Professional Documents
Culture Documents
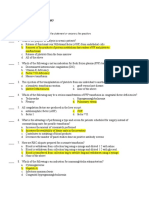
Placental Abruption - Management
Uploaded by
dixoonOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Placental Abruption - Management
Uploaded by
dixoonCopyright:
Available Formats
1/9/2014 Placental abruption: Management
http://www.uptodate.com/contents/placental-abruption-management?topicKey=OBGYN%2F6803&elapsedTimeMs=7&source=search_result&searchTerm=desp 1/8
Official reprint from UpToDate
www.uptodate.com 2014 UpToDate
Authors
Yinka Oyelese, MD
Cande V Ananth, PhD, MPH
Section Editor
Charles J Lockwood, MD, MHCM
Deputy Editor
Vanessa A Barss, MD
Placental abruption: Management
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: Jul 2014. | This topic last updated: Jun 10, 2014.
INTRODUCTION Abruption of the placenta can lead to serious maternal and infant morbidity, as well as
maternal or perinatal death. The risks to the mother are primarily related to the severity of the abruption, while the
risks to the fetus are related to both the severity of the abruption and the gestational age at which delivery occurs
[1]. (See "Placental abruption: Clinical features and diagnosis", section on 'Consequences'.)
Although the impact of placental abruption on pregnancy outcomes is well-described, no randomized trials and very
few studies have examined the management of pregnancies complicated by this disorder [2]. As a result,
recommendations for the management of placental abruption are based on case series and reports, personal
experience, and good clinical sense.
INITIAL APPROACH
General measures Acute abruption can be life-threatening for the mother and fetus and can be associated with
co-morbid disorders (preeclampsia, cocaine abuse, trauma), thus pregnant women with signs and symptoms of
abruption should be evaluated promptly. (See "Placental abruption: Clinical features and diagnosis".)
Management of these pregnancies is determined on a case-by-case basis, and will depend upon the severity of the
abruption, the gestational age, and maternal and fetal status. Any patient who presents with even slight bleeding
from placental separation is at risk of developing sudden severe abruption. Therefore, all of these patients should be
monitored and undergo continuous fetal heart rate assessment until their status is clear. (See "Placental abruption:
Clinical features and diagnosis", section on 'Chronic abruption'.)
The following actions are reasonable initial interventions for women with potentially severe acute abruption:
Immediately initiate continuous fetal monitoring, given the high likelihood of a reduction in placental perfusion.
Secure intravenous access with at least one, and preferably two, wide-bore intravenous lines. Closely monitor
the mother's hemodynamic status (heart rate, blood pressure, urine output). Urine output should be
maintained at above 30 mL/hour and monitored with a Foley catheter. Assessment of multiple parameters is
important because normal blood pressure may mask hypovolemia if the mother was
hypertensive/preeclamptic prior to the abruption.
Keep maternal oxygen saturation >95 percent and keep the patient warm.
Estimate the extent of blood loss by collection in a volumetric container and/or by weighing pads/towels used
to absorb vaginal bleeding. In addition to the practical difficulties in determining the volume of blood passed
from the vagina, actual blood loss may be far in excess of what is observed due to retained retroplacental
hemorrhage.
Draw blood for a complete blood count, blood type and Rh, and coagulation studies. A crude clotting test can
be performed at the bedside by placing 5 mL of the patient's blood in a tube with no anticoagulant for 10
minutes [3-5]. Failure to clot within this time or dissolution of an initial clot implies impairment of coagulation,
1/9/2014 Placental abruption: Management
http://www.uptodate.com/contents/placental-abruption-management?topicKey=OBGYN%2F6803&elapsedTimeMs=7&source=search_result&searchTerm=desp 2/8
Indications for delivery are discussed below. (See 'Management' below.)
Treatment of disseminated intravascular coagulation In women with DIC, we transfuse blood and blood
products to achieve the following minimum levels:
Management of DIC during pregnancy is discussed in detail separately. (See "Disseminated intravascular
coagulation during pregnancy".)
MANAGEMENT After initial assessment and stabilization, management of pregnancies complicated by an
acute, clinically significant abruption depends primarily on whether the fetus is alive or dead, and maternal status. If
the fetus is alive, then gestational age and fetal status also play a role in decision-making. The following guidelines
provide a general approach that should be modified as appropriate for individual patients.
Severe abruption at any gestational age and nonsevere abruption at >36 weeks We recommend
expeditious delivery for pregnancies at any gestational age complicated by severe abruption, which can be defined
as an abruption where the mother is unstable (eg, significant coagulopathy, hypotension, and/or ongoing major
blood loss) or the fetal heart rate tracing is nonreassuring. We also recommend delivery for pregnancies with
nonsevere abruption at 36 weeks of gestation [1]. For nonsevere abruptions at 36 weeks, this approach takes
into account the relatively low neonatal morbidity of the near-term infant in pregnancies at risk of severe maternal-
fetal morbidity or mortality in the event of a future sudden severe abruption.
Vaginal delivery is reasonable if the mother is stable and the fetal heart tracing is reassuring. With a clinically
significant abruption, the patient is often contracting vigorously, but if she is not in active labor, then amniotomy and
administration of oxytocin frequently result in rapid delivery. Partial abruption can progress to total abruption
suddenly and without warning. Thus, the fetus should be continuously monitored and preparations must be made in
case urgent operative delivery is required. Because these patients often progress rapidly in labor, they have a high
likelihood of successful vaginal birth. However, an attempt at vaginal birth should only be undertaken if there is
access to immediate cesarean delivery, if necessary.
Prompt cesarean delivery is indicated if the mother is unstable or the fetal heart tracing is nonreassuring and
vaginal delivery is not imminent, or when vaginal delivery is contraindicated (eg, malpresentation, prior classical
cesarean delivery) or unsuccessful (failure to progress). In one of the only studies that evaluated cesarean delivery
for severe abruption, a decision to delivery interval of less than 20 minutes was associated with better outcomes
than a 30-minute interval when fetal bradycardia was present [6]. Although this was a small case-control study of
31 cases, it underscores the principle that the duration of prolonged bradycardia influences outcome when the
and is suggestive of a low fibrinogen level. Prolonged oozing from needle puncture sites also suggests
coagulopathy.
Repeat coagulation tests in patients with clinical signs of severe abruption as coagulopathy may develop or
worsen over time.
Notify the blood bank so blood replacement products (red blood cells, fresh frozen plasma, cryoprecipitate,
platelets) will be readily available, if needed. Blood products should be replaced aggressively, as required. If
disseminated intravascular coagulation (DIC) is suspected, activate the institutions massive transfusion
protocol. (See 'Treatment of disseminated intravascular coagulation' below.)
Notify the anesthesia team. Anesthesia-related issues in these patients include management of
hemodynamic instability, technical issues related to bleeding diathesis, and the potential need for emergency
cesarean delivery.
Platelet count 50,000/microL
Fibrinogen 100 mg/dL
Prothrombin (PT) and partial thromboplastin time (PTT) less than 1.5 times control
Hematocrit 25 to 30 percent
1/9/2014 Placental abruption: Management
http://www.uptodate.com/contents/placental-abruption-management?topicKey=OBGYN%2F6803&elapsedTimeMs=7&source=search_result&searchTerm=desp 3/8
abruption is severe.
Major maternal morbidity or death is a real risk when a cesarean is performed in the presence of coagulopathy.
Some experts recommend that operative intervention should not begin until coagulopathy is corrected. However,
such a delay could lead to fetal death, further blood loss, and worsening of the coagulopathy. It is desirable, but not
always possible, to correct the clotting abnormality prior to cesarean. If a cesarean has to be performed urgently,
blood, fresh frozen plasma, platelets, and cryoprecipitate should be available in the operating room and should be
administered if there are signs of impaired hemostasis (eg, persistent bleeding without clotting from incision and
needle sites), without waiting for the results of coagulation studies. (See "Disseminated intravascular coagulation
during pregnancy".)
At cesarean delivery, blood extravasated into the myometrium (called a Couvelaire uterus) may be observed. The
Couvelaire uterus is atonic and thus prone to postpartum hemorrhage. Patients with a Couvelaire uterus are less
likely to respond to conservative measures, and have a much higher risk for hysterectomy. If a Couvelaire uterus is
detected, aggressive management of atony is needed to prevent disseminated intravascular coagulation (DIC) and
exsanguination.
Neonates are at risk of problems related to prematurity and hypoxia so a neonatal resuscitation team should be in
the delivery room. (See "Neonatal resuscitation in the delivery room".)
Postpartum care Postpartum, we administer an intravenous oxytocin infusion as the first line uterotonic
agent. Maternal vital signs, blood loss, urine output, uterine size and consistency, and laboratory results
(hemoglobin/hematocrit, coagulation studies) should be monitored closely to ensure that bleeding has been
controlled and that coagulopathy is resolving, and to guide replacement of fluids and blood products, as needed.
If the uterus remains atonic after delivery of the placenta, we suggest methylergonovine as a first-line treatment (in
the absence of preeclampsia) [7]. In patients who fail methylergonovine or have contraindications to use of this
drug, we recommend a prostaglandin F2a analog (eg, carboprost tromethamine [Hemabate]). Misoprostol is an
alternative. When these measures fail, uterine vessel ligation, uterine compression sutures, embolization, and/or
hysterectomy may be necessary to prevent exsanguination. (See "Overview of postpartum hemorrhage".)
Women with severe abruption, shock, and DIC are at risk of multiorgan failure, especially acute renal insufficiency.
After delivery, organ function usually improves with aggressive supportive care and treatment of complications, as
appropriate. (See "Clinical features, diagnosis, and treatment of disseminated intravascular coagulation in adults"
and "Treatment of severe hypovolemia or hypovolemic shock in adults" and "Acute kidney injury (acute renal failure)
in pregnancy".)
Nonsevere abruption at 34 to 36 weeks We tend to deliver most patients with a new diagnosis of abruption at
34 to 36 weeks of gestation, even if the abruption is not severe (ie, fetal status reassuring, maternal vital signs
normal, laboratory tests normal or mildly abnormal, mild to moderate bleeding), since these patients remain at risk
of developing a sudden severe abruption. Decision-making in these cases is based on patient-specific factors,
balancing the estimated risk of progression/recurrence against the relatively small risks of prematurity in the late
preterm infant. (See "Late preterm infants".)
Minor abruption at 34 to 36 weeks For carefully selected patients between 34 and 36 weeks with probable
minor abruption (ie, minimal signs and symptoms of abruption), conservative management is a reasonable approach
if the mother is stable, fetal status is reassuring, laboratory tests are normal, and active bleeding has stopped.
However, as discussed above, these patients are at increased risk for sudden, severe abruption. They should be
monitored closely and delivered if they have recurrent bleeding.
Nonsevere abruption at <34 weeks Expectant management of abruption in pregnancies <34 weeks of
gestation is reasonable when the mother is stable and when tests of fetal well-being are reassuring [1,8-10].
Coagulopathy of any significant degree, in our opinion, constitutes patient instability and is an indication for
delivery. Similarly, non-reassuring fetal heart rate evaluation (persistent fetal bradycardia, late decelerations, loss of
1/9/2014 Placental abruption: Management
http://www.uptodate.com/contents/placental-abruption-management?topicKey=OBGYN%2F6803&elapsedTimeMs=7&source=search_result&searchTerm=desp 4/8
variability or a sinusoidal fetal heart rate pattern), or nonreassuring biophysical scores are indications for delivery;
these patients should not be managed conservatively, even if <34 weeks.
Corticosteroids to promote fetal lung maturation should be administered to pregnancies at 23 to 34 weeks of
gestation, given the increased risk of need for preterm delivery. (See "Antenatal corticosteroid therapy for reduction
of neonatal morbidity and mortality from preterm delivery".)
Abruption frequently causes uterine contractions. These contractions are partly caused by thrombin and may lead
to further placental separation, which may in turn cause further bleeding, creating a cycle of bleeding and
contractions. Tocolytics may prevent further contractions, in theory breaking this cycle. However, tocolytics may
cause cardiovascular symptoms (tachycardia, hypotension), which may worsen any hemodynamic instability
resulting from abruption, and may also make it difficult to recognize signs of worsening hypovolemia. For these
reasons, several authorities have argued against their use in this setting.
A few small, retrospective, uncontrolled studies have examined tocolytic use (eg, ritodrine, terbutaline, magnesium
sulfate, indomethacin) in management of abruption in hemodynamically stable pregnant women with reassuring
fetal heart rate tracings [10-12]. These studies have not demonstrated harm and have suggested a potential benefit;
however, given the limitations of these data, the results of these studies need to be interpreted with caution. In the
rare cases in which we use tocolytics, we give a 48-hour course of indomethacin (only at gestational ages <32
weeks), nifedipine, or magnesium sulfate. We generally administer these drugs for 48 hours to allow
administration of corticosteroids for fetal lung maturation. Although the effectiveness of magnesium sulfate as a
tocolytic is unclear, it has the potential benefit of fetal neuroprotection. (See "Inhibition of acute preterm labor".)
We perform fetal assessment with a non-stress test or biophysical profile at least weekly. We also perform serial
sonographic estimation of fetal weight to assess growth since over time these fetuses are at risk of developing
growth restriction [13].
There are no compelling data to guide the length of a hospital stay in these pregnancies. A reasonable approach is
to monitor the patient in the hospital until the bleeding has subsided for at least 48 hours, fetal heart rate tracings
and ultrasound examinations are reassuring, and the patient is asymptomatic. At that point, discharge may be
considered. Importantly, the patient should be counseled to return immediately should she experience further
bleeding, contractions, reduced fetal movement, or abdominal pain. In patients with sonographic evidence of a large
hematoma, we feel it is prudent to keep the patient in the hospital for a longer period of close monitoring.
For patients with abruption <34 weeks who have been managed conservatively without any further symptoms, it is
reasonable to schedule delivery at 37 to 38 weeks because of the increased risk of stillbirth [1]. We do not typically
perform amniocentesis to document fetal lung maturity prior to delivery. For each patient, the potential risk of
neonatal respiratory problems, which is low at this gestational age, should be weighed against the potential risk
that a serious abruption will occur while awaiting development of fetal pulmonary maturity.
Delivery before 37 weeks is indicated if additional complications arise (eg, fetal growth restriction, preeclampsia,
premature rupture of membranes, nonreassuring fetal assessment, recurrent abruption with maternal instability).
Placental abruption occurring in the second trimester carries an especially poor prognosis when accompanied by
oligohydramnios.
Fetal demise When fetal death has occurred, the mode of delivery should be chosen to minimize the risk of
maternal morbidity or mortality. Vaginal delivery is generally preferable. Since the patient is often contracting
vigorously, amniotomy may be all that is required to expedite delivery. Oxytocin can be given, if needed to augment
labor.
The frequency of coagulopathy is much higher in abruptions in which fetal death has occurred and blood
replacement is often necessary. Cesarean delivery is often the best option when (1) rapid control of bleeding is
required, or (2) there are obstetrical contraindications to vaginal birth, or (3) the mother is unwilling to accept
adequate blood replacement therapy, as a prolonged labor complicated by severe abruption may be associated with
1/9/2014 Placental abruption: Management
http://www.uptodate.com/contents/placental-abruption-management?topicKey=OBGYN%2F6803&elapsedTimeMs=7&source=search_result&searchTerm=desp 5/8
greater blood loss than cesarean delivery. A previous classical hysterotomy is a relative contraindication to vaginal
birth. Although these patients are at increased risk of uterine rupture during labor, this risk is relatively small (4 to 9
percent) and may be acceptable since cesarean delivery has no benefit for the fetus. The approach to these
patients should be individualized, taking into account factors such as gestational age and cervical status. (See
"Uterine dehiscence and rupture after previous cesarean delivery".)
If possible, coagulopathy should be corrected prior to, or during, the cesarean delivery. (See "Disseminated
intravascular coagulation during pregnancy".)
Ultrasound diagnosed placental abruption Placental abruption is occasionally an incidental finding on
ultrasound examination of an asymptomatic patient [8-10]. These cases are managed on a case-by-case basis. A
thorough history and physical examination should be performed, with particular attention to risk factors such as
smoking, hypertension, trauma, and use of cocaine [1].
If the pregnancy has reached term, we expedite delivery to avoid potential complications in case the area of
placental separation extends. In preterm pregnancies, conservative management is a reasonable approach. For
pregnancies less than 34 weeks of gestation, we administer corticosteroids to promote fetal lung maturation. (See
"Antenatal corticosteroid therapy for reduction of neonatal morbidity and mortality from preterm delivery".)
RECURRENCE RISK AND MANAGEMENT OF SUBSEQUENT PREGNANCIES
Recurrence risk Women with placental abruption are at several-fold higher risk of abruption in a subsequent
pregnancy [14-19]. The risk of recurrence has been reported to be 5 to 15 percent, compared to a baseline
incidence of 0.4 to 1.3 percent in the general population [15,20,21]. After two consecutive abruptions, the risk of a
third rises to 20 to 25 percent [19,22]. The risk of recurrence is higher after a severe abruption than after a mild
abruption, and the woman's sisters appear to be at increased risk of also having an abruption (OR 1.7-2.1) [19].
When the abruption is severe enough to kill the fetus, there is a 7 percent incidence of the same outcome in a
future pregnancy [23].
Unfortunately, there are no studies demonstrating that any intervention lowers this risk. Nonetheless, it is
reasonable to identify risk factors for abruption and address those risk factors that are modifiable. Women who
smoke or use cocaine should be encouraged to stop. Poorly controlled hypertension should be controlled. These
changes have proven health benefits even in the absence of pregnancy. On the other hand, placental abruption
resulting from trauma is not likely to recur, so these women can be reassured.
There are no laboratory screening tests that are predictive of an increased risk for abruption. Testing women with a
history of abruption for antiphospholipid antibodies or an inherited thrombophilia is not indicated. (See "Pregnancy
in women with antiphospholipid syndrome" and "Inherited thrombophilias in pregnancy".)
Antenatal monitoring There is limited evidence on which to base a recommendation regarding antenatal
surveillance of subsequent pregnancies. A cohort study using data from the Medical Birth Registry of Norway
calculated gestational age-specific risks of complicated placental abruption (eg, abruptions resulting in preterm
birth, a small for gestational age infant, or perinatal death) in a second pregnancy [24]. The authors determined the
risk of complicated placental abruption was 7 per 1000 for an initial event and 33 per 1000 for a first recurrence. To
reduce the risk of recurrent abruption to the baseline rate, both antenatal surveillance and delivery six weeks prior to
the gestational age of the initial abruption would be necessary during the subsequent pregnancy [24].
An active area of investigation is the hypothesis that placental abruption, intrauterine growth restriction, and
preeclampsia are different manifestations of ischemic placental disease and predispose the patient to preterm labor
and birth. There is evidence that these disorders often co-exist in a pregnancy, or one may occur in one pregnancy
while another occurs in a subsequent pregnancy (eg, abruption in the first pregnancy, growth restriction in the
second pregnancy) [18,25-27]. For this reason, in our practice, we perform an ultrasound examination to look for
growth restriction in subsequent pregnancies and, if fetal growth restriction is detected, we manage these
pregnancies accordingly. Monitoring for preeclampsia is already a standard focus of routine antenatal care. (See
1/9/2014 Placental abruption: Management
http://www.uptodate.com/contents/placental-abruption-management?topicKey=OBGYN%2F6803&elapsedTimeMs=7&source=search_result&searchTerm=desp 6/8
"Fetal growth restriction: Evaluation and management".)
Timing of delivery We typically await spontaneous labor until the estimated date of delivery, or perform a
repeat cesarean delivery at 39 to 40 weeks of gestation. In selected patients, such as those with a prior perinatal
death or with more than one prior abruption, delivery before 37 weeks of gestation after documentation of fetal lung
maturity is reasonable.
INFORMATION FOR PATIENTS UpToDate offers two types of patient education materials, The Basics and
Beyond the Basics. The Basics patient education pieces are written in plain language, at the 5 to 6 grade
reading level, and they answer the four or five key questions a patient might have about a given condition. These
articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the
Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the
10 to 12 grade reading level and are best for patients who want in-depth information and are comfortable with
some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these
topics to your patients. (You can also locate patient education articles on a variety of subjects by searching on
patient info and the keyword(s) of interest.)
SUMMARY AND RECOMMENDATIONS
th th
th th
Basics topic (see "Patient information: Placental abruption (The Basics)")
The risks of abruption for the fetus depend on the gestational age at which it occurs, as well as its severity,
whereas for the mother, the risks depend entirely on its severity. (See 'Introduction' above.)
A potentially severe placental abruption is an obstetrical emergency. These women should undergo rapid
evaluation, including continuous fetal heart rate monitoring, placement of large bore intravenous lines, and
assessment of blood loss, hypovolemia, and coagulopathy. Blood and blood products should be replaced
aggressively, when indicated. (See 'Initial approach' above.)
After initial evaluation and stabilization, the management of pregnancies complicated by clinically significant
abruption depends on whether the fetus is alive or dead, the gestational age, and maternal/fetal status. (See
'Management' above.)
For pregnancies where the mother is unstable at any gestational age (eg, significant coagulopathy,
hypotension, and/or ongoing major blood loss), or the fetal heart rate tracing is nonreassuring at any
gestational age, or the gestational age is 36 weeks, we suggest expeditious delivery (Grade 2C). When
there is partial placental separation, total abruption may occur suddenly and without warning in pregnancies
managed conservatively. (See 'Severe abruption at any gestational age and nonsevere abruption at >36 weeks'
above.)
Prompt cesarean delivery is indicated if the mother is unstable (in these cases, correction of hypovolemia and
coagulopathy should be performed concurrently) or the fetal heart tracing is nonreassuring and vaginal delivery
is not imminent, or when vaginal delivery is contraindicated (eg, malpresentation, prior classical cesarean
delivery) or unsuccessful (failure to progress). Otherwise, vaginal delivery may be attempted. (See 'Severe
abruption at any gestational age and nonsevere abruption at >36 weeks' above.)
It is desirable, but not always possible, to correct the clotting abnormality prior to cesarean. If a cesarean has
to be performed urgently, blood products should be available in the operating room and administered if there
are signs of impaired hemostasis. (See "Disseminated intravascular coagulation during pregnancy".)
Expectant management of carefully selected cases of abruption in pregnancies <36 weeks of gestation is
reasonable when the mother is stable and when tests of fetal well-being are reassuring. We administer a
course of glucocorticoids to women with pregnancies between 23 and 34 weeks of gestation. (See 'Minor
abruption at 34 to 36 weeks' above and 'Nonsevere abruption at <34 weeks' above.)
1/9/2014 Placental abruption: Management
http://www.uptodate.com/contents/placental-abruption-management?topicKey=OBGYN%2F6803&elapsedTimeMs=7&source=search_result&searchTerm=desp 7/8
Use of UpToDate is subject to the Subscription and License Agreement.
REFERENCES
1. Oyelese Y, Ananth CV. Placental abruption. Obstet Gynecol 2006; 108:1005.
2. Neilson JP. Interventions for treating placental abruption. Cochrane Database Syst Rev 2012; :CD003247.
3. POE MF. Clot observation test for clinical diagnosis of clotting defects. Anesthesiology 1959; 20:825.
4. WEINER AE, REID DE, ROBY CC. Incoagulable blood in severe premature separation of the placenta: a
method of management. Am J Obstet Gynecol 1953; 66:475.
5. Lee RI, White PD. A clinical study of the coagulation time of blood. Am J Med Sci 1913; 145:494.
6. Kayani SI, Walkinshaw SA, Preston C. Pregnancy outcome in severe placental abruption. BJOG 2003;
110:679.
7. Liabsuetrakul T, Choobun T, Peeyananjarassri K, Islam QM. Prophylactic use of ergot alkaloids in the third
stage of labour. Cochrane Database Syst Rev 2007; :CD005456.
8. Bond AL, Edersheim TG, Curry L, et al. Expectant management of abruptio placentae before 35 weeks
gestation. Am J Perinatol 1989; 6:121.
9. Combs CA, Nyberg DA, Mack LA, et al. Expectant management after sonographic diagnosis of placental
abruption. Am J Perinatol 1992; 9:170.
10. Sholl JS. Abruptio placentae: clinical management in nonacute cases. Am J Obstet Gynecol 1987; 156:40.
11. Saller DN Jr, Nagey DA, Pupkin MJ, Crenshaw MC Jr. Tocolysis in the management of third trimester
bleeding. J Perinatol 1990; 10:125.
12. Towers CV, Pircon RA, Heppard M. Is tocolysis safe in the management of third-trimester bleeding? Am J
Obstet Gynecol 1999; 180:1572.
13. Ananth CV, Berkowitz GS, Savitz DA, Lapinski RH. Placental abruption and adverse perinatal outcomes.
JAMA 1999; 282:1646.
14. Ananth CV, Cnattingius S. Influence of maternal smoking on placental abruption in successive pregnancies: a
population-based prospective cohort study in Sweden. Am J Epidemiol 2007; 166:289.
15. Ananth CV, Savitz DA, Williams MA. Placental abruption and its association with hypertension and
prolonged rupture of membranes: a methodologic review and meta-analysis. Obstet Gynecol 1996; 88:309.
16. Kregrd M, Gennser G. Incidence and recurrence rate of abruptio placentae in Sweden. Obstet Gynecol
1986; 67:523.
17. Rasmussen S, Irgens LM, Dalaker K. The effect on the likelihood of further pregnancy of placental abruption
and the rate of its recurrence. Br J Obstet Gynaecol 1997; 104:1292.
18. Rasmussen S, Irgens LM, Dalaker K. Outcome of pregnancies subsequent to placental abruption: a risk
assessment. Acta Obstet Gynecol Scand 2000; 79:496.
19. Rasmussen S, Irgens LM. Occurrence of placental abruption in relatives. BJOG 2009; 116:693.
20. Toivonen S, Heinonen S, Anttila M, et al. Obstetric prognosis after placental abruption. Fetal Diagn Ther
When fetal death has occurred, the mode of delivery should minimize the risk of maternal morbidity or
mortality. Vaginal delivery is preferable, but cesarean delivery may be the best option when (1) rapid control of
bleeding is required, or (2) there are obstetrical contraindications to vaginal birth (eg, previous classical
hysterotomy), or (3) the mother is unwilling to accept adequate blood replacement therapy. (See 'Fetal
demise' above.)
The risk of recurrent abruption is 5 to 15 percent, compared to a baseline incidence of 0.4 to 1.3 percent in
the general population. A past history of placental abruption predicts a greater likelihood of a small for
gestational age infant, spontaneous preterm birth, or preeclampsia in future pregnancies, even in the absence
of recurrent abruption. (See 'Recurrence risk and management of subsequent pregnancies' above.)
1/9/2014 Placental abruption: Management
http://www.uptodate.com/contents/placental-abruption-management?topicKey=OBGYN%2F6803&elapsedTimeMs=7&source=search_result&searchTerm=desp 8/8
Di scl osures: Yinka Oyelese, MD Consultant/Advisory Board: Bayer Pharmaceutical [postpartum hemorrhage (drugs in development)].
Cande V Ananth, PhD, MPH Nothing to disclose. Charles J Lockwood, MD, MHCM Nothing to disclose. Vanessa A Barss, MD
Employee of UpToDate, Inc. Equity Ownership/Stock Options: Merck; Pf izer; Abbvie.
Contributor disclosures are reviewed f or conf licts of interest by the editorial group. When f ound, these are addressed by vetting through
a multi-level review process, and through requirements f or ref erences to be provided to support the content. Appropriately ref erenced
content is required of all authors and must conf orm to UpToDate standards of evidence.
Conflict of interest policy
2004; 19:336.
21. Tikkanen M, Nuutila M, Hiilesmaa V, et al. Prepregnancy risk factors for placental abruption. Acta Obstet
Gynecol Scand 2006; 85:40.
22. Clark, SL. Placentae Previa and Abruptio Placentae. In: Maternal Fetal Medicine, 4th ed, Creasy, RK,
Resnik, R, (Eds), WB Saunders Company, Philadelphia, Pennsylvania 1999. p. 623.
23. Pritchard JA, Mason R, Corley M, Pritchard S. Genesis of severe placental abruption. Am J Obstet Gynecol
1970; 108:22.
24. Rasmussen S, Irgens LM, Albrechtsen S, Dalaker K. Women with a history of placental abruption: when in a
subsequent pregnancy should special surveillance for a recurrent placental abruption be initiated? Acta
Obstet Gynecol Scand 2001; 80:708.
25. Rasmussen S, Irgens LM, Dalaker K. A history of placental dysfunction and risk of placental abruption.
Paediatr Perinat Epidemiol 1999; 13:9.
26. Ananth CV, Vintzileos AM. Maternal-fetal conditions necessitating a medical intervention resulting in preterm
birth. Am J Obstet Gynecol 2006; 195:1557.
27. Ananth CV, Peltier MR, Chavez MR, et al. Recurrence of ischemic placental disease. Obstet Gynecol 2007;
110:128.
Topic 6803 Version 10.0
Disclosures
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Diagnostic Procedure For Thrombocyte Disorders: Angelic Trina I. Escoto, RMTDocument57 pagesDiagnostic Procedure For Thrombocyte Disorders: Angelic Trina I. Escoto, RMTDayledaniel SorvetoNo ratings yet
- Anticoagulant & Thrombolytic DrugsDocument68 pagesAnticoagulant & Thrombolytic Drugsezrider7No ratings yet
- Abruptio Placentae 2Document23 pagesAbruptio Placentae 2api-370504650% (2)
- Clinical Study: Development of Dengue Infection Severity ScoreDocument6 pagesClinical Study: Development of Dengue Infection Severity ScoreValencius SunandarNo ratings yet
- Perioperative Reda Harby NotesDocument23 pagesPerioperative Reda Harby NotesSazzad100% (2)
- 75-Practice Questions-Staff-Nurse Gov ExamDocument4 pages75-Practice Questions-Staff-Nurse Gov ExamPrakashNo ratings yet
- Pathanatomy Unit 1 - Unit 6 Q&ADocument12 pagesPathanatomy Unit 1 - Unit 6 Q&AChris Queiklin0% (1)
- IFU Dia TT EN 20170915Document2 pagesIFU Dia TT EN 20170915P managerNo ratings yet
- Ecthyma Gangrenosum - StatPearls - NCBI BookshelfDocument5 pagesEcthyma Gangrenosum - StatPearls - NCBI BookshelfSyafira Laila NurulitaNo ratings yet
- Li v. Soliman-DigestDocument3 pagesLi v. Soliman-DigestEloisa SalitreroNo ratings yet
- Transfusion TherapyDocument14 pagesTransfusion TherapyCMLNo ratings yet
- Advanced Trauma and Surgery PDFDocument455 pagesAdvanced Trauma and Surgery PDFyuliandiazhadi100% (1)
- Petechiae Purpura and Vasculitis ModuleDocument69 pagesPetechiae Purpura and Vasculitis ModulestNo ratings yet
- Anesthetic Management of Amniotic Fluid EmbolismDocument14 pagesAnesthetic Management of Amniotic Fluid Embolismyumna ziaNo ratings yet
- S.I.R.S & M.O.DDocument36 pagesS.I.R.S & M.O.Dshrikanth007No ratings yet
- NCP Resiko PerdarahanDocument3 pagesNCP Resiko PerdarahanRifky FaishalNo ratings yet
- Fitzpatricks Color Atlas and Synopsis of Clinical Dermatology - Exfoliative Erythroderma SyndromeDocument17 pagesFitzpatricks Color Atlas and Synopsis of Clinical Dermatology - Exfoliative Erythroderma SyndromextraqrkyNo ratings yet
- Hemophilia and Factor Assay PDFDocument17 pagesHemophilia and Factor Assay PDFSumaira JunaidNo ratings yet
- Thrombosis Research: Sachin David, Vikram MathewsDocument7 pagesThrombosis Research: Sachin David, Vikram MathewsLaura LópezNo ratings yet
- T. Akahoshi H. Sugimori N. Kaku K. Tokuda T. Nagata E. Noda M. Morita M. Hashizume Y. MaeharaDocument8 pagesT. Akahoshi H. Sugimori N. Kaku K. Tokuda T. Nagata E. Noda M. Morita M. Hashizume Y. Maeharadr. Ayu Nabila Kusuma PradanaNo ratings yet
- Amniotic Fluid EmbolismDocument5 pagesAmniotic Fluid EmbolismDenim Embalzado MaghanoyNo ratings yet
- Lec Framework Care of MotherDocument27 pagesLec Framework Care of MotherRica ParcasioNo ratings yet
- Kasabach Merritt SyndromeDocument33 pagesKasabach Merritt SyndromeAndrew Arnold David VillanuevaNo ratings yet
- Koagulasi Intravaskuler Diseminata Pada Kanker: January 2015Document13 pagesKoagulasi Intravaskuler Diseminata Pada Kanker: January 2015Zinnan Al-FaqihNo ratings yet
- OB PACU Severe PreeclampsiaDocument65 pagesOB PACU Severe Preeclampsiasurbakti_christineNo ratings yet
- Laboratory Evaluation FibrinolysisDocument4 pagesLaboratory Evaluation FibrinolysisMaritoni ReyesNo ratings yet
- Borromeo vs. Family Care HospitalDocument2 pagesBorromeo vs. Family Care HospitalRyo100% (1)
- The Thromboelastogram (TEG®) : A Five-Minute Primer For The Emergency PhysicianDocument11 pagesThe Thromboelastogram (TEG®) : A Five-Minute Primer For The Emergency PhysicianMarcelliaNo ratings yet
- Boc QL - HemaDocument20 pagesBoc QL - HemaFrancis Inno MorandanteNo ratings yet
- ASA Physical Status Classification System - UpToDateDocument2 pagesASA Physical Status Classification System - UpToDateDaniel Rico FuentesNo ratings yet