Professional Documents
Culture Documents
Anatomy & Physiology - Wk2 Assignment
Uploaded by
Abhishek SuranaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anatomy & Physiology - Wk2 Assignment
Uploaded by
Abhishek SuranaCopyright:
Available Formats
Running head: BLOOD 1
Blood
Name:
Course:
Institution:
Instructor:
Date:
BLOOD 2
Which of the formed elements would increase after the donation of a pint of blood and why?
Reticulocytes are released into the blood after donation. (Martini, F. & Nath, J. 2009).
When one loses a large amount of blood, reticulocytes are quickly produced to enable bodies
quickly replenish the blood supplies. (Martini, F. & Nath, J. 2009).
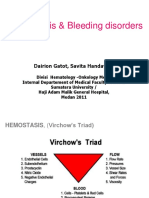
Describe the three phases of the normal blood-clotting process.
Vascular phase: Soon after blood vessels are injured, prothrombotic activities are initiated as a
result of exposure of collagen, subendothelial tissues and basement membrane. The clotting
activities in this phase include platelet adhesion and aggregation through release of von
Willebrand factor (vWF) and adenosine diphosphate (ADP) (Gerard J Tortora; Sandra Reynolds
Grabowski; 2003). At this juncture, the initial layer of platelet plug is developed at the injury
site.
Platelet phase: Platelets play a role in blood clotting process which includes: maintaining the
health of inner lining of vascular wall; forming platelet plug when there is vessel wall injury;
initiating coagulation phase. In the platelet phase, the platelets stick and adhere to the damaged
surface, change shape, and aggregate forming a hemostatic platelet plug in the injured vessel site
(Gerard J Tortora; Sandra Reynolds Grabowski; 2003). This results to primary cessation of the
particular bleed by hemostatic plug formation.
Coagulation phase: This phase begins with initiation of plasma proteins produced by the liver.
These coagulation factors are gradually activated within their respective pathways. The extrinsic
pathway is activated by a plasma protein factor VII when its exposed to tissue factor within the
BLOOD 3
injured blood vessel while the intrinsic pathway is activated when plasma protein factor XII
contacts with the injury-exposed tissues (Gerard J Tortora; Sandra Reynolds Grabowski; 2003).
The pathways then merge and a factor X is initiated, yielding the initiation of a common
pathway. This results to conversion of prothrombin to thrombin which acts as a catalyst for
conversion of fibrinogen, which is a precursor to fibrin (Gerard J Tortora; Sandra Reynolds
Grabowski; 2003). The fibrin is then converted to an insoluble and stringy protein which forms
minute delicate structures referred to as fibrils. This results to plasma and blood cells being
enmeshed in the fibrils network to form a clot (Gerard J Tortora; Sandra Reynolds Grabowski;
2003). The fibrils are therefore responsible for the tightly binding and stabilizing the platelet
plug, as well as affixing it to the injury site. This definitive clot therefore prevents excessive
bleeding from the injury site.
Describe ABO and Rh blood groups
ABO The ABO is the basic system of classifying blood types. It divides blood into 4 types
namely A, B, AB and O. There are two definite antigens found on the surface of ones red blood
cells. A persons blood contains an inherited as well as a specific set of distinct antigens (Gerard
J Tortora; Sandra Reynolds Grabowski; 2003). In this classification system, one of the antigens
is named A while the other is B. If the red blood cells have only A antigen, then that blood
is type A. If the red blood cells have B antigen, then the blood is type B. If the red blood
cells have both A and B antigen, then the blood is type AB. If the red blood cells have neither
antigen, then the blood is type O.
BLOOD 4
Rhesus system The Rh system is the second main blood grouping system. The Rh factor is a
form of inherited blood antigen or protein on the red blood cells (Cecelia Gatson Grindel;
Leonard V Crowley; Charlotte A Johnston; 1997). Those with it are Rh positive while those
without are Rh negative. Rh positive is more common with about 85% people being Rh
positive. From the Rh system, there are around 35 different possibilities which can be inherited
from each parent, which are grouped into positive or negative types.
For example, when ones blood is AB+, this means that they have a type AB blood and are Rh
positive. If one has O- blood, then it means they have blood O type and are RH negative. This
shows that there is a connection between Rh factor and ABO blood type.
Explain the antigen-antibody response as it relates to blood groups.
Antigens are surface proteins that are found in all cells. Antigen-antibody response is
activated if a person receives transfusion of blood that contains antigens which it identifies as
being foreign (Martini, F. & Nath, J. 2009). The antibodies found in an individuals blood
usually bind the foreign antigen, causing clumping. The complexes of antigen-antibody clogs
small blood vessels while the foreign red blood cells are lysed, thereby releasing hemoglobin
into the bloodstream.
BLOOD 5
References
Martini, F. & Nath, J. (2009). Fundamentals of Anatomy and Physiology New York: Wiley.
Gerard J Tortora; Sandra Reynolds Grabowski; (2003) Principles of Anatomy and Physiology
New York: Wiley.
Cecelia Gatson Grindel; Leonard V Crowley; Charlotte A Johnston; (1997) Anatomy and
Physiology Springhouse, Pa: Springhouse Corp.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 326 Project 1 Spring15 Workbook. - DonexlsxDocument41 pages326 Project 1 Spring15 Workbook. - DonexlsxAbhishek SuranaNo ratings yet
- ACL TOP 50seriesDocument8 pagesACL TOP 50seriesRizky Fajar Maa'dinaNo ratings yet
- DataSheet CoaLAB 1000 EN 11-2017 PDFDocument4 pagesDataSheet CoaLAB 1000 EN 11-2017 PDFAgnesNo ratings yet
- Drugs Used For Blood Coagulation Disorders - KatzungDocument3 pagesDrugs Used For Blood Coagulation Disorders - Katzungsarguss14100% (6)
- Robbins Pathology - Chapter 4 TransDocument9 pagesRobbins Pathology - Chapter 4 Transnath nath100% (1)
- Precise Data Business Plan PDFDocument12 pagesPrecise Data Business Plan PDFAbhishek SuranaNo ratings yet
- MaytagDocument2 pagesMaytagAbhishek SuranaNo ratings yet
- FIN 341 - Exercise#6 - PAYBACKDocument3 pagesFIN 341 - Exercise#6 - PAYBACKAbhishek SuranaNo ratings yet
- Week 3 - Discussion 2Document2 pagesWeek 3 - Discussion 2Abhishek SuranaNo ratings yet
- Sheet1: Workings 2013 2012 Liquidity RatiosDocument1 pageSheet1: Workings 2013 2012 Liquidity RatiosAbhishek SuranaNo ratings yet
- Business PlanDocument13 pagesBusiness PlanAbhishek SuranaNo ratings yet
- FIN 341 - Quiz#6 - Based On - Exercise#6: Due Date - 3-03-15 - Tuesday-MidnightDocument5 pagesFIN 341 - Quiz#6 - Based On - Exercise#6: Due Date - 3-03-15 - Tuesday-MidnightAbhishek SuranaNo ratings yet
- Comparisonnetwork-Based Approach and A Gantt ChartDocument4 pagesComparisonnetwork-Based Approach and A Gantt ChartAbhishek SuranaNo ratings yet
- FIN 341 - Quiz#3 - Based On Exercise#3 Due Date - To Be DeterminedDocument6 pagesFIN 341 - Quiz#3 - Based On Exercise#3 Due Date - To Be DeterminedAbhishek SuranaNo ratings yet
- Fin 341 Quiz#5 Basedonexercise#5Document5 pagesFin 341 Quiz#5 Basedonexercise#5Abhishek SuranaNo ratings yet
- $13,511.28 Highest Present Value Financial Theory Supports Choosing Option CDocument5 pages$13,511.28 Highest Present Value Financial Theory Supports Choosing Option CAbhishek SuranaNo ratings yet
- DSF Report 24022015 VapDocument9 pagesDSF Report 24022015 VapAbhishek SuranaNo ratings yet
- $13,511.28 Highest Present Value Financial Theory Supports Choosing Option CDocument5 pages$13,511.28 Highest Present Value Financial Theory Supports Choosing Option CAbhishek SuranaNo ratings yet
- Anatomy & Physiology WK 9 - Proff ResponseDocument2 pagesAnatomy & Physiology WK 9 - Proff ResponseAbhishek SuranaNo ratings yet
- Ethics AssignmentDocument1 pageEthics AssignmentAbhishek SuranaNo ratings yet
- Health WK 4 - Wilson ResponseDocument2 pagesHealth WK 4 - Wilson ResponseAbhishek SuranaNo ratings yet
- Finance DiscussionsDocument4 pagesFinance DiscussionsAbhishek SuranaNo ratings yet
- Annual Report Project (ARP)Document17 pagesAnnual Report Project (ARP)Abhishek SuranaNo ratings yet
- Problem Set 2 CompletedDocument2 pagesProblem Set 2 CompletedAbhishek Surana33% (3)
- Finance DiscussionsDocument4 pagesFinance DiscussionsAbhishek SuranaNo ratings yet
- Exercise 9 SolutionDocument13 pagesExercise 9 Solutionsl00redNo ratings yet
- Business MemoDocument1 pageBusiness MemoAbhishek SuranaNo ratings yet
- Math 135Document2 pagesMath 135Abhishek SuranaNo ratings yet
- Anatomy & Physiology Wk3-Baker ResponseDocument2 pagesAnatomy & Physiology Wk3-Baker ResponseAbhishek SuranaNo ratings yet
- Anatomy and Physiology WK 2-DQ-Challenging QuestionDocument1 pageAnatomy and Physiology WK 2-DQ-Challenging QuestionAbhishek SuranaNo ratings yet
- AdlyDocument1 pageAdlyAbhishek SuranaNo ratings yet
- CH 5 - 6 ProblemsDocument4 pagesCH 5 - 6 ProblemsAbhishek SuranaNo ratings yet
- Anatomy and Physiology WK 2-DQ-Challenging QuestionDocument1 pageAnatomy and Physiology WK 2-DQ-Challenging QuestionAbhishek SuranaNo ratings yet
- Basic Principles of HemostasisDocument5 pagesBasic Principles of HemostasisSean Matthew100% (1)
- ORBCON-EN-BE Coagulation 02259Document24 pagesORBCON-EN-BE Coagulation 02259Леон Деспотоски100% (1)
- Bleeding Case SampleDocument7 pagesBleeding Case SampleNikko CabrestanteNo ratings yet
- Hemophilia: Factor IX (Hemophilia B)Document38 pagesHemophilia: Factor IX (Hemophilia B)Jhvhjgj JhhgtyNo ratings yet
- Schramm 2014Document6 pagesSchramm 2014Sexy BooksNo ratings yet
- 33-Hemostasis and Coagulation ProfileDocument40 pages33-Hemostasis and Coagulation ProfileOsman Mohamed MuhumedNo ratings yet
- MT Activity 1Document18 pagesMT Activity 1Luigie TorresNo ratings yet
- 4.1 Antibodi TrombositDocument36 pages4.1 Antibodi Trombositrani fatinNo ratings yet
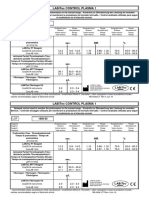
- LABiTec Control 1 Insert 1956 35 Revision 2.0Document1 pageLABiTec Control 1 Insert 1956 35 Revision 2.0Carla YcoNo ratings yet
- Coagulation Tests and FibrinolysisDocument7 pagesCoagulation Tests and FibrinolysisgraceyNo ratings yet
- 3 4Document2 pages3 4cherryNo ratings yet
- Advanced Haemostasis Semi-Automated Systems: Cat No Product / Analyte Package Name Package SizeDocument2 pagesAdvanced Haemostasis Semi-Automated Systems: Cat No Product / Analyte Package Name Package SizeSmithesh TpNo ratings yet
- Hema 2 - Prelim Topic 3 - Platelet Disorders and Laboratory TestsDocument8 pagesHema 2 - Prelim Topic 3 - Platelet Disorders and Laboratory TestsLowenstein JenzenNo ratings yet
- Morrissey 2004Document6 pagesMorrissey 2004Marija NikolicNo ratings yet
- Laboratory Evaluation of PlateletsDocument28 pagesLaboratory Evaluation of PlateletsTom Anthony TonguiaNo ratings yet
- Secondary Hemostasis Activity BACHARODocument3 pagesSecondary Hemostasis Activity BACHAROGilliana KathrynNo ratings yet
- Basic Concepts Of: HemophiliaDocument2 pagesBasic Concepts Of: Hemophiliaapi-265604636No ratings yet
- HemostasisDocument48 pagesHemostasisBintang Ruth Cecilia FebrinaNo ratings yet
- Anticoagulant Activities of Curcumin and Its DerivativeDocument6 pagesAnticoagulant Activities of Curcumin and Its DerivativeAlfred YangaoNo ratings yet
- Haemophilia AssignmentDocument2 pagesHaemophilia AssignmentKhadija JaraNo ratings yet
- Bleeding and Clotting - PPT 2Document13 pagesBleeding and Clotting - PPT 2kholoud22067% (3)
- Clotting Factor Table 0814Document1 pageClotting Factor Table 0814Sundar100% (1)
- Automated Blood Coagulation Analyzer CA-500: Basic Data Sheet - (Fibrinogen)Document9 pagesAutomated Blood Coagulation Analyzer CA-500: Basic Data Sheet - (Fibrinogen)Aahsan Iqbal احسن اقبالNo ratings yet
- Hemophilia and Its Treatment: Brief ReviewDocument7 pagesHemophilia and Its Treatment: Brief ReviewSalsa BillaNo ratings yet
- Secondary Clotting DisordersDocument34 pagesSecondary Clotting DisordersLyra Dennise LlidoNo ratings yet
- Haemostasis: CatalogueDocument24 pagesHaemostasis: CatalogueGabriela Alegre UgartemendíaNo ratings yet