Professional Documents
Culture Documents
Patho Pneumonia
Uploaded by
Renz Ivan FuntilonOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Patho Pneumonia
Uploaded by
Renz Ivan FuntilonCopyright:
Available Formats
ANATOMY &
PHYSIOLOGY
Anatomy and Physiology of the respiratory system
Respiration is necessary because all living cells of the body require oxygen and produce
carbon dioxide. The respiratory system assists in gas exchange and performs other functions as
well.
1. Gas Exchange
The respiratory system allows oxygen from the air to enter the blood and carbon
dioxide to leave the blood and enter in the air. The cardiovascular system transports
oxygen from the lungs to the cells of the body and carbon dioxide from the cells of the
body to the lungs. Thus the respiratory and cardiovascular systems work together to
supply oxygen to all cells and to remove carbon dioxide. Without healthy respiratory and
cardiovascular systems, the capacity to carry out normal activity is reduced, and without
adequate respiratory and cardiovascular system functions, life itself is impossible.
2. Regulation of Blood pH.
The respiratory system can alter blood pH by changing blood carbon dioxide
levels.
3. Voice Production.
Air movement past the vocal cords makes sound and speech possible.
4. Olfaction.
The sensation of smell occurs when airborne molecules are drawn into the nasal
cavity.
5. Innate Immunity.
The respiratory system provides protection against some microorganism by
preventing their entry into the body and by removing them from respiratory
surfaces
The job of the respiratory system is to keep the body constantly supplied with oxygen
and to remove carbon dioxide. The Respiratory System consist of the nose, pharynx (throat),
larynx (voice box), trachea (windpipe), bronchi and the lungs. Its parts can be classified
according to either structure or function. Structurally, the respiratory system is composed of the
upper and lower respiratory. The upper tract, known as the upper airway, warms and filters
inspired air so that the lower respiratory tract (the lungs) can accomplish gas exchange.
Functionally it is divided into conducting zone and respiratory zone. Conducting Zone is a series
of interconnecting cavities and tubes both outside and within the lungs; nose, pharynx, larynx,
trachea, bronchi, bronchioles, and terminal bronchioles that filter, warm and moisten air and
conduct it into the lungs. Respiratory Zone consisting tissues within the lungs where gas
exchange occurs; the respiratory bronchioles, alveolar ducts, alveolar sacs and alveoli where
the main sites of gas exchange between air and blood. Gas exchange involves delivering
oxygen to the tissues through the bloodstream and expelling waste gases, such as carbon
dioxide, during expiration.
ANATOMY OF THE UPPER RESPIRATORY TRACT
NOSE
* The external portion protrudes from the face and is supported by the nasal bones and cartilage
* Serve as passageway for air to pass and from the lungs
* Filters impurities, humidifies and warms the air as it is inhaled
PARANASAL SINUSES
* Include four pairs of bony cavities that are lined with nasal mucosa and ciliated
pseudostratified columnar epithelium
* The sinuses are named by their location: frontal, ethmoidal, sphenoidal, and maxillary
* Serve as a reasoning chamber in speech
TURBINATE BONES (CONCHAE)
* The name conchae suggested by their shell-like appearance, because of their curves, these
bones increase the mucous membrane surface of the nasal passages and slightly obstruct the
air flowing through them.
PHARYNX, TONSILS, and ADENOIDS
* Pharynx or throat, is a tubeline structure that connects the nasal and oral cavities to the larynx
* Is divided into these regions: nasal, oral, and laryngeal
* Nasopharynx is located posterior to the nose and above the soft palate
* Oropharynx houses the faucial, or palatine, tonsils
* Laryngopharynx extends from the hyoid bone to the cricoids cartilage
* The epiglottis forms the entrance of the larynx
* The adenoids, or pharyngeal tonsils, are located in the roof of the nasopharynx.
LARYNX
* Voice organ; a cartilaginous epithelium-lined structure
that
connects the pharynx and the trachea
* Major function is vocalization
* Protects the lower airway from foreign substances
and facilitates coughing
TRACHEA
* Windpipe; composed of smooth muscle with C-shaped
rings of cartilage at regular intervals
* Serves as the passage between the larynx and the
Bronchi
ANATOMY OF THE LOWER RESPIRATORY TRACT: LUNGS
LUNGS
* Are paired elastic structures enclosed in the thoracic
cage, which is an airtight chamber with distensible
walls
* The narrow superior portion of each lung, the apex, is
located just deep to the clavicle
PLEURA
* Serous membrane lining the lungs and wall of the
thorax
* Visceral pleura covers the lungs
* Parietal pleura lines the thorax
* The visceral and parietal pleura and the small amount of pleural fluid between these two
membranes serve to lubricate the thorax and lungs and permit smooth motion of the lungs
within the thoracic cavity with each breath
LOBES
* The left lung consist of an upper and lower lobe, whereas the right lung has an upper, middle,
and lower lobe
* Each lobe is further divided into two to five segments by fissures, which are extensions of the
pleura
BRONCHI and BRONCHIOLES
* Lobar bronchi (three in the right lung and
two in the left lung); divide into segmental
bronchi (10 on the right and 8 on the left);
segmental bronchi; these bronchi are
surrounded by connective tissue that
contains areteries, lymphatics, and
nerves.
* Bronchioles contain submucosal glands,
which produce mucus that covers the
inside lining of the airways; bronchioles,
which do not have mucous glands or cilia
* The bronchi and bronchioles are lined
also with cells that have surfaces
covered with cilia, these cilia create
constant whipping motion that propels mucus and foreign substances away from lung toward
larynx.
* Terminal bronchioles the become respiratory bronchioles, which are considered to be the
transitional passageways between the conducting airways and gas exchange airways
* The respiratory bronchioles then lead into alveolar ducts and alveolar sac and then alveoli
ALVEOLI
* Oxygen and carbon dioxide exchange takes
place
* The lung is made up of about 300 million
alveoli, which are arranged in clusters of 15 to
20
* 3 types of alveolar cells:
1. Type I alveolar cells are epithelial cells
that form the alveolar walls;
2. Type II alveolar cells arte metabolically
active, these cells secrete surfactant, a phospholipids that lines the inner surface and prevents
alveolar collapse
3. Type III alveolar cell macrophages are large phagocytes that ingest foreign matter and act as
an important defense mechanism
PHYSIOLOGY OF THE RESPIRATORY SYSTEM
The cells of the body derive the energy they need from the oxidation of carbohydrates, fats, and
proteins. Certain vital tissues, such as those of the brain and the heart, cannot survive for long
without a continuing supply of oxygen. However, as a result of oxidation in the body tissues,
carbon dioxide is produced and must be removed from the cells to prevent the build-up of acid
waste products. The respiratory system performs this function by facilitating life-sustaining
process such as oxygen transport, respiration and ventilation, and gas exchange.
OXYGEN TRANSPORT
* Oxygen is supplied to, and carbon
dioxide is removed from cells by way
of the circulating blood
* Oxygen diffuses from the capillary
through the capillary wall to the
interstitial fluid. At this point, it
diffuses through the membrane of
tissue cells, where it is used by
mitochondria for cellular respiration
* The movement of carbon dioxide
occurs by diffusion in the opposite
direction- from cell to blood
RESPIRATION
End of expiration End of Inspiration
* After tissue capillary exchanges, blood enters the systematic veins (where it is called venous
blood) and travels to the pulmonary circulation. The oxygen concentration in the blood within the
capillaries of the lungs is lower than in the lungs air sacs (alveoli). Because of this
concentration gradient, oxygen diffuses from the alveoli to the blood. Carbon dioxide, which has
a higher concentration in the blood into the alveoli. Movement of air in and out of airways
(ventilation) continually replenishes the oxygen and removes the carbon dioxide from the
airways in the lung. This whole process of gas exchange between the atmospheric air and the
blood and between the blood and cells of the body is called respiration.
INSPIRATION
External intercostals muscles Actively contract
- Ribs and sternum move upwards and outwards
- Width of chest increases from side to side, from front to back and from top to bottom
Diaphragm contracts
- Descends
- Depth of chest increases
Capacity of thorax is increased
Pressure between pleural surfaces is reduced.
Elastic tissue of lungs is stretched.
Lungs Expand to fill thoracic cavity
Air pressure within alveoli is now less than atmospheric pressure
Air is sucked into alveoli from atmosphere
EXPIRATION
External intercostals muscles relax
- Rib and sternum move downwards and inwards
- Width of chest diminishes
Diaphragm relaxes
- Ascends
- Depth of chest diminishes
Capacity of thorax is decreased
Pressure between pleural surfaces is increased
Elastic tissue of lungs recoils
Air pressure within alveoli is now greater than atmospheric pressure
Air is forced out of alveoli to atmosphere.
Air pressure variances
> Air flows from a region of higher pressure to a region of lower pressure.
> During inspiration, movement of the diaphragm and the other muscles of respiration enlarge
the thoracic cavity and thereby lower the pressure inside the thorax to a level below that of
atmospheric pressure. As a result, air is drawn through the trachea and bronchi into the small
alveoli.
> During normal expiration, the diaphragm relaxes and the lungs recoil, resulting in the
decrease in the size of thoracic cavity. The alveolar pressure then exceeds atmospheric
pressure, and air flows from the lungs into the atmosphere
Airway resistance
> Resistance is determined chiefly by the radius or size of the airway through which the air is
flowing
> With increased resistance, greater than the normal respiratory effort is required by the patient
to achieve normal levels of ventilation
Compliance
> A measure of the elasticity, expandability, and dispensability of the lungs and thoracic
structures
> Factors that determine lung compliance are the surface tension of the alveoli (normally low
with the presence of surfactant) and the connective tissue of the lungs
> In normal compliance (1.0 L/cm H2O), the lungs and thorax easily stretch and distend when
pressure is applied
DIFFUSION AND PERFUSION
* Diffusion is the process by which oxygen and carbon dioxide are exchange at the air blood
interface
* Pulmonary perfusion is the actual blood flow through the pulmonary circulation; also is
influenced by alveolar pressure
PROTECTIVE MECHANISM OF THE RESPIRATORY SYSTEM
The respiratory system has a number of protective mechanisms;
* Nasal hairs: The large airborne particles are trapped in the nasal hairs which stretch across
the nares.
* Mucus production: The respiratory tract above the bronchioles is lined with epithelium, which
secretes thick, sticky mucas. This waterproofs the inside of the respiratory system and provides
a protective barrier against any irritants.
* Cilia: These are minute hair-like projections of the epithelium lining along the respiratory
tract. They move the mucas and trapped particles towardsthe throat
* Sneezing: Protective reflex which is stimulated when the nasal mucosa is irritated.
* Coughing: Reflex mechanism for removing excess mucus or other irritants from the air
passengers beyond the nose.
* Phagocyte activity: Phagocytic cells in the epithelium engulf debris, dust and bacteria s well
as help to filter incoming air.
* Epithelial lining: The filtration in the nasal cavity removes large particles, small particles are
trapped as they pass through the bronchial tree and smaller particles are trapped in the mucus
of the respiratory bronchioles or in the alveolar fluid where they are engulfed by the
macrophages. The debris are cleared out of the system by the coughing and sneezing reflexes.
PATHOPHYSIOLOGY
A. Etiology
Community Acquired Pneumonia is differentiated from pneumonia from
contact with germs you encounter in the course of your normal routine. These
commonplace germs generally cause mild forms of pneumonia that doctors can
treat without difficulty. The microbes responsible for most community-acquired
pneumonia are:
Bacteria.
The bacterium that causes most cases of community-acquired
pneumonia is Streptococcus pneumoniae. Other possible agents include
Staphylococcus aureus, Haemophilus influenzae and Klebsiella
pneumoniae. It's not unusual to have pneumonia caused by more than one
type of bacteria at a time. Methicillin-resistant Staphylococcus aureus
(MRSA), an antibiotic-resistant bacterium once found only in health care
settings, now causes skin infections and pneumonia in the community, too.
Bacteria-like organisms.
Mycoplasma pneumoniae is a tiny organism that typically produces
milder signs and symptoms than other types of pneumonia. Walking
pneumonia, a term used to describe pneumonia that isn't severe enough to
require bed rest, may result from Mycoplasma pneumoniae. Legionella and
Chlamydia pneumonia are two other pneumonia-causing germs that are
neither bacteria nor viruses.
Viruses.
Some of the same types of viruses that cause the flu and colds can
also cause pneumonia. Although most cases of viral pneumonia are mild
and resolve in time with rest and fluids, viral pneumonia caused by influenza
viruses can become very serious. Viral pneumonia can set up a prime
environment for the invasion of bacteria, causing a second infection.
Fungi and parasites.
Other less-common causes of community-acquired pneumonia
include fungi, parasites and the germ that causes tuberculosis. Most cases
of parasitic pneumonia occur in people who live or have traveled in
developing countries.
PREDISPOSING FACTORS
PREDISPOSING
FACTORS
ACTUAL RATIONALE
Age
In general, pneumonia is more likely to
affect those who have weaker immune
systems. It is most common among
very young children, whose immune
systems aren't fully developed and also
to people around the age of 65 or older,
particularly if they have other conditions
that make them more prone to
developing pneumonia.
Nationality/Race
X
When it comes to race, African
Americans, American Indians and
Alaskans have a higher risk of getting
pneumonia. According to the American
Lung Association, African Americans
tend to die from influenza and
pneumonia more often than Caucasians
and other ethnicities due to improper
treatment of the condition.
Season
Community Acquired Pneumonia is
most prevalent during winter and spring.
or in our country, rainy season. This is
also the time where most cases of
upper respiratory Tract Infection occur.
Medical History
X
One of the main reasons that people's
immune systems are weaker than
normal is that they suffer from some
other chronic medical condition. People
with AIDS/HIV, chronic lung disease,
diabetes, gastro esophageal reflux
disease (GERD), heart disease and
congenital defects are at risk for CAP.
PRECIPITATING FACTORS
PRECIPITATING
FACTORS
ACTUAL RATIONALE
Smoking
X
People who Smoke or are 2
nd
hand
smokers, and work or live close to
factories are more likely to acquire
pneumonia.
Hygiene
X
People who do not have good
hygiene are more likely to have CAP
especially those who practice
improper hand washing and improper
handling of food. Frequent hygiene
care is needed to prevent acquiring
pneumonia. Children are more likely
to be at risk especially when they are
not guided to do proper washing.
Poor Immune
System
Very young children are at risk for
acquiring CAP because of their
underdeveloped immune system.
Immunizations and nutrition play an
important part in the immune system
and may prevent the child from
acquiring pneumonia.
Symptomatology
SYMPTOMS ACTUAL RATIONALE
Pleuritic Chest Pain
X
It Indicates pleural inflammation in
the parietal pleura which is rich in
sensory nerve endings.
Fever
It is caused by the release of
pyrogens that reset the
hypothalamus thermostat.
Sudden onset of
chills
X
It is because of the invasion of
microorganism which causes the
inflammatory process.
Crackles
This is due to lung congestion or
consolidation.
Wheezes
X
This is due to the accumulation of
secretions in the airway which
causes it to be narrowed.
Cyanosis
X
This is because of the interference
in the oxygen and carbon dioxide
exchange which then causes
hypoxemia.
Dyspnea
Due to the narrowed airway and
lung congestion, dyspnea may
occur.
Cough
X
This is also caused by bacterial
invasion. It usually brings up
yellowish and greenish mucous.
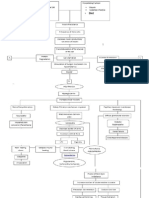
SCHEMATIC DIAGRAM
PREDISPOSING FACTORS
Age Season
PRECIPITATING FACTORS
Poor Immune System
Inhalation of microorganisms
Activation of the upper airway defense mechanism, cough
reflex, mucocillary clearance and nasopharyngeal defense
Invasion of foreign bodies in the URT
Pathogen tries to enter the lower
respiratory tract
The body tries to remove the
pathogen that entered the URT
Pathogens begin to colonize
Activation of inflammatory process
Release of nasal discharges
A
Engorgement
Red Hepatization
Gray Hepatization
Resolution
A
WBCs enter the alveoli Vascular Engorgement/
Vasodilation
Increase in vascular
permeability
Hypersecretion of mucus
membrane
Release of pyrogens
Stimulates the thermoregulatory
center of the body to reset
temperature
Fever
Fluid accumulation in the
alveolar sac
Impaired gas exchange
Dyspnea and Tachypnea
Hypoxemia and Pallor
Chest pain
Crackles
B C
Treatment:
Tepid Sponge bath
Administer antipyretics
B
C
If not treated If treated
Bacteremia
Respiratory Failure
Empyema Necrosis of the lung Lung abscess Acute Respiratory
Distress Syndrome
Multi Organ Failure
Death
Bad Prognosis
Responds well to
antimicrobial therapy
Good Prognosis
NARRATIVE
Community-acquired pneumonia (CAP) is one of several diseases in which
individuals who have not recently been hospitalized develop an infection of the lungs
(pneumonia). CAP is a common illness and can affect people of all ages. CAP often
causes problems like difficulty in breathing, fever, chest pains, and a cough. It occurs
because the areas of the lung which absorb oxygen (alveoli) from the atmosphere
become filled with fluid and cannot work effectively.
Community-acquired pneumonia occurs throughout the world and is a leading
cause of illness and death. Causes of CAP include bacteria, viruses, fungi, and
parasites. It can be diagnosed by symptoms and physical examination alone, though x-
rays, examination of the sputum, and other tests are often used. Though some people
with CAP need to be hospitalized, it is primarily treated with antibiotic medication. Some
forms can even be prevented by vaccination.
Meanwhile, CAP in children is basically a self-limiting condition most of the time.
It starts with the inhalation of microorganisms that may be caused by the predisposing
and precipitating factors. This causes an invasion of foreign bodies in the Upper
respiratory tract. As a result, the body activates the upper airway defense mechanism;
the cough reflex, the mucocillary clearance and the nasopharyngeal defense.
Pathogens then begin to colonize if the defense mechanism fails. The pathogens will
then try to enter the lower respiratory tract. The body again tries to remove the
pathogen that entered the upper respiratory tract by releasing nasal discharges, which
will cause the person to sneeze.
Meanwhile damage occurs to mucous membrane when the defense proves to be
unsuccessful.
The 4 stages of pneumonia occur and the first is the engorgement phase or
the edema phase (4-12 h). There will be the presence of proteinaceous exudates. Next is the
red hepatization (next 48 h).in this phase, there is the presence of erythrocyte and presence of
neutrophils. Third is the gray hepatization (3-8 d), here, no new erythrocytes are extravastating,
neutrophils is the predominant cell and improvement in gas exchange. Last stage is the
resolution (7-11 d).Macrophage is the dominant cell, neutrophils, bacteria, and fibrin has been
cleared.
With the pathogen entering the lower respiratory tract to the alveoli, the bodys
inflammatory defense mechanism activates. White blood cells enter the alveolar sac to combat
the pathogens and releasing pyrogens thus causing fever, which is a normal inflammatory
response of the body to infection. There is also vasodilation of alveolar capillaries, vascular
permeability increases making the RBCs, fibrin, cytokines, serous fluids and exudates to enter
and accumulate in the alveolar sac which now will cause impaired gas exchange making it
harder to breath( Dyspnea ), decreased O2 and chest pain. Hypersecretion of the mucus
membrane as a way to remove pathogens, upon auscultation crackles will be present.
With treatment, most patients will improve within 2 weeks. Some patients with
viral infection often resolve without treatment. However, without treatment, Community Acquired
Pneumonia may lead to complications such as Bacteremia, Lung abscess, Empyema, Necrosis
of the lung, Acute Respiratory Distress Syndrome (ARDS) and many more that may cause
death.
You might also like
- How Do Humans Breathe? Science Book Age 8 | Children's Biology BooksFrom EverandHow Do Humans Breathe? Science Book Age 8 | Children's Biology BooksNo ratings yet
- Lung Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandLung Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Human Respiratory System Aniket DasDocument11 pagesHuman Respiratory System Aniket DasChep KepNo ratings yet
- Anatomic and Physiologic OverviewDocument8 pagesAnatomic and Physiologic OverviewJoseph King MacaranasNo ratings yet
- Respiratory SystemDocument74 pagesRespiratory SystemJonald Pulgo IcoyNo ratings yet
- Respiratory System (Anatomy and Physiology)Document71 pagesRespiratory System (Anatomy and Physiology)Butch Dumdum100% (11)
- Respiratorysystem 120105050542 Phpapp01Document43 pagesRespiratorysystem 120105050542 Phpapp01Buuvee BeNo ratings yet
- Respiratory System FinalDocument70 pagesRespiratory System FinalmosabNo ratings yet
- LEC - Week 9 (Respiratory)Document42 pagesLEC - Week 9 (Respiratory)Al SerenosoNo ratings yet
- Respiratory SystemDocument8 pagesRespiratory Systemkayeemperado997No ratings yet
- Supplementary Material 3.1 Basic Concepts and Assessment (N) - 2Document13 pagesSupplementary Material 3.1 Basic Concepts and Assessment (N) - 2Kent Borro CantomayorNo ratings yet
- Introduction To Respiratory SystemDocument21 pagesIntroduction To Respiratory Systemangel demonyoNo ratings yet
- Respiratory System 8Document32 pagesRespiratory System 8Naanmatha PuspanathanNo ratings yet
- Respiratory System: Anatomy of Respiratory Organs and Their FunctionsDocument6 pagesRespiratory System: Anatomy of Respiratory Organs and Their FunctionsRishabh SharmaNo ratings yet
- AaDocument324 pagesAaBirhanu AyenewNo ratings yet
- Anatomy & Physiology of Respiratory SystemDocument12 pagesAnatomy & Physiology of Respiratory SystemDgjj CompuiterNo ratings yet
- Animalphysio2nd 180428184330Document28 pagesAnimalphysio2nd 180428184330environmentalgyanNo ratings yet
- Chapter 13 The Respiratory SystemDocument7 pagesChapter 13 The Respiratory Systemqueen nurseNo ratings yet
- Human Biology: Respiratory SystemDocument33 pagesHuman Biology: Respiratory SystemSaikrishna RaoNo ratings yet
- Anatomy and Physiology Respiratory SystemDocument6 pagesAnatomy and Physiology Respiratory SystemCarlos Alfonso Borromeo AmoresNo ratings yet
- Anatomy and Physiology: PHYSIOLOGY-the Branch of Biology That Deals With The Internal Workings ofDocument4 pagesAnatomy and Physiology: PHYSIOLOGY-the Branch of Biology That Deals With The Internal Workings ofshonievin100% (2)
- The Respiratory SystemDocument16 pagesThe Respiratory SystemAirene Mae Lamputi SupilarNo ratings yet
- Anatomy and Physiology Respiratory SystemDocument7 pagesAnatomy and Physiology Respiratory Systemnoronisa talusobNo ratings yet
- Iv. Anatomy and Physiology of The Human Respiratory SystemDocument5 pagesIv. Anatomy and Physiology of The Human Respiratory SystemJenny Vi CodenieraNo ratings yet
- Anaphy - Respi & LiverDocument13 pagesAnaphy - Respi & LiverANAMAZING CHANNELNo ratings yet
- ANATOMYDocument53 pagesANATOMYJocel Mae OrtegaNo ratings yet
- Chapter II - Respiratory SystemDocument3 pagesChapter II - Respiratory SystemIndranil SinhaNo ratings yet
- Anatomy and Physiology of Respiratory SystemDocument9 pagesAnatomy and Physiology of Respiratory SystemLiza Marie Cayetano AdarneNo ratings yet
- Respiratory System PreDocument11 pagesRespiratory System PrecontehamosaNo ratings yet
- Respiratory System in Human BeingsDocument11 pagesRespiratory System in Human BeingsSarada KasyapNo ratings yet
- Anatomy and Physiology: The Respiratory SystemDocument82 pagesAnatomy and Physiology: The Respiratory SystemMaria Angelique Ofciar100% (2)
- A & P RespiratoryDocument18 pagesA & P Respiratoryamirul haakimNo ratings yet
- OxygenationDocument20 pagesOxygenationKhie-An OcampoNo ratings yet
- Respiiiraatatoory SystemDocument78 pagesRespiiiraatatoory Systempriyanshuraj717No ratings yet
- Parts and Functions of Respiratory SystemDocument18 pagesParts and Functions of Respiratory Systemjosephabram051590No ratings yet
- X Respiratory SystemDocument31 pagesX Respiratory SystemHannah DiñosoNo ratings yet
- Respiratory SystemDocument53 pagesRespiratory SystemRotan CirebonNo ratings yet
- Respiratory System Anatomy, Assessment & Diagnostic TestsDocument24 pagesRespiratory System Anatomy, Assessment & Diagnostic TestsPrince Rener Velasco PeraNo ratings yet
- Res (Iratory SystemDocument2 pagesRes (Iratory SystemJosielyn ValladolidNo ratings yet
- Respiratory Anatomy Physiology and Dse DefinitionDocument4 pagesRespiratory Anatomy Physiology and Dse Definitionmiss RN100% (2)
- Module 4 Respiratory SystemDocument8 pagesModule 4 Respiratory SystemJake Donely C. PaduaNo ratings yet
- Gas Exchange in HumansDocument23 pagesGas Exchange in HumansVNo ratings yet
- Anatomi Saluran PernapasanDocument6 pagesAnatomi Saluran PernapasanfidyaNo ratings yet
- ReproductiveDocument5 pagesReproductiveJason Vinluan CarinanNo ratings yet
- Group1 Review of Respiratory SystemDocument41 pagesGroup1 Review of Respiratory Systemjohn obinaNo ratings yet
- Body SystemDocument15 pagesBody SystemChris Timothy TurdanesNo ratings yet
- Respiratory System s2 2019Document56 pagesRespiratory System s2 2019noviantyramadhani12No ratings yet
- Respiratory System: Nose and Nasal CavityDocument8 pagesRespiratory System: Nose and Nasal CavityJasper AlbuferaNo ratings yet
- 1.oxygenation DisordersDocument8 pages1.oxygenation Disorders2BGrp3Plaza, Anna MaeNo ratings yet
- Breathing and Exchange of GasesDocument17 pagesBreathing and Exchange of GasesArjun ChristopherNo ratings yet
- Anatomy and Physiology Power PointDocument8 pagesAnatomy and Physiology Power PointJoanna Diongson GonzalesNo ratings yet
- Respiratory System: Group 5Document16 pagesRespiratory System: Group 5Rashid DayaoNo ratings yet
- Science Reviewer (MID)Document53 pagesScience Reviewer (MID)Francesca KatigbakNo ratings yet
- Anatomy & PhysiologyDocument42 pagesAnatomy & PhysiologyArah Lyn ApiagNo ratings yet
- Introduction To Acute Respiratory FailureDocument6 pagesIntroduction To Acute Respiratory FailureErieca Barsabal PamittanNo ratings yet
- Gaseous ExchangeDocument37 pagesGaseous ExchangeSolángé MirembeNo ratings yet
- Respiratory SystemDocument31 pagesRespiratory SystemMark Jhosua Austria GalinatoNo ratings yet
- Problems With OxygenationDocument92 pagesProblems With OxygenationEbiNo ratings yet
- Parts and Functions of Respiratory System.Document3 pagesParts and Functions of Respiratory System.Alvin Patrick Colobong AsisNo ratings yet
- Respiratory Physiology Part 1Document9 pagesRespiratory Physiology Part 1kabir musa ladanNo ratings yet
- Pathophysiology of Protein S DeficiencyDocument5 pagesPathophysiology of Protein S DeficiencyRenz Ivan FuntilonNo ratings yet
- Drug AmpicillinDocument2 pagesDrug AmpicillinRenz Ivan FuntilonNo ratings yet
- Anatomy and Physiology of The Respiratory SystemDocument57 pagesAnatomy and Physiology of The Respiratory SystemRenz Ivan FuntilonNo ratings yet
- AFRICA and EGYPT (Humanities)Document5 pagesAFRICA and EGYPT (Humanities)Renz Ivan FuntilonNo ratings yet
- HydrocortisoneDocument2 pagesHydrocortisoneRenz Ivan Funtilon100% (1)
- OgiveDocument16 pagesOgiveRenz Ivan FuntilonNo ratings yet
- Pathophysiology of Diabetes Mellitus Type 2Document6 pagesPathophysiology of Diabetes Mellitus Type 2Renz Ivan FuntilonNo ratings yet
- Anatomy and Mechanics of The Human HandDocument14 pagesAnatomy and Mechanics of The Human Handerwinmiranda20033No ratings yet
- Janoras, DM (Tissue Mind Map)Document1 pageJanoras, DM (Tissue Mind Map)maxine janorasNo ratings yet
- Schuyler 1932Document10 pagesSchuyler 1932Kev aqpNo ratings yet
- Brachial Plexus InjuriesDocument346 pagesBrachial Plexus InjuriesvinaymanNo ratings yet
- Bates CH 17 NeuroDocument11 pagesBates CH 17 NeurokandeeNo ratings yet
- SEMI q4 Nervous SystemDocument10 pagesSEMI q4 Nervous Systemdhanessa condes100% (2)
- CNS Case PresentationDocument9 pagesCNS Case Presentation073-NAGULAN SHIVAKUMARNo ratings yet
- Control and CoordinationDocument22 pagesControl and CoordinationMozibor RahmanNo ratings yet
- Science 9 Final ExamDocument4 pagesScience 9 Final ExamGusthe Jebb AzarconNo ratings yet
- Kanski Clinical Ophthalmology Chapter 3 ORBITDocument43 pagesKanski Clinical Ophthalmology Chapter 3 ORBITSekar Ayu WulandariNo ratings yet
- Physical AssessmentDocument2 pagesPhysical AssessmentEdmar DalmacioNo ratings yet
- Skull Connections of The Skull BonesDocument72 pagesSkull Connections of The Skull BonesBianca VaidaNo ratings yet
- Anatomía Relacional de Los Músculos MiméticosDocument5 pagesAnatomía Relacional de Los Músculos MiméticosLizeth Conde OrozcoNo ratings yet
- 1.2E Strabismus: ObjectivesDocument2 pages1.2E Strabismus: ObjectivesBea SamonteNo ratings yet
- Autonomic Nervous System For MBBSDocument20 pagesAutonomic Nervous System For MBBSjacobsNo ratings yet
- Exercise Program PDF SadekDocument1 pageExercise Program PDF SadekowenbNo ratings yet
- Spartan Elite Gym 1Document9 pagesSpartan Elite Gym 1Sunil RathodNo ratings yet
- 15 Spinal Cord External FeaturesDocument81 pages15 Spinal Cord External FeaturesPraveen BaddipudiNo ratings yet
- Trauma: Accidental Temporal Bone Fractures Classification SchemesDocument12 pagesTrauma: Accidental Temporal Bone Fractures Classification SchemesDr-Firas Nayf Al-ThawabiaNo ratings yet
- Asymmetric Extraction in Orthodontic Treatment of Malocclusion Class I LeftDocument9 pagesAsymmetric Extraction in Orthodontic Treatment of Malocclusion Class I LeftdianaglezherediaNo ratings yet
- El Yoga Facelift - M-V Nadeau - TraducidoDocument164 pagesEl Yoga Facelift - M-V Nadeau - TraducidoNancy SavinoNo ratings yet
- Class1 Open BiteDocument24 pagesClass1 Open Bitetowncommitteeabdulhakim15401No ratings yet
- BBB Month 13 Workout Log PDFDocument8 pagesBBB Month 13 Workout Log PDFGeraldyneNo ratings yet
- Psychology PresentationDocument16 pagesPsychology PresentationFasih RehmanNo ratings yet
- BRIEF 3.0 PDF Fill-In PDFDocument1 pageBRIEF 3.0 PDF Fill-In PDFSMIT SHARMANo ratings yet
- Dave Tate - Supplemental StrengthDocument20 pagesDave Tate - Supplemental StrengthLegenda Kralj100% (1)
- Posterior Hip Dislocation Case FileDocument2 pagesPosterior Hip Dislocation Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Pictorial Essay: Anatomical Variations of Paranasal Sinuses On Multidetector Computed Tomography-How Does It Help FESS Surgeons?Document8 pagesPictorial Essay: Anatomical Variations of Paranasal Sinuses On Multidetector Computed Tomography-How Does It Help FESS Surgeons?claragustin_53768590No ratings yet
- June 2021 Case Census BlankDocument2 pagesJune 2021 Case Census BlankJustitia Et PrudentiaNo ratings yet
- Vocabulary in 1 Hour - Speak English With VanessaDocument10 pagesVocabulary in 1 Hour - Speak English With VanessaEderson Gomes da SilvaNo ratings yet