescope For Double-Lumen Endobronchial IntubationDocument3 pagesUse of The Glidescope For Double-Lumen Endobronchial IntubationStephanus Kinshy Imanuel PangailaNo ratings yet
- FM 8-230 Medical Specialist PDFDocument720 pagesFM 8-230 Medical Specialist PDFJames100% (1)
- MBA-Thesis-Marketing Thesis-Marketing Strategy of An International Publication House: Particular Reference To Internet MarketingDocument7 pagesMBA-Thesis-Marketing Thesis-Marketing Strategy of An International Publication House: Particular Reference To Internet MarketingAdwait DeNo ratings yet
- Employee Engagement in MOH-consolidatedDocument30 pagesEmployee Engagement in MOH-consolidatedMalak MagablehNo ratings yet
- E Health AssessmentDocument9 pagesE Health AssessmentarisNo ratings yet
- Evaluascdc Hiv MethodDocument11 pagesEvaluascdc Hiv MethodmasaruddinNo ratings yet
- Medication Errors - The Importance of Safe DispensingDocument5 pagesMedication Errors - The Importance of Safe DispensingRyan Rahman OesmanNo ratings yet
- TracheostomyDocument29 pagesTracheostomyFemi AustinNo ratings yet
- 2nd Quarter - School Health Services Accomplishment ReportDocument4 pages2nd Quarter - School Health Services Accomplishment ReportJimmellee EllenNo ratings yet
- Letter of Certification For EECP TherapyDocument1 pageLetter of Certification For EECP TherapytomriedmanNo ratings yet