Professional Documents
Culture Documents
The Body Fluid Compartments
Uploaded by
Alya Putri KhairaniCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Body Fluid Compartments
Uploaded by
Alya Putri KhairaniCopyright:
Available Formats
THE BODY FLUID COMPARTMENTS: EXTRACELLULAR & INTRACELLULAR
Fluid Intake and Output are balanced during Steady-State Conditions
INTAKE
Water is added to the body by 2 major sources: ingested in the form of liquids or water in the food (2100ml/day) and synthesized in
the body as a result of oxidation of carbohydrates (200 ml/day). This provides a total water intake of about 2300 ml/day.
OUTPUT
Insensible water loss
Loss through the skin occurs independently of sweating; average water loss by diffusion through the skin is about 300 400
ml/day. As air enters the respiratory tract, it becomes saturated with moisture, to a vapor pressure of about 47 mmHg, before its
expelled.
Fluid loss in sweat
The amount of water loss by sweating is highly variable, depending on physical activity and environmental temperature. The
volume of sweat normally is about 100 ml/day, but in very hot weather or during heavy exercise water loss in sweat occasionally
increases to 1 2 L/hour
Fluid loss in feces
Only a small amount of water (100ml/day) normally is lost in the feces. This can increase to several liters a day in people with
severe diarrhea
Fluid loss by the kidneys
The remaining water loss from the body occurs in the urine excreted by the kidneys. The kidneys are faced with the task of
adjusting the excretion rate of water and electrolytes to match precisely the intake of these substances, as well as compensating
for excessive losses of fluids and electrolytes that occur in certain disease states
Body Fluid Compartments
Blood Volume
The average blood volume of adults is about 7% of body weight, or about 5 L. About 60% of blood is plasma and 40% is RBC.
Hematocrit is the fraction of the blood composed of RBC. It is determined by centrifuging blood in a "hematocrit tube" until the cells
become tightly packed in the bottom of the tube. It is impossible to completely pack the red cells together; therefore, about 3 to 4
percent of the plasma remains entrapped among the cells, and the true hematocrit is only about 96 percent of the measured
hematocrit
Constituents of Extracellular and Intracellular Fluids
IONIC COMPOSITIONS
Ionic concentration between plasma and interstitial fluid is similar. The most important difference between these 2 compartments is
the higher concentration of protein in the plasma.
Because of the Donnan effect, the concentration of positively charged ions (cations) is slightly greater in the plasma than in the
interstitial fluid. The plasma proteins have a net negative charge and tend to bind cations, such as Na and K ions, thus holding extra
The total body fluid is distributed mainly between 2 compartments: the
extracellular fluid and the intracellular fluid. The extracellular fluid is
divided into the interstitial fluid and the blood plasma. There is another
small compartment of fluid, transcellular fluid. That compartment
includes fluid in the synovial, peritoneal, pericardial, intraocular spaces,
as well as the cerebrospinal fluid. All together constitute 1 2 L.
Intracellular fluid compartment
About 28 of the 42 L of the fluid in the body are inside the 100
trillion cells, or constitutes 40% of the total body weight. The
intracellular fluid of all the different cells together is considered to
be one large fluid compartment
Extracellular fluid compartment
All the fluid outside the cells are called extracellular fluid. These
fluids account for 20% of the body weight, or about 14 L in a normal
70 kg man. Two largest compartments are interstitial fluid, make up
more than (11 L) of the extracellular fluid, and the blood plasma,
makes up almost of extracellular fluid, or about 3 L.
amounts of these cations in the plasma along with plasma proteins. Conversely, negatively charged ions (anions) tend to have a slightly
higher concentration in the interstitial fluid, because the negative charges of plasma proteins repel the negatively charged anions.
INTRACELLULAR FLUID CONSTITUENTS
Intracellular fluid contains only small quantities of Na
+
and Cl
-
ions and almost no Ca
2+
ions. Instead, contains large amounts of K
+
and
PO
4
3-
ions plus moderate quantities of Mg
2+
and SO
4
3-
ions, all of which have low concetrations in the extracellular fluids. Also, cells
contain large amounts of protein
Regulation of Fluid Exchange & Osmotic Equilibrium between Intracellular and Extracellular Fluid
The relative amounts of extracellular fluid distributed between the plasma and interstitial spaces are determined mainly by the balance
of hydrostatic and colloid osmatic forces across the capillary membranes. The distribution of fluid between intracellular and
extracellular compartments, in contrast, is determined mainly by the osmotic effect of the smaller solutes especially Na, Cl, and other
electrolytes acting across the cell membrane. Therefore, water moves across the cell membrane rapidly and the intracellular fluid
remains isotonic with the extracellular fluid
Basic Principles of Osmosis and Osmotic Pressure
Osmosis is the net diffusion of water across a selectively permeable membrane from a region of high water concentration to one that
has a lower water concentration. Water diffuses from a region of low solute concentration (high water concentration) to one with high
solute concentration (low water concentration).
Because cell membranes are relatively impermeable to most solutes but highly permeable to water, whenever there is a higher
concentration of solute on one side of the cell membrane, water diffuses across the membrane toward the region of higher solute
concentration. The rate of diffusion of water is called rate of osmosis
OSMOLALITY AND OSMOLARITY
Definitions
Osmole The number of osmotically active particles in a solution rather than to the molar concentration
Osmolality The osmolal concentration of a solution, expressed as osmoles per kilogram of water
Osmolarity The osmolal concentration of a solution, expressed as osmoles per liter of solution
Osmotic Equilibrium is maintained between Intracellular and Extracellular Fluids
ISOTONIC, HYPOTONIC, AND HYPERTONIC FLUIDS
If a cell is placed in a solution of impermeant solutes having an osmolarity of
282mOsm/L, the cells will not shrink or swell because water concentration in
the intracellular and extracellular fluids is equal and the solutes cannot enter or
leave the cell Isotonic
If a cell is placed into a solution that has a lower concentration of impermeant
solutes (<282 mOsm/L), water will diffuse into the cell, causing it to swell,
diluting the intracellular fluid while also concentrating the extracellular fluid
until both solutions have about the same osmolarity Hypotonic
If a cell is placed in as solution having a higher concentration of impermeant solutes, wateCer will flow out of the cell into extracellular
fluid, concentrating the intracellular fluid and diluting the extracellular fluid. The cell will shrink until the two concentrations become
equal Hypertonic
ISOSMOTIC, HYPEROSMOTIC, AND HYPO-OSMOTIC FLUIDS
The terms isotonic, hypotonic, and hypertonic refer to whether solutions will cause a change in cell volume. The tonicity of solutions
depends on the concentration of impermeant solutes. Some solutes can permeate cell membrane. Solution with an osmolarity the
same as the cell are called isosmotic, regardless of whether the solute can penetrate the cell membrane.
The terms hyperosmotic (ex: urea) and hypo-osmotic refer to solutions that have a higher or lower osmolarity, respectively, compared
with the normal extravellular fluid, without regard for whether the solute permeates the cell membrane
Volume and Osmolality of Extracellular and Intracellular Fluids in Abnormal States
Some of different factors that can cause extrtacellular and intracellular volumes to change markedly are ingestion of IV infusion of
different types of solutions, loss of large amounts of fluid from the GI tract, and loss of amounts of fluid by sweating or through the
kidneys. Basic principles that should be kept in mind:
1. Water moves rapidly across cell membranes: The osmolarities of intracellular and extracellular fluids remain almost exactly equal
to each other except for a few minutes after change in one of the compartments
2. Cell membranes are almost completely impermeable to many solutes: The number of osmoles in the extracellular or intracellular
fluid generally remains constant unless solutes are added to or lost from the extracellular compartments
Clinical Abnormalities of Fluid Volume Regulation: Hyponatremia and Hypernatremia
Definitions
Hyponatremia when plasma sodium concentration is reduced more than a few miliequivalents below normal (142 mEq/L)
Hypernatremia when plasma sodium concentration is elevated above normal
CAUSE OF HYPONATREMIA: EXCESS WATER OR LOSS OF SODIUM
Decreased plasma sodium concentration can result from loss of NaCl from the extracellular fluid or addition of excess water to the
extracellular fluid.
Hyponatremia-dehydration and is associated with decreased extracellular fluid volume
Diarrhea and vomiting causing loss of NaCl
Overuse if diuretics inhibit the ability of kidneys to conserve sodium and certain types of sodium-wasting kidney disease can also
cause modest degrees of hyponatremia
Addisons disease impairs the ability of the kidney to reabsorb sodium
Hyponatremia-overhydration due to excess water retention that dilutes the Na in the extracellular fluid, ex: over secretion of ADH
CONSEQUENCES OF HYPONATREMIA: CELL SWELLING
A rapid reduction in plasma sodium concentration can cause brain cell edema and neurological symptoms, including headache, nausea,
lethargy, and disorientation. If plasma sodium concentration rapidly falls below 115 to 120 mmol/L, brain swelling may lead to seizures,
coma, permanent brain damage, and death. Because the skull is rigid, the brain cannot increase its volume by more than about 10
percent without it being forced down the neck (herniation), which can lead to permanent brain injury and death
When hyponatremia evolves more slowly over several days, the brain and other tissues respond by transporting sodium, chloride,
potassium, and organic solutes, such as glutamate, from the cells into the extracellular compartment. This attenuates osmotic flow of
water into the cells and swelling of the tissues.
Transport of solutes from the cells during slowly developing hyponatremia, however, can make the brain vulnerable to injury if the
hyponatremia is corrected too rapidly. When hypertonic solutions are added too rapidly to correct hyponatremia, this can outpace the
brain's ability to recapture the solutes lost from the cells and may lead to osmotic injury of the neurons that is associated with
demyelination, a loss of the myelin sheath from nerves
(Pictures are left below)
CAUSE OF HYPERNATREMIA: WATER LOSS OR EXCESS SODIUM
Hypernatremia-dehydration cause primary loss of water from the extracellular fluid. This condition can occur from an inability to
secrete antidiuretic hormone, which is needed for the kidneys to conserve water
As a result of lack of antidiuretic hormone, the kidneys excrete large amounts of dilute urine (a disorder referred to as diabetes
insipidus), causing dehydration and increased concentration of sodium chloride in the extracellular fluid. In certain types of renal
diseases, the kidneys cannot respond to antidiuretic hormone, also causing a type of nephrogenic diabetes insipidus.
A more common cause of hypernatremia associated with decreased extracellular fluid volume is dehydration caused by water
intake that is less than water loss, as can occur with sweating during prolonged, heavy exercise.
Hypernatremia can also occur as a result of excessive sodium chloride added to the extracellular fluid. This often results in
hypernatremia-overhydration because excess extracellular sodium chloride is usually associated with at least some degree of
water retention by the kidneys as well
CONSEQUENCES OF HYPERNATREMIA: CELL SHRINKAGE
Severe hypernatremia can occur in patients with hypothalamic lesions that impair their sense of thirst, in infants who may not have
ready access to water, or elderly patients with altered mental status
Edema: excess fluid in the tissues
Edema is the presence of excess fluid in the body tissues, occurs mainly in the extracellular fluid compartment.
INTRACELLULAR EDEMA
Three conditions are prone to cause intracellular swelling: Hyponatremia, Depression of the metabolic systems of the tissues, and
Lack of adequate nutrition to the cells (when blood flow to a tissue is decreased, the delivery of O
2
and nutrients is reduced. If the
blood flow becomes toolow, the cell membrane ionic pumps become depressed. When this occurs, Na that normally leak into the
interior of the cell can no longer be pumped out of the cells and the excess intracellular Na cause osmosis of water into the cells). Can
also occur in inflamed tissues (inflammation increases cell membrane permeability, allowing Na and other ions to diffuse with
subsequent osmosis of water into the cells).
HYPO
NATREMIA
HYPER
NATREMIA
EXTRACELLULAR EDEMA
Two general causes of edema: Abnormal leakage of fluid from the plasma to the interstitial space across the capillaries and Failure of
the lymphatics to return fluid from the interstitium back to the blood (Lymphedema). The most common clinical cause is excessive
capillary fluid filtration.
Factors that can increase capillary filtration
=
)
Lymphedema: failure of the lymph vessel to return fluid and protein to the blood
When lymph vessel function is greatly impaired, due to blockage or loss of the lymph vessels, edema can become especially severe
because plasma proteins that leak into the interstitium have no other way to be removed. The rise in protein concentration raises the
colloid osmotic pressure of the interstitial fluid, which draws even more fluid out of the capillaries.
Lymphedema can also occur in certain types of cancer or after surgery in which lymph vessels are removed or obstructed.
Summary Causes of Extracellular Edema
I. Increased capillary pressure
A. Excessive kidney retention of salt and water
1. Acute or chronic kidney failure
2. Mineralocorticoid excess
B. High venous pressure and venous constriction
1. Heart failure
2. Venous obstruction
3. Failure of venous pumps
(a) Paralysis of muscles
(b) Immobilization of parts of the body
(c) Failure of venous valves
C. Decreased arteriolar resistance
1. Excessive body heat
2. Insufficiency of sympathetic nervous system
3. Vasodilator drugs
II. Decreased plasma proteins
A. Loss of proteins in urine (nephrotic syndrome)
B. Loss of protein from denuded skin areas
1. Burns
2. Wounds
C. Failure to produce proteins
1. Liver disease (e.g., cirrhosis)
2. Serious protein or caloric malnutrition
May related to the case:
EDEMA CAUSED BY DECREASED KIDNEY EXCRETION OF SALT AND WATER
Capillary filtration rate:
K
f
= Capillary filtration coefficient (the product of the
permeability and surface area of the capillaries)
P
c
= Capillary hydrostatic pressure
P
if
= Interstitial fluid hydrostatic pressure
c
= Capillary plasma colloid osmotic pressure
if
= Interstitial fluid colloid osmotic pressure
Any one of the following changes can increase the capillary filtration
rate:
Increased capillary filtration coefficient.
Increased capillary hydrostatic pressure.
Decreased plasma colloid osmotic pressure
III. Increased capillary permeability
A. Immune reactions that cause release of
histamine and other immune products
B. Toxins
C. Bacterial infections
D. Vitamin deficiency, especially vitamin C
E. Prolonged ischemia
F. Burns
II. Blockage of lymph return
A. Cancer
B. Infections (e.g., filaria nematodes)
C. Surgery
D. Congenital absence or abnormality of
lymphatic vessels
Even though many disturbances can cause edema, usually the abnormality must be severe before serious edema develops. The reason
for this is that three major safety factors prevent excessive fluid accumulation in the interstitial spaces:
Low compliance of the interstitium when interstitial fluid pressure is in the negative pressure range
The ability of lymph flow to increase 10- to 50-fold
Washdown of interstitial fluid protein concentration, which reduces interstitial fluid colloid osmotic pressure as capillary filtration
increases
Putting together all the safety factors against edema, we find the following:
1. The safety factor caused by low tissue compliance in the negative pressure range is about 3 mm Hg.
2. The safety factor caused by increased lymph flow is about 7 mm Hg.
3. The safety factor caused by washdown of proteins from the interstitial spaces is about 7 mm Hg
Therefore, the total safety factor against edema is about 17 mm Hg. This means that the capillary pressure in a peripheral tissue could
theoretically rise by 17 mm Hg, or approximately double the normal value, before marked edema would occur.
You might also like
- Electrocardiogram: Electrocardiogram EKG Heart Heart's Electrical Activity DiagnosisDocument38 pagesElectrocardiogram: Electrocardiogram EKG Heart Heart's Electrical Activity DiagnosislorhenzsoNo ratings yet
- CARDIAC CYCLE New For StudentDocument54 pagesCARDIAC CYCLE New For StudentDavi DzikirianNo ratings yet
- Renal Physiology: Done byDocument28 pagesRenal Physiology: Done byJanine Marie Kathleen Uy-CuanangNo ratings yet
- Blood: Beenish Gul Khattak Lecturer Pharmacy Abasyn University PeshawarDocument66 pagesBlood: Beenish Gul Khattak Lecturer Pharmacy Abasyn University PeshawarEsperanza KtkNo ratings yet
- 1.cardiac Muscle The Heart As A Pump and Function of The Heart Valves 2022Document73 pages1.cardiac Muscle The Heart As A Pump and Function of The Heart Valves 2022Sezanur Taalaibek kyzyNo ratings yet
- Maintaining Internal BalanceDocument6 pagesMaintaining Internal BalanceJayrelle D. SafranNo ratings yet
- Vasoactive DrugsDocument61 pagesVasoactive DrugsAde Gustina SiahaanNo ratings yet
- Cardiac CycleDocument29 pagesCardiac CycleRussell Suter100% (1)
- 2012-Fluid and ElectrolytesDocument192 pages2012-Fluid and ElectrolytesHarley Justiniani Dela CruzNo ratings yet
- Mechanisms of Hormone Action NotesDocument3 pagesMechanisms of Hormone Action Notesapi-390361165No ratings yet
- Patterns of RespirationDocument67 pagesPatterns of Respirationsteven hkNo ratings yet
- Endocrine Notes - All in One FileDocument182 pagesEndocrine Notes - All in One FilekjNo ratings yet
- Apoptosis tutorial notes: Understanding programmed cell deathDocument8 pagesApoptosis tutorial notes: Understanding programmed cell deathismealNo ratings yet
- CSF Protection & Flow of the BrainDocument25 pagesCSF Protection & Flow of the BrainchintyamontangNo ratings yet
- Adrenergic Agonist and AntagonistDocument35 pagesAdrenergic Agonist and AntagonistFirjat AfiataNo ratings yet
- Renal PhysiologyDocument75 pagesRenal PhysiologyAmanuel MaruNo ratings yet
- Body FluidsDocument38 pagesBody FluidsGift AiyegbeniNo ratings yet
- Leucocytes 160619161725Document44 pagesLeucocytes 160619161725Rohit K Y100% (1)
- 4 Adrenergic and Anti-Adrenergic DrugsDocument51 pages4 Adrenergic and Anti-Adrenergic DrugsLoai Mohammed IssaNo ratings yet
- Plasma Physiology (1-2020) by DR Khaled A AbulfadleDocument9 pagesPlasma Physiology (1-2020) by DR Khaled A AbulfadleUzama Binu AliNo ratings yet
- Haemotology Notes Haemotology Notes: Medicine (University of Glasgow) Medicine (University of Glasgow)Document20 pagesHaemotology Notes Haemotology Notes: Medicine (University of Glasgow) Medicine (University of Glasgow)shravaniNo ratings yet
- Heart Failure 1Document50 pagesHeart Failure 1dhiraj parmar100% (1)
- (PHYSIO B) 1.2 Renal Physio Pt. 3Document8 pages(PHYSIO B) 1.2 Renal Physio Pt. 3miguel cuevasNo ratings yet
- Posture and EquilibriumDocument26 pagesPosture and Equilibriumshwetha pc100% (1)
- Embryology Cardiovascula Rsystem DevelopmentDocument128 pagesEmbryology Cardiovascula Rsystem DevelopmentGhaidaa SadeqNo ratings yet
- Group 6-B2 - Telomerase, Aging and CancerDocument76 pagesGroup 6-B2 - Telomerase, Aging and CancerJohn Michael Vicente100% (1)
- Metabolism and NutritionDocument52 pagesMetabolism and NutritionAlex SaljayNo ratings yet
- Adrenergic Agonists: Classification and UsesDocument44 pagesAdrenergic Agonists: Classification and UsesAneeza AhmadNo ratings yet
- Bacterial Binary FissionDocument4 pagesBacterial Binary FissionjayweinxNo ratings yet
- 02 AntiarrhythmicAgentsDocument83 pages02 AntiarrhythmicAgentsSiddhant BanwatNo ratings yet
- Cardiac Cycle - DR Rakesh JainDocument97 pagesCardiac Cycle - DR Rakesh JainEmmieNo ratings yet
- Prehospital MedicationsDocument123 pagesPrehospital Medicationshilwaalfi100% (1)
- Arrythmic DrugsDocument43 pagesArrythmic DrugsjanakaNo ratings yet
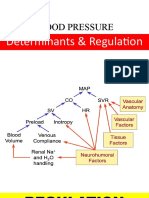
- Short and Long Term Regulation and Determinants of BPDocument90 pagesShort and Long Term Regulation and Determinants of BPDan Tristam MicabaloNo ratings yet
- Disorders of Calcium and Phosphate MetabolismDocument20 pagesDisorders of Calcium and Phosphate MetabolismThirupathi Jakkani100% (1)
- Intravenous FluidsDocument19 pagesIntravenous Fluidsblack pink in ur area 21100% (1)
- Cell Cycle: - Dr. Ishita SinghalDocument69 pagesCell Cycle: - Dr. Ishita SinghalDR. ISHITA SINGHAL100% (1)
- Table of Leukemias and LymphomasDocument7 pagesTable of Leukemias and LymphomasRhenjay Ferrer Lagoy100% (1)
- Multiple Choice Questions: Control of Gene ExpressionDocument82 pagesMultiple Choice Questions: Control of Gene ExpressionJing Li100% (1)
- Cardiomyopathy Joisy AloorDocument31 pagesCardiomyopathy Joisy AloorJoisy AloorNo ratings yet
- PTT Body FluidsDocument29 pagesPTT Body FluidsMalla Nova LayukNo ratings yet
- ED Dilution Guide 2018 - Jan 2019Document42 pagesED Dilution Guide 2018 - Jan 2019asyrafrusydi9901No ratings yet
- Diabetic Nephropathy: Assisstant Professor Dr. Mihaela-Dora DonciuDocument65 pagesDiabetic Nephropathy: Assisstant Professor Dr. Mihaela-Dora DonciuFloreaAndreiNo ratings yet
- Blood Pressure Regulation-2Document40 pagesBlood Pressure Regulation-2Juliza FelicianoNo ratings yet
- Acute Leukemias: Causes, Types, Symptoms and TreatmentDocument60 pagesAcute Leukemias: Causes, Types, Symptoms and TreatmentThaveeshaLindsayWhite100% (1)
- Blood Cells, Immunity and Blood ClottingDocument65 pagesBlood Cells, Immunity and Blood Clottingmunaamuummee100% (1)
- 10 Adrenergic Agonists (Notes) AtfDocument13 pages10 Adrenergic Agonists (Notes) AtfFeven AbrahamNo ratings yet
- Membrane Transport Mechanisms and HomeostasisDocument29 pagesMembrane Transport Mechanisms and Homeostasisramadan100% (1)
- Traumatic Brain InjuryDocument49 pagesTraumatic Brain InjuryCHANGEZ KHAN SARDARNo ratings yet
- Transport of Oxygen and Carbon Dioxide-PartialDocument24 pagesTransport of Oxygen and Carbon Dioxide-PartialMarie PetalcorinNo ratings yet
- 18 Vessels and Flow DynamicsDocument57 pages18 Vessels and Flow Dynamicsraanja2No ratings yet
- 3-Major Veins of The BodyDocument26 pages3-Major Veins of The BodyTJPlayz100% (1)
- Vitamin D and CalcitoninDocument28 pagesVitamin D and CalcitoninEsome SharmaNo ratings yet
- DNA Topology Supercoiling and Linking PDFDocument5 pagesDNA Topology Supercoiling and Linking PDFmanoj_rkl_07No ratings yet
- Anatomy of Larynx Lecture 7Document21 pagesAnatomy of Larynx Lecture 7sallykamareddine100% (1)
- Describe The Factors Affecting Cardiac OutputDocument6 pagesDescribe The Factors Affecting Cardiac OutputSis SukarnoNo ratings yet
- L - 2 Physiology of Respiration IIDocument25 pagesL - 2 Physiology of Respiration IIkaukab azimNo ratings yet
- Leading U: Inspirational Stories from UAlberta Alumni & StudentsFrom EverandLeading U: Inspirational Stories from UAlberta Alumni & StudentsNo ratings yet
- Uric Acid and Its MetabolismDocument3 pagesUric Acid and Its MetabolismAlya Putri KhairaniNo ratings yet
- Inhalation InjuryDocument2 pagesInhalation InjuryAlya Putri KhairaniNo ratings yet
- Chapter 3 A Neuro Disorders Public H ChallengesDocument71 pagesChapter 3 A Neuro Disorders Public H ChallengesAnna Francesca AbarquezNo ratings yet
- Inhalation InjuryDocument2 pagesInhalation InjuryAlya Putri KhairaniNo ratings yet
- Function of SinusesDocument1 pageFunction of SinusesAlya Putri KhairaniNo ratings yet
- Iccu / Cicu: Patients Heart Attacks Unstable Angina Cardiac DysrhythmiaDocument4 pagesIccu / Cicu: Patients Heart Attacks Unstable Angina Cardiac DysrhythmiaAlya Putri KhairaniNo ratings yet
- Pericardium:: AnatomyDocument4 pagesPericardium:: AnatomyAlya Putri KhairaniNo ratings yet
- Leptospira SP.: Leptospira Are Spiral Bacteria (Spirochaete) in The Family of LeptospiraceaeDocument3 pagesLeptospira SP.: Leptospira Are Spiral Bacteria (Spirochaete) in The Family of LeptospiraceaeAlya Putri KhairaniNo ratings yet
- Community Nutrition & Physician's ResponsibilityDocument16 pagesCommunity Nutrition & Physician's ResponsibilityAlya Putri KhairaniNo ratings yet
- Bleeding: Blood VesselDocument2 pagesBleeding: Blood VesselAlya Putri KhairaniNo ratings yet
- Normal X RayDocument6 pagesNormal X RayAlya Putri KhairaniNo ratings yet
- Hypersensitivity Type IDocument3 pagesHypersensitivity Type IAlya Putri KhairaniNo ratings yet
- Colorectal CacinomaDocument2 pagesColorectal CacinomaAlya Putri KhairaniNo ratings yet
- Renal Regulation of PotassiumDocument5 pagesRenal Regulation of PotassiumAlya Putri KhairaniNo ratings yet
- Colorectal CacinomaDocument2 pagesColorectal CacinomaAlya Putri KhairaniNo ratings yet
- Congenital Syphilis Causes and TreatmentDocument4 pagesCongenital Syphilis Causes and TreatmentAlya Putri Khairani100% (1)
- Kinesiology of Shoulder Complex MusclesDocument7 pagesKinesiology of Shoulder Complex MusclesAlya Putri KhairaniNo ratings yet
- Histogenesis and Cell Types in Bone FormationDocument6 pagesHistogenesis and Cell Types in Bone FormationAlya Putri KhairaniNo ratings yet
- Clobetasol Propionate and Urea CreamDocument4 pagesClobetasol Propionate and Urea CreamAlya Putri KhairaniNo ratings yet
- Anatomy of Oral RegionDocument6 pagesAnatomy of Oral RegionAlya Putri KhairaniNo ratings yet
- Hemolytic Anemia: MorphologyDocument10 pagesHemolytic Anemia: MorphologyAlya Putri KhairaniNo ratings yet
- How Tetanus or Dental Caries Can Cause Cardiovascular DiseaseDocument3 pagesHow Tetanus or Dental Caries Can Cause Cardiovascular DiseaseAlya Putri KhairaniNo ratings yet
- Diagnosing and Managing Systemic Lupus ErythematosusDocument3 pagesDiagnosing and Managing Systemic Lupus ErythematosusAlya Putri KhairaniNo ratings yet
- Influenza: Laboratory FindingsDocument6 pagesInfluenza: Laboratory FindingsAlya Putri KhairaniNo ratings yet
- Staging of HerniaDocument1 pageStaging of HerniaAlya Putri KhairaniNo ratings yet
- Leptospira SP.: Leptospira Are Spiral Bacteria (Spirochaete) in The Family of LeptospiraceaeDocument3 pagesLeptospira SP.: Leptospira Are Spiral Bacteria (Spirochaete) in The Family of LeptospiraceaeAlya Putri KhairaniNo ratings yet
- Failure To ThriveDocument3 pagesFailure To ThriveAlya Putri KhairaniNo ratings yet
- Herpes VirusesDocument6 pagesHerpes VirusesAlya Putri KhairaniNo ratings yet
- Inhalation InjuryDocument2 pagesInhalation InjuryAlya Putri KhairaniNo ratings yet
- Conversion DisorderDocument2 pagesConversion DisorderAlya Putri KhairaniNo ratings yet