Professional Documents
Culture Documents
Bones and Joints
Uploaded by
applesncore0 ratings0% found this document useful (0 votes)
30 views20 pagespath notes
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentpath notes
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
30 views20 pagesBones and Joints
Uploaded by
applesncorepath notes
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 20
Bones and Joints
Dr Dexter MD FRC Path Undercover Professor
Department of Pathology, School of Medicine
St. Georges University, Grenada (West Indies)
Define and use in proper context:
metaphysis
eburnation
Felty syndrome
Heberden node
involucrum
osteoblast
osteoclast
osteocyte
Alkaline
phosphatase
cancellous bone
lamellar bone
chondrocytes
Codman triangle
cortical bone
diaphysis
epiphysis
Objectives
osteoid
osteomalacia
osteopenia
pannus
Pott disease
sequestrum
synovium
tophus
woven bone
Discuss the following hereditary
disorders, in terms of pathogenesis,
morphology, and clinical presentation:
achondroplasia
osteopetrosis
osteogenesis imperfecta
Discuss the following non-neoplastic
bone disorders, in terms of etiology,
pathogenesis, morphology, and clinical
findings and course:
osteoporosis
renal osteodystrophy
Pagets disease
hyperparathyroidism
osteomyelitis
Describe the following tumors of
bone, joint, and soft tissue:
osteoma
osteoid osteoma
osteoblastoma
osteochondroma
chondroma
osteosarcoma
chondrosarcoma
giant cell tumor of
bone
Ewing sarcoma
primitive
neuroectoderm
al tumor (PNET)
multiple
myeloma
metastatic
malignancy to
bone
in terms of:
biology (benign vs. malignant)
age distribution
etiology and pathogenesis
cell type and site of origin
morphologic and radiological features
clinical findings and course
Compare osteoarthritis (degenerative
joint disease) and rheumatoid arthritis
in terms of:
age and sex incidence
laboratory findings
etiology
morphologic findings
pathogenesis
clinical findings and course
Discuss the following disorders:
gout
calcium pyrophosphate crystal
deposition disease (pseudogout)
ankylosing spondylitis
infectious arthritis
Reiter syndrome
psoriatic arthritis
in terms of:
age and sex incidence
etiology
pathogenesis
findings (laboratory, morphologic,
clinical)
clinical course
Bone
Bone is specialized connective tissue
Ground substance Fibres
Cells
Type I
collagen
Inorganic elements
Osteoblasts
Osteoclasts
Osteocytes
Organic elements
Mineralized
Unmineralized
(Osteoid)
BONE
WOVEN LAMELLAR
Trabecular
Cortical
-Circumferential
-Concentric
-Interstitial
Hematopoietic progenitor
cells
Osteoprogenitor cells
Osteoclast
Osteoblasts
Osteocytes
Cellular Elements
Osteoblasts
Synthesize osteoid
Cytoplasm contains alkaline phosphatase, increase can be
measured in proliferative diseases
Contain PTH receptor, signals osteoclast to resorb bone
Osteoclasts
Multinucleated giant cells, responsible for bone resorption
Contain collagenases and acid phosphatase
Reside in cavities called Howships lacunae
Osteocytes
Arise as osteoblasts entrapped in osteoid they secrete
Maintain bone composition and structure
Overview Of The Pathological
Lesions
Developmental and
acquired Abnormalities
in bone cells, matrix
and structure
Tumors and tumor
like conditions
-Congenital malformations / dysostoses
-Achondroplasia
-Osteogenesis imperfecta
-Osteopetrosis
-Osteoporosis
-Pagets disease
-Rickets and osteomalacia
-Osteitis fibrosa cystica
-Renal osteodystrophy
Infections
(Osteomyelitis)
-Pyogenic
-Tubercular
-Bone forming tumors
-Cartilage forming tumors
-Fibrous and fibro-osseous
tumors
-Miscellaneous
Congenital Malformations
Failure of development of bone
Formation of extra bones -
Supernumerary digits
Fusion of digits - Syndactyly
Achondroplasia
Autosomal dominant
80% represent new spontaneous
mutations
Point mutation in gene coding for FGF-3
receptor (becomes constitutively active)
Clinically
Disproportionate short limbs
Shortened proximal extremities
Enlarged head
Depressed nose
Bulging forehead
NO MENTAL RETARDATION
Pathology
Problem with endochondral ossification
Constitutively active FGFR3 promotes fibrosis
and inhibits proliferation of chondrocytes at
growth plate
Disorganized clusters of chondrocytes at
growth plates
Premature deposition of horizontal struts of
bone
Cortices appear thickened
Zones of proliferating cartilage are either thin
or absent
Osteogenesis Imperfecta
Aka brittle bone disease
Weak, brittle, thin bones highly susceptible
to fracture
Autosomal dominant
Deficiencies in synthesis of Type I
collagen
Other organs containing type I collagen are
Four variants
Type I form
usually an acquired defect
Increased fractures
Blue sclerae (thin collagen translucent veins)
Dental imperfectations (Dentinogenesis imperfecta)
Hearing loss (defect of ear bones)
LIFE SPAN NORMAL (stops at puberty)
Type II form
most severe and fatal in utero
Osteopetrosis
Aka Marble bone disease
Autosomal dominant (more common) or
Autosomal recessive (more severe)
Reduced osteoclastic bone resorption
Leads to dense diffuse symmetric
skeletal sclerosis
Stony, thick, hard BUT BRITTLE bones
Osteoclast
Defect of carbonic
anhydrase
Decreased acidification in resorption pits
Decreased bone resorption
Bulbous, misshapen
ends of long bones
ERLENMEYERS FLASK
DEFORMITY
(widened, flaring
deformity of
metaphyses)
Narrowing of skull
neural foramina
Nerve compression
Defect in chloride
channels at abnormal
ruffled border
Thickening bone & medullary
canal displaces marrow
Decreased hematopoesis
Extra-medullary hematopoesis
Cranial nerve
deficits
Autosomal recessive variant is more
severe (death in utero)
Autosomal dominant one is less severe
so detected late
Repeated fractures
Pancytopenia (anemia, bleeding, infections
Hepatosplenomegaly (extramedullary
erythropoiesis)
Cranial nerve deficits
X-ray: Hyperdensity of bones
Treatment: Bone marrow transplantation
Osteoporosis
Decreased bone mass (osteopenia)
and increased porosity of skeleton to a
point that it no longer provide
mechanical support
Primary
Type I because of enhanced osteoclastic
activity (menopause)
Type II aka senile type (Attenuated
osteoblast function)
Secondary - associated with defined
causes (endocrine and genetic
abnormalities)
Synthetic potential
of Osteoblasts
(SENILE
OSTEOPOROSIS)
Lack of stimuli for normal
bone remodeling
(reduced physical activity)
Nutritional
factors
PATHOGENESIS
Deficiency of hormones
(estrogen deficiency-
menopause)
(POST MENOPAUSAL
OSTEOPOROSIS)
Genetic factors
(polymorphisms in Vitamin D
receptors)
(Caucasians)
Can affect any part of the skeleton
Parts with increased surface area
Thinned out bony trabeculae (but
normally mineralized)
Widened haversian system
Clinically
Mostly asymptomatic
Backache
Loss of height (microfractures of weight bearing
bones and vertebral compression/collapse)
Lumbar lordosis, Kyphoscoliosis
Diagnosis
Serum calcium, phosphate and alkaline
phosphatase normal
X ray (radiolucencies from osteopenia)
CT
Dual energy X- ray absorptiometry (DEXA)
measures bone densities
Pagets disease
AKA Osteitis Deformans
Chronic condition characterized by
disordered remodeling,
Initial haphazard bone resorption (lytic
lesions), followed by disorganized and
excessive bone formation (osteoblastic
lesions)
Common in populations of British isle
? Slow virus infection - paramyxovirus
? Hyper responsive osteoclasts
THREE STAGES: Osteolytic /
resorptive stage:
Sharply defined wedge shaped areas of
osteolysis
Increased osteoclastic activity
Abnormally large osteoclasts with increased
number of large hyperchromatic nuclei
Marrow fibrosis and dilation of sinusoids
Mixed osteolytic and osteoblastic stage
Bones look larger than normal
Bony surfaces lined by prominent
osteoblasts
Burnt out / osteosclerotic stage:
Little cellular activity
Thickened, brittle disordered bones
Abnormal lamellar pattern of bone
Islands of irregular bone resemble pieces
of jigsaw puzzle, separated by prominent
disarranged cement lines (Mosaic
pattern)
Large thick coarse bone trabeculae
Soft, porous and weak bones
Clinically
Most cases incidental radiological
finding
Patient hat size no longer fits head
Mono-ostotic or Polyostotic (# of bones)
Pain in the affected bones
Chalk stick fractures
Bowing of the tibial and femoral bones
Secondary osteoarthritis
Warm skin because of increased
vascularity of bone (hyperdynamic
circulation)
Skull:
-Platybasia (flattening of the skull base
-Abnormal growth of maxillary bones
-Leontiasis ossea (lion-like face deformities)
Laboratory investigations:
Serum calcium, phosphate normal
Alkaline phosphatase markedly elevated
(high turnover)
Urinary hydroxyproline
(bone degradation product)
elevated
Complications
High output cardiac failure (due to
increased bone vascularity)
Thickened skull may result in
narrowed foramens which compress
auditory nerve (deafness)
Development of tumors and tumor like
conditions
Giant cell tumor
Giant cell reparative granuloma
Secondary osteosarcomas
Rickets
Characterized by inadequate
mineralization of the bony matrix and
cartilaginous matrix of the growth plate
in children causing softening of the
bone
Causes
Inadequate exposure to sunlight
Dietary deficiency
Malabsorption
Disorders of Vitamin D metabolism
Inherited deficiency of alpha 1 hydroxylase
Mutations in Vitamin D receptor
Impaired renal tubular transport of
phosphate (Vitamin D resistant rickets)
Serum: PTH, Ca, Phosphorus, ALP
Pathology:
Overgrowth of the cartilage because
of inadequate provisional calcification
results in flared or cup shaped
epiphyses
Thickening of the growth plate
Deposition of osteoid matrix on
inadequately mineralized cartilaginous
remnants
Exaggerated widening of uncalcified
osteoid seams
Clinically
Apathy, irritability
Delayed closure of fontanelle, frontal
bossing, prominent suture lines, softened
skull bones, flattening of back of head
(cranio tabes)
Delayed dentition, dental caries
Bowing of legs, lumbar lordosis
Rachitic rosary (beaded appearance of
the costochondral junctions)
Pigeon chest (pectus carinatum)
Osteomalacia
Disorder seen in adults characterized by
inadequate mineralization of the bony
matrix
Exaggerated widening of osteoid seams
Bone contours are not affected but the
bones are weak and prone to fracture
Vertebral bodies and femoral neck are
prone to fracture
X-ray - Lack of calcification causes
radiolucency
Hyperparathyroidism
Caused by inappropriate PTH levels
Common causes include parathyroid
adenoma, parathyroid hyperplasia
Increased PTH levels
Sensed by Osteoblasts
Stimulate Osteoclasts
Increased bone resorption
Early stage:
Bone resorption by osteoclasts
Osteoclasts bore the cortex as cutting cones
Osteitis fibrosa:
Marrow replaced by loose fibrous tissue,
hemosiderin laden macrophages and
reactive woven bone formation (appear
like brown tumors)
Osteitis fibrosa cystica:
AKA Von Recklinghausen disease
Areas of cystic degeneration, filled with
fibrosis and hemorrhage appear
Clinical features
Can be summarized as
stones
bones
moans
groans
Radiological changes:
Initially no changes
Subperiosteal bone resorption
Loss of lamina dura of teeth
Multiple localized lytic lesions
Laboratory investigations:
Serum calcium increased
Serum phosphate low
Alkaline phosphatase elevated
Serum PTH elevated
Renal osteodystrophy
Complex metabolic bone disease
associated with chronic renal failure
Common in patients maintained on long
term dialysis
Pathogenesis
Low calcium & phosphate:PTH
Kidney unable to hydroxylate vitamin D:
Reduced absorbtion of calcium
CRF
Retention of
phosphate
Vit D Metabolic
acidosis
Aluminum deposition
(because of dialysis)
Interfere with mineralization
OSTEOMALACIA
Hypocalcemia
Increased PTH
INCREASED BONE
RESORPTION
Amyloid deposition
Skeletal changes associated with
chronic renal disease include
Increased osteoclastic bone resorption
Delayed matrix mineralization
Osteosclerosis
Growth retardation
Osteoporosis
Combination of osteomalacia and
osteitis fibrosa cystica is common
Osteomyelitis
Infection of bone and bone marrow
Pyogenic
Tubercular
Pyogenic Osteomyelitis
Spread to bone can be
Hematogenous (metaphysis)
Extension from contiguous site
Direct impaction
80-90% cases - Staphylococcus aureus
Patients with sickle cell disease -
Salmonella
In sexually active patients - Gonnorhea
Site depends upon age of the patient
Neonates - metaphysis or epiphysis
Children- metaphysis
Adults - epiphysis and subchondral region
Onset can be
Acute
Chronic
Subacute
Pathogenesis
Localization of bacteria
Acute inflammatory reaction
Necrosis of bone
Spread to periosteum in Haversian canals
Subperiosteal abscess
Lifting of periosteum
Further impair blood supply
Death of bony trabeculae
(SEQUESTRUM)
RELEASE OF CYTOKINES
Stimulate osteoclasts and growth
of fibrous tissue
Also deposition of reactive bone
Around periphery
(INVOLUCRUM)
1
2 3
4
Clinically
Malaise, fever and chills
Throbbing pain over the affected area
Infants-unexplained fever
5-25% becomes chronic
Complications
Pathological fractures (from bone
microabscesses)
Septic arthritis
Sepsis
Endocarditis
Secondary Amyloidosis
Ischemic necrosis by vessel destruction
Squamous cell carcinoma in the sinus
tract from draining abscess (irritant pus)
Rarely secondary osteosarcomas
Tubercular osteomyelitis
Usually hematogenous spread
Focus is usually solitary
Multifocal in immunocompromised
Sites
Spine (Pott disease) - destruction of both
vertebral bodies & intervertebral disks
Bones of knee joint
Bones of hip joint
Clinically
Low grade fever, chills
Pain on motion
Localized tenderness
Deformities
Scoliosis, kyphosis because of compression
fractures from vertebral necrosis
Neurological deficits
Can spread to adjacent muscles hip
(psoas) causing psoas cold abscess
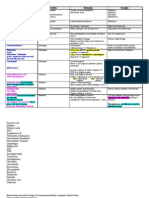
Bone tumors and tumor like
conditions
PRIMARY TUMORS
E EEP PPI IIP PPH HHY YYS SSI IIS SS
G GGi iia aan nnt tt c cce eel lll ll t ttu uum mmo oor rr
C CCh hho oon nnd ddr rro oob bbl lla aas sst tto oom mma aa
M MME EET TTA AAP PPH HHY YYS SSI IIS SS
O OOs sst tte eeo oos ssa aar rrc cco oom mma aa
D DDI IIA AAP PPH HHY YYS SSI IIS SS
E EEw wwi iin nng gg s ssa aar rrc cco oom mma aa
E EEn nnc cch hho oon nnd ddr rro oom mma aa
O OOs sst tte eeo oob bbl lla aas sst tto oom mma aa
O OOs sst tte eeo ooc cch hho oon nnd ddr rro oom mma aa
O OOs sst tte eeo ooi iid dd o oos sst tte eeo oom mma aa
Osteoblastoma
Osteochondroma
Osteoid osteoma
Giant cell tumor
Chondroblastoma
Ewing sarcoma
Osteosarcoma
Juxta cortical
Osteosarcoma
Enchondroma
Fibrous dyspasia
Osteoma
Solitary, benign lesions commonly seen on
skull and facial bones
Middle aged adults
Multiple osteoma + GI polyps - Gardener
syndrome (familial polyposis)
Composed of lamellar and woven bone
Rarely symptomatic
Osteoid Osteomas
Small, painful benign lesion composed of
osseous tissue (nidus) and surrounded
by reactive bone formation
Arise from osteoblasts
Measure less than 2 cm
5-25 years
Cortex of the diaphysis of the tubular
bones of the lower limb (e.g. tibia)
Nocturnal pain (PGE 2 production)
relieved by aspirin
X-ray - radiolucent centers
surrounded by sclerotic bone
Osteoblastoma
Similar to osteoid osteoma but larger size
Commonly involves vertebrae
Dull pain non-responsive to aspirin
Nocturnal relief of pain
Does not induce marked fibroblastic
reaction
Microscopy
- Interconnecting trabeculae of woven
bone rimmed by osteoblasts
- Stroma contains loose connective
tissue and congested capillaries
Osteosarcoma (osteogenic sarcoma)
Malignant mesenchymal tumor in which
tumor cells produce bone matrix
(osteoid)
Most common primary malignant tumor
of bone (not marrow)
Bimodal age distribution
75% less than 20 years of age
Second peak in elderly
Knee bones most common site
Osteosarcoma
PRIMARY SECONDARY
Pagets disease
Pre-existing bone
tumors
Bone infarcts
(osteomyelitis)
Prior radiation
Mutation in Rb gene
Hereditary retinoblastoma 1000 times
increased risk
Clinically:
Mild intermittent pain around the knee
Sometimes pathological fracture
Radiologically:
Evidence of bone destruction and new bone
formation
Reactive bone formation causing periosteal
lifting - Codman's triangle
Sun burst appearance - white, perpendicular
radiating lines from neoplastic bone
Gross:
Gray white with areas of hemorrhage,
cystic degeneration
Invasion of the cortex, marrow,
epiphyses and soft tissues
Microscopically:
Malignant, anaplastic cells with
osteoblastic differentiation producing
woven bone
Neoplastic bone is coarse lace-like
75% develop lung metastasis (hemoptysis)
Osteochondroma / Exostosis
Arise from metaphysis near growth
plate at end of long bone
Solitary or Multiple (Multiple hereditary
exostosis - Autosomal dominant)
Growth cartilage grows laterally into
soft tissues
Leads to formation of cartilage capped
growth
Medullary cavity of the bone and the
lesion are in continuity
Grow away from the joint
Microscopically:
Cartilage capped, bony mass surrounded by
fibrous membrane (perichondrium)
Clinically:
Solitary lesions are usually asymptomatic
Hereditary (Multiple) type:
Dwarfism can occur
Shortened metacarpals, compromised supination
and pronation
Unequal leg length
Disturbed joint function
Chondroma
Benign tumors of hyaline cartilage
When arise in medullary cavity known
as enchondroma
Metaphyses of tubular bones especially
metacarpals and phalanges
Usually solitary
Multiple chondromas - Ollier disease
Multiple chondromas + soft tissue
hemangiomas - Maffucci syndrome
Slow growing tumors usually in hands
and feet
Multiple chondromas are associated
with risk of other malignancies
Rarely sarcomatous transformation
Gross:
Small semitranslucent lesions with few
calcified areas
Microscopically:
Composed of well
differentiated chondrocytes
Radiologically:
Well circumscribed lucent cartilage
growth surrounded by rim of radiodense
bone O-ring sign
Chondrosarcoma
Malignant neoplasm of cartilage cells,
associated with production of cartilage
Patients usually older than 40 years
Associated with pre-existing
enchondromas, osteochondromas,
chondroblastoma or Pagets disease
Commonly involves pelvis, clavicle,
shoulder and ribs
Clinically:
Progressively swelling painful masses
Radiologically:
Nodular lucent masses with calcifications
Grossly:
Bulky gray white gelatinous tumors
Spotty calcification
Microscopically:
Malignant chondrocytes in various stages of
maturity
Multiple chondrocytes in single lacuna
Divided into three grades
Grade I - Mild hypercellularity, sparse
mitosis
Grade 3 - Marked hypercellularity,
pleomorphism, frequent mitoses
Direct correlation between grade and
biological behavior
Tumors measuring more than 10 cm do
worse
Mostly metastasize to lungs, skeleton
Giant cell tumor
Locally aggressive, potentially malignant
neoplasm characterized by presence of
osteoclastic giant cells (Osteoclastoma)
uniformly distributed in a back ground of
mononuclear cells
Common in age group 20-40 years
90% originate at junction between
metaphyses and epiphyses (near end)
Majority arise in bones around knee joint
X-ray: Osteolytic soap bubble appearance
Gross:
Reddish brown cystic tumors with areas of
cystic degeneration, often limited by
periosteum
Microscopically:
Spindle cells - mononuclear plump cells
with large nuclei, mitoses evident
Multinucleated giant cells: formed by
fusion of mononuclear cells, more than 100
nuclei
Areas of necrosis, hemorrhage and
reactive bone formation can be seen
Patient can present with symptoms of
arthritis
Some times pathologic fractures
All are potentially malignant
Simple curettage is associated with 40-
60% recurrence
Very rarely sarcomatous
transformation
Ewings sarcoma / Primitive
Neuroectodermal Tumor (PNET)
Malignant tumor of bones and soft tissues
with neural differentiation
Young average age (10-15 years)
More than 85% cases t(11:22) EWS:FLI 1
fusion gene
Commonly arises medullary cavity of
diaphyses of long bones (humerus, tibia,
femur)
Clinically:
Pain, swelling, redness
Fever, leucocytosis and increased ESR
X-ray:
Lytic lesion extending into soft tissues
Reactive bone formation can lead to
onion skin appearance
Gross:
Grayish white tumor with areas of
hemorrhage
Can infiltrate medullary cavity without
destroying bony trabeculae
Microscopically:
Sheets of small, blue, round cells
twice the size of lymphocyte
Little stroma, infrequent mitosis
In some areas neoplastic cells tend to
form Homer-Wright pseudorosettes
(indicate neural differentiation)
Positive for PAS stain (glycogen)
Multiple Myeloma
Malignant tumor of plasma cells
Localized or diffuse
Skull, spine, ribs, pelvis, femur
Marrow looks reddish fleshy
Sheets of immature plasma cells
Metastatic tumors
Most common malignancy of bone
Three pathways of spread:
Direct
Hematogenous/lymphatic
Intraspinal seedlings
Adults:
Breast, Prostate, Kidney, Lung, Thyroid
Children:
Neuroblastoma, Wilms tumor,
Osteosarcoma
Most involve axial skeleton
Vertebral column
Pelvis
Ribs
Skull
Sternum
Radiologically:
Commonly mixed osteolytic & osteoblastic
appearance
But in case of prostate osteoblastic
response
Kidney, lung, melanoma mainly lytic
lesions
Osteoarthritis
Degenerative (wear & tear) joint disorder
Slowly progressive destruction of the
articular cartilage
Manifested in weight bearing joints (hip,
knee, spine) and fingers of elderly
Primary- intrinsic defect in the articular
cartilage
Secondary- known underlying cause
Pathogenesis
Genetic factors, aging
Increased unit load
Biochemical abnormalities
Resilience of articular cartilage
Joint trauma, hemarthrosis
Commonly affected joints are:
Knee, hip, cervical and lumbar vertebrae
Proximal and distal interphalangeal joints
Loss of proteoglycans and death of chondrocytes
Surface cracks in the articular cartilage - fibrillations
Seepage of synovial fluid, loss and degeneration of
cartilage
Loss of articular cartilage and exposure of subchondral
bone - eburnation (smoothing/polishing of bone)
Cracking of subchondral bone and fluid enters
subchondral cysts
Bony outgrowths at the edges of bones - osteophytes
(Osteophytes at the distal interphalangeal joints are known
as Heberden nodes, proximal are Bouchards)
Clinically
Asymmetric large joint involvement
Deep aching joint pain that follows
activity
Morning stiffness
Restricted joint movement
Joint crepitus
Nerve root compression by osteophytes
Joint deformities in late stage but no
fusion of joints
X-ray - loss of joint space, osteophytes
Gout
Characterized by hyperuricemia and
deposition of needle shaped urate
crystals in joints and kidney
Acute and chronic arthritis
Primary: hyperuricemia in absence of
any other disease (idipathic 90%)
Secondary: hyperuricemia secondary to
some other illness
Secondary gout
Increased turnover of nucleic acids
Leukemias, lymphomas, polycythemia
Alcohol abuse
Glycogen storage disorders
Drugs
Renal disease
Lesch-Nyhan syndrome (HGPRT
mutation)
Clinically
Asymptomatic hyperuricemia
Acute gouty arthritis: involvement of
usually one joint which is usually
red, warm and tender
Usually first metatarsophalangeal joint is
involved
Intercritical period: asymptomatic
period between acute attacks
Chronic gout
Chronic / tophaceous gout usually in
untreated patients
Tophi in cartilage, soft tissues, tendons
Urate nephropathy and renal failure in
about 10-20% patients
Pseudogout
AKA Chondrcalcinosis or Calcium
pyrophospthate dihydrate (CPPD)
deposition disease
Deposition of CPPD crystals in synovium,
articular cartilage, ligaments and tendons
Common in elderly people
More than 50% are older than 85 years
Pathogenesis
Nucleoside triphosphates
(chondrocytes)
CPPD
X
+
Accumulation of
CPPD
Metabolic end
products
Favor
Nucleation
Deposits in joints
Trauma
Aging
Self limiting attacks of arthritis
Knees, wrists, elbows, shoulders
Chalky white deposits on the articular
cartilage
CPPD crystals do not easily dissolve in
water
Weakly positive birefringent
(whereas gout negative birefringence)
Stubby, rhomboid or coffin shaped
Little associated inflammation
Infectious Arthritis
SUPPURATIVE
ARTHRITIS
(Septic arthritis)
Hematogenous seedlings
Contiguous spread
Direct inoculation
LYME ARTHRITIS
Multiorgan disease
Caused by a spirochete
Septic arthritis
Less than 2 years Hemophilus influenzae
Sexually active young adults N. gonorrhae
Older adults Staphylococcus aureus
Sickle cell disease Salmonella enteritidis
Clinically
Fever, joint pain, swelling and redness
over the affected joint
Restricted joint movements
Usually monoarticular (non-
gonococcal)
Leucocytosis, increased ESR
Purulent joint aspirate
Gram staining can help in identifying the
infecting organism
Requires rapid intervention
Lyme arthritis
Caused by Borrelia burgdorferi
Transmitted by deer tick Ixodes
Common arthropod borne disease in
United States
Three stages
Stage I:
Fever, lymphadenopathy, fatigue
Multiplication of organisms at the site of
entry (erythema migrans chronicum)
Stage II:
Hematogenous spread
Migratory joint pains, arrhythmias
Stage III:
Chronic arthritis (large joints)
Encephalitis
Pathogenesis:
Immune mediated damage to the joints
Microscopy:
Papillary hyperplasia of the synovium
Fibrin depositions
Pannus formation
Diagnosis: serology of joint aspirate (ELISA)
silver stain of the biopsy
Seronegative Diseases
Group of diseases involving the axial
skeleton
Ankylosing spondylitis
Reiter Syndrome
Psoriatic arthritis
Enteropathic arthritis
Associated with HLA B27
No rheumatoid factor
Ankylosing Spondylitis
Inflammatory arthropathy of vertebral
column and sacroiliac joints
Most common in young men
More than 90% HLA B27 positive
Begins in sacroiliac joints then
ascends along vertebral column
Small joints of the posterior elements
of the vertebrae
Late stage spine fusion occurs -
bamboo appearance
Reiter syndrome
Exclusively in men
Following a venereal exposure
(Chlamydia) or bacillary dysentery
Clinically resembles RA
In most patients disease remits
Clinically
Triad of seronegative polyarthritis,
conjunctivitis and non specific urethritis
Described as patients cant see, pee, or
climb a tree
Mucocutaneous lesions
10-20 % progressive arthritis
Psoriatic arthritis
7-10 % patients of psoriasis
Asymmetric involvement of joints of hands
and feet
Distal interphalangeal joints
Simultaneous involvement of tendons and
synovium leads to typical sausage shaped
fingers
Histologically similar to RA but less severe
and less frequent joint destruction
Rheumatoid arthritis
Chronic systemic inflammatory
disorder
Immune mediated, non-suppurative
proliferative and inflammatory arthritis
More common in females
40-70 years
Genetic
factors
Infectious
agents
Auto reactive T cells
Autoreactive B cells
Activation of macrophages
Cytokines IL-1. TNF
Proliferation of synovial cells
Recruitment of inflammatory cells
Auto antibodies hence
Immune complex formation
(Rheumatoid factor)
Further release of cytokines,
matrix metalloproteinases
JOINT INJURY
JOINTS:
Synovium thickened, edematous and
hyperplastic
Synovial membrane thrown into villi
Cytokine mediated juxta-articular osteopenia
by osteoclasts
Dense perivascular chronic inflammatory
infiltrate, lymphoid follicles
Fibrin deposition, congestion
Pannus (flap-like) formation - inflamed
synovial tissue composed of granulation
tissue, inflammatory cells and fibrin
Creeps over and erodes the articular
cartilage and bone
SKIN:
Rheumatoid nodules - the most common
cutaneous lesion
Ulnar surface of forearm, occiput, elbows
some times visceral organs
Area of fibrinoid necrosis surrounded by rim of
epithelioid cells
BLOOD VESSELS:
Vasculitis involving small to medium sized
arteries due to immune complex deposition
But kidneys are spared
Clinically
Symmetric arthritis of small joints
Warm swollen painful joints
Joint pain increases after period
of disuse
Metacarpophalangeal joints, proximal
interphalangeal joints,
metatarsophalangeal joints, wrists,
ankles, elbows (DIP joints commonly
spared)
Flexion and extension deformities
of fingers
Investigations
X-ray - Juxta-articular osteopenia
- Decreased joint space
and deformities
Rheumatoid factor-IgM against Fc
portion of IgG, high titers associated
with severe disease
Synovial fluid analysis - increased
proteins, increased WBC count,
(neutrophils), low mucin content
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Renal Pathology: Kidney and The Urinary Collecting SystemDocument37 pagesRenal Pathology: Kidney and The Urinary Collecting Systemapplesncore100% (1)
- CardiopathophysiologyDocument63 pagesCardiopathophysiologyapplesncoreNo ratings yet
- Gastrointestinal Tract (Partial Edit)Document47 pagesGastrointestinal Tract (Partial Edit)applesncoreNo ratings yet
- Pediatric PathologyDocument27 pagesPediatric PathologyapplesncoreNo ratings yet
- CardiopathophysiologyDocument63 pagesCardiopathophysiologyapplesncoreNo ratings yet
- Hematopoietic SystemDocument39 pagesHematopoietic SystemapplesncoreNo ratings yet
- Cardiovascular + Clinical ScenariosDocument36 pagesCardiovascular + Clinical ScenariosapplesncoreNo ratings yet
- Pathology of The Lung Objectives: Define and Use in Proper Context The Following TermsDocument45 pagesPathology of The Lung Objectives: Define and Use in Proper Context The Following TermsapplesncoreNo ratings yet
- Fluid and Hemodynamic DisordersDocument19 pagesFluid and Hemodynamic DisordersapplesncoreNo ratings yet
- Pathology of Infections Objectives: ©bharti B-Pathologyof infections-SGUSOM 2Document25 pagesPathology of Infections Objectives: ©bharti B-Pathologyof infections-SGUSOM 2applesncoreNo ratings yet
- ImmunopathologyDocument21 pagesImmunopathologyapplesncoreNo ratings yet
- Neoplasia Path NotesDocument13 pagesNeoplasia Path NotesapplesncoreNo ratings yet
- Cover Letter Language ExamplesDocument2 pagesCover Letter Language ExamplesapplesncoreNo ratings yet
- Gluteraldehyde, Peracetic Acid Alcohol, Iodophors QAC (Quarternary Ammonium Compounds)Document3 pagesGluteraldehyde, Peracetic Acid Alcohol, Iodophors QAC (Quarternary Ammonium Compounds)applesncoreNo ratings yet
- My Labeled Slides - UterusDocument19 pagesMy Labeled Slides - UterusapplesncoreNo ratings yet
- Chapter 3 ImmunoDocument4 pagesChapter 3 ImmunoapplesncoreNo ratings yet
- Lecture 9Document7 pagesLecture 9applesncoreNo ratings yet
- Draft of PICO 2questionDocument5 pagesDraft of PICO 2questionapplesncoreNo ratings yet
- Bordetella PertussisDocument5 pagesBordetella PertussisapplesncoreNo ratings yet
- Lecture 1Document2 pagesLecture 1applesncoreNo ratings yet
- Midterm GOLD NotesDocument41 pagesMidterm GOLD NotesapplesncoreNo ratings yet
- Epidemiology 2Document5 pagesEpidemiology 2applesncoreNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Allopurinol Drug StudyDocument3 pagesAllopurinol Drug StudyFrancis Corpuz0% (2)
- # CLINICAL PHARMA FINALS MCQs 2021-1-30Document30 pages# CLINICAL PHARMA FINALS MCQs 2021-1-30Pavan chowdaryNo ratings yet
- Rheumatology: With Kartik Rangaraj MDDocument39 pagesRheumatology: With Kartik Rangaraj MDNailahRahmahNo ratings yet
- 16 Nucleotide MetabolismDocument71 pages16 Nucleotide MetabolismkalkidanNo ratings yet
- Human Anatomy and Physiology 9th Edition Marieb Test BankDocument16 pagesHuman Anatomy and Physiology 9th Edition Marieb Test Bankjillhenrysetcjnzrfp100% (28)
- 316 FinalsDocument21 pages316 FinalsKatherine BautistaNo ratings yet
- Common Causes of Severe Knee PainDocument8 pagesCommon Causes of Severe Knee PainRatnaPrasadNalamNo ratings yet
- Drugs On RespiratoryDocument17 pagesDrugs On RespiratoryIrwan M. IskoberNo ratings yet
- Coca-Cola Drinking - DangersDocument4 pagesCoca-Cola Drinking - DangersLeničkaNo ratings yet
- Pharmacology Test 3 Drug ListDocument32 pagesPharmacology Test 3 Drug ListSHRIKANTNo ratings yet
- How Nanorobots Will WorkDocument8 pagesHow Nanorobots Will WorkshivangivighNo ratings yet
- Musculoskeletal Problems Rev 11.21.07Document191 pagesMusculoskeletal Problems Rev 11.21.07jeshemaNo ratings yet
- Gout (Also Known As Podagra When It Involves The Big ToeDocument54 pagesGout (Also Known As Podagra When It Involves The Big ToearunshreerajendranNo ratings yet
- Hyperuricemia XXXX XXXXX XxjeuneDocument32 pagesHyperuricemia XXXX XXXXX XxjeuneOziq Juga ReMa-eNo ratings yet
- QuizletDocument67 pagesQuizletnaimNo ratings yet
- Biology - CHP 5 Practice Data AnalysisDocument1 pageBiology - CHP 5 Practice Data AnalysisJhiyuan (Max) HsuNo ratings yet
- Drugs For GoutDocument29 pagesDrugs For GoutSsempijja Joshua BuyinzaNo ratings yet
- Rheumatology Saif 2013 Wesmosis PDFDocument30 pagesRheumatology Saif 2013 Wesmosis PDFMohamed A SalehNo ratings yet
- Lessons in ResearchDocument125 pagesLessons in ResearchJho BanNo ratings yet
- Hubungan Antara Kadar Asam Urat Dengan Indeks Massa Tubuh... (Ulfa F, Zuraida Z, Enggar W)Document10 pagesHubungan Antara Kadar Asam Urat Dengan Indeks Massa Tubuh... (Ulfa F, Zuraida Z, Enggar W)Enggar WijayantiNo ratings yet
- SexologyDocument91 pagesSexologyGuduna Guduna Darbuashvili100% (1)
- Change Gout - The Gout Diet PDFDocument2 pagesChange Gout - The Gout Diet PDFManzar Khan100% (1)
- Diagnosing Acute Monoarthritis in Adults PDFDocument8 pagesDiagnosing Acute Monoarthritis in Adults PDF蔡季霖No ratings yet
- 736-Article Text-2116-1-10-20171005Document4 pages736-Article Text-2116-1-10-20171005Dr.upendra goudNo ratings yet
- IM RheumatologyDocument56 pagesIM RheumatologySujoud AbuserdanehNo ratings yet
- Clinical Pathology of Mother Tinctures &lower PotenciesDocument64 pagesClinical Pathology of Mother Tinctures &lower PotenciesAntony antony100% (1)
- Disorders of Purine and Pyrimidine MetabolismDocument17 pagesDisorders of Purine and Pyrimidine MetabolismUbaid AhmedNo ratings yet
- Yoga For Arthritis The Complete GuideDocument465 pagesYoga For Arthritis The Complete GuideRomina Mascetti100% (2)
- Nursing PresentationDocument63 pagesNursing PresentationDeekayNo ratings yet
- Grade 8 Skeletal System Enhanced SciDocument126 pagesGrade 8 Skeletal System Enhanced SciCin TooNo ratings yet