Professional Documents
Culture Documents
Pathology of The Lung Objectives: Define and Use in Proper Context The Following Terms
Uploaded by
applesncore0 ratings0% found this document useful (0 votes)
130 views45 pageslung pathology
Original Title
Lung
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentlung pathology
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
130 views45 pagesPathology of The Lung Objectives: Define and Use in Proper Context The Following Terms
Uploaded by
applesncorelung pathology
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 45
Pathology of the Lung
Dr. Dexter MD FRC Path
Undercover Professor
Dept. of Pathology
St.George's University
Objectives
Define and use in proper context
the following terms
adult respiratory distress syndrome (ARDS)
alveolar-capillary membrane Asteroid body
Asthma Atelectasis Barrel chest Bleb
blue bloater bronchial cyst Bulla chronic
bronchitisBronchiectasis bronchiolitis obliterans
bronchogenic carcinoma chronic obstructive
pulmonary disease (COPD) coin lesion
Consolidation cor pulmonale diffuse alveolar
damage (DAD) Emphysema empyema extrinsic
allergic alveolitis (EAA) Ghon complex
Goodpasture syndrome Hemothorax heart
failure cell Hemoptysis Honeycomb lung Horner
syndrome
Hyaline membrane Hydrothorax Hypertrophic
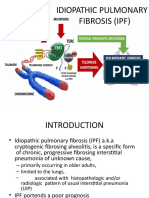
pulmonary osteoarthropathy Idiopathic interstitial
pneumonia Idiopathic pulmonary fibrosis (IPF)
Non-small cell lung cancer (NSCLC) Obstructive
lung disease Organizing pneumonia Pancoast
tumor Paraneoplastic syndrome Pink puffer
Plexiform lesion Pneumothorax Pulmonary edema
Pulmonary embolism Pulmonary veno-occlusive
disease (PVOD) Rales Reid index Restrictive
lung disease Rhonchi Saddle embolus
Schaumann body Severe acute respiratory
syndrome (SARS) Small airways disease Status
asthmaticus Tension pneumothorax
Clinical
The student should be able to
Enlist the steps in clinical examination
of the respiratory system, usual related
investigations performed (listed) and
normal results of spirometry and
arterial blood gases.
Explain the pathogenesis of common
symptoms related to respiratory illnesses
(listed).
Pain
Cough
dyspnea
sputum production
cyanosis
clubbing of fingers
hypertrophic pulmonary
osteoarthropathy
secondary polycythemia
hemoptysis
cor pulmonale
Define atelectasis, classify and explain
the pathogenesis
Infections
Explain the normal defense mechanisms against
infections in lung.
Distinguish the settings for primary versus
secondary pneumonias. Derive the clinical features
of pneumonias based on the common structural and
functional alterations in lungs.
Identify the common cause of pneumonias in the
following clinical settings- community acquired,
immunodeficiency, neutropenia, hospital acquired,
alcoholics, post viral infection, COPD, malnutrion,
preexisting cardiac conditions, diabetes, aspiration
Explain the concepts of airspace pneumonia and interstitial
pneumonias , indicate the common category of organisms
responsible for each.
Distinguish grossly and microscopically lobar and broncho
pneumonias and identify commonly responsible organisms for
each.
Outline the usual investigations and the course of illness.
Explain steps in the evolution of histopathology of pneumonias
(4 listed), the usual settings and outcomes for the following
pneumonias - Strep. pneumonia, legionella pneumophilia,
klebsiella, staph. Aureus, pseudomonas and aspiration.
Distinguish Interstitial Pneumonias as a
group and derive their clinical features,
pathology and common agents
responsible,
Explain the pathogenesis of lung
abscesses and characterize the
features of that secondary to
aspiration.
Recapitulate the lung lesions caused
by tuberculosis, CMV, pneumocystis
carinii, cryptococcus, histoplasma,
actinomycosis and nocardia. ( not
included in the exam)
Vascular and hemodynamic
diseases
List the causes of passive and active
pulmonary edema (listed)
Explain the pathogenesis of adult
respiratory distress syndrome (ARDS)
and mention the clinical settings
(listed)
Derive the pathologic features and
clinical features and the course of
ARDS.
Explain the common settings for the
development of pulmonary embolism;
differentiate the effects of large,
medium and small emboli.
Describe the gross and microscopic
appearances of pulmonary infarcts and
correlate them with clinical features.
Classify pulmonary hypertension into
primary, secondary and list the causes
for secondary type.
Describe the vascular changes in
pulmonary hypertension.
Distinguish lesions of Goodpastures
syndrome from idiopathic pulmonary
hemosiderosis by morphology and
etiology.
Restrictive lung disease
Explain the meaning of restrictive lung
disease and why it leads to respiratory
difficulty.
Explain the pathogenesis of Adult
Respiratory Distress Syndrome (ARDS)
and name at least 3 common causes.
Explain the pathogenesis of idiopathic
pulmonary fibrosis (Hamman Rich
Syndrome) and derive the clinical
features.
Differentiate desquamative interstitial
pneumonia, pulmonary alveolar
proteinosis and lymphocytic interstitial
pneumonia theoretically.
Explain the pathology, pathogenesis
and clinical features of sarcoidosis and
distinguish it from tuberculosis on
histology.
Give three examples of hypersensitivity
pneumonitis (listed) and highlight the
main pathogenetic mechanism.
Mention the salient clinical and
pathologic features of Goodpastures
syndrome and explain the
pathogenesis.
Distinguish idiopathic pulmonary
hemosiderosis from Goodpastures
syndrome theoretically.
Recapitulate( not included in the exam)
the pathology and pathogenesis of
common pneumoconiosis like
anthracosis, silicosis, asbestosis and
berylliosis and recognize that they are
included in the spectrum of restrictive
lung disease.
Chronic obstructive pulmonary
disease (COPD)
Explain the concept of COPD and
mention the common diseases
included in the category (listed).
Define emphysema, classify into centri
acinar, panacinar and septal, explain
the pathogenesis, and derive the
clinical features.
Define chronic bronchitis, classify into
simple, mucopurulent , asthmatic and
obstructive types, explain the
pathogenesis and derive the clinical
features.
Distinguish pink puffers from blue
bloaters theoretically.
Define bronchial asthma, classify into
intrinsic and extrinsic, explain the
pathogenesis, pathology and derive the
clinical features. Define status
asthmaticus.
Define bronchiectasis, identify the
components (destruction, fibrosis,
dilatation), etiology, pathologic and
clinical features.
Name the components of Kartageners
syndrome and identify the basic defect.
Derive the complications of
bronchiectasis (listed).
Explain the role of exercise therapy in
COPD
Neoplasms/ tumors
Classify the lung tumors
(histologically) and indicate relative
frequencies.
Distinguish hilar and peripheral tumors
with examples and clinical features.
Explain what is occult lung cancer.
Intelligently analyze data on
relationship of smoking and lung
cancer (statistics, clinical,
experimental, histological subtypes)
Identify oncogenes related to lung
cancer
List the predominant clinical features,
growth pattern, spread and prognosis
of Squamous cell carcinoma, Adeno
carcinoma, Bronchioloalveolar
carcinoma, Small cell carcinoma,
bronchial carcinoids and
Mesotheliomas.
Highlight the peculiarities of
Bronchioloalveolar carcinoma -
(resemblance to pneumonia, X-ray,
histology).
Describe the different modes of Spread
of lung cancer
Explain Horners Syndrome, Pancoast
syndrome, Carcinoid Syndrome.
Identify usual sites of metastasis of
lung cancer.
Explain the importance of Virchows
lymph node; coin lesion on X-ray
Define paraneoplastic syndromes,
enlist those associated with
bronchogenic carcinoma, identify any
specific relationship to histologic
subtypes.
Explain why liver metastasis is not a
prerequisite to manifest Carcinoid
syndrome in bronchial carcinoids as
compared to gut carcinoids.
Concerning Mesotheliomas, identify
etiology, special feature of histology
and mode of spread.
Concerning nasopharyngeal
carcinoma, analyze the relationship
with EBV and discuss the term
Lymphoepithelioma.
Outline the investigations that can be
performed for diagnosis of lung cancer
-Sputum, X-ray, pleural tap, pleural
biopsy, bronchoscopy, bronchoscopic
biopsy, bronchoscopic cytology,
bronchioalveolar lavage,
ultra sound/ CT guided FNAC, Lymph
node or Liver FNAC, open lung biopsy,
hormonal assay.
Normal lung, signs and symptoms,
investigations, atelectasis and
infections
Lung-1
Clinical features of lung diseases
Infections of lung
Clinical symptoms of lung
disease
Dyspnea - aware, obstruction,
pain
Cyanosis - >5-gm / dl reduced Hb
Clinical symptoms of lung
disease
Dyspnea - aware, obstruction,
pain
Cyanosis - >5-gm / dl reduced Hb
Chest pain- parietal pleura
Chest pain
Cardiovascular
Gastrointestinal
Respiratory
Chest wall
Clinical symptoms
Cough - dry, productive
Sputum - purulent, frothy
Hemoptysis - Tb, Carcinoma, Left
heart failure
Clinical signs of lung disease
Physical Examination of Chest:
movement - symmetry
accessory muscles of respiration
palpation
percussion
auscultation
Investigations:
Examination of sputum:
microbes
malignant cells
RBCs
Imaging:
Chest X- ray
CT scan
MRI
Bronchography
Arteriography
Investigations
Bronchoscopy:
visualize,
cytology
biopsy
broncho alveolar lavage
Investigations
Ventilation scan
Perfusion scan
Investigations
FNAC
Open lung biopsy
Pleural tap - exudate, neoplastic
cells, microbes
Pleural biopsy
Tests of pulmonary function
Arterial blood gases (increased
pCo
2
, decreased pO
2
)
Spirometry - Ventilatory function
Total Lung Capacity
Vital Capacity
Residual Volume
Tests of pulmonary function
Forced Vital Capacity - FVC
Forced Expiratory Volume in first
second - FEV1
FEV1 : FVC ratio (normal > 75%)
Respiratory failure
Fall in pO 2
Rise in pCO 2
Atelectasis
Incomplete expansion
or collapse of previously inflated
lung
Newborn
Atelectasis
Adult-------
Obstruction (resorption)-
asthma, chronic bronchitis,
aspiration
Compression- pleural fluid, air
(pneumothorax)
Contraction- fibrosis of lung
Microatelectasis
Pneumonia
Acute infection of lung
Fever, cough, dyspnea, chest pain
Lung- defense mechanisms
Mucociliary reflex, cough reflex,
alveolar macrophages
Non immune opsonins - surfactant,
fibronectin
Lung- defense mechanisms
Immune opsonins (alveolar
macrophages)
C3b, IgA, IgG
T lymphocytes normally in airspaces
Neutrophils (not normal), easily
recruited
Pneumonia-classifications
Primary, Secondary
Mode of infection- community,
hospital, aspiration
Site of action- alveolar space
(typical), alveolar wall (atypical)
Microorganism- Bacterial, Viral,
Chlamydia, Fungi etc
Pneumonia
Primary, Secondary
Primary pneumonia
Healthy person
Virulent organism
e.g. Strep. pneumonia, L. pneumophilia
Secondary pneumonia
Underlying abnormality predisposes
Postoperative (ventilation reduced)
Smoking (mucociliary reflex, aspiration
due to loss of cough and swallowing
reflex, pmn, macrophage, chemotaxis)
Preexisting lung disease - viral infection,
emphysema,bronchiectasis
Immunosuppression
Secondary pneumonia contd.
Bronchial obstruction- tumor, foreign
bodies
Coma - cough reflex lost
Alcoholics, diabetes
Pneumonia
Community acquired
Hospital acquired
Community acquired pneumonias
Healthy individual
Acute pneumonia- sudden illness-
Strep. pneum, H. influenza,
Moraxella catarrhalis, Legionella
Atypical pneumonia- mycoplasma,
chlamydia, viral (influenza),
rickettsiae
Hospital acquired pneumonias
Nosocomial
Gram negative-Klebsiella, E.coli,
Pseudomonas, Staph
Immunosuppression, antibiotics,
catheters, ventilators
Aspiration pneumonias
Acid
Organisms
Mixed nature of organisms
Immune abnormality and type of
organisms
CMI
viral, mycobacteria, low virulence -
Pneumocystis
Innate
pmn, complement and humoral
immunity -- pyogenic organisms
Pneumonia
Site of action-
alveolar space (typical)- airspace
alveolar wall (atypical)- interstitial
Airspace pneumonia
Types of pneumonia
Airspace pneumonia- Bacteria
Interstitial pneumonia -Virus
Bacterial pneumonias
Multiply extracellularly in alveoli
Inflammatory exudate in alveoli -
airless (consolidated)
Air space pneumonia Lobar Pneumonia:
Large confluent areas of
consolidation
Almost whole lobe
Bronchi not involved
Spread through pores of Kohn
Usually virulent organism- Strep.
pneumonia
Bronchopneumonia:
bronchi + surrounding alveoli
Patchy
Usually less virulent organisms
Bronchopneumonia
lesions are patchy, confluent
bronchi, bronchioles also damaged
intervening areas normal
less chances of pleuritis
Pneumonia: stages
Both lobar and broncho pneumonia
go through 4 stages if untreated
Antibiotics halt the process
Acute Congestion
heavy red boggy lungs
bacteria multiply in
alveoli, dilated alveolar
capillaries, early fluid
exudation
early PMNs + early red
cells
Red Hepatization
consistency liver like
lining alveolar cells lost
PMNs, fibrin, red cells
Pleuritis
infection controlled
Gray hepatization
dry, gray, firm
exudation and
hyperemia stop
red cells depleted
Resolution
Removal of exudate
complete resolution can occur because
structure of alveoli not damaged in
lobar pneumonia
Bronchopneumonia has structural
damage
Complications of pneumonia
Complications
Abscess (Staph.aureus, gm -ve
bacilli, type 3 pneumococci)
Empyema
Organization - scar tissue
Bacteremia - menigitis, arthritis,
endocarditis
Recurrent pneumonias , bronchiolitis
obliterans
Clinical - pneumonia
Abrupt high fever, cough, rusty
purulent sputum
Chest pain, pleural rub (if there is
pleuritis)
p air entry, consolidation, X- ray
Microbe - sputum, blood
Pneumococcal pneumonia
Settings- usually nil, viral infection,
CHF, COPD, immune
deficiency, splenectomy (auto)
Sputum - gram positive diplococci- normal
flora, look for intracellular in pmn
Blood culture - more specific
Vaccines
H. Influenzae pneumonia
COPD, cystic fibrosis, bronchiectasis
Common cause of acute exacerbation
of COPD
Moraxella catarrhalis
Elderly individuals
Second most common cause of
pneumonia in COPD
Klebsiella Pneumonia
Most frequent gram negative
pneumonia
Debilitated and malnourished
Chronic alcoholics
Thick gelatinous sputum ( viscid
capsular material)
Extensive destruction
Staph. aureus pneumonia:
After viral respiratory illness -
secondary
Hospitalized patients - primary
Abscess formation, empyema
i/v drug abusers- endocarditis
Penicillin resistance
Psuedomonas aeroginosa
Progressive necrotizing pneumonia
Nosocomial, neutropenic patients,
burns
Vasculitis and vascular spread
Extensive destruction, abscess
formation
Empyema
Cystic fibrosis
Legionella pneumonia
Sporadic, epidemic
Artificial water pools- tubing, cooling
towers
In chronically ill patients, post
transplant
High fatality
Culture- best for diagnosis, others-
sputum, urine
Quiz
10 questions
2 friends sitting together
9 correct each but one gets 9
other 8 points
Answer to Q.5-
I dont know
Neither do I
Types of pneumonia
Airspace pneumonia- Bacteria
Interstitial pneumonia -Virus
Interstitial pneumonia
Interstitial Pneumonias
(Atypical)
Infection by obligate intracellular
pathogens
Mostly community acquired
Sporadic - Mycoplasma pneumonia
(children, young adults),
chlamydiae, rickettsiae
Endemic Influenza
Immune Compromised - Herpes,CMV
AIDS - Pneumocystis
Usual Interstitial Pneumonia
Patchy lung involvement
Alveolar septa involved
Pathology interstitial pneumonia
Tracheo bronchitis ( nose to alveoli)
Attach to alveolar epithelial cells, kill
them, inflame alveolar septa
Alveolar septa - edema, hyperemia,
lymphocytes, plasma cells
Alveolar cells - necrosis, inclusions,
multinucleation
Pathology interstitial pneumonia
Hyaline membrane
Alveolar lumen clear (except in
pneumocystis cariini - frothy
exudate rich in organisms)
Prone for secondary bacterial
infection
Severe acute respiratory distress
syndrome-SARS
Mar 2003- China- Avian flu
Pathology similar
More necrosis and hyaline
membranes in fatal cases (ARDS)
Corona virus
Clinical interstitial pneumonias
Variable
Mild illness usually
Fever, cough- nonproductive, dyspnea
(sometimes out of proportion to
chest signs and radiology)
Very few clinical signs
Reticular shadows on chest X- ray
Clinical interstitial pneumonias
Organisms difficult to demonstrate,
check antibody titers
Treat with Erythromycin - covers
Chlamydia, mycoplasma which are
the common offenders
Complications: Secondary bacterial
pneumonia
Mycoplasma pneumoniae
Children, young adults
Endemic
Diagnosis- Mycoplasma Ag or PCR for
Mycoplasma DNA
Rising titers of antibodies - takes
time to demonstrate
Lung infections
Lung abscess
Lung abscess
Chronic Lung Abscess
1. Sequela of acute suppurative
pneumonia (Staph. Aureus,
Klebsiella, Pseudomonas)
2. Bronchial obstruction - foreign body
(inhalation, aspiration), tumor
Lung abscess
3. Bronchiectasis
4. Secondary infection on tuberculous
cavity
5. Septic embolus from infective
endocarditis right heart
Abscess single vs multiple
Aspiration of infected material
Single , right side
Apical portion of lower lobe or
subapical, axillary portion of
upper lobe
Secondary to pneumonia or septicemia
or bronchiectasis - multiple
-
Lung Abscess - Clinical
Copious, foul sputum, hemoptysis,
fever, malaise
Complications bronchopleural
fistula, empyema, septicemia,
amyloidosis
Treat with antibiotics, drainage
Pneumonia not responding to
treatment
Bronchiectasis, lung abscess
Lung tumor- hilar obstruction,
bronchioloalveolar carcinoma
Vasculitis
Lung
Vascular and hemodynamic
pathology
Pulmonary edema- Passive
Left ventricular failure
Excess IV fluids
Severe hypoproteinemia
Lymphatic obstruction (carcinoma)
Pulmonary edema--Active
Damage to vascular endothelium
(ARDS)
Capillaries and venules
Exudate into interstitium and lumen,
hyperemia
Direct injury
Infections
Toxic gases
Corrosive liquids (aspiration)
Drugs like cancer chemotherapy,
heroin, cocaine
Oxygen toxicity, noxious fumes,
weed killers - paraqat poisoning
Indirect injury
Severe trauma (hemorrhage, shock),
septic shock (endotoxemia)
Severe burns
Acute pancreatitis, post surgery
(abdominal)
Adult ( Acute)Respiratory
Distress Syndrome (ARDS)
Syn. Shock Lung Syndrome, Acute
lung injury, Diffuse alveolar
damage (DAD), Acute lung injury
(ALI)
(cf. RDS in neonates due to
deficiency of surfactant)
Shock lung
Endothelial damage, damage to type
1 pneumonocytes
Exudate, impaired gas exchange
Hyaline membrane (necrotic debris
from epithelial cells plus edema
fluid coagulate)
Type II pneumonocyte necrosis- loss
of surfactant- microatelectasis
Mechanism of damage
Imbalance between pro and anti
inflammatory cytokines
Macrophages -> IL8 -> pmn chemotaxis and
activation
IL-1,TNF -> pulmonary vascular
sequestration of pmn and exude into
septa and lumen
PMNs, macrophages -with leukotrine B4
Mechanism of damage
Alternate pathway of complement,
tumor necrosis factor (TNF) tissue
thromboplastin
If hyperbaric oxygen -> further damage
TGF-,PGDF -> promote fibrosis
Clinical features
Respiratory difficulty- acute
Gasping for breath
Severe hypoxemia, cyanosis
Bilateral infiltrates on chest X-ray
Absence of clinical features of LVF
Predisposes to infections
High mortality
Nitric oxide- NO- inhalation reduces PA pressure
and resistance
Healing may result in diffuse interstitial fibrosis
Phases of ARDS
Exudation- 0-7 days
Proliferation - 1-3 weeks
macrophages phagocytose dead
cells and hyaline membrane, type
II pneumonocytes proliferate
mature in to type I cells
Fibrosis- TGF-, PDGF
SARS
Acute respiratory distress syndrome
due to infection
Corona virus
China, Hongkong, Singapore, Canada
Pulmonary embolism
95% from deep leg veins
Sick, bedridden patients with
pulmonary, cardiovascular disease
BIG -> bifurcation of PA, sudden
death from acute right heart
failure - no time to develop any
changes in lungs
Pulmonary embolism
MEDIUM -> hemorrhage, infarction
only if circulatory status already
compromized
SMALL -> usually no infarct because
of dual supply, resolve ( lysis),
if recurrent- pulmonary hypertension
Infarction
Clinically resembles myocardial
infarction - chest pain, dyspnea,
shock
Gross: Wedge shaped, hemorrhagic
infarct, may be multiple
Micro: coagulation necrosis
Pulmonary hypertension
Primary-
Rare, young women,recurrent dyspnea
,syncope
Reynauds phenomenon (vasopasm
of peripheral vessels)
? Neurohormonal hyperactivity
? Vasotropic virus- HSV 8
Pulmonary hypertension
Secondary
COPD - Chronic bronchitis,
emphysema, diffuse fibrosis
Congenital shunts- VSD
Recurrent pulmonary
thromboembolism in small sized
vessels
Morphology of pulmonary
hypertension
Changes in medium sized arteries
Medical thickening
Intimal hyperplasia / fibrosis
Reduplication of elastica,
Morphology of pulmonary hypertension
Plexogenic changes in severe
varieties only (primary)
Necrosis of wall (fibrinoid)
Thrombosis
Rupture, bleed
Dilation lesions, angiomatoid
lesions
Hemosiderin
Primary pulmonary hypertension-
clinical
Symptoms appear late
Fatigue, dyspnoea
Syncope on exercise
Chest pain
Respiratory insufficiency, cyanosis
Cor pulmonale
Goodpasture syndrome
Hemoptysis, oliguria, hematuria
Pulmonary alveolar hemorrhages,
hemosiderin
Rapidly progressive
glomerulonephritis- linear
immunofluorescence
Antibodies targeted against collagen
IV- basement membrane
Lung
Restrictive lung disease
Extrinsic
Chest wall injury,deformity
( kyphoscoliosis)
Severe obesity
Neuromuscular (Guillain Barre
Syndrome)
Intrinsic
Acute - ARDS
Chronic-
Idiopathic Pulmonary Fibrosis ( IPF )
Bronchiolitis obliterans
Pneumoconiosis
Sarcoidosis
Hypersensitivity pneumonitis
Restrictive lung disease
Introduction
Lung stiff, hard, difficult to expand
Diffusion across blood air barrier is
difficult
Referred to as interstitial lung disease
Restrictive lung disease
Acute - Adult respiratory distress
syndrome (vascular)
Chronic - many entities
FEV
1
p, FVC p, FEV
1
: FVC ratio
normal
Restrictive lung disease
Idiopathic- pulmonary fibrosis-IPF
Occupational- inorganic-
pneumoconiosis, organic-
hypersensitivity pneumonitis
Drug- chemotherapy, radiation,
oxygen therapy
Immunological- autoimmune
diseases, sarcoidosis
Idiopathic pulmonary fibrosis
(Hamman Rich Syndrome) (Honey
comb Lung)
Cause not known
Diffuse fibrosis in alveolar septa
M > F
> 60 years age
Idiopathic pulmonary fibrosis
Immunological damage (responds to
steroids)
Probably starts as alveolitis
damage to type I epithelial cells
Proliferation of type II cells - attract T
cells, macrophages
Idiopathic pulmonary fibrosis
Type II cells-
Replace type I cellls
Secrete chemotactic factors for
macrophages, T cells
Contribute to fibrosis by secreting
PDGF and TGF-
Pathology - IPF
Early - edema, hyaline membrane,
mononuclear cells in septa
necrosis of type I cells
Later - type II cells - cuboidal cell
hyperplasia
Lymphocytes, plasma cells, macrophages
Septal fibrosis
Honey comb lung
Clinical IPF
Progressive dyspnea, hypoxia,
cyanosis, pulmonary hypertension
Bilateral basal lesions
CT- early detection of IPF, exclude
other causes of pulmonary fibrosis
subpleural wedge biopsy- image
guided
Clinical IPF
Cor pulmonale- JVP, edema
Progression- variable
Death in 2-4 years
Similar end result in many ->
rheumatoid arthritis, systemic
sclerosis, SLE etc.
Variants
Unusual interstitial pneumonia
Desquamative interstitial pneumonia
(DIP)
(Alveolar macrophages aggregate)
Lymphocytic interstitial pneumonia
(LIP)
(Psuedo lymphoma)
Bronchiolitis
Idiopathic
Organizing fibrosis in bronchioles
Cigarette smoke settling on respiratory
bronchioles and setting up
inflammation and fibrosis
If lumen obliterated- obstructive
features also- bronchiolitis obliterans
Sarcoidosis -
In the lung - restrictive disease
Multisystem involvement,
noncaseating epitheloid
granulomas
Differentiate from Tb, berylliosis,
fungal infections
Cell mediated hypersensitivity to
some unidentified antigen
Sarcoidosis
Lymph nodes, lungs, skin, eye,
spleen, liver etc
Asteroid bodies, Schaumann bodies
- suggestive but not diagnostic
Sarcoidosis
May be associated with
hypercalcemia (activation of vit. D
by epitheloid cells)
Raised serum angiotensin
converting enzyme (ACE) - 60%
Sarcoidosis
Mikulicz Syndrome - Parotid,
sublingual, submaxillary, Uveal
Bilateral uniform enlargement
Sarcoid, lymphoma-leukemia,
Sjogrens syndrome
Hypersensitivity pneumonitis
Allergic alveolitis (not bronchioles)
Granulomas in alveolar walls, less
fibrosis
Acute (type III) or Chronic (type IV)
Irritation, complement, immune
complex damage
Farmers lung (hay), Bagassosis
(sugar cane), Pegion breeders
lung etc.
Hypersensitivity lesions
Size of particles
Hay fever (type I)
Bronchitis / asthma
Bronchiolitis obliterans
Pneumonitis (type III,IV)
Diffuse pulmonary hemorrhage
(Good Pastures Syndrome)
Lung hemorrhage + acute
glomerulonephritis
Antibody to basement membrane
(linear immunofluoroscence)- type II
Hemoptysis + nephritic illness
Triad- hemoptysis, anemia, diffuse
pulmonary infiltrates
Goodpastures syndrome
Oliguria, hematuria, hypertension
Progressive dyspnea, right heart
failure
Treat by plasmapheresis,
immunosuppression
Idiopathic pulmonary hemosiderosis
Younger patients
Cause not known - no antibodies, no
renal involvement
Recurrent hemorrhage, fibrosis
Pneumoconiosis
(Revise environmental pathology)
Anthracosis, silicosis, asbestosis,
berylliosis -> Restrictive lung
disease
Other causes of interstitial fibrosis
Anticancer drugs- busulfan,
methotrexate, cyclophosphamide
Paraquat (herbicide)
Radiation pneumonitis
Toxic gases
Intravenous heroin (contaminants)
Other causes of Interstitial fibrosis
Autimmune disorders- SLE,
rheumatoid arthritis, scleroderma
Wegener's granulomatsis- pulmonary
angiitis and granulomatosis-
sinusitis, lung involvement, kidney
involvement, c-ANCA
Lung
Chronic obstructive pulmonary
disease (COPD, COAD)
COPD
Common disease
There is chronic obstruction to flow
of air.
COPD
Chronic obstruction to flow of air
Common disease; 4th leading cause of deaths in the
US; 3rd most common cause of death worldwide by
2020
Once principally a disease of men, it now affects men
and women equally
In 2000, COPD was responsible for 8 million physician
office visits, 1.5 million emergency department visits,
and 726,000 hospitalizations (about 13% of total
hospitalizations)
Second only to coronary heart disease as a reason for
payment of Social Security disability benefits.
NEJM March 2009
Case Vignette
A 61-year-old woman is referred for pulmonary
consultation.
She smoked one pack of cigarettes a day for 45 years but
quit a year ago.
For 2 years she has noted progressive exertional dyspnea,
with breathlessness occurring when she is walking up one
flight of stairs or hurrying on level ground.
A diagnosis of chronic obstructive pulmonary disease
(COPD) was made a year ago, and she was treated with
inhaled medications.
Casaburi R, ZuWallack R. N Engl J Med 2009;360:1329-1335
She is sedentary and recently gained 15 lb
(6.8 kg); her only frequent social activity is
playing cards.
Her physical examination is normal except for
a weight of 195 lb (88.5 kg) (body-mass index
[the weight in kilograms divided by the square
of the height in meters], 32) and for
decreased breath sounds and prolonged
expiration on chest auscultation.
Spirometry reveals moderate airway
obstruction; an echocardiogram is normal.
Obstructive lung disease
Reversible- Bronchial asthma
Irreversible- Chronic bronchitis,
emphysema, bronchiectasis
Obstructive lung disease
Total lung capacity (TLC)- increased
Forced vital capacity(FVC)- Normal or
decreased
FEV-1 reduced
So FEV1 : FVC ratio reduced (<75%)
Chronic Obstructive
Pulmonary Disease-COPD
Emphysema and Chronic bronchitis
are the two main conditions causing
COPD
Definition of Emphysema is based on
morphological changes that occur
and the definition of Chronic
bronchitis is based on clinical
features
Emphysema
Permanent enlargement and
destruction of airspaces beyond
terminal bronchioles ( not just
overinflation )
There is no real obstruction for a
long time after the disease starts
and hence no symptoms develop.
When symptoms develop it means
obstruction has occurred.
Emphysema
Permanent dilation of terminal air
spaces with destruction of their
wall.
Elasticity lost, cannot recoil to expel
air
( Inspiration is active, expiration is
passive).
Emphysema
Elderly males with dyspnea (after
significant damage). No organic
obstruction - only failure of recoil.
May develop chronic bronchitis in
addition.
Types of emphysema
Normal
Septal
Centriacinar
Panacinar
Emphysema-Types
1 Centriacinar ( Centrilobular)
2 Panacinar ( Panlobular)
Distinction possible in early stages and
not in late stages.
Centrilobular emphysema
Damage is at respiratory bronchioles
(central and proximal part of
acinus)
Distal alveoli spared,
Common in upper lobes (apex)
Panacinar emphysema
Uniform enlargement from respiratory
bronchioles, alveolar ducts and alveoli,
Common in lower lobes.
Pathogenesis of emphysema
Excessive protease (Elastase) + less anti
protease
1. Alpha -1- antitrypsin deficiency (2%
of all emphysema)
Polymorphic Pi ; Pi MM normal, PiZZ
worst
2. Neutrophils release elastase
(e.g. cigarette smoking)
Cigarette smoking
Cigarette smoke particles lodge at
bifurcation of respiratory
bronchioles
Engulfed by macrophages which
release elastase
This elastase is not inhibited by
A1AT and can digest the A1AT
Cigarette smoking
Cigarette smoke also contains oxidants
These oxidants along with free oxy
radicals released by pmn.s inhibit A1AT
Pathology of emphysema
Panacinar - Large, pale,voluminous
lungs, cover the heart
Centriacinar - no gross changes
Micro: alveoli large, wall
thin, destroyed
Pathology of emphysema
terminal and respiratory bronchioles
deformed
loss of tethering by surrounding
alveoli leads to obstruction in
expiration
Emphysema- Clinical
Symptoms appear late
Barrel chest, dyspnea, prolonged
expiration
X- ray flat domes of diaphragm
Hyperventilation oblood gases normal till
late
Pink Puffers,
Late stage - hypoxia, respiratory acidosis
Emphysema
Usually the patients are weak and
skinny
Weight loss because of excess
puffing and panting due to hyper
ventilation
Emphysema- Clinical
Hypoxia and hypercapnia
Pulmonary vasoconstriction,
compensatory polycythemia
Loss of pulmonary capillary surface
area from alveolar destruction
Pulmonary hypertension
Cor pulmonale ( RVH, RVD,RVF )
Death in emphysema
Respiratory failure - acidosis, hypoxia,
coma
or
Cor pulmonale
Other types of emphysema
Compensatory : eg. Pneumoconiosis
Senile
Obstructive overinflation : tumor,
foreign body-- danger of collapse
of rest of lung, pneumothorax due
to rupture
Mediastinal emphysema
Air escapes in to the connective tissue
of lung stroma, mediastinum and
subcutaneous tissue
Sudden increase in intra alveolar
pressure
violent cough, vomiting, whooping cough,
trauma usually with some obstruction to
the bronchial passage- eg mucus plug
tear in the interstitium
Mediastinal emphysema
Patient bloats suddenly like a balloon
including chest head and neck
Crackling crepitations over chest
wall
Recovers spontaneously after the
defect is sealed
Chronic bronchitis
Cigarette smokers, smoke in city
Persistent productive cough for at
least 3 consecutive months in at
least 2 consecutive years.
Types: Simple , mucopurulent ,
asthmatic ,obstructive
Pathogenesis
Irritation oExcess secretion by
mucus glands ohypertrophy of
glands oMetaplastic goblet cells
in surface epithelium, secondary
bacterial infection.
Inflammation and fibrosis o
obstruction of small airways
Superimposed emphysema.
Pathology
Externally lungs appear normal
Large airways - hyperemia, edema,
mucous secretion
Chronic bronchitis - bronchi
hypertrophy and hyperplasia of
mucous glands
(Reid Index > 0.5)
Goblet cells in the surface epithelium
Squamous metaplasia
Chronic bronchitis - bronchioles
Goblet cell metaplasia
Inflammation
fibrosis (collapse in expiration)
smooth muscle hyperplasia
Chronic bronchitis - Clinical
Definition
Eventually small airways obstruction
pO
2
p, pCO
2
n, Cyanosis
Blue bloaters (edema due to heart
failure)
Pulmonary hypertension, Cor
pulmonale
Secondary infections
Chronic bronchitis
Persistent hypercapnia makes
respiratory centers insensitive to
pCO
2
stimulus
Respiration is now driven by low O
2
If you administer oxygen othe drive
is lost and they die of CO
2
narcosis
Exercise intolerance resulting from dyspnea
or fatigue is often the chief symptom reported
by patients with COPD.
The degree of exercise intolerance roughly
parallels the severity of the disease, but
exercise intolerance is also distinctly present
in patients with only mild disease.
The extent to which quality of life is impaired
is reflected in patients' symptoms, decreased
functional status, and frequency of
exacerbations.
Pathophysiology
Extrapulmonary effects
Skeletal muscle dysfunction (legs)
Low type 1 fibres; early onset of lactic
acidosis
Fatigue leads to decreased ambulation
rather than dyspnea
Effects of therapy
Pulmonary rehab doesnt improve lungs
Optimizes function of the rest of the body
Effect of lung dysfunction on the rest of the
body is minimized
Decreased lactic acidosis, decreased
ventilatory demand
Bronchial asthma
Sudden attacks of respiratory distress
Expiratory dyspnea
Wheezing / Rhonchi
Episodic
Relieved spontaneously or by
bronchodilators
Thick sputum
Bronchial Asthma
Hypersensitivity of tracheobronchial
tree
Bronchiolar smooth muscle spasm
Bronchial inflammation precipitates
the hyper reaction of bronchial
tree
Bronchial inflammation is now
considered the important feature
Types of asthma
Intrinsic
Extrinsic
Final mechanism of damage similar
and hence the distinction may not
be that relevant
Types of asthma - extrinsic
3 types
Atopic
Occupational
Allergic bronchopulmonary
aspergillosis
Intrinsic asthma (nonallergic)
Precipitated by
Cold
Aspiration
Viral infection
Psychological
Exercise induced
Extrinsic (Atopy)
(Type I hypersensitivity)
Childhood, familial, serum IgEn,
sensitivity to many antigens
Raised eosinophils in blood
Older patients serum IgE normal
Genesis
CD4 cells of Th2 subtype release IL
4,5,13
These favor synthesis of IgE, growth
of mast cells and growth and
activation of eosinophils
Genesis early phase
Early Phase starts in 30-60 minutes of
exposure and lasts up to 4-6 hours
Antigen + IgE on mast cells in mucosa
Release Histamine, bradykinin,
Leukotreines, Prostaglandins,
platelet activating factors
Bronchoconstriction, acute
inflammation, thick mucus
Genesis early phase
Epithelial damage
Opens the intercellular junctions
Antigens get in
Sensitize mast cells in submucosa
Aggravation of reaction
Stimulation of submucosal vagal
fibers leads to reflex smooth
muscle contraction
Eosinophils
Eosinophils attracted by IL5, PAF
(mast cells), eotaxin (epithelial
cells)
Amplify and sustain the reaction.
Recruitment of pmn.s, basophils,
eosinophils, CD4 cells
Eosinophils
Have granules like mast cells
The granules contain eosinophil
cationic protein and myelobasic
protein which are toxic to
epithelial cells
Late phase
Epithelial cells secrete- endothelin and
Eotaxin
Lead to smooth muscle contraction
Late phase
Eosinophils produce Leukotreines
C4,PAF activate mast cells
Cytokines activate myofibroblasts to
lay down more collagen in the
basement membrane
Genesis
Microenvironment of brochial tree-
altered due to genetic mutations in
metalloproteinases- ADAM-33
This precedes the development of
asthmatic attacks and may predispose
to it
Effects of Asthma
Obstruction, more in expiration
(wheeze)
FEV-I < 30%, hyperventilation
Hypoxia, hypercapnia, respiratory
acidosis
Asthma - lungs
Occlusion of bronchi, bronchioles by
thick tenacious mucus
Overinflated lungs
Asthma lungs- micro
Eosinophils, mucus plugs in lumen
Inflammation- eosinophils, mast
cells, basophils, macrophages,
CD4 lymphocytes, neutrophils
Edema
Asthma lungs- micro
Thick basement membrane
Patchy necrosis and shedding of
epithelial cells
Hypertrophy of submucosal glands and
increase in goblet cells in bronchial
lining
Hypertrophy of smooth muscle
Asthma - Clinical
Short, acute attacks - Expiratory
dyspnea, wheeze, dry cough
Thick stringy mucus, casts,
(Curschmans spirals)
Charcot Leyden crystals
Asthma - Clinical
Respond to bronchodilators
Skin tests - desensitize
Status asthmaticus (severe,
prolonged)
Asthma - management
Acute attacks-
bronchodilators
Steroid inhalers (anti-inflammatory)
Antihistamines
Leucotrine blockers ( Accolate)
Prevention , Desensitization
Bronchiectasis
Permanent, abnormal, irreversible
dilatation of bronchial tree
proximal to terminal bronchioles
Result of chronic infection o
destruction, fibrosis, dilatation.
Causes
Obstruction - tumors, foreign bodies
Mucoviscidosis (cystic fibrosis)
Necrotizing bronchopneumonia
(Sequela to measles,Whooping cough)
Kartageners syndrome
Kartageners syndrome
ciliary abnormality of microtubules
1/3 also have dextrocardia called
Kartageners syndrome
upper respiratory Infections + sterility
in male + Dextrocardia (loss of
ciliary action during embryogenesis)
Pathology of bronchiectasis
Localized or generalized
Cylindrical, fusiform or saccular
Bronchi reach up to pleura
Walls inflamed, fibrosed, ulcerated,
purulent
Lung abscess
Bronchiectasis - Clinical
Productive cough
Large amount foul sputum
Episodic fever
Clubbing of fingers
Pulmonary hypertension, Cor
pulmonale
Amyloidosis
LUNG -Neoplasms
Lung tumors
Secondary
Primary
Lung tumors
Secondary multiple (Cannon balls)
peripheral
rarely lymphangitis carcinomatosa,
peribronchial, (perivascular,
lymphatics)
restrictive lung disease
Primary
Bronchial epithelium - 95%
5% Carcinoid, mesotheliomas,
bronchial gland, mesenchyme,
lymphoma
Hamartomas (coin lesion, cartilage,
fat, blood vessels)
Bronchogenic carcinoma
No. 1 cause of cancer deaths in the
U.S.
No. 1 cause of cancer deaths in
females also
Cigarettes smoking : 10 times more
common in smokers, 40 - 70 years
age group
Classification
1. NSCLC - Non Small Cell Lung
Carcinoma (70-75%)
Squamous Cell Carcinoma (25- 30%)
Adeno Carcinoma (30- 35%)
Large Cell Carcinoma (10-15%)
2. SCLC - Small Cell Lung Carcinoma
(20-25%)
3. Combined Patterns
Etiopathogenesis
SCLC myc amplification, p53, Rb
deletion short arm of chr 3 (3p 14-25)
(tumor suppressor genes)
NSCLC = K- ras
Field of exposure - metaplasia,
atypical hyperplasia, dysplasia,
Carcinoma insitu, invasive
carcinoma
Smoking and lung cancer
evidences
STATISTICAL - Pack years -
Heavy Smokers vs Nonsmokers- 20
times
15 years after stopping smoking - risk
normal
Passive smoking (x2)
Smoking
CLINICAL -
Epithelial changes in sequence
EXPERIMENTAL - Missing link
Smoking
Why all exposed to smoking do not
develop cancer?
Genetic predisposition. (P-450
mono-oxygenase systems for
activation of mutagens)
What is it in smoking? Polycyclic
hydrocarbons?
Others ( > 1200 elements identified)
Other etiologies
Asbestos - (x55)
Radioactive ore mining
Arsenic, Uranium
General features
Majority HILAR
Smoking - special relation to
Squamous cell, Small cell
Aggressive infiltration
Metastasis: Liver, Adrenal,
brain,bones,kidneys
Paraneoplastic Syndrome (specially
SCLC)
Squamous cell carcinoma
Male > female
Central (hilar) location
Hilar lymph nodes
Cumulative pre cancerous histologic
changes
Obstruction, atelectasis, infection
Adenocarcinoma
Younger age < 40 years
Women, Non smokers
Peripheral (coin lesion)
May relate to scars (infarct,
granuloma, TB, diffuse fibrosis)
Scar carcinomachronic scarring
leading to carcinoma
Adenocarcinoma
AAH- atypical adenomatous
hyperplasia
? Precursor of adenocarcinoma
Is there a spectrum from AAH-
bronchoalveolar carcinoma to
frank adenocarcinoma?
Distinguish from scar caused by
cancer
Slow growth
Early metastasis
Types= Glandular (mucin) and
Bronchioloalveolar (papillary)
Bronchiolo alveolar carcinoma
Multiple coalescing nodules -
pneumonia like, alveolar growth
pattern
Tall columnar cells with mucin
Arise from surfactant producing type
II pneumonocytes
(South African sheep - infection -
Jagziekte shows similar features)
Large Cell Carcinomas
Squamous or Adeno
with no differentiation
Poor prognosis, early
metastasis
Small Cell Carcinomas
Male > females
Related to Smoking
Hilar location
Cells resemble lymphocytes (oat
cells)
Frequent mitosis
Oat cell carcinoma
Frequent vascular invasion
Infiltrate and metastasize widely
Not resectable
Responsive to chemotherapy
Neuro endocrine origins
(Paraneoplastic Syndromes)
Oat cell carcinoma
Neuron Specific Enolase,
Neurosecretory granules
Neurofilaments, Polypeptidie
Hormones
ACTH, Calcitonin, Gastrin Releasing
Polypeptide etc.
Spread of lung cancer
Infiltration lung, pleura, pericardium,
Superior venacava (SVC),
Sympathetic plexus,
Lymph nodes (Carina ,
Mediastinal,Scalene, Supra
clavicular)
Virchows LN
Spread of lung cancer
Vascular - liver, adrenal, brain, bones
TNM classification
Clinical features
Peripheral- may be clinically silent
Hilar (Central)-
Obstruction- partial or total
Infection- pneumonia, abscess,
bronchiectasis
Atelectasis
Clinical features
Cough, weight loss, hemoptysis,
dyspnea
Pulmonary osteoarthropathy -
(clubbing)
Hoarseness, chest pain
Pericardial and pleural effusion
Clinical features
Persistent atelectasis, pneumonitis
(obstruction)
Suprior vena cava (SVC) syndrome due
to obstruction
Horners Syndrome: Cervical
sympathetic plexus damaged
Ipsilateral enophthalmos, ptosis,
meiosis, anhidrosis
Clinical features
Pancoasts syndrome (apical
neoplasm) T
1
T
2
destruction
wasting of hand muscles, pain in
arms
Recurrent laryngeal nerve paralysis
Esophagus involvement- dysphagia
Thoracic duct obstruction-
chylothorax
Clinical features- metastasis
LN mets most common
Adrenal (50%)-very rarely
Addisons (insufficiency)
Liver (30-50%) hepatomegaly
Brain (20%) mental, neurologic
Bone (15-20%) Pain, fracture
Kidney- (15%)
Prognosis in lung cancer
SCLC carries worst prognosis
Usually metastasis by the time of
detection
Median survival l year
Chemotherapy for SCLC
Lobectomy or pneumonectomy for
NSCLC if localized
Paraneoplastic syndromes
10% of all lung cancers(SCLC)
Hypercalcemia (PTH)- more with
squamous cell carcinomas
Cushings (ACTH) obilateral adrenal
hyperplasia
Syndrome of inappropriate
ADHsecretion oHyponatremia
Gonadotropins - gynecomastia
Paraneoplastic syndromes
Neuropathy, myopathy
Clubbed fingers, hypertrophic
pulmonary osteoarthropathy
Migratory thrombophlebitis
DIC, nonbacterial thrombotic
endocarditis ( NBTE) more
common with adenocarcinoma
Carcinoid tumor
Cells look like carcinoma cells but are
not truly carcinoma cells because
they do not arise from epithelial
cells
Arise from Neuroendocrine
(Kulchitsky) cells
Carcinoid tumor
Belong to the APUD cells system (Amine
Precursor Uptake
Deamination)
Part of a widespread system
Neuro secretory granules seen in the
cytoplasm
? Precursor lesion in the form of local or
diffuse neuroendocrine hyperplasia
? Carcinoid tumor is a precursor for Small
cell carcinoma
Carcinoid tumor
Usually localized
Located in the main bronchi (Hilar)
Resectable
Age group of 40 years
Carcinoid tumor
Growth oPolypoid,may grow in and
out of bronchial wall- collar button
Micro:- uniform round cells in nests,
no pleomorphism or mitosis
Nuclei not hyperchromatic
Carcinoid tumor- death
Pneumonia
Lung abscess
Bleeding
Carcinoid tumor - clinical
Obstruction - cough, hemoptysis,
infections (Hilar location)
May be incidentally detected
Carcinoid Syndrome may be
produced
Good Prognosis- usually benign
Rare metastasis
Carcinoid syndrome
1% of all Carcinoid tumor patients
show carcinoid syndrome
Symptoms due to high 5HT, 5HIAA in
blood and urine (produced by the
tumor cells)
Others may be histamine, bradykinin,
prostaglandins
Carcinoid tumor
Lung carcinoids osecrete into
systemic circulation (produce
symptoms of the syndrome)
Carcinoid tumors occur in the gut
also
Carcinoid syndrome
Gut carcinoidsosecrete into portal
circulation oLiver metabolizes the
secretions (no symptoms)
If metastasis to liver from gut
carcinoids - secretions from the
tumor cells in the liver get into
circulation - carcinoid syndrome
produced
Systemic fibrosis
Heart involvement
gut carcinoids - right ventricle
endocardium, pulmonary and tricuspid
valve ;
bronchial carcinoids -
Left ventricle
Retroperitoneal fibrosis
Hamartoma - Lung
Made up of cartilage, blood vessels,
fat, spaces lined by bronchial
epithelium
Silent clinically, picked up
incidentally by X- ray
Peripheral location- Coin lesion
Resection cures it
Coin Lesions
Peripheral nodular lesion picked by by
X-ray chest
peripheral adenocarcinoma
hamartoma
inflammation
FNAC to make a diagnosis
Mesothelioma
Asbestos (shipyards, miners,
insulators)
25 - 40 years
Asbestos + Smoking oIncreased
bronchogenic carcinoma not
increased risk for mesothelioma
Amphibole variety not serpentine
Mesothelioma
Fibers stay in the body for life
Preceded by - Extensive pleural
fibrosis, plaque formation
Pleural effusion, spread along pleura
Yellowish firm gelatinous encasement
Obliterates pleural space
Mesothelioma
Metastasis rare but infiltrates lungs and
thoracic wall
Micro: Combination of epithelial
(adenocarcinoma) and connective
tissue (sarcoma) elements
Nasopharyngeal carcinoma
Common in Chinese (? Genetic)
EBV - genome in all of them
Occult primary-usually presents as
metastatic lymph nodes in the
neck
Nasopharyngeal carcinoma
Squamous cell carcinoma
Poorly differentiated carcinoma
(EBV)
Lympho epitheliomas
radiosensitive
Carcinoma larynx
M: F 7:1
Smoking, alcohol, asbestos
Squamous cell carcinoma
Intrinsic, Extrinsic (extended outside
larynx)
Carcinoma larynx
Clinical: Hoarseness, pain,
dysphagia, hemoptysis
Infection of lung
60% localized oresect
Investigations for lung cancer
Sputum (can detect overt and occult
cancer)
X-ray, CT
Pleural fluid tap
Pleural biopsy
Investigations for lung cancer
Bronchoscopy
Bronchoscopic cytology, biopsy
Bronchoalveolar lavage
Investigations for lung cancer
Ultrasound / CT guided FNAC
Open lung biopsy
Lymph node, liver FNAC
Hormonal assay- ( paraneoplastic
syndrome )
You might also like
- Journal Reading PulmonologiDocument21 pagesJournal Reading PulmonologiGina ArianiNo ratings yet
- Approach To Interstitial Lung Disease 1Document33 pagesApproach To Interstitial Lung Disease 1MichaelNo ratings yet
- Expt. 26 Lung Volumes and Capacities (A)Document5 pagesExpt. 26 Lung Volumes and Capacities (A)api-3769252100% (2)
- Community-Acquired Pneumonia: Strategies for ManagementFrom EverandCommunity-Acquired Pneumonia: Strategies for ManagementAntoni TorresRating: 4.5 out of 5 stars4.5/5 (2)
- IDSA-ATS - Consensus Guidelines On The Management of CAP in AdultsDocument46 pagesIDSA-ATS - Consensus Guidelines On The Management of CAP in AdultscharliedelNo ratings yet
- Adrenal Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandAdrenal Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Interstitial Lung Disease Slide ShareDocument18 pagesInterstitial Lung Disease Slide ShareEmma E. Vincent100% (1)
- COPD Lecture Slides For BlackBoardDocument52 pagesCOPD Lecture Slides For BlackBoardClayton JensenNo ratings yet
- Copd Exacerbations in EdDocument23 pagesCopd Exacerbations in EdEzequiel MenesesNo ratings yet
- Interstitial Lung Diseases (ILD)Document17 pagesInterstitial Lung Diseases (ILD)Rashed ShatnawiNo ratings yet
- Cardiovascular Disease Risk FactorsDocument22 pagesCardiovascular Disease Risk FactorsCornelius OgegaNo ratings yet
- Diffuse Parenchymal Lung DiseaseDocument36 pagesDiffuse Parenchymal Lung DiseaseVeerapong Vattanavanit100% (1)
- Chalasani Et Al 2018 HepatologyDocument30 pagesChalasani Et Al 2018 HepatologyAlex DcostaNo ratings yet
- Cirrhosis and Its Complications Evidence Based TreatmentDocument20 pagesCirrhosis and Its Complications Evidence Based TreatmentSucii Sekar NingrumNo ratings yet
- Discuss The Management of Septic ShockDocument38 pagesDiscuss The Management of Septic ShockKelvin Obiano100% (1)
- Asthma COPDDocument81 pagesAsthma COPDBeby NajlaNo ratings yet
- Evaluation of Liver FunctionDocument64 pagesEvaluation of Liver FunctionMustafa KhandgawiNo ratings yet
- 1 Cell Counts and Leucocyte Differential CountDocument58 pages1 Cell Counts and Leucocyte Differential CountGloria Grace100% (1)
- Lung Ultrasound For Neonatal Cardio-Respiratory Conditions: Daniele de Luca (MD, PHD)Document52 pagesLung Ultrasound For Neonatal Cardio-Respiratory Conditions: Daniele de Luca (MD, PHD)Claudia Kosztelnik100% (1)
- Approach To The Adult With Interstitial Lung Disease Clinical Evaluation UpToDateDocument31 pagesApproach To The Adult With Interstitial Lung Disease Clinical Evaluation UpToDatePablo Souza100% (1)
- Hepatotoxic Drugs: Direct, Indirect and Immune Reaction TypesDocument17 pagesHepatotoxic Drugs: Direct, Indirect and Immune Reaction Typesani bandasoNo ratings yet
- Respiratory DiseasesDocument2 pagesRespiratory Diseasessarguss14No ratings yet
- Patient with fever: Causes and typesDocument46 pagesPatient with fever: Causes and typesNosheen hafeez100% (1)
- Salmonella: Praveen Rao, Sophia W. Riccardi, Danielle Birrer Seminar in Nucleic Acids-Spring 2004 Prof. ZubayDocument125 pagesSalmonella: Praveen Rao, Sophia W. Riccardi, Danielle Birrer Seminar in Nucleic Acids-Spring 2004 Prof. ZubayPaolaForeroNo ratings yet
- MBChB Year 5 Surgery: Arterial AneurysmsDocument1 pageMBChB Year 5 Surgery: Arterial AneurysmsJason HarryNo ratings yet
- Clinpharm SGD Bronchial AsthmaDocument9 pagesClinpharm SGD Bronchial AsthmaBea SamonteNo ratings yet
- Cardiovascular System: Mungcal, Dharlynette RTRPDocument77 pagesCardiovascular System: Mungcal, Dharlynette RTRPDharlyn MungcalNo ratings yet
- 2D2016 3.4-2 Azotemia and Urinary Abnormalities (Harrison's)Document7 pages2D2016 3.4-2 Azotemia and Urinary Abnormalities (Harrison's)elleinas100% (1)
- Interstitial Lung Disease Diffuse Parenchymal Lung DiseaseDocument59 pagesInterstitial Lung Disease Diffuse Parenchymal Lung Diseaseapi-19641337No ratings yet
- Merge From OfoctDocument536 pagesMerge From OfoctAjîsh MNo ratings yet
- Interstitial Lung Diseases ILD AbebeDocument85 pagesInterstitial Lung Diseases ILD Abebemekonnenchirotaw11No ratings yet
- Chest AyuDocument70 pagesChest AyuAbebe GelawNo ratings yet
- COPD, Pneumoconioses, Cor PulmonaleDocument3 pagesCOPD, Pneumoconioses, Cor PulmonaleMadeline WanhartNo ratings yet
- 1 - Respiratory Idone.Document24 pages1 - Respiratory Idone.Hinna SinghNo ratings yet
- Research MethodsDocument8 pagesResearch MethodsSilver DrakeNo ratings yet
- Respiratory Medicine For FinalsDocument52 pagesRespiratory Medicine For FinalsAmelia SeifalianNo ratings yet
- COPD Student Lec DR Atef Alkarn 6-2022Document42 pagesCOPD Student Lec DR Atef Alkarn 6-2022mohamed albnaNo ratings yet
- Bronchogenic Carcinoma Diagnosis GuideDocument55 pagesBronchogenic Carcinoma Diagnosis GuidePandu AlanNo ratings yet
- Respiratory FailureDocument21 pagesRespiratory FailureDennis MiritiNo ratings yet
- Sypmtoms and Signs of Respiratory DiseasesDocument22 pagesSypmtoms and Signs of Respiratory DiseasesPrincewill SeiyefaNo ratings yet
- DR - Donal Anjar Simanjuntak.M, Ked (Paru) .SP.PDocument15 pagesDR - Donal Anjar Simanjuntak.M, Ked (Paru) .SP.PM.Satria PerdanapNo ratings yet
- Pneumonia GuideDocument68 pagesPneumonia GuidefatiniNo ratings yet
- COPDDocument23 pagesCOPDUsamaNo ratings yet
- A Grand Tour of Pulmonary MedicineDocument115 pagesA Grand Tour of Pulmonary MedicineKaram SarhanNo ratings yet
- Hemoptysis: Bahman Saatian, M.DDocument57 pagesHemoptysis: Bahman Saatian, M.DRovanNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument45 pagesChronic Obstructive Pulmonary DiseaseAlexander Santiago ParelNo ratings yet
- Copd, Chronic Bronchitis, EmphysemaDocument28 pagesCopd, Chronic Bronchitis, EmphysemaHoney BoneyNo ratings yet
- Basic Chest RadDocument112 pagesBasic Chest Radtesfayegermame95.tgNo ratings yet
- Lung Cancer Types, Risks, Symptoms & Treatment GuideDocument49 pagesLung Cancer Types, Risks, Symptoms & Treatment GuidefajarnugrahamulyaNo ratings yet
- Chronic Obstructive Disease by HibaDocument38 pagesChronic Obstructive Disease by HibahibaNo ratings yet
- Idiopathic Pulmonary FibrosisDocument52 pagesIdiopathic Pulmonary FibrosisOlga GoryachevaNo ratings yet
- Lung CancerDocument24 pagesLung CancerArshamNo ratings yet
- HemoptysisDocument35 pagesHemoptysisElad MizrahiNo ratings yet
- Lung Cancer Presentation FinalDocument48 pagesLung Cancer Presentation Finalراس زهد ارفنندNo ratings yet
- COPD Vs RLDDocument64 pagesCOPD Vs RLDXine DeeNo ratings yet
- 2023 PneumothoraxDocument27 pages2023 PneumothoraxYasser KamalNo ratings yet
- Merged 37Document21 pagesMerged 37abdulkreemsalem4No ratings yet
- Pulmonary EmbolismDocument96 pagesPulmonary Embolismsamice5100% (1)
- Cor PulmonaleDocument21 pagesCor Pulmonalemaibejose100% (1)
- CardiopathophysiologyDocument63 pagesCardiopathophysiologyapplesncoreNo ratings yet
- Renal Pathology Guide on Kidney Structure and FunctionDocument37 pagesRenal Pathology Guide on Kidney Structure and Functionapplesncore100% (1)
- Gastrointestinal Tract (Partial Edit)Document47 pagesGastrointestinal Tract (Partial Edit)applesncoreNo ratings yet
- Bones and JointsDocument20 pagesBones and JointsapplesncoreNo ratings yet
- Pediatric PathologyDocument27 pagesPediatric PathologyapplesncoreNo ratings yet
- Hematopoietic SystemDocument39 pagesHematopoietic SystemapplesncoreNo ratings yet
- CardiopathophysiologyDocument63 pagesCardiopathophysiologyapplesncoreNo ratings yet
- Blood Vessel Functions and DiseasesDocument36 pagesBlood Vessel Functions and DiseasesapplesncoreNo ratings yet
- Immunopathology Guide for Medical StudentsDocument21 pagesImmunopathology Guide for Medical StudentsapplesncoreNo ratings yet
- Draft of PICO 2questionDocument5 pagesDraft of PICO 2questionapplesncoreNo ratings yet
- Pathology of Infections Objectives: ©bharti B-Pathologyof infections-SGUSOM 2Document25 pagesPathology of Infections Objectives: ©bharti B-Pathologyof infections-SGUSOM 2applesncoreNo ratings yet
- Fluid and Hemodynamic DisordersDocument19 pagesFluid and Hemodynamic DisordersapplesncoreNo ratings yet
- Neoplasia Path NotesDocument13 pagesNeoplasia Path NotesapplesncoreNo ratings yet
- Cover Letter Language ExamplesDocument2 pagesCover Letter Language ExamplesapplesncoreNo ratings yet
- Gluteraldehyde, Peracetic Acid Alcohol, Iodophors QAC (Quarternary Ammonium Compounds)Document3 pagesGluteraldehyde, Peracetic Acid Alcohol, Iodophors QAC (Quarternary Ammonium Compounds)applesncoreNo ratings yet
- Lecture 9Document7 pagesLecture 9applesncoreNo ratings yet
- My Labeled Slides - UterusDocument19 pagesMy Labeled Slides - UterusapplesncoreNo ratings yet
- Midterm GOLD NotesDocument41 pagesMidterm GOLD NotesapplesncoreNo ratings yet
- Chapter 3 ImmunoDocument4 pagesChapter 3 ImmunoapplesncoreNo ratings yet
- Lecture 1Document2 pagesLecture 1applesncoreNo ratings yet
- Bordetella PertussisDocument5 pagesBordetella PertussisapplesncoreNo ratings yet
- Epidemiology 2Document5 pagesEpidemiology 2applesncoreNo ratings yet
- Ventilator Management: Introduction To Ventilator Management, Modes of Mechanical Ventilation, Methods of Ventilatory SupportDocument12 pagesVentilator Management: Introduction To Ventilator Management, Modes of Mechanical Ventilation, Methods of Ventilatory SupportDellNo ratings yet
- Pathophysiology and Classification of Respiratory Failure. Tejpreet Singh Lamba. 2016Document9 pagesPathophysiology and Classification of Respiratory Failure. Tejpreet Singh Lamba. 2016Danitza VeraNo ratings yet
- Clinical Nursing JudgementDocument5 pagesClinical Nursing Judgementapi-403115643No ratings yet
- Corona VirusDocument8 pagesCorona VirusIndraNo ratings yet
- Mechanical Power FormulaDocument9 pagesMechanical Power FormulaEzeBorjesNo ratings yet
- Acute Respiratory Distress SyndromeDocument70 pagesAcute Respiratory Distress SyndromeAndrea Del Villar100% (1)
- Case Study An Older COVID-19 Patient in A Turkish IntensiveDocument7 pagesCase Study An Older COVID-19 Patient in A Turkish IntensiveAJENGNo ratings yet
- Internal Medicine STUDY GUIDEDocument276 pagesInternal Medicine STUDY GUIDEanabananan100% (1)
- 54819adb0cf22525dcb6270c PDFDocument12 pages54819adb0cf22525dcb6270c PDFEmaa AmooraNo ratings yet
- Antonelli - Fiberoptic Bronchoscopy During Noninvasive Positive Pressure Ventilation Delivered by HelmetDocument4 pagesAntonelli - Fiberoptic Bronchoscopy During Noninvasive Positive Pressure Ventilation Delivered by HelmetXaralyn XaviereNo ratings yet
- Respiratory Failure: Dr. Sat Sharma Univ of ManitobaDocument38 pagesRespiratory Failure: Dr. Sat Sharma Univ of ManitobaGonzalo Venegas RojasNo ratings yet
- Understanding The Essentials of Critical Care Nursing by Perrin - Test BankDocument50 pagesUnderstanding The Essentials of Critical Care Nursing by Perrin - Test BankalishcathrinNo ratings yet
- Emergency in Respiratory Medicine HandbookDocument73 pagesEmergency in Respiratory Medicine HandbookIndra MahaputraNo ratings yet
- Pneumonia in The Intensive Care Unit: Jordi Rello Emili DiazDocument8 pagesPneumonia in The Intensive Care Unit: Jordi Rello Emili DiazMario A. Humeres RNo ratings yet
- Absolute Hospital Medicine Review An Intensive Question & Answer Guide 2016 (PDF) (UnitedVRG) PDFDocument213 pagesAbsolute Hospital Medicine Review An Intensive Question & Answer Guide 2016 (PDF) (UnitedVRG) PDFDiwakesh C BNo ratings yet
- ARDS: Etiology, Pathogenesis, and ManagementDocument15 pagesARDS: Etiology, Pathogenesis, and ManagementLiri AndiyaniNo ratings yet
- COVID 19 Associated Opportunistic Infections: A Snapshot On The Current ReportsDocument20 pagesCOVID 19 Associated Opportunistic Infections: A Snapshot On The Current ReportsAndreea CiorneaNo ratings yet
- Diagnosis, Management, and Prevention of Pulmonary Barotrauma During Invasive Mechanical Ventilation in Adults - UpToDateDocument34 pagesDiagnosis, Management, and Prevention of Pulmonary Barotrauma During Invasive Mechanical Ventilation in Adults - UpToDatevmdcabanillaNo ratings yet
- MCU 2021 The Ventilator Book 3rd EditionDocument280 pagesMCU 2021 The Ventilator Book 3rd EditionAlvaro Estupiñan100% (2)
- MRCS B VivaDocument8 pagesMRCS B Vivatahir_the_great2939No ratings yet
- Wiki Resp Mcqs ExplainedDocument7 pagesWiki Resp Mcqs ExplainedArvinth Guna SegaranNo ratings yet
- Brazilian Recommendations of Mechanical Ventilation: Recomendações Brasileiras de Ventilação Mecânica 2013. Parte 2Document25 pagesBrazilian Recommendations of Mechanical Ventilation: Recomendações Brasileiras de Ventilação Mecânica 2013. Parte 2Renata Araújo Borges XavierNo ratings yet
- Properties of A Well-Written TextDocument5 pagesProperties of A Well-Written TextRine CabusaoNo ratings yet
- Ventilation: This IsDocument12 pagesVentilation: This IsAli Mohamed AbdallaNo ratings yet
- Cor Pulmonale EmedicineDocument16 pagesCor Pulmonale EmedicineHengki Permana PutraNo ratings yet
- MCQ For Medical StudentDocument6 pagesMCQ For Medical StudentFatma Shnewra100% (11)
- Efferent Therapy in Cases of Malaria: V. A. VoinovDocument3 pagesEfferent Therapy in Cases of Malaria: V. A. VoinovEliDavidNo ratings yet
- Bleomycin Monograph 1dec2014Document10 pagesBleomycin Monograph 1dec2014cmeytasNo ratings yet
- NLE PRE-TEST Q Only 150 ITEMS (The Nurse Is Caring... ) - Refresher Nov 2021Document11 pagesNLE PRE-TEST Q Only 150 ITEMS (The Nurse Is Caring... ) - Refresher Nov 2021Epaphras Joel MilitarNo ratings yet
- Best Practices in The Management of Orthopaedic Trauma: Acs TqipDocument38 pagesBest Practices in The Management of Orthopaedic Trauma: Acs TqipandhiyatnoermandakaNo ratings yet