Professional Documents
Culture Documents
11 - Novel Decision Tree Algorithms For The Treatment Planning of Compromised Teeth
Uploaded by
kochikaghochi0 ratings0% found this document useful (0 votes)
417 views10 pagessdf
Original Title
11 . Novel Decision Tree Algorithms for the Treatment Planning of Compromised Teeth
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentsdf
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
417 views10 pages11 - Novel Decision Tree Algorithms For The Treatment Planning of Compromised Teeth
Uploaded by
kochikaghochisdf
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 10
VOLUME 44 NUMBEP 1 JANUAPY 2013 75
QUI NTESSENCE I NTERNATI ONAL
GENERAL DENTISTRY
an attempt to guide clinicians in their treat-
ment planning, these systems are not very
helpful in the decision-making process of
whether to extract or retain the tooth: It has
been shown that unless the tooth has a
good prognosis, it is hard to accurately pre-
dict its long-term survival.
24
Specically,
only 35% of prognostication accuracy was
reported after 8 years of maintenance in
teeth that were not given a good progno-
sisafter retrospective evaluation, the
accuracy of the prognosis was very low in
regard to outcomes.
5
Moreover, some retro-
spective studies reported that more than
90% of teeth that had questionable progno-
ses were retained at maintenance if a strict
maintenance protocol was followed.
5,6
Booauso o tnoso oontradiotions, tno
authors propose that a different (algorith-
mic) approach is needed to provide more
accurate treatment planning for teeth with
less than a good prognosis. In an algorith-
mic approach to treatment planning, to pro-
vide easier and clearer manipulation of all
available data, quantitative representation of
knowledge should be analyzed and all avail-
able data compared to sharpen the bound-
aries between different treatment plans.
7
Treatment planning in respect to tooth
retention or extraction has historically been
the most challenging and thought-provok-
ing decision in oral rehabilitation. In most
cases, decisions are derived from the prog-
nosis of the compromised teeth and their
impact on the health of the overall dentition;
they are relative rather than absolute ver-
dicts.
1
Since tooth extraction is irreversible,
it is highly desirable to create an evidence-
based decision-making algorithm that will
minimize or eliminate error.
Although there are several prognostica-
tion systems that have been formulated in
1
Alumni, New Jersey Dental School, University of Medicine and
Dentistry, Newark, New Jersey, USA.
2
Adjunct Clinical Assistant Professor, Department of
Periodontics, New Jersey Dental School, University of Medicine
and Dentistry, Newark, New Jersey, USA.
3
Clinical Professor, Vice Chairman,Department of Periodontics,
New Jersey Dental School, University of Medicine and Dentistry,
Newark, New Jersey, USA.
All authors have contributed equally to this manuscript.
Correspondence: Dr Sofia D. Petrov, Department of
Periodontics, University of Medicine and Dentistry of New
Jersey, 110 Bergen St, Newark, NJ 07103. Email: drpetrovs@
gmail.com
Novel decision tree algorithms for the
treatment planning of compromised teeth
Amy Ovaydi-Mandel, DDS, MSD
1
/Sofa D. Petrov, DDS, MSD
2
/
Howard J. Drew, DMD
3
In clinical practice, dentists are faced with the dilemma of whether to treat, maintain, or
extract a tooth. Of primary importance are the patients desires and the restorability and
periodontal condition of the tooth/teeth in question. Too often, clinicians extract teeth when
endodontic therapy, crown-lengthening surgery, forced orthodontic eruption, or regenera-
tive therapy can be used with predictable results. In addition, many clinicians do not con-
sider the use of questionable teeth as provisional or transitional abutments. The aim of this
article is to present a novel decision tree approach that will address the clinical deductive
reasoning, based on the scientic literature and exemplied by selective case presenta-
tions, that may help clinicians make the right decision. Innovative decision tree algorithms
will be proposed that consider endodontic, restorative, and periodontal assessments to
improve and possibly eliminate erroneous decision making. Decision-based algorithms are
dynamic and must be continually updated in accordance with new evidence-based stud-
ies. (Quintessence Int 2013;44:7584)
Key words: decision trees, periodontal prognosis, questionable teeth, treatment
planning
76 VOLUME 44 NUMBEP 1 JANUAPY 2013
QUI NTESSENCE I NTERNATI ONAL
Pet rov et al
Pooontly, sovoral intorosting and tnor-
ough approaches were offered in various
forms: decision charts, tables, and survival
trees.
810
Although all can be used to sig-
nicantly help with the decision-making
process, none provide clinicians with the
systematic sequential approach algorithms
can. An algorithm is dened as a nite set
of unambiguous instructions performed in a
prescribed sequence to achieve a goal.
11
The purpose of this article is to propose
novel decision tree algorithms, supported
by scientic evidence, where more dened
and sequential instructions will be delineat-
ed to assist clinicians in determining wheth-
er to extract or save the tooth.
The article will use the McGuire prog-
nostication system with ve categories of
periodontal tooth prognosisgood, fair,
poor, questionable, and hopelessas the
critical points of algorithmic decision trees.
2
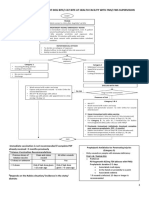
Endodontic and restorative assessment
algorithms (Fig 1) will also be presented
that will be utilized with the periodontal
decision tree algorithms and extraction
algorithm (Fig 2).
Booro disoussing tno algoritnms, it is
important to emphasize that there are other
important clinical parameters, such as
patient history, expectations, psychologic
needs, nances, and compliance. However,
those will vary from patient to patient, and
while they should be incorporated into the
nal decision-making process on a patient-
to-patient basis, they are not within the
scope of this paper. In the cases present-
ed, the authors make the ideal assumption
that there are no nancial restrictions or
medical contraindications to therapy.
ENDODONTIC
ASSESSMENT
Although the majority of the studies report
no difference in the long-term prognosis
between successfully restored and main-
tained root canaltreated teeth and single
tooth implants,
12,13
a signicant decrease in
the success rate, from 94% to 85.9%, was
reported for nonsurgically retreated teeth
when compared with nonsurgically (initially)
treated teeth. There was a statistically sig-
nicant better healing rate for patients ages
50 to 59 and a lower percentage of success
for molars (when compared with premolars
and anterior teeth) as well as for teeth with
preexisting periapical lesions.
14
The criteria
for successful root canal therapy used in
this article follow those established by the
European Society of Endodontology.
15
The
signicance of these factors can be illus-
trated by the endodontic decision tree algo-
rithms (Fig 1). Another major factor that was
considered in developing the endodontic
decision tree algorithms is periodontal bio-
type, which can be classied as thin and
scalloped or thick and at.
16
Since it has
been shown that a thin friable biotype is
more prone to postsurgical recession after
periodontal or implant surgery,
17,18
it has
been generally recommended to favor the
retention of a tooth with a thin biotype.
19,20
RESTORATIVE
ASSESSMENT
The crown-to-root ratio is an important clinical
parameter that has historically been used to
determine whether the tooth can be success-
fully restored and maintained. It is dened as
the radiographic distance of the portion of the
tooth not within the alveolar bone divided by
the radiographic portion of the tooth within
the bone.
21
Although no denitive recommen-
dations exist in regard to the optimal tooth
ratio, a minimal 1:1 ratio for a tooth abutment
has been suggested.
22
It should also be
noted that a recommendation for extraction
does not take into account a patients psy-
chologic opposition to losing a tooth.
PERIODONTAL
ASSESSMENT
Good periodontal prognosis
The authors will omit the discussion of teeth
with good periodontal prognoses because
only the endodontic (and restorative) algo-
rithms should be utilized in these cases
(see Fig 1).
VOLUME 44 NUMBEP 1 JANUAPY 2013 77
QUI NTESSENCE I NTERNATI ONAL
Pet rov et al
3
1
RESTORATIVE ALGORITHM
PERIODONTAL ALGORITHM
(Fair Periodontal Prognosis)
PERIODONTAL ALGORITHM
(Poor Periodontal Prognosis / Esthetic Zone)
PERIODONTAL ALGORITHM
(Poor Periodontal Prognosis / Non-Esthetic Zone)
NON-VITAL
TOOTH
NON-VITAL
TOOTH
No previous
treatment done
Previous
RCT/ Apicoectomy
Thin Biotype
in Esthetic
Zone
Thin/Thick Biotype
in Non-esthetic Zone
or Thick Biotype in
Esthetic Zone
RCT
Retreatment,
if possible
Extraction
(GBR) / Implant
Can not be restored
without
compromising
crown to root ratio
Can be restored
without
compromising crown
to root ratio
Extraction
(GBR) / Implant
FOE / Finishing
Periodontal
Procedures
Crown
Lengthening
Surgery
FRACTURED
TOOTH
Subgingival decay
Occlusional discrepancy
No previous
treatment done
RCT RCT
Previous
RCT / Apicoectomy
Extraction
(GBR) / Implant
FAIR
PROGNOSIS
Hamp I
25%CAL
Deep (>=4mm)
Intrabony
Defects
Shallow(>4mm)
Intrabony Defects
or Horizontal Bone
Loss
Regenerative
Surgery
(GTR, Emdogain, etc)
S/RP with/without
Local Chemotherapy,
Periodontal
Reparative Surgery
S/RP with/without
Local Chemotherapy,
Furcation Plasty
Interproximal Bone
Height Apical to
Furcation
Interproximal Bone
Height Coronal to
Furcation
Apically positioned
fap (AFP), tunelling,
root amputation,
hemisection,
bicuspidization
Intrabony
Defects
4
POOR
PROGNOSIS
Esthetic Zone
POOR
PROGNOSIS
Non-Esthetic Zone
Horizontal
Bone Loss
Extraction
(GBR) / Implant
Extraction
(GBR) / Implant
Extraction
(GBR) / Implant
Regenerative
Surgery
Regenerative
Surgery
Regenerative
Surgery
FOE if vertical
augmentation is needed
Extraction (GBR) / Implant
FOE if vertical
augmentation is needed
Extraction (GBR) / Implant
Intrabony
Defects
1 wall
2 wall
3 wall
1 wall
2 wall
3 wall
Hamp Class II
ENDODONTIC ALGORITHM
(Good Periodontal Prognosis)
ENDODONTIC ALGORITHM
(Fair / Poor Periodontal Prognosis)
FOE Forced Orthodontic Eruption
GBR Guided Bone Regeneration
RCT Root Canal Treatment
S/RP Scaling/Root Planing
GTR Guided Tissue Regeneration
APF Apical Positioned Flap
CAL Clinical Attachment Level
Fig 1 Restorative, endodontic, and periodontal algorithms.
78 VOLUME 44 NUMBEP 1 JANUAPY 2013
QUI NTESSENCE I NTERNATI ONAL
Pet rov et al
PERIODONTAL ALGORITHM
(Questionable Periodontal Prognosis / Non-Molars)
PERIODONTAL ALGORITHM
(Questionable Periodontal Prognosis / Molars)
EXTRACTION ALGORITHM
EXTRACTION
GBR is needed for
Delayed
implant placement
FOE
Staged
treatment Plan
Maintain as
transitional
abutment
No staging,
or vertical
augmentation is
needed
Extraction
(GBR) / Implant
Extraction
Extraction
(GBR) / Implant
QUESTIONABLE
PROGNOSIS IN
NON-MOLARS
Horizontal Bone
Loss
Intrabony
defects
Mobility >1
Mobility <1
Mobility >1
Mobility <1
Extraction
(GBR) / Implant
Extraction
(GBR) / Implant
Extraction
(GBR) / Implant
Extraction
(GBR) / Implant
Periodontal
Reparative
Surgery
1-wall
Intrabony
Defects
2-wall or 3-wall
Intrabony
Defects
Esthetic Zone
Non-Esthetic Zone
Regenerative
Surgery
QUESTIONABLE
PROGNOSIS IN
MOLARS
Interproximal Bone
Height Apical to
Furcation
Intrabony
defects
Mobility >1
Mobility <1
Mobility >1
Mobility <1
Extraction
(GBR) / Implant
Extraction
(GBR) / Implant
Extraction
(GBR) / Implant
Extraction
(GBR) / Implant
Periodontal
Reparative
Surgery
1-wall
Intrabony
Defects
2-wall or 3-wall
Intrabony
Defects
Esthetic Zone
Non-Esthetic Zone
Regenerative
Surgery
2
FOE Forced Orthodontic Eruption
GBR Guided Bone Regeneration
Fig 2 Periodontal and extraction algorithms.
VOLUME 44 NUMBEP 1 JANUAPY 2013 79
QUI NTESSENCE I NTERNATI ONAL
Pet rov et al
Fair periodontal prognosis
Basod on ourront soiontiho ovidonoo, tnoro
is no evidence to support the extraction of
teeth with 25% clinical attachment level
and/or Hamp I furcation involvement.
Furcation plasty in cases of furcation
involvement, different regenerative treat-
ment options in cases of intrabony defects,
and different surgical and nonsurgical treat-
ment options in cases of horizontal bone
loss or shallow vertical defects are predict-
able treatment options.
2325
While all
intrabony defects in this category can be
predictably treated, the literature illustrates
that the best clinical results are in cases of
three-walled defects 4 mm deep.
26
Poor periodontal prognosis
Since correct gingival size and shape
become exceptionally signicant in the suc-
cess of the cases in the esthetic zone (pri-
marily with high smile lines), different
algorithms have been designed for teeth
with poor periodontal prognoses in the
ostnotio and nonostnotio zonos. Posootivo
and regenerative periodontal surgeries,
although successful in decreasing probing
depths, often result in recession of the gin-
gival tissue and interdental papilla.
18
Consequently, the algorithm favors extrac-
tion with subsequent immediate or delayed
implant placement in the esthetic zone,
while the algorithm favors resective or
regenerative periodontal surgery in non-
esthetic zone. Forced orthodontic eruption
is proposed for two- and three-walled
intrabony defects in the esthetic zone to
achieve a more optimal bone architecture
and soft tissue contours.
27
Questionable periodontal
prognosis
Since the prerequisite to successful regen-
eration of intrabony defects is wound stabil-
ity,
25
teeth with mobility > I (Miller
classication) would not be recommended
for retention. However, it is important to note
that mobility by itself is not a prerequisite for
tooth extraction. Teeth with questionable
prognoses,
2
in addition to hypermobility,
present with a poor crown-to-root ratio,
Class II/III furcation involvement, and >50%
clinical attachment loss, and it was the
combination of all the listed factors that
contributed to the questionable algorithm
design.
Extraction algorithm for teeth
with a questionable periodontal
prognosis
The extraction algorithm for questionable
teeth distinguishes questionable teeth that
can be extracted immediately from ques-
tionable teeth that can be used as transi-
tional abutments for a xed prosthesis in a
staged approach.
28
Another important use
of questionable teeth destined for extraction
is that the teeth can be used to augment the
future implant site by forced orthodontic
eruption.
29
The purpose of the following cases is to
illustrate the basic application of the use of
the proposed decision tree algorithms. The
emphasis is placed on the main decision of
whether to maintain or extract the tooth
rather than on the details pertaining to dif-
ferent treatment modalities.
CASE REPORTS
Case 1: Esthetic crown-
lengthening surgery (restorative
algorithm)
A 43-year-old woman presented with the
chief complaint, I am not happy with my
smile. My teeth are short and yellow, and I
am missing teeth on my [mandibular] right
quadrant. I want a nonremovable solution
that will give me better esthetics as now I
can afford it. The patients medical history
was noncontributory, and she was not a
smoker. The initial clinical evaluation
revealed a thick periodontal biotype, as well
as severe tooth structure loss due to attri-
tion and localized abfraction explained by a
history of bruxism (Fig 3a). Upon clinical
examination, her teeth presented with no
mobility and minimal probing depths. Every
tooth tested positive to vitality tests. The
selected treatment plan was to perform
crown lengthening on the maxillary right rst
premolar to left rst premolar and deliver
xed crowns on every tooth to enhance
esthetics and replace missing teeth with a
xed partial denture in the mandibular right
80 VOLUME 44 NUMBEP 1 JANUAPY 2013
QUI NTESSENCE I NTERNATI ONAL
Pet rov et al
Fig 3b Clinical photograph after completion of
crown legthening and restorative treatment demon-
strating mantainance of papilla height and overall
soft tissue esthetics. Photograph courtesy of Dr Eric
Weiss, Clinical Assistant Professor, Department of
Periodontics, UMDNJ, Newark, New Jersey, USA.
Fig 3a Initial clinical photograph demonstrating a
wide band of keratinized tissue, thick biotype, and
severe tooth structure loss. Photograph courtesy of
Dr Eric Weiss, Clinical Assistant Professor, Department
of Periodontics, UMDNJ, Newark, New Jersey, USA.
b a
quadrant, followed by the delivery of a at
plane hard acrylic nightguard to address
the bruxism. This was determined by the
restorative algorithm. Figure 1 (restorative
algorithm) shows the teeth can be restored
without compromising the crown-to-root
ratio.
Full-mouth rehabilitation with a xed
solution targeted all the parients chief com-
plaints (Fig 3b). Soft tissue esthetics were
preserved, in part as a result of preserving
the natural dentition. Even though there is
hard tissue removal during crown lengthen-
ing, this will be at the control of the dentist,
which makes it more predictable and pro-
vides a positive bone architecture to create
and preserve the papillae.
Case 2: Forced orthodontic
extrusion (restorative and
extraction algorithms)
A 59-year-old man presented with pain in
the area of the maxillary left central incisor.
The patients medical history was noncon-
tributory, and he was not a smoker. Clinical
evaluation revealed marginal erythema and
edema, with mesial pocketing (Fig 4a).
Upon radiographic examination, the maxil-
lary left central incisor revealed an end-
odontically treated tooth with a porcelain
crown and evidence of cervical caries, as
well as an intrabony defect on the mesial
suraoo (Fig 4b). Bono noignt on tno ad|a-
cent teeth was adequate. Treatment plans
presented to the patient included forced
eruption with subsequent immediate implant
placement, immediate implant placement,
or a removable partial denture of the maxil-
lary incisors. The patient and clinician opted
for forced orthodontic eruption with subse-
quent implant placement based upon the
extraction algorithm. Forced orthodontic
eruption is indicated to advance the alveo-
lar bone coronally to increase vertical bone
height at the future implant site (Fig 2).
Following scaling and root planing and
oral hygiene instructions, forced eruption
was initiated. Keratinized tissue followed
the eruption pattern of the tooth, and the
occlusion was adjusted by reducing the
height of the crown as eruption occurred
(Fig 4c). The radiograph demonstrated that
the bone structure accompanied the tooth
as it migrated coronally and that resolution
of the mesial intrabony defect was achieved
(Fig 4d). A radiograph was taken after
extraction and immediate implant place-
ment (Fig 4e). A clinical photograph taken
at the 3-month postoperative evaluation
(after implant placement) depicts a provi-
sional crown that is out of occlusion and the
maintenance of papilla height and overall
esthetics (Fig 4f). Implant precise position-
ing was achieved in part by the well-estab-
lished bone morphology. The possibility of
papilla reforming was enhanced as a result
of the coronal migration of the bone in the
interproximal area.
VOLUME 44 NUMBEP 1 JANUAPY 2013 81
QUI NTESSENCE I NTERNATI ONAL
Pet rov et al
Figs 4e and f Final radiograph demonstrates ideal
implant placement and interproximal bone level.
Clinical photograph at 3 months after implant place-
ment and provisional temporization demonstrating
preservation of interproximal papilla height and
keratinized tissue. Photograph courtesy of Dr Eric
Weiss, Department of Periodontics, UMDNJ, Newark,
New Jersey, USA.
Figs 4c and d Clinical photograph and radiograph
after completion of forced orthodontic eruption
depicts keratinized tissue that accompanied the
tooth on its coronal migration and resolution of the
intrabony defect. Photograph courtesy of Dr Eric
Weiss, Department of Periodontics, UMDNJ, Newark,
New Jersey, USA.
Figs 4a and b Initial clinical photograph and radio-
graph demonstrating edema, erythema, and reces-
sion and radiographic evidence of an intrabony
defect as well as cervical caries in the mesial area.
Photograph courtesy of Dr Eric Weiss, Department of
Periodontics, UMDNJ, Newark, New Jersey, USA.
a
b
c
d
e
f
82 VOLUME 44 NUMBEP 1 JANUAPY 2013
QUI NTESSENCE I NTERNATI ONAL
Pet rov et al
Fig 5a Initial clinical radiograph dem-
onstrating radiolucent area involving
both roots granting a diagnosis of an
endodontic-periodontic lesion on the
distal root and endodontic lesion on the
mesial root. Photograph courtesy of Dr
Meghan Hatfeld, endodontics resident,
UMDNJ, Newark, New Jersey, USA.
Fig 5b Radiograph demonstrating suc-
cessful nonsurgical root canal therapy.
Photograph courtesy of Dr Meghan
Hatfeld, endodontics resident, UMDNJ,
Newark, New Jersey, USA.
Fig 5c Radiograph at the 1-year post-
operative visit demonstrating full defect
fll. Photograph courtesy of Dr Meghan
Hatfeld, endodontics resident, UMDNJ,
Newark, New Jersey, USA.
Case 3: Good periodontal
prognosis (endodontic
algorithm)
A 56-year-old woman presented complain-
ing of pain in the area of her mandibular
right rst molar. The patients medical his-
tory revealed high blood pressure that was
controlled by medication. The patient was a
nonsmokor. Padiograpns (Fig 5a) and a
clinical examination revealed an endodon-
ic-periodontic lesion on the distal root, and
an endodontic lesion on the mesial root.
The tooth tested negative for vitality tests,
presented with tenderness to percussion,
and had no mobility. The probing depth on
the direct distal aspect was 13 mm and only
3 mm on the mesial aspect. After all the
diagnostic tests were carried out, the patient
was given a treatment plan consisting non-
surgical root canal therapy followed by
meticulous debridement and scaling and
root planing. This was determined by the
endodontic algorithm. The treatment plan
was accepted by the patient. Endodontic
therapy is recommended for a nonvital tooth
with a fair-to-poor periodontal prognosis
(see Fig 1).
A radiograph was taken immediately
after root canal therapy was completed
(Fig 5b). Successful obturation of the canals
and absence of lling material surpassing
the radiographic apex is visible.
Padiograpnio ovidonoo o tno rosolution o
the defect is observed (Fig 5c), which was
conrmed by intraoral probing examination.
Case 4: Hamp degree II
furcation involvementpoor
prognosis in the nonesthetic
zone (periodontal algorithm)
A 52-year-old woman presented with Hamp
degree II furcation involvement at the maxil-
lary right rst molar. The patients medical
history was noncontributory, and she was
not a smoker. An initial radiograph clearly
depicted a furcation defect with interproxi-
mal bone levels adequate enough to con-
sider regeneration as a primary treatment
option (proximal bone coronal to the furca-
tion) (Fig 6a) (see Fig 2). The tooth tested
positive for vitality tests and presented with
no mobility. Treatment plans presented to
the patient included extraction/grafting fol-
lowed by implant placement or periodontal
regeneration. After discussing the therapy,
prognoses, and algorithm choices (poor
periodontal prognosis algorithm/degree II
furcation), the patient selected periodontal
regeneration. A tooth with an interproximal
bone height coronal to the furcation, with
VOLUME 44 NUMBEP 1 JANUAPY 2013 83
QUI NTESSENCE I NTERNATI ONAL
Pet rov et al
Fig 6a Hamp degree II furcation with enough
interproximal bone height to consider regeneration
therapy. Photograph courtesy of Dr Tat Chiang,
Department of Periodontics, UMDNJ, Newark, New
Jersey, USA.
Fig 6b Radiographic evidence of complete defect
fill at the 1-year postoperative evaluation.
Photograph courtesy of Dr Tat Chiang, Department
of Periodontics, UMDNJ, Newark, New Jersey, USA.
Hamp II furcation classication, is recom-
mended to undergo regeneration therapy
(poor periodontal prognosis algorithm [see
Fig 1]).
A radiograph at the 1-year postoperative
evaluation, after regeneration, suggests
defect resolution with preservation of the
interproximal bone height (Fig 6b).
CONCLUSION
The innovative algorithmic approach pre-
sented in this article may be used by clini-
cians to aid in their thinking process about
whether to save or extract compromised
teeth. It is imperative to note that the algo-
rithms were simplied for the purpose of
clarity by not including such variables such
as systemic health, nances, psychologic
factors, strategic position of the tooth, etc.
These variables will differ from patient to
patient and should be incorporated in the
decision-making process on an individual
basis. For example, in cases in which the
psychologic state of the patient precludes
extraction, heroic therapy with strict mainte-
nance regimen should be attempted since
edentulism signicantly affects patients
quality of life.
30
While we did not discuss
edentulism in this paper, and implant thera-
py was always an option, in cases of failed
osseointegration, psychologic consequen-
ces in these patient groups are inevitable.
Furthermore, with current advances in
growth factors, tissue engineering, and
restorative biomaterials (optimization in
periodontal, endodontic, and restorative
therapies), the authors anticipate the algo-
rithms will have to be constantly revisited
and updated.
REFERENCES
1. Samet N, Jotkowitz A. Classifcation and Prognosis
evaluation of Individual teeth: A Comprehensive
Approach. Quintessence Int 2009;40:377387.
2. McGuire MK, Nunn ME. Prognosis versus actual out-
come. III. The efectiveness of clinical parameters in
accurately predicting tooth survival. J Periodontol
1996;67:666674.
3. Kwok V,Caton JG.Commentary: Prognosis revisited:
A system for assigning periodontal prognosis. J
Periodontol 2007;78:20632071.
4. Ghiai S, Bissada NF. Prognosis and actual treat-
ment outcome of periodontally involved teeth.
Periodontal Clin Invest 1996;18:711.
84 VOLUME 44 NUMBEP 1 JANUAPY 2013
QUI NTESSENCE I NTERNATI ONAL
Pet rov et al
5. Fardal O, Johannessen AC, Linden G. Tooth loss
during maintenance following periodontal treat-
ment in a periodontal practice in Norway. J Clin
Periodontol 2004;31:550555.
6. Checchi L, Montevecchi M, Gatto MR, et al.
Retrospective study of tooth loss in 92 treated peri-
odontal patients. J Clin Periodontol 2002;29:651656.
7. Slowinski R. Intelligent Decision Support: hand-
book of applications and advances of the rough
sets theory. Dordrecht: Kluwer Academic Publishers
1992.
8. Avila G, Galindo-Moreno P, Soehren S, Misch C,
Morelli T, Wang HL. A Novel decision-making pro-
cess for tooth retention or extraction. J Periodontol
2009;3:476491.
9. Greenstein G, Greenstein B, Cavallaro J. Prerequisite
for treatment planning implant dentistry: peri-
odontal prognostication of compromised teeth.
Compendium 2007;28:436444.
10. Fan J, Nunn ME, Su X. Multivariate exponential sur-
vival trees and their application to tooth prognosis.
Comp Stat Data Anal 2009;53:1110-1121.
11. American Heritage Dictionary, 4
th
ed. Houghton
Mufn Company, 2006:946.
12. Doyle SL, Hodges JS, Pesun IJ, Law AS, Bowles WR.
Retrospective cross sectional comparison of initial
nonsurgical endodontic treatment and single-tooth
implants. J Endod 2006;32:822827.
13. Iqbal MK, Kim S. A review of factors Infuencing treat-
ment planning decisions of single-tooth implants
versus preserving natural teeth with nonsurgical
endodontic therapy. J Endod 2008;34:519529.
14. Immura N, Pinheiro ET, Gomes B, Zaia AA, Ferraz
C, Souza-Filho FJ. The outcome of endodontics
treatment: a retrospective study of 2000 cases per-
formed by a specialist. J Endod 2007;33:12781282.
15. European Society of Endodontology. Consensus
report of the European Society of Endodontology
on quality guidelines for endodontic treatment. Int
Endod J 1994;27:115124.
16. Olsson M, Lindhe J. Periodontal characteristics in
individuals with varying forms of the upper central
incisors. J Clin Periodontol 1991;18:7882.
17. Christensen GJ. Implant therapy versus endodontic
therapy. Am Dent Assoc 2006;137:14401443.
18. Chen ST, Buser D. Clinical and esthetic outcomes
of implants placed in postextraction sites. Int J Oral
Maxillofac Implants 2009;24(suppl):186217.
19. Torabinejad M, Goodacre CJ. Endodontic or dental
implant therapy: the factors afecting treatment
planning. J Am Dent Assoc 2006;137:973977.
20. Greenstein G, Cavallaro J, Tarnow D. When to save
or extract a tooth in the esthetic zone: a commen-
tary. Compendium 2008;29:136146.
21. Grossman Y, Sadan A. The prosthodontic concept
of crown-to-root ratio: A review of the literature. J
Prosth Dent 2005;93:559562.
22. Schillinburg HT Jr, Hobo S, Whitsett LD, et al.
Fundamentals of Fixed Prosthodontics. 3rd ed.
Chicago, IL: Quintessence Publishing, 1997:8990.
23. Hamp SE, Nyman S, Lindhe J. Periodontal treatment
of multi-rooted teeth. Results after 5 years. J Clin
Periodontol 1975;2:126135.
24. Nevins M, Camelo M, Nevins ML, Schenk RK, Lynch
SE. Periodontal regeneration in humans using
recombinant human platelet-derived growth
factor-BB (rhPDGF-BB) and allogenic bone. J
Periodontol 2003;74:12821292.
25. Wang H-L. Position Paper: Periodontal Regeneration.
J Periodontol 2005;76:16011622.
26. Laurell L, Gottlow J, Zybutz M, Persson R.
Treatment of intrabony defects by diferent surgi-
cal procedures. A literature review. J Periodontol
1998;69:303313.
27. Salama H, Salama M. The role of orthodontic extru-
sive remodeling. Int J Periodontics Restorative Dent
1993;13:313333.
28. Drew HJ, Alnassar T, Gluck K, Rynar JE. Consideration
for a staged approach in implant dentistry.
Quintessence Int 2012;43:2936.
29. Celenza F. The development of forced eruption as
a modality for implant site enhancement. Alpha
Omegan 1997;90(2):4043.
30. Allen PF, McMillan AS. A longitudinal study of
quality of life outcomes in older adults requesting
implant prosthesis and complete removable den-
tures. Clin Oral Implants Res 2003;14:173179.
You might also like
- Patient Centered Pharmacology Tindall William N Sedrak Mona M Boltri John M SRG PDFDocument575 pagesPatient Centered Pharmacology Tindall William N Sedrak Mona M Boltri John M SRG PDFTedpwer100% (3)
- Sorting Out Endodontic Symptoms: ©JK Mitchell, DDS, Med April 2012Document2 pagesSorting Out Endodontic Symptoms: ©JK Mitchell, DDS, Med April 2012sao_tren_troi100% (1)
- Cone Beam Computed Tomography: Oral and Maxillofacial Diagnosis and ApplicationsFrom EverandCone Beam Computed Tomography: Oral and Maxillofacial Diagnosis and ApplicationsDavid SarmentNo ratings yet
- Peri-Implantitis: Presented By: Kriti Dalmia. Moderated By: Dr. Shobha RDocument29 pagesPeri-Implantitis: Presented By: Kriti Dalmia. Moderated By: Dr. Shobha RDr Farhat100% (1)
- Osteopathic Considerations in Systemic Dysfunction (2nd Ed)Document296 pagesOsteopathic Considerations in Systemic Dysfunction (2nd Ed)Natan Babek100% (1)
- Statistics and Propaganda: by Jon RappoportDocument6 pagesStatistics and Propaganda: by Jon RappoportSkogspilen Sprett100% (1)
- Inlay Onlay Parte 222 PDFDocument23 pagesInlay Onlay Parte 222 PDFKhenny Jhynmir Paucar VillegasNo ratings yet
- Antibiotics in Periodontics PerioDocument51 pagesAntibiotics in Periodontics PerioSiddhartha BanerjeeNo ratings yet
- Supportive Periodontal TreatmentDocument29 pagesSupportive Periodontal TreatmentAtul Koundel100% (2)
- Regressive Changes of TeethDocument45 pagesRegressive Changes of TeethNader AlaizariNo ratings yet
- Introduction To ProsthodonticsDocument98 pagesIntroduction To ProsthodonticsmarwaNo ratings yet
- RecessionsDocument68 pagesRecessionsmaryamNo ratings yet
- Treatment Planning Single Maxillary Anterior Implants for DentistsFrom EverandTreatment Planning Single Maxillary Anterior Implants for DentistsNo ratings yet
- The Single-Tooth RestorationDocument5 pagesThe Single-Tooth Restorationumerjaved86No ratings yet
- Odontogenic Cysts Summary Chart: Radicular Cyst (Periapical Cyst)Document4 pagesOdontogenic Cysts Summary Chart: Radicular Cyst (Periapical Cyst)ML90No ratings yet
- Restoration of Endodontically Treated TeethDocument7 pagesRestoration of Endodontically Treated TeethCattleya Tanosselo100% (1)
- Ridge Preservation for Implant TreatmentDocument24 pagesRidge Preservation for Implant TreatmentFadly RasyidNo ratings yet
- CHAPTER 13. Interdisciplinary ConsiderationsDocument13 pagesCHAPTER 13. Interdisciplinary ConsiderationsAlina AnechiteiNo ratings yet
- 1 Cbct-Evaluation of Remaining Dentin Thickness and Fracture Resistance of Conventional and Conservative Access and Biomechanical Preparation in Molars Using Cone-beam Computed Tomography- An in Vitro StudyDocument4 pages1 Cbct-Evaluation of Remaining Dentin Thickness and Fracture Resistance of Conventional and Conservative Access and Biomechanical Preparation in Molars Using Cone-beam Computed Tomography- An in Vitro StudyalbertaugustineNo ratings yet
- CNL Final Exam Study GuideDocument15 pagesCNL Final Exam Study GuideGelsey Gelsinator JianNo ratings yet
- Renvert Et Al (2018) - Peri Implant Health, Peri Implant Mucositis, and Peri Implantitis - Case Definitions and Diagnostic Considerations - 1Document9 pagesRenvert Et Al (2018) - Peri Implant Health, Peri Implant Mucositis, and Peri Implantitis - Case Definitions and Diagnostic Considerations - 1FelipeOyarceSalazarNo ratings yet
- Bioclear Posterior KitDocument32 pagesBioclear Posterior KitSilvio DTNo ratings yet
- Advance in MaterialsDocument10 pagesAdvance in Materialssami robalinoNo ratings yet
- Lasers in PeriodonticsDocument61 pagesLasers in PeriodonticsDrRanjeet Kumar ChaudharyNo ratings yet
- Conservative Endodontics Textbooks PDFDocument1 pageConservative Endodontics Textbooks PDFVenkatesh Gavini0% (1)
- Retreatment in Persistent Apical PeriodontitisDocument169 pagesRetreatment in Persistent Apical PeriodontitisAnciya NazarNo ratings yet
- Journal of EndodonticsDocument220 pagesJournal of EndodonticsFauzan100% (2)
- Tips On Access Cavity Preparation.: How To' TechniqueDocument4 pagesTips On Access Cavity Preparation.: How To' TechniqueGoran TosicNo ratings yet
- Relationship Between Bruxism and Temporomandibular Disorders: A Systematic Review of Literature From 1998 To 2008Document25 pagesRelationship Between Bruxism and Temporomandibular Disorders: A Systematic Review of Literature From 1998 To 2008AARON DIAZ RONQUILLONo ratings yet
- Rationale For Dental ImplantsDocument18 pagesRationale For Dental ImplantsSamir Nayyar100% (1)
- An Alternative Treatment Approach To Gingival Recession: Gingiva-Colored Partial Porcelain Veneers: A Clinical ReportDocument22 pagesAn Alternative Treatment Approach To Gingival Recession: Gingiva-Colored Partial Porcelain Veneers: A Clinical ReportSoumya Promod100% (1)
- 001 Hilton Dr. Directory 2Document20 pages001 Hilton Dr. Directory 2Muhammad Siraj KhanNo ratings yet
- ARMAMENTARIUMDocument105 pagesARMAMENTARIUMchanaish6No ratings yet
- Smile Line and Periodontium Visibility: Clinical and Research ReportDocument9 pagesSmile Line and Periodontium Visibility: Clinical and Research ReportMed-Amine TouloutNo ratings yet
- MdsDocument356 pagesMdsARJUN SreenivasNo ratings yet
- Modern Endodontic Access and Directly Conserving DentinDocument5 pagesModern Endodontic Access and Directly Conserving Dentinizeldien5870No ratings yet
- Jung 2018Document11 pagesJung 2018Sebastien MelloulNo ratings yet
- Direct Posterior Restoration PDFDocument14 pagesDirect Posterior Restoration PDFياسر نادر حسين فليحNo ratings yet
- Clinical Applications of Digital Dental TechnologyDocument397 pagesClinical Applications of Digital Dental TechnologyTheo_96100% (1)
- New Microsoft Office Word DocumentDocument3 pagesNew Microsoft Office Word DocumentAtulsanapNo ratings yet
- Literature GuideDocument60 pagesLiterature Guide12345sagarNo ratings yet
- Failure of Root Canal Treatment PDFDocument2 pagesFailure of Root Canal Treatment PDFMelissaNo ratings yet
- Porcelain Fused To Metal (PFM) Crowns and Caries in Adjacent TeetDocument5 pagesPorcelain Fused To Metal (PFM) Crowns and Caries in Adjacent Teetbaiq rengganis dewiNo ratings yet
- Is CBCT Necessary For Implant PlacementDocument5 pagesIs CBCT Necessary For Implant PlacementcopyourpairNo ratings yet
- Surgical Extrusion: A Dental TechniqueDocument6 pagesSurgical Extrusion: A Dental TechniqueDragos CiongaruNo ratings yet
- Management of Intricate S-Shaped Root Canals - An Endodontist's ChallengeDocument4 pagesManagement of Intricate S-Shaped Root Canals - An Endodontist's ChallengeAdvanced Research PublicationsNo ratings yet
- Guidelines for Surgical Endodontic ProceduresDocument11 pagesGuidelines for Surgical Endodontic ProceduresgrzeniouNo ratings yet
- Journal of Prosthetic DentistryDocument7 pagesJournal of Prosthetic DentistryAmar BhochhibhoyaNo ratings yet
- Polyetheretherketone PEEK Dental Implants A Case FDocument8 pagesPolyetheretherketone PEEK Dental Implants A Case FPhoebe David100% (1)
- Working LengthDocument67 pagesWorking LengthnishthaNo ratings yet
- Esthetic Considerations in Interdental Papilla PDFDocument11 pagesEsthetic Considerations in Interdental Papilla PDFXavier AltamiranoNo ratings yet
- Thick vs. Thin Gingival Biotypes: A Key Determinant in Treatment Planning For Dental ImplantsDocument6 pagesThick vs. Thin Gingival Biotypes: A Key Determinant in Treatment Planning For Dental ImplantsLuiz Guilherme Loivos100% (1)
- Australian Dental Journal Reviews Interim Restorations During Endodontic TreatmentDocument17 pagesAustralian Dental Journal Reviews Interim Restorations During Endodontic TreatmentKaren RodNo ratings yet
- 2 Nonsurgical Periodontal Therapy - Pocket DentistryDocument14 pages2 Nonsurgical Periodontal Therapy - Pocket DentistryRizki OktavianiNo ratings yet
- Review Peek PDFDocument11 pagesReview Peek PDFAlexandra Dumitrache100% (1)
- A Guide To Succeeding in The Df1 Interview (Sample Pages Only)Document15 pagesA Guide To Succeeding in The Df1 Interview (Sample Pages Only)jaipald9067% (3)
- Bopt PanizDocument9 pagesBopt PanizIvan CarreraNo ratings yet
- AGGRESSIVE PERIODONTITIS: AN INTRODUCTIONDocument101 pagesAGGRESSIVE PERIODONTITIS: AN INTRODUCTIONdileep900100% (1)
- Operative Dentistry: Patient Evaluation, Diagnosis and Treatment PlanningDocument5 pagesOperative Dentistry: Patient Evaluation, Diagnosis and Treatment PlanningMohammed100% (1)
- Endodontic Failures-A Review: Dr. Sadashiv Daokar, DR - Anita.KalekarDocument6 pagesEndodontic Failures-A Review: Dr. Sadashiv Daokar, DR - Anita.KalekarGunjan GargNo ratings yet
- Denture Related StomatitisDocument8 pagesDenture Related StomatitisLike OliviaNo ratings yet
- Definition:: Types of Forceps Used For Tooth ExtractionDocument28 pagesDefinition:: Types of Forceps Used For Tooth Extractionayman moaed alyasen100% (1)
- Article 009Document9 pagesArticle 009MedstudNo ratings yet
- Essential Tissue Healing of the Face and NeckFrom EverandEssential Tissue Healing of the Face and NeckRating: 5 out of 5 stars5/5 (2)
- Antigen-Presentation and The Role of Dendritic Cells in PeriodontitisDocument23 pagesAntigen-Presentation and The Role of Dendritic Cells in PeriodontitiskochikaghochiNo ratings yet
- 3mespe Cements v5Document12 pages3mespe Cements v5kochikaghochiNo ratings yet
- Cytokine Gene Polymorphism and Immunoregulation in Periodontal DiseaseDocument25 pagesCytokine Gene Polymorphism and Immunoregulation in Periodontal DiseasekochikaghochiNo ratings yet
- Per I Tons IllerDocument25 pagesPer I Tons IllerkochikaghochiNo ratings yet
- 14Document13 pages14kochikaghochiNo ratings yet
- Ijp 18 5 Editorial 1Document3 pagesIjp 18 5 Editorial 1kochikaghochiNo ratings yet
- Ijp 18 5 Hassel 11Document5 pagesIjp 18 5 Hassel 11kochikaghochiNo ratings yet
- Ijp 18 5 Mack 9Document6 pagesIjp 18 5 Mack 9kochikaghochiNo ratings yet
- Ijp 18 5 Coward 8Document9 pagesIjp 18 5 Coward 8kochikaghochiNo ratings yet
- 15Document9 pages15kochikaghochiNo ratings yet
- Ijp 18 5 Elmowafy 13Document2 pagesIjp 18 5 Elmowafy 13kochikaghochiNo ratings yet
- Ijp 18 5 Grandini 7Document6 pagesIjp 18 5 Grandini 7kochikaghochiNo ratings yet
- Effect of Original Water Content in Acrylic Resin On Processing ShrinkageDocument2 pagesEffect of Original Water Content in Acrylic Resin On Processing ShrinkagekochikaghochiNo ratings yet
- 10Document10 pages10kochikaghochiNo ratings yet
- Peri-Implant Bone Loss As A Function of Tooth-Implant DistanceDocument7 pagesPeri-Implant Bone Loss As A Function of Tooth-Implant DistancekochikaghochiNo ratings yet
- 11Document16 pages11kochikaghochiNo ratings yet
- The Use of Oral Implants in Compromised Patients: Daniel Van SteenbergheDocument3 pagesThe Use of Oral Implants in Compromised Patients: Daniel Van SteenberghekochikaghochiNo ratings yet
- Ijp 18 5 Botelho 2Document6 pagesIjp 18 5 Botelho 2kochikaghochiNo ratings yet
- 6Document15 pages6kochikaghochi100% (1)
- 8Document15 pages8kochikaghochiNo ratings yet
- 9Document14 pages9kochikaghochiNo ratings yet
- Preoperative Radiologic Planning of Implant Surgery in Compromised PatientsDocument14 pagesPreoperative Radiologic Planning of Implant Surgery in Compromised PatientskochikaghochiNo ratings yet
- 14Document10 pages14kochikaghochiNo ratings yet
- 7Document8 pages7kochikaghochiNo ratings yet
- 5Document13 pages5kochikaghochiNo ratings yet
- 3Document10 pages3kochikaghochiNo ratings yet
- 4Document18 pages4kochikaghochiNo ratings yet
- Diagnosis of Periodontal Manifestations of Systemic DiseasesDocument13 pagesDiagnosis of Periodontal Manifestations of Systemic DiseaseskochikaghochiNo ratings yet
- 11Document39 pages11kochikaghochiNo ratings yet
- 12Document13 pages12kochikaghochiNo ratings yet
- Test Bank For Ethics and Law in Dental Hygiene 3rd Edition by BeemsterboerDocument36 pagesTest Bank For Ethics and Law in Dental Hygiene 3rd Edition by Beemsterboertyphous.madrierdvfzai100% (46)
- Registered Health Information Technician Rhit Exam Content OutlineDocument2 pagesRegistered Health Information Technician Rhit Exam Content Outlineapi-278092659No ratings yet
- Administering Intramuscular Injections To Children - What Does The Evidence Say?Document8 pagesAdministering Intramuscular Injections To Children - What Does The Evidence Say?ZACHARIAH MANKIRNo ratings yet
- Confidential United Nations Nations Unies Employment Medical Review QuestionnaireDocument2 pagesConfidential United Nations Nations Unies Employment Medical Review QuestionnaireHaythem FarhatiNo ratings yet
- 2016 Issue 1Document86 pages2016 Issue 1Fareesha KhanNo ratings yet
- Obesity The Number 1 Problem in America Reading Comprehension Exercises 31128Document3 pagesObesity The Number 1 Problem in America Reading Comprehension Exercises 31128Dixon adolfo Tapia arayaNo ratings yet
- Work-Based Learning in Nursing Education: The Value of PreceptorshipsDocument5 pagesWork-Based Learning in Nursing Education: The Value of Preceptorshipssyamsul anwarNo ratings yet
- Analysis of Us Health Care PolicyDocument7 pagesAnalysis of Us Health Care Policyapi-520841770No ratings yet
- Gene Therapy For Parkinson's DiseaseDocument2 pagesGene Therapy For Parkinson's DiseaseBhaswan Indu JanaNo ratings yet
- Uri Flush 3 Liquid Stones ProblemDocument4 pagesUri Flush 3 Liquid Stones ProblemSourabh KoshtaNo ratings yet
- Comprehensive Cancer Care CenterDocument40 pagesComprehensive Cancer Care CenterKINJALNo ratings yet
- MANAGING DOG/CAT BITES AT HEALTH FACILITYDocument5 pagesMANAGING DOG/CAT BITES AT HEALTH FACILITYleo89azman100% (1)
- Group 1 PWC and Group 2 PWC No Power OptionsDocument3 pagesGroup 1 PWC and Group 2 PWC No Power OptionslisamaurerNo ratings yet
- Nursing Informatics 453X Assessment 1 Foundations of HealthDocument3 pagesNursing Informatics 453X Assessment 1 Foundations of Healthjames mwangiNo ratings yet
- Compensation Fy2018sDocument218 pagesCompensation Fy2018sJesse YoungbloodNo ratings yet
- Ma. Lammatao: Trion AKG Marble LLCDocument11 pagesMa. Lammatao: Trion AKG Marble LLCNasir AhmedNo ratings yet
- VRBPAC 12.10.20 Meeting Briefing Document FDADocument53 pagesVRBPAC 12.10.20 Meeting Briefing Document FDAZerohedge100% (2)
- Population Dynamics and Control of ContraceptionDocument16 pagesPopulation Dynamics and Control of Contraceptionjaish8904No ratings yet
- ScheduleDocument52 pagesSchedulerohitNo ratings yet
- Demography: Sources of Demographic DataDocument8 pagesDemography: Sources of Demographic DataSHERMINA HASANNo ratings yet
- HB Year 1 and 2 MBBS Programme Handbook - Apr 2018Document149 pagesHB Year 1 and 2 MBBS Programme Handbook - Apr 2018Peter GadielNo ratings yet
- Quality Issu in Midwifery ICM PDFDocument9 pagesQuality Issu in Midwifery ICM PDFFarhatiNo ratings yet
- Artikel Efek Menyusui Terhadap Perubahan Berat Badan Pada Wanita JepangDocument13 pagesArtikel Efek Menyusui Terhadap Perubahan Berat Badan Pada Wanita JepangSuredaNo ratings yet
- Igims Directory PDFDocument28 pagesIgims Directory PDFBambam KumarNo ratings yet
- ImmunizationDocument2 pagesImmunizationannamcconkeyNo ratings yet