Professional Documents
Culture Documents
ContentServer 2
Uploaded by
Ni Wayan Ana PsOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ContentServer 2
Uploaded by
Ni Wayan Ana PsCopyright:
Available Formats
Anaesthesia and Intensive Care, Vol. 39, No.
3, May 2011
Pre-eclampsia and eclampsia are well-
known causative factors of posterior reversible
encephalopathy syndrome (PRES). As the name
suggests, manifestations of PRES are usually
transient and complete recovery is the rule. Most
cases of PRES reported in the obstetric literature
involve postpartum patients, with only a few cases
of antepartum PRES
1-4
. We report a primigravid
woman who presented with an abrupt onset of
eclampsia and PRES. She was managed with
supportive care, labour was induced and maternal
and neonatal outcomes were good. The challenges
posed by PRES occurring in the antepartum period,
as opposed to non-obstetric or postpartum PRES,
are discussed.
CASE HISTORY
A 25-year-old primigravid woman with eight
months of amenorrhoea presented with history of
a fall at home, six hours before admission to the
emergency department of our hospital. Her husband
gave the history of fve episodes of generalised
tonic-clonic convulsions over a period of three hours
and three episodes of vomiting. She had received
regular antenatal checkups and her examination
during the last visit (one month before the episode)
had not revealed any abnormalities.
On examination in the emergency department,
she was conscious, disoriented and restless. Both
her pupils were 3 mm in size and reacting to light.
There was a lacerated wound of the scalp over the
occipital area. She was afebrile, pulse rate was
90 bpm, blood pressure 184/140 mmHg, respiratory
rate 38 breaths/minute and arterial oxygen saturation
(SpO
2
) 99% on room air. There was no pedal oedema
and central cardiovascular system and respiratory
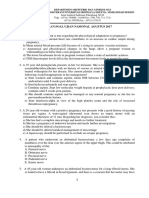
system fndings were normal. An urgent non-contrast
computed tomography (CT) scan of the head,
performed under sedation (total dose of propofol
60 mg), showed ill-defned hypodense areas in both
parieto-occipital lobes and the right temporal lobe,
involving the cortex and subcortical white matter
(Figure 1). There was no intracranial haemorrhage.
Based on these fndings, PRES and superior sagittal
sinus thrombosis were considered the differential
diagnosis.
The patient was transferred to the surgical
intensive care unit, where on admission she was
restless, with pulse rate 84 bpm and blood pressure
of 196/124 mmHg. She was administered intra-
venous fentanyl 100 g, midazolam 1 mg and labetalol
* M.D., Assistant Professor, Department of Anaesthesiology.
D.M.R.D., D.N.B., Assistant Professor, Department of Radiodiagnosis.
M.D., Assistant Professor, Department of Obstetrics and Gynaecology.
M.D., D.N.B., Assistant Professor, Department of Obstetrics and
Gynaecology.
** M.D., Professor and Head, Department of Obstetrics and Gynaecology.
M.D., Professor and Head, Department of Anaesthesiology.
Address for correspondence: Dr H. V. Hegde, Department of
Anaesthesiology, Shri Dharmasthala Manjunatheshwara College of
Medical Sciences and Hospital, Dharwad, Karnataka 580 009, India. Email:
drharryhegde@yahoo.co.in
Accepted for publication on December 9, 2010.
A rare case of antepartum posterior reversible
encephalopathy syndrome
H. V. HEGDE*, P. B. PATIL, R. RAMESHKUMAR, T. H. SUNITA, M. T. BHAT*, R. M. DESAI**,
P. R. RAO
Departments of Anaesthesiology, Radiodiagnosis, Obstetrics and Gynaecology, Shri Dharmasthala Manjunatheshwara College of
Medical Sciences and Hospital, Dharwad, Karnataka, India
SUMMARY
Pre-eclampsia and eclampsia are well-known causative factors of posterior reversible encephalopathy syndrome
(PRES). There are only a few reported cases of antepartum PRES. We report a 25-year-old primigravid woman
who presented with eight months of amenorrhoea and an abrupt onset of eclampsia associated with a history of a
fall. A computed tomography scan ruled out intracranial haemorrhage and PRES was diagnosed. She responded
well to supportive care, labour was induced and maternal and neonatal outcomes were good. Antepartum PRES
poses different challenges to those of PRES in non-obstetric or postpartum patients, because of the additional
management aspects required to ensure foetal wellbeing. We were posed with a difficult decision about the
disadvantages of caesarean section versus those of vaginal delivery in our patient.
Key Words: posterior reversible encephalopathy syndrome, eclampsia, antepartum, seizures
Anaesth Intensive Care 2011; 39: 499-502
500
H. V. HEGDE, P. B. PATIL ET AL
Anaesthesia and Intensive Care, Vol. 39, No. 3, May 2011
20 mg. The right radial artery was cannulated
and intra-arterial blood pressure monitoring
initiated. Magnesium sulphate 5 g was administered
intravenously over 10 minutes, followed by an
infusion at 1 g/hour. The blood pressure reduced to
166/110 mmHg. Intravenous betamethasone 12 mg
was administered and repeated after 12 hours to
accelerate foetal lung maturity
5
.
Her baseline investigations were haemoglobin
128 g/l, leucocyte count 13,830 /mm
3
(neutrophils
88%, lymphocytes 6%), platelet count 131,000 /mm
3
,
blood sugar 5.1 mmol/l, serum Na
+
134 mmol/l,
serum K
+
4.3 mmol/l, blood urea 7.8 mmol/l, serum
creatinine 97.2 mol/l, uric acid 0.5 mmol/l, urinary
protein 4
+
, prothrombin time 12.8 seconds (control
12.2 seconds), international normalised ratio 1.04,
activated partial thromboplastin time 28 seconds
(control 30 seconds) and liver function tests were
normal. A bedside obstetric ultrasound showed a live
foetus with estimated gestational age of 31 weeks
and body weight of 1.1 kg (<5th percentile of the
expected weight, representing severe intrauterine
growth retardation). On vaginal examination,
the cervix was 50% effaced, 2 cm dilated and
membranes were intact. Her blood pressure
remained in the range of 152/106 to 170/118 mmHg
and pulse rate 70 to 85 /minute over the next three
hours. An ophthalmic evaluation showed a normal
fundus.
While preparations for caesarean section were
made, her sensorium improved and four hours after
admission to the surgical intensive care unit she
started obeying commands. At review, it was decided
to induce labour, in view of the severe intrauterine
FIGURE 1: Computed tomography scan on admission. Ill-defined
hypodense areas in bilateral parieto-occipital and right temporal
lobes.
growth retardation and prematurity, good Bishop
Score, adequate control of blood pressure and no
signs of maternal deterioration. Induction of labour
was with misoprostol 50 g vaginally. She had
spontaneous rupture of membranes four hours later
and contractions were augmented with an oxytocin
infusion. The labour progressed smoothly, the foetus
being monitored continuously by cardiotocograph.
The woman was delivered of a male baby (weight
950 g) vaginally, 14 hours after induction. The
baby cried soon after the birth and in the neonatal
intensive care unit was managed with oxygen
administered via hood, antibiotics and intravenous
fuids. He developed sepsis on the third day but was
treated successfully and discharged on the 25th day
with a weight of 1.35 kg.
The patients urine output was 800 ml in the frst
12 hours and her blood pressure was between
150/106 and 170/118 mmHg during the active phase
of labour. She did not receive analgesia during
the course of labour as she was unable to give
adequate feedback regarding the pain. Her blood
pressure gradually reduced to 140/100 mmHg while
remaining on the magnesium sulphate infusion and
also receiving intravenous labetalol 20 mg six hourly.
Serum magnesium level was 1.5 mmol/l. Magnesium
sulphate and labetalol were stopped 24 hours after
delivery and oral nifedipine 10 mg twice daily was
started. She was transferred to the ward on the third
day. A magnetic resonance imaging (MRI) scan
performed on the eighth day (Figure 2) showed near-
complete resolution of the lesions seen on CT at
admission and also excluded superior sagittal sinus
thrombosis. The patient was discharged on day 10,
FIGURE 2: Follow-up magnetic resonance image eight days later,
showing near-complete resolution of the lesions seen in Figure 1.
501
CASE REPORT
Anaesthesia and Intensive Care, Vol. 39, No. 3, May 2011
showing complete neurological recovery. She gave
consent for publication of this report.
DISCUSSION
PRES has been reported in a wide variety of clinical
settings. Presentation is varied but the most common
feature has been hypertension. Precipitating factors
6
include abrupt hypertension, immunosuppressant
drug use, infection, pre-eclampsia, eclampsia and
renal disease. Rarely, intrathecal morphine
7
and
intravenous caffeine therapy for post lumbar puncture
headache
8
have also been implicated as causative
factors.
Other presenting symptoms include seizures,
encephalopathy, visual symptoms and headache
6
.
Although most patients recover completely, a 27-year-
old woman in the 38th week of pregnancy who
developed persistent hypertension, complicated by
fatal subarachnoid haemorrhage, has been reported
1
.
PRES may also be associated with intracerebral
haemorrhage, which is generally considered an
atypical fnding. The clinical outcome of PRES with
associated intracerebral haemorrhage appears more
variable
9
.
Although PRES classically manifests in parieto-
occipital white or grey matter, the temporal lobes,
frontal lobes, brainstem and cerebellum may be
involved
10
. The posterior cerebral circulation is
thought to be more susceptible, possibly because
of lower sympathetic innervation than that of the
internal carotid artery territory, with a consequent
reduction in autoregulation of already impaired areas
of circulation
11
. The exact pathogenesis of PRES
remains incompletely understood and is likely
multifactorial. The most likely mechanism in an
eclamptic patient is vasogenic oedema secondary to
an acute increase in arterial blood pressure, which
overwhelms the autoregulatory capacity of the
cerebral vasculature causing arteriolar vasodilation,
endothelial dysfunction and interstitial extravasation
of fuid
2,10
. In a retrospective analysis of 120
patients, Fugate et al
12
reported a high prevalence
of autoimmune and infammatory conditions in
PRES patients, suggesting that endothelial dys-
function may lie at the core of its pathophysiology.
PRES is a clinical and radiological diagnosis.
Clinical fndings are not suffciently specifc but
neuroimaging is often characteristic
13
. It is important
to distinguish PRES from acute stroke, to guide
treatment
14
. Even though MRI is considered the
investigation of choice to diagnose PRES
15,16
, this
would have required either deep sedation or general
anaesthesia during the procedure, thus exposing our
patient to the risks of aspiration, haemodynamic
fuctuation and the direct and indirect effects of
maternally administered medications on the foetus.
It might also have led to a signifcant delay in
instituting treatment. The CT scan ruled out
trauma and intracranial haemorrhage as the causes,
confrming the history of a seizure frst and then the
fall. Clinical and radiological fndings were more in
favour of PRES rather than superior sagittal sinus
thrombosis and subsequent MRI confrmed resolution
of the pathology.
We opted in favour of induction of labour and
vaginal delivery for the following reasons: the patient
did not have intracranial haemorrhage and showed
rapid neurological improvement; this avoided the
short- and long-term maternal risks of caesarean
delivery
10
and the neonatal outcome was not expected
to be favourable (preterm with severe intrauterine
growth retardation).
The main signifcance of this report lies in the
antepartum presentation of PRES. Antepartum
PRES poses different challenges to PRES in non-
obstetric or postpartum patients because of the
additional management aspects to ensure foetal
wellbeing. We were posed with a diffcult decision
when balancing the disadvantages of caesarean
section versus the risks of vaginal delivery and the
rapid neurological improvement of the patient
infuenced our decision. This case supports others
in suggesting that the outcome for obstetric patients
with PRES is favourable and that timely supportive
therapy is the single most important aspect of
management. Magnesium sulphate was effective
in stabilising this patient. Labour pain might have
contributed to the slightly higher than recommended
blood pressure because we did not provide analgesia
during labour, other than fentanyl at admission to
the surgical intensive care unit. In addition, an
infusion of labetalol (rather than the intermittent
dosing) would probably have avoided fuctuations in
blood pressure.
Although PRES was frst described in 1996
17
and
is considered a rare clinical syndrome, a single
search term of posterior reversible encephalopathy
syndrome yielded nearly 450 articles in PubMed,
with more than 200 articles (mostly case reports and
a few case series) published in the last two years.
This indicates increased awareness about PRES
among clinicians and the impact of widespread
availability of imaging modalities like CT and MRI.
One obstetric textbook states that the radiological
and clinical features of PRES are almost universally
present in eclamptic patients
10
. This questions
whether PRES should still be considered a rare
syndrome, especially amongst obstetric patients,
502
H. V. HEGDE, P. B. PATIL ET AL
Anaesthesia and Intensive Care, Vol. 39, No. 3, May 2011
and whether all eclamptic patients should undergo
neuroimaging. A study of PRES in severe pre-
eclampsia and eclampsia may help. Early recognition
of PRES is important for timely institution of
therapy, which typically consists of gradual blood
pressure control and removal or management of
precipitating factors.
REFERENCES
1. Servillo G, Striano P, Striano S, Tortora F, Boccella P, De
Robertis E et al. Posterior reversible encephalopathy syndrome
(PRES) in critically ill obstetric patients. Intensive Care Med
2003; 29:2323-2326.
2. Powell ES, Goldman MJ. Posterior reversible encephalopathy
syndrome (PRES) in a thirty-six-week gestation eclamptic. J
Emerg Med 2007; 33:377-379.
3. Gasco J, Rangel-Castilla L, Clark S, Franklin B,
Satchithanandam L, Salinas P. Hemorrhagic stroke with intra-
ventricular extension in the setting of acute posterior reversible
encephalopathy syndrome (PRES): case report. Neurocirugia
(Astur) 2009; 20:57-61.
4. Morelli N, Gori S, Michelassi MC, Falorni M, Cafforio G,
Bianchi MC et al. Atypical posterior reversible encephalopathy
syndrome in puerperium. Eur Neurol 2008; 59:195-197.
5. Brownfoot FC, Crowther CA, Middleton P. Different corticos-
teroids and regimens for accelerating fetal lung maturation for
women at risk of preterm birth. Cochrane Database Syst Rev
2008; 4:CD006764.
6. Lee VH, Wijdicks EF, Manno EM, Rabinstein AA. Clinical
spectrum of reversible posterior leukoencephalopathy syn-
drome. Arch Neurol 2008; 65:205-210.
7. Eran A, Barak M. Posterior reversible encephalopathy syn-
drome after combined general and spinal anesthesia with
intrathecal morphine. Anesth Analg 2009; 108:609-612.
8. Ortiz GA, Bianchi NA, Tiede MP, Bhatia RG. Posterior revers-
ible encephalopathy syndrome after intravenous caffeine for
post-lumbar puncture headaches. AJNR Am J Neuroradiol
2009; 30:586-587.
9. Aranas RM, Prabhakaran S, Lee VH. Posterior reversi-
ble encephalopathy syndrome associated with hemorrhage.
Neurocrit Care 2009; 10:306-312.
10. Pregnancy Hypertension. In: Cunningham FG, ed. Williams
Obstetrics, 23rd ed. New York, NY: McGraw-Hill 2010. p. 706-
756.
11. Witlin AG, Friedman SA, Egerman RS, Frangieh AY, Sibai
BM. Cerebrovascular disorders complicating pregnancy
beyond eclampsia. Am J Obstet Gynecol 1997; 176:1139-1148.
12. Fugate JE, Claassen DO, Cloft HJ, Kallmes DF, Kozak OS,
Rabinstein AA. Posterior reversible encephalopathy syndrome:
associated clinical and radiologic findings. Mayo Clin Proc
2010; 85:427-432.
13. Moratalla MB. Posterior reversible encephalopathy syndrome.
Emerg Med J 2010; 27: 547.
14. Stott VL, Hurrell MA, Anderson TJ. Reversible posterior
leukoencephalopathy syndrome: a misnomer reviewed. Intern
Med J 2005; 35:83-90.
15. Casey SO, Sampaio RC, Michel E, Truwit CL. Posterior
reversible encephalopathy syndrome: utility of fluid-attenuated
inversion recovery MR imaging in the detection of cortical and
subcortical lesions. Am J Neuroradiol 2000; 21:1199-1206.
16. Covarrubias DJ, Luetmer PH, Campeau NG. Posterior revers-
ible encephalopathy syndrome: prognostic utility of quantita-
tive diffusion-weighted MR images. Am J Neuroradiol 2002;
23:1038-1048.
17. Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A et
al. A reversible posterior leukoencephalopathy syndrome. N
Engl J Med 1996; 334:494-500.
Copyright of Anaesthesia & Intensive Care is the property of Australian Society of Anaesthetists and its content
may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express
written permission. However, users may print, download, or email articles for individual use.
You might also like
- 4810cr10 PDFDocument2 pages4810cr10 PDFdr.putra888No ratings yet
- Spontaneous Haemorrhagic Stroke Complicating Severe Pre-Eclampsia in Pregnancy: A Case Report in A Resource-Limited Setting in CameroonDocument4 pagesSpontaneous Haemorrhagic Stroke Complicating Severe Pre-Eclampsia in Pregnancy: A Case Report in A Resource-Limited Setting in CameroonDewina Dyani RosariNo ratings yet
- Postpartum Eclampsia PDFDocument2 pagesPostpartum Eclampsia PDFMo Fadra0% (1)
- Late Postpartum EclampsiaDocument4 pagesLate Postpartum Eclampsiaapi-3702092No ratings yet
- Pentalogy of Fallot Review NotesDocument11 pagesPentalogy of Fallot Review NotesMutivanya Inez MaharaniNo ratings yet
- Hydatidiform Mole With Hyperthyroidism - Perioperative ChallengesDocument2 pagesHydatidiform Mole With Hyperthyroidism - Perioperative ChallengesAl MubartaNo ratings yet
- A Severe Asphyxiated Newborn: A Case ReportDocument13 pagesA Severe Asphyxiated Newborn: A Case ReportEeeeeeeeeNo ratings yet
- BJOG P 380Document2 pagesBJOG P 380Amanqui Alex DerlyNo ratings yet
- Anaesthetic Management of A Child With A Positive Family History of Malignant Hyperthermia For Posterior Fossa Surgery in The Sitting PositionDocument3 pagesAnaesthetic Management of A Child With A Positive Family History of Malignant Hyperthermia For Posterior Fossa Surgery in The Sitting PositionkrishNo ratings yet
- Transient Acute Decompensated Heart Failure Following Propofol and Fentanyl Administration in A Healthy 19-Year-Old PatientDocument2 pagesTransient Acute Decompensated Heart Failure Following Propofol and Fentanyl Administration in A Healthy 19-Year-Old PatientAchmad Ageng SeloNo ratings yet
- Atyp EclmDocument6 pagesAtyp Eclmzamurd76No ratings yet
- Medicine: Sudden Seizure During Cesarean SectionDocument2 pagesMedicine: Sudden Seizure During Cesarean SectionDavid RefuncionNo ratings yet
- Peripartum Care of The Parturient With Acute Fatty Liver of PregnancyDocument3 pagesPeripartum Care of The Parturient With Acute Fatty Liver of PregnancyDebNo ratings yet
- Pregnancy Induced Hypertension (PIH) : Case Scenario 4Document4 pagesPregnancy Induced Hypertension (PIH) : Case Scenario 4Mae Arra Lecobu-anNo ratings yet
- Cardiac Arrest in Pregnancy and Perimortem Cesarean Delivery CaseDocument5 pagesCardiac Arrest in Pregnancy and Perimortem Cesarean Delivery CaseYoomiif BedadaNo ratings yet
- MefenamicDocument9 pagesMefenamicmisslhenNo ratings yet
- Anaesthesia For Caesarean Section in A Patient With Eisenmenger's SyndromeDocument3 pagesAnaesthesia For Caesarean Section in A Patient With Eisenmenger's SyndromeRasyid DorkzNo ratings yet
- J Jclinane 2005 08 012Document3 pagesJ Jclinane 2005 08 012Novi Yanti NyNo ratings yet
- 2015 319 TJOG RefractoryVTinpregnancyDocument3 pages2015 319 TJOG RefractoryVTinpregnancyIsmul 'D' SadlyNo ratings yet
- Uterine Rupture in A Primigravid Patient and Anesthetic Implications: A Case ReportDocument4 pagesUterine Rupture in A Primigravid Patient and Anesthetic Implications: A Case ReportYahia AhmadNo ratings yet
- Pregnant Patient With Eclampsia For Emergency Cesarean Section Case FileDocument2 pagesPregnant Patient With Eclampsia For Emergency Cesarean Section Case Filehttps://medical-phd.blogspot.comNo ratings yet
- The Use of Plasma Exchange in A Very Earlyonset and Life Threatening Hemolysis Elevated Liver Enzymes and Low Platelet Hellp Syndr 2161 0932 1000387Document4 pagesThe Use of Plasma Exchange in A Very Earlyonset and Life Threatening Hemolysis Elevated Liver Enzymes and Low Platelet Hellp Syndr 2161 0932 1000387Alfa FebriandaNo ratings yet
- Acute Fatty Liver of Pregnancy: A Case ReportDocument0 pagesAcute Fatty Liver of Pregnancy: A Case ReportnajmulNo ratings yet
- Thalssemia & Spinal Cord Compression in PregnancyDocument1 pageThalssemia & Spinal Cord Compression in PregnancyThao NguyenNo ratings yet
- Severe Preeclampsia BahanDocument7 pagesSevere Preeclampsia BahanelenNo ratings yet
- Unas UnsriDocument29 pagesUnas UnsriMuhammad DasawarsaNo ratings yet
- Journal Hellp SyndromDocument3 pagesJournal Hellp SyndromElang SudewaNo ratings yet
- Yayie Case PresentationDocument12 pagesYayie Case PresentationYayie Querubin SilvestreNo ratings yet
- West Avenue, Molo, Iloilo City NCM 109 Rle: Care of Mother, Child at Risk or With Problems (Acute and Chronic)Document3 pagesWest Avenue, Molo, Iloilo City NCM 109 Rle: Care of Mother, Child at Risk or With Problems (Acute and Chronic)snow.parconNo ratings yet
- Case Study of Pediatric CareDocument4 pagesCase Study of Pediatric CareazafatimatuzzahraNo ratings yet
- International Journal of Scientific Research: AnesthesiologyDocument2 pagesInternational Journal of Scientific Research: AnesthesiologyALfuNo ratings yet
- Severe Erythroderma As A Complication of Continuous Epoprostenol TherapyDocument3 pagesSevere Erythroderma As A Complication of Continuous Epoprostenol Therapy568563No ratings yet
- Takayasu's Artheritis During PregnancyDocument11 pagesTakayasu's Artheritis During PregnancyAgung Sunarko PutraNo ratings yet
- Fernandez 1989Document2 pagesFernandez 1989Muhammad IqsanNo ratings yet
- Anestesi Pada GBSDocument4 pagesAnestesi Pada GBSyudhalantankNo ratings yet
- Case ReportDocument6 pagesCase ReportEka Budi UtamiNo ratings yet
- The Use of Levosimendan in Children With Cancer With Severe Acute Cardiac Dysfunction Case Series and A Review of The LiteratureDocument4 pagesThe Use of Levosimendan in Children With Cancer With Severe Acute Cardiac Dysfunction Case Series and A Review of The Literaturehadi40canadaNo ratings yet
- Management of Severe Postpartum Haemorrhage by Uterine Artery EmbolizationDocument4 pagesManagement of Severe Postpartum Haemorrhage by Uterine Artery EmbolizationAndi Tri SutrisnoNo ratings yet
- Persistent Paralysis After Spinal Paresthesia PDFDocument6 pagesPersistent Paralysis After Spinal Paresthesia PDFNadia Gina AnggrainiNo ratings yet
- Kumari - Ephedrine Versus Phenylephrine Effects On Fetal Acid-Base Status During Spinal Anesthesia For Elective Cesarean DeliveryDocument5 pagesKumari - Ephedrine Versus Phenylephrine Effects On Fetal Acid-Base Status During Spinal Anesthesia For Elective Cesarean DeliveryFadil AhmadNo ratings yet
- An Extremely Rare and Life Threatening Thyrotoxicosis - FinalDocument12 pagesAn Extremely Rare and Life Threatening Thyrotoxicosis - FinalChristian PoerniawanNo ratings yet
- Trisomy 21 Fetus Co-Existent With A Partial Molar Pregnancy: Case ReportDocument2 pagesTrisomy 21 Fetus Co-Existent With A Partial Molar Pregnancy: Case ReportArga KafiNo ratings yet
- Approach To The PatientDocument11 pagesApproach To The PatientNaya FarmsiBthreendy X'iNo ratings yet
- Eclampsia: VI. Maternal-Perinatal Outcome in 254 Consecutive CasesDocument6 pagesEclampsia: VI. Maternal-Perinatal Outcome in 254 Consecutive CasesrizkaNo ratings yet
- Atypical EclampsiaDocument3 pagesAtypical EclampsiadianaristinugraheniNo ratings yet
- 631-Article Text-2378-1-10-20180830Document6 pages631-Article Text-2378-1-10-20180830azizhamoudNo ratings yet
- Postpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiDocument4 pagesPostpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiAstrit GashiNo ratings yet
- 4408 Case Report of Severe Preeclampsia and Associated Postpartum ComplicationsDocument3 pages4408 Case Report of Severe Preeclampsia and Associated Postpartum ComplicationsMesu MitchNo ratings yet
- Thoracic Epidural For Modified Radical Mastectomy in A High-Risk PatientDocument2 pagesThoracic Epidural For Modified Radical Mastectomy in A High-Risk PatientBianca CaterinalisendraNo ratings yet
- CPR PregnancyDocument25 pagesCPR PregnancyCutie PieNo ratings yet
- Cesarean Hysterectomy With Cystotomy in Parturient Having Placenta Percreta, Gestational Thrombocytopenia, and Portal Hypertension - A Case ReportDocument4 pagesCesarean Hysterectomy With Cystotomy in Parturient Having Placenta Percreta, Gestational Thrombocytopenia, and Portal Hypertension - A Case ReportasclepiuspdfsNo ratings yet
- 1 s2.0 S2211419X13000578 MainDocument4 pages1 s2.0 S2211419X13000578 Mainindra040293No ratings yet
- Anes MNGMT Ped TraumaDocument5 pagesAnes MNGMT Ped Traumaramzi MohamedNo ratings yet
- Spontaneous Splenic Rupture in A 21-Year Old Male Patient Patient: H.MDocument4 pagesSpontaneous Splenic Rupture in A 21-Year Old Male Patient Patient: H.MJoherNo ratings yet
- Sme PropofolDocument2 pagesSme PropofolAntonella Jazmín AssadNo ratings yet
- tmp2CD0 TMPDocument4 pagestmp2CD0 TMPFrontiersNo ratings yet
- Ondan Hipo 2Document6 pagesOndan Hipo 2putri maharani andesNo ratings yet
- 24 Fix PDFDocument4 pages24 Fix PDFmelvaNo ratings yet
- Anaesthesia For Caesarean Section in Patients With Uncontrolled HyperthyroidismDocument6 pagesAnaesthesia For Caesarean Section in Patients With Uncontrolled HyperthyroidismNut RonakritNo ratings yet
- Congenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementFrom EverandCongenital Hyperinsulinism: A Practical Guide to Diagnosis and ManagementDiva D. De León-CrutchlowNo ratings yet
- The Hypercoagulable State in Thalassemia: Hemostasis, Thrombosis, and Vascular Biology Clinical Trials and ObservationsDocument9 pagesThe Hypercoagulable State in Thalassemia: Hemostasis, Thrombosis, and Vascular Biology Clinical Trials and ObservationsNi Wayan Ana PsNo ratings yet
- Cerebrovascular Accident in B-Thalassemia Major (B-TM) and B-Thalassemia Intermedia (b-TI)Document3 pagesCerebrovascular Accident in B-Thalassemia Major (B-TM) and B-Thalassemia Intermedia (b-TI)Ni Wayan Ana PsNo ratings yet
- Cervical Stitch (Cerclage) For Preventing Pregnancy Loss: Individual Patient Data Meta-AnalysisDocument17 pagesCervical Stitch (Cerclage) For Preventing Pregnancy Loss: Individual Patient Data Meta-AnalysisNi Wayan Ana PsNo ratings yet
- Using Antimicrobial Surgihoney To Prevent Caesarean Wound InfectionDocument5 pagesUsing Antimicrobial Surgihoney To Prevent Caesarean Wound InfectionNi Wayan Ana PsNo ratings yet
- Do Clear Cell Ovarian Carcinomas Have Poorer Prognosis Compared To Other Epithelial Cell Types? A Study of 1411 Clear Cell Ovarian CancersDocument7 pagesDo Clear Cell Ovarian Carcinomas Have Poorer Prognosis Compared To Other Epithelial Cell Types? A Study of 1411 Clear Cell Ovarian CancersNi Wayan Ana PsNo ratings yet
- The Role of Honey in The Management of Wounds: DiscussionDocument4 pagesThe Role of Honey in The Management of Wounds: DiscussionNi Wayan Ana PsNo ratings yet
- Distosia Ncbi (Ana)Document8 pagesDistosia Ncbi (Ana)Ni Wayan Ana PsNo ratings yet
- Title of The Presentation: Your SubtitleDocument2 pagesTitle of The Presentation: Your SubtitleNi Wayan Ana PsNo ratings yet
- Cytokeratin 7 and Cytokeratin 19 Expressions in Oval Cells and Mature Cholangiocytes As Diagnostic and Prognostic Factors of CholestasisDocument6 pagesCytokeratin 7 and Cytokeratin 19 Expressions in Oval Cells and Mature Cholangiocytes As Diagnostic and Prognostic Factors of CholestasisNi Wayan Ana PsNo ratings yet
- CMV Primer Non PrimerDocument3 pagesCMV Primer Non PrimerNi Wayan Ana PsNo ratings yet
- Pendapat Holy GrailDocument4 pagesPendapat Holy GrailNi Wayan Ana PsNo ratings yet
- Insertion of An Intrauterine Contraceptive Device After Induced or Spontaneous Abortion: A Review of The EvidenceDocument6 pagesInsertion of An Intrauterine Contraceptive Device After Induced or Spontaneous Abortion: A Review of The EvidenceNi Wayan Ana PsNo ratings yet
- Human Rabies: Neuropathogenesis, Diagnosis, and Management: ReviewDocument16 pagesHuman Rabies: Neuropathogenesis, Diagnosis, and Management: ReviewNi Wayan Ana PsNo ratings yet
- Uterine StimulantsDocument24 pagesUterine StimulantsKilp MosesNo ratings yet
- Maternal Health: Ekta Modi 2 MPT in RehabDocument368 pagesMaternal Health: Ekta Modi 2 MPT in RehabMihir_Mehta_5497100% (1)
- Induction of Labour For Post MaturityDocument6 pagesInduction of Labour For Post MaturityYwagar YwagarNo ratings yet
- Labor and Delivery ComplicationsDocument50 pagesLabor and Delivery ComplicationskjayjocsinNo ratings yet
- Complications With The Passenger 2Document77 pagesComplications With The Passenger 2JudyNo ratings yet
- 1-Drugs Affecting Uterine Muscle ContractilityDocument40 pages1-Drugs Affecting Uterine Muscle ContractilityjojolilimomoNo ratings yet
- High - Risk Labor and Delivery 2Document106 pagesHigh - Risk Labor and Delivery 2Charmaine Louie Macalanda Lopez-Soriano100% (2)
- Get Through MRCOG Part 1 2nd EditionDocument142 pagesGet Through MRCOG Part 1 2nd Editionmustafa benmuhsen50% (2)
- 2-Post TermDocument13 pages2-Post TermAbc DefNo ratings yet
- Induction and Augmentation of LabourDocument73 pagesInduction and Augmentation of LabourSanthosh.S.U100% (4)
- Preterm and Posterm Birth: Oleh: DR Adi Setyawan Prianto SP - OG (K)Document31 pagesPreterm and Posterm Birth: Oleh: DR Adi Setyawan Prianto SP - OG (K)ATIKAH NUR HAFIZHAHNo ratings yet
- Management For PROMDocument2 pagesManagement For PROMSajaratul Syifaa'No ratings yet
- MU-MCQs (2020) OBS & GYNDocument330 pagesMU-MCQs (2020) OBS & GYNGhaiidaa khh100% (1)
- Safe Prevention of The Primary Cesarean Delivery - ACOGDocument16 pagesSafe Prevention of The Primary Cesarean Delivery - ACOGAryaNo ratings yet
- Augmentation of LabourDocument45 pagesAugmentation of LabourLamnunnem HaokipNo ratings yet
- Robsons Ten Group Classification of Cesarean Section at A Tertiary Center in NepalDocument6 pagesRobsons Ten Group Classification of Cesarean Section at A Tertiary Center in NepalgehanathNo ratings yet
- Hypertensive Disorders in PregnancyDocument96 pagesHypertensive Disorders in PregnancySalman Habeeb100% (4)
- Progression of First Stage LaourDocument14 pagesProgression of First Stage LaourAlmira Dyah PuspitariniNo ratings yet
- (PBL) Induction of Labor and Bishop's ScoreDocument10 pages(PBL) Induction of Labor and Bishop's ScoreSean WangNo ratings yet
- Rekap Inap Obsetetri PerdiagnosaDocument142 pagesRekap Inap Obsetetri Perdiagnosafatha_87No ratings yet
- Hypnosis Antenatal Training For Childbirth: A Randomised Controlled TrialDocument12 pagesHypnosis Antenatal Training For Childbirth: A Randomised Controlled TrialEka AfriliaNo ratings yet
- Katharine GravesDocument34 pagesKatharine GravesDanaNo ratings yet
- Update On Uterine Tachysystolehobson2018Document9 pagesUpdate On Uterine Tachysystolehobson2018Raul A UrbinaNo ratings yet
- Labour Interventions ReportDocument20 pagesLabour Interventions Reportdwi handayaniNo ratings yet
- Mcqs Test Unit 8 With KeyDocument5 pagesMcqs Test Unit 8 With Keyyasodha maharajNo ratings yet
- Premature Rupture of MembranesDocument10 pagesPremature Rupture of Membranessami samiNo ratings yet
- Easier Shorter Safer BirthDocument53 pagesEasier Shorter Safer Birthmw101mw100% (1)
- ObstetricsDocument216 pagesObstetricsሌናፍ ኡሉምNo ratings yet
- Edit - HIL - Daily IGD 25.09.19Document30 pagesEdit - HIL - Daily IGD 25.09.19Inez WijayaNo ratings yet
- Nur 2310 Maternal Exam Questions and AnswersDocument80 pagesNur 2310 Maternal Exam Questions and AnswersNelson MandelaNo ratings yet