Professional Documents
Culture Documents
Exercicios Funcionais em Idosos
Uploaded by
Débora Souza0 ratings0% found this document useful (0 votes)
11 views5 pagesThe physical benefits of a functional exercise circuit are not well known in an elderly population. A supervised functional exercise circuit included 10 different upperand lower-body exercises. Subjects were 119 men and women (aged 74 [Ti4.2] years) who received preand posttests of mobility (e.g., sit to stand, get up and go, timed walk), flexibility (sit and reach), and balance (standing reach)
Original Description:
Original Title
Exercicios Funcionais Em Idosos
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe physical benefits of a functional exercise circuit are not well known in an elderly population. A supervised functional exercise circuit included 10 different upperand lower-body exercises. Subjects were 119 men and women (aged 74 [Ti4.2] years) who received preand posttests of mobility (e.g., sit to stand, get up and go, timed walk), flexibility (sit and reach), and balance (standing reach)
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views5 pagesExercicios Funcionais em Idosos
Uploaded by
Débora SouzaThe physical benefits of a functional exercise circuit are not well known in an elderly population. A supervised functional exercise circuit included 10 different upperand lower-body exercises. Subjects were 119 men and women (aged 74 [Ti4.2] years) who received preand posttests of mobility (e.g., sit to stand, get up and go, timed walk), flexibility (sit and reach), and balance (standing reach)
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
647
Journal of Strength and Conditioning Research, 2005, 19(3), 647651
2005 National Strength & Conditioning Association
THE BENEFITS OF A FUNCTIONAL EXERCISE CIRCUIT
FOR OLDER ADULTS
MICHAEL A. WHITEHURST,
1
BEVERLY L. JOHNSON,
2
CHERIE M. PARKER,
2
LEE E. BROWN,
3
AND
ALLISON M. FORD
1
1
Department of Exercise Science and Health Promotion, Florida Atlantic University, Davie, Florida 33314;
2
DeVos-Blum Family YMCA of Boynton Beach, Boynton Beach, Florida 33435;
3
FACSM Division of Kinesiology
and Health Promotion, California State University, Fullerton, California 92834.
ABSTRACT. Whitehurst, M.A., B.L. Johnson, C.M. Parker, L.E.
Brown, and A.M. Ford. The benets of a functional exercise cir-
cuit for older adults. J. Strength Cond. Res. 19(3):647651.
2005.The physical benets of a functional exercise circuit are
not well known in an elderly population. The purpose of this
study was to evaluate the effect of a functional exercise circuit
on mobility and perceived health in the elderly. Subjects were
119 men and women (aged 74 [4.2] years) who received pre-
and posttests of mobility (e.g., sit to stand, get up and go, timed
walk), exibility (sit and reach), and balance (standing reach)
and who completed the Medical Outcomes Study 36-Item Short-
Form Health Survey (SF-36). A supervised functional exercise
circuit that included 10 different upper- and lower-body exercis-
es performed under time constraints was performed 3 times per
week for 12 consecutive weeks. Paired t-tests showed signicant
differences at posttest for the get up and go (p 0.001), standing
reach (p 0.001), sit and reach (p 0.001), and selected items
from the SF-36, including physical functioning (p 0.001), pain
(p 0.001), vitality (p 0.001), and number of doctor visits (p
0.001). A functional exercise circuit such as the one employed
in this study may offer promise as an effective means of pro-
moting mobility and perceived health in older adults.
KEY WORDS. enhanced mobility, perceived health
INTRODUCTION
W
hile resistance exercise has been used exten-
sively during the past decade to promote
strength, muscle hypertrophy, and mobility
in the elderly (6, 7, 10, 17), few if any studies
have reported using a functional approach in
which movement patterns common to activities of daily
living (ADL) were employed as the primary exercise stim-
ulus. The idea that exercise should be strict linear move-
ments typical of resistance machines and free weights
may be impractical for many older adults. Rather, a func-
tional exercise, particularly one performed in a circuit
fashion, may be well suited to older persons wishing to
improve function and mobility.
Using an exercise circuit to induce physiological stress
in an effort to promote health-related tness is not new.
For example, circuit weight training has been shown to
improve strength and, to a lesser extent, cardiorespira-
tory endurance in young, healthy subjects (8, 19). Simi-
larly, circuit or workstation exercise interventions have
been used to improve function and physical work capacity
in stroke patients (4, 12) and cardiac patients (5). In a
recent study, Nelson et al. (13) exposed older adults to a
home-based exercise program that included progressive
resistance exercise and mobility challenges. Nelson and
colleagues found signicant improvements in dynamic
balance, whereas strength and gait speed did not differ
between exercise and control groups. Although the au-
thors concluded that a home-based exercise program of-
fers benets, it could be argued that their failure to nd
signicant results across all outcome measures resulted
from the older subjects inability to perform exercises cor-
rectly in the absence of feedback and/or sustain an ap-
propriate intensity throughout the exercise session.
Our intention was to develop a functional exercise cir-
cuit that required movement patterns and mobility chal-
lenges common to ADL. In doing so, we sought to provide
a supervised exercise setting and effectively eliminate the
need for specialized equipment while providing physically
demanding exercise performed in a group setting. We hy-
pothesized that the functional exercise circuit would pro-
vide an exercise stimulus suitable for improving function-
al mobility in older adults. In addition, considering that
a psychologic benet is often attributed to regular exer-
cise (1), we examined the inuence of the functional ex-
ercise circuit on perceived health. Again, consistent with
other forms of exercise, we hypothesized that the benets
of the functional exercise circuit would extend beyond the
physical.
METHODS
Subjects
This study sought to determine whether elderly subjects
could improve their mobility and perceived health from a
nontraditional functionally (i.e., movement patterns com-
mon to ADL) based exercise program. This study was ap-
proved by Florida Atlantic Universitys Institutional Re-
view Board for Human Subjects Research. Subjects were
119 (aged 73 [4.6] years) volunteers from Palm Beach
County, Florida. Upon phone inquiry, subjects were
scheduled for a physical examination (an informed con-
sent and a detailed medical history were also obtained).
Subjects whose medical history and/or physical exami-
nation showed more than 2 major coronary heart disease
risk factors and/or who presented with an unstable con-
dition (e.g., heart disease, high blood pressure, abnormal
levels of blood lipids) within the last 12 months and/or
who had mobility issues were referred to their physician
for follow-up (n 3) and deemed unt for participation
in this study.
Immediately following the physical examination, sub-
jects completed the Medical Outcomes Study 36-Item
Short-Form Health Survey (SF-36) and a battery of tests
that targeted mobility (e.g., sit to stand, get up and go,
timed walk), exibility (sit and reach), and balance
648 WHITEHURST, JOHNSON, PARKER ET AL.
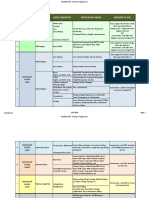
FIGURE 1. Layout of functional exercise circuit.
(standing reach). The SF-36 (numeric responses, e.g., 1
all of the time; 6 none of the time) dealt with general
health, physical functioning, mental state, social activity,
pain, and vitality. Subjects were also asked to provide the
number of falls, emergency room visits, hospitalizations,
and doctor visits, where pretest was dened as 12 months
prior to their participation in this study. All tests were
repeated within 1 week following the conclusion of the 12
weeks of continuous exercise.
Procedures
The sit-to-stand maneuver was electronically timed and
required the subject to rise from a seated to a standing
position, without the aid of the arms, as quickly as pos-
sible. The best of 3 trials was recorded. A detailed de-
scription of this test may be found elsewhere (18).
The get-up-and-go test required the subject to rise
from a seated position, walk 8 ft (2.44 m), turn, and re-
turn to the seated position as quickly as possible (14).
The timed walk test was an aerobic endurance test
lasting 6 minutes. Briey, the subject walked a rectan-
gular course (13.4 3.35 m) for 6 minutes, covering as
much distance as possible (14).
Flexibility was measured in the sit-and-reach position
using a standard sit-and-reach box, and the best of 3 tri-
als was recorded (9).
The standing-reach test was a eld test of balance and
provided a measure of the subjects stability and risk of
falling. Subjects stood with the shoulder of the dominant
arm next to a wall. Afxed to the wall was a slide. The
start position was dened as the subject grasping the
handle of the slide mechanism, arm in front of the body
and parallel to the oor. The subject moved the slide
mechanism forward by leaning forward as far as possible
or just prior to the point that a step was necessary to
avoid falling. The distance from the start position (mea-
sured from the handle on the slide mechanism) to the
stopping point was recorded. Each subject received 3 tri-
als, and the greatest reach was recorded. All tests were
administered in the order described.
Functional Exercise CircuitOverview
A functional exercise circuit was performed 3 times per
week for 12 consecutive weeks. The circuit consisted of 10
exercises or stations performed consecutively, each last-
ing 60 seconds, with 3 circuits completed each session.
During the 60 seconds, participants were able to complete
1030 repetitions before transitioning (1520 seconds) to
the next station. A total of 1530 subjects participated in
each session. Subjects were monitored at all times to en-
sure safety and adherence to good form and were in-
structed to avoid the Valsalva maneuver while perform-
ing the different exercises in the circuit. Subjects were
not allowed to complete more than several repetitions at
each station of the circuit for the rst week. More repe-
titions and hence difculty were introduced slowly during
subsequent weeks (weeks 23). A timer called out times
(e.g., 15, 30, 45 seconds) during the 60-second interval.
Finally, subjects wore a heart rate monitor while exercis-
ing and were instructed to monitor their intensity by
checking their monitor periodically (training heart rate
7080% predicted maximum heart rate) as well as using
the Borg scale (1314). Periodic inspections by the inves-
tigators showed that subjects were at or just below 70%
of their THR during the functional exercise circuit. Of the
36 possible sessions, subjects averaged slightly more than
30 sessions or 83% of all possible sessions.
While the stations of the circuit required specic
movement patterns, the circuit was designed to empha-
size level changes, directional changes, and the negoti-
ating of obstacles. In this way, the circuit was more than
just a repetitive process. Rather, the conguration of the
circuit and its inherent obstacles placed cognitive and at-
tentional demands on the subjects at all times. The sta-
tions were labeled by number and name while the sub-
jects rotated through the circuit numerically (12 . . . .10
1). See Figure 1 for a layout of the exercise circuit.
Functional Exercise Circuit
Wall Exercise. The subject stood with his or her back to
the wall. A large rubber ball (1.06 m) was placed between
the midback and the wall. While leaning against the ball,
the subject exed the knees, trying to attain a 90 bend
before returning to the straight-legged starting position.
Single Leg Balance. With a foam cushion (5.08 cm)
positioned near a wall, the subject balanced on 1 leg while
standing on the foam cushion. This task will was repeated
on both legs, approximately 30 seconds per leg.
Cross-Legged Seated Torso. The subject assumed a
seated cross-legged position (back straight) on the oor to
perform a series of 4 gentle stretches. With the arms out-
stretched and the hands resting on the knees, the rst
FUNCTIONAL EXERCISE CIRCUIT AND THE ELDERLY 649
movement included bending forward at the waist and
throughout the spine, in order to move the head toward
the oor, and then returning to the straight-back posi-
tion. The second and third movements required the sub-
ject to maintain the straight back while rotating the torso
position (arms were allowed to follow the torso but did
not provide assistance) as far as possible in one direction
and then in the opposite direction. The fourth and nal
movement required the subject to place the hands behind
the buttocks for support while arching the back such that
the chest moved toward the ceiling. Each position was
held for 310 seconds and repeated several times in se-
quence.
Modied Push-Up. From a kneeling position, the
hands were placed on the oor, shoulder width apart, and
arms straight. The goal was to lower the chest to the oor
and return to the straight-arm position. Subjects who
could not perform the modied push-up performed wall
push-ups in which their feet were shoulder width and
parallel and as far from the wall as could be tolerated
while they were still able to ex the arms and move the
chest as close to the wall as possible.
Crunch. While lying on the back, arms crossed against
the chest and knees bent so the feet were at on the oor,
the subject tucked the chin against the sternal notch and
raised the back from the oor as far as possible while, at
the same time, contracting the abdominal muscles such
that the back rounded and the chest moved toward the
bent knees. The subject held the upright position for 1
count before returning the back to the oor and repeating
the movement.
Superman. While lying facedown on the oor with
arms outstretched overhead, the subject lifted the thighs
and chest off the oor simultaneously. At the top, the sub-
ject paused for 1 count before lowering the chest and
thighs to the oor.
V-Sit. The subject assumed a seated position with the
legs outstretched, the back straight (some subjects placed
their hands on either side of the hips to assist in main-
taining a straight back), and the feet spread 0.61.2 m,
depending on individual capability. Alternating between
legs, the subject leaned toward an outstretched leg as far
as possible. Upon stretching to a comfortable limit, the
subject paused and held the stretch for 510 seconds be-
fore returning to the start position. The subject then
stretched toward the other leg. This process was repeated
several times for each leg.
Stretch and Balance. Standing with feet shoulder
width apart and arms at the sides of the body, the subject
reached overhead with the right arm while simultaneous-
ly abducting the left leg such that that foot left the oor.
In the outstretched position, the arm and leg formed a
diagonal line that was held for as long as 10 seconds. The
same action was repeated for the other side of the body.
These movements were repeated 24 times per side. Sub-
jects were allowed to hold a chair with the uninvolved
hand for support.
Star Exercise. Six rubber cones (height 0.07 m) were
positioned in a circle around the subject, with each cone
approximately 0.094 m from the subject. While balancing
on 1 leg, the subject exed the knee, reached down, and
touched the top of a cone. The subject returned to the
upright posture (starting position) before attempting to
touch another cone. It should be pointed out that the sub-
jects used opposing limbs (e.g., right leg as the base and
left arm to touch the cone). Additionally, the subject was
oriented in a constant direction during the task. This
meant that touching a cone in the rear required bending
and exing the knee and blindly reaching back. The long-
term goal for each subject was for him or her to touch the
6 cones with all combinations of balanced leg and out-
reached arm. However, not all subjects could touch all
cones at all times without temporarily losing balance and
having to temporarily stabilize themselves with the other
foot.
Weight Transfer. The subject picked up tote bags, one
in each hand, representing approximately 20% of his or
her body weight. With the arms at the sides, the subject
walked around the outside of the exercise circuit and
through or around obstacles that included stepping over
barriers (there were 3 to choose from: 4.7, 7.0, and 9.4
cm), reversing direction, and walking backward while car-
rying the tote bags.
Statistical Analyses
Mean and standard deviation were calculated for each
variable. Paired t-tests were used to determine differenc-
es over time for each variable. The p 0.05 was used. All
data analysis was completed using SPSS version 11.0
(SPSS Inc., Chicago, IL).
RESULTS
As shown in Table 1, paired t-tests detected signicant
differences in pre- and posttests for get up and go ( p
0.000), standing reach ( p 0.000), sit and reach ( p
0.000), self-reports of physical functioning ( p 0.001),
pain ( p 0.001), vitality ( p 0.001), and doctor visits
( p 0.000). The initial alpha level of p 0.05 was cor-
rected (0.05 per number of paired t-tests or 18).
DISCUSSION
This study sought to evaluate the relative value of a func-
tional exercise circuit as a means of promoting mobility
and perceived health in an elderly population. On the ba-
sis of the results obtained in the get-up-and-go test, it
appears that the functional exercise circuit intervention
promoted mobility. Although not signicant (0.006), the
timed walk test, indicative of cardiorespiratory endur-
ance and mobility, improved by 7.4%. These ndings are
consistent with other studies in which mobility improved
in an elderly population following exercise training (6, 7,
10). However, unlike previous studies, the current study
employed movements common to ADL, with resistance
provided by the subjects body weight. Given the nature
of the circuit (e.g., directional changes, obstacles) and the
time limit imposed at each station, we speculate that a
progressive overload was produced that manifested itself
as improved mobility.
Standing reach, a eld measure of stability and fall
risk, improved 12.9%. This improvement may be a prod-
uct of the dynamic nature of the training regimen. A dy-
namic exercise intervention in the form of agility training
was employed in a recent investigation by Liu-Ambrose
et al. (11). Using body sway as a measure of fall risk,
these authors reported a 29.6 and 30.6% reduction in
sway following agility and resistance training. Given that
there was no signicant difference in body sway following
agility or resistance training, it could be argued that the
more functionally based agility exercise is at least as good
as traditional resistance exercise at reducing the risk of
650 WHITEHURST, JOHNSON, PARKER ET AL.
TABLE 1. Changes in mobility and perceived health following 12 weeks of functional exercise (mean SD).
Variable Test 1 Test 2 % change Signicance
Get up and go
Sit to stand
Standing reach (m)
Timed walk
Sit and reach (m)
7.92 2.1
0.78 0.65
0.3432 0.08
7.5 1.8
0.248 0.14
7.25 2.0
0.74 1.5
0.386 0.06
8.1 2.2
0.289 0.13
8.4
5.1
12.9
7.4
14.0
0.000*
0.816
0.000*
0.006
0.000*
Physical functioning
Role physical
Pain
General health
Vitality
66.5 23.2
67.2 38.6
66.8 21.1
68.9 18.6
57.5 21.4
72.7 20.7
73.9 34.9
73.2 20.9
70.1 17.2
63.5 20.0
8.5
9.0
8.7
1.7
9.4
0.001*
0.110
0.001*
0.452
0.001*
Social functioning
Role emotional
Mental health
Falls
85.3 19.4
79.2 35.2
76.0 15.3
0.18 0.64
90.0 17.0
83.1 30.3
79.5 16.2
0.08 0.30
5.2
4.7
4.4
55.5
0.006
0.252
0.008
0.131
Emergency department visits
Hospitalizations
Doctor visits
Number of medications
0.11 0.34
0.08 0.27
1.34 1.1
3.87 2.6
0.03 0.18
0.01 0.09
0.91 0.87
3.68 2.8
72.7
87.5
32.0
4.9
0.038
0.006
0.000*
0.110
* p 0.002.
falling in older subjects. Using another form of dynamic
exercise, Tai Chi, Wolf et al. (20) found that Tai Chi train-
ing reduced the risk of multiple falls by 47% compared to
those of an education group. We would suggest that the
functional exercise circuit employed in this study was
similar to the aforementioned dynamic training interven-
tions. Assuming as much, a functional or dynamic ap-
proach may activate the centers for postural control (i.e.,
somatosensory, vestibular, visual) (15) with the synaptic
plasticity occurring in the postural control centers as a
function of repetition and learning (18). Speculatively, an
additional benet of the functional exercise circuit was
task complexity. That is, the required movement patterns
were not always easy to remember or easy to produce.
Hence, the functional exercise circuit represented a con-
tinuum of perceptual, cognitive, and action challenges
that, over time, may have affected cognitive and cerebel-
lum function as well (16).
The improved sit-and-reach performance was not un-
expected. Again, given the dynamic nature of the exer-
cise, including level changes and both static and dynamic
movements, improved hip and lower-back exion was ex-
pected and consistent with the ndings of other studies
in which exibility was targeted through specic exercis-
es (2).
Perceptions of physical functioning, pain, and vitality
were all signicantly improved following training. As far
as physical functioning is concerned, there appears to be
a relationship between function and mobility, particularly
walking speed (3). Therefore, it is logical to conclude that
improved mobility was associated with a high degree of
physical functioning. Similarly, subjects in this study ap-
peared to perceive less pain and feel more vital following
12 weeks of exposure to a functional exercise circuit. Fi-
nally, a reduction in the number of doctor visits would
seem to go hand in hand with improved mobility as well
as a reduction in pain and a feeling of more vitality. Other
investigators have reported that older adults who report
a high level of physical functioning also perceived them-
selves as being healthy (21). Hence, such subjects are less
apt to make scheduled visits to their doctor.
This study offers support for using a functional exer-
cise circuit as a safe and cost-effective alternative to tra-
ditional exercise interventions for older adults. Subjects
did appear to derive both functional and perceived health
benets from their participation in the functional exercise
circuit. Clearly, these nding must be interpreted with
caution. Without an experimental investigation, we may
not conclude a cause-and-effect relationship. However,
considering the adherence rate of 83% and the fact that
no subjects sustained injury during the course of the
study, the functional exercise circuit did appear to be
suitable for older adults. Future investigations should fo-
cus on comparing a traditional exercise intervention with
the functional exercise circuit.
PRACTICAL APPLICATIONS
A practitioner may nd that a functional exercise circuit
can be both challenging and benecial for an elderly sub-
ject wishing to improve physical functioning and mobility.
In addition, because the functional exercise circuit in-
cludes a series of movement patterns that must be pro-
duced under varying conditions (i.e., space negotiations,
directional changes, level changes), the subject is afforded
cognitive stimulation. Still, it is unclear at this time
whether better results could be expected from a function-
al exercise circuit like the one employed here when com-
pared to traditional exercise interventions. Nevertheless,
considering that none of the subjects in this study was
injured and that the participation is both time- and cost-
effective, it seems logical to consider a functional exercise
circuit an alternative form of exercise for older adults.
REFERENCES
1. AMERICAN COLLEGE OF SPORTS MEDICINE. ACSMs Guidelines
for Exercise Testing and Prescription (6th ed.). Philadelphia:
Lippincott Williams & Wilkins, 2000.
2. BARBOSA, A.R., J.M. SANTAREM, W.J. FILHO, AND M.F. MARUC-
CI. Effects of resistance training on the sit-and-reach test in
elderly women. J. Strength Cond. Res. 1:1418. 2002.
FUNCTIONAL EXERCISE CIRCUIT AND THE ELDERLY 651
3. CRESS, M.E., D.M. BUCHNER, K.A. QUESTAD, P.C. ESSELMAN,
B.J. DELATEUR, AND R.S. SCHWARTZ. Exercise: Effects on phys-
ical functional performance in independent older adults. J. Ger-
ontol. A Biol. Sci. Med. Sci. 5:M242248. 1999.
4. DEAN, C.M., C.L. RICHARDS, AND F. MALOUIN. Taks-related cir-
cuit training improves performance of locomotor tasks in
chronic stroke: A randomized, controlled trial. Arch. Phys. Med.
Rehabil. 4:409417. 2000.
5. DEGROOT, D.W., T.J. QUINN, R. KERTZER, N.B. VROMAN, AND
W.B. OLNEY. Circuit weight training in cardiac patients: De-
termining optimal workloads for safety and energy expendi-
ture. J. Cardiopulm. Rehabil. 2:145152. 1998.
6. FIATARONE, M.A., E.C. MARKS, N.D. RYAN, C.N. MEREDITH,
L.A. LIPSITZ, AND W.J. EVANS. High-intensity strength training
in nonagenarians. Effects on skeletal muscle. JAMA 22:3029
3034. 1990.
7. FRONTERA, W.R., C.N. MEREDITH, K.P. OREILLY, H.G. KNUTT-
GEN, AND W.J. EVANS. Strength conditioning in older men:
Skeletal muscle hypertrophy and improved function. J. Appl.
Physiol. 3:10381044. 1988.
8. GETTMAN, L.R., J.J. AYRES, M.L. POLLOCK, AND A. JACKSON.
The effect of circuit weight training on strength, cardiorespi-
ratory function, and body composition of adult men. Med. Sci.
Sports Exerc. 3:171176. 1978.
9. GOLDING, L.A., C.R. MYERS, AND W.E. SINNING, eds. Ys Way to
Physical Fitness: The Complete Guide to Fitness Testing and
Instruction (3rd ed.). Champaign, IL: Human Kinetics, 1989.
10. HRUDA, K.V., A.L. HICKS, AND N. MCCARTNEY. Training for
muscle power in older adults: Effects on functional abilities.
Can. J. Appl. Physiol. 2:178189. 2003.
11. LIU-AMBROSE, T., K.M. KHAN, J.J. ENG, P.A. JANSSEN, S.R.
LORD, AND H.A. MCKAY. Resistance and agility training reduce
fall risk in women aged 75 to 85 with low bone mass: A 6-
month randomized, controlled trial. J. Am. Geriatr. Soc. 5:657
665. 2004.
12. LOW CHOY, N., R. ISLES, R. BARKER, AND J. NITZ. The efcacy
of a work-station intervention programme to improve function-
al ability and exibility in aging clients with cerebral palsy: A
pilot study. Disabil. Rehabil. 21:12011207. 2003.
13. NELSON, M.E., J.E. LAYNE, M.J. BERNSTEIN, A. NUERNBERGER,
C. CASTANEDA, D. KALITON, J. HAUSDORFF, J.O. JUDGE, D.M.
BUCHNER, R. ROUBENOFF, AND M.A. FIATRONE SINGH. The ef-
fects of multidimensional home-based exercise on functional
performance in elderly people. J. Gerontol. A Biol. Sci. Med. Sci.
2:154160. 2004.
14. RIKLI, R.E., AND C.J. JONES. Senior Fitness Test Manual.
Champaign, IL: Human Kinetics, 2001.
15. SHUMWAY-COOK, A., AND M.H. WOOLLACOTT. Motor Control:
Theory and Practical Applications (2nd ed.). Philadelphia: Lip-
pincott Williams & Wilkins, 2001.
16. SWANSON, L.W. Brain Architecture: Understanding the Basic
Plan. New York: Oxford University Press, 2003.
17. WHITEHURST, M., J. BOONE, S. DOMBROWSKI, J. WEINER, AND
L.E. BROWN. The effect of resistance training on functional
ability in the elderly. Med. Sci. Sports Exerc. 5S:S131. 1993.
18. WHITEHURST, M., L.E. BROWN, A. DANGELO, AND S. EIDELSON.
Functional mobility performance in an elderly population with
lumbar spinal stenosis. Arch. Phys. Med. Rehabil. 4:464467.
2001.
19. WILMORE, J.H., R.B. PARR, R.N. GIRANDOLA, P. WARD, P.A. VO-
DAK, T.J. BARSTOW, T.V. PIPES, G.T. ROMERO, AND P. LESLIE.
Physiological alterations consequent to circuit weight training.
Med. Sci. Sports Exerc. 10:7984. 1978.
20. WOLF, S.L., R.W. SATTIN, M. KUTNER, M. OGRADY, A.I.
GREENSPAN, AND R.J. GREGOR. Intense tai chi exercise training
and fall occurrences in older, transitionally frail adults: A ran-
domized, controlled trial. J. Am. Geriatr. Soc. 12:16931701.
2003.
21. YASUNAGA, A., AND M. TOKUNAGA. The relationships among
exercise behavior, functional ADL, and psychological health in
the elderly. J. Physiol. Anthropol. Appl. Hum. Sci. 6:33943.
2001.
Acknowledgments
This study was supported by a grant from the Quantum
Foundation, Inc., West Palm Beach, Florida.
Address correspondence to Dr. Michael Whitehurst,
whitehur@fau.edu.
You might also like
- Injury Mechanisms For Anterior Cruciate Ligament Injuries in Team HandballDocument11 pagesInjury Mechanisms For Anterior Cruciate Ligament Injuries in Team HandballDébora SouzaNo ratings yet
- Lesõoes Músculo Esqueléticas No Ombro Do AtletaDocument5 pagesLesõoes Músculo Esqueléticas No Ombro Do AtletaDébora SouzaNo ratings yet
- Blunted Muscle Vasodilatation During Chemoreceptor Stimulation in Patients With Heart FailureDocument8 pagesBlunted Muscle Vasodilatation During Chemoreceptor Stimulation in Patients With Heart FailureDébora SouzaNo ratings yet
- Treinamento Sensório MotorDocument8 pagesTreinamento Sensório MotorDébora SouzaNo ratings yet
- Força Muscular em Superficies Instaveis e EstáveisDocument5 pagesForça Muscular em Superficies Instaveis e EstáveisDébora SouzaNo ratings yet
- Feedforward Vs FeedbackDocument10 pagesFeedforward Vs FeedbackDébora Souza100% (1)
- As Essências Do Treinamento Integrado - Mike ClarkDocument8 pagesAs Essências Do Treinamento Integrado - Mike ClarkDébora SouzaNo ratings yet
- Controle Da Postura EretaDocument20 pagesControle Da Postura EretaDébora SouzaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Startup Time Reduction For Combined Cycle Power PlantsDocument8 pagesStartup Time Reduction For Combined Cycle Power PlantsEnrique TamayoNo ratings yet
- Robodrill 01Document298 pagesRobodrill 01vuchinhvdcNo ratings yet
- JEE Mains 2024 Question Paper Shift 2 27 JanDocument4 pagesJEE Mains 2024 Question Paper Shift 2 27 JanAnjali SahooNo ratings yet
- All About Ocean Life-Rachel BladonDocument6 pagesAll About Ocean Life-Rachel BladonRichard TekulaNo ratings yet
- Rodents and Sectional Title ComplexDocument2 pagesRodents and Sectional Title ComplexFredSmith777No ratings yet
- Lord You Know All Things, You Can Do All Things and You Love Me Very MuchDocument4 pagesLord You Know All Things, You Can Do All Things and You Love Me Very Muchal bentulanNo ratings yet
- New-DLP Phase2 Assignment-3 Module-B Final-9.8.18Document6 pagesNew-DLP Phase2 Assignment-3 Module-B Final-9.8.18PNo ratings yet
- High Resolution Computed Tomography of The Lungs - UpToDateDocument83 pagesHigh Resolution Computed Tomography of The Lungs - UpToDatejjjkkNo ratings yet
- (VOLKSWAGEN) Manual de Taller Volkswagen Jetta 1999 2006Document4 pages(VOLKSWAGEN) Manual de Taller Volkswagen Jetta 1999 2006Carlos AntonioNo ratings yet
- Laboratory Diagnosis of Parasitic DiseasesDocument57 pagesLaboratory Diagnosis of Parasitic DiseasesAmanuel MaruNo ratings yet
- Ship Captain's Medical Guide - 22nd EdDocument224 pagesShip Captain's Medical Guide - 22nd EdcelmailenesNo ratings yet
- 3 Composites PDFDocument14 pages3 Composites PDFKavya ulliNo ratings yet
- NANOGUARD - Products and ApplicationsDocument2 pagesNANOGUARD - Products and ApplicationsSunrise VenturesNo ratings yet
- Handover Paper Final 22 3 16 BJNDocument13 pagesHandover Paper Final 22 3 16 BJNsisaraaah12No ratings yet
- Remote Control RC902V1 ManualDocument3 pagesRemote Control RC902V1 ManualdezdoNo ratings yet
- Banco de Oro (Bdo) : Corporate ProfileDocument1 pageBanco de Oro (Bdo) : Corporate ProfileGwen CaldonaNo ratings yet
- Indian MaDocument1 pageIndian MaAnass LyamaniNo ratings yet
- FCE Writing 14 - ArticleDocument4 pagesFCE Writing 14 - Articlepingu70No ratings yet
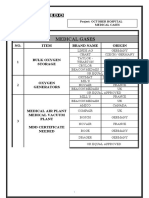
- Medical Gases: NO. Item Brand Name OriginDocument4 pagesMedical Gases: NO. Item Brand Name OriginMahmoud AnwerNo ratings yet
- Radiation Hazards & Radiation ProtectionDocument62 pagesRadiation Hazards & Radiation ProtectionGurupada JanaNo ratings yet
- Philosophy For Management and DisciplineDocument8 pagesPhilosophy For Management and Disciplineapi-300120362No ratings yet
- Nursing Care of A Family With An InfantDocument26 pagesNursing Care of A Family With An InfantJc GarciaNo ratings yet
- Monopoly Tycoon TipsDocument8 pagesMonopoly Tycoon TipsVictoria SmithNo ratings yet
- Charla Krupp - How To Never Look Fat Again - Over 1,000 Ways To Dress Thinner - Without Dieting!-Grand Central Publishing (2010) PDFDocument316 pagesCharla Krupp - How To Never Look Fat Again - Over 1,000 Ways To Dress Thinner - Without Dieting!-Grand Central Publishing (2010) PDFben0% (1)
- 2mw Biomass Gasification Gas Power Plant ProposalDocument9 pages2mw Biomass Gasification Gas Power Plant ProposalsabrahimaNo ratings yet
- Activity 2: College of EngineeringDocument3 pagesActivity 2: College of EngineeringMa.Elizabeth HernandezNo ratings yet
- Worksheet 2 - TLC - Updated Summer 2021Document4 pagesWorksheet 2 - TLC - Updated Summer 2021Bria PopeNo ratings yet
- Carapace DigitalDocument15 pagesCarapace DigitalVillain ChatNo ratings yet
- Mercury II 5000 Series Encoders: High Performance Encoders With Digital OutputDocument21 pagesMercury II 5000 Series Encoders: High Performance Encoders With Digital OutputRatnesh BafnaNo ratings yet