Professional Documents
Culture Documents
Pharmacology Lecture Hypertension: Dealwithmaie6523
Uploaded by
Maielyne Keith B. DalilisOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmacology Lecture Hypertension: Dealwithmaie6523
Uploaded by
Maielyne Keith B. DalilisCopyright:
Available Formats
Pharmacology Lecture Hypertension 2014
1
dealwithmaie6523
A. Blood Pressure
1. What is Blood Pressure?
a.k.a: Arterial Pressure the pressure exerted by the circulating volume of blood on the walls of the arteries and veins and on the chambers of the
heart
pressure exerted by the blood on the walls of a blood vessel
2. Types of Blood Pressure
a. Systole pressure exerted by the heart to pump out blood
contraction of the heart driving blood into the aorta and pulmonary arteries
refers to the upper number, in mmHg
ventricular contraction
b. Diastole pressure when the heart is at rest; exerted against the walls of the blood vessels
period within contractions of the atria or the ventricles during which blood enters the relaxed chambers from the systemic circulation and
the lungs
refers to the lower number, in mmHg
ventricular relaxation
Normal: 120/80 Range:
3. Hydrostatic equation
According to the hydrostatic equation, arterial blood pressure (BP) is directly proportional to the product of the blood flow (CO) and the
resistance to passage of blood through precapillary arterioles (PVR).
BP = CO x PVR
*Cardiac Output volume of blood ejected from the left ventricle/right ventricle into the aorta/pulmonary trunk each minute. Cardiac output equals
the stroke volume (volume of blood ejected by the ventricle during each contraction) multiplied by the heart rate (number of heartbeats per
minute)
CO = SV x HR
*Peripheral Vascular Resistance force of the blood pressure; the opposition to blood flow due to friction between blood and the walls of blood
vessels. (size of BV lumen, blood viscosity, total BV length)
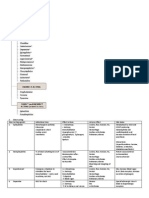
4. Classification of Blood Pressure by JNC (Joint National Committee)
Systole Diastole
Normal 120 80
Prehypertension 121 - 139 81 89
Stage 1 140 - 159 90 99
Stage 2 160 100
5. Regulation of BP
Organs involved include: heart, blood vessels, ANS-SANS
Neural Regulation of Blood Pressure
a. Baroreceptor Reflexes - a sensory receptor located in the aorta, internal carotid arteries (found in the neck that supplies blood in the
brain), and other large arteries in the neck and chest; regulate BP
Stimuli BP Baroreceptors CV Center (+)inotropy-F of contraction SV & HR BP
(+)chronotropy-HR PVR
(+)dromotropy-conduction of impulse
(+)bathmotropy-excitability,sensitive impulse
change in body position particularly form sitting to standing position blood will rush below the heart detected by baroreceptors
b. Chemoreceptor Reflexes - a sensory receptor that monitor the chemical composition of blood, are located close to the baroreceptors of
the carotid sinus and arch of aorta
detects changes in O2(hypoxia= O2), CO2(hypercapnia= CO2), and H
+
(acidosis= H
+
conc)
Pharmacology Lecture Hypertension 2014
2
dealwithmaie6523
Stimuli chemoreceptors CV Center sympathetic vasoconstriction BP
(arterioles & veins)
Hormonal Regulation of BP
a. Renin-angiotensin-aldosterone (RAA) System
b. Epinephrine and Norepinephrine adrenal medulla
Epi & Nor (+)chronotropy CO BP
(+)inotropy
c. Antidiuretic hormone (ADH) aka vasopressin; pdc by hypothalamus and released by posterior pituitary in response to dehydration
and BV
ADH vasoconstriction BP
H2O to bloodstream BV,urine
d. Atrial Natriuretic Peptide released by cells in the atria of the heart
ANP loss of NaCl and H2O BV,vasodilation BP
Autoregulation of BP
Ability of a tissue to automatically adjust its blood flow to match its metabolic demands
a. Physical changes warming promotes vasodilation, cooling causes vasoconstriction
b. Vasodilating and vasoconstricting chemicals
Vasodilating: K
+
, H
+
, lactate, ATP, NO, kinins, histamine
Vasoconstricting: thromboxane, A2, superoxide radicals, serotonin, endothelins
B. Hypertension
1. What is Hypertension?
persistent elevation of blood pressure after 3-4 occasions
elevated systemic arterial blood pressure
cardiovascular disease risk factor (not a disease)
Pharmacology Lecture Hypertension 2014
3
dealwithmaie6523
2. Types
a. Primary/Idiopathic/Essential htn
no identifiable cause
Theories:
i. Age
body systems efficiency
elasticity of BV is lost
NP = release as you age because there are no peptides that control
ii. RAAS
aldosterone is an end product therefore reabsorption of sodium ions
eg. Black Race cant efficiently handle sodium ions; ACE inibitors is not used in the management of htn
iii. Na
Normal: [135-145 mEq/L] [135-145 mmol/L]
excess NP = urine is salty
iv. ANS/SANS
Stresses? release of catecholamines which act on CVS causing hypertension
v. Ca
2+
Calcium ions plus contractile CHONs (actin and myosin) leads to vasoconstriction thereby increasing PVR and thus,
increase in BP
b. Non-essential/Secondary htn
i. Renal/glomerular dse
ii. DM
iii. Cushings Syndrome/pheochromocytoma
iv. Excessive ROH intake
v. Heart dse
vi. Coarctation of the aorta
vii. Drugs NSAIDS, SANS, Adrenergic Drugs
c. White coat htn anxiety induced when BP is taken by a HCP
d. Pregnancy-induced htn because of BP; hormonal; 2 circulations
e. Isolated systolic htn SBP >140 with DBP <90
occurs in elderly
3. Risk Factors
a. Age
b. Obesity
c. Sedentary lifestyle no exercise
d. Smoking
e. Excessive ROH intake
f. Diet - cholesterol/fatty foods, Na, Ca
g. Stress
h. Drugs = NSAIDS, steroids
i. Family history
j. Co-morbid dse chronic dse such as kidney, heart,
DM
k. Black race / ethnicity
4. Management
a. Interview F Hx, s/s (asymptomatic)
s/s
o nape pain
o chest pain
o dizziness
o palpitations
o fatigue
o HA
o epistaxis
o fainting
o shortness of breath
o tinnitus
b. Get BP
3 separate occasions (3-4 mos interval)
BP remains elevated
Pharmacology Lecture Hypertension 2014
4
dealwithmaie6523
c. Lab Tests identify the organs involved in htn
Eg. Blood glucose DM
Blood lipids cholesterol/triglycerides
Urinalysis kidneys, BUN
ECG heart is normal or enlarged
CXR - lungs
5. Treatment
Principle involved in treating hypertension
a. Individualization dependent on the individual characteristics (age, gender, race, height and weight, co-morbid factors)
b. Stepped Care Approach/Laddered Approach
a. Non-PCOL modify their lifestyle
i. DASH diet
fruits, vegetables, wheat, whole grains, low-fat dairy foods
K balance the amount of sodium in cells
Na in diet 1,500 mg a day for hypertensive patients (2,300 mg for healthy individuals); retain fluid
ii. Limit alcohol intake moderateROH can raise BP even in healthy individuals
iii. Maintain a healthy weight more weight means more blood needed to supply oxygen and nutrients to your tissues thus, BV
increases and so does pressure
iv. Regular exercise brisk walking; 30 mintues of physical activity a day
Not active? Tend to have higher heart rates; the higher HF, the harder the heart must work with each contraction and the
stronger the force on the arteries. Also increase the risk of being overweighed
v. Stop smoking injures blood vessel walls causing it to narrow; speeds up the process of hardening of the arteries
vi. Manage stress muscle relaxation, deep breathing, plenty of sleep
b. PCOL
i. Alpha-adrenergic blockers
ii. ACE inhibitors
iii. Beta-Blockers
iv. Calcium Channel Blockers
v. Diuretics
vi. Sympatholytics
vii. Vasodilators
Pharmacology Lecture Hypertension 2014
5
dealwithmaie6523
C. Drugs for Hypertension
1. Diuretics
MOA ADR Agents Brand Name
Thiazide/Thiazide-like Diuretics
Promotes excretion of Na
+
Prevents Na
+
reabsorption
Decrease in BV
Decrease in CO
Decrease in BP
hypokalemia
hyponatremia
hyperuricemia
orthostatic hypotension
hypercalcemia
hyperglycemia
hyperlipidemia
Bendroflumethiazide
HCTZ / CTZ
Chlorthalidone
Indapamide
Metolazone
Naturetin
Hytaz
Diuzid
Urilzid
ThalitoneTenoretic
(+Atenolol)
Natrilix
Zaroxolyn
Loop Diuretics ototoxicity
hyperuricemia
acute hypovolemia
hypokalemia
hypomagnesemia
Furosemide
Torsemide
Bumetanide
Ethacrynic acid
Metazolide
Lasix
Fretic
Frusema
Demadex
Bumex
BurinexFontego
Edecrin
Potassium-sparing Diuretics gastric upset
gynecomastia
menstrual irregularities
hyperkalemia
nausea
lethargy
mental confusion
Spirinolactone
Eplerenone
Aldactone
Inspra
2. Sympatholytics
aka anti-adrenergics (targets the SANS)
MOA ADR Agents Brand Name
-Blockers
Types:
a. Cardioselective
b. Non-cardioselective
Blocks / receptors
preventing the reaction of
catecholamines
CO by (-)inotropy,
chronotropy, dromotropy,
bathmotropy
BP
renin = angiotensinogen
to aldosterone
hypotension
bradycardia
arrhythmia
bronchospasm
dyspnea
sedation
HDL
fatigue
insomnia
sexual dysfunction
Acebutolol
Atenolol
Carvedilol
Labetalol
Metoprolol
Nadolol
Propranolol
Timolol
Sectral
Tenormin
Coreg
Carvid
Normodyne
Trandate
Neobloc
Corgard
Inderal
Hemangeol
InnoPran
Blocadren
-Blockers
DI: Sit for 10-15 min before
getting up to avoid postural
hypotension
Best given at HS
Inhibit/block asdrenergic
receptors at vascular
tissues (blood vessels)
causing vasodilation
PVR
BP
orthostatic hypotension
edema
bradycardia
lightheadedness
syncope
HA
reflex tachycardia
salt and water retention
Prazosin
Terazosin
Doxazosin
Phentolamine
Phenoxybenzamine
Minipress
Hytrin
Cardura
OraVerse
Regitine
Dibenzyline
Centrally-acting
agonists
Blocks sympathetic
outflow in the brain stem
to cause vasodilation
PVR
BP
sedation
drowsiness
hemolytic anemia
bradycardia
constipation
dry mouth
edema
Clonidine with renal dse
Methyldopa PIH
Guanfacine
Guanabenz
Catapres
Kapvay
Jenloga
Aldomet
Aldoclor
Medopa
Intuniv
Tenex
Estulic
Wytensin
Adrenergic Neuron Depletes norepinephrine depression (CI to Px with Reserpine
Pharmacology Lecture Hypertension 2014
6
dealwithmaie6523
Blocker from circulation
depression)
sexual dysfunction
(libido)
orthostatic hypotension
angina
bradycardia
3. Agents that suppress RAAS
MOA ADR Agents Brand Name
ACE Inhibitors
prils
Inhibits conversion of
Angiotensin I to Angiotensin
II to Aldosterone
hyperkalemia
dry cough
angioedema
proteinuria
dysgeusia
ACE: rash, fever
ARB: diarrhea
Benazepril
Captopril
Enalapril
Fosinopril
Lisinopril
Moexipril
Quinalapril
Ramipril
Trandolapril
Lotensin
Capoten
Vasotec
Epaned
Monopril
Zestril
Prinivil
Univasc
Accupril
Altace
Mavik
ARBs
sartans
Inhibits release of renin so
no conversion of
angiotensinogen into
aldosterone
Candesartan
Eprosartan
Irbesartan
Losartan
Olmesartan
Telmisartan
Valsartan
Blopress
Atacand
Candez
Teveten
Aprovel
Avapro
Cozaar
Losart
Benicar
Micardis
Diovan
4. Calcium Channel Blockers
usually non-selective since it affects all muscles
MOA ADR Agents Brand Name
Dihydropyridines
Inhibits entry of Ca
2+
Inhibit rxn with contractile
CHONs into myocardial and
vascular cells to promote
vasodilation
Also cause relaxation of
other cells skeletal and
smooth muscles
Constipation
Weakness
Periopheral edema
Reflex tachycardia
(-)inotropy can lead to HF
Amlodipine
Felodipine
Isradipine
Nicardipine
Nifedipine
Nimodipine
Nisoldipine
Norvasc
Amvasc
Plendil
Dynacirc
Cardene
Adalat
Procardia
Nifediac
Nimodin
Nymalize
Sular
Non-dihydropyridines
Diphenylalkylamine
Verapamil
Benzothiazepines
Diltiazem
Diltiazem
Verapamil
Dilzem
Cardizem
Dilacor
Isoptin
Covera-HS
Calan
Pharmacology Lecture Hypertension 2014
7
dealwithmaie6523
5. Vasodilators
MOA: acts directly on blood vessels (arteries and veins) to PVR leading to BP
Brand Name Notes Specific ADR General ADR
Hydralazine Apresoline
Drug that undergoes
acetylation polymorphism
which is a part of Phase II
metabolism
Rapid/slow acetylators
Drug-induced SLE
Type II allergic reactions
postural hypotension
epinephrine reversal
reflex tachycardia
palpitation
HA
arrhythmia
peripheral neuropathy
edema
Minoxidil Loniten
Hyoertrichosis
Hirsutism
Diazoxide Proglycem
Hyperstat
Inhibits insulin release from
the pancreas
Hyperglycemia
Fenoldapam Corlopam
Targets the dopamine
receptors
Dilation of peripheral
arteries
Natriuresis
Na Nitroprusside Nitropress
Nitroprusside = enzyme
rhodanase, liver metabolize
to inactive substance
Rhodanase ]= metabolize
to toxic subs
*Thiocyanate has the
tendency to accumulate in
the blood causing
methemoglobinemia
(0xidize)
Reducing agent:
Methylene blue urine blue
CN toxicity
Antidote: Na2S2O3
You might also like
- Hypertension: Margaret Xaira R. Mercado RNDocument36 pagesHypertension: Margaret Xaira R. Mercado RNMargaret Xaira Rubio MercadoNo ratings yet
- Hypertension: Rojina Bhurtel Lecturer MmihsDocument36 pagesHypertension: Rojina Bhurtel Lecturer MmihsRojina Bhurtel100% (2)
- Chapter 33 HypertensionDocument5 pagesChapter 33 HypertensiongytmbiuiNo ratings yet
- 5 Nutrition Therapy For Cardiovascular DiseasesDocument74 pages5 Nutrition Therapy For Cardiovascular Diseaseskarinablanca adranedaNo ratings yet
- Nursing Pharmacology Perfusion Study GuideDocument9 pagesNursing Pharmacology Perfusion Study GuideChelsea SmithNo ratings yet
- Hypertension: Prepared By: Eden Marie D. Francisco Lorraine Nicolne B. CortejoDocument27 pagesHypertension: Prepared By: Eden Marie D. Francisco Lorraine Nicolne B. CortejoAlecNo ratings yet
- Hypertension Definition:: Nitric OxideDocument5 pagesHypertension Definition:: Nitric OxideAnonymous bbeAZHxZNo ratings yet
- Drugs Acting in CVSDocument63 pagesDrugs Acting in CVSMeghan Norico Cristuta100% (1)
- PathophysiologyDocument24 pagesPathophysiologyVikash KushwahaNo ratings yet
- 11A Drugs Acting On The Cardiovascular SystemDocument85 pages11A Drugs Acting On The Cardiovascular SystemJaps De la CruzNo ratings yet
- CHF Preparation QuestionsDocument6 pagesCHF Preparation Questionsgenium0689% (9)
- CVS, 2021Document16 pagesCVS, 2021g.4ssilaNo ratings yet
- Anatomy NotesDocument86 pagesAnatomy NoteskNo ratings yet
- Antihypertensive Drugs Lecture-1Document94 pagesAntihypertensive Drugs Lecture-1onyeukwudaniel12No ratings yet
- Cardiac FailureDocument63 pagesCardiac FailureNina OaipNo ratings yet
- HTN-Chapter 32: Systemic Vascular Resistance-Force Opposing The Movement of Blood Within The Blood VesselsDocument5 pagesHTN-Chapter 32: Systemic Vascular Resistance-Force Opposing The Movement of Blood Within The Blood Vesselssylviawaller100% (2)
- Hypertension: Hypertension Is One of The Most Common Worldwide Diseases Afflicting Humans. BecauseDocument8 pagesHypertension: Hypertension Is One of The Most Common Worldwide Diseases Afflicting Humans. BecauseKramojNo ratings yet
- HTA Eng NouaDocument56 pagesHTA Eng NouaAnna HaritonencoNo ratings yet
- MIDTERM-PCOL 1-MODULE 1-2&3-Topic 1Document29 pagesMIDTERM-PCOL 1-MODULE 1-2&3-Topic 1ZEITAIMENo ratings yet
- Hyper TentionDocument19 pagesHyper TentionAnthony MarkNo ratings yet
- Hypertension: Medical Management and Nutritional ApproachesDocument65 pagesHypertension: Medical Management and Nutritional ApproachesWelki VernandoNo ratings yet
- HYPERTENSIONDocument10 pagesHYPERTENSIONChelsea Faith SarandiNo ratings yet
- Shock and SIRSDocument85 pagesShock and SIRSBryan Mae H. DegorioNo ratings yet
- Anatomy & Physiologyc: Y CC CC CC C C CCC CCCCC C CDocument4 pagesAnatomy & Physiologyc: Y CC CC CC C C CCC CCCCC C CroothanngNo ratings yet
- CardioDocument9 pagesCardioVirgilio Reyes ManuelNo ratings yet
- Congestive Cardiac FailureDocument24 pagesCongestive Cardiac FailureFarheen KhanNo ratings yet
- Blood PressureDocument15 pagesBlood PressureKiran DeviNo ratings yet
- Unit IV. Drugs For CHFDocument26 pagesUnit IV. Drugs For CHFChinenye AkwueNo ratings yet
- Assessment Cardiac SystemDocument51 pagesAssessment Cardiac Systemejarnmd100% (2)
- Hipertensi 3-6-14Document37 pagesHipertensi 3-6-14tbhuhoriNo ratings yet
- Hypertension - CH 33 (Lewis)Document4 pagesHypertension - CH 33 (Lewis)Marisol AaronsNo ratings yet
- 6 HypertensionDocument95 pages6 HypertensionZeleke temechewNo ratings yet
- Cardiovascular DrugsDocument11 pagesCardiovascular DrugsKhyra Ysabelle VillanuevaNo ratings yet
- Nursing Management OF A Patient With HypertensionDocument39 pagesNursing Management OF A Patient With HypertensionJEEJANo ratings yet
- Congestive Heart FailureDocument14 pagesCongestive Heart Failurelolo0880No ratings yet
- Hypertension 1Document44 pagesHypertension 1intanNo ratings yet
- Lec 6 Anti-Hypertensive DrugsDocument31 pagesLec 6 Anti-Hypertensive Drugsph211333No ratings yet
- Cardiology HFDocument11 pagesCardiology HFdhayemaruNo ratings yet
- 12-Blood Vessels PathologyDocument37 pages12-Blood Vessels PathologyRodriguez Vivanco Kevin DanielNo ratings yet
- Allan Lester VDocument6 pagesAllan Lester VA'Lester MedinaNo ratings yet
- Clinical PharmacyDocument8 pagesClinical PharmacyMissy NaguitNo ratings yet
- CA ReviewerDocument16 pagesCA ReviewerJheanAlphonsineT.MeansNo ratings yet
- ShockDocument33 pagesShockVijith.V.kumarNo ratings yet
- Hypertension Group 9Document19 pagesHypertension Group 9Putri AuliaNo ratings yet
- Chapter 31 HypertensionDocument3 pagesChapter 31 HypertensionVen SemillaNo ratings yet
- Cardiac Failure: Definition: Compensatory Changes in Heart FailureDocument5 pagesCardiac Failure: Definition: Compensatory Changes in Heart FailureMatyie SmkasNo ratings yet
- Cardiovascular PhysiologyDocument6 pagesCardiovascular PhysiologyatefmaboodNo ratings yet
- HypertensionDocument11 pagesHypertensionJyoti singhNo ratings yet
- Past Years SNQ Answer by RCSIDocument47 pagesPast Years SNQ Answer by RCSIhelamahjoubmounirdmo100% (1)
- Arterial Blood Pressure RegulationDocument21 pagesArterial Blood Pressure Regulationnaresh sharmaNo ratings yet
- Week 2 Blpressoureoduph - 20 Februari 2012week 2 Blpressoureoduph - 20 Februari 2012Document43 pagesWeek 2 Blpressoureoduph - 20 Februari 2012week 2 Blpressoureoduph - 20 Februari 2012Maria Dini AdmiratiNo ratings yet
- داتا حيداشر محاضرة فسيولوجىDocument6 pagesداتا حيداشر محاضرة فسيولوجىMohaned MokhtarNo ratings yet
- Case Study HypertensionDocument7 pagesCase Study Hypertensionsanthyakunjumon67% (3)
- HypertensionDocument1 pageHypertensionAllyne GavinoNo ratings yet
- Ch35 CardiovascularDocument11 pagesCh35 CardiovascularJessie Jennings100% (3)
- Classification: HypertensionDocument13 pagesClassification: HypertensiontermskipopNo ratings yet
- Hypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Document81 pagesHypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Alan K MhamadNo ratings yet
- Congestive Heart FailureDocument39 pagesCongestive Heart FailureEthiopia TekdemNo ratings yet
- Chapter 24 OrgMedDocument1 pageChapter 24 OrgMedMaielyne Keith B. DalilisNo ratings yet
- Adrenergic AgonistDocument3 pagesAdrenergic AgonistMaielyne Keith B. DalilisNo ratings yet
- Adrenergic AgonistDocument3 pagesAdrenergic AgonistMaielyne Keith B. DalilisNo ratings yet
- ManufLec 1Document3 pagesManufLec 1Maielyne Keith B. DalilisNo ratings yet
- Emergency RadiologyDocument79 pagesEmergency RadiologyRahul Yadav100% (3)
- Somalia Launches First Ever-Cleft Lip and Palate Surgery ClinicDocument4 pagesSomalia Launches First Ever-Cleft Lip and Palate Surgery ClinicAMISOM Public Information ServicesNo ratings yet
- Antepartum Fetal Surveillance ACOG Bulletin 2014 PDFDocument11 pagesAntepartum Fetal Surveillance ACOG Bulletin 2014 PDFDanNo ratings yet
- Medel SonataDocument54 pagesMedel Sonatamaclab macNo ratings yet
- Caring For Older AdultsDocument5 pagesCaring For Older AdultsOsama Elsayed AhmedNo ratings yet
- Energy Drink AssignmentDocument4 pagesEnergy Drink AssignmentSukh Prabhleen DhaliwalNo ratings yet
- SIADH, DI and Cerebral Salt Wasting: Karim Rafaat, MDDocument54 pagesSIADH, DI and Cerebral Salt Wasting: Karim Rafaat, MDMahendra PrasetyoNo ratings yet
- Hyper Parathyroid IsmDocument7 pagesHyper Parathyroid IsmEllene Mae Dejapa VillasisNo ratings yet
- Patient and Family Discharge Checklist: Patient Name: Reason For AdmissionDocument7 pagesPatient and Family Discharge Checklist: Patient Name: Reason For Admissiondwirabiatul adwiyahaliNo ratings yet
- USFDA Guidance For Industry - PSUR - What To ReportDocument7 pagesUSFDA Guidance For Industry - PSUR - What To ReportErshad Shafi AhmedNo ratings yet
- Drug and Therapeutics Committee: Session 4. Assessing and Managing Medicine SafetyDocument40 pagesDrug and Therapeutics Committee: Session 4. Assessing and Managing Medicine SafetyPratyNo ratings yet
- Koo Quay Keong V Ooi Peng Jin London Lucien (2016) 5 SLR 0130Document16 pagesKoo Quay Keong V Ooi Peng Jin London Lucien (2016) 5 SLR 0130a b cNo ratings yet
- Operation by Marc Nair EssayDocument3 pagesOperation by Marc Nair EssayVasuda MukundanNo ratings yet
- Yesterday's Tomorrow - Suvika PDFDocument223 pagesYesterday's Tomorrow - Suvika PDFSindhu Jhaveri100% (2)
- Anatomy and Physiology of PlacentaDocument5 pagesAnatomy and Physiology of PlacentaAdrianne Basa100% (1)
- Diagnosis of Adjustment Disorder Reliability of Its Clinical Use and Long-Term StabilityDocument6 pagesDiagnosis of Adjustment Disorder Reliability of Its Clinical Use and Long-Term StabilitydmsdsNo ratings yet
- Oxygen Therapies: Interview With Ed MccabeDocument5 pagesOxygen Therapies: Interview With Ed MccabeOrlando Gunther100% (1)
- SJT Med SchoolDocument101 pagesSJT Med SchoolErine Novita BasukiNo ratings yet
- The Health Insurance SpecialistDocument8 pagesThe Health Insurance SpecialistsaranyaNo ratings yet
- Chest MobilityDocument25 pagesChest Mobilitywahyuni pelita sariNo ratings yet
- Physical and DiagnosticDocument20 pagesPhysical and DiagnosticHaziq MarsNo ratings yet
- Stephanie Resume Updated 3-4-19Document1 pageStephanie Resume Updated 3-4-19StephNo ratings yet
- Anticoagulants 2019Document11 pagesAnticoagulants 2019Srijan VermaNo ratings yet
- Anatomy of The Human Airways. Lymph Node Stations and InterventionalDocument6 pagesAnatomy of The Human Airways. Lymph Node Stations and Interventionalandika pradanaNo ratings yet
- Anatomy of The KidneyDocument7 pagesAnatomy of The KidneyArgie Arguson IINo ratings yet
- Physostigmine Antidote FactsDocument1 pagePhysostigmine Antidote FactsLidwina Liniati GeografiNo ratings yet
- Moses Cone Hospital MapDocument2 pagesMoses Cone Hospital MapWfmy TegnaNo ratings yet
- Suggamadex Remifentanyl PalonosetronDocument28 pagesSuggamadex Remifentanyl PalonosetronSai TejeswiNo ratings yet
- Nursing DiagnosisDocument86 pagesNursing DiagnosisMarianne Gonzales100% (5)
- Guidelines For Prescribing EyeglassesDocument18 pagesGuidelines For Prescribing Eyeglassesratujelita100% (1)